Abstract
Background:
Nonsurgical guidelines recommend implementing a correctly fitted bra when managing back pain among larger breasted women. Achieving this is challenging with current bra solutions, sizing principles, and fitting approaches. Persistent wearing of an ill-fitting bra can cause negative health implications, including non-specific back pain.
Objectives:
This study investigated immediate and short-term biomechanical and pain responses to changing breast support garment among larger breasted women with non-specific back pain.
Methods:
Participants (n = 24) performed a standing task, drop jumps, and seated typing tasks while bra and spinal kinematic data were recorded. Five breast support conditions were assessed: participants’ usual bra (control), a professionally fitted bra in the immediate term (standard) and after 4 weeks wear (standard28), and a bra with an alternative design, measurement, and fitting approach in both the immediate term (alternative) and after 4 weeks wear (alternative28). A bra fit assessment and clinical pain/disability questionnaires were included.
Results:
All participants failed the bra fit assessment in the control bra, compared with 87.5% (n = 21) in the standard and 4.2% (n = 1) in the alternative bras. The standard28 and alternative28 bras provided symptomatic relief, with the alternative28 bra improving a greater number of outcome measures. Reduced nipple-sternal-notch distance was observed only in the alternative28 bra condition.
Conclusions:
Symptomatic relief may be associated with the resting position of the breast tissue on the anterior chest wall. The alternative bra may provide potential clinical benefit if implemented as part of a nonsurgical or conservative pain management strategy. Alternative breast support garments should be considered to provide solutions to the problems associated with traditional bras.
Keywords: back pain, rehabilitation, breast support, bra fit, bra biomechanics
Background
Larger breasted women (D±) regularly seek medical assistance for symptoms associated with chronic back pain.1,2 The prevalence of chronic back pain among larger breasted women may increase due to the continuously increasing average bra size.2 Current treatment strategies for this patient group are mostly surgical, although specific eligibility criteria limit accessibility to reduction surgery through the National Health Service (NHS).3 Because the NHS does not record the annual number of patients who are denied surgery, the number of larger breasted women living with chronic back pain is not known.
Conservative strategies for managing chronic back pain among larger breasted women recommend the introduction of a correctly fitted bra.3 Between 75% and 100% of women wear the wrong-sized bra daily, regardless of whether they have used a professional bra-fitting service,4-6 and this highlights the challenge of achieving correct bra fit with current standard solutions. It has been suggested that synergies may exist between the development of non-specific back pain (NSBP) and wearing an ill-fitting bra.6-8 However, whether it is breast size or bra fit that contributes to the development of chronic back pain remains unknown. Proposed causal mechanisms for the development of NSBP among larger breasted women who fail to correctly support their breasts relate to compensatory, mechanical postural changes at the thoracic region, due to the heavy load of the breasts on the anterior chest wall.1 Wearing a sports bra to achieve symptomatic relief through increased support has been advocated, and it has been hypothesized that implementing a correctly fitting bra may lead to improvements comparable with surgical intervention,4 but this is yet to be confirmed.
This study explores changes in painful symptoms in response to a short-term conservative intervention implementing different breast support garments. This study aimed to explore how different breast support garment designs affect bra fit quality, painful symptoms, and biomechanical parameters of breast support and posture among larger breasted women with chronic NSBP.
Methods
The University Ethics Committee approved this study (STEMH241), and written informed consent was obtained.
Participants
The sample size calculation was based on studies that have used a Numerical Pain Rating Scale as an outcome among individuals with chronic back pain to measure responsiveness to a conservative intervention.9,10 A sample size calculation suggested that 19 participants were required to detect a significant difference of 1.4 with a standard deviation of 1.3 at the 5% significance level with 90% power.
Initial eligibility criteria stipulated that participants had to be female, aged older than 18 years – 50 years and not yet experiencing menopausal symptoms, with chronic NSBP, and a bra cup size D+. A screening process was implemented to exclude anybody with indicators of potentially serious pathology.11 Pregnant and breastfeeding women or those with a history of breast surgery were also excluded.5,10,12,13
Study design
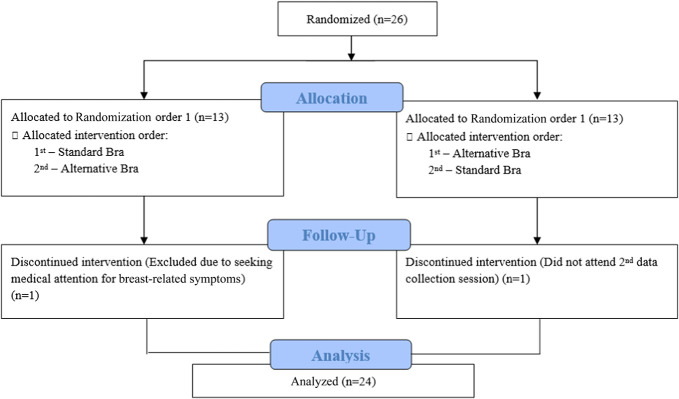
This study was a crossover intervention study, where all participants were exposed to all interventions. Data collection comprised 3 sessions over 8 weeks. Data collection sessions were conducted in the University’s motion analysis laboratory and were separated by two, 4-week intervention phases (Figure 1). Each intervention period incorporated 1 of 2 different breast support garments, the order of which was randomized among participants, using permuted block randomization.14 An intervention period of 4 weeks was considered suitable based on previous studies investigating conservative interventions to improve posture and symptoms of chronic back pain.10,15-17
Figure 1.
Consort diagram.
Breast support conditions
Three breast support garments generated 5 breast support conditions within this study: (1) Control—participants' own usual bra; (2) Standard—a brand new professionally fitted bra (full cupped, with straps, not a sports bra), which reflects a traditional bra; (3) Standard28—the standard bra after a 4-week intervention period; (4) “Alternative”—a brand new breast support garment, which adopts an alternative approach to measurement, sizing, and fitting (Optifit, Saddleworth, United Kingdom; Figure 2); and (5) “Alternative28”—the alternative bra after a 4-week intervention period. To offer ecological validity to the study, the Standard bras were fitted at high street retail stores who offered a professional bra-fitting service by bra fitters who were blinded to the study. To emphasize, the Standard bra condition used a professional bra-fitting service, but this did not guarantee correct fit.
Figure 2.

The alternative bra (www.optifitbra.com). Reprinted with permission from Optifit Bra Company Ltd.
The alternative intervention implemented a different measurement, sizing, and fitting approach. Predominant differences compared with a traditional bra are as follows:
Measurement: 3 anthropometric measurements are taken to generate a bra size rather than 2 measurements as per the standard bra.
Design: a patented wire-free technology, a diagonally positioned underband that supports the breasts high under the inframammary fold and transfers the breast weight from the thoracic to lumbar region with a lower posterior band.18
Protocol
A 10-camera motion capture system (Qualisys, SE) was used to record bra and intersegmental spinal kinematics,13 during upright standing, sitting, and a drop jump task from a 20-cm high step.13 A review of previous breast biomechanics research suggests that the supportive capabilities of a bra can be best determined using an activity that induces vertical breast displacement,19 and therefore, a vertical drop jump task was considered a suitable task to include.
Retroreflective markers were applied bilaterally over the acromions, anterior superior iliac spines, posterior superior iliac spines, calcanei, and suprasternal notch. Spinal marker clusters were positioned at C7,T7, L3, and L5 to define 4 spinal segments; upper thoracic, lower thoracic, upper lumbar, and lower lumbar.13,20 A 4-marker pelvic cluster was also included within the marker set to ensure marker visibility.
For the bra-related kinematic data, the first marker of the breast cluster was placed directly over the nipple, guided by the participant. To standardize the breast marker placement, a template was used to ensure that markers were placed equidistant around the central nipple marker. Although analysis of breast displacement is not a new concept, published research generally tends to use only 1 nipple marker to assess the displacement of the whole breast.21-23 It has been identified that although a single nipple marker suitably represents whole breast motion,24 recent research recommends the use of a breast marker set rather than a single nipple marker to enable capturing of complex breast motion.19 Therefore, the breast marker cluster combined 5 markers.
Bra fit assessment
A bra fit assessment was conducted by the researchers in all 3 bras (control, standard, and alternative) to evaluate bra fit quality. The assessment considers the fit of component parts of the bra (cup, band, straps, underwire) against set criteria and has been used in previous breast-related research.5,13,25 Identification by the researchers of 1 or more bra fit issues resulted in a failed assessment, indicating incorrect bra fit.5,13,25
Participant-reported outcome measures
Participant-Reported Outcome Measures (PROMs) were collected at baseline (reported as the control condition), to understand symptoms before intervention, and after the 2 intervention periods (standard28 and alternative28). Three validated pain measures were used: (1) body chart pain location analysis1,26-29; (2) Numerical Rating Scales (NRS)10,30-32 for back pain, stiffness, and discomfort; and (3) Short-Form McGill Pain Questionnaire 2 (SF-MPQ-2).33,34 Two functional disability outcomes were used: (1) Neck Disability Index (NDI)32,35 and (2) World Health Organization Disability Assessment Schedule 2.0 (WHODAS 2.0).36
Data processing and analysis
Kinematic data were collected using Qualisys Track Manager (QTM v2.13; Qualisys AB, Sweden). Raw coordinate data were imported into Visual 3D (Version 6.01.08, C-Motion, Maryland) in c3d format for processing.
Nipple-Sternal-Notch (NSN) distance was recorded as a measure of static breast position. In Visual 3D, left and right nipple marker signals were subtracted from the sternal notch marker in the X, Y, and Z axis. Data were exported into Microsoft Excel 2016 (Microsoft Corp) where the mean and standard deviations were calculated from the normalized data. NSN distance was then calculated, in centimeters, using the three-dimensional Pythagorean equation.13
All remaining kinematic measures were calculated using the local coordinate system of 1 marker cluster relative to the local coordinate system of another marker cluster; the axis conventions for each marker cluster are shown in Figure 3. From the drop jump data, bra displacement was calculated in 3 directions: mediolateral, anterior-posterior, and superior-inferior. The locations of the left and right breast marker clusters were calculated relative to the lower thoracic marker cluster from when the participant’s feet left the step to the point at which the anterior superior iliac spine markers ceased moving upward after landing. The left and right breasts were selected as the targeted segments, with the reference segment and resolution coordinate system set as the lower thoracic segment. The X, Y, and Z data signals were exported into Microsoft Excel where minimum and maximum values for the 3 signal components were calculated. To determine the displacement in each direction, the difference between minimum and maximum values was calculated.
Figure 3.
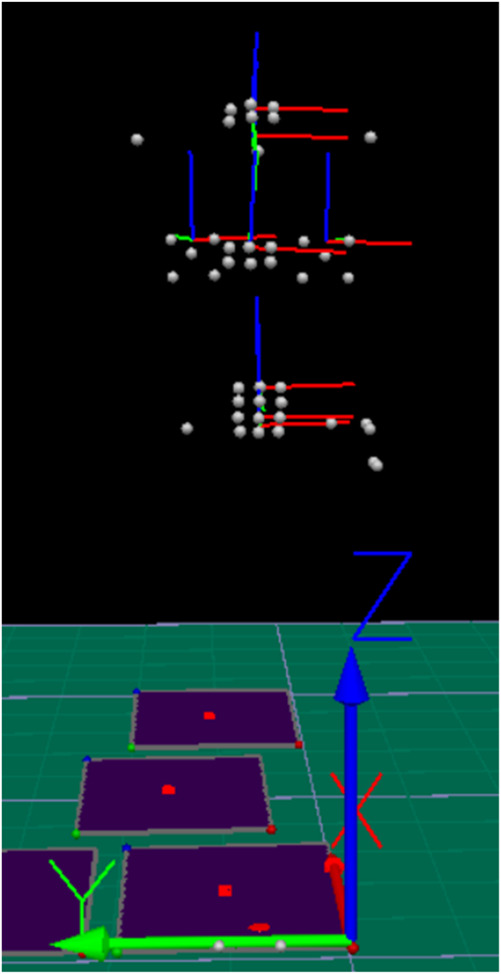
Axis conventions of each marker cluster.
Intersegmental spinal posture was calculated for standing and sitting postures.13 The position of each spinal marker segment relative to another was identified during five 2-s measurements throughout the duration of a 30-s standing and typing task.32 Five measurements were included to ensure stability of the data over time. Intersegmental spinal analysis focused on relative position between upper thoracic region relative to the lower thoracic region, upper lumbar region relative to the lower lumbar region, and lower lumbar region relative to the pelvis.
Changes in intersegmental spinal posture were calculated in 3 movement planes: flexion/extension (X), left/right side flexion (Y), and left/right rotation (Z).13 Spinal analysis using the torso as a single segment was also conducted by assessing the trunk’s position relative to the pelvis, as described in full elsewhere.13
Responses to the PROMs were processed in Microsoft Excel (Microsoft Corp). Body chart pain location analysis was reported as a prevalence (%) per region of interest (cervical, thoracic, and lumbosacral); the number of participants who experienced pain in this region. Change in NRS score in response to the interventions were calculated as percentage change and total point change; a Minimal Clinically Important Change (MCIC) of 15% was required for clinical relevance.30 For the SF-MPQ-2, 4 subscale scores (continuous, intermittent, affective, and neuropathic), and a total score was calculated as per the standardized scoring method.34
Responses to the NDI were coded from 0 to 5 and presented as a total score. With an MCIC of 5 points, for intervention effects to be considered clinically relevant, a minimum change of 5 points or 10% difference was required for clinical significance.35 Responses to the WHODAS 2.0 were quantified (from none, “1, to extreme, 5”) and presented as a total score.
Statistical analysis
Due to the number of outcomes included within this study, only significant findings are reported in this article. Kinematic data for both bra and intersegmental spinal data, which were parametric data, were analyzed using repeated measures analysis of variance. The bra-related data considered the effect of both side (left/right) and breast support condition (control, standard, standard28, alternative, and alternative28) while the spinal data considered the effect of condition only.
Changes in the prevalence of pain by location were analyzed using Friedman tests with post hoc Wilcoxon signed rank tests. Friedman tests with post hoc Wilcoxen signed rank tests were used to assess within (standard/standard28, alternative/alternative28) and between (control, standard28, alternative28) bra differences of the ordinal NRS data. Short-form McGill Pain Questionnaire 2, WHODAS, and NDI data were considered continuous; repeated measures analysis of variance tests with post hoc pairwise comparisons were conducted. Statistical significance was set at P < 0.05.
Results
Twenty-four participants were included in the study (Table 1). Eleven participants (46%) were professionally fitted with the same band size as the control bra, while 7 (28%) were given a larger band size in the standard bra and 6 (25%) were given a smaller size. For cup size, 3 (12%) participants had the same cup size in both bras, 15 (63%) had increased cup size in the standard bra, and 6 (25%) had reduced cup size. Analysis of the alternative bra sizes was not applicable due to its unique sizing approach.
Table 1.
Participant demographics and measurements—mean (SD) and range (n = 24).
| Measurement | Mean (SD) | Range |
| Age (y) | 31.5 (8.8) | 20–46 |
| Height (m) | 1.7 (0.06) | 1.58–1.83 |
| Weight (kg) | 85.6 (21.7) | 63.00–154.50 |
| Body mass index (kg/m2) | 30.80 (6.0) | 22.72–46.13 |
| Chest circumference (cm) | 107.0 (10.3) | 92.37–132.83 |
| Waist circumference (cm) | 90.6 (12.2) | 71.67–113.33 |
| Hip circumference (cm) | 112.8 (13.6) | 95.87–150.67 |
| Waist-hip ratio | 0.80 (0.07) | 0.68–0.98 |
| Control bra size (median) | ||
| Cup | FF | C—HH |
| Band | 34 | 32–40 |
| Standard bra size (median) | ||
| Cup | FF | DD—K |
| Band | 36 | 30–44 |
Bra fit assessment
All the control bras (n = 24) failed the bra fit assessment, and 21 (88%) of the standard bras and 1 (4%) of the alternative bras failed because of loose straps that could not be adjusted to achieve an acceptable fit. In the control bras, 73 bra fit issues were identified among 24 bras, with all but 1 bra presenting with multiple bra fit issues. The most common bra fit issues in the control bras were a tight band (58%), the front band not being in contact with the sternum (46%) and large cups (42%). In the standard bras, there were 42 bra fit issues among 24 bras, with 15 bras presenting with multiple bra fit issues. The most common bra fit issues in the standard bras were a tight band (54%), large cups (33%), and tight straps (42%).
Bra kinematics
NSN distance
Of the 24 participants recruited to the study, 21 (88%) permitted recording of bra kinematics (Table 2). While there was no significant effect of side in NSN distance (P = 0.297), there were significant interactions between breast support conditions; immediately, the standard bra significantly reduced NSN distance compared with the control bra by 0.7 cm (P = 0.014). The alternative bra significantly reduced NSN distance both immediately (1.2 cm, P = 0.000) and after 4 weeks wear (0.7 cm, P = 0.030) compared with the control bra.
Table 2.
Mean (SD) NSN distances and breast displacement (cm). ML, AP, and SI breast displacement.
| Control | Standard | Standard28 | Alternative | Alternative28 | ||
| NSN distance (cm) | Mean | 23.1 (2.1) | 22.4a (2.0) | 23.1b,c (2.1) | 21.9a (2.1) | 22.4a,c (2.5) |
| Breast displacement (cm) | ML | 1.6 (0.7) | 1.4 (0.6) | 1.5 (0.8) | 1.5 (0.5) | 1.4 (0.6) |
| AP | 1.4 (0.8) | 1.7 (0.8) | 1.5 (0.7) | 1.4 (0.6) | 1.5 (1.0) | |
| SI | 5.0 (2.0) | 5.5a,c (1.8) | 6.0a (2.4) | 4.9c (2.2) | 5.2 (2.7) |
Abbreviations: AP, anterior-posterior; ML, mediolateral; NSN, nipple-sternal-notch; SI, superior-inferior.
Indicates significance compared with control (control vs. standard, control vs. standard28, control vs. alternative, or control vs. alternative28).
Indicates significance within bras (standard vs. standard28, alternative vs. alternative28).
Indicates significance between intervention bras (standard vs. alternative, standard28 vs. alternative28).
Bra displacement
There was no significant effect of side in mediolateral, anterior-posterior, and superior-inferior bra displacement (P > 0.05). There were significant interactions between breast support conditions, but only in the superior-inferior direction; the control bra significantly reduced breast movement compared with the standard bra (0.5 cm, P = 0.030) and standard28 (1.0 cm, P = 0.008). The alternative bra also immediately significantly reduced superior-inferior displacement compared with the standard bra (0.6 cm, P = 0.009).
Standing posture
At the lumbo-pelvic region, posture was significantly affected only in the frontal plane (Table 3); participants presented with a more left laterally flexed position in the standard28 condition compared with the control bra (0.2 degree difference, P = 0.015). The alternative28 placed participants in a right laterally flexed position, significantly different to the effects of the standard28 (2.4 degree difference, P = 0.011). When considering the position of the trunk relative to the pelvis, the standard bra significantly reduced trunk flexion when first put on, compared with both the control bra (5.1 degree difference, P = 0.005) and alternative bra (4.1 degree difference, P = 0.036).
Table 3.
Mean standard deviation change in intersegmental spinal posture in standing, comparing between breast support conditions.
| Comparison | Flexion-extension | Side flexion | Rotation | |
| Upper thoracic relative to lower thoracic | Standard vs. control | +0.8 ° (38.5) | −0.9 ° (5.6) | +0.8 ° (3.8) |
| Standard28 vs. control | −0.6 ° (12.8) | +0.3 ° (6.9) | +0.2 ° (3.2) | |
| Standard28 vs. standard | −1.5 ° (11.4) | +1.2 ° (6.90) | −0.6 ° (3.3) | |
| Alternative vs. control | +2.1 ° (12.6) | +0.7 ° (4.9) | −0.2 ° (2.6) | |
| Alternative28 vs. control | −1.9 ° (14.2) | −0.5 ° (4.9) | +0.7 ° (4.6) | |
| Alternative28 vs. alternative | −4.0 (12.3) | −1.2 ° (4.1) | +0.9 ° (3.3) | |
| Standard vs. alternative | +1.3 ° (13.0) | +1.6 ° (6.5) | −1.0 ° (3.5) | |
| Standard28 vs. alternative28 | −1.2 ° (10.4) | −0.8 ° (4.6) | +0.5 ° (2.9) | |
| Upper lumbar relative to lower lumbar | Standard vs. control | −1.3 ° (13.8) | +1.3 ° (6.1) | +0.3 ° (1.6) |
| Standard28 vs. control | −3.0 ° (18.3) | −0.1 ° (5.2) | −7.1 ° (3.3) | |
| Standard28 vs. standard | −1.7 ° (22.3) | −1.4 ° (5.9) | −1.4 ° (2.8) | |
| Alternative vs. control | +0.2 ° (16.6) | +0.9 ° (5.3) | +0.7 ° (1.9) | |
| Alternative28 vs. control | −4.9 ° (18.9) | +1.1 ° (6.7) | +0.3 ° (3.2) | |
| Alternative28 vs. alternative | −5.0 (20.9) | +0.2 ° (6.1) | −0.4 ° (2.3) | |
| Standard vs. alternative | +1.5 ° (24.1) | −0.4 ° (7.7) | +0.4 ° (1.9) | |
| Standard28 vs. alternative28 | −1.9 ° (15.5) | +1.2 ° (5.3) | +7.3 ° (2.5) | |
| Lower lumbar relative to the pelvis | Standard vs. control | +1.1 ° (7.1) | +2.0 ° (4.0) | 0.0 ° (2.5) |
| Standard28 vs. control | +5.4 ° (7.7) | −0.2 ° (4.1)a | −7.2 ° (3.2) | |
| Standard28 vs. standard | +4.3 ° (9.8) | −2.2 ° (4.5)b | −7.2 ° (4.1)a | |
| Alternative vs. control | +1.0 ° (9.4) | +0.9 ° (4.0) | +1.0 ° (4.2) | |
| Alternative28 vs. control | −1.8 ° (8.3) | +2.2 ° (5.2) | +0.1 ° (3.2) | |
| Alternative28 vs. alternative | −2.7 ° (9.5) | +1.3 ° (5.1) | −0.9 (4.6) | |
| Standard vs. alternative | −0.2 ° (11.0) | −1.1 ° (4.8) | +1.0 (4.4) | |
| Standard28 vs. alternative28 | −7.2 ° (8.4) | +2.4 ° (4.2)c | +7.3 ° (4.3) | |
| Trunk relative to the pelvis | Standard vs. control | +5.1 ° (8.1)a | −0.9 ° (3.0) | −0.1 ° (3.2) |
| Standard28 vs. control | +2.1 ° (9.1) | −0.2 ° (3.9) | −0.6 ° (3.4) | |
| Standard28 vs. standard | −3.0 ° (6.9) | +0.7 ° (3.4) | −0.5 ° (4.0) | |
| Alternative vs. control | +1.0 ° (8.3) | +0.5 ° (4.4) | +0.5 ° (4.1) | |
| Alternative28 vs. control | +3.8 ° (11.5) | −0.5 ° (3.9) | −0.2 ° (4.0) | |
| Alternative28 vs. alternative | +2.8 ° (8.1) | −1.0 ° (3.8) | +0.7 ° (3.6) | |
| Standard vs. alternative | −4.1 ° (8.9)c | +1.4 ° (3.7) | +0.6 ° (3.8) | |
| Standard28 vs. alternative28 | +1.7 ° (7.1) | −0.3 ° (2.9) | +0.4 ° (3.8) |
Flexion-extension: + indicates movement towards extension, −indicates movement into flexion.
Side flexion/rotation: + indicates movement to left, − indicates movement to right.
Indicates significance compared with control (control vs. standard, control vs. standard28, control vs. alternative28).
Indicates significance within bras (standard vs. standard28, alternative vs. alternative28).
Indicates significance between intervention bras (standard vs. alternative, standard28 vs. alternative28).
PROMs
Body chart pain location analysis
The body chart pain location analysis revealed that in the control bra, 6 (25%) participants reported pain in the cervical region (Figure 4). Before wearing the standard bra, 2 (8%) participants reported cervical region pain; this increased significantly (P = 0.046) to 6 (25%) participants post-intervention (standard28). Pain among participants was most prevalent at the thoracic region; in the control bra, 22 (92%) participants reported pain. Before the standard bra intervention, 19 participants had thoracic region pain, compared with 22 postintervention (16% increase). The alternative bra significantly reduced prevalence of pain by 36% (P = 0.011) compared with the control bra. The alternative bra also significantly reduced prevalence of pain at the lumbar region by 37% (P = 0.035) compared with the control bra.
Figure 4.
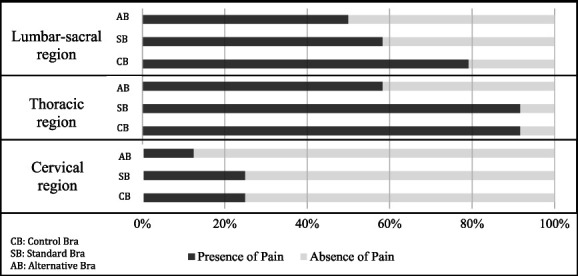
The prevalence of pain per anatomical region. AB, alternative bra; CB, control bra; SB, standard bra.
NRS
For back pain NRS, there was no statistically significant change throughout (P = 0.056; Figure 5). However, with an MCIC of 15%,30 a pain reduction of 23% between the control bra and the alternative28 indicates a clinically important improvement. For back stiffness, the effects of the breast support conditions were significantly different (P = 0.027). The alternative bra intervention significantly reduced back stiffness by 34% (P = 0.010). The alternative bra also significantly reduced back stiffness compared with both the control (P = 0.003, 42%) and the standard28 (P = 0.017) garments. Changing breast support garment had no statistically significant effect on back discomfort NRS scores (P = 0.068), although there were clinically important reductions when comparing the standard28 and alternative28 with the control bra with reductions of 23% and 22%, respectively.
Figure 5.
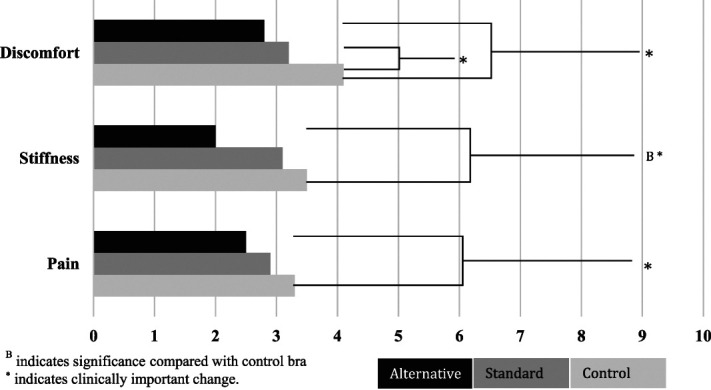
Mean NRS scores for back pain, stiffness, and discomfort. BIndicates significance compared with CB. *Indicates clinically important change. CB, control bra; NRS, numerical rating scale.
SF-MPQ-2
There were significant differences in pain in the continuous (P = 0.007) and intermittent (P = 0.018) subscales and total pain scores (P = 0.004) because of changing breast support garment (Figure 6). In the continuous pain subscale, the alternative bra significantly reduced pain by 44% compared with the control bra (P = 0.000). The intermittent pain subscale reported that both the standard bra and the alternative bra significantly reduced pain compared with the control bra (P < 0.018). Total pain scores significantly reduced following the alternative intervention compared with those observed using the control bra (P = 0.012).
Figure 6.
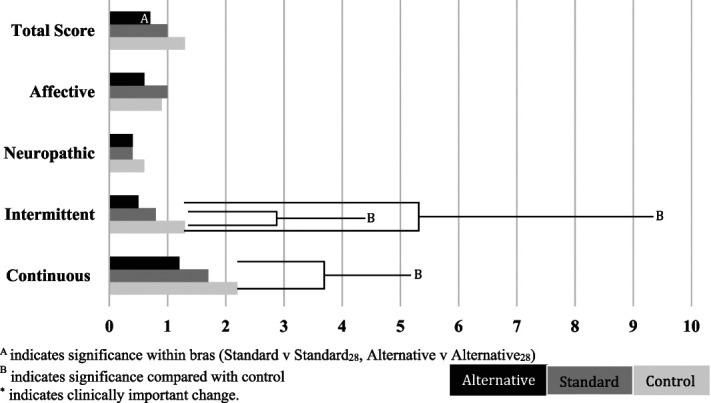
Mean subscale and total score for SF-MPQ-2. AIndicates significance within bras (standard vs. standard28, alternative vs. alternative28). BIndicates significance compared with control. *Indicates clinically important change. SF-MPQ-2, short-form McGill Pain Questionnaire 2.
NDI
Changing breast support garment had a significant effect on participants' perceived level of disability (P = 0.001). The standard bra reduced NDI score by 14% compared with the control bra, a magnitude large enough to be of clinical significance.35 The alternative bra significantly reduced NDI score (P = 0.000) by 35% compared with the control bra; a change of significantly greater magnitude than the standard (P = 0.000).
Discussion
While current strategies for conservatively managing NSBP among larger breasted women advocate the implementation of a correctly fitted bra, previous research consistently highlights how problematic this is (Figure 7).4,5,13,37 The findings from this study suggest that although the use of professional bra-fitting services goes some way to improving bra fit quality, the incidence of ill-fitting bras remains high, and alternative garment designs and fitting approaches may afford more women to achieve correct bra fit. This study also supports previous notions that addressing poor bra fit may improve painful symptoms, which until now had not been explored.4 While research investigating the impact of nonsurgical interventions among individuals with back pain is not lacking,31 this is the first conservative intervention study to measure symptomatic change among larger breasted women.
Figure 7.
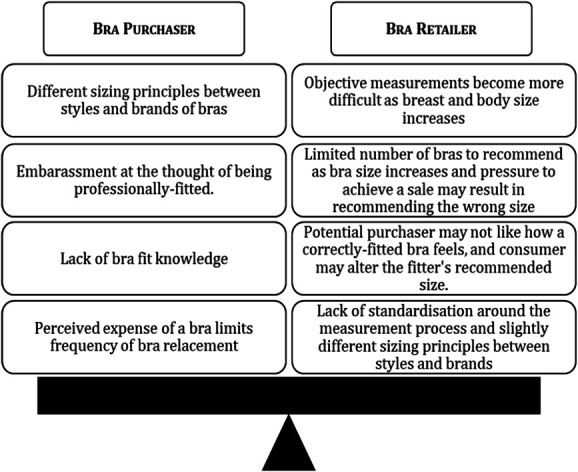
An overview of the challenges faced by the bra purchaser and retailer (professional-fitting service) when trying to achieve correct bra fit among larger breasted women.
Baseline pain measures suggest that the intensity of pain, stiffness, and discomfort was of a mild severity38 with respective mean NRS scores of 3.3, 3.5, and 4.1 of 10. The subscale pain descriptor and total pain scores from the SF-MPQ-2 ranged from 0.6 to 2.2 of 10, with continuous pain reporting the most severe rating. These 2 clinical measures alone provide a clear picture of participants’ pain characteristics; mostly, symptoms are mildly discomforting and of a continuous nature. At the start of the study, when participants presented in their control bra, 25% of participants reported pain at the cervical region, 92% at the thoracic region, and 79% at the lumbar region. Potential causal mechanisms of back pain among larger breasted women with ill-fitting bras suggest that pain is most likely to be experienced at the cervical and thoracic regions.4,7,39 Given that lifetime prevalence of low back pain is 60%–70%40 a high prevalence among participants was not surprising. Though the severity of pain at baseline was mild, significant symptomatic improvement was observed in line with bra fit improvement. The extent of symptomatic relief seems to be related to the quality of bra fit; the standard bra improved bra fit quality compared with participants’ control bras, and some painful symptoms significantly reduced. The alternative bra further improved bra fit compared with the standard bra and in turn symptomatic improvement was of a greater magnitude.
While the standard bra demonstrated clinically meaningful reductions in back discomfort (23%), the alternative bra resulted in clinically meaningful reductions in back discomfort (33%), pain (23%), and stiffness (42%). Similar patterns were seen in the results of the SF-MPQ-2; the standard bra significantly reduced intermittent pain after 4 weeks, while the alternative bra significantly reduced intermittent, continuous, and total pain scores. The findings from these 2 clinical measures suggest that although the use of a professional bra-fitting service (standard bra) does result in symptomatic improvement, the alternative bra intervention demonstrated a superior ability improve more symptoms and to a greater extent.
To compare these findings with surgical approaches, significant reductions in neck and upper back pain NRS scores have previously been reported 6 months after breast reduction surgery,41 and significant reductions (58%–77%) in the prevalence of pain at different anatomical locations have also been observed 9 months postoperatively.42 These findings, however, reflect a more longitudinal review of symptomatic improvement, while this study measures symptomatic change in the short-term. Although a nonsurgical approach may not be suitable for all larger breasted women with back pain, considering alternative breast support garments as a nonsurgical approach initially may be appropriate during the decision-making process for determining the need for surgical intervention. Implementation of a correctly fitted bra may provide an effective and accessible alternative for those women who do not wish to have surgery, who do not fit NHS eligibility criteria, or who cannot afford private health care.
Analysis of pain by location revealed that the alternative bra significantly reduced the number of people reporting pain at the thoracic region by 36% compared with the control bra, while the standard bra had no effect on the prevalence of pain at the thoracic region. The main design difference of the alternative bra is the positioning of the underband posteriorly. In a traditional bra, the underband’s function is to extend horizontally around the torso to keep the bra in place and support the weight of the breasts from underneath to reduce the strain through the straps.6 Within the design of the alternative bra, the underband is positioned much lower posteriorly, underneath the 12th rib at the lumbar region. In the alternative bra, significant reductions in the prevalence of pain at the thoracic region were observed, without leading to an increase in prevalence of pain at the lumbar region; by contrast, a reduction of 33% was observed. Reductions in thoracic pain prevalence in the alternative bra may be associated with changing the design of the underband, and therefore, the underband no longer extends horizontally around the body to support the weight of the breasts from underneath, and as such, the strain on the thoracic region is reduced.
Potential reasoning for significant symptomatic improvement in the alternative bra relate to changing the resting position of the breast tissue on the anterior chest wall (NSN distance) resulting in changes in muscle length and resting tension. When the body is exposed to sustained passive postural positioning, a strain (unsupported or poorly supported breast weight in this case) combines with gravity to create a sustained, direction-specific loading mechanism.43 Over time, this strain-loading mechanism may result in muscular imbalances; abnormal overpull anteriorly and underpull posteriorly, eventually leading to stretch weakness and pain in the posterior aspect of the torso,43 specifically the scapular elevators and protractors.7 Stretch weakness can be rehabilitated through relieving resting tension, shortening muscle length, and restoring optimal resting length and tension. This study identified that the alternative bra positioned the breasts higher on the anterior chest wall both initially and after an intervention period compared with the remaining conditions, as evidenced by the NSN distance findings. If the breast is positioned higher on the anterior chest wall through improved external breast support, the sustained direction-specific loading mechanism may be reduced through minimizing the strain acting on the body. Given that the additional support offered by the alternative bra was sustained over 4 weeks, the effects of the strain-loading mechanism was reduced because at least some of the breast weight was absorbed by a correctly fitting bra.
The statistically significant changes observed in NSN distance measures were of very small magnitude (0.7–1.2 cm), in combination with significant symptomatic relief, suggesting that only a small degree of change may be required to provide clinically meaningful symptomatic change. Although this requires further work, the potential for these findings to be translated into clinical practice during the implementation of conservative measures such as implementing correctly fitting breast support garments among larger breasted women with NSBP is possible due to the use of a clinical measure as an objective measure of external breast support.
Conclusions
Through a combination of improving bra fit quality and altering the resting position of the breast tissue on the anterior chest wall at rest, the results from this study demonstrate that implementation of an alternative bra can significantly relieve symptoms of NSBP among larger breasted women, more effectively than current standard solutions. As such, alternative approaches to achieving correct bra fit could be considered in the future. This study provides evidence that if a correctly fitted bra can be implemented, symptomatic relief can in fact be obtained conservatively, and looking ahead, this may be a positive foundation on which to build future research to improve patient care and the management of larger breasted women with NSBP.
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research study was funded through internal institution funding (University of Central Lancashire), including the Undergraduate Research Internship Program, UNITE with Business, and a University Investment voucher.
Declaration of conflicting interest
The authors disclosed the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: The alternative bras used within this study were provided, in kind by the bra manufacturer (Optifit, Saddleworth, United Kingdom).
Supplemental material
No supplemental digital content is available in this article.
Footnotes
Associate Editor: Cleveland Barnett
Contributor Information
Karen May, Email: KAMay@uclan.ac.uk.
Jessie Janssen, Email: jessie.janssen@fh-krems.ac.at.
James Selfe, Email: j.selfe@mmu.ac.uk.
Ambreen Chohan, Email: AChohan@uclan.ac.uk.
References
- 1.McGhee D, Coltman KA, Riddiford-Harland D, et al. Upper torso pain and musculoskeletal structure and function in women with and without large breasts: a cross sectional study. Clin Biomech 2018;51:99–104. [DOI] [PubMed] [Google Scholar]
- 2.Zieliński G, Filipiak Z, Suwała M, et al. Bust size and pain of the musculoskeletal system – a literature review. Medycyna Ogólna i Nauki o Zdrowiu 2019;25:44–47. [Google Scholar]
- 3.NHS England, NHS Clinical Commissioners, the Academy of Medical Royal Colleges. NHS Improvement, the National Institute for Health and Care Excellence. Evidence-Based Interventions: Guidance for CCGs; 2019. Available at: https://www.england.nhs.uk/wp-content/uploads/2018/11/ebi-statutory-guidance-v2.pdf. Accessed August 4, 2016. [Google Scholar]
- 4.Greenbaum A, Heslop T, Morris J, et al. An investigation of the suitability of bra fit in women referred for reduction mammaplasty. Br J Plast Surg 2003;56:230–236. [DOI] [PubMed] [Google Scholar]
- 5.McGhee D and Steele J. Optimising breast support in female patients through correct bra fit. A cross-sectional study. J Sci Med Sport 2010;13:568–572. [DOI] [PubMed] [Google Scholar]
- 6.Coltman C Steele J and McGhee D. Which bra components contribute to incorrect bra fit in women across a range of breast sizes? Cloth Text Res J 2018;36:78–90. [Google Scholar]
- 7.Spencer L and Briffa K. Breast size, thoracic kyphosis and thoracic spine pain - association and relevance of bra fitting in post-menopausal women: a correlational study. Chiropr Man Ther 2013;21:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Spencer L, McKenna L, Fary R, et al. Upper back pain in postmenopausal women and associated physical characteristics. PLoS One 2019;14:e0220452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chohan A, Ramli K, Cook A, et al. Spinal alignment” cushion in the management of low back pain–a randomized controlled study. PRM+ 2019;2:35–40. [Google Scholar]
- 10.Alexander J, Selfe J, Richards J, et al. Determining effectiveness of passive gravity assisted traction (PGAT) device in management of low back pain. J Quant Res Rehabil Med 2019;2:11–15. [Google Scholar]
- 11.Greenhalgh S and Selfe J. Red Flags II: A Guide to Solving Serious Pathology of the Spine. London, UK: Elsevier Sciences; 2010. [Google Scholar]
- 12.Wood K Cameron M and Fitzgerald K. Breast size, bra fit and thoracic pain in young women: a correlational study. Chiropr Osteopat 2008;16:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Haworth L, May K, Janssen J, et al. The impact of breast support garments on fit, support and posture of larger breasted women. Appl Ergon 2022;101:103701. [DOI] [PubMed] [Google Scholar]
- 14.Sibbald B and Roland M. Understanding controlled trials: why are randomised controlled trials important? BMJ 1998;316:201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Garcia A, Costa L, da Silva T, et al. Effectiveness of back school versus McKenzie exercises in patients with chronic nonspecific low back pain: a randomized controlled trial. Phys Ther 2013;93:729–747. [DOI] [PubMed] [Google Scholar]
- 16.Hwang-Bo G Lee JH and Kim HD. Efficacy of kinesiology taping for recovery of dominant upper back pain in female sedentary worker having a rounded shoulder posture. Technol Health Care 2013;21:607–612. [DOI] [PubMed] [Google Scholar]
- 17.Kim MK Lee JC and Yoo KT. The effects of shoulder stabilization exercises and pectoralis minor stretching on balance and maximal shoulder muscle strength of healthy young adults with round shoulder posture. J Phys Ther Sci 2018;30:373–380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McDonald S. Benefits Healthy Body, Happy Woman. Optifit Bra Company Ltd; 2014. Available at: https://www.optifitbra.com/benefits/. Accessed August 20, 2020. [Google Scholar]
- 19.McGhee D and Steele J. Biomechanics of breast support for active women. Exerc Sport Sci Rev 2020;48:99–109. [DOI] [PubMed] [Google Scholar]
- 20.Chohan A, Payne K, Selfe J, et al. Biomechanical testing of a spinal lignment cushion (“ROPHI™” cushion) in adults with lower back pain. Bone Joint J 2013;95B. [Google Scholar]
- 21.Haake S and Scurr J. A method to estimate strain in the breast during exercise. Sports Eng 2011;14:49–56. [Google Scholar]
- 22.McGhee D, Steele J, Zealey W, et al. Bra-breast forces generated in women with large breasts while standing and during treadmill running: implications for sports bra design. Appl Ergon 2013;44:112–118. [DOI] [PubMed] [Google Scholar]
- 23.Risius D, Milligan A, Mills C, et al. Multiplanar breast kinematics during different exercise modalities. Eur J Sport Sci 2014;15:111–117. [DOI] [PubMed] [Google Scholar]
- 24.Milligan A and Scurr J. Measurement of Breast Motion Across the Breast Surface Leads To Better Recommendations for Breast Support. In: International Conference of Biomechanics in Sport 2015; 2015:672–675. [Google Scholar]
- 25.White J and Scurr J. Evaluation of professional bra fitting criteria for bra selection and fitting in the UK. Ergonomics 2012;55:704–711. [DOI] [PubMed] [Google Scholar]
- 26.Lacey R, Lewis M, Jordan K, et al. Interrater reliability of scoring of pain drawings in a self-report health survey. Spine 2005;30:E455–E458. [DOI] [PubMed] [Google Scholar]
- 27.Lacey R Lewis M and Sim J. Presentation of pain drawings in questionnaire surveys: influence on prevalence of neck and upper limb pain in the community. Pain 2003;105:293–301. [DOI] [PubMed] [Google Scholar]
- 28.Schierhout J, Myers G, Schierhout GH, et al. Is self-reported pain an appropriate outcome measure in ergonomic-epidemiologic studies of work-related musculoskeletal disorders? Am J Ind Med 1996;30:93. [DOI] [PubMed] [Google Scholar]
- 29.Coltman C Steele J and McGhee D. Can breast characteristics predict upper torso musculoskeletal pain? Clin Biomech 2018;53:46–53. [DOI] [PubMed] [Google Scholar]
- 30.Salaffi F, Stancati A, Silvestri C, et al. Minimal clinically important changes in chronic musculoskeletal pain intensity measured on a numerical rating scale. Eur J Pain 2004;8:283–291. [DOI] [PubMed] [Google Scholar]
- 31.Artus M, van der Windt D, Jordan K, et al. Low back pain symptoms show a similar pattern of improvement following a wide range of primary care treatments: a systematic review of randomized clinical trials. Rheumatology (Oxford) 2010;49:2346–2356. [DOI] [PubMed] [Google Scholar]
- 32.Kuo YL, Wang PS, Ko PY, et al. Immediate effects of real-time postural biofeedback on spinal posture, muscle activity, and perceived pain severity in adults with neck pain. Gait Posture 2019;67:187–193. [DOI] [PubMed] [Google Scholar]
- 33.Dworkin R, Turk D, Trudeau J, et al. Validation of the short-form McGill pain questionnaire-2 (SF-MPQ-2) in acute low back pain. J Pain 2015;16:357–366. [DOI] [PubMed] [Google Scholar]
- 34.Trudeau J, Turk D, Dworkin R, et al. Validation of the revised short form McGill Pain Questionnaire (SF-MPQ-2) for self-report of pain qualities in patients with acute low back pain. J Pain 2012;13:S4. [DOI] [PubMed] [Google Scholar]
- 35.MacDermid J, Walton D, Avery S, et al. Measurement properties of the neck disability index: a systematic review. J Orthop Sports Phys Ther 2009;39:400–417. [DOI] [PubMed] [Google Scholar]
- 36.Andrews G, Kemp A, Sunderland M, Von Korff M, Ustun T. Normative data for the 12 item WHO Disability Assessment Schedule 2.0. PLoS One 2009;4:8343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.McGhee D, Steele J, Pechter E, et al. How do respiratory state and measurement method affect bra size calculations? Br J Sports Med 2006;40:970–974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Boonstra A, Stewart R, Köke A, et al. Cut-off points for mild, moderate, and severe pain on the numeric rating scale for pain in patients with chronic musculoskeletal pain: variability and influence of sex and catastrophizing. Front Psychol 2016;7:1466–1469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.McGhee D and Steele J. Breast biomechanics: what do we really know? Physiology 2020;35:144–156. [DOI] [PubMed] [Google Scholar]
- 40.World Health Organization. 6.24 Low Back Pain; 2014. Available at: https://www.who.int/medicines/areas/priority_medicines/Ch6_24LBP.pdf?ua=1. Accessed January 3, 2021. [Google Scholar]
- 41.Spector JA and Karp NS. Reduction mammaplasty: a significant improvement at any size. Plast Reconstr Surg 2007;120:845–850. [DOI] [PubMed] [Google Scholar]
- 42.Gonzalez F, Walton R, Shafer B, et al. Reduction mammaplasty improves symptoms of macromastia. Plast Reconstr Surg 1993;91:1270–1276. [DOI] [PubMed] [Google Scholar]
- 43.Comerford M and Mottram S. Kinetic Control E-Book: The Management of Uncontrolled Movement. London, UK: Elsevier Health Sciences; 2019. [Google Scholar]