Abstract
Background
Undernutrition is the leading cause of mortality among children infected with HIV particularly in resource-deprived settings. Despite several studies were disclosed the effect of undernutrition on mortality of children living with HIV in Ethiopia, the findings were fragmented and inconclusive. Therefore, this review aimed to determine the pooled effects of undernutrition on mortality of children infected with HIV in Ethiopia.
Methods
The search were performed using international online electronic data bases (MEDLINE/though PubMed, Google scholar, Hinari, Scopus and open Google). The review included only retrospective/prospective cohort studies reporting the effects of undernutrition on mortality of children infected with HIV. Heterogeneity between included studies was assessed using Cochrane Q-test and the I2 statistics. Sub-group analysis was done by study regions, sample size and publication year.
Results
A total of 1345 articles were identified from databases. Among these, 14 studies met the inclusion criteria and included in the study. Meta-analysis of 4 studies revealed that stunting has a significant effect on mortality of children infected with HIV (AHR: 3.36; 95 % CI: 2.95–3.77). Of 14 included studies, 6 articles indicated that wasting has a significant effect on mortality in children infected with HIV (AHR: 3.93; 95 % CI: 2.56–5.30) as compared to their counterparts. Furthermore, the pooled effect of 8 studies showed that underweight has 3.4 times hazard of death among children who lived with HIV as compared to well-nourished children.
Conclusion
This review revealed that undernutrition has deleterious effect on mortality of children infected with HIV/AIDS by disease progression and prone the children to serious opportunistic infections. From the study, the authors recommended that nutritional status of children on antiretroviral therapy need to be evaluated regularly.
Keywords: Children living with HIV, Undernutrition, Effect, Ethiopia
1. Introduction
Human Immunodeficiency Virus (HIV) is still remaining a major public health concern [1,2] which cause the death of 40.1 million people worldwide since the start of the epidemic [3]. Globally, at the end of 2021, there were an estimated 38.4 million people living with HIV, of which 1.7 million were children aged less than 15 years [4]. Sub-Saharan Africa is heavily affected region in the globe which is home to two-thirds of all people living with HIV [5].
Children and adolescents are among the most victimized groups of all populations for infection, morbidity and mortality of HIV/AIDS. Worldwide, about 5 percent of all people living with HIV are under 15 years of age, and 15 percent of all AIDS-related deaths [6,7]. Although the use of Antiretroviral Therapy (ART) sunstanicially decrease AIDS-related mortality [8], in resource-limited settings the mortality risk due to HIV/AIDS is still high among children [9]. Evidences indicated that among HIV-infected children who admitted to hospital, about 14 % were died [10]. A similar evidence also disclosed that the overall mortality of HIV-infected children were 24 % [9]. A systematic review and meta-analysis studies conducted in Sub-Saharan Africa showed that the pooled proportion of mortality among HIV-infected children was 7.9 % [1].
Undernutrition in the form of (wasting, stunting and underweight) is the leading cause of morbidity, low survival and mortality among children infected with HIV particularly in resource-deprived settings [[11], [12], [13]].In fact, initiation of ART dramatically reduce HIV/AIDS-related morbidity, mortality, and boost survival rate [[14], [15], [16]]. However, the responses of HIV-infected children for HAART(Highly Active Antiretroviral Therapy) are not similar to adults, because of deleterious impacts of the virus on the immature immunity system, nutritional status and negative consequence on the immunologic response of children living with HIV [8,17]. Undernutrition, especially severe acute malnutrition (SAM) decreased the numbers of T-helper cells, cytotoxic T-cells, and natural killer cells and predisposing children to opportunistic infections [18,19].
HIV- infection and undernutrion coexists in a viscous cycle and deadly duo with each one fuelling the other [11,20]. Children living with HIV are more vulnerable to undernutrition [21] due to several mechanisms: HIV- infection exposed children for decreased appetite [22], increase energy needs as a result of infection, exacerbating of gastrointestinal infections, enteropathy and food insecurity [20]. Moreover, children with HIV are prone to undernutrion due to reduced food intake resulting from decreased appetite [23], poor absorption of nutrients that result of recurrent or chronic diarrhea [24], increased energy needs as a result of virus replication and opportunistic infections [25]. Undernutrition on its part increases susceptibility to infection by causing immune dysfunction in manifold ways and it adds fuel to the fire by accelerating the progress of HIV- infection to AIDS [11,19].
Ethiopia has been planned and endorsed nutritional care and support program as a cost-effective strategy in the management of HIV/AIDS patients to reduce morbidity and mortality [25,26]. Despite these interventions, undernutrition is continued to be a major predictor of morbidity and mortality of people with HIV, particularly children are among the most victimized populations [12,15,24,27]. Even though there is common understanding that HIV and undernutrion are intricate and intertwined to predict mortality and decrease survival rate, there is a lacking of comprehensive nationally pooled evidence estimating the pooled effects of undernutrition on mortality among children living with HIV.
In Ethiopia several studies were conducted and disclosed the effect of undernutrition on mortality of children with HIV [12,[28], [29], [30], [31], [32], [33], [34], [35]]. However, there were a fragment and inconclusive among studies finding. Therefore, the review aimed to determine the pooled effects of undernutrition on mortality among children living with HIV in Ethiopia. Evidences reported from this study will be used as one input for program planners and decision-makers in designing strategies to halt undernutrition related mortality among children living with HIV and to achieve the target held by 2025.
2. Methods
2.1. Search strategy
The search were performed using international online electronic data bases (MEDLINE/though PubMed, Google scholar, Hinari, Scopus and open Google). Additionally, unpublished papers were reviewed out from research centers and library sources as well as the hand search of reference lists of eligible articles were also searched. Searches were limited to full text articles, human studies and English language studies. Using pre-determined search terms/keywords and MeSH terms, the following search map was built: Undernutrition OR malnutrition OR “nutritional deficienc*” OR malnourish* OR "Nutritional Status"[Mesh] OR “nutritional status” OR stunting OR Wasting OR underweight OR “micronutrient deficienc*” OR “Thinness"[Mesh] AND "Mortality"[Mesh] OR Mortality OR survival OR “death rate” OR “risk factors” OR “time to death” OR “case fatality rate” OR “mortality rate” AND "Child"[Mesh] OR child* OR pediatric* OR paediatric* AND "Antiretroviral Therapy” OR “Highly Active"[Mesh] OR "anti-retroviral agents" OR "anti-retroviral agents"[MeSH] OR “antiretroviral treatment” OR “anti-retroviral therapy” AND "Ethiopia"[Mesh] OR Ethiopia (S1 Table). To access the eligible articles, the adapted PICO framework was used. This review was prospectively registered at the Prospero with a registration number of CRD42023448563.
2.2. Inclusion and exclusion criteria
The review included only retrospective/prospective cohort studies that report the adjusted pooled effects of undernutrition on mortality of children with HIV. However, articles with no full texts, case series, case reports, case control, cross-sectional and qualitative studies were excluded from this study. The study was selected if their publication period is between 2008 and 2023 as the revised version of national guidelines for HIV/AIDS and nutrition developed in 2008 [25].
2.3. Outcome measurement
This study primarily focuses on the pooled effect of undernutrition (stunting, wasting and underweight) reported from primary studies on mortality and survival of children infected with HIV. Stunting(height for age < −2Zscore), wasting (Weight for height < -2Z score) and underweight (Weight for age < −2Z score) [36].
2.4. Quality assessment
The quality of included studies were appraised using the Joanna Briggs Institute (JBI) critical appraisal checklists for cohort studies [37]. Accordingly, all eligible studies were critically appraised by two independent reviewers (TMA and SZ) and scored for the validity of their results. Arguments between reviewers were settled through discussion. Based on this, among 14 included articles nine studies were scored 9 out of 11 questions 82 %(low risk).Whereas, 4 of them scored 8 out of 11 questions 73 %(low risk) and one study score 7 out of 11 questions(low risk)(S1 checklist). Studies were considered to be low risk when scored 50 % or higher on the quality assessment tools [37]. Thus, the quality of all the included studies was high.
2.5. Data extraction
The relevant data were extracted by two authors (AK& DK) by using standardized JBI data extraction format [38]. Any discrepancies between two authors were handled by discussion. For each included study; first author name, publication year, study region, study design, study setting, sample size, adjusted hazard ratio with 95 % confidence intervals (CI),standard error and follow-up period were extracted on Microsoft excel spread sheet.
2.6. Statistical analysis
STATA version17 software was used for meta-analysis of extracted data to determine the pooled effect size. The presence of heterogeneity between included studies was assessed using Cochrane Q-test and the I2 statistics [39]. To adjust random variation in the presence of significant heterogeneity between primary studies, sub-group analysis was done by study regions, sample size and publication year. Furthermore, the presence of publication bias was checked through graphical (funnel plot) and statistical (Egger's) test.
3. Results
3.1. Study identification
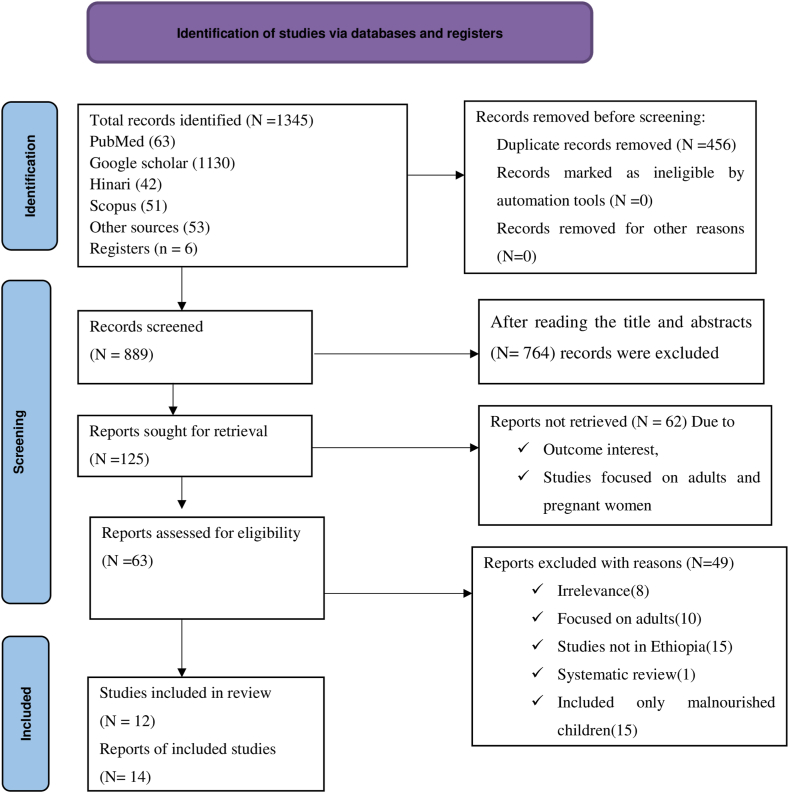
A total of 1345 articles were identified from different electronic databases and other approach of searching methods. After removal of 456 duplicate studies, 889 studies were remained for the next screening. Reading the title and abstracts, 764 articles were removed as they are not relevant for this systematic review. Again after evaluating full text articles, 125 reports were retrieved. Next, 62 studies were removed as studies did not report data on the outcome interest, report only descriptive statics and studies focused on adults and pregnant women. Finally, 14 studies were included for analysis after removal of 49 studies with reasons (Fig. 1).
Fig. 1.
PRISMA flow diagram of article selection for systematic review and meta-analysis of the Effects of undernutrion on mortality of children after initiation of Antiretroviral Therapy in Ethiopia.
3.2. Characteristics of included studies
This systematic review included 14 studies from different regions of Ethiopia with a total sample size of 5491 children living with HIV and all are retrospective cohort studies. The sample size was ranged from 222 in South Nation and Nationalities and Peoples Regional States (SNNPRS) [40] to 721 in Benishangul Gumuz regional state [31].The highest mortality rate was reported as (22.9 %) in Amhara region [14] while the least (4.2 %) was reported from study done in Benishangul Gumuz region [31]. Concerning the study settings, six studies were from Amhara region [12,14,34,35,41,42], one from Oromia [32], four studies from SNNPRS [29,30,40,43], two from Addis Ababa [28,33] and one study from Benishangul Gumuz region [31](Table 1).
Table 1.
Characteristics of the included studies of effects of undernutrion on mortality of children living with HIV in Ethiopia.
| S.N | Author/year | Study region | Study Design |
Sample size | Overall mortality (%) | Quality score |
|---|---|---|---|---|---|---|
| 1 | Adem, A.k. et al.,[2014] [32] | Oromia | Retrosp-cohort | 560 | 43(7.6) | Low risk |
| 2 | Alebel, A. et al.,[2018] [12] | Amhara | Retrosp-cohort | 390 | 38(9.7) | Low risk |
| 3 | Alebel, A. et al.,[2020] [34] | Amhara | Retrosp-cohort | 538 | 38(7.1) | Low risk |
| 4 | Arage, G. et al.,[2019] [14] | Amhara | Retrosp-cohort | 426 | 97(22.9) | Low risk |
| 5 | Ashagre, S. et al.,[2012] [40] | SNNPRS | Retrosp-cohort | 222 | 26(11.7) | Low risk |
| 6 | Bitew, s. et al.,[2017] [27] | SNNPRS | Retrosp-cohort | 228 | 16(7) | Low risk |
| 7 | Biyazin, Y. et al.,[2022] [35] | Amhara | Retrosp-cohort | 251 | 16(6.4) | Low risk |
| 8 | Chekole,B. et al., [2022] [41] | Amhara | Retrosp-cohort | 588 | 27(4.6) | Low risk |
| 9 | Ebsa, G. et al.,[2015] [33] | Addis Ababa | Retrosp-cohort | 253 | 58(10.4) | Low risk |
| 10 | Marie, B.T. et al. [2022] [42] | Amhara | Retrosp-cohort | 376 | 21(5.6) | Low risk |
| 11 | Molla, M. et al.,[2022] [31] | Benishangul | Retrosp-cohort | 721 | 30(4.2) | Low risk |
| 12 | Omer, A. et al.,[2019] [30] | SNNPRS | Retrosp-cohort | 242 | 13(5.3) | Low risk |
| 13 | Sidemo, N.B. and S.H. Hebo,[2019] [29] | SNNPRS | Retrosp-cohort | 421 | 65(15.4) | Low risk |
| 14 | Taye,B. et al.,[2010] [28] | Addis Ababa | Retrosp-cohort | 475 | 42(8.8) | Low risk |
3.3. Meta-analysis of the effects of undernutrition on mortality of children living with HIV
Among the total of 14 retrospective cohort studies included in the review, twelve studies were reporting nutritional status as well-nourished and undernourished (stunting, wasting and underweight). The remaining two studies reporting undernutrition based on the three categories of mild, moderate and severe undernutrition [14,42].
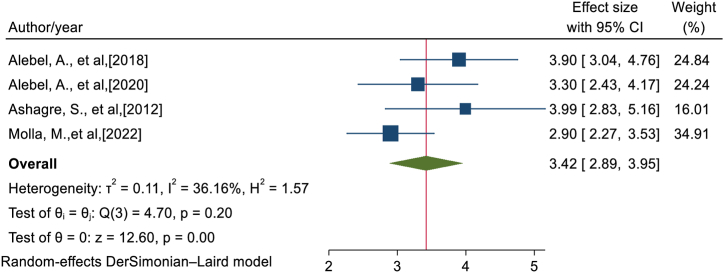
3.4. The effects of stunting on mortality of children living with HIV
A total of four [12,31,34,40] cohort studies revealed that stunting has a significant effect on mortality of children infected with HIV. The pooled AHR (adjusted hazard ratio) of these studies disclosed that stunted children living with HIV were 3.36 times hazard of death (AHR: 3.36; 95 % CI: 2.95–3.77) as compared to their counterparts. Since studies included in this meta-analysis were exhibited no heterogeneity (I2 = 36.16 %, p = 0.195), fixed effect model was undertaken (Fig. 2).
Fig. 2.
Forest plot showing of the effects of stunting on mortality among children living with HIV in Ethiopia.
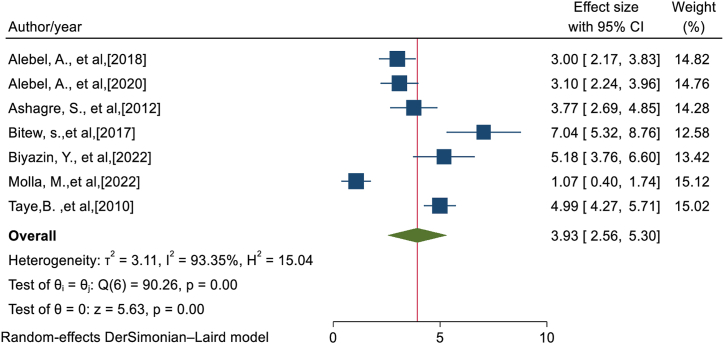
3.5. The effects of wasting on mortality of children living with HIV
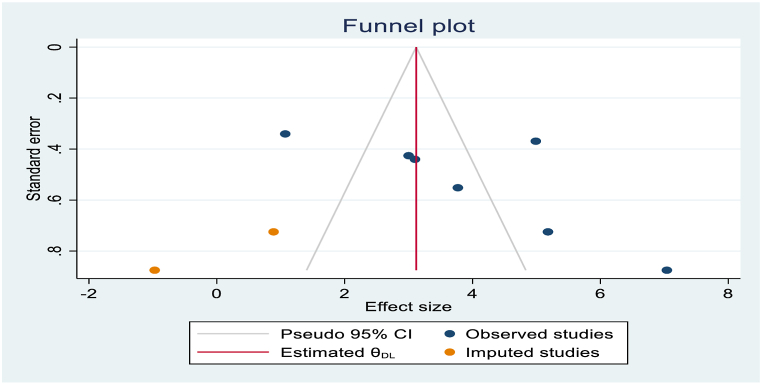
Among seven included [12,27,28,31,34,35,40] studies, six articles indicated that wasting has a significant effect on mortality in children infected with HIV. From random effects model, statistical heterogeneity was observed among studies (I2 = 93.35 %, P-value<0.001) and there was no single study that excessively influenced the pooled effects of wasting on mortality. Egger's statistical test revealed that there is evidence of publication bias (P-value = 0.0206). After trim and fill analysis (Fig. 3), wasting had negative impact on mortality of children with HIV. Therefore, from trimfill analysis the pooled hazard effects of mortality among wasted children living with HIV were 3.93 times as compared to well-nourished children with HIV(AHR: 3.93; 95 % CI: 2.56–5.30) (Fig. 4).
Fig. 3.
Trim and fill analysis of funnel plot for effects of wasting on mortality among children living with HIV.
Fig. 4.
Forest plot showing of the effects of wasting on mortality among children infected with HIV in Ethiopia.
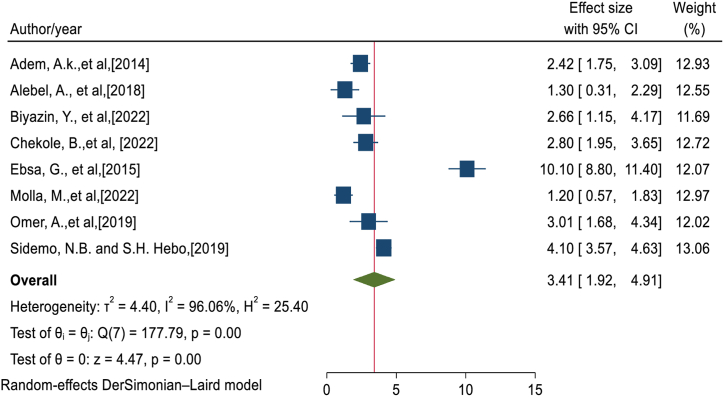
3.6. The effects of underweight on mortality of children living with HIV
Eight studies [12,[29], [30], [31], [32], [33],35,41] were included in the meta-analysis of this category. Of these four studies showed that underweight has a significant effect on mortality in children living with HIV while four of them reported that underweight has no significant effect on mortality. However, the pooled effect of all 8 studies showed that underweight has 3.4 times hazard of death among children who lived with HIV as compared to their compartments. Statistical heterogeneity was observed among studies (I2 = 96.06 %, P-value<0.001) (Fig. 5) and there was no single study that excessively influenced the pooled effects of underweight on mortality of children with HIV. Egger's statistical test revealed that there is no evidence of publication bias (P-value = 0.2679). Additionally, the remaining two [14,42] studies reporting undernutrition interms of mild, moderate and severe which were not suitable for meta-analysis in this study. The studies indicated that children with severe undernutrion were more likely to die than children with mild undernutrion.
Fig. 5.
Forest plot showing of the effects of underweight on mortality among children living with HIV in Ethiopia.
3.7. Subgroup analyses of effects of wasting on mortality of children living with HIV
From random effects pooled estimate, significant heterogeneity was observed. To handle this heterogeneity, Subgroup analyses was performed based on the region, sample size and publication year (Table 2).The result of this analysis showed that wasting has higher effect(AHR: 5.33; 95%CI: 2.13–8.54]) on mortality among studies done SNNPRS as compared to other parts of the country [27,40]. The Sub-group analyses based on sample size indicated that wasting has more effect (AHR: 4.62; 95%CI: 3.05–6.19) among studies conducted with sample size less than 450 [12,27,35,40] compared to their counterparts. Furthermore, subgroup analyses also evidenced that wasting has a more effect on mortality in studies published before 2019 [12,27,28,40] as compared to studies published after 2019.
Table 2.
Summary of sub-group analysis on effects of wasting among children living with HIV in Ethiopia by region, sample size and publication year.
| Variables Sub-group | Included studies | AHR | Heterogeneity (I2 %, p-value) | |
|---|---|---|---|---|
| Region | Amhara | 3 | 3.61[2.50–4.73] | 72.85,p = 0.03 |
| SNNPRS | 2 | 5.33[2.13–8.54] | 89.99, p < 0.001 | |
| Others | 2 | 3.03[2.81–6.87] | 98.36,p < 0.001 | |
| Sample size | <450 | 4 | 4.62[3.05–6.19] | 85.30,p < 0.001 |
| ≥450 | 3 | 3.05[0.67–5.43] | 96.73, p < 0.001 | |
| Publication year | <2019 | 4 | 4.57[3.17–5.97] | 87.26, p < 0.001 |
| ≥2019 | 3 | 3.04[0.89–5.19] | 93.87, p < 0.001 | |
NB: others; Oromia, Benishangul and Addis Ababa.
3.8. Sub-group analyses of effects of underweight on mortality of children living with HIV
To handle heterogeneity, a sub-group analysis was performed using sample size and publication year. The effect of underweight on mortality of children living with HIV was higher (AHR:4.23; 95 % CI:1.72–6.73) among studies done with sample size less than 450 [12,29,30,33,35] compared with studies conducted with sample size greater than 450. The result of sub-group analyses also disclosed that underweight has an exaggerated effect (AHR: 4.58; 95%CI: 1.17–8.99) on mortality among studies published before 2019 (Table 3).
Table 3.
Summary of sub-group analysis on effects of underweight on mortality among children living with HIV in Ethiopia by sample size and publication year.
| Variables Sub-group | Included studies | AHR | Heterogeneity (I2,p-value) | |
|---|---|---|---|---|
| Sample size | <450 | 5 | 4.23[1.72–6.73] | 96.63, p < 0.001 |
| ≥450 | 3 | 2.11[1.14–3.08] | 82.07, p < 0.001 | |
| Publication year | <2019 | 3 | 4.58[1.17–8.99] | 98.43, p < 0.001 |
| ≥2019 | 5 | 2.75[1.45–4.05] | 91.75, p < 0.001 | |
4. Discussion
Despite several interventions undertaken regarding to HIV/AIDS related mortality, undernutrition (wasting, stunting and underweight) is continued to be a major predictors of mortality among HIV-infected children. Therefore, this review aimed to estimate the pooled effects of undernutrition on mortality among children living with HIV in Ethiopia.
The finding of this systematic review and meta-analysis indicated that undernutrition has significant role to increases the risk of mortality in children living with HIV/AIDS.
The review disclosed that stunted children living with HIV were 3.36 times more likely to die as compared to well-nourished children. This is reasoned by bidirectional relationship nature of chronic undernutrition and HIV- infection [44]. The coexistence of HIV-infection and stunting further compromises the immune system [45,46]. Studies evidenced that nutritional status, immune system and HIV are intricate and intertwined [19]. As immunity system weakened, the risk for acquiring of opportunistic infections increased [47].Decreased immunity also complicates the treatment of HIV by interfere with intestinal absorption of drugs and various nutrients [48] and thereby increases the progression HIV to AIDS which finally hastens morbidity and mortality rate of children infected with HIV [46].
This study also showed that HIV-infected children complicated with acute undernutrition were more hazards to die than well-nourished children. It is supported by a study done in Tanzania, Malawi, low income countries and a systematic review and meta-analysis study conducted in Sub-Saharan Africa and East Africa [[48], [49], [50], [51], [52], [53]]. Similarly, an evidence from elsewhere also revealed that HIV- infected children with severe acute malnutrition(SAM) were nine times risk of death compared with their normal peers. This is due to the double burden of acute malnutrition/wasting and HIV which results in increased incidence and severity of concurrent infections, making clinical management more challenging [54]. SAM on the background of HIV prone children for further complications, electrolyte disorders, micronutrient deficiencies, lethal opportunistic infections like tuberculosis, persistent diarrhea, pneumonia which contribute to high mortality [55].
Furthermore, the review indicated that underweight is major predictor of mortality and low survival among children with HIV. Our finding is in line with the study done in Zambia, Kenya and democratic Republic of Congo [[56], [57], [58]]. This is justified by HIV-infected children who is manifested with low weight for age ratio is a marker of disease progression and significant factors to low survival and premature death [59]. Nutritional deficiency/underweight and HIV/AIDS are jeopardized conditions that exposed children delayed immune recovery and life threatening medical complications which increase the risk of death [13].
Sub-group analyses based on publication year also disclosed that undernutrion has an exaggerated effect on mortality among studies published before 2019.This is explained by that the country has planned and implemented different strategies to reduce morbidity and mortality of people due to HIV/AIDS afterwards [60]. Moreover, the result of sub-group analysis based on the sample size revealed that stunting and underweight have significant effect on mortality of children living with HIV among studies done with sample size less than 450.
4.1. Strength and limitation of the study
This is the first review to determine the pooled effects of undernutrion on the mortality of children infected with HIV in Ethiopia. Sub-group analysis was done to minimize statistically significant heterogeneity and all the included studies were cohort study design which better identifies cause and effect relationship. Although the above strength of the study, it has some drawbacks that the reader should consider. Qualitative studies and articles published other than English language was excluded. The study included some studies with small sample size and significant heterogeneity which might affect the pooled effect estimates. The review included a small number of primary studies which minimize the strength of representativeness.
5. Conclusion
This Meta-analysis and systematic review revealed that undernutrition (stunting, wasting and underweight) has deleterious effect on mortality of children infected with HIV/AIDS by disease progression and prone the children to serious opportunistic infections. From the study, the authors recommended that nutritional status of children on antiretroviral therapy need to be evaluated regularly. In addition, parents/care providers are counseled to nourish the recommended balance diet and the complex nature of undernutrion and HIV-infections.
Funding statement
This research did not receive any specific grant.
Ethics statement
Ethical clearance is not applicable for this systematic review and meta-analysis, because we extracted the data from previous primary studies.
Data availability statement
All data are available on the manuscript and supporting files.
CRediT authorship contribution statement
Amare Kassaw: Writing – review & editing, Writing – original draft, Visualization, Validation, Supervision, Software, Resources, Methodology, Investigation, Formal analysis, Conceptualization. Bogale Chekole: Writing – review & editing, Writing – original draft, Methodology. Muluken Chanie Agimas: Writing – review & editing, Writing – original draft, Software, Project administration. Molla Azmeraw: Writing – review & editing, Writing – original draft, Resources. Biruk Beletew: Writing – review & editing, Writing – original draft. Shegaw Zeleke: Writing – review & editing, Writing – original draft, Visualization, Software. Worku Necho Asferi: Writing – review & editing, Writing – original draft. Solomon Demis: Writing – review & editing, Writing – original draft, Investigation. Habtamu Shimeles Hailemeskel: Writing – review & editing, Writing – original draft, Validation. Wubet Alebachew Bayih: Writing – review & editing, Writing – original draft. Ermias Sisay Chane: Writing – review & editing, Writing – original draft. Demewoz Kefale: Writing – review & editing, Writing – original draft. Tigabu Munye Aytenew: Writing – review & editing, Writing – original draft, Visualization, Validation.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.heliyon.2024.e29308.
Abbreviations
- HIV
Humane Immune Virus
- AIDS
Acquired Immune Deficiency Virus
- HAART
Highly Active Antiretroviral Therapy
- ART
Antiretroviral Therapy
- SAM Severe acute Malnutrition
- AHR
Adjusted Hazard Ratio
- CI
Confidence Interval
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Ahmed I., Lemma S. Mortality among pediatric patients on HIV treatment in sub-Saharan African countries: a systematic review and meta-analysis. BMC Publ. Health. 2019;19(1):1–13. doi: 10.1186/s12889-019-6482-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Alebel A., et al. Effects of undernutrition on mortality and morbidity among adults living with HIV in sub-Saharan Africa: a systematic review and meta-analysis. BMC Infect. Dis. 2021;21:1–20. doi: 10.1186/s12879-020-05706-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.WHO HIV/Aids factsheets. https://www.who.int/news-room/fact-sheets/detail/hiv-aids Available from:
- 4.UNAIDS Global HIV & AIDS statistics. 2022. https://www.unaids.org/en/resources/fact-sheet Fact sheet Available from:
- 5.Kff G.h.p. The global HIV/AIDS epidemic. 2023 access date, july 12/2203] https://www.kff.org/global-health-policy/fact-sheet/the-global-hivaids-epidemic/#endnote_link_560330-9 Available from:
- 6.UNICEF . 2021. HIV and AIDS Global Snapshot.https://www.google.com/search?q=2021+HIV+and+AIDS+Global+Snapshot&oq=2021+HIV+and+AIDS+Global+Snapshot&gs_lcrp=EgZjaHJvbWUyBggAEEUYOdIBCDEyMDJqMGo3qAIAsAIA&sourceid=chrome&ie=UTF-8 Access date July,21/2023]; Available from: [Google Scholar]
- 7.USAID UNAIDS global AIDS update 2022. https://reliefweb.int/report/world/danger-unaids-global-aids-update-2022-enru?gclid=Cj0KCQjw2eilBhCCARIsAG0Pf8vvrfyGkx8IYx1LjzMo_z4spvyaLzFYoIewRFFKXR2tSmhT99pWqy8aAvnxEALw_wcB Accese date July 21, 2023]; Available from:
- 8.Edmonds A., et al. The effect of highly active antiretroviral therapy on the survival of HIV-infected children in a resource-deprived setting: a cohort study. PLoS Med. 2011;8(6) doi: 10.1371/journal.pmed.1001044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Njuguna I.N., et al. Urgent versus post-stabilization antiretroviral treatment (ART) in hospitalized children: a randomized controlled trial. The lancet. HIV. 2018;5(1):e12. doi: 10.1016/S2352-3018(17)30167-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ford N., et al. Causes of hospital admission among people living with HIV worldwide: a systematic review and meta-analysis. The lancet HIV. 2015;2(10):e438–e444. doi: 10.1016/S2352-3018(15)00137-X. [DOI] [PubMed] [Google Scholar]
- 11.Sashindran V.K., Thakur R. 2020. Malnutrition in HIV/AIDS: Aetiopathogenesis. Nutrition and HIV/AIDS-Implication for Treatment, Prevention and Cure. [series online] [Google Scholar]
- 12.Alebel A., et al. Effects of undernutrition on survival of human immunodeficiency virus positive children on antiretroviral therapy. Ital. J. Pediatr. 2018;44(1):1–10. doi: 10.1186/s13052-018-0472-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fabusoro O.K., Mejia L.A. Nutrition in HIV-infected infants and children: current knowledge, existing challenges, and new dietary management opportunities. Adv. Nutr. 2021;12(4):1424–1437. doi: 10.1093/advances/nmaa163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Arage G., et al. vol. 7. SAGE open medicine; 2019. Survival Rate of HIV-Infected Children after Initiation of the Antiretroviral Therapy and its Predictors in Ethiopia: a Facility-Based Retrospective Cohort. 2050312119838957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Aynalem Y.A., et al. 2020. Mortality and its Predictors Among Children on Antiretroviral Treatment in Ethiopia: A Systematic Review and Meta–Analysis. [Google Scholar]
- 16.Wubneh C.A., Belay G.M. Mortality and its association with CD4 cell count and hemoglobin level among children on antiretroviral therapy in Ethiopia: a systematic review and meta-analysis. Trop. Med. Health. 2020;48(1):1–11. doi: 10.1186/s41182-020-00267-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Thimmapuram R., et al. Correlation of nutrition with immune status in human immunodeficiency virus outpatients. Mo. Med. 2019;116(4):336–339. [PMC free article] [PubMed] [Google Scholar]
- 18.Scrimshaw N.S., SanGiovanni J.P. Synergism of nutrition, infection, and immunity: an overview. Am. J. Clin. Nutr. 1997;66(2):464S–477S. doi: 10.1093/ajcn/66.2.464S. [DOI] [PubMed] [Google Scholar]
- 19.Duggal S., Chugh T.D., Duggal A.K. Clinical and Developmental Immunology. 2012. HIV and malnutrition: effects on immune system. 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Aguilera‐Alonso D., et al. nutritional, clinical and immunological status of children at HIV diagnosis in the continental region of Equatorial Guinea. Trop. Med. Int. Health. 2020;25(2):248–254. doi: 10.1111/tmi.13325. [DOI] [PubMed] [Google Scholar]
- 21.Ndirangu M., et al. Nutritional status of under-five children in HIV-affected households in western Kenya. Food Nutr. Bull. 2011;32(2):159–167. doi: 10.1177/156482651103200208. [DOI] [PubMed] [Google Scholar]
- 22.Tsegaye D., Kebede T., Kebede F. Rate, risk factors and estimations of time to develop severe acute malnutrition after children receiving antiretroviral therapy at selected health facilities in northwest Ethiopia. J. Nutr. Sci. 2023;12:e60. doi: 10.1017/jns.2023.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rose A.M., Hall C.S., Martinez-Alier N. Aetiology and management of malnutrition in HIV-positive children. Arch. Dis. Child. 2014;99(6):546–551. doi: 10.1136/archdischild-2012-303348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Frigati L., et al. Priorities for decreasing morbidity and mortality in children with advanced HIV disease. Clin. Infect. Dis. 2018;66(suppl_2):S147–S151. doi: 10.1093/cid/ciy013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Efdr M. The federal democratic republic of Ethiopia ministry of health. National Guidelines for HIV/AIDS and nutrition. 2008:1–73. [Google Scholar]
- 26.EFDRE, NATIONAL NUTRITION PROGRAM. 2016: Addis Ababa.
- 27.Bitew S., Mekonen A., Assegid M. Predictors on mortality of human immunodeficiency virus infected children after initiation of antiretroviral treatment in Wolaita zone health facilities, Ethiopia: retrospective cohort study. J. AIDS HIV Res. 2017;9(4):89–97. [Google Scholar]
- 28.Taye B., Shiferaw S., Enquselassie F. The impact of malnutrition in survival of HIV infected children after initiation of antiretroviral treatment (ART) Ethiop. Med. J. 2010;48(1):1–10. [PubMed] [Google Scholar]
- 29.Sidemo N.B., Hebo S.H. Nutrition and HIV/AIDS-Implication for Treatment, Prevention and Cure. 2019. Nutritional status and its effect on treatment outcome among HIV-infected children receiving first-line antiretroviral therapy in arba minch general hospital and arba minch health center, gamo zone, southern Ethiopia: retrospective cohort study. IntechOpen. [Google Scholar]
- 30.Oumer A., Kubsa M.E., Mekonnen B.A. Malnutrition as predictor of survival from anti-retroviral treatment among children living with HIV/AIDS in Southwest Ethiopia: survival analysis. BMC Pediatr. 2019;19(1):1–10. doi: 10.1186/s12887-019-1823-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Molla M., et al. Effects of undernutrition and predictors on the survival status of HIV-positive children after started antiretroviral therapy (ART) in Northwest Ethiopia. Int. J. Pediatr. 2022;2022 doi: 10.1155/2022/1046220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Adem A.K., Alem D., Girmatsion F. Factors affecting survival of HIV positive children taking antiretroviral therapy at Adama Referral Hospital and Medical College, Ethiopia. J. AIDS Clin. Res. 2014;5(3) [Google Scholar]
- 33.Ebissa G., Deyessa N., Biadgilign S. Predictors of early mortality in a cohort of HIV-infected children receiving high active antiretroviral treatment in public hospitals in Ethiopia. AIDS Care. 2015;27(6):723–730. doi: 10.1080/09540121.2014.997180. [DOI] [PubMed] [Google Scholar]
- 34.Alebel A., et al. Mortality rate among HIV-positive children on ART in Northwest Ethiopia: a historical cohort study. BMC Publ. Health. 2020;20(1):1–11. doi: 10.1186/s12889-020-09418-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Biyazin Y., et al. Survival and predictors of mortality among HIV-positive children on antiretroviral therapy in public hospitals. Journal of Pharmaceutical Policy and Practice. 2022;15(1):48. doi: 10.1186/s40545-022-00448-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Turck D., et al. World health organization 2006 child growth standards and 2007 growth reference charts: a discussion paper by the committee on nutrition of the European society for pediatric gastroenterology, hepatology, and nutrition. J. Pediatr. Gastroenterol. Nutr. 2013;57(2):258–264. doi: 10.1097/MPG.0b013e318298003f. [DOI] [PubMed] [Google Scholar]
- 37.Belay D.M., et al. Macrosomia and its predictors in pregnant women with diabetes in Ethiopia. Trop. Med. Int. Health. 2021;26(12):1539–1552. doi: 10.1111/tmi.13684. [DOI] [PubMed] [Google Scholar]
- 38.Peters M., Godfrey-smith P., Mcinerney P. Joanna Briggs Institute Reviewer's Manual. South. Joanna Briggs Institute; Australia: 2019. Guidance for the conduct of JBI scoping reviews. [Google Scholar]
- 39.Higgins J.P., Thompson S.G. Quantifying heterogeneity in a meta‐analysis. Stat. Med. 2002;21(11):1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 40.Ashagre S. Addis Ababa University; 2012. Survival and its Predictors Among Children on ART in Hawassa Referral Hospital, Adare Hospital and Bushulo Health Centre, South Ethiopia: Retrospective Cohort Study. [Google Scholar]
- 41.Chekole B., et al. vol. 10. SAGE Open Medicine; Ethiopia: 2020. Survival Status and Predictors of Mortality Among HIV-Positive Children Initiated Antiretroviral Therapy in Bahir Dar Town Public Health Facilities Amhara Region. 2022. 20503121211069477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Marie B.T., Argaw W.S., Bazezew B.Y. Time to death among HIV-infected under-five children after initiation of anti-retroviral therapy and its predictors in Oromiya liyu zone, Amhara region, Ethiopia: a retrospective cohort study. BMC Pediatr. 2022;22:1–9. doi: 10.1186/s12887-022-03295-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bitew S. SNNPR, Ethiopia. Addis Ababa University; 2014. Assessment of the effect of malnutrition on survival of HIV infected children after initiation of antiretroviral treatment in wolaita zone health facilities. [Google Scholar]
- 44.Ajari E.E., Adewale B.A. The Bi-directional relationship between childhood malnutrition and HIV/AIDS. International Journal of Health and Life Sciences. 2021;7(2) [Google Scholar]
- 45.Jesson J., et al. Prevalence of malnutrition among HIV-infected children in Central and West-African HIV-care programmes supported by the Growing up Programme in 2011: a cross-sectional study. BMC Infect. Dis. 2015;15(1):1–12. doi: 10.1186/s12879-015-0952-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Weiser S.D., et al. Conceptual framework for understanding the bidirectional links between food insecurity and HIV/AIDS. Am. J. Clin. Nutr. 2011;94(6):1729S–1739S. doi: 10.3945/ajcn.111.012070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Colecraft E. HIV/AIDS: nutritional implications and impact on human development. Proc. Nutr. Soc. 2008;67(1):109–113. doi: 10.1017/S0029665108006095. [DOI] [PubMed] [Google Scholar]
- 48.Mwiru R.S., et al. Nutritional status and other baseline predictors of mortality among HIV-infected children initiating antiretroviral therapy in Tanzania. J. Int. Assoc. Phys. AIDS Care. 2015;14(2):172–179. doi: 10.1177/2325957413500852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Liu E., et al. Nutritional status and mortality among HIV-infected patients receiving antiretroviral therapy in Tanzania. JID (J. Infect. Dis.) 2011;204(2):282–290. doi: 10.1093/infdis/jir246. [DOI] [PubMed] [Google Scholar]
- 50.Braitstein P., et al. Mortality of HIV-1-infected patients in the first year of antiretroviral therapy: comparison between low-income and high-income countries. Lancet (London, England) 2006;367(9513):817–824. doi: 10.1016/S0140-6736(06)68337-2. [DOI] [PubMed] [Google Scholar]
- 51.Fergusson P., Tomkins A. HIV prevalence and mortality among children undergoing treatment for severe acute malnutrition in sub-Saharan Africa: a systematic review and meta-analysis. Trans. R. Soc. Trop. Med. Hyg. 2009;103(6):541–548. doi: 10.1016/j.trstmh.2008.10.029. [DOI] [PubMed] [Google Scholar]
- 52.Chinkhumba J., et al. The impact of HIV on mortality during in-patient rehabilitation of severely malnourished children in Malawi. Trans. R. Soc. Trop. Med. Hyg. 2008;102(7):639–644. doi: 10.1016/j.trstmh.2008.04.028. [DOI] [PubMed] [Google Scholar]
- 53.Abate B.B., Aragie T.G., Tesfaw G. Magnitude of underweight, wasting and stunting among HIV positive children in East Africa: a systematic review and meta-analysis. PLoS One. 2020;15(9) doi: 10.1371/journal.pone.0238403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Preidis G.A., et al. Pneumonia and malnutrition are highly predictive of mortality among African children hospitalized with human immunodeficiency virus infection or exposure in the era of antiretroviral therapy. J. Pediatr. 2011;159(3):484–489. doi: 10.1016/j.jpeds.2011.02.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Musoke P.M., Fergusson P. Severe malnutrition and metabolic complications of HIV-infected children in the antiretroviral era: clinical care and management in resource-limited settings. Am. J. Clin. Nutr. 2011;94(6):1716S–1720S. doi: 10.3945/ajcn.111.018374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Sutcliffe C.G., et al. Risk factors for pre-treatment mortality among HIV-infected children in rural Zambia: a cohort study. PLoS One. 2011;6(12) doi: 10.1371/journal.pone.0029294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Wamalwa D.C., et al. Predictors of mortality in HIV-1 infected children on antiretroviral therapy in Kenya: a prospective cohort. BMC Pediatr. 2010;10:1–8. doi: 10.1186/1471-2431-10-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Callens S.F., et al. Mortality and associated factors after initiation of pediatric antiretroviral treatment in the Democratic Republic of the Congo. Pediatr. Infect. Dis. J. 2009;28(1):35–40. doi: 10.1097/INF.0b013e318184eeb9. [DOI] [PubMed] [Google Scholar]
- 59.Almeida F.J., Kochi C., Sáfadi M.A.P. Influence of the antiretroviral therapy on the growth pattern of children and adolescents living with HIV/AIDS. J. Pediatr. 2019;95:S95–S101. doi: 10.1016/j.jped.2018.12.007. [DOI] [PubMed] [Google Scholar]
- 60.FHAPCO . 2021-2025. HIV/AIDS Strategic Plan for Ethiopia. Addis Ababa. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data are available on the manuscript and supporting files.