Highlights
-
•
Training technical professionals for Radiotherapy is essential due to growing demand caused by early cancer diagnoses, global population aging, rising cancer rates, and evolving equipment and techniques.
-
•
A cross-sectional study (approved at the local Research Ethics Committee) was conducted, involving an online survey for the opinion of professionals already qualified as radiotherapy technicians or technologists and engaged in this work.
-
•
The data underscores the need to adjust technical training in Radiotherapy, emphasizing the importance of a recognized professional team, practical learning, flexible schedules, and financial viability.
-
•
The strategic perspective of radiotherapy technicians currently working in this job market, emphasized the need for an adjustment in the offering of courses. These insights provide more well-structured foundations for contemporary teaching and learning processes, considering current societal characteristics, technological advances, and future student demands.
Abstract
Training technical professionals for Radiotherapy is essential due to growing demand caused by early cancer diagnoses, global population aging, rising cancer rates, and evolving equipment and techniques. Our objective was to gather insights from graduates of various courses who are now working professionally, based on the principle that one way to assess educational training is by considering the attributes that trained and active professionals deem important in the improvement courses they have taken.
A cross-sectional study (approved at the local Research Ethics Committee) was conducted, involving an online survey for the opinion of professionals already qualified as radiotherapy technicians or technologists and engaged in this work. The questionnaire consisted of 12 objective multiple-choice questions and four open-ended questions.
Of the 59 received responses, 49 professionals completed some course. Thirty-one (64.6%) pursued improvement/enhancement, followed by specialization (15; 31.2%) and extension (two; 4.2%). Thirty-four (69.4%) respondents had not engaged in any practical activities during their training. As for course weaknesses, respondents cited: inflexible schedule (29; 59.2%), distance from residence (12; 24.5%), low hourly load (four; 8.2%), and other issues (four; 8.2%).
The data underscores the need to adjust technical training in Radiotherapy, emphasizing the importance of a recognized professional team, practical learning, flexible schedules, and financial viability.
The strategic perspective of radiotherapy technicians currently working in this job market, emphasized the need for an adjustment in the offering of courses. These insights provide more well-structured foundations for contemporary teaching and learning processes, considering current societal characteristics, technological advances, and future student demands.
Introduction
Radiotherapy is a therapeutic modality primarily aimed at treating neoplasms, utilizing ionizing radiation with the primary goal of destroying or reducing cell duplication [1].
Over 100 years old, it initially involved empirical and artisanal approaches, using implants of radioactive materials (Radium-226) or orthovoltage equipment, primarily for superficial diseases like skin cancer 1. With the evolution of radiotherapy equipment, such as Linear Electron Accelerators and Telecobalt Therapy Units, the need for involvement of Medical Physics professionals became evident. They are responsible for calculations and ensuring the quality of radiation offered to patients. With increased demand and higher treatment quality requirements, the role of the radiotherapy technician emerged. These professionals play a crucial role in administering sessions prescribed by doctors and calculated by physicists. Their training begins with a Radiology technician course or through Radiology technologist training [2]. Currently, there are several public and private institutions in Brazil that offer training courses in radiotherapy. Unfortunately, its characteristics are very varied, with a very heterogeneous constitution. Several institutions offer Extension courses (12 class hours), others have improvement/enhancement courses (normally 180 class hours) and few schools offer specialization courses (approximately 360 class hours) 14.
In Brazil, Radiology technicians undergo a minimum 1,200-hour secondary level course, covering radiation physics, anatomy, biosafety, and conventional radiology techniques. The National Catalog of Technical Courses, produced by the Ministry of Health, outlines their professional functions, including performing radiological exams such as X-rays, mammograms, computed tomographies, and magnetic resonances [3].
The first course for these professionals in Brazil originated in 1952. Currently, Radiology technicians must be registered with the Regional Council of Radiology Technicians (CRTR) to practice regularly [4].
While there is no official regulation requiring Radiology technicians to undergo specific training to work in Radiotherapy, the uniqueness of the field and the lack of information on radiotherapy in radiology technician training make specialized instruction increasingly indispensable for those choosing to work in this market segment.
The main difference between a Radiology technician and a Radiology technologist lies in their level of education, responsibilities, and involved skills. Technicians usually complete shorter technical courses lasting about one to two years, while technologists have longer academic training, obtaining a degree in radiology technology. Technicians are trained mainly to operate radiology equipment and perform imaging exams following specific protocols, while technologists have a deeper understanding of anatomy, medical physics, and professional ethics. They are trained to operate radiology equipment and perform some more complex procedures. In many cases, radiology technologists can work with greater autonomy and less direct supervision, potentially overseeing other radiology technicians [3].
Thus, Radiology technicians undergo shorter training, focusing primarily on performing imaging exams, while Radiology technologists have a more in-depth education, allowing them to take on additional responsibilities and more complex procedures, both playing vital roles in healthcare, contributing to patient diagnosis and treatment.
In Radiotherapy, radiotherapy technicians or technologists are responsible for positioning patients in radiotherapy equipment and performing location images directly on the machine, ensuring the adequacy of the position in each radiotherapeutic session. In practice, there is no difference in the responsibilities of radiotherapy technicians and technologists. They are professionals who perform essentially the same professional activities, with the technologist being able to accumulate a little more responsibilities and, depending on the size of the service in which they work, occupy a position of coordinating technicians. In this clinical context, it is the fundamental role of the radiotherapy technician or technologist, under the guidance of the doctor and physicist, to execute the prescribed treatment [5].
The Current Landscape of Radiotherapy in Brazil
According to the Ministry of Health's 2018 Radiotherapy Census, 363 radiotherapy devices are in operation in Brazil. This number is notably considered insufficient for the oncological demands of the country. The shortage of radiotherapy devices and the resulting inaccessibility of a significant portion of the Brazilian population to oncological treatment, especially radiotherapy, have been reported by the media [6].
A 2020 report by the Brazilian Society of Radiotherapy showed a deficit of at least 182 devices nationwide. Considering that all currently active devices operate with the appropriate number of technicians, it can be inferred that 1,274 new radiotherapy technicians or technologists are needed promptly to address this deficit. This does not consider personnel turnover or transfers in the job market and the expected aging of the population [6].
According to the National Commission on Nuclear Energy (CNEN) and the National Health Surveillance Agency (ANVISA) regulations, radiotherapy technicians or technologists should work in pairs for four hours and 48 min shifts, totaling a 24-hour weekly schedule. Assuming each radiotherapy device operates for three shifts, with technicians or technologists working in pairs, it can be concluded that, on average, each device requires seven radiotherapy technicians or technologists, including one standby professional [7].
Thus, in addition to playing a fundamental role in radiotherapy service routines, the profession of radiotherapy technician or technologist is expected to be extremely in demand in the future. Therefore, the fundamental offering of improvement courses in this area is envisioned, both quantitatively (as previously outlined) and qualitatively, given the progression of scientific and technological knowledge, leading to higher qualification requirements. Furthermore, the current moment demands new educational approaches, including the application of active methodologies in various stages of educational formation, integration between theory and practice, and the innovation of student performance evaluation processes. The active teaching methodology has been successful in health professional education due to its focus on students' active participation in the learning process, strengthening the understanding and application of concepts. This allows for greater engagement, development of practical skills, and more accurate decision-making. Training in real problem-solving helps future professionals better deal with complex situations in the health field. Therefore, the offer of new education courses should respect these premises, providing students with incentives to actively participate in learning activities, maintaining their interest and high motivation, including simulations, case studies, and real situations. Reflection, analysis, and problem-solving promote the development of critical thinking, an essential attribute in the health sector.. This investigation was designed based on the principle that assessing educational training can be done by considering the attributes that trained and active professionals find important in the improvement courses they have completed.
Material and method
The project that described the tools used for the evaluative analysis with professionals working in the job market was submitted to the Research Ethics Committee of the School of Medical and Health Sciences of PUCSP and approved with CAAE No. 64582422.0.0000.5373.
The online questionnaire, created on the Google Forms platform, covered various aspects related to the training of radiology technicians in the market, working as radiotherapy technicians.
Questionnaire template:
Number of questions: 12 objective questions (four open questions).
The initial question asked whether or not to complete the course (since it is not mandatory for entry into the job market). If the professional had completed the course, the questionnaire continued. If not, he was forwarded to his last question which analyzed the reason for not taking the course.
Subsequent questions for respondents who attended a course included how long ago they completed it, the duration of their work in the job market, the course duration, and the frequency of classes. Additionally, they were invited to specify the strengths and weaknesses of the course undertaken. Finally, the last two questions in the form addressed whether practical classes were conducted and whether the course contributed to the participants' entry into the job market.
The Brazilian Society of Radiotherapy (SBRT) was contacted and assisted in directing the questionnaires to its members registered in the professional category of interest. Thus, an email was sent to 169 radiology technicians or technologists currently working in the field of Radiotherapy. In addition, personal contacts were made, and the survey was promoted on social media, with a request for responses to be submitted via the provided link.The data collection period spanned 166 days (starting on 17/11/2022 and ending on 01/05/2023). The first response was recorded on 17/11/2022, and the last on 17/04/2023, totaling 153 consecutive days of data collection.
The obtained results were subjected to descriptive statistical analysis based on the frequency of responses.
Results
A total of 59 completed questionnaires were received. The questionnaire did not allow tracking how respondents were located or their identification to preserve their identity. The most direct method was through the list of 169 emails, which was the number considered for inferences about response frequencies.
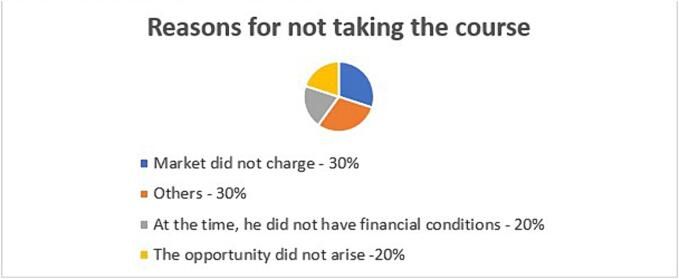
The initial question addressed the respondents' education, i.e., whether they had undergone any professional training courses. Out of the 59, ten (16.9 %) had not taken any Radiotherapy training courses, and the justifications are presented in Graph 1.
Graph 1.
Professional training of respondents
Three (30 %) of the respondents who marked the “other” option provided reasons: still attending the course; having completed a degree in Medical Radiology and being a Radiology technologist.
Out of the 49 professionals who had actually taken a course, the majority (31; 64.6 %) pursued improvement/enhancement, followed by specialization (15; 31.2 %) and extension (two; 4.2 %). One (2.0 %) individual indicated that they took the course online.
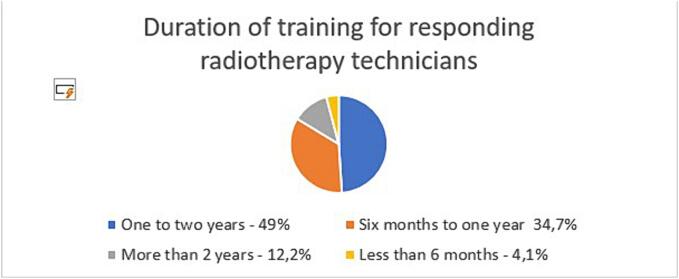
Most respondents (33 out of 49; 67.3 %) completed the course between five and ten years ago. Similarly, 29 (59.2 %) of the 49 had been working in the field for five to ten years.Regarding the course duration, two responses were more frequent: one to two years (24; 49.0 %) and six months to one year (17; 34.7 %), as shown in Graph 2.
Graph 2.
Duration of training for responding radiotherapy technicians
Thirty-three (67.3 %) participants took their training course with monthly activities, followed by 11 (22.4 %) weekly, three (6.1 %) bi-weekly, and two (4.1 %) did not specify the frequency.
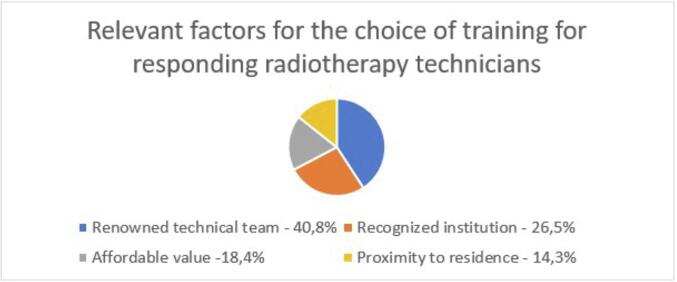
Respondents were asked about their personal perception of the strengths of their training course, with responses presented in Graph 3.
Graph 3.
Relevant factors for the choice of training for responding radiotherapy technicians.
As for weaknesses, respondents cited: inflexible schedule (29; 59.2 %), distance from residence (12; 24.5 %), low hourly load (four responses; 8.2 %), and others (four responses; 8.2 %). This question also allowed specifying weaknesses openly, and there was only one justification, indicating “unqualified teachers.”.
Participants were asked if the course included practical activities. Thirty-four (69.4 %) respondents had not participated in any practical activities during their training.
Respondents were also asked if the course contributed to their entry into the job market. Forty-seven (95.9 %) answered affirmatively. Table 1 summarizes the data obtained in the study. Graph 4.
Table 1.
Data described in an online survey with 59 radiotherapy technicians working in the job market regarding their training.
| Question | Response | Percentage |
|---|---|---|
| Did you take the course? | Yes | 83,1% |
| No | 16,9% | |
| Reasons for not taking the course | Market did not charge | 30% |
| Others | 30% | |
| At the time, he did not have financial conditions. | 20% | |
| The opportunity did not arise | 20% | |
| What course did you take? | Improvement/improvement | 63,3% |
| Specialization | 30,6% | |
| Extension | 4,1% | |
| EAD | 2% | |
| How long ago did you finish thecourse? | Between 5 and less than 10 years old | 67,3% |
| Less than 5 years ago | 18,4% | |
| More then 15 years | 8,2% | |
| Between 10 and less than 15 years old | 6,1% | |
| How long have you been in themarket? | Between 1 year and less than 1 year | 49,0% |
| Between 6 months and less than | 34,7% | |
| 1 year | ||
| More then 2 years | 12,2% | |
| How was the frequency ofclasses offered on your course? | Less than 6 months | 4,1% |
| Monthly activities | 67,3% | |
| Weekly activities | 22,4% | |
| Biweekly activities | 6,1% | |
| Others | 4,1% | |
| What were the strengths of yourcourse? | Renowned technical team | 40,8% |
| Recognized institution | 26,5% | |
| Affordable value | 18,4% | |
| Proximity to residence | 14,3% | |
| What were the weak points ofyour course? | Schedule inflexibility | 52,2% |
| Distance from residence | 24,5% | |
| Others | 8,2% | |
| Little workload | 8,2% | |
| Your training course offered practical activity | No | 69,4% |
| Yes | 30,6% | |
| Did the specialization course contribute to your entry into the job market? | Yes | 95,9% |
| No | 4,1% |
Graph 4.
Practical activities during the training of responding radiotherapy technicians.
Discussion
Specialization in radiotherapy has become an increasingly necessary option for radiology technicians seeking improvement and better positioning in the job market. This online survey, based on 59 respondents, revealed that 10 professionals working in the field did not undergo any specific training. Additionally, approximately 70 % of those who attended a course did not receive practical training associated with their education. Most respondents did not experience synchronicity between theoretical and practical learning, which is crucial for meaningful, assertive, and innovative learning [8].
The online questionnaire received 59 responses, a considerable sample given the uniqueness of the survey in this professional class. The list of names sent by SBRT was compiled over time and includes contacts of professionals who no longer work in the field or have outdated contact information. Questionnaire-based studies often face discreet participation due to addressing difficulties and professionals' lack of availability amid their routine challenges. A European survey that evaluated the satisfaction of radiotherapy professionals in relation to their training reached an audience of 38 professionals working in France, Germany and Belgium [9]. In other words, the scope of the sample detailed here was quite reasonable.
It is known that there are 363 radiotherapy devices nationwide, with an average of approximately five technicians working in each. Therefore, there should be around 1815 technicians working in radiotherapy in the country. Thus, we understand that this questionnaire impacted approximately 3.25 % of all practicing technicians in Brazil and can be considered an important sample, given the lack of specific databases for radiology technicians with specialization in radiotherapy. These are assumptions since there are no reliable data regarding the quantity of radiology technicians with specialization in radiotherapy working in the Brazilian job market. Additionally, this study was conducted with a convenience sample, acquired from individuals who received and volunteered to respond to the survey. Senger and collaborators, in a 2018 publication, pointed to the same weaknesses arising from this data collection method. Usually, research based on questionnaires sent virtually can reach a response rate of 20 to 30 % 14–15. In any case, the 59 responses were from radiology technical professionals who work in the area of Radiotherapy and define a specific audience, genuinely portraying their training [4], [10], [11], [12].
Of the respondents, about 17 % had not undergone formal training in radiotherapy. Considering that radiology technicians and technologists with an emphasis on radiotherapy are more concentrated in large urban centers (where there are more devices), and the surveyed population is likely located in major cities in the Southeast region, it is reasonable to conclude that the percentage of technicians working in the job market without formal training is even higher outside these training centers [6].
The reason described by 30 % of the respondents for not taking the training course was that there was no demand from the job market. It is essential to emphasize that, with the technical specificity and technological advances in radiotherapy, the market tends to become more selective and demanding regarding technicians' continuous training. An important article published by the International Atomic Energy Agency and the European Society for Radiotherapy indicates that the lack of concern for the training of radiotherapy technicians is closely related to historical context. In the past, when radiotherapy was offered using conventional techniques, in large fields where geometric failure was unlikely, the procedure was less dependent on the technical skill of the professional. The concept practiced was that the tumor was “somewhere around there”, and small changes in location were not likely to lead to significant errors [5].
With high technology, this changes radically. Higher doses per fraction are used in smaller, controllable areas. Therefore, the dose gradient is higher, and small changes can cause significant failures. The radiotherapy technician assumes greater responsibility, leading to increased market demand [13].
These arguments align with the responses of 20 % of respondents who reported not having had the opportunity to take the course. In a way, coupled with the limited number of offerings, it is a similar argument to the lack of market demand and is expected to diminish over time.
An important point analyzed concerns a socioeconomic issue: 20 % of demanded professionals who did not take the training course reported that the reason was a lack of financial capacity to cover the course costs. This is a very relevant demand: there are no free courses for training radiotherapy technicians. Some institutions offer online training, but lack any associated completion certificate or practical training connection. Students interested in this specialization are often professionals already working in areas of radiology (magnetic resonance, computed tomography, radiography) and are interested in specializing in radiotherapy. However, few are willing to give up their current profession for further training. This issue will be discussed more thoroughly later [14].
The question of analyzing professional satisfaction with their training is usual. Dubonis and colleagues published the results of a survey with 38 radiotherapy professionals (including doctors, physicists, and technicians) working in France, Germany, and Belgium, highlighting a significant lack in the practical aspect of training. Only a fifth of the respondents felt that their training was adequate when they entered the job market [9].
Often, professionals followed more experienced individuals. Although there is no data to criticize this situation, the training may have been conducted under conditions that can now be better controlled. Hence the need for the formalization of the teaching and learning process.
Of the 49 professionals who effectively completed a course, the majority (64.6 %) pursued improvement/enhancement, while 30 % took a specialization course. Specialization courses are known to be longer and more expensive, often limiting access for many professionals. The results reflect the current state of the radiotherapy technician profession in the country, highlighting the need for accessible and economically viable courses. In developing countries like Russia, similar challenges are faced, with the profession lacking regulation and recognition. Glebovskay proposed actions to professionalize radiotherapy technician training, emphasizing the importance of adapting courses to meet professionals' expectations. The study underscores the relevance of course duration, favoring accessibility and aligning content with practical aspects.This informal training lasted from six to 18 months, depending on the equipment's complexity. The first course, involving 15 participants, integrated theory and practice, lasting one month with 144 h of classes and four groups of instructors: physicians, physicists, radiobiologists, and technologists. However, the second course, with the same content, had to be condensed into two weeks due to the challenge faced by students who couldn't afford to be without work. In other words, the course duration is a relevant aspect that must be taken into consideration [15].
The enhancement courses are more accessible, with reduced costs, allowing the provision of suitable content linked to practical aspects. Recommendations from the International Atomic Energy Agency (IAEA) and the European Society for Radiotherapy (ESTRO) do not differentiate or tie appropriate training to the type of course offered. What matters is the content provided, the quality of classes and materials, and synchronization with practical aspects [16], [17], [18].
It's worth noting that the course needs to offer not only quality education but also financial viability to its students. According to data from the General Register of Employed and Unemployed (CAGED), the average salary for the Brazilian population aged 20 to 30 is R$ 1,696.22, while the minimum wage for a Radiology technician is currently R$ 2,331.38. In other words, it's necessary to align these numbers with the course cost and mobilize institutions interested in offering such training to facilitate potential cost-sharing in this accounting.
The results regarding the completed courses directly reflected in responses about the duration of the courses: 49 % took courses lasting between one and two years. 34.7 % underwent training lasting from six months to one year, and 12.2 % of respondents stated their professional course took more than two years to complete. Radiotherapy is a field lacking qualified professionals, still relatively unknown, yet offering numerous opportunities. However, only a minority of respondents had the availability to dedicate more than two years to a professional course. A duration of one to two years seems to be ideal, based on the target population of professionals [18].
The interviewed individuals constituted a relatively young population in the field of Radiotherapy. The majority (67.3 %) completed their training within a range of five to ten years from the present moment. In the subsequent question, aiming to assess how long the professional had been in the job market, this trend persisted, with 59.2 % of professionals having worked in the market for five to ten years. Despite being young, most respondents were not recent graduates but technicians with a wealth of knowledge, enhancing the credibility of the sample. It can also be concluded that a significant percentage of respondents – 59.2 % - underwent professional training and subsequently entered the job market.
Thirty-three (67.3 %) participants completed their training course with monthly activities, followed by 11 (22.4 %) with weekly activities, and three (6.1 %) with biweekly activities. The majority pursued the course with monthly activities, involving dedicating a few days each month to technical training. Given that it is a specialized refinement course primarily intended for professionals already engaged in the radiology job market, offering the course monthly is considered important since the 'frequency' factor can be a significant limitation for the interest and commitment of participants. Furthermore, focusing on the target population, it would be beneficial to provide the course on weekends, perhaps one weekend per month, to facilitate enrollment and accommodate the students' mobility.
Crucial information was gathered from the question that asked professionals to list the strengths of their training. The majority (40.8 %) emphasized the renowned team, valuing the technical expertise and recognition of the professionals comprising the teaching staff. In a 2022 article, Mary Coffey explored this relationship between the radiotherapy technician and the multidisciplinary team. Although the ultimate responsibility for the entire treatment lies with the radiation oncologist, encompassing clinical assessment, examination analysis, and precise delivery of the radiation dose, the responsibilities regarding patient positioning and the arrangement of technical parameters of the radiotherapy device fall directly on the radiotherapy technician. Often, this professional serves as an effective link between the patient and the rest of the multidisciplinary team. This responsible stance of the radiotherapy technician is a significant ally in ensuring high-quality support care. Therefore, training should provide this link as a facilitator of an effective connection with the patient [19], [20].
The questionnaire also allowed respondents to list the weaknesses of their training. This question was crucial for understanding students' expectations. The responses were more diverse, with the majority citing inflexibility of schedule as a weakness (29; 59.2 %), followed by the distance from their residence (12; 24.5 %). This issue was further explored by providing an open-ended opportunity to specify course weaknesses. There was only one justification, pointing to 'unqualified instructors' as a weakness. By identifying schedule inflexibility as the primary weakness in professional training, respondents confirmed information collected throughout the questionnaire: these are professionals aiming for specialization but intend to undergo training without interrupting their professional activities. This highlights the need for the educational institution to adapt by offering schedule flexibility and suitable curricula to meet this demand.
Often, educational institutions offer specialization or improvement courses to students, consisting only of theoretical coursework and requiring the student to independently find a radiation therapy service in the job market that willingly accepts them to complete a certain number of hours/lessons as an internship. Hence, the response of approximately 70 % of respondents having completed their course without a guarantee of practical learning. Without this, students are unable to receive the course completion certificate. This reality occurs nationwide in Brazil and leads to frustration and even revolt among many students. Besides investing in a course that doesn't provide comprehensive training, students often end up without the Certificate of Completion, posing a significant challenge to entering the job market.
With the innovation in radiotherapy and the incorporation of increasingly localized and precise techniques that allow radiation to be delivered to more specific areas with a high dose gradient, sparing healthy peri-lesional structures, the knowledge of the radiotherapy technician has become crucial. This professional is taking on greater responsibility, and their role in the patient care workflow is becoming increasingly important. The success of dose delivery in radiotherapy essentially depends on the delineation performed by the doctor, the planning by the physics professional, and the proper execution of the treatment carried out by the radiotherapy technician. The training of this professional, once neglected, must be highly qualified and valued.
The understanding that adequate training involves well-founded theoretical knowledge, and the assisted practical application of that knowledge is a consensus among educators and a goal to be pursued. This is a current and still understudied topic in the field of technical training in radiotherapy, lacking robust data in Brazilian and worldwide literature. Hence, this is a pioneering study on the national scene that sought to elucidate the real situation of the training of radiotherapy technicians in the workforce. [21].
In other words, the knowledge acquired through the application of the evaluative instrument provided important support for the creation of an Enhancement Course in Radiotherapy for Radiology Technicians with Synchronicity of Theoretical and Practical Learning.
Conclusion
The data obtained through the exploration of essential characteristics for the quality training of professionals (radiation therapy technicians or technologists), from the strategic perspective of those currently working in this job market, emphasized the need for an adjustment in the offering of courses for technical training in Radiotherapy. Specifically, the presence of a recognized team in the professional field should be combined with ensuring practical learning to support significant educational foundations. Furthermore, flexibility in schedules must be considered. This information aims to provide more well-structured foundations for the contemporaneity of the teaching–learning process, considering the current characteristics of society, technological advancements, and the demands of future students.
Recommendations for the future
Taking into account the reality of Brazil, we understand that the radiotherapy training course may cover 180 h/class (being characterized as an Improvement Course), containing practical activities included in its timetable, allowing the student flexibility regarding class times, since many of them are working in other areas of radiology and, finally, contain the Active teaching methodology since the active teaching methodology in a radiotherapy improvement course can provide a more engaging, practical learning environment and focused on the real application of knowledge, preparing professionals to face the challenges of the area more effectively [22], [23].
CRediT authorship contribution statement
M. Strasser: Writing – original draft. M.H. Senger: Writing – review & editing.
References
- 1.Barton M.B., Allen S., Delaney G.P., Hudson H.M., Hao Z., Allison R.W., et al. Patterns of retreatment by radiotherapy. Clin Oncol (R Coll Radiol) 2014 Oct;26(10):611–618. doi: 10.1016/j.clon.2014.03.008. [DOI] [PubMed] [Google Scholar]
- 2.Brasil. Ministério da Saúde. INCA; Rio de Janeiro: 2000. Instituto nacional de câncer. curso para técnicos em radioterapia. [Google Scholar]
- 3.Brasil. Ministério da Educação. Catálogo Nacional de Cursos Técnicos [Internet]. [2023] [acessed in: 22 jun. 2023]. Available in: http://cnct.mec.gov.br.
- 4.Brasil. Presidência da República. Casa Civil Subchefia para Assuntos Jurídicos. Decreto no 41.907, de 29 de Julho de 1957 [Internet] [acessed in: 22 jun. 2023]. Available in: https://legislacao.presidencia.gov.br/atos/?tipo=DEC&numero=41907&ano=1957&ato=b10QTSU5ENNRVT7c6.
- 5.IAEA. Human health series. Planning national radiotherapy services: a practical tool [internet] Internacional Atomic Energy Agency. 2010 https://www.iaea.org/publications/8419/planning-national-radiotherapy-services-a-practical-tool [acessed. In: 15 abr. 2020]. Available in: [Google Scholar]
- 6.Sociedade Brasileira de Radioterapia. RT2030: Plano de Desenvolvimento da Radioterapia para a próxima Década [Internet]. 2020 [acessed in: 17 fev. 2023]. Available in: https://sbradioterapia.com.br/rt2030/.
- 7.Sintaresp – Sindicato dos Técnicos em Radiologia do Estado de São Paulo. Convenções coletivas [Internet]. [acessed in: 12 set. 2023]. Available in: https://www.sintaresp.com.br/site/Midias/Pagina/54/ConvencoesColetivas.
- 8.Bibault J.E., Franco P., Borst G.R., Van Elmpt W., Thorwhart D., Schmid M.P., et al. Learning radiation oncology in Europe: results of the ESTRO multidisciplinary survey. Clin Transl Radiat Oncol. 2018 Feb;8(9):61–67. doi: 10.1016/j.ctro.2018.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dubois N., Nguyet Diep A., Ghuysen A., Declaye J., Donneau A.F., Vogin G., et al. Training of radiotherapy professionals: status, content, satisfaction and improvement suggestions in the greater region. BMC Med Educ. 2022 Jun 22;22(1):485. doi: 10.1186/s12909-022-03567-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Senger MH, Campos MCG, Servidoni M de FCP, Passeri SMRR, Velho PENF, Toro IFC, et al.. Trajetória profissional de egressos do curso de Medicina da Universidade de Campinas (Unicamp), São Paulo, Brasil: o olhar do ex-aluno na avaliação do programa. Interface (Botucatu). 2018;22:1443–55. doi:10.1590/1807-57622017.0190.
- 11.Castellanos M.E.P., Silveira A.F.M.H., Martins L.C., Nascimento V.B., Silva C.S., Bortollotte F.H.B., et al. Perfil dos egressos da Faculdade de Medicina do ABC: o que eles pensam sobre a atenção primária a saúde? Arq Bras Cienc Saúde. 2009;34(2):71–79. doi: 10.7322/abcs.v34i2.130. [DOI] [Google Scholar]
- 12.Caovilla F., Leitzke L., Menezes H.S., Martinez P.F. Perfil do medico egresso do curso de medicina da universidade luterana do brasil (ULBRA) Rev AMRIGS. 2008;52(2):103–109. [Google Scholar]
- 13.Karadza V., Manestar V., Cipric D. Case report: ESTRO/IAEA project: “best Practice in radiation oncology – a course to train RTT (radiation TherapisTs) trainers” – croatian experience. Tech Innov Patient Supp Radiat Oncol. 2018;8:8–9. doi: 10.1016/j.tipsro.2018.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Portal de Cusrsos técnicos [Internet]. [acessed in: 24 set. 2023]. Available in: https://portalidea.com.br/index.php.
- 15.Glebovskaya V.V., Tkachev S.I., Nazarenko A.V., Dolgushin B.I., Khmelevskiy E.V., Kislyakova M.V. Case report: education and training of RTTs for radiation oncology departments in Russia. Tech Innov Patient Support Radiat Oncol. 2018 Nov;13(8):15–16. doi: 10.1016/j.tipsro.2018.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Iaea A syllabus for the education and training of rtts (radio therapists/therapy radiographers) [Internet] Internacional Atomic Energy Agency. 2005 https://www-pub.iaea.org/MTCD/Publications/PDF/TCS-25_web.pdf [acessed in 15 abr. 2020]. Available. In: [Google Scholar]
- 17.Benstead K., Lara P.C., Andreopoulos D., Bibault J.E., Dix A., Eller Y.G. Recommended ESTRO Core curriculum for radiation oncology/radiotherapy. Radiother Oncol. 2019 Dec;141:1–4. doi: 10.1016/j.radonc.2019.08.013. [DOI] [PubMed] [Google Scholar]
- 18.Brasil. Ministério do Trabalho e Emprego. Portal do Fundo de Amparo ao Trabalhador. Cadastro Geral de Empregados e Desempregados (CAGED) [Internet] [acessed in: 23 jun. 2023]. Available in: https://portalfat.mte.gov.br/programas-e-acoes-2/caged-3/.
- 19.Iaea . IAEA; Vienna: 2014. A handbook for the education of radiation therapists (RTTs) [Google Scholar]
- 20.Coffey M., Naseer A., Leech M. Exploring radiation therapist education and training. Tech Innov Patient Support Radiat Oncol. 2022 Sep;30(24):59–62. doi: 10.1016/j.tipsro.2022.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Frenk J., Chen L., Bhutta Z.A., Cohen J., Crisp N., Evans T. Health professionals for a new century: transforming education to strengthen health systems in an interdependent world. Lancet. 2010 Dec 4;376(9756):1923–1958. doi: 10.1016/S0140-6736(10)61854-5. [DOI] [PubMed] [Google Scholar]
- 22.Bollela V.R., Senger M.H., Tourinho F.S.V., Amaral E. Aprendizagem baseada em equipes: da teoria à prática. Medicina (Ribeirão Preto) 2014;47(3):293–300. [Google Scholar]
- 23.Cotta R.M.M. UFV; Viçosa: 2023. Organizadora. Métodos ativos de ensino, Aprendizagem e avaliação: da teoria à prática. [Google Scholar]