Abstract
Background:
The purpose of this study was to quantify the articular surfaces of the naviculocuneiform (NC) joint to help clinicians better understand common pathologies observed such as navicular stress fractures and arthrodesis nonunions.
Methods:
Twenty cadaver NC joints were dissected and the articular cartilage of the navicular, medial, middle, and lateral cuneiforms were quantified by calibrated digital imaging software. Statistical analysis included calculating the mean cartilage surface area dimensions of the distal navicular and proximal cuneiform bones. Length measurements on the navicular were obtained to estimate the geographic location of the interfacet ridges. Lastly, all facets of the articular surfaces were described in regard to the shape and location of cartilaginous or fibrous components. Results were compared using Student t tests.
Results:
Navicular cartilage was present over 75.4% of the surface area of the proximal NC joint, compared with 72.6% of combined cuneiform cartilage distally. The mean height of the deepest (dorsal-plantar) measurement of navicular articular cartilage was 18 ± 3 mm. The mean heights of the distal medial, middle, and lateral cuneiform articular facets were 15 ± 1 mm, 17 ± 2 mm, and 15 ± 2 mm, respectively.
Conclusion:
There is significant variation among the articular surfaces of the NC joint. Additionally, the central third of the navicular was calculated to lie in the inter-facet ridge between the medial and middle articular facets of the navicular.
Clinical Relevance:
Surgeons may consider this study data when performing joint preparation for NC arthrodesis as cartilage was present to a mean depth of 18 mm at the NC joint. Additionally, this study demonstrates that the central third of the navicular, where most navicular stress fractures occur, lies in the interfacet ridge between the medial and middle articular facets of the navicular.
Keywords: naviculocuneiform joint, midfoot, arthrodesis, navicular stress fracture
Introduction
The naviculocuneiform (NC) joint has an important role in numerous pathologies of the foot and ankle including primary and secondary arthritis, medial column instability, pes planovalgus deformity, and navicular stress fractures, among others.2,8,10 There is little published demonstrating the anatomic features of the NC joint complex or how it may relate to the development of these pathologies. There are studies in the published literature that investigate NC joint biomechanics as they relate to range of motion. It has been shown that the NC joint proportionally contributes the most to first ray range of motion in the sagittal plane, which has been linked to bunion deformities and other pathologies, demonstrating its importance in normal biomechanics. 2 Knowledge of the articular anatomy of the NC joint in the context of the function of the joint may assist in understanding the development of NC joint pathology. A common procedure to treat NC joint arthritis is arthrodesis; however, nonunion rates have been found to be as high as 6.5%, which may be contributed to by inadequate cartilage resection. 3 Providing mean values of cartilage depth may assist surgeons in understanding the level of resection required and instill confidence the appropriate amount of cartilage has been removed, increasing chance for union.
The purpose of the current study was to quantify and describe the articular surface of the NC joint to better understand its role in associated foot pathologies, notably arthrodesis nonunion.
Methods
Ten paired, below-knee embalmed specimens were obtained and dissected. All specimens included an intact foot and ankle. Specimens with evidence of previous foot and ankle surgery were excluded. The mean age of the donors was 76.9 (range, 56-91) years. There were 4 male and 6 female specimens. There were 10 left and 10 right specimens.
At room temperature, the specimens were carefully dissected at the level of the NC joint. The bones of interest included the navicular, medial cuneiform, middle cuneiform, and lateral cuneiform. Cadaver dissection was done under the guidance and supervision of a fellowship-trained orthopaedic foot and ankle surgeon. The cartilage of the involved joints was identified and quantified by calibrated digital imaging software. This was done by taking digital images of the joint surface, calibrating the image size, and processing this data with an image processing software as described by others (ImageJ 1.47, http://rsbweb.nih.gov/ij/). 4 In summary, the software uses an object (calibrated ruler) in the same image to use as calibration to base other geometric measurements (length, area, etc) on. Figures 1 to 7 demonstrate examples of the digital images with orientations labeled and included radiographs highlighting the direction each joint was viewed. After directly examining the individual navicular joint facets and the associated articular cartilage, a descriptive geometric shape was provided to assist with grouping variants of the facets (example: rhomboidal, arrowhead-shaped, and crescent). All statistical analysis was performed with Microsoft Excel.
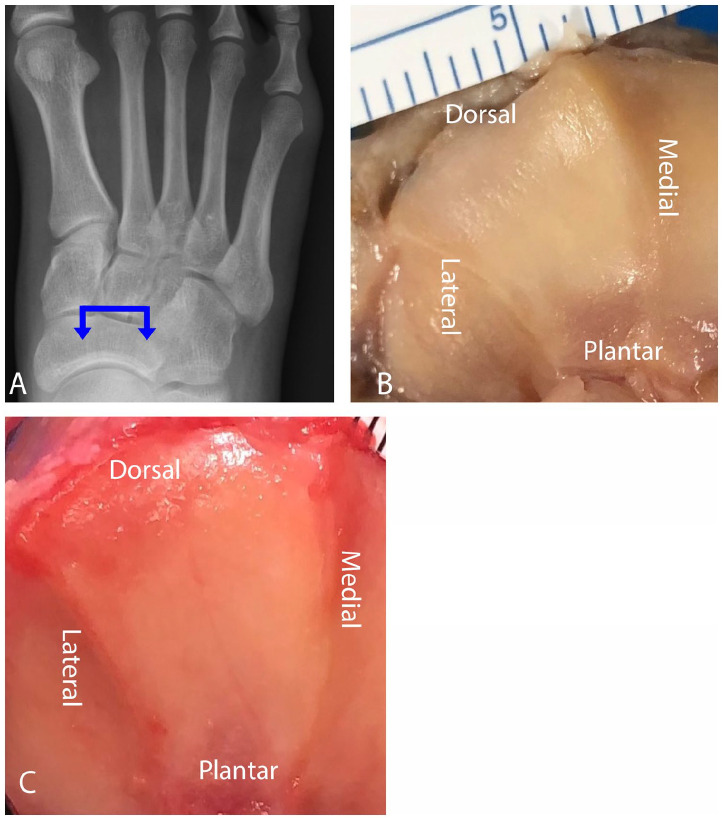
Figure 1.
(A) The proximal medial cuneiform articulation. The blue arrow denotes the direction of the viewing plane. (B) The “arrowhead” variant takes on the shape of a modified traditional triangle with a convex plantar base, 2 rounded corners at the base, and a dorsal directed apex. The majority of the fibrous component was located plantar. (C) The “rhomboidal” variant outlined by a rim of fibrous tissue dorsally, medially, and plantarly, with the fibrous thickening plantar to the articular cartilage.
Figure 7.
(A) The distal navicular articulation. The blue arrow denotes the direction of the viewing plane. (B) Example of the dorsal to plantar height of the navicular articular facet with the final mean and SD values displayed. The height value recorded for each specimen was obtained from one of the 3 navicular facets with the greatest measured height. (C) Example of length measurements of the navicular facets with final mean, SD, and percentage of the mean total navicular length displayed. Lengths measured were from the most medial aspect of the medial facet to the medial aspect of the middle facet and the medial aspect of the middle facet to the most lateral aspect of the lateral facet. (D) Example of total navicular length measurement with final mean and SD values displayed.
Results
For the proximal medial cuneiform articulation, the total mean surface area was 272 ± 61 mm2, with 69.6% of the area composed of articular cartilage (Table 1). The shape of the articular cartilage had 2 variations: arrowhead-shaped and rhomboidal (Figure 1). The arrowhead variant was the most common shape appreciated (70%, 14 of 20 specimens) and the rhomboidal variant was noted in 30% of specimens (6 of 20). The arrowhead variant had the basic shape of a traditional triangle; however, slightly modified with features of a convex plantar base with 2 rounded corners and a dorsal-directed apex. The fibrous aspect of the articulation could be found dorsal at the apex, as well as medial and plantar to the articular cartilage with most of the fibrous component located plantar. The rhomboidal variant was outlined by a rim of fibrous tissue dorsally, medially, and plantarly with the fibrous tissue thickening plantar to the articular cartilage. All surfaces of the articulations were found to be concave.
Table 1.
Joint Surface Measurements.
| Joint Surface | Mean Total Surface Area, mm2 (SD, Range) | Mean Articular Cartilage Surface Area, mm2 (SD, Range) | Mean Total Surface Area that is Articular Cartilage (%) | Mean Facet Dorsal to Plantar Height, mm (SD, Range) |
|---|---|---|---|---|
| Proximal medial cuneiform | 272 (61, 173-370) | 190 (29, 143-253) | 70 | 15 (1, 13-18) |
| Proximal middle cuneiform | 234 (36, 153-299) | 177 (32, 113-215) | 76 | 17 (2, 14-21) |
| Proximal lateral cuneiform | 202 (28, 145-269) | 153 (21, 117-195) | 76 | 15 (2, 12-19) |
| Proximal navicular | 739 (83, 627-917) | 557 (71, 456-707) | 75 | 18 (3, 16-24) |
For the proximal middle cuneiform articulation, the mean total surface area was 234 ± 36 mm2, with 75.7% of the area composed of articular cartilage. The shape of the articular cartilage had 2 variations: triangular and crescent-shaped (Figure 2). The triangular variant was the most common (90%, 18 of 20 specimens), and the crescent variant was appreciated in 10% of specimens (2 of 20). The triangular variant had a dorsal base outlined with a thin rim of fibrous tissue and a blunted plantar-directed apex for which fibrous tissue notably thickens. The crescent variant could be described as that of a “half-moon,” with the medial aspect of the facet being convex and the lateral aspect concave. The majority of the fibrous portion of the articulation was located plantarly. Of all specimens, 90% (18 of 20) of the articular surfaces were found to be concave, with 10% (2 of 20) noted to be convex.
Figure 2.
(A) The proximal middle cuneiform articulation. The blue arrow denotes the direction of the viewing plane. (B) The “triangular” variant with a dorsal base outlined with a thin rim of fibrous tissue and a blunted plantar-directed apex. (C) The “crescent” variant could be described as that of a “half-moon” with the medial aspect of the facet convex and the lateral aspect concave. The majority of the fibrous component of the articulation was located plantarly.
For the proximal lateral cuneiform articulation, the total mean surface area was 202 ± 28 mm2, with 75.8% of the area composed of articular cartilage. The shape of the articular cartilage had 2 variations: oval and rhomboidal (Figure 3). The oval variant was the most common (90%, 18 of 20 specimens) and the rhomboidal variant was noted in 10% of specimens (2 of 20). The oval and rhomboidal variants both had similar distributions of fibrous tissue with a very thin rim found dorsal to the articulation with notable thickening of the fibrous tissue laterally and plantarly. All surfaces of the articulations were found to be flat to slightly convex.
Figure 3.
(A) The proximal lateral cuneiform articulation. The blue arrow denotes the direction of the viewing plane. The (B) “oval” and (C) “rhomboidal” variants, both with thin rims of fibrous tissue found dorsal to the articulation with significant thickening of the fibrous tissue laterally and plantarly.
For the distal navicular articulation, the total mean surface area was 739 ± 83 mm2, with 75.4% of the area composed of articular cartilage. The shape of the medial navicular facet had 3 variations: triangular, trapezoidal, and rhomboidal, with the triangular variant being the most common (50%, 10 of 20 specimens) (Figure 4). The trapezoidal variant was seen in 45% of specimens (9 of 20) and the rhomboidal variant was seen in 5% of specimens (1 of 20). The triangular variant had a dorsal directed apex with 2 rounded corners at the plantar base. The fibrous component of the facet articulation was predominantly located at the plantar base with a thin rim of fibrous tissue along the medial border of the facet and at the dorsal apex. The trapezoidal and rhomboidal variants were noted to have an abundance of fibrous tissue outlining the plantar base and medial border of the facets, and with a thin rim along their dorsal border. All surfaces of the articulations were found to be convex.
Figure 4.
(A) The distal medial navicular articulation. The blue arrow denotes the direction of the viewing plane. (B) The “triangular” variant with a dorsal-directed apex and 2 rounded corners at the plantar base. The fibrous component of the articulation is predominantly located at the plantar base with a thin rim of fibrous tissue along the medial border and dorsal apex. (C, D) The (C) “trapezoidal” and (D) “rhomboidal” variants, both with fibrous tissue outlining the plantar base and medial border of the facets, with a thin rim of fibrous tissue along their dorsal border.
The middle navicular facets in all specimens were noted to be triangular in shape with a dorsal base and plantar directed apex (Figure 5). There was a thin rim of fibrous tissue at the dorsal base, and the apex of the facet served as a convergence point for the fibrous tissue located at the plantar aspect of the navicular bone. Of all specimens, 80% (16 of 20) of the articular surfaces were found to be convex, with 20% (4 of 20) noted to be concave. The lateral navicular facet had 3 variations: quadrilateral, egg-shaped, and triangular (Figure 6). The most common variant observed at 50% of specimens was quadrilateral (10 of 20). The egg-shaped variant was present in 35% of specimens (7 of 20) and the triangular variant in 15% of specimens (3 of 20). The fibrous component of the quadrilateral variant was located at the dorsal, lateral, and plantar edges of the facet. The egg-shaped and triangular variants had similar morphology consisting of a plantar-directed apex, medial and lateral borders, and a dorsal base. However, the egg-shaped variant differed from the triangular variant, with the egg-shaped variant possessing a relatively convex dorsal base compared to the flat base of the triangular variant. The egg-shaped and triangular variants also had similar fibrous components located at the dorsal and lateral borders of the facet, as well as the plantar apex. All surfaces of the articulations were found to be concave.
Figure 5.
(A) The distal navicular middle articulation. The blue arrow denotes the direction of the viewing plane. (B) The “concave” variant of the facet. The facet is triangular with a dorsal base and a plantar-directed apex. There is a thin rim of fibrous tissue located at the dorsal base, and the plantar apex of the triangle acts as a convergence point for the plantar fibrous tissue of the navicular. (C) The “convex” variant demonstrating a triangular-shaped facet with a dorsal base and a plantar-directed apex. Similar to the concave variant, there is a thin rim of fibrous tissue located at the dorsal base, and the plantar apex of the triangle acts as a convergence point for the plantar fibrous tissue of the navicular.
Figure 6.
(A) The distal lateral navicular articulation. The blue arrow denotes the direction of the viewing plane. (B) The quadrilateral variant with fibrous tissue located at the dorsal, lateral, and plantar edges of the facet. (C) The triangular variant with a plantar-directed apex, medial, and lateral borders and a flat dorsal base. The fibrous component of the facet was located at the dorsal and lateral borders, as well as the plantar apex. (D) The egg-shaped variant with a plantar-directed apex, medial and lateral borders, and a convex dorsal base. The fibrous component of the facet was located at the dorsal and lateral borders, as well as the plantar apex.
The difference between the mean total articular surface area of the medial vs the middle cuneiform, the medial vs the lateral cuneiform, and the middle vs the lateral cuneiform was statistically significant (Table 2). The difference between the mean surface area that was articular cartilage of the medial vs the lateral cuneiform and the middle vs the lateral cuneiform was statistically significant. However, the difference between the mean surface area that was articular cartilage of the medial vs the middle cuneiform was not statistically significant (Table 3).
Table 2.
Comparison of Proximal Cuneiform Joint Mean Total Surface Area Measurements.
| Proximal Medial Cuneiform Joint Surface Area, mm2, Mean (SD) |
Proximal Middle Cuneiform Joint Surface Area, mm2, Mean (SD) |
Proximal Lateral Cuneiform Joint Surface Area, mm2, Mean (SD) |
P Value a |
|---|---|---|---|
| 272 (61) | 234 (36) | .03 | |
| 272 (61) | 202 (28) | .0001 | |
| 234 (36) | 202 (28) | .006 |
Boldface indicates statistical significance (P < .05).
Table 3.
Comparison of Proximal Cuneiform Joint Mean Articular Cartilage Surface Area Measurements.
| Proximal Medial Cuneiform Joint Surface Area, mm2, Mean (SD) |
Proximal Middle Cuneiform Joint Surface Area, mm2, Mean (SD) |
Proximal Lateral Cuneiform Joint Surface Area, mm2, Mean (SD) |
P Value a |
|---|---|---|---|
| 190 (29) | 177 (32) | 0.25 | |
| 190 (29) | 153 (21) | 0.0002 | |
| 177 (32) | 153 (21) | 0.0143 |
Boldface indicates statistical significance (P < .05).
The mean total length of the navicular from the most medial aspect of the medial navicular articular facet to the most lateral aspect of the lateral navicular articular facet was 34 ± 3 mm. The mean length from the most medial aspect of the medial navicular facet to the most medial aspect of the middle navicular facet was 14 ± 2 mm, approximately 41.3% of the mean total length across all 3 navicular articular facets. The mean length from the most medial aspect of the middle navicular facet to the most lateral aspect of the lateral navicular facet was 23 ± 2 mm, approximately 66.3% of the mean total length across all 3 navicular articular facets (Figure 7).
The mean height of the navicular articular facet measured in a dorsal to plantar direction was 18 ± 3 mm. For simplicity, the value included in the data was the navicular facet, with the greatest height measured of the medial, middle, and lateral facets (Figure 7). The mean height of the medial, middle, and lateral cuneiform articular facet was 15 ± 1 mm, 17 ± 2 mm, and 15 ± 2 mm, respectively.
Discussion
The current study demonstrates that the NC articulations are composed of greater than 50% articular cartilage. There was variation appreciated between the cuneiforms in the mean total articular surface area and the mean surface area that was articular cartilage. A wide range of measured values for both articular surface area and facet height were observed.
A common procedure to treat NC joint arthritis is arthrodesis. Nonunion rates of NC joint arthrodesis have been found to be as high as 6.5%, and there remains little in the literature regarding contributory factors for NC joint arthrodesis nonunion. 3 One potential reason for nonunion may be inadequate cartilage resection. The current study demonstrates that the greatest mean height of the navicular articular facet was 18 ± 3 mm. The mean heights of the medial, middle, and lateral cuneiform facets were 15 ± 1 mm, 17 ± 2 mm, and 15 ± 2 mm, respectively. These values can help guide the surgeon intraoperatively to ensure adequate cartilage resection including the plantar aspect, providing confidence that adequate resection was obtained, and decreasing the risk for nonunion. Additionally, this study offers data to guide implant length near these joints.
The NC joint has been described by several authors. In his text titled Sarrafian’s Anatomy of the Foot and Ankle, Kelikian describes the NC joint in detail. 6 Our results both support and refute portions of this description. With regard to the medial navicular facet, similar to Kelikian, our results demonstrate the medial facet as strictly convex with 100% of specimens in our study possessing a convex medial navicular facet articular surface. However, although a triangular medial navicular facet was the most common geometric shape observed in our study, there was variation. Our data revealed 2 additional geometric variants to the medial navicular facet, including a trapezoidal and rhomboidal variant. With regard to the middle navicular facet, our results are similar to Kelikian in that 100% of specimens had a triangular shape with the orientation of a dorsal base and plantar directed apex. However, although most specimens in our study possessed a convex middle navicular facet articular surface, a portion of specimens (20%) demonstrated a concave middle navicular facet articular surface. Lastly, with regard to the lateral navicular facet, Kelikian describes the facet as quadrilateral. Although most specimens in our study demonstrated a quadrilateral shape, there were 2 additional variants appreciated including a triangular and egg-shaped variant. Similar to Kelikian, our data support the lateral navicular facet having a concave surface, with 100% of cadaveric specimens possessing a concave articular surface. The differences appreciated between our results and what Kelikian describes suggests there is notable variation in the geometric shape and concavity or convexity of the navicular articular facets.
Ajmani et al 1 studied 300 adult cuneiform bones (100 of each medial, middle, and lateral cuneiform bones) from 75 male and 25 female sources. They found notable anatomic variation in cuneiform articular facet patterns including 10 medial cuneiform patterns, 7 middle cuneiform patterns, and 14 lateral cuneiform patterns. The incidence of various patterns of the articular facets of the cuneiform bones were significantly different both between males and females, as well as between right and left sides. Our study supports these findings by also demonstrating multiple variants in cuneiform articular facet patterns with 2 medial cuneiform facet shapes, 2 middle cuneiform facet shapes, and 2 lateral cuneiform facet shapes identified. Unlike Ajmani et al, our study included descriptions of the navicular facets including 3 medial navicular facet shape variants, 1 middle navicular facet shape variant, and 3 lateral navicular facet shape variants. In addition, the current study adds to the work of Ajmani et al by quantifying the cartilage of the NC joint articulation.
Renner et al reported the mean height and width of the navicular articular surface, as well as the medial, middle, and lateral cuneiform facets in 10 cadaveric specimens. They found that the middle cuneiform facet had the largest height of the 3 cuneiform facets, followed by the medial, then the lateral cuneiform facet. 9 However, they did not quantify the articular surface area of the navicular or cuneiform articular surfaces and did not include measurements of the cartilaginous portion of each articular surface, which our study addresses. Our study supports Renner’s data with regard to the middle cuneiform facet having the greatest height, the medial cuneiform facet being the next greatest in height, and the lateral cuneiform facet having the lowest height. Although the order of greatest to lowest height value is comparable to Renner’s findings, the values of heights obtained in our study differ. This may be explained by the different measurement techniques between studies. Although our study used digital, calibrated images of the joint surface that were quantified by an image processing software, Renner et al utilized a depth gauge to obtain height measurements.
Navicular stress fractures represent one-third of all stress fractures in the human body, most commonly in young, high-demand athletes. 11 Relative hypovascularity of the central aspect of the navicular is thought to increase the risk of stress fracture and osteonecrosis in the middle or central third of the bone. 8 Additionally, there is a biomechanical etiology theory implying the central third of the navicular being at highest risk due to mechanical impingement by the talar head and cuneiforms. 7 More specifically, during the end of the stance phase when the forefoot becomes loaded, the navicular bone experiences maximal compression between the talar head and the first and second tarsometatarsal (TMT) joint. 5 The talonavicular (TN) joint is subjected to medial compression forces originating from the first TMT joint, as well as lateral compression forces originating from the second TMT joint. In addition, the posterior tibialis tendon insertion subjects the medial navicular to increased medial stress, producing an unequal distribution of medial and lateral forces creating a shear force. During activities such as running, this shear force is localized at the center third of the navicular, the known watershed area of the bone, causing a bending phenomenon. 5 Our study may support this biomechanical theory with results suggesting the central third of the navicular lies in the interfacet ridge between the medial and middle facet articulations of the NC joint, demonstrating there likely is a difference in contact forces between the first and second ray at the navicular. However, it should be noted there are some baseline assumptions applying our data to this theory and it would be better validated with a biomechanical study demonstrating direct pressure measurements on each of the NC joints.
The current study has several limitations. First, this was a cadaver study with a relatively small sample size and may not represent the general population. Second, the articular surface is not flat and is projected onto a flat digital image. The accuracy of this image-based measurement technique has not been quantified. In the current joints studied, we estimate the error caused by this parallax to be less than 1% because the joint surfaces are nearly flat.
In conclusion, our data support the notion that the NC joint is not completely uniform articular cartilage and there are 3 distinct articular surfaces. This builds on previous cadaveric studies completed and adds further data by including articular surface area and depth calculations. Perhaps most importantly, the data describing this variation in cuneiform cartilaginous anatomy and depth may highlight a primary risk factor for isolated NC joint arthrodesis nonunion. Surgeons can use the current study’s reported NC joint articular facet variation and calculated mean NC joint articular facet heights to perform a successful arthrodesis and minimize risk of bony nonunion. Lastly, our study’s further analysis of the facet anatomy of the navicular may provide additional insight into the anatomic biomechanical origin of navicular stress fractures.
Supplemental Material
Supplemental material, sj-pdf-1-fao-10.1177_24730114241245396 for Anatomy of the Naviculocuneiform Joint Complex by George Borrelli, Maxwell Albiero and James Jastifer in Foot & Ankle Orthopaedics
Footnotes
Ethics Approval: Ethical approval was not sought for the present study.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. Disclosure forms for all authors are available online.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Maxwell Albiero, MD,  https://orcid.org/0009-0005-0499-9610
https://orcid.org/0009-0005-0499-9610
References
- 1. Ajmani ML, Ajmani K, Jain SP. Variations in the articular facets of the adult cuneiform bones. Anthropol Anz. 1984;42(2):121-126. Accessed April 1, 2020. http://www.ncbi.nlm.nih.gov/pubmed/6465870 [PubMed] [Google Scholar]
- 2. Chan F, Bowlby MA, Christensen JC. Medial column biomechanics: nonsurgical and surgical implications. Clin Podiatr Med Surg. 2020;37(1):39-51. doi: 10.1016/j.cpm.2019.08.004 [DOI] [PubMed] [Google Scholar]
- 3. Chu AK, Wilson MD, Lee J, So E, Prissel MA, Hyer CF. The incidence of nonunion of the naviculocuneiform joint arthrodesis: a systematic review. J Foot Ankle Surg. 2019;58(3):545-549. doi: 10.1053/j.jfas.2018.09.014 [DOI] [PubMed] [Google Scholar]
- 4. Collins TJ. ImageJ for microscopy. Biotechniques. 2007;43(1 suppl):S25-S30. doi: 10.2144/000112517 [DOI] [PubMed] [Google Scholar]
- 5. Hossain M, Clutton J, Ridgewell M, Lyons K, Perera A. Stress fractures of the foot. Clin Sports Med. 2015;34(4):769-790. doi: 10.1016/j.csm.2015.06.011 [DOI] [PubMed] [Google Scholar]
- 6. Kelikian AS, Sarrafian SK. Sarrafian’s Anatomy of the Foot and Ankle: Descriptive, Topographic, Functional. 3rd ed. Wolters Kluwer Health/Lippincott Williams & Wilkins; 2011:73. [Google Scholar]
- 7. Mandell JC, Khurana B, Smith SE. Stress fractures of the foot and ankle, part 2: site-specific etiology, imaging, and treatment, and differential diagnosis. Skeletal Radiol. 2017;46(9):1165-1186. doi: 10.1007/s00256-017-2632-7 [DOI] [PubMed] [Google Scholar]
- 8. Prapto D, Dreyer MA. Anatomy, Bony Pelvis and Lower Limb, Navicular Bone. 2020. Accessed March 31, 2020. http://www.ncbi.nlm.nih.gov/pubmed/31613455 [PubMed]
- 9. Renner K, McAlister JE, Galli MM, Hyer CF. Anatomic description of the naviculocuneiform articulation. J Foot Ankle Surg. 2017;56(1):19-21. doi: 10.1053/j.jfas.2016.09.013 [DOI] [PubMed] [Google Scholar]
- 10. Roddy E, Thomas MJ, Marshall M, et al. The population prevalence of symptomatic radiographic foot osteoarthritis in community dwelling older adults: cross-sectional findings from the clinical assessment study of the foot. Ann Rheum Dis. 2015;74(1):156-163. doi: 10.1136/annrheumdis-2013-203804 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Shakked RJ, Walters EE, O’Malley MJ. Tarsal navicular stress fractures. Curr Rev Musculoskelet Med. 2017;10(1):122-130. doi: 10.1007/s12178-017-9392-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-fao-10.1177_24730114241245396 for Anatomy of the Naviculocuneiform Joint Complex by George Borrelli, Maxwell Albiero and James Jastifer in Foot & Ankle Orthopaedics