ABSTRACT
The Bernese periacetabular osteotomy (PAO) is a surgical procedure used to treat hip dysplasia in young adults, but it carries the risk of neurological complications, including injury to the motor ascending branch of the rectus femoris (MABRF). This study aimed to describe anatomical considerations to prevent MABRF injuries during PAO. A cadaveric study was conducted on seven specimens. The original and modified PAO approaches were used, with and without disinsertion of the rectus femoris muscle origin. The femoral nerve was dissected in all specimens from the endopelvic position to the MABRF origin (T-point). The average distance from the anterosuperior iliac spine to the T-point was 10.2 ± 0.4 cm. To protect the MABRF, a safety zone was identified for the osteotome placement during the ischial cut. The osteotome was slid over the joint capsule, deflecting the iliocapsularis muscle medially and distally. This manoeuvre shields the MABRF with the iliocapsularis muscle, reducing the risk of neurological injury. Both the original and modified PAO approaches were considered safe techniques with low risk to the rectus femoris innervation. These findings offer valuable insights for surgeons performing PAO, emphasizing the significance of understanding anatomical relationships and implementing protective measures to enhance patient outcomes and minimize complications. In conclusion, implementing these anatomical considerations can help prevent MABRF injuries during PAO, contributing to safer and more successful surgical interventions for hip dysplasia in young adults.
INTRODUCTION
Periacetabular osteotomy (PAO) is a surgical technique originally described by Ganz et al. to improve biomechanical joint conditions in patients with hip dysplasia and closed triradiate cartilage [1]. It aims to achieve adequate femoral head coverage through acetabular reorientation. Tan et al. published a systematic review of 24 studies with a total of 3471 patients and 3655 hips. The median survival time of PAO was 16 years, extending the longevity of the native hip by 10 and 20 years for 75.9% [95% confidence interval (CI): 74.5–77.5%] and 36.5% (95% CI: 35.0–38.1%) of patients, respectively. Long-term studies have reported good outcomes in 30% of cases at 30 years of follow-up [2, 3]. However, like any surgical procedure, PAO is associated with potential complications, including neurovascular injury, overcorrection or insufficient correction, heterotopic ossification, acetabular necrosis and scar issues [4]. Among the complications, nerve injuries, particularly involving the femoral nerve, have been reported with variable incidences ranging from 0.6% to 2% [5, 6]. A systematic review by Tan et al. [3] showed a rate of lateral femoral cutaneous nerve dysesthesia of 8.2%, transient major nerve palsy (peroneal, sciatic and femoral nerve) of 0.88% and permanent major nerve palsy of 0.05%, but there is a lack of reporting regarding motor ascending branch of the rectus femoris (MABRF) injuries in the literature.
The original technique for Bernese PAO involved partial detachment of the tensor fascia lata from the iliac to the gluteus medius tubercle and complete removal of the rectus femoris muscle to expose the joint capsule and perform the osteotomy [1]. However, a modified technique has been developed by the senior author, which allows for the preservation of the rectus femoris muscle from the anteroinferior iliac spine (AIIS) and enables early and active rehabilitation of patients [7]. In this modified approach, the interval between the rectus femoris and psoas is dissected, medially retracting the lateral rectus femoris (in its direct and reflected portions) and the psoas muscle. When viewing the iliocapsularis muscle, it is retracted, exposing the joint capsule. From this point, as described in the original technique, the bone structures are identified and the corresponding osteotomies are performed. This approach is similar to the technique developed by Khan et al. [8], where the direct head of rectus femoris is identified and the interval between iliopsoas and rectus femoris is developed, leaving rectus femoris attached to the AIIS. The fibres of iliocapsularis are elevated from the hip joint capsule, and dissection is performed between iliopsoas and the hip joint capsule to allow the passage of a specialized osteotome down to the ischium.
During the PAO procedure, structures within the rectus femoris muscle, such as the motor branch (originating from the femoral nerve) and the ascending branch of the lateral femoral circumflex artery, may be at risk of displacement or injury. The femoral nerve provides four motor branches that innervate each of the four muscular bellies of the quadriceps, including the motor branch of the rectus femoris muscle, which is in close proximity to the ascending branch of the lateral femoral circumflex artery.
Sung et al. described a specific target point, referred to as the ‘T-point’, located at the bifurcation of the ascending and descending branches of the motor branch of the rectus femoris muscle [9]. This point is situated at the medial border of the muscle, approximately 6.9 ± 0.7 cm from the inguinal ligament (measured from the origin of the femoral nerve to the superior pole of the patella) and 10.7 ± 1.7 cm from the anterosuperior iliac spine (ASIS), along a line oriented towards the medial condyle of the knee. However, one mechanism that has not been adequately described in the literature is the possibility of femoral nerve injury during the ischial osteotomy. This anatomical cadaveric study aims to describe considerations that can help prevent lesions of the MABRF during PAO.
MATERIALS AND METHODS
An anatomical descriptive study was conducted on seven fresh-frozen cadaveric specimens to investigate the anatomical relationships and measurements relevant to the MABRF muscle during PAO. The cadaveric specimens were selected based on the absence of macroscopic traumatic lesions at the hip level.
Of the seven cadaveric specimens, three were subjected to the original technique of PAO with disinsertion of the origin of the rectus femoris muscle, representing the traditional approach. The remaining four specimens were used to study the extended dissection technique without muscle disinsertion, which represents a modified approach to PAO.
The original technique involved the following steps:
Longitudinal hip incision: a longitudinal incision was made starting from the ASIS to expose the hip joint.
Dissection of fascia and soft tissues: the fascia and overlying soft tissues were carefully dissected to access the underlying structures.
Disinsertion of the rectus femoris muscle: the rectus femoris muscle was dissected and detached from its origin at the AIIS.
Exposure of the joint capsule: the dissection continued to expose the joint capsule and provide access for performing the PAO.
In the extended dissection technique without muscle disinsertion, the procedure involves the following steps:
An anterior longitudinal hip incision is made distally from the ASIS to provide access to the hip joint (Fig. 1).
The fascia surrounding the hip joint is carefully identified (Fig. 2). Additionally, the deep and superficial femorocutaneous nerves adjacent to the sartorius muscle are located. Dissection is performed in the plane between the sartorius muscle and the tensor fascia lata.
Osteotomy is then performed at the level of the ASIS, resulting in the displacement of the sartorius muscle medially (Fig. 3).
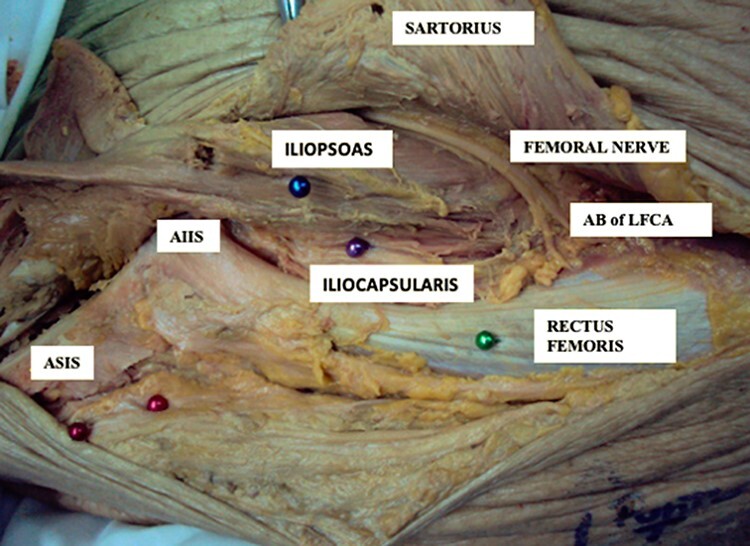
With further dissection, the iliopsoas muscle, surrounding vessels and the femoral nerve are exposed. The motor branch of the rectus femoris muscle is identified (Fig. 4), along with its bifurcation point (referred to as the ‘T-point’) into ascending and descending branches.
The distance between the T-point and the ASIS is measured (Fig. 5).
Additionally, the intersection point between the ascending motor branch of the rectus femoris muscle and the ascending branch of the lateral femoral circumflex artery is identified (Fig. 6).
Fig. 1.
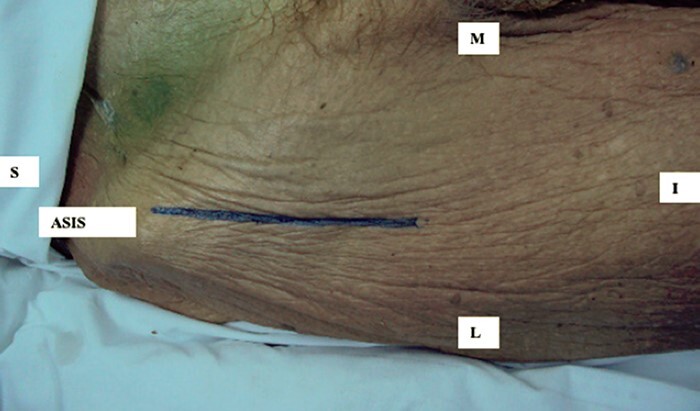
The anterior longitudinal hip incision.
Fig. 2.
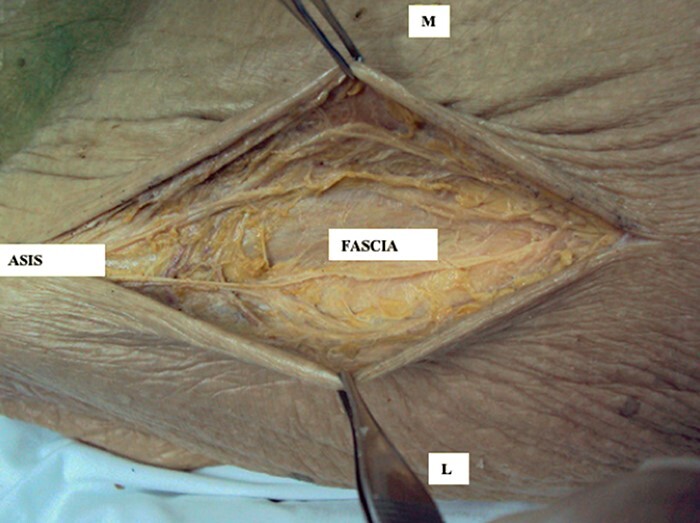
Fascia surrounding the hip joint is identified.
Fig. 3.
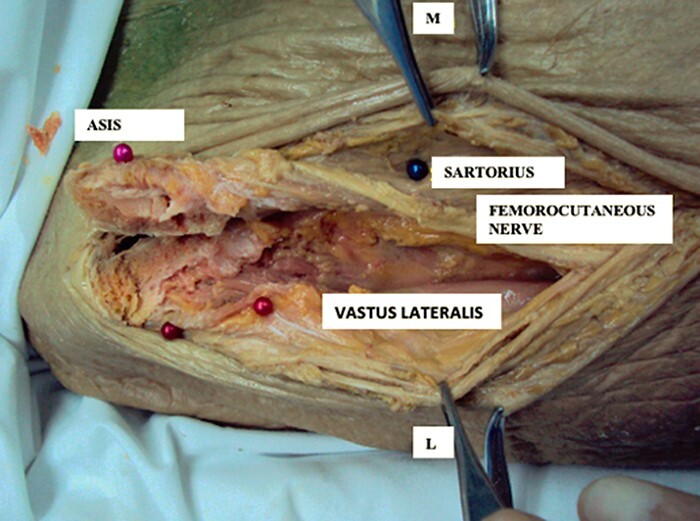
Osteotomy is performed at the level of the ASIS displacing medially sartorius muscle.
Fig. 4.
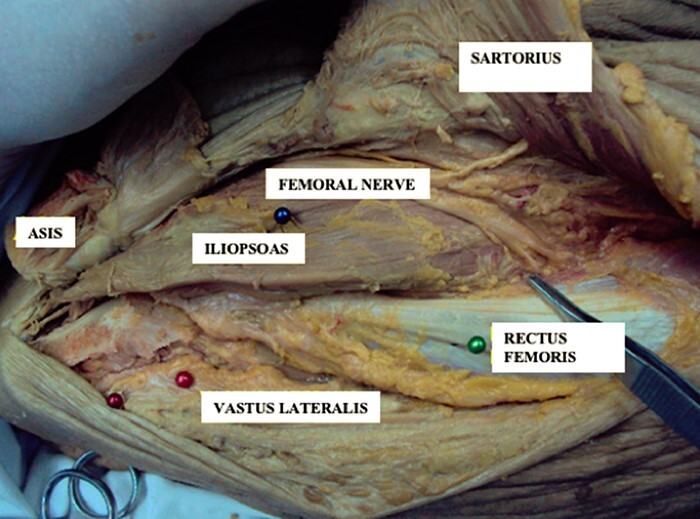
Motor branch of the rectus femoris muscle is identified.
Fig. 5.
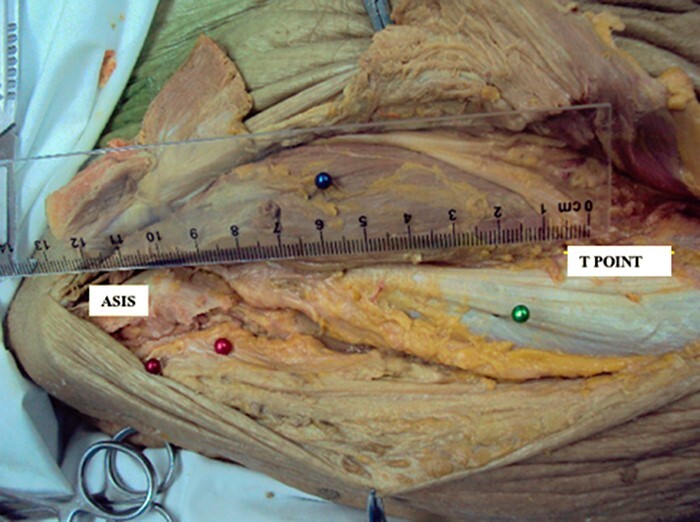
The distance between the T-point and the ASIS is measured.
Fig. 6.
The identification of the point between the ascending motor branch of the rectus femoris muscle and the ascending branch of the lateral femoral circumflex artery.
Finally, the proximity and risk of injury to the motor innervation of the rectus femoris muscle are assessed in both the original and modified surgical techniques of Bernese PAO.
RESULTS
In this anatomical descriptive study, we examined seven fresh-frozen cadaveric specimens to investigate the anatomical variations and protective measures associated with the modified and original techniques of Bernese PAO.
The T-point, representing the bifurcation of the motor branch of the rectus femoris muscle, was consistently located at the interface between the psoas muscle and the rectus femoris muscle in all cadaveric samples. The average distance from the ASIS to the T-point was measured to be 10.2 ± 0.4 cm. This finding provides valuable information regarding the precise location of the motor branch of the rectus femoris muscle in relation to the ASIS during the modified technique of Bernese PAO (Fig. 7).
Fig. 7.
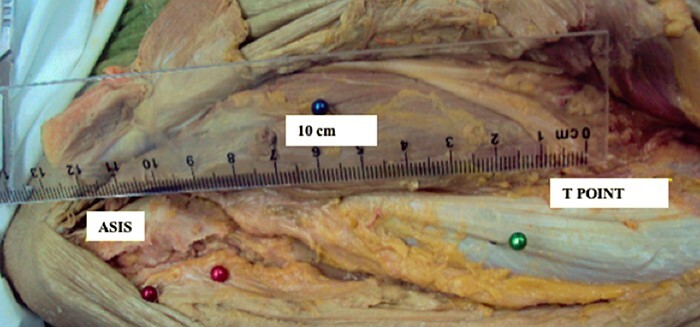
T-point distance.
Additionally, we observed that the motor ascending branch consistently intersected with the ascending branch of the lateral femoral circumflex artery before entering the rectus femoris muscle. This anatomical relationship highlights the importance of understanding the neurovascular structures in the region and their potential vulnerability during surgical procedures (Fig. 8).
Fig. 8.
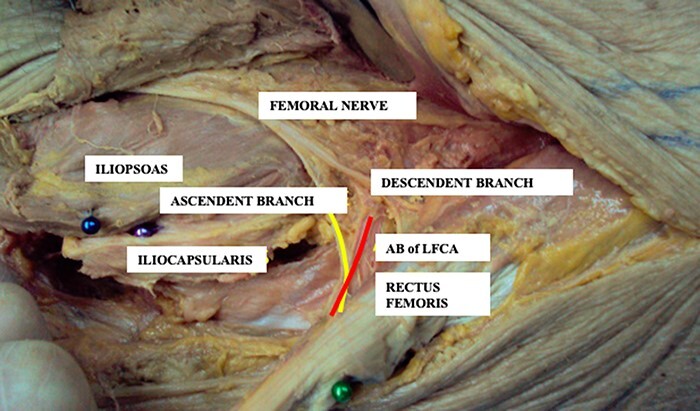
The motor ascending branch consistently intersected with the ascending branch of the lateral femoral circumflex artery before entering the rectus femoris muscle.
With this approach, the bifurcation point of the motor branch of the rectus femoris muscle is distal to the exposed surgical area. To protect the ascending and descending branches of the rectus femoris nerve and the ascending branch of the lateral femoral circumflex artery, we performed dissection of the iliocapsularis muscle and displaced it medially to access the joint capsule. This protective manoeuvre ensured that the neurovascular structures were shielded by the iliacus and iliocapsularis muscles, thus eliminating the risk of injury during the determination of the entry site for the ischial osteotomy (Fig. 9).
Fig. 9.
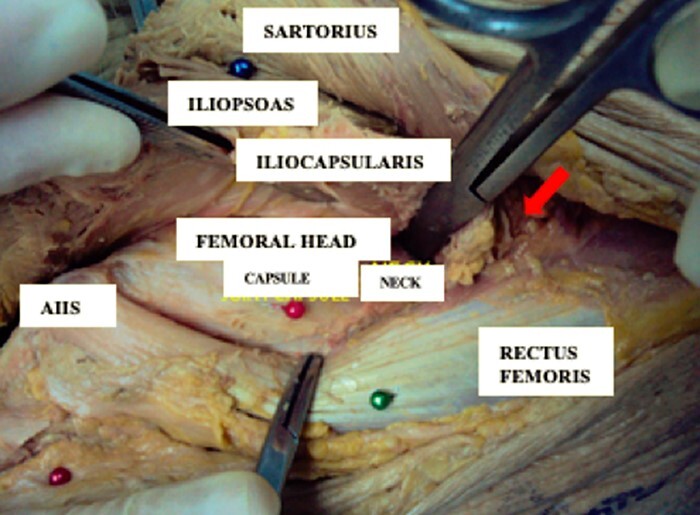
Modified technique—dissection of the iliocapsularis muscle and displaced it medially to access the joint capsule.
In contrast, the original technique of Bernese PAO involves the medial displacement of both the direct and reflex portions of the rectus femoris muscle. This inherent displacement naturally protects the muscular innervation, reducing the risk of neurovascular injury (Fig. 10).
Fig. 10.
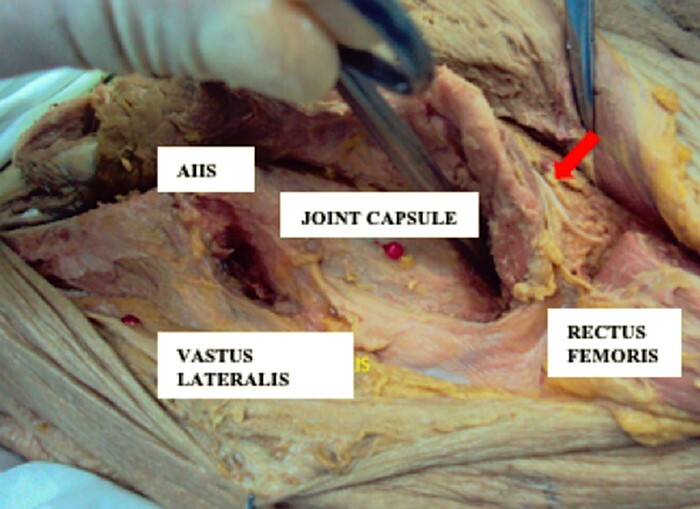
Original technique—medial displacement of both the direct and reflex portions of the rectus femoris muscle.
DISCUSSION
Our study provides valuable insights into the innervation of the rectus femoris muscle and the protective manoeuvres involved in Bernese PAO. The knowledge of precise anatomical landmarks during PAO is crucial for surgeons to ensure a safe and successful procedure.
The ‘T-point’, located at the bifurcation of the motor branch of the rectus femoris muscle, serves as a critical reference point during PAO [9]. Our findings confirm the consistent location of this point, approximately 10.2 ± 0.4 cm from the ASIS, which aligns with previous measurements reported in the literature [10–13].
This anatomical reference provides surgeons with a reliable safety zone of approximately 10 cm from the ASIS to the distal region, enabling precise surgical planning and minimizing the risk of neurovascular injury.
The protection of the rectus femoris muscle innervation is of paramount importance during PAO. In the original technique, the direct and reflex portions of the rectus femoris muscle naturally safeguard the motor branch and the ascending branch of the lateral femoral circumflex artery [1]. Similarly, in the modified technique, the preservation of the iliocapsularis and ilipsoas muscles ensures the protection of these neurovascular structures [7, 11, 12, 14]. According to Khan et al. [8], concern may be raised about passing between the rectus femoris and iliopsoas, wherein the branch of the femoral nerve to the rectus femoris lies. They feel that this branch is not particularly at risk during this approach as the dissection is more medial rather than distal, and the focus is on elevating iliocapsularis and iliopsoas from the hip joint capsule and the superior pubic ramus in order to open up the space down to the ischium. By implementing these protective manoeuvres, surgeons can preserve the innervation and blood supply to the rectus femoris muscle, reducing the risk of postoperative complications and optimizing patient outcomes.
Neurological permanent injuries during PAO, although relatively rare, have been documented in the literature. Our study provides valuable anatomical references that can assist surgeons in navigating these potential risks. For instance, some studies have reported the potential for femoral nerve entrapment during acetabular reorientation or in the presence of a significant gap in the pubic osteotomy [15]. By understanding the anatomical relationship between the rectus femoris muscle and the surrounding structures, surgeons can take appropriate precautions to minimize the risk of nerve entrapment and associated complications, thus further enhancing the safety and efficacy of PAO [16, 17].
The clinical relevance of our findings is further emphasized by the successful application of the modified PAO technique by the senior author, who has performed the procedure in 147 patients without any incidence of neurological injury [18].
The comprehensive understanding of the innervation of the rectus femoris muscle and the practical implications for surgical planning and decision-making make our study a significant contribution to the field.
In conclusion, our study provides crucial insights into the innervation of the rectus femoris muscle and the protective manoeuvres involved in Bernese PAO. The identification of the ‘T-point’ and the understanding of anatomical considerations for neurovascular structures have practical implications for surgical planning and intraoperative decision-making. Surgeons can utilize this knowledge to perform the procedure safely, minimizing the risk of neurovascular complications. Further studies and long-term follow-ups are warranted to evaluate the outcomes and refine surgical techniques to ensure optimal patient outcomes during PAO.
ACKNOWLEDGEMENTS
All authors agree that this work is original and not previously published and presented.
Contributor Information
Joaquín Lara, Clínica MEDS, Hip Unit, Avenida José Alcalde Délano 10581, Santiago 7691236, Chile.
Alan Garín, Intituto Traumatológico, Hip Unit, San Martín 771, Santiago 8340220, Chile; Clínica RedSalud Santiago, Hip Unit, Avenida Libertador Bernardo O’Higgins 4850, Santiago 9190015, Chile.
Selim Abara, Hospital DIPRECA, Hip Unit, Avenida Vital Apoquindo 1200, Santiago 7601003, Chile.
Javier del Río, Clínica MEDS, Hip Unit, Avenida José Alcalde Délano 10581, Santiago 7691236, Chile; Hospital Clínico Mutual de Seguridad, Hip Unit, Avenida Libertador Bernardo O’Higgins 4848, Santiago 9190015, Chile.
Javier Besomi, Clínica Alemana de Santiago, Hip Unit, Avenida Vitacura 5951, Santiago 7650568, Chile; Hospital Clínico San Borja Arriarán, Hip Unit, Avenida Santa Rosa 1234, Santiago 8360160, Chile.
Cristhián Herrera, Clínica Alemana de Santiago, Hip Unit, Avenida Vitacura 5951, Santiago 7650568, Chile; Hospital Clínico San Borja Arriarán, Hip Unit, Avenida Santa Rosa 1234, Santiago 8360160, Chile.
Jaime Cancino, Hospital Clínico Mutual de Seguridad, Hip Unit, Avenida Libertador Bernardo O’Higgins 4848, Santiago 9190015, Chile.
Diego Villegas, Clínica RedSalud Providencia, Hip Unit, Avenida Salvador 100, Santiago 7500995, Chile.
Carlos Tobar, Clínica RedSalud Providencia, Hip Unit, Avenida Salvador 100, Santiago 7500995, Chile.
DATA AVAILABILITY
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to restrictions, e.g. as they contain information that could compromise the privacy of research participants.
FUNDING
No funding was received directly or indirectly to support this investigation.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- 1. Ganz R, Klaue K, Vinh TS et al. A new periacetabular osteotomy for the treatment of hip dysplasias. Clin Orthop Relat Res 1988; 232: 26–36. [PubMed] [Google Scholar]
- 2. Lerch TD, Steppacher SD, Liechti EF et al. One-third of hips after periacetabular osteotomy survive 30 years with good clinical results, no progression of arthritis, or conversion to THA. Clin Orthop Relat Res 2017; 475: 1154–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Tan JHI, Tan SHS, Rajoo MS et al. Hip survivorship following the Bernese periacetabular osteotomy for the treatment of acetabular dysplasia: a systematic review and meta-analysis. Orthop Traumatol Surg Res 2022; 108: 103283. [DOI] [PubMed] [Google Scholar]
- 4. Clohisy JC, Nunley RM, Carlisle JC et al. Incidence and characteristics of complications from femoral nerve palsy following contemporary PAO. Clin Orthop Relat Res 2013; 471: 1702–8. [Google Scholar]
- 5. Yang J, Zhang Z, Cheng H et al. Sciatic and femoral nerve injury among patients who received Bernese peri-acetabular osteotomy. Int Orthop 2019; 43: 573–7. [DOI] [PubMed] [Google Scholar]
- 6. Sierra RJ, Beaule P, Zaltz I et al. Prevention of nerve injury after periacetabular osteotomy. Clin Orthop Relat Res 2012; 470: 2209–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Lara J, Tobar C, Besomi J. Bernese periacetabular osteotomy for hip dysplasia. A modification to original technique and South American perspective. Curr Rev Musculoskelet Med 2014; 7: 337–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Khan OH, Malviya A, Subramanian P et al. Minimally invasive periacetabular osteotomy using a modified Smith-Petersen approach. Bone Joint J 2017; 99: 22–8. [DOI] [PubMed] [Google Scholar]
- 9. Sung KH, Kwon SS, Park MS et al. Anatomical study of the motor branch of the rectus femoris. J Bone Joint Surg Br 2010; 92: 999–1003.20595122 [Google Scholar]
- 10. Novais EN, Kim YJ, Carry PM et al. The Bernese periacetabular osteotomy: is transection of the rectus femoris tendon essential? Clin Orthop Relat Res 2014; 472: 3142–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Peters CL, Erickson JA, Anderson MB et al. Preservation of the rectus femoris origin during periacetabular osteotomy does not compromise acetabular reorientation. Clin Orthop Relat Res 2015; 473: 608–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Podeszwa DA, Tulchin-Francis K, De La Rocha A et al. Rectus-sparing approach to the periacetabular osteotomy in adolescents preserves hip flexion strength. J Child Orthop 2020; 14: 315–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Plante D, Janelle N, Angers-Goulet M et al. Anatomical variants of the rectus femoris motor innervation. J Hip Preserv Surg 2019; 6: 170–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Samuel LT, Munim M, Acuña AJ et al. Modified iliac spine wafer osteotomy for exposure during Bernese periacetabular osteotomy. J Hip Preserv Surg 2019; 6: 421–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kalhor M, Gharehdaghi J, Schoeniger R et al. Reducing the risk of nerve injury during Bernese periacetabular osteotomy: a cadaveric study. Bone Joint J 2015; 97: 636–41. [DOI] [PubMed] [Google Scholar]
- 16. Maranho DA, Williams KA, Millis MB et al. Mid-Term Results of Periacetabular Osteotomy for the Treatment of Hip Dysplasia Associated with Down Syndrome: Minimum Follow-up of Five Years. J Bone Joint Surg Am. 2018; 100: 428–34. [DOI] [PubMed] [Google Scholar]
- 17. Kalhor M, Gharehdaghi J, Leunig M et al. Surgical anatomy of the rectus-sparing approach for periacetabular osteotomy: a cadaveric study. JBJS Essent Surg Tech 2021; 11: e20.00030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Lara J, Villegas D, Besomi J et al. Oblique inguinal incision in Bernese periacetabular osteotomy: surgical technique. J Am Acad Orthop Surg Glob Res Rev 2017; 1: e061. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to restrictions, e.g. as they contain information that could compromise the privacy of research participants.


