Abstract
Objectives
This study aimed to explore how the unprecedented stressors associated with the COVID-19 pandemic may have contributed to heightened levels of depression and anxiety among pregnant Indigenous persons, and identify protective individual-level factors.
Design
The current study used a mixed-methods design including standardised questionnaires and open-ended response questions. Using hierarchical regression models, we examined the extent to which COVID-19-related factors of service disruption (ie, changes to prenatal care, changes to birth plans and social support) were associated with mental well-being. Further, through qualitative analyses of open-ended questions, we examined the coping strategies used by pregnant Indigenous persons in response to the pandemic.
Setting
Participants responded to an online questionnaire consisting of standardised measures from 2020 to 2021.
Participants
The study included 336 self-identifying Indigenous pregnant persons in Canada.
Results
Descriptive results revealed elevated rates of clinically relevant depression (52.7%) and anxiety (62.5%) symptoms among this population. 76.8% of participants reported prenatal care service disruptions, including appointment cancellations. Thematic analyses identified coping themes of staying informed, social and/or cultural connections and activities, and internal mental well-being strategies. Disruptions to services and decreased quality of prenatal care negatively impacted mental well-being of Indigenous pregnant persons during the COVID-19 pandemic.
Conclusions
Given the potential for mental well-being challenges to persist and long-term effects of perinatal distress, it is important to examine the quality of care that pregnant individuals receive. Service providers should advance policies and practices that promote relationship quality and health system engagement as key factors linked to well-being during the perinatal period for Indigenous persons.
Keywords: COVID-19, OBSTETRICS, Social Support, MENTAL HEALTH
STRENGTHS AND LIMITATIONS OF THIS STUDY.
This study includes important implications for the perinatal healthcare access and service provisions for Indigenous persons in Canada.
The findings from this study discuss the resiliency and coping strategies used by Indigenous persons in Canada to counter barriers in the healthcare system during the height of the COVID-19 pandemic.
The participant sample largely consists of participants with a higher than Canadian average median income, which may limit the transferability of findings to the larger population.
This study lacked the incorporation of traditional birthing and healing practices when assessing healthcare service usage for Indigenous pregnant persons.
Supportive and ongoing prenatal care is vital to optimise pregnancy outcomes,1–3 with regular and secure access to high-quality prenatal care supporting the mental and physical health of the pregnant person, thereby increasing the likelihood of birthing a healthy child.4 5 By providing education, counselling and emotional support, prenatal care can help pregnant people maintain their overall well-being and promote positive outcomes.5 Establishing a long-term relationship with care providers also ensures consistent and coordinated care, builds trust and improves communication, allows for more personalised care and promotes positive health outcomes for the birthing parent and baby.6 7
The COVID-19 pandemic brought widespread health restrictions, limiting people’s access to healthcare practitioners and services, including prenatal care.8 9 Pandemic-related stressors, including service restrictions, have been associated with an increase in emotional distress in individuals experiencing pregnancies.10 Due to the historical and ongoing impacts of colonialism, Indigenous peoples of Canada already experience tremendous health inequities, including restricted access to healthcare.11 12 Access to pregnancy-specific healthcare services is also impacted by issues such as cultural misalignment, distance to services, cost, lack of transport and lack of awareness of available services.13 14 Additionally concerning are the ways in which distrust of systems of support and systemic racism can impede access to care. In Canada, a deficit-based discourse around Indigenous health has contributed to stigmatisation, discrimination and marginalisation of Indigenous peoples.15 16 Consequently, this leads to a lack of trust in the healthcare system, making pregnant Indigenous persons less likely to seek care.17
As a result of the COVID-19 pandemic, prenatal care was restricted across Canada, with some individuals experiencing limited or complete loss of access to their primary healthcare providers, obstetricians, and/or midwives, and limited social support during their pregnancies.2 18 A lack of a culturally aligned pandemic response created additional barriers for pregnancy Indigenous persons.19 Smylie et al 20 found that even prepandemic, Indigenous peoples had to travel away from their home communities more often for prenatal care, particularly birthing, highlighting disparities in care accessibility. Coupled with a lack of social support and ongoing systemic racism, this resulted in increased stress levels for pregnant Indigenous persons.20
Mental Well-being in the prenatal period
Pregnancy is a time of major change for individuals, both physically and psychologically, and is often associated with increased feelings of stress.21 22 Substantial research has demonstrated heightened levels of prenatal depression and anxiety experienced during the COVID-19 pandemic compared with prepandemic.23–27 Pregnant individuals with specific sociodemographic factors, such as decreased income and lower education levels, are more vulnerable to adverse mental well-being symptoms during pregnancy.28–30 Canadian Indigenous populations are at a particular disadvantage in this regard31 due to the economic disadvantages they experience as a result of continuing legacies of colonialism.11 Across Canada, approximately one-in-five Indigenous persons live in poverty and one-in-six Indigenous persons experience difficulties with their current form of housing.32 In addition to these economic disparities, Indigenous persons are also between one-and-a-half to five times as likely to experience trauma-inducing experiences such as childhood abuse and intimate partner violence.33 Maintaining positive mental well-being and low stress levels can have positive health outcomes for both the pregnant individual and their developing baby.22 This can prove difficult for Indigenous communities who already face barriers in accessing proper prenatal care and mental well-being support.26 34
Service disruptions
Adequate and accessible service provisions are vital to the health and well-being of pregnant persons. Groulx et al 2 noted that service disruptions increased mental well-being concerns among Canadian pregnant individuals. While social distancing and virtual doctor appointments have been the primary alternative for health services in Canada,35 36 this requires individuals to have adequate housing, reliable internet access and access to electronic devices, most of which are not easily accessible to a large portion of the population. This is particularly the case in many Indigenous communities37 which face significantly more barriers in technology access and in accessing medical care, specifically prenatal care, than non-Indigenous populations,26 38 including forced travel from home communities to larger cities to give birth. This further restricts social support availability and access to adequate healthcare.26 Long-distance travel for birthing has increased during the COVID-19 pandemic as obstetrical and health services were closed.26 Indigenous persons who are pregnant face poorer birth outcomes, including higher rates of low birth weight, preterm birth and stillbirth,38 39 related to the racial disparities in access to and quality of prenatal care.40
Social support
The WHO (2015) reports that community support and engagement is largely impactful to positive outcomes among pregnant people. Social support, specifically partner support, has been cited as a resiliency factor for pregnant individuals, particularly those with high-risk pregnancies.26 41 42 Social support during the prenatal period can mitigate adverse mental well-being outcomes for pregnant individuals, and subsequently, developmental outcomes for their babies, such as low birth weight.22 36 41 However, due to the COVID-19 pandemic, support persons were frequently not allowed to join doctor appointments or had limited involvement in the birthing process, adding to the stress levels of pregnant individuals.2 26
Coping strategies
Commonly used coping strategies for pregnant people during the pandemic include avoidance, connection with spirituality and preparation.43–45 For Indigenous persons specifically, perinatal stress can be experienced at a greater intensity than in other demographics.46 47 However, reported coping strategies in the literature generally focus on substance use as a coping method, in the context of pregnant Indigenous persons.48–51
Current study
There is limited knowledge on the impacts of prenatal service disruption due to the COVID-19 pandemic on pregnant Indigenous persons, and how changes to birth plans and support levels have impacted the mental well-being of these individuals. The objectives of this study were to (1) examine mental well-being (ie, anxiety and depression symptoms) among a sample of pregnant Indigenous persons during the COVID-19 pandemic, (2) to examine the associations of pandemic-related service disruptions (ie, changes to prenatal care, changes to birth plans) and social support with mental well-being and (3) to generate knowledge on Indigenous pregnant peoples self-described coping strategies, as they relate to the mental well-being of this population. This mixed-methods study aims to further develop an understanding of both adaptive and maladaptive coping strategies used among Indigenous pregnant persons throughout the pandemic. Obtaining this information may be done most appropriately using a qualitative approach based on literature suggesting that these methods are most ethically aligned with culturally safe research practices.52
Methods
Participants
The current study reports data collected from the Pregnancy During the COVID-19 Pandemic study,2 an ongoing longitudinal study examining the health impacts of the COVID-19 pandemic on pregnant individuals and their children. Participants were recruited from April 2020 to 2021 through online recruitment methods, including social media posts and ads on Facebook, Instagram and Twitter. Participants were invited to join the study if they met the inclusion criteria of: residing in Canada, having the ability to read and write in English and/or French and having a confirmed pregnancy <35 weeks gestation.35 Participant consent was collected through Research Electronic Data Capture where participants signed the electronic consent to answer questionnaires and open-ended response questions.
For the purpose of this study, data include only participants who self-identified as Indigenous (First Nations, Métis, Inuit) or mixed Indigenous descent. Out of the larger sample (N=10 669), 336 individuals self-identified as Indigenous; 45.2% self-identified as Métis, 42.6% self-identified as First Nations, 11.3% self-identified as mixed Indigenous ancestry and 0.9% self-identified as Inuit. Participants were located in Quebec (25.3%), Ontario (18.8%), Alberta (18.2%), British Columbia (13.7%), Manitoba (11.0%), Saskatchewan (6.8%), Nova Scotia (3.3%), Northwest Territories (1.2%), Yukon (1.2%), and Newfoundland and Labrador (0.6%). On average, participants were 30.33±5.0 years. Most participants were married or living with a common law partner (86.9%), had completed community college, an equivalent trade or vocational degree, or greater (77.7%) and had an annual household income greater than $C70 000 (57.8%).
Patient and public involvement
The public was not involved in the design, reporting and dissemination of our study.
Measures
Depression
To measure symptoms of depression, the Edinburgh Postnatal Depression Scale (EPDS) was used.53 The EPDS is a 10-item self-report scale, with scores ranging from 0 to 30, and is commonly used to assess depression levels among pregnant and postnatal individuals.53 Higher self-report scores indicate increased depressive symptoms, and a cut-off of ≥13 is used to indicate clinically elevated symptoms of depression.53
Anxiety
To measure symptoms of anxiety, the Patient-Reported Outcomes Measurement Information System (PROMIS) Anxiety Adult 7-item short form was used. This self-report measure has possible t-scores ranging from 36.7 to 82.7, with higher scores indicating greater levels of anxiety. A cut-off of 60 is used to indicate clinically elevated symptoms of anxiety.54
Prenatal care and birth plans
Participants were asked questions about experiencing changes in prenatal care, prenatal appointment cancellations, changes to birth plans (eg, changes to birth location, inclusion of support persons, childcare arrangements or other). Home births were not differentiated within changes to birth plans. The ability to bring a partner or support person to appointments was also considered. Participants were also asked to indicate which health services were difficult to access due to the pandemic (eg, massage, chiropractic, physiotherapy, acupuncture, psychological counselling or other). Finally, participants were asked if they felt that the quality of care had decreased and if they were concerned about self and baby not receiving necessary care. Responses on these last two items were measured on a scale from 0 to 100, with anchors being 0=not at all, 50=somewhat and 100=very much so.
Social support
To assess perceived social support, participants completed two questionnaires: The Social Support Effectiveness Questionnaires (SSEQ55) and the Interpersonal Support Evaluation List (ISEL55). The SSEQ is a 25-item questionnaire that evaluates the perceived effectiveness of support received from another person, which for this study was the pregnant individual’s partner. Psychometric evaluation reveals reliability of the SSEQ with alpha (a=0.8755).
The ISEL is a 12-item questionnaire that evaluates general support received from a broader network, including friends and family.56 Reliability for the ISEL has been demonstrated in a cohort of mothers from a general population, with alpha (a=0.8657).
Additionally, participants reported whether they regularly attended a religious, cultural or social group that could not meet during the COVID-19 pandemic.
Coping
To explore how individuals were coping with the uncertainty and stress of being pregnant during the COVID-19 pandemic, participants were asked an open-ended question, ‘People are responding to the pandemic in many ways. Can you tell us what things you are doing to cope with the COVID-19 pandemic?’
Data analysis
Statistical analysis
IBM SPSS Statistics V.28 was used for all statistical analysis. Survey responses were checked for incomplete or invalid responses, which were removed prior to analyses. Outliers in the data were also examined and winsorised if >3 SD from the mean of the corresponding measure. This resulted in the winsorisation of two PROMIS Anxiety t-score data points and one ISEL data point. Descriptive statistics (n=336) were computed for demographic information, including geographical location, age, marital status, household income and education. Additionally, descriptive statistics (n=336) were computed for mental well-being, social support and disruptions to prenatal care.
Hierarchical linear regression analyses (n=260) were used to examine the impact of various predictors on anxiety (model 1) and depression (model 2) for pregnant Indigenous persons. Block 1 included demographic characteristics, such as age, household income, education, marital status, savings, gestation and parity. Block 2 included social support characteristics, such as levels of general social support, partner social support and social group attendance. Finally, block 3 included COVID-19-related disruptions to prenatal care, such as changes in care, prenatal appointment cancellations, decrease in quality care, concern about self and baby not receiving necessary care, changes to birthing plans, trouble accessing healthcare and ability to bring partner or support person to appointments. Approximately 23% of participants (n=76) were missing data for one or more of the predictor variables, and these cases were handled through listwise deletion for this portion of the analyses.
Qualitative analysis
The open-ended response question asking participants to report on the ways they were coping was analysed qualitatively using a thematic approach. The responses to this question were exported from SPSS to NVivo where they were analysed and coded thematically for identified themes.58 As a first phase step, potential codes were documented based on topics from raw data. Analysis began with a deductive assessment of identifying data to fit within the codes. Subsequently, further coding was conducted inductively through the creation of codes based on emerging themes within the data.59 Themes were exported from SPSS to a password-protected file where they were summarised. Due to language constraints resulting form the collection of qualitative responses in both French and English, and time constraints, one coder conducted these analyses for the qualitative data. This coder identifies as an Indigenous woman who has particular interest and experience in studies related to Indigenous family wellness.
Results
Participants in this study experienced a broad range of service disruptions due to the COVID-19 pandemic. The majority of participants (76.8%) experienced changes in prenatal care, including appointment cancellations (59.5%), with close to one-third of participants (32.1%) having made changes to their birthing plan. Specific changes included changes to birth location (11.3%), childcare arrangements (8.3%) and other unspecified changes (2.7%). Additionally, participants also reported changes to support people (25.6%), specifically, not being able to bring a support person to prenatal care appointments (84.5%). Just over half (54.8%) reported difficulties in accessing healthcare services such as massage (43.8%), chiropractic care (21.4%), psychological counselling (15.8%), physiotherapy (10.7%), other unspecified services (9.2%) and acupuncture (8.6%). A quarter (25%) of participants reported that religious, cultural or social groups that they regularly attended could not meet during the pandemic. Participants also experienced high levels of psychological distress, with 40% meeting clinical cut-offs for comorbid depression and anxiety, 14% meeting cut-offs for only anxiety and 5% meeting cut-offs for only depression. Additional sample characteristics for psychological distress, protective factors and COVID-19-related prenatal care disruptions are noted in table 1.
Table 1.
Sample characteristics for psychological distress, protective factors and COVID-19-related prenatal care disruptions
| Measure | Mean | SD | Range |
| Psychological distress | |||
| Edinburgh Postnatal Depression Scale | 12.77 | 5.26 | 0–29 |
| PROMIS anxiety t-scores* | 61.15 | 8.07 | 42.1–82.7 |
| Protective factors | |||
| General social support* | 37.42 | 7.33 | 14–48 |
| Partner social support | 51.21 | 16.92 | 4–80 |
| Social group attendance | 83 yes / 220 no / 7 n/a | ||
| COVID-19-related service disruption | |||
| Changes in prenatal care | 258 yes/45 no | ||
| Prenatal appointment cancellations | 103 yes/200 no | ||
| Decrease in quality care | 45.69 | 33.07 | 0–100 |
| Concern about self and baby not receiving necessary care | 35.64 | 31.50 | 0–100 |
| Changes in birth plan | 108 yes/194 no | ||
| Trouble accessing healthcare | 184 yes/118 no | ||
| Ability to bring partner or support person to appointments | 47 yes/256 no | ||
*Winsorised.
PROMIS, Patient-Reported Outcomes Measurement Information System.
Depression
Analysis of the first hierarchical linear regression model revealed that all three blocks significantly predicted levels of prenatal depression symptoms among pregnant Indigenous persons. The first block included the demographic variables of age, household income, education, marital status, household savings, gestational age and parity. This first block accounted for 14.4% of the variance, F(7,252)=6.047, p<0.001, f2=0.17. Increased levels of household income (p=0.004) and savings (p=0.006) significantly predicted decreased depression symptoms. Additionally, being married, living in a common-law relationship or living with a partner was also a significant predictor of decreased depression symptoms (p=0.036).
When added in the second block, general social support, partner social support and social group attendance significantly accounted for an additional 15.9% of the variance in depression symptoms, F(3,249)=18.881, p<0.001, f2=0.23. Overall, the second block accounted for 30.2% of the variance in depression symptoms, F(10,249)=10.798, p<0.001, f2 = 0.43. Higher levels of savings continued to significantly predict decreased depression symptoms (p=0.021). With respect to social support variables, increased general social support (p=0.006) and partner social support (p<0.001) were significantly predictive of decreased depression symptoms.
The third block added COVID-19-related prenatal care disruptions into the model, which accounted for an increased 6.9% of the variance, F(7,242)=3.809, p≤0.001, f2=0.11. This block accounted for 37.2% of the variance in depression symptoms, F(17,242)=8.422, p<0.001, f2=0.59. Increased general social support (p=0.009) and partner social support (p<0.001) continued to significantly predict decreased depression symptoms. Of prenatal care disruption variables, experiencing increased concerns about self and baby not receiving necessary care (p=0.022) and having trouble in accessing healthcare (p=0.017) significantly predicted increased depression symptoms. See table 2 for results of the whole model.
Table 2.
Hierarchical multiple regression analysis predicting depression symptoms
| Predictors | β | SE | T | P value | Adjusted R2 | |
| Block 1 | Constant | <0.001* | 0.120 | |||
| Age | −0.026 | 0.08 | −0.37 | 0.713 | ||
| Household income | −0.218 | 0.21 | −2.90 | 0.004* | ||
| Education, | 0.018 | 0.35 | 0.26 | 0.799 | ||
| Marital status | −0.131 | 1.14 | −2.11 | 0.036* | ||
| Savings | −0.173 | 0.29 | −2.75 | 0.006* | ||
| Gestation | −0.015 | 0.04 | −0.25 | 0.805 | ||
| Parity | 0.047 | 0.49 | 0.72 | 0.470 | ||
| Block 2 | Constant | <0.001* | 0.274 | |||
| Age | −0.093 | 0.08 | −1.41 | 0.161 | ||
| Household income | −0.105 | 0.20 | −1.50 | 0.135 | ||
| Education | 0.013 | 0.33 | 0.19 | 0.849 | ||
| Marital status | −0.087 | 1.06 | −1.53 | 0.127 | ||
| Savings | −0.134 | 0.27 | −2.32 | 0.021* | ||
| Gestation | −0.006 | 0.04 | −0.12 | 0.907 | ||
| Parity | −0.033 | 0.46 | −0.54 | 0.587 | ||
| General social support | −0.173 | 0.02 | −2.75 | 0.006* | ||
| Partner social support | −0.312 | 0.05 | −4.65 | <0.001* | ||
| Social group attendance | 0.073 | 0.73 | 1.28 | 0.200 | ||
| Block 3 | Constant | <0.001* | 0.328 | |||
| Age | −0.079 | 0.08 | −1.22 | 0.225 | ||
| Household income | −0.133 | 0.20 | −1.92 | 0.056 | ||
| Education | −0.013 | 0.32 | −0.20 | 0.839 | ||
| Marital status | −0.101 | 1.02 | −1.82 | 0.070 | ||
| Savings | −0.105 | 0.26 | −1.87 | 0.063 | ||
| Gestation | −0.051 | 0.04 | −0.95 | 0.345 | ||
| Parity | −0.012 | 0.45 | −0.21 | 0.834 | ||
| General social support | −0.161 | 0.02 | −2.62 | 0.009* | ||
| Partner social support | −0.243 | 0.05 | −3.65 | <0.001* | ||
| Social group attendance | 0.020 | 0.73 | 0.35 | 0.727 | ||
| Changes in prenatal care | 0.003 | 1.17 | 0.05 | 0.962 | ||
| Prenatal appointment cancellations | −0.037 | 0.75 | −0.60 | 0.552 | ||
| Decrease in quality care | −0.030 | 0.02 | −0.32 | 0.751 | ||
| Concern about self and baby not receiving necessary care | 0.207 | 0.02 | 2.31 | 0.022* | ||
| Changes in birth plan | 0.097 | 0.69 | 1.70 | 0.090 | ||
| Trouble accessing healthcare | 0.136 | 0.68 | 2.41 | 0.017* | ||
| Ability to bring partner or support person to appointments | −0.030 | 0.88 | −0.53 | 0.596 | ||
*p<0.05.
Anxiety
Similar to the first model, analysis of the second hierarchical linear regression model revealed that all three blocks significantly predicted levels of prenatal anxiety symptoms. The first block demonstrated that demographics accounted for 8.0% of the explained variance in anxiety symptoms, F(7,252)=3.110, p=0.004, f2=0.09. Increased levels of household income (p=0.038) and savings (p=0.007) were significantly predictive of decreased anxiety symptoms. Meanwhile, education, marital status, gestation and parity did not significantly predict anxiety symptoms.
In the second block, the addition of general social support, partner social support and social group attendance increased the explained variance in anxiety symptoms by 10.9%, F(3,249)=11.201, p<0.001, f2=0.13. As a whole, the second block accounted for 18.9% of the variance in anxiety symptoms, F(10,249)=5.801, p<0.001, f2=0.23. Increased levels of savings (p=0.019) continued to be predictive of decreased anxiety symptoms. With respect to social support variables, increased partner social support predicted lower anxiety symptoms (p<0.001), while social group attendance and general social support were not significant predictors (p>0.05).
The addition of COVID-19-related prenatal care service disruptions in the third block increased the explained variance in anxiety symptoms by 10.1%, F(7,242)=4.908, p<0.001, f2=0.14. This final block was responsible for predicting 29.0% of the variance in anxiety symptoms, F(17,242)=5.808, p<0.001, f2=0.41. Of the demographic and social support variables, only increased partner social support continued to significantly predict decreased anxiety symptoms (p=0.002). Regarding service care disruptions, experiencing changes in birth plans (p=0.026) and having trouble accessing healthcare (p=0.038), significantly predicted increased anxiety symptoms. Further, experiencing increased concerns about self and baby not receiving necessary care also significantly predicted increased anxiety symptoms (p<0.001). See table 3 for results of the whole model.
Table 3.
Hierarchical multiple regression analysis predicting anxiety symptoms
| Predictors | β | SE | T | P value | Adjusted R2 | |
| Block 1 | 0.004* | 0.054 | ||||
| Age | −0.032 | 0.12 | −0.44 | 0.663 | ||
| Household income | −0.162 | 0.31 | −2.08 | 0.038* | ||
| Education | 0.096 | 0.51 | 1.31 | 0.192 | ||
| Marital status | −0.065 | 1.67 | −1.01 | 0.315 | ||
| Savings | −0.176 | 0.43 | −2.70 | 0.007* | ||
| Gestation | −0.003 | 0.06 | −0.04 | 0.965 | ||
| Parity | 0.055 | 0.72 | 0.81 | 0.418 | ||
| Block 2 | <0.001 | 0.156 | ||||
| Age | −0.095 | 0.12 | −1.34 | 0.181 | ||
| Household income | −0.069 | 0.30 | −0.91 | 0.364 | ||
| Education | 0.094 | 0.50 | 1.29 | 0.197 | ||
| Marital status | −0.021 | 1.60 | −0.35 | 0.729 | ||
| Savings | −0.146 | 0.41 | −2.36 | 0.019* | ||
| Gestation | 0.004 | 0.05 | 0.07 | 0.941 | ||
| Parity | −0.007 | 0.70 | −0.11 | 0.914 | ||
| General social support | −0.086 | 0.03 | −1.27 | 0.205 | ||
| Partner social support | −0.299 | 0.08 | −4.12 | <0.001* | ||
| Social group attendance | 0.086 | 1.11 | 1.40 | 0.162 | ||
| Block 3 | <0.001* | 0.240 | ||||
| Age | −0.083 | 0.12 | −1.20 | 0.231 | ||
| Household income | −0.090 | 0.30 | −1.22 | 0.223 | ||
| Education | 0.064 | 0.48 | 0.91 | 0.364 | ||
| Marital status | −0.034 | 1.53 | −0.59 | 0.559 | ||
| Savings | −0.113 | 0.39 | −1.89 | 0.061 | ||
| Gestation | −0.046 | 0.05 | −0.80 | 0.423 | ||
| Parity | 0.023 | 0.68 | 0.36 | 0.718 | ||
| General social support | −0.079 | 0.03 | −1.21 | 0.227 | ||
| Partner social support | −0.216 | 0.08 | −3.06 | 0.002* | ||
| Social group attendance | 0.019 | 1.09 | 0.32 | 0.749 | ||
| Changes in prenatal care | 0.020 | 1.75 | 0.28 | 0.780 | ||
| Prenatal appointment cancellations | −0.072 | 1.12 | −1.10 | 0.273 | ||
| Decrease in quality care | −0.091 | 0.03 | −0.90 | 0.371 | ||
| Concern about self and baby not receiving necessary care | 0.319 | 0.03 | 3.36 | <0.001* | ||
| Changes in birth plan | 0.135 | 1.04 | 2.24 | 0.026* | ||
| Trouble accessing healthcare | 0.125 | 1.02 | 2.09 | 0.038* | ||
| Ability to bring partner or support person to appointments | 0.003 | 1.31 | 0.05 | 0.964 | ||
*p<0.05.
Coping
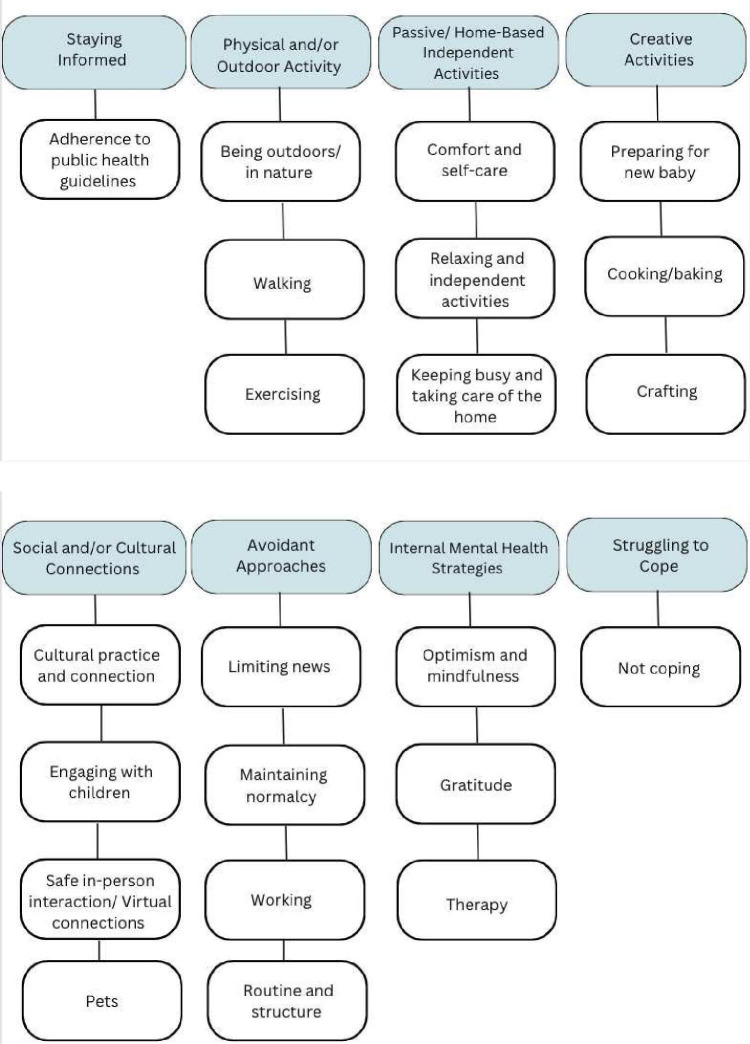
Approximately half of participants (n=167) responded to the open-ended question about coping, with the majority of responses (67.5%) being between 1 and 20 words in length. Eight themes emerged: staying informed, physical and/or outdoor activities, passive or independent home-based activities, creative activities, social and/or cultural activities, avoidant approaches, internal mental health strategies and struggling to cope. Subcodes (see figure 1) were developed within each theme. Results from open-ended response questions are summarised in table 4.
Figure 1.
Coping strategies themes and subthemes.
Table 4.
Coping strategies—qualitative themes
| Theme | Subtheme(s) | Overview | Quotes |
| Staying informed | Adherence to public health guidelines | This theme is characterised by caution and care related to public health advisory in response to the pandemic. Staying home, handwashing, wearing a mask, social distancing and adapting daily activities such as work, shopping and school to virtual mediums were expressed by some participants as eliciting peace of mind. | ‘Using PPE, being extra cautious.’ ‘Following health authorities’ guidelines.’ ‘Staying home. No friends over for the kids or any visiting friends.’ |
| Physical and/or outdoor activity | Being outdoors/in nature; Walking; Exercising |
Participants shared that spending time outdoors, in nature and being physically active are practices that support coping through pregnancy during the pandemic. Most commonly, walking and gardening were referenced in this sample. | ‘I find dealing with your head easier when you can put it all into a project with long term benefits. Food and living life are always solid go-to’s for mental health, try to live in the present.’ ‘I have always been very active outside wilderness trips, kayaking hikes… so I've turned to gardening, making my yard beautiful getting a few chickens to focus on.’ |
| Passive and/or home-based independent activities | Comfort and self-care; Relaxing and independent activities; Keeping busy and taking care of the home |
Activities ranging from reading, increasing hours of rest, tackling yard work, and home cleaning, were found to be comforting by many participants. While this theme is characterised by independent activities that can be enjoyed in the home, we differentiate between those who preferred more passive activities such as bathing and napping, and those who preferred more energetic activities, such as household chores. | ‘Keeping my mind occupied with television, reading or sleeping during the day.’ ‘Keeping the house tidy and clean which has been very satisfying.’ |
| Creative activities | Preparing for new baby; Cooking/baking; Crafting | Creative activities were shared by some participants as being beneficial additions to their coping strategies. These included making arrangements for a new baby, cooking, baking and crafting. | ‘I am finding ways to make myself more excited about the baby having a friend do weekly bump photos outside my home and making a pregnancy book.’ ‘Cooking nice food and getting excited about meals.’ |
| Social and/or cultural activities | Cultural practice and connection; Engaging with children; Safe in-person interactions; Virtual social connection; Pets |
Socialising was a key theme among participants for maintaining well-being through the pandemic and navigating isolation during pregnancy. Cultural values were also referenced by some. Of particular note were the challenges communities faced engaging in community connection and cultural practices due to additional barriers brought forth by the pandemic. Participants found that interacting at home with their children, pets and partners was helpful in mitigating stress. Staying connected to extended family and friends in person when it was safe to do so, or virtually when necessary, was also noted as helpful. | ‘I am taking this extra time to really learn new ways to grow and have been reaching out for support more and talking more about my struggles with family and peers. Using snapchat had helped me keep in contact with my friends and loved ones.’ ‘Trying to connect with the Indigenous community online.’ ‘Moved into my parent’s house to have more help with the toddler and more socialization for all of us.’ |
| Avoidant approaches | Limiting news; Maintaining normalcy; Working; Routine and structure |
In contrast to those who found solace in staying informed on matters related to the pandemic, others found it more helpful to avoid news consumption and attempt to remain grounded in normalcy and routine. For example, by continuing to work and be consistent in the structure of their prepandemic lives, as well as those of their children, participants felt it easier to cope with circumstances of the broader environment. | ‘Only watch a little news in the morning but otherwise tuning it out.’ ‘Keeping to my normal pre-pandemic routine as much as possible.’ |
| Internal mental health strategies | Optimism and mindfulness; Gratitude; Therapy |
Perception-based strategies were employed by some participants in order to combat stressors arising as a result of the pandemic. These included being optimistic and mindful, finding opportunities to reflect and experience gratitude, taking life 1 day and a time, and attending mental health therapy sessions. | ‘I lost my mom and brother the year before the pandemic. So, comparatively, perspective has been important. I had already turned ‘inward’ and slowed my life to accommodate my grief journey. Pandemic felt like an extension of this.’ ‘I’ve also been able to find joy in many things, and am extremely grateful to be in such a position to be able to work, help, feel financially stable, and re-connect with my family during what is globally such an uncertain time’ |
| Struggling to cope | Not coping | Some participants stated that they are not coping well, if at all. Expressions of frustration with public health regulations were also shared. | ‘I am not coping well.’ ‘I’m not [coping].’ ‘Beyond the things above grocery shopping, it really stresses me out. I hate all the stupid rules…’ |
Discussion
During the COVID-19 pandemic, over half (>50%) of Indigenous pregnant individuals in our sample experienced clinically significant levels of prenatal depression and/or anxiety. Heightened levels of both depression and anxiety may have been impacted by uncertainty around the impacts of COVID-19, and time during which the data was collected, as health restrictions were high. Our results are consistent with other studies reporting increased depression and anxiety among pregnant individuals,2 31 along with increased mental well-being concerns among Indigenous populations.11 26 Participants reported increased service disruptions due to the COVID-19 pandemic, including restricted access to quality care and decreased quality of prenatal care, changes to birthing plans and decreased opportunities for social support during birthing.
Healthcare service use among pregnant individuals is dependent on several elements related to sociodemographic factors, economics and facility logistics, including distance to and quality of healthcare.60 The COVID-19 pandemic presented with unique challenges that further limited healthcare service use among pregnant individuals due to issues such as decreased access to prenatal services and concerns about contracting COVID-19.61 For Indigenous communities, systemic racial discrimination and inequalities in healthcare accessibility create further barriers in accessing quality prenatal care.11 12 26 Previous research suggests that there are strong associations between limited access to prenatal care and psychological distress among pregnant individuals, and our results mirror these findings when examining the Indigenous pregnant population in Canada.2
The importance of accessible quality prenatal care for both the pregnant individual and unborn baby cannot be overstated in discussions to support the psychological well-being of Indigenous pregnant individuals. Experiencing difficulties in access to prenatal care and having greater concerns about quality of care was significantly predictive of both prenatal depression and anxiety symptoms. Additionally, experiencing changes in birthing plans was significantly predictive of prenatal anxiety. Pregnancy care service quality and accessibility issues along with changes in birth plan are linked to depressive and anxiety-based symptoms across multiple studies.62–65 Discomfort with novel healthcare processes, such as virtual or telehealth appointments, and overlapping stress from experiencing a pregnancy during a global health pandemic may have further impacted self-reported levels of depression and anxiety. As pregnancies can be a time of heightened stress levels, uncertainties about accessing, and quality of, prenatal care are likely to impact mental well-being.66–68
These findings are aligned with others that have emerged in the literature regarding pregnancy during the pandemic with anxiety, depression and healthcare challenges noted consistently.24 69–71 Theoretical foundations to support these findings can be seen in Maslow’s classic conceptualisation of the Hierarchy of Needs72 where it is said that certain needs must be addressed prior to others. Specifically, physiological needs are posited to be of primary importance and said to be critical to address first, in order to then consider other needs. In this study, participants’ disclosures of distress related to issues with basic healthcare reflects the imperative nature of caring for such fundamental needs. In addition to health inequities, Indigenous peoples also face socioeconomic disparities73 which create further barriers in accessing healthcare and is consistent with policies to reduce poverty-related stress.74 The impacts of colonisation and generational wealth policies systematically create barriers for the wellness of pregnant Indigenous individuals. Due to the recruitment methodology of the larger pregnancy during the COVID-19 pandemic study, the sample generally skews towards higher socioeconomic status, thus, we may expect the importance of financial security to be more relevant in a more representative sample.
In addition to prenatal care, findings of this study also suggest the notable influence of social support on the well-being of pregnant Indigenous persons. Increased partner social support was predictive of decreased levels of depression and anxiety, while increased general social support was predictive of decreased levels of depression only. Similar findings were reported in the larger pregnancy during the pandemic sample by Lebel et al, 25 which found that both partner and general social support predicted reduced levels of anxiety and depression in pregnant individuals. These findings mirror previous literature in the field, which demonstrates significant associations between social support and mental well-being concerns among pregnant individuals broadly75–77 and among Indigenous pregnant individuals.34 The emergence of partner social support as the most significant predictor for prenatal anxiety and depression in comparison to other levels of social support (ie, general social support and social group attendance) is expected. At the height of the COVID-19 pandemic, numerous public health measures, such as mandatory lockdowns and social distancing, were introduced to limit transmission of the virus. For many individuals, these changes inadvertently affected access to social support systems outside the home, thereby increasing reliance on such systems within the home.78 The COVID-19 family disruption model78 highlights the importance of these relationships and social support systems in maintaining well-being during periods of heightened stress. For pregnant individuals, the significant association between prenatal mental well-being and partner social support during the COVID-19 pandemic24 79 80 presents partner support as a modifiable protective factor to enhance prenatal well-being.
In alignment with our objective to understand coping strategies, qualitative results reveal various approaches to coping with stressors as arisen through experiencing a pregnancy during a global health pandemic. These include strategies such as staying informed on the progression of the pandemic and public health guidelines, engaging in physical and/or outdoor activity, engaging in home-based and/or other independent activities, engaging in creative activities, engaging in social and cultural activities with family, developing mental well-being strategies and routines, (eg, meditation, practising gratitude, therapy) and attempting to avoid the pandemic reality (eg, limiting news consumption). This is consistent with extant literature on coping mechanisms related to avoidance-based activities, connection-driven activities and alignment with recommendations for safety from public health governing bodies.43–45 Some participants expressed struggles to cope or a perceived lack of coping entirely. Struggling to cope has been a consistent experience across pregnant individuals during the pandemic with shifting availability of prepandemic coping strategies and a substantial deviation from normalcy.81
In Canada specifically, pregnant individuals during the pandemic were found to have increased rates of depression and anxiety as amplified by financial strain, social isolation, risk of contracting the COVID-19 infection and relationship difficulties, which were buffered by social support.36 82 With Indigenous persons in Canada, we expect to see increased levels of distress due to disproportionate negative mental well-being experiences observed within that demographic.46 47 83 This is exacerbated through neglectful and harmful interactions with healthcare systems.84 It is important to acknowledge the resilience developed among Indigenous parents who continue to engage in support service-oriented research despite negative past and ongoing experiences throughout their pursuit of care in the perinatal period. Respondents in this study reported strengths with social and partner support and the use of various coping strategies which appear to add to resilience factors.
According to Lazarus and Folkman Transactional Theory of Stress and Coping (TTSC),85 individuals interact with stress in a transactional exchange with their environment. Coping that ensues is said to be categorised based on problem focused and emotion-focused strategies. Active coping aimed at addressing a given stressor is characteristic of a problem focused approach, whereas passive and avoidance-based coping is often representative of emotion-focused strategies. Given that addressing the ‘problem’ at the root of the stressor in this circumstance, namely the COVID-19 virus, was largely outside of participants’ control, active coping was seen in this sample through adherence to public health guidelines and taking steps to engage in health promoting activities such as being physically active and spending time outdoors. Additionally, avoidance-oriented coping was also noted in this sample, such as limited new consumption. Therefore, in keeping with the TTSC, both problem and emotion focused coping strategies are exemplified in our findings.
The Breath of Life Theory, coined by Blackstock,86 has been proposed as a critical framework for understanding relational elements of well-being and culturally centred understanding of needs for Indigenous, specifically First Nations, people. Our findings related to coping and social support provide evidence to support this in this study, as these factors revealed connection to spiritual and cultural practice, as well as social connection, were vital supports in the face challenges imposed by the pandemic provide evidence to support this in this study.
Limitations
A limitation of this study is the lack of inclusion of telehealth service use. As the participant sample consisted of Indigenous populations, the issue of limited access to reliable Wi-Fi and technology within some Indigenous communities should be noted as potentially impacting service use and disruption. Recruitment relying primarily on social media potentially reduced the number of participants that may have otherwise been recruited with a broader reach through other means. This may have also inflated the socioeconomic status of the sample due to the need for participants to have access to technology and social media. Therefore, our sample demographics reported household income as greater than the median for Canadian families in 2019,87 which does not accurately reflect median incomes for Indigenous populations.88
There was no assessment of the role of traditional birthing and health practices, such as midwives, in the original study. Access to traditional healing practices may have impacted differently than Western medical practices. Further, research practices have been historically harmful when conducted with Indigenous populations.74 89 90 This has led to mistrust of research groups and practices among Indigenous peoples and, consequently, may have impeded the participation of some Indigenous pregnant persons in this study. Finally, due to the heterogeneity of Indigenous communities, these findings may not be generalisable across all Indigenous Nations and individuals, as values and beliefs held by one Nation or individual are not necessarily reflective of all. Accordingly, caution must be exercised in interpreting these results to not erroneously assume pan-Indigeneity of perspectives shared and conclusions drawn herein. Given the rapid-response survey development and broad reach of the original study, baseline stressors were not included as part of data collection. Additionally, anxiety and depression symptom scores were based on self-report scores and not clinical diagnoses.
Implications and future directions
These results carry important implications for the information of pregnant Indigenous persons through the illustration of challenges in accessibility of care and changes in prenatal care resulting from the pandemic. Healthcare providers may benefit from findings produced through this study to inform change aimed at adequately accommodating the healthcare-related needs of Canadian Indigenous peoples experiencing a pregnancy. As part of the greater longitudinal objectives, future research will continue to track mental well-being of individuals who were pregnant during the pandemic and examine child well-being outcomes. Postpartum care will be studied to understand the extent to which services are improved or hindered as the pandemic progresses. Additionally, examining the racial and ethnicity concordance of service providers, along with access to traditional birthing services, should be examined for any potential influences on service access and use among the population in this study.
Service disruptions and/or low qualitive prenatal care is a serious issue which exacerbates systemic inequities and contributes to poor mental well-being.13 26 Aspects of service disruptions, such as access to traditional birthing methods and the use of telehealth services should be carefully considered. Social support, including partners and social groups, seems to be a protective factor for pregnant individuals. Enhancing the efficacy of policies and programming surrounding prenatal care, including the incorporation of a framework grounded in Indigenous perspectives,19 to increase accessibility and incorporate protective factors can increase quality of care. Further research in this area is warranted to understand the impact of COVID-19 on pregnant individuals, as exemplified by the following open-text response received from one of our participants:
‘I appreciate your researchers looking into this as for some time when the pandemic started, I felt invisible as a pregnant person as no one was paying attention to us so this makes me feel really good that as a group we are being considered. Thank you for your work.’
Supplementary Material
Footnotes
Contributors: GG, CAL and LT-M act as guarantors of the study and conceptualised the original study for which this study branches from. All authors were involved in conceptualisation of this study. MM, SL-P, JK and JD were involved in drafting the manuscript, data analysis and interpretation. GG, CAL, LT-M, LR and LW were involved in reviewing the manuscript. All authors gave final approval of the version to be published and agreement to be accountable for all aspects of the work.
Funding: This research was funded in part, by a Social Sciences and Humanities Research Council (SSHRC) Insight Grant (award/grant number N/A). Funding for author GG was provided by the Owerko Center, Alberta Children’s Hospital Research Institute. Salary funding for authors CAL and LT-M was provided by the Canada Research Chairs (CRC) program (award/ grant number N/A). Funding for author LR was provided by Research Manitoba, Canadian Institutes of Health Research (CIHR), SSHRC and the Children’s Hospital Research Institute of Manitoba (award/grant numbers N/A).
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
All data relevant to the study are included in the article or uploaded as online supplemental information. Not applicable.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study involves human participants and was approved by University of Calgary Conjoint Health Research Ethics Board (REB20-0500). Participants gave informed consent to participate in the study before taking part.
References
- 1. Chen XK, Wen SW, Yang Q, et al. Adequacy of prenatal care and neonatal mortality in infants born to mothers with and without Antenatal high-risk conditions. Aust N Z J Obstet Gynaecol 2007;47:122–7. 10.1111/j.1479-828X.2007.00697.x Available: 10.1111/j.1479-828X.2007.00697.x [DOI] [PubMed] [Google Scholar]
- 2. Groulx T, Bagshawe M, Giesbrecht G, et al. Prenatal care disruptions and associations with maternal mental health during the COVID-19 pandemic. Front Glob Womens Health 2021;2:648428. 10.3389/fgwh.2021.648428 Available: 10.3389/fgwh.2021.648428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Hohmann-Marriott B. The couple context of pregnancy and its effects on prenatal care and birth outcomes. Matern Child Health J 2009;13:745–54. 10.1007/s10995-009-0467-0 Available: 10.1007/s10995-009-0467-0 [DOI] [PubMed] [Google Scholar]
- 4. American Academy of Pediatrics and the American College of Obstetricians and Gynecologists . Preconception and Antepartum care, Intrapartum and postpartum care of the mother. guidelines for perinatal care. American Academy of Pediatrics and American College of Obstetricians and Gynecologists, 2012: 95–210. Available: 10.1542/9781581107715 [DOI] [Google Scholar]
- 5. Buultjens M, Gill J, Fielding J, et al. Maternity care during a pandemic: can a hybrid Telehealth model comprising group Interdisciplinary education support maternal psychological health? Women Birth 2023;36:305–13. 10.1016/j.wombi.2022.09.007 Available: 10.1016/j.wombi.2022.09.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Evans WN, Lien DS. The benefits of prenatal care: evidence from the PAT bus strike. Journal of Econometrics 2005;125:207–39. 10.1016/j.jeconom.2004.04.007 Available: 10.1016/j.jeconom.2004.04.007 [DOI] [Google Scholar]
- 7. McDuffie RS, Beck A, Bischoff K, et al. Effect of frequency of prenatal care visits on perinatal outcome among low-risk women: A randomized controlled trial. JAMA 1996;275:847–51. Available: 10.1001/jama.1996.03530350029030 [DOI] [PubMed] [Google Scholar]
- 8. Pant S, Koirala S, Subedi M. Access to maternal health services during COVID-19. Europasian J Med Sci 2020;2:46–50. 10.46405/ejms.v2i2.110 Available: 10.46405/ejms.v2i2.110 [DOI] [Google Scholar]
- 9. Sanders J, Blaylock R. Anxious and Traumatised”: users’ experiences of maternity care in the UK during the COVID-19 pandemic. Midwifery 2021;102. 10.1016/j.midw.2021.103069 Available: 10.1016/j.midw.2021.103069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Futterman ID, Grace H, Weingarten S, et al. Maternal anxiety, depression and Posttraumatic stress disorder (PTSD) after natural disasters: a systematic review. J Matern Fetal Neonatal Med 2023;36:2199345. 10.1080/14767058.2023.2199345 [DOI] [PubMed] [Google Scholar]
- 11. Kim PJ. Social determinants of health inequities in indigenous Canadians through a life course approach to colonialism and the residential school system. Health Equity 2019;3:378–81. 10.1089/heq.2019.0041 Available: 10.1089/heq.2019.0041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Richmond CAM, Cook C. Creating conditions for Canadian aboriginal health equity: the promise of healthy public policy. Public Health Rev 2016;37:2. 10.1186/s40985-016-0016-5 Available: 10.1186/s40985-016-0016-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Akter S, Davies K, Rich JL, et al. Indigenous women’s access to maternal Healthcare services in Lower- and middle-income countries: a systematic integrative review. Int J Public Health 2019;64:343–53. 10.1007/s00038-018-1177-4 Available: 10.1007/s00038-018-1177-4 [DOI] [PubMed] [Google Scholar]
- 14. Leason JL. Exploring the complex context of Canadian indigenous maternal child-health through maternity experiences: the role of social determinants of health. Social Determinants of Health 2018;4:54–67. Available: 10.22037/sdh.v4i2.19504 [DOI] [Google Scholar]
- 15. Harding L. What’s the harm? examining the stereotyping of indigenous peoples in health systems. Simon Fraser University; 2018. [Google Scholar]
- 16. Joseph B. 21 Things you may not know about the Indian Act: Helping Canadians make reconciliation with Indigenous peoples a reality. Indigenous Relations Press, 2018. [Google Scholar]
- 17. Hyett SL, Gabel C, Marjerrison S, et al. Deficit-based indigenous health research and the stereotyping of indigenous peoples. Bioethics 2019;2:102–9. 10.7202/1065690ar Available: 10.7202/1065690ar [DOI] [Google Scholar]
- 18. Public Health Agency of Canada . Pregnancy, Childbirth and Caring for Newborns: Advice for Mothers During COVID-19, . 2020. Available: https://www.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection/prevention-risks/pregnancy-childbirth-newborn.html#a1
- 19. Quinn P, Williamson B, Gibbs L. Indigenous-informed disaster recovery: addressing collective trauma using a healing framework. Progress in Disaster Science 2022;16:100257. 10.1016/j.pdisas.2022.100257 [DOI] [Google Scholar]
- 20. Smylie J, O’Brien K, Beaudoin E, et al. Long-distance travel for birthing among indigenous and non-indigenous pregnant people in Canada. CMAJ 2021;193:E948–55. 10.1503/cmaj.201903 Available: 10.1503/cmaj.201903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Leason J. Indigenous women’s stress and postpartum depression: discussions from the Canadian maternity experiences survey and indigenous maternity narratives. IJIH 2021;16:225–43. 10.32799/ijih.v16i2.33180 Available: 10.32799/ijih.v16i2.33180 [DOI] [Google Scholar]
- 22. Dayan J, Creveuil C, Marks MN, et al. Prenatal depression, Prenatal anxiety, and spontaneous Preterm birth: a prospective cohort study among women with early and regular care. Psychosom Med 2006;68:938–46. 10.1097/01.psy.0000244025.20549.bd Available: 10.1097/01.psy.0000244025.20549.bd [DOI] [PubMed] [Google Scholar]
- 23. Elsenbruch S, Benson S, Rücke M, et al. Social support during pregnancy: effects on maternal depressive symptoms, smoking and pregnancy outcome. Hum Reprod 2007;22:869–77. 10.1093/humrep/del432 Available: 10.1093/humrep/del432 [DOI] [PubMed] [Google Scholar]
- 24. Hessami K, Romanelli C, Chiurazzi M, et al. COVID-19 pandemic and maternal mental health: a systematic review and meta-analysis. The Journal of Maternal-Fetal & Neonatal Medicine 2022;35:4014–21. 10.1080/14767058.2020.1843155 Available: 10.1080/14767058.2020.1843155 [DOI] [PubMed] [Google Scholar]
- 25. Lebel C, MacKinnon A, Bagshawe M, et al. Elevated depression and anxiety symptoms among pregnant individuals during the COVID-19 pandemic. J Affect Disord 2020;277:5–13. 10.1016/j.jad.2020.07.126 Available: 10.1016/j.jad.2020.07.126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Racine N, Hetherington E, McArthur BA, et al. Maternal depressive and anxiety symptoms before and during the COVID-19 pandemic in Canada: a longitudinal analysis. Lancet Psychiatry 2021;8:405–15. 10.1016/S2215-0366(21)00074-2 Available: 10.1016/S2215-0366(21)00074-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Tomfohr-Madsen LM, Racine N, Giesbrecht GF, et al. Depression and anxiety in pregnancy during COVID-19: a rapid review and meta-analysis. Psychiatry Res 2021;300:113912. 10.1016/j.psychres.2021.113912 Available: 10.1016/j.psychres.2021.113912 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Cena L, Gigantesco A, Mirabella F, et al. Prevalence of comorbid anxiety and depressive Symptomatology in the third trimester of pregnancy: analysing its association with Sociodemographic, obstetric, and mental health features. J Affect Disord 2021;295:1398–406. 10.1016/j.jad.2021.09.015 Available: 10.1016/j.jad.2021.09.015 [DOI] [PubMed] [Google Scholar]
- 29. Giesbrecht GF, van de Wouw M, Rioux C, et al. Cumulative effects of pre-pandemic Vulnerabilities and pandemic-related hardship on psychological distress among pregnant individuals. General Hospital Psychiatry 2023;83:93–100. 10.1016/j.genhosppsych.2023.04.016 Available: 10.1016/j.genhosppsych.2023.04.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Matsumura K, Hamazaki K, Tsuchida A, et al. Education level and risk of postpartum depression: results from the Japan environment and children’s study (JECS). BMC Psychiatry 2019;19:419. 10.1186/s12888-019-2401-3 Available: 10.1186/s12888-019-2401-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Bowen A, Bowen R, Maslany G, et al. Anxiety in a socially high-risk sample of pregnant women in Canada. Can J Psychiatry 2008;53:435–40. 10.1177/070674370805300708 Available: 10.1177/070674370805300708 [DOI] [PubMed] [Google Scholar]
- 32. Statistics . Statistics Canada; Indigenous population continues to grow and is much younger than the non-Indigenous population, although the pace of growth has slowed, . 2021. Available: https://www150.statcan.gc.ca/n1/daily-quotidien/220921/dq220921a-eng.htm [Google Scholar]
- 33. Toombs E, Lund J, Mushquash CJ. Adverse childhood experiences (aces) are increasing in indigenous populations in Canada: now what Canadian Psychology / Psychologie Canadienne 2022;63:576–88. 10.1037/cap0000331 Available: 10.1037/cap0000331 [DOI] [Google Scholar]
- 34. Bowen A, Stewart N, Baetz M, et al. Antenatal depression in socially high-risk women in Canada. Journal of Epidemiology & Community Health 2009;63:414–6. 10.1136/jech.2008.078832 Available: 10.1136/jech.2008.078832 [DOI] [PubMed] [Google Scholar]
- 35. Giesbrecht GF, Bagshawe M, van Sloten M, et al. Protocol for the pregnancy during the COVID-19 pandemic (Pdp) study: A longitudinal cohort study of mental health among pregnant Canadians during the COVID-19 pandemic and developmental outcomes in their children. JMIR Res Protoc 2021;10:e25407. 10.2196/25407 Available: 10.2196/25407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Khoury JE, Atkinson L, Bennett T, et al. COVID-19 and mental health during pregnancy: the importance of cognitive appraisal and social support. J Affect Disord 2021;282:1161–9.:S0165-0327(21)00040-9. 10.1016/j.jad.2021.01.027 Available: 10.1016/j.jad.2021.01.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Richardson L, Crawford A. Covid-19 and the Decolonization of indigenous public health. CMAJ 2020;192:E1098–100.:38. 10.1503/cmaj.200852 Available: 10.1503/cmaj.200852 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Shah PS, Zao J, Al-Wassia H, et al. Pregnancy and neonatal outcomes of aboriginal women: A systemic review and meta-analysis. Womens Health Issues 2011;21:28–39. 10.1016/j.whi.2010.08.005 Available: 10.1016/j.whi.2010.08.005 [DOI] [PubMed] [Google Scholar]
- 39. Wenman WM, Joffres MR, Tataryn IV. A prospective cohort study of pregnancy risk factors and birth outcomes in aboriginal women. Canadian Medical Association Journal 2004;171:585–9. 10.1503/cmaj.1031730 Available: 10.1503/cmaj.1031730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Cox RG, Zhang L, Zotti ME, et al. Prenatal care utilization in Mississippi: racial disparities and implications for unfavorable birth outcomes. Matern Child Health J 2011;15:931–42. 10.1007/s10995-009-0542-6 Available: 10.1007/s10995-009-0542-6 [DOI] [PubMed] [Google Scholar]
- 41. World Health Organization . Coronavirus disease (COVID-19) pandemic. World Health Organization; 2015. Available: https://www.who.int/emergencies/diseases/novel-coronavirus-2019?adgroupsurvey={adgroupsurvey}&gclid=Cj0KCQjwqoibBhDUARIsAH2OpWg7LF8VOzjaOhcblGl9HYFxwtM-waYjs7kg8W3U2z5Im7el1wEQFRsaAm4BEALw_wcB [Google Scholar]
- 42. Carlin E, Seear KH, Ferrari K, et al. Risk and resilience: a mixed methods investigation of aboriginal Australian women’s perinatal mental health screening assessments. Soc Psychiatry Psychiatr Epidemiol 2021;56:547–57. 10.1007/s00127-020-01986-7 Available: 10.1007/s00127-020-01986-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Ilska M, Przybyła-Basista H. The role of partner support, ego-resiliency, Prenatal attitudes towards maternity and pregnancy in psychological well-being of women in high-risk and low-risk pregnancy. Psychology, Health & Medicine 2020;25:630–8. 10.1080/13548506.2020.1737718 Available: 10.1080/13548506.2020.1737718 [DOI] [PubMed] [Google Scholar]
- 44. Firouzbakht M, Rahmani N, Sharif Nia H, et al. Coping strategies and depression during the COVID-19 pandemic in pregnant women: a cross sectional study. BMC Psychiatry 2022;22:153. 10.1186/s12888-022-03792-8 Available: 10.1186/s12888-022-03792-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Penengo C, Colli C, Cesco M, et al. Stress, coping, and psychiatric symptoms in pregnant women in outpatient care during the 2021 second-wave COVID-19 pandemic. Front Psychiatry 2021;12:775585.:775585. 10.3389/fpsyt.2021.775585 Available: 10.3389/fpsyt.2021.775585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Wheeler JM, Misra DP, Giurgescu C. Stress and coping among pregnant black women during the COVID‐19 pandemic. Public Health Nursing 2021;38:596–602. 10.1111/phn.12909 Available: https://onlinelibrary.wiley.com/toc/15251446/38/4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Rieger KL, Heaman MI. Factors associated with high levels of perceived Prenatal stress among inner-city women. Journal of Obstetric, Gynecologic & Neonatal Nursing 2016;45:180–95. 10.1016/j.jogn.2015.12.005 Available: 10.1016/j.jogn.2015.12.005 [DOI] [PubMed] [Google Scholar]
- 48. Owais S, Faltyn M, Johnson AVD, et al. The perinatal mental health of indigenous women: a systematic review and meta-analysis. Can J Psychiatry 2020;65:070674371987702. 10.1177/0706743719877029 Available: 10.1177/0706743719877029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Niccols A, Dell CA, Clarke S. Treatment issues for aboriginal mothers with substance use problems and their children. Int J Ment Health Addict 2010;8:320–35. 10.1007/s11469-009-9255-8 Available: 10.1007/s11469-009-9255-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Ritland L, Jongbloed K, Mazzuca A, et al. Culturally safe, strengths-based parenting programs supporting indigenous families impacted by substance use—a Scoping review. Int J Ment Health Addiction 2020;18:1586–610. 10.1007/s11469-020-00237-9 Available: 10.1007/s11469-020-00237-9 [DOI] [Google Scholar]
- 51. Roy A. Intergenerational trauma and aboriginal women: implications for mental health during pregnancy 1. Fpcfr 2019;14:211–24. 10.7202/1071297ar Available: 10.7202/1071297ar [DOI] [Google Scholar]
- 52. Kovach M. Indigenous methodologies: Characteristics, conversations, and contexts. University of Toronto Press, 2010. [Google Scholar]
- 53. Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression: development of the 10-item Edinburgh postnatal depression scale. Br J Psychiatry 1987;150:782–6. 10.1192/bjp.150.6.782 Available: 10.1192/bjp.150.6.782 [DOI] [PubMed] [Google Scholar]
- 54. Pilkonis PA, Choi SW, Reise SP, et al. Item banks for measuring emotional distress from the patient-reported outcomes measurement information system (PROMIST): depression, anxiety, and anger. Assessment 2011;18:263–83. 10.1177/1073191111411667 Available: 10.1177/1073191111411667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Rini C, Schetter CD, Hobel CJ, et al. Effective social support: antecedents and consequences of partner support during pregnancy. Personal Relationships 2006;13:207–29. 10.1111/j.1475-6811.2006.00114.x Available: https://onlinelibrary.wiley.com/toc/14756811/13/2 [DOI] [Google Scholar]
- 56. Cohen S, Hoberman HM. Positive events and social supports as buffers of life change stress . J Applied Social Pyschol 1983;13:99–125. 10.1111/j.1559-1816.1983.tb02325.x Available: https://onlinelibrary.wiley.com/toc/15591816/13/2 [DOI] [Google Scholar]
- 57. Aftyka A, Rozalska I, Pawlak A, et al. Internal consistency and accuracy of interpersonal support evaluation list (ISEL-40) in mothers of healthy children and those with a medical history. Ann Agric Environ Med 2019;26:85–91.:91783. 10.26444/aaem/91783 Available: 10.26444/aaem/91783 [DOI] [PubMed] [Google Scholar]
- 58. Braun V, Clarke V. Using thematic analysis in psychology. Qualitative Research in Psychology 2006;3:77–101.:77—101. 10.1191/1478088706qp063oa Available: 10.1191/1478088706qp063oa [DOI] [Google Scholar]
- 59. Delve . PowerPoint Slides; Introduction to qualitative coding with Delve, . 2020. Available: https://documentcloud.adobe.com/link/review?uri=urn:aaid:scds:US:660c0e6d-45bf-4c00-8752-3a6139414feb [Google Scholar]
- 60. Aziz Ali S, Ahmed Dero A, Aziz Ali S, et al. Factors affecting the utilization of Antenatal care among pregnant women: a literature review. Neonatal-Medicine 2018;02. 10.35841/neonatal-medicine.2.2.41-45 Available: 10.35841/neonatal-medicine.2.2.41-45 [DOI] [Google Scholar]
- 61. Aranda Z, Binde T, Tashman K, et al. Disruptions in maternal health service use during the COVID-19 pandemic in 2020: experiences from 37 health facilities in low-income and middle-income countries. BMJ Glob Health 2022;7:e007247. 10.1136/bmjgh-2021-007247 Available: 10.1136/bmjgh-2021-007247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Bayrampour H, Tamana SK, Boutin A. Pregnant people’s responses to the COVID-19 pandemic: a mixed-methods, descriptive study. Cmajo 2022;10:E146–54. 10.9778/cmajo.20210136 Available: 10.9778/cmajo.20210136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Brislane Á, Larkin F, Jones H, et al. Access to and quality of Healthcare for pregnant and postpartum women during the COVID-19 pandemic. Front Glob Womens Health 2021;2:628625. 10.3389/fgwh.2021.628625 Available: 10.3389/fgwh.2021.628625 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Kotlar B, Gerson EM, Petrillo S, et al. The impact of the COVID-19 pandemic on maternal and perinatal health: a Scoping review. Reprod Health 2021;18:10.:10. 10.1186/s12978-021-01070-6 Available: 10.1186/s12978-021-01070-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Liu CH, Koire A, Erdei C, et al. Unexpected changes in birth experiences during the COVID-19 pandemic: implications for maternal mental health. Arch Gynecol Obstet 2022;306:687–97. 10.1007/s00404-021-06310-5 Available: 10.1007/s00404-021-06310-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Psychosocial risk factors: perinatal screening and intervention. Obstetrics & Gynecology 2006;108:469. 10.1097/00006250-200608000-00046 Available: 10.1097/00006250-200608000-00046 [DOI] [PubMed] [Google Scholar]
- 67. Geller PA. Pregnancy as a stressful life event. CNS Spectr 2004;9:188–97. 10.1017/s1092852900008981 Available: 10.1017/s1092852900008981 [DOI] [PubMed] [Google Scholar]
- 68. Kingston D, Heaman M, Fell D, et al. Factors associated with perceived stress and stressful life events in pregnant women: findings from the Canadian maternity experiences survey. Matern Child Health J 2012;16:158–68. 10.1007/s10995-010-0732-2 Available: https://doi.org/0.1007/s10995-010-0732-2 [DOI] [PubMed] [Google Scholar]
- 69. Cameron EE, Joyce KM, Delaquis CP, et al. Maternal psychological distress & mental health service use during the COVID-19 pandemic. J Affect Disord 2020;276:765–74.:S0165-0327(20)32526-X. 10.1016/j.jad.2020.07.081 Available: 10.1016/j.jad.2020.07.081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Rudrum S. Pregnancy during the global COVID-19 pandemic: Canadian experiences of care. Front Sociol 2021;6:611324. 10.3389/fsoc.2021.611324 Available: 10.3389/fsoc.2021.611324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Stirling Cameron E, Ramos H, Aston M, et al. COVID affected us all:” the birth and postnatal health experiences of resettled Syrian refugee women during COVID-19 in Canada. Reprod Health 2021;18:256.:256. 10.1186/s12978-021-01309-2 Available: 10.1186/s12978-021-01309-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Maslow AH. A theory of human motivation. Psychological Review 1943;50:370–96. 10.1037/h0054346 Available: 10.1037/h0054346 [DOI] [Google Scholar]
- 73. Hajizadeh M, Hu M, Bombay A, et al. Socioeconomic inequalities in health among indigenous peoples living off-Reserve in Canada: trends and determinants. Health Policy 2018;122:854–65. 10.1016/j.healthpol.2018.06.011 Available: 10.1016/j.healthpol.2018.06.011 [DOI] [PubMed] [Google Scholar]
- 74. Truth and Reconciliation Commission of Canada . Honouring the trust and reconciling for the future: summary of the final report of the truth and reconciliation Commission of Canada. The Truth and Reconciliation Commission of Canada; 2015. Available: https://ehprnh2mwo3.exactdn.com/wp-content/uploads/2021/01/Executive_Summary_English_Web.pdf [Google Scholar]
- 75. Bedaso A, Adams J, Peng W, et al. The relationship between social support and mental health problems during pregnancy: A systematic review and meta-analysis. Reprod Health 2021;18:162. 10.1186/s12978-021-01209-5 Available: 10.1186/s12978-021-01209-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Leach LS, Poyser C, Fairweather‐schmidt K. Maternal perinatal anxiety: A review of prevalence and correlates. Clinical Psychologist 2017;21:4–19. 10.1111/cp.12058 Available: 10.1111/cp.12058 [DOI] [Google Scholar]
- 77. Westdahl C, Milan S, Magriples U, et al. Social support and social conflict as predictors of Prenatal depression. Obstet Gynecol 2007;110:134–40. 10.1097/01.AOG.0000265352.61822.1b Available: 10.1097/01.AOG.0000265352.61822.1b [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Prime H, Wade M, Browne DT. Risk and resilience in family well-being during the COVID-19 pandemic. Am Psychol 2020;75:631–43. 10.1037/amp0000660 Available: 10.1037/amp0000660 [DOI] [PubMed] [Google Scholar]
- 79. Daugherty JC, Bueso-Izquierdo N, Lara-Cinisomo S, et al. Partner relationship quality, social support and maternal stress during pregnancy and the first COVID-19 Lockdown. Journal of Psychosomatic Obstetrics & Gynecology 2022;43:563–73. 10.1080/0167482X.2022.2101446 Available: 10.1080/0167482X.2022.2101446 [DOI] [PubMed] [Google Scholar]
- 80. Farewell CV, Thayer Z, Paulson J, et al. Fostering resilience among mothers early (FRAME): using growth mixture modeling to identify resources that mitigate perinatal depression. Arch Womens Ment Health 2022;25:451–61. 10.1007/s00737-022-01211-1 Available: 10.1007/s00737-022-01211-1 [DOI] [PubMed] [Google Scholar]
- 81. Kinser P, Jallo N, Moyer S, et al. It’s always hard being a mom, but the pandemic has made everything harder”: A qualitative exploration of the experiences of perinatal women during the COVID-19 pandemic. Midwifery 2022;109. 10.1016/j.midw.2022.103313 Available: 10.1016/j.midw.2022.103313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Ahmad M, Vismara L. The psychological impact of COVID-19 pandemic on women’s mental health during pregnancy: A rapid evidence review. Int J Environ Res Public Health 2021;18:7112. 10.3390/ijerph18137112 Available: 10.3390/ijerph18137112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Black KA, MacDonald I, Chambers T, et al. Postpartum mental health disorders in indigenous women: A systematic review and meta-analysis. J Obstet Gynaecol Can 2019;41:1470–8. 10.1016/j.jogc.2019.02.009 Available: 10.1016/j.jogc.2019.02.009 [DOI] [PubMed] [Google Scholar]
- 84. Nerestant A. If Joyce Echaquan were white, she would still be alive, Quebec coroner says |. CBC News; 2021. Available: https://www.cbc.ca/news/canada/montreal/echaquan-coroner-report-health-care-system-racism-1.6199964 [Google Scholar]
- 85. Lazarus RS, Folkman S. Stress, appraisal, and coping. Springer, 1984. [Google Scholar]
- 86. Blackstock C. The emergence of the breath of life theory. J Soc Work Values Ethics 2011;8:1–16. [Google Scholar]
- 87. Statistics Canada . Median after-tax income, median market income and median government transfers for families and unattached individuals. Statistics Canada; 2022. Available: https://www150.statcan.gc.ca/n1/daily-quotidien/220323/cg-a001-eng.htm [Google Scholar]
- 88. Statistics Canada . Results from the 2016 census: housing, income and residential Dissimilarity among indigenous people in Canadian cities. Statistics Canada; 2019. Available: https://www150.statcan.gc.ca/n1/pub/75-006-x/2019001/article/00018-eng.htm [Google Scholar]
- 89. Lux M. Perfect subjects: race, tuberculosis, and the Qu’Appelle BCG vaccine trial. Can Bull Med Hist 1998;15:277–95. 10.3138/cbmh.15.2.277 Available: 10.3138/cbmh.15.2.277 [DOI] [PubMed] [Google Scholar]
- 90. Mosby I. Administering colonial science: nutrition research and human BIOMEDICAL experimentation in aboriginal communities and residential schools, 1942–1952. Histoire Sociale/Social History 2013;46:145–72. 10.1353/his.2013.0015 Available: 10.1353/his.2013.0015 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data relevant to the study are included in the article or uploaded as online supplemental information. Not applicable.