ABSTRACT
Arthroscopic iliopsoas fractional lengthening (IFL) is a surgical option for the treatment of internal snapping hip syndrome (ISHS) after failing conservative management. Systematic review. A search of PubMed central, National Library of Medicine (MEDLINE) and Scopus databases were performed by two individuals from the date of inception to April 2023. Inclusion criteria were ISHS treated with arthroscopy. Sample size, patient-reported outcomes and complications were recorded for 24 selected papers. Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines were followed and registered on PROSPERO database for systematic reviews (CRD42023427466). Thirteen retrospective case series, ten retrospective comparative studies, and one randomized control trial from 2005 to 2022 were reported on 1021 patients who received an iliopsoas fractional lengthening. The extracted data included patient satisfaction, visual analogue scale, the modified Harris hip score and additional outcome measures. All 24 papers reported statistically significant improvements in post-operative patient-reported outcome measures after primary hip arthroscopy and iliopsoas fractional lengthening. However, none of the comparative studies found a statistical benefit in performing IFL. Existing studies lack conclusive evidence on the benefits of Iliopsoas Fractional Lengthening (IFL), especially for competitive athletes, individuals with Femoroacetabular Impingement (FAI), and borderline hip dysplasia. Some research suggests IFL may be a safe addition to hip arthroscopy for Internal Snapping Hip Syndrome, but more comprehensive investigations are needed. Future studies should distinguish between concurrent procedures and develop methods to determine if the psoas muscle is the source of pain, instead of solely attributing it to the joint.
INTRODUCTION
Hip pain is a common orthopedic condition that can significantly impact an individual’s quality of life [1]. Internal snapping hip syndrome (ISHS), which presents with a snapping sensation over the hip joint during certain activities, can be a cause of hip pain. The condition occurs when the iliopsoas tendon slides over the iliopectinal eminence or the anterior aspect of the femoral head. Oftentimes, this mechanism can lead to iliopsoas tendinitis. While conservative measures are often used for initial management, surgical intervention may be necessary if these methods fail [2].
Arthroscopic iliopsoas release is a minimally invasive surgical option that involves releasing the iliopsoas tendon to reduce friction and snapping in the hip joint [3]. Despite the well-defined arthroscopic techniques, there still remain several controversial aspects of the procedure. The release of the iliopsoas carries inherent risks and has the potential to heighten instability or lead to intraabdominal fluid extravasation [3]. Surgeons often run into the question of whether to combine iliopsoas releases with their arthroscopic labral repairs when a patient has a concomitant internal snapping hip pathology. In addition, iliopsoas impingement may be found during arthroscopy and there is no consensus of whether to treat the impingement in addition to the original labral pathology [4].
To inform clinical decision-making, this systematic review examines the efficacy and safety of performing an iliopsoas release during hip arthroscopy. The studies reviewed provide insights into the medium and long-term functional outcomes, return to sport rates, and reoccurrence of hip pain following surgical intervention. The results of this systematic review will help optimize patient outcomes in the management of internal snapping hip.
METHODS
This systematic review adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines to identify a final selection of papers for analysis. The plan was registered on PROSPERO before starting the systematic review (CRD42023427466). The inclusion criteria for this study specified patients diagnosed with ISHS who underwent arthroscopic iliopsoas fractional lengthening (IFL). Exclusion criteria encompassed open surgical procedures, previous total hip arthroplasty and studies lacking patient outcome reporting.
To compile the definitive list of papers for inclusion, a comprehensive search was conducted of the PUBMED Central, MEDLINE, and Scopus databases by two independent reviewers. The search strategy employed the following Boolean terms: ‘iliopsoas OR snapping hip OR extra-articular hip’ in the title, resulting in an initial pool of 1103 papers. Subsequently, the inclusion criteria were refined by incorporating ‘arthroscopy OR surgical management’ in any field, reducing the number to 176 papers.
Further application of exclusion criteria involved excluding papers with the keywords ‘arthroplasty OR external snapping’ in the title, which yielded a set of 75 papers. The abstracts of these papers were then scrutinized, leading to the exclusion of various study types such as cadaveric studies, surgical tutorials, commentary, case studies, imaging studies and systematic reviews. Additional exclusion criteria were employed based on the subject matter of the study, resulting in the elimination of papers related to abscesses, hematomas and studies with unreported patient outcome measures. Ultimately, a total of 17 papers met the inclusion and exclusion criteria and were reviewed and analyzed to address the research question of this study.
To augment the analysis, the references of these 17 papers were examined, leading to the identification of 7 additional relevant studies. Consequently, a final set of 24 papers was utilized for the comprehensive analysis of the research question Figure 1.
Fig. 1.
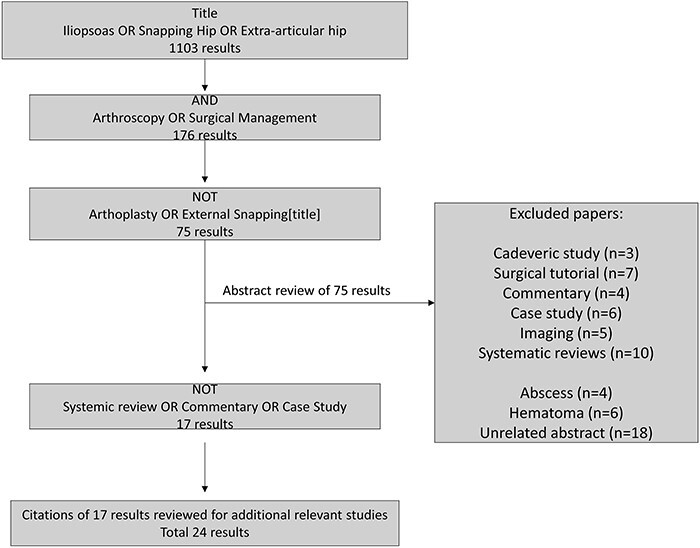
Methodology flow chart.
RESULTS
Paper characteristics
Thirteen papers from 2005 to 2018 reported on case series with cohort sizes ranging from 6 to 67, totaling 374 patients. An additional nine papers from 2016 to 2022 reported retrospective comparative studies with a total of 641 patients in the study groups and 704 patients in the control groups. Additionally, one randomized controlled trial in 2009 and a similar comparative study in 2014 reported on smaller patient groups of two different techniques, with 10 and 9 patients in one and 6 and 14 patients in the other, respectively. Various surgical techniques were examined and listed in Table I. Eighteen papers reported a modified Harris Hip Score (mHHS), ten papers reported a visual analogue scale (VAS), eight papers reported a non-arthritic hip score (NAHS), five papers reported a hip outcome score (HOS), five papers reported a hip outcome score sport scale (HOS-SSS), four papers reported a hip outcome score activities daily living (HOS-ADL), five papers reported patient satisfaction, four papers reported an international hip outcome tool (iHOT) and 3 papers reported a Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC).
Table I.
Study design, sample size and outcome scores
| Study (Authors) | Study design | Sample size | Outcome scores | ||
|---|---|---|---|---|---|
| Ilizaliturri et al. [2005] [14] | Prospective case series [4] | 6 patients and 7 hips | WOMAC score: | ||
| Pre-operative 82.5 Post-operative 91 |
|||||
| Flanum et al. [2007] [15] | Retrospective case series [4] | 6 patients | mHHS: | ||
| Pre-operative 58.3 6 weeks post-operative 62.3 12 weeks post-operative 84.5 24 weeks post-operative 90.3 1 year post-operative 95.7 |
|||||
| Anderson and Keene [2008] [16] | Retrospective case series [4] | 15 athletes (5 competitive and 10 recreational) | mHHS: | ||
| Pre-operative recreational 44.4 52 weeks recreational 96.0 Pre-operative competitive 40.6 52 weeks competitive 96.8 |
|||||
| Ilizaliturri et al. [2009] [17] | Randomized control trial | 19 patients | WOMAC score: | ||
| Group 1 (iliopsoas release at lesser trochanter) | Group 2 (Transcapsular iliopsoas tendon release) | ||||
| Pre-operative 70.1 1 year post-operative 83.7 |
Pre-operative 67 1 year post-operative 83.6 |
||||
| Conteras et al. [2010] [18] | Retrospective case series [4] | 7 patients | mHHS: | ||
| Pre-operative 56.1 12 months post-operative 88.4 (P-value 0.018) 24 months post-operative 87.9 (P-value 0.02) |
|||||
| VAS: | |||||
| Pre-operative 7.7 3 months post-operative 4.3 (P-value 0.051) 6 months post-operative 3.6 (P-value 0.015) 12 months post-operative 2.4 (P-value 0.011) 24 months post-operative 2.4 (P-value 0.011) |
|||||
| Domb et al. [2011] [19] | Retrospective case series [4] | 25 patients | mHHS: | ||
| Post-operative 87.17 | |||||
| HOS-SSS: | |||||
| Post-operative 78.8 | |||||
| HOS-ADL: | |||||
| Post-operative 92.46 | |||||
| Fabricant et al. [2012] [20] | Retrospective case series [4] | 67 patients | Low/normal version | High version | |
| mHHS: | |||||
| Pre-operatively 61.3 ± 16.3 Post-operatively 86.1 ± 14.8 |
Pre-operatively 66.0± 13.5 Post-operatively 76.9± 16.8 |
||||
| P-value 0.031 between two groups post-operatively | |||||
| HOS-ADL: | |||||
| Pre-operative 69.6 ± 18.2 | Pre-operative 66.0 ± 11.9 | ||||
| Post-operative 87.9 ± 14.4 | Post-operative 82.5 ± 18.2 | ||||
| HOS-SSS | |||||
| Pre-operative 50.0± 24.7 | Pre-operative 26.6 ± 21.5 | ||||
| Post-operative 70.7 ± 25.6 | Post-operative 59.4 ± 33.7 | ||||
| Hain et al. [2013] [21] | Retrospective case series [4] | 20 patients | mHHS: | ||
| 79 | |||||
| Garala et al. [2014] [22] | Retrospective case series [4] | 15 patients | NAHS: | ||
| Post-operative 66.4 | |||||
| Ilizaliturri et al. [2014] [23] | Prospective comparative study [2] | 20 patients | Central release | Lesser trochanter release | |
| WOMAC score: | |||||
| Pre-operative 56 ± 13.21 | Pre-operative 46.33 ± 21.83 | ||||
| Post-operative 89.57 ± 3 | Post-operative 89.33 ± 1.36 | ||||
| El Bitar et al. [2014] [24] | Prospective case series [4] | 55 patients | mHHS: | ||
| Pre-operatively 63.3 ± 17.5 | |||||
| 2-year follow-up 84.6 ± 16.5 | |||||
| P-value <0.001 | |||||
| VAS: | |||||
| Pre-operatively 6.0 ± 2.2 | |||||
| 2-year follow-up 2.4 ± 2.1 | |||||
| P-value <0.001 | |||||
| HOS-SSS: | |||||
| Pre-operatively 43.8 ± 25.9 | |||||
| 2-year follow-up 74.4 ± 24.4 | |||||
| HOS-ADL | |||||
| Pre-operatively 61.9 ± 22.0 | |||||
| 2-year follow-up 85.5 ± 18.4 | |||||
| P-value <0.001 | |||||
| NAHS: | |||||
| Pre-operatively 58.2 ± 20.3 | |||||
| 2-year follow-up 84.1 ± 16.5 | |||||
| P-value <0.001 | |||||
| Nelson and Keene [2014] [12] | Retrospective case series [4] | 30 patients | mHHS: | ||
| Pre-operative 43 | |||||
| 6-week post-operative 71 | |||||
| 6-months post-operative 81 | |||||
| 1-year post-operative 84 | |||||
| Hwang et al. [2015] [25] | Retrospective case series [4] | 25 patients | mHHS: | ||
| Pre-operative 65 | |||||
| Post-operative 84 | |||||
| P-value <0.0001 | |||||
| VAS: | |||||
| Pre-operative 6 | |||||
| Post-operative 2 | |||||
| HOS-SSS: | |||||
| Pre-operative 60% | |||||
| Post-operative 82% | |||||
| HOS-ADL: | |||||
| Pre-operative 66% | |||||
| Post-operative 87% | |||||
| Brandenburg et al. [2016] [26] | Retrospective comparative study [3] | 2 groups of 18 patients | NR | ||
| Mardones et al. [2016] [27] | Retrospective case series [4] | 15 patients | mHHS: | ||
| Pre-operative 74.7 | |||||
| Post-operative 95.8 | |||||
| VAS: | |||||
| Pre-operative 5.5 | |||||
| Post-operative 0 | |||||
| Walczak et al. [2017] [9] | Prospective case series [4] | 28 patients | mHHS: | ||
| Group 1 (atrophy of grades 4,3 and 2) | Group 2 (Atrophy of grades 1 and 0) | ||||
| Pre-operative 48.0 | Pre-operative 42.7 | ||||
| Score at 2nd MRA 70.5 | Score at 2nd MRA 64.1 | ||||
| Hartigan et al. [2018] [28] | Retrospective case series [4] | 32 patients | mHHS: | ||
| Pre-operative 68.7 | |||||
| Latest 83.5 | |||||
| P-value <0.001 | |||||
| VAS: | |||||
| Pre-operative 5.6 | |||||
| Latest 1.9 | |||||
| NAHS: | |||||
| Pre-operative 64.9 | |||||
| Latest 86.8 | |||||
| P-value <0.001 | |||||
| HOS-ADL: | |||||
| Pre-operative ADL 71.6 | |||||
| Latest ADL 86.7 | |||||
| P-value ADL <0.001 | |||||
| HOS-SSS: | |||||
| Pre-operative SSS 52.6 | |||||
| Latest SSS 75.8 | |||||
| P-value SSS <0.001 | |||||
| Perets et al. [2018] [6] | Retrospective comparative study [3] | 60 patients | IFL group | Control group (Athletes not requiring IFL) | |
| mHHS: | |||||
| Pre-operative 65.7 ± 12.1 | No significant differences | ||||
| latest 82.4 ± 14.1 | No significant differences | ||||
| P-value <0.001 | No significant differences | ||||
| VAS: | |||||
| Pre-operative 5.7 ± 2.3 | No significant differences | ||||
| latest 2.6 ± 2.4 | No significant differences | ||||
| P-value <0.001 | No significant differences | ||||
| HOS: | |||||
| Pre-operative 44.1 ± 17.7 | No significant differences | ||||
| latest 73.0 ± 24.7 | No significant differences | ||||
| P-value <0.001 | No significant differences | ||||
| NAHS: | |||||
| Pre-operative 64.2 ± 16.6 | No significant differences | ||||
| latest 83.2 ± 15.8 | No significant differences | ||||
| P-value <0.001 | No significant differences | ||||
| Patient satisfaction | |||||
| 7.9 ± 1.9 | |||||
| Maldonado et al. [2018] [29] | Retrospective comparative study [3] | 351 hips IFL and 392 hips in control | IFL group | Control group (Without IFL) | P-value |
| mHHS: | |||||
| 83.2 ± 15.8 | 84.0 ± 16.8 | 0.24 | |||
| HOS: | |||||
| 72.1 ± 26.6 | 73.3 ± 27.1 | 0.69 | |||
| iHot | |||||
| 71.4 ± 25.9 | 72.2 ± 26.1 | 0.41 | |||
| Perets et al. [2019] [7] | Retrospective comparative study [3] | 57 patients in both IFL and control group | IFL group | Control group | |
| mHHS: | |||||
| Pre-operative 64.3 ± 13.6 Latest 84.9 ± 15.8 P-value <0.001 |
Pre-operative 61.6 ± 14.4 Latest 85.9 ± 13.5 P-value <0.001 |
0.298 0.907 |
|||
| VAS: | |||||
| Pre-operative 6.5 ± 2.1 Latest 2.2 ± 2.0 P-value <0.001 |
Pre-operative 5.8 ± 2.1 Latest 2.3 ± 2.3 P-value <0.001 |
0.171 0.965 |
|||
| HOS | |||||
| Pre-operative 47.0 ± 21.6 Latest 75.0 ± 24.0 P-value <0.001 |
Pre-operative 45.9 ± 22.9 Latest 75.9 ± 20.8 P-value <0.001 |
0.784 0.859 |
|||
| NAHS | |||||
| Pre-operative 61.7 ± 18.2 Latest 85.2 ± 15.7 P-value <0.001 |
Pre-operative 65.14 ± 15.75 Latest 82.96 ± 17.97 |
0.436 0.576 |
|||
| Patient satisfaction | |||||
| 8.1 ± 1.7 | 8.2 ± 1.6 | 0.835 | |||
| Meghpara et al. [2020] [4] | Retrospective comparative study [3] | 37 hips in non-IFL group and 87 hips in IFL group | IFL group | Control group | |
| mHHS: | |||||
| Pre-operative 63.61 ± 16.15 Latest 86.10 ± 16.45 |
Pre-operative 63.87 ± 13.06 Latest 86.06 ± 15.31 |
0.53 | |||
| VAS: | |||||
| Pre-operative 4.95 ± 2.40 Latest 2.19 ± 2.61 |
Pre-operative 5.49 ± 2.28 Latest 2.24 ± 2.28 |
||||
| HOS | |||||
| Pre-operative 41.35 ± 23.31 Latest 76.54 ± 25.52 |
Pre-operative 39.96 ± 19.26 Latest 78.14 ± 20.67 |
0.87 | |||
| NAHS: | |||||
| Pre-operative 62.51 ± 18.18 Latest 84.73 ± 17.31 |
Pre-operative 65.14 ± 15.75 Latest 82.96 ± 17.97 |
0.40 | |||
| iHOT | |||||
| 77.54 ± 24.48 | 74.47 ± 21.33 | ||||
| Patient satisfaction | |||||
| 8.01 ± 2.50 | 8.47 ± 1.83 | ||||
| Maldonado et al. [2021] [8] | Retrospective comparative study [3] | 74 hips (29 matched 1:1) | IFL group | Control group | |
| mHHS: | |||||
| Pre-operative 59.24 ± 14.75 Latest 79.79 ± 19.46 P-value <0.0001 |
Pre-operative 62.26 ± 13.41 Latest 87.12 ± 14.63 P-value <0.0001 |
0.418 0.141 |
|||
| VAS: | |||||
| Pre-operative 5.54 ± 2.38 Latest 3.19 ± 2.65 P-value 0.0005 |
Pre-operative 4.84 ± 2.18 Latest 1.99 ± 1.98 P-value <0.0001 |
0.345 0.058 |
|||
| HOS | |||||
| Pre-operative 43.86 ± 26.07 Latest 66.18 ± 29.62 P-value 0.0004 |
Pre-operative 39.86 ± 20.82 Latest 70.52 ± 24.06 P-value <0.0001 |
0.528 0.065 |
|||
| NAHS | |||||
| Pre-operative 59.37 ± 18.91 (52.49–66.25) Latest 78.02 ± 22.96 (68.90–85.66) P-value <0.0001 |
Pre-operative 61.91 ± 16.55 (55.88–67.93) Latest 87.27 ± 12.39 (82.59–91.94) P-value <0.0001 |
0.589 0.065 |
|||
| iHOT | |||||
| 67.23 ± 27.52 (57.21–77.24) | 77.72 ± 19.62 (70.17–85.26) | 0.199 | |||
| Patient satisfaction | |||||
| 7.14 ± 3.32 (5.93–8.35) | 8.42 ± 1.88 (7.70–9.15) | 0.081 | |||
| Matsuda et al. [2021] [10] | Retrospective comparative study [3] | 16 patients (compared to 76 who did not undergo surgery for iliopsoas) | IFL group | Control group | |
| iHOT | |||||
| Pre-operative 35 [24] Post-operative 57 [11] |
Pre-operative psoas involvement without tenotomy 36 [27] Post-operative psoas involvement without tenotomy 67(32) |
Pre-operative without psoas involvement 35 [26] Post-operative without psoas involvement 73 [7] |
0.95 0.02 |
||
| Jimenez et al. [2022] [5] | Retrospective comparative study [3] | 42 athletes in IFL group and 54 matched control athletes | IFL group | Control group | |
| mHHS: | |||||
| Pre-operative 64.2 ± 13.8 Latest 88.4 ± 14.2 P-value <0.001 |
Pre-operative 67.0 ± 14.7 (33.0 to 96.0) Lastest 87.9 ± 15.7 P-value <0.001 |
0.360 0.789 |
|||
| VAS: | |||||
| Pre-operative 5.0 ± 2.4 Latest 2.1 ± 2.2 P-value <0.001 Improvement 3.3 6 3.3 |
Pre-operative 4.9 ± 2.8 Latest 1.9 ± 2.3 P-value <0.001 |
0.892 0.466 |
|||
| HOS: | |||||
| Pre-operative 44.6 ± 20.0 Latest 79.4 ± 26.1 P-value <0.001 |
Pre-operative 51.5 ± 23.8 Latest 81.1 ± 22.5 P-value <0.001 |
0.137 0.795 |
|||
| NAHS: | |||||
| Pre-operative 63.1 ± 16.6 Latest 87.0 ± 15.5 P-value <0.001 |
Pre-operative 68.8 ± 19.8 Latest 87.2 ± 15.9) P-value <0.001 |
0.052 0.899 |
|||
| Patient satisfaction | |||||
| Patient satisfaction 8.6 ±1.7 | Patient Satisfaction 8.1 ± 2.3 | 0.238 | |||
All papers reported primarily on the outcomes following IFL or iliopsoas tenotomy but included various concomitant arthroscopic repairs as well. While the primary focus of the papers was the IFL, additional procedures listed included debridement, acetabuloplasty, femoroplasty, labral repair and capsule repair.
Clinical outcomes
This systematic review provides evidence for the effectiveness of surgical treatments for ISHS, particularly IFL, in alleviating associated symptoms. Patients who underwent IFL in conjugation with other surgical interventions reported improved patient-reported outcome (PRO) scores, pain and snapping resolution and restoration of function. The results of this systematic review provide important clinical considerations for patients undergoing hip arthroscopy with concomitant internal snapping hip such as athletes, patients with femoroacetabular impingement (FAI) and patients with hip dysplasia. In addition, new comparative studies question whether IFL is beneficial for all patients with ISHS.
When looking at athletes, two recent studies by Jimenez et al. and Perets et al. evaluate the use of IFL and the impact on return to sport [5, 6]. In the Jimenez et al. study, athletes with FAI and painful ISHS were identified as a specific patient population that could benefit from intrabursal IFL [5]. The study found that this treatment approach was effective for managing hip pain in these athletes, allowing them to return to their pre-injury level of sport and achieve favorable functional outcomes. The Perets et al. study, on the other hand, focused on athletes with hip flexor pain and found that arthroscopic IFL can be an effective treatment option for this population [6]. These studies suggest that IFL can be used in conjunction with arthroscopic labral repair surgery to manage hip pain in competitive athletes.
Another large population undergoing hip arthroscopy are patients with labral tears and FAI. The Perets and Maldonado study both added IFL to this population. Both of these studies found IFL does not adversely affect clinical outcomes [7, 8]. However, there was no statistical significant improvement in patient outcomes.
Similar to FAI, hip dysplasia is a condition that can affect individuals with ISHS, especially women. It is a condition where the socket of the hip joint is slightly shallow, which can lead to early degeneration of the hip joint and other hip pathologies. Importantly, the degree of hip dysplasia should be carefully considered prior to surgery. In patients with moderate to severe hip dysplasia, arthroscopic treatment may not be sufficient and they may require a periacetabular osteotomy. A recent study by Maldonado et al. focused on the addition of IFL with hip arthroscopy in female patients with borderline dysplasia and painful ISHS. In this population, iatrogenic hip instability is of increased concern because the iliopsoas is an important dynamic anterior stabilizer. In their study, Maldonado performed the IFL with capsular plication to address this instability risk. The Jimenez et al. study reiterated the importance of capsular management in individuals at risk of instability. In their study, Maldonado et al. study found that IFL followed by capsular plication was beneficial to patients in addition to a primary arthroscopic hip procedure. Specifically, the paper found significantly improved patient outcome measures and there were no instances of post-operative complications or reoperations related to IFL. Even with this paper showing positive results, this procedure is highly controversial due to the inherent risk of instability.
While there is positive evidence for IFL, it is important not to overlook the potential complications associated with this procedure. IFL and tenotomy have been linked to damaging surrounding soft tissues, such as the iliopsoas and gluteal tendons, or the lateral femoral cutaneous nerve, according to Walczak et al. [9]. Iliopsoas tendon tears are a common complication of IFL arthroscopy, with some studies reporting rates as high as 20%. Revision surgery and conversion to total hip arthroplasty (THA) may also be necessary in some cases. Additionally, two recent studies by Matsuda et al. (2021) and Meghpara et al. (2020) have highlighted the importance of careful patient selection and judicious use of IFL [4, 10]. Matsuda et al. found that only 1% of their patients undergoing arthroscopic hip surgery had iliopsoas pathology, and only 17% of those with pathology were surgically managed [10]. Meghpara et al. found that IFL did not significantly improve PRO for patients without painful internal snapping, further emphasizing the need for careful patient selection and consideration of alternative treatment options [4]. Thus, iliopsoas tenotomy and IFL should not be routinely used without clear internal snapping hip pathology present pre-operatively.
DISCUSSION
This literature review builds on the findings of two previous studies by Gouveia et al. and Longstaffe et al. in 2021 regarding the effectiveness of arthroscopic release of the iliopsoas tendon (IFL) for the treatment of ISHS [3, 11]. Since the cutoff for these systematic reviews in 2018, six additional level 3 comparative cohort studies have provided significant clinical insights into the use of IFL. Both review papers found that the procedure is an effective treatment for internal snapping hip. However, prior to 2020, no paper focused on IFL concluded that the procedure should be used with caution. Before the Meghpara et al. paper in 2020, all the papers reviewed in this paper emphasized the benefits of IFL and the positive PRO results [4]. However, since the pioneering paper in 2005, many complications have been reported. Table II in this review discusses the complications each paper reported, including the Meghpara et al. paper and a paper by Matsuda et al., which directly reported negative outcomes for the IFL group in their study [4, 10]. An important complication that must be considered is the high rate of muscular atrophy of the iliopsoas which can highly impact athlete’s performance [9].
Table II.
Results and complications
| Study Authors (year) | Results and conclusions | Recurrence/complications |
|---|---|---|
| Ilizaliturri et al. [2005] [14] | No snapping symptoms were present in any patient after surgery of at last follow up. | None |
| Flanum et al. [2007] [15] | None of the patients experienced recurrence of their snapping or pain | At 1-year follow-up 2 patients noted occasional slight pain in their hips. |
| Anderson and Keene [2008] [16] | All patients had resolution of snapping and all returned to sport on average 9 months after surgery | Six patients still experienced pain |
| Ilizaliturri et al. [2009] [17] | No differences were found between the 2 groups | None |
| Contreras et al. [2010] [18] | All patients returned to original or better level of function shortly after operation. All had maximum strength of hip flexion, extension, abduction, and adduction | Two patients had no improvement in pain despite resolution of the snapping. No patient had any post-operative complications. |
| Fabricant et al. [2012] [20] | The purpose of this study was to identify the functional outcomes of high version compared to low/normal version. | Patients with increased femoral anteversion may be at greater risk for inferior clinical outcomes after arthroscopic lengthening. No intraoperative or perioperative complications. |
| Hain et al. [2013] [21] | The majority of post-operative symptomatic patients have atrophy of the iliacus and psoas muscles and distortion and disruption of the iliopsoas tendon. | |
| Garala et al. [2014] [22] | Ten patients reported pain relief after their tenotomy and 5 patients reported no change in pain. For those patients with only temporary relief from injection, psoas tenotomy can provide good long-term pain relief. | In both groups of patients, exercise was the most affected category identified. Symptoms that patients complained of at 49 months after the tenotomy included pain (26%), stiffness (13%), instability (20%), decreased range of motion (20%) and snapping sensation (33%). |
| Ilizaliturri et al. [2014] [23] | Every patient in both groups had an improvement in WOMAC score. | One patient in group 2 presented with recurrence of snapping that required surgical intervention. |
| El Bitar et al. [2014] [24] | Statistically significant improvement in all PROs 81.8% good/excellent satisfaction and 81.8% resolution of painful snapping. | Revision surgery (n = 8; labral retear [n = 6], stiffness [n = 1], heterotopic ossification [n =1]), superficial wound infection (n = 1), perigenital numbness (n = 1) |
| Nelson and Keene [2014] [12] | An arthroscopic release of the iliopsoas tendon at the level of the labrum was effective for alleviating hip pain from labral lesions caused by impingement of the tendon in 23 of 30 patients (77%). | Recurrent snapping (n = 3) requiring iliopsoas bursa injections.Development of avascular necrosis (n = 1)Progression of degenerative joint disease (n = 1)Chronic greater trochanteric bursitis (n = 2) |
| Hwang et al. [2015] [5] | Snapping sound disappeared in 24 out of 25. Improvement in Harris Hip Score Values | Revision surgery (n = 1) for painful snapping |
| Brandenburg et al. [2016] [26] | In the release group, the iliopsoas muscle of the surgical limb was significantly smaller and weaker in the seated position (both P<001) than the contralateral limb | Iliopsoas atrophy with 25% volume loss and a 19% reduction in seated hip flexion strength in (25.3% of IFL group) |
| Mardones et al. [2016] [27] | Statistically significant improvement in patients functional scores (mHHS and Vail Sport Test) | Recurrence of pain 1-year post-operatively (n = 2) |
| Walczak et al. [2017] [9] | A majority of patients (89%) developed iliopsoas (IP) muscle atrophy after labral level IP tenotomies. The lesser trochanteric IP tenotomies did not develop atrophy of the gluteus maxims (n = 1) and vastus lateralis muscles, have chronic IP tendon disruption (n = 2), or develop the severity of IP atrophy (n = 3). | Iliopsoas tendon tear (n = 2), gluteal tendon tear (n = 1), lateral femoral cutaneous nerve injury (n = 1) |
| Hartigan et al. [2018] [28] | Patients with an LCEA of less than 25 and associated painful iliopsoas snapping can be treated by central-compartment IFL and have high satisfaction, improvement in PROs, and improved pain scores without significant progression of osteoarthritis. | Revision (n = 4) for traumatic labral retear, no complications |
| Perets et al. [2018] [6] | All PRO scores demonstrated significant improvements at latest follow-up (P < 0.001). Mean satisfaction was 7.9. No patients converted to arthroplasty. Painful snapping was resolved in 55 athletes (91.7%) | Temporary numbness (n = 1) |
| Maldonado et al. [2018] [8] | The IFL group showed comparable results to the control group with respect to PRO improvement. | Revision surgery (n = 17 in IFL group) and (n = 11 in non-IFL group); conversion to THA (n = 4 in IFL group) and (n = 7 in non-IFL group) |
| Perets et al. [2019] [7] | IFL as part of hip arthroscopy for treatment of FAI and labral tears demonstrated similar favorable improvement, complication rates, and secondary surgeries when compared with a control group that did not undergo IFL | Ten hips (17.5%) required secondary arthroscopy. Three hips (5.3%) required total hip arthroplasty. One case (1.8%) had minor post-operative complications |
| Meghpara et al. [2020] [4] | Both groups experienced significant improvements from pre-surgery to latest follow-up for all recorded PROs. The IFL group compared favorably with the control group for mHHS (86.0 versus 86.1; P = 0.53), NAHS (83.0 versus 84.7; P = 0.40), and HOSSSS (78.1 versus 76.5; P = 0.87). Additionally, iHOT-12, VAS, patient satisfaction, and rates of achieving the minimal clinically important difference for mHHS, NAHS, and HOS-SSS were similar between groups at the latest follow-up. | Study group (IFL): one hip required revision arthroscopy for labral tear and 2 hips converted to THA. 13 hips will persistent PISControl group (non-IFL) 1 hip required revision arthroscopy because of residual FAI |
| Maldonado et al. [2021] [8] | All patients in the study group demonstrated statistically significant improvement from pre-operative to latest follow-up in mHHS, NAHS, HOS-SSS, and VAS scores. Fifty-seven (78.1%) patients achieved or exceeded the minimal clinical important difference (MCID) for mHHS. For HOS-SSS 68.1% met or surpassed the MCID. | Study group 2 secondary arthroscopy and 1 total hip arthroplastyControl group 1 secondary arthroscopy and 1 total hip arthroplasty |
| Matsuda et al. [2021] [10] | Co-afflicted patients treated without tenotomy have similar successful outcomes to patients with primary FAI. | Co-afflicted patients with iliopsoas pathology treated with tenotomy had poorer outcomes compared with controls with FAI without iliopsoas pathology |
| Jimenez et al. [2022] [5] | 89.5% of athletes who attempted to return to sport in IFL were successful. 76.0% of athletes who attempted to return in the non-IFL were successful. e main finding of the present study was that at minimum 5-year follow-up, competitive athletes who underwent primary hip arthroscopy for FAIS and IFL for painful internal snapping hip demonstrated significant improvement in all recorded PROs. | The IFL group underwent 2 revision arthroscopiesThe control group underwent 3 revision arthroscopiesControl group had higher rates of undergoing femorplasties when compared to the IFL group. |
While these studies are essential to consider the possible negative outcomes of IFL, the methodology should be closely analyzed to fully interpret their findings. When analyzing the Meghpara study methodology, the results should only be used to answer the question of how to manage benign iliopsoas impingement, as described by Domb et al. in 2011 [12]. In their methodology, the control group that did not undergo an IFL did not have any pain. Therefore, this study should not be used to compare the overall effectiveness of IFL. Instead, this study should be used to conclude that patients without pain should not be considered good candidates for IFL.
The Matsuda study made even bolder claims against IFL. The tenotomy group (n = 16) was significantly smaller than the iliopsoas group without tenotomy (n = 76) [10]. There could have been selection bias for the tenotomy group, and their pathology could have been worse pre-operatively. The only PRO outcome was iHOT, while many of the studies in this review also included additional PRO such as mHHS, VAS and HOS. While there may be weaknesses in their methodology, both studies clearly show the importance of the patient selection process for success. To achieve optimal patient outcomes, surgeons should carefully assess patients’ suitability for the procedure based on individual needs and circumstances.
Regarding the most agreed-upon technique to treat ISHS, the literature does not state a superior technique. Several studies have used the central compartment technique and lesser trochanter technique, but none of the studies found a statistical difference in PRO. Further randomized clinical trials would be beneficial in this area.
As hip arthroscopy becomes increasingly popular and commonly used, additional techniques may be added to the procedures. Specifically, IFL has been shown to have positive PRO outcomes. Recently, these positive outcomes have been called into question which is exemplified by none of the comparative studies showing a significant improvement compared to the control non-IFL group. These new studies align with the trends reported in the paper by Chen et al. In their study, they reported that 75% of surgeons indicated a decrease in frequency of IFL. This is understandable because the IFL does have risks such as hip flexion weakness [9, 13].
Future research endeavors should prioritize investigating the complications linked to Iliopsoas Impingement (IFL). Additionally, forthcoming studies should aim to establish diagnostic methods that can distinguish between hip pain stemming from the iliopsoas muscle and that originating from the hip joint itself. To date, no studies have reported cases of persistent painful snapping hip after successfully addressing hip joint issues and resolving Femoroacetabular Impingement (FAI). Hence, it is advisable to address painful snapping hip through a two-stage approach. Initially, surgical correction of the hip joint should be pursued. If persistent pain remains, a subsequent surgery involving Iliopsoas Lengthening (IFL) may be considered.
LIMITATIONS
Limitations of this study include the lack of high-quality evidence, primarily relying on retrospective studies with only one randomized controlled trial. Potential publication bias arises from excluding unpublished data, which may affect the comprehensiveness of the review. The varying follow-up durations hinder the assessment of long-term outcomes and complications. Heterogeneous outcome measures make comparisons challenging. Confounding factors and the absence of long-term complications data were not adequately addressed. The study’s generalizability is limited due to the specific populations included in the analysis. These limitations should be considered when interpreting the findings and applying them to clinical practice.
CONCLUSION
Based on the available evidence, it is unclear if IFL provides any additional benefits to patients. Furthermore, there are inherent risks associated with the procedure, such as the potential for iliopsoas muscle atrophy. Therefore, the preferred treatment approach for individuals with internal snapping hip syndrome should prioritize addressing the underlying hip joint issue.
However, if the iliopsoas muscle is indeed responsible for the pain, there might be a role for IFL. Many of the studies in this review showed positive outcomes, including improved patient-reported assessments, pain relief, cessation of snapping sensations, and enhanced functionality across various patient populations. It's crucial to acknowledge, though, that these improvements cannot be solely attributed to IFL alone, as concurrent arthroscopic treatment for coexisting hip pathologies was also performed.
ACKNOWLEDGEMENTS
The authors would like to express their gratitude to the following institutions for their support and contributions to this systematic review:
Liberty University College of Osteopathic Medicine
Department of Orthopaedic Surgery, Virginia Commonwealth University School of Medicine
The authors acknowledge the valuable resources and facilities provided by these institutions, which greatly facilitated the execution of this review. The collaborative efforts of researchers, clinicians and experts from these organizations have significantly enriched the quality and depth of the analysis presented in this systematic review.
Contributor Information
Alexander Baur, 2nd year Medical Student, Liberty University College of Osteopathic Medicine, Lynchburg, VA 24502, USA.
Wesley Lemons, PGY-1, Virginia Commonwealth University School of Medicine, Richmond, VA 23298, USA.
James Satalich, PGY-4, Virginia Commonwealth University School of Medicine, Richmond, VA 23298, USA.
Alexander Vap, Department of Orthopaedic Surgery, Virginia Commonwealth University School of Medicine, Richmond, VA 23298, USA.
Robert O’Connell, Department of Orthopaedic Surgery, Virginia Commonwealth University School of Medicine, Richmond, VA 23298, USA.
DATA AVAIILABILITY
A total of 24 studies met the inclusion criteria and were included in the systematic review. The full-text articles for the included studies were obtained through institutional subscriptions, and the data extracted for analysis were reported in the review. No additional data beyond what is reported in the review is available.
FUNDING
This systematic review was conducted without receiving any external funding or financial support. The research was carried out voluntarily by the authors using their own resources and expertise.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- 1. Calcei JG, Safran MR Evaluation of athletes with hip pain. Clin Sports Med 2021; 40: 221–40. [DOI] [PubMed] [Google Scholar]
- 2. Walker P, Ellis E, Scofield J et al. Snapping hip syndrome: a comprehensive update. Orthop Rev 2021; 13: 25088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Longstaffe R, Hendrikx S, Naudie D et al. Iliopsoas release: a systematic review of clinical efficacy and associated complications. Clin J Sport Med 2020; 31: 522–9. [DOI] [PubMed] [Google Scholar]
- 4. Meghpara MB, Bheem R, Diulus SC et al. An iliopsoas impingement lesion in the absence of painful internal snapping may not require iliopsoas fractional lengthening. Am J Sports Med 2020; 48: 2747–54. [DOI] [PubMed] [Google Scholar]
- 5. Jimenez AE, George T, Lee MS et al. Competitive athletes with femoroacetabular impingement and painful internal snapping treated arthroscopically with intrabursal iliopsoas fractional lengthening: high rate of return to sport and favorable midterm functional outcomes. Am J Sports Med 2022; 50: 1591–602. [DOI] [PubMed] [Google Scholar]
- 6. Perets I, Hartigan DE, Chaharbakhshi EO et al. Clinical outcomes and return to sport in competitive athletes undergoing arthroscopic iliopsoas fractional lengthening compared with a matched control group without iliopsoas fractional lengthening. Arthroscopy 2018; 34: 456–63. [DOI] [PubMed] [Google Scholar]
- 7. Perets I, Chaharbakhshi EO, Mansor Y et al. Midterm outcomes of iliopsoas fractional lengthening for internal snapping as a part of hip arthroscopy for femoroacetabular impingement and labral tear: a matched control study. Arthroscopy 2019; 35: 1432–40. [DOI] [PubMed] [Google Scholar]
- 8. Maldonado DR, Diulus SC, Annin S et al. Borderline dysplastic female patients with painful internal snapping improve clinical outcomes at minimum 2-year follow-up following hip arthroscopy with femoroplasty, labral repair, iliopsoas fractional lengthening, and capsular plication: a propensity-matched controlled comparison. Arthroscopy 2021; 37: 2473–84. [DOI] [PubMed] [Google Scholar]
- 9. Walczak BE, Blankenbaker DG, Tuite MR et al. Magnetic resonance imaging appearance of the hip musculature after arthroscopic labral-level iliopsoas tenotomies. Orthop J Sports Med 2017; 5: 232596711770749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Matsuda D, Kivlan BR, Nho SJ et al. Tenotomy for iliopsoas pathology is infrequently performed and associated with poorer outcomes in hips undergoing arthroscopy for femoroacetabular impingement. Arthroscopy 2021; 37: 2140–8. [DOI] [PubMed] [Google Scholar]
- 11. Gouveia K, Shah A, Kay J et al. Iliopsoas tenotomy during hip arthroscopy: a systematic review of postoperative outcomes. Am J Sports Med 2020; 49: 817–29. [DOI] [PubMed] [Google Scholar]
- 12. Nelson IR, Keene JS Results of labral-level arthroscopic iliopsoas tenotomies for the treatment of labral impingement. Arthroscopy 2014; 30: 688–94. [DOI] [PubMed] [Google Scholar]
- 13. Chen AW, Steffes MJ, Laseter JR et al. How has arthroscopic management of the iliopsoas evolved, and why? A survery of high-volume arthroscopic hip surgeons. J Hip Preserv Surg 2020; 7: 322–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Ilizaliturri VM, Villalobos FE, Chaidez PA et al. Internal snapping hip syndrome: treatment by endoscopic release of the iliopsoas tendon. Arthroscopy 2005; 21: 1375–80. [DOI] [PubMed] [Google Scholar]
- 15. Flanum ME, Keene JS, Blankenbaker DG et al. Arthroscopic treatment of the painful “internal” snapping hip. Am J Sports Med 2007; 35: 770–9. [DOI] [PubMed] [Google Scholar]
- 16. Anderson SA, Keene JS Results of arthroscopic iliopsoas tendon release in competitive and recreational athletes. Am J Sports Med 2008; 36: 2363–71. [DOI] [PubMed] [Google Scholar]
- 17. Ilizaliturri VM, Chaidez C, Villegas P et al. Prospective randomized study of 2 different techniques for endoscopic iliopsoas tendon release in the treatment of internal snapping hip syndrome. Arthroscopy 2009; 25: 159–63. [DOI] [PubMed] [Google Scholar]
- 18. Contreras ME, Dani WS, Endges WK et al. Arthroscopic treatment of the snapping iliopsoas tendon through the central compartment of the hip. J Bone Surg 2010; 92-B: 777–80. [DOI] [PubMed] [Google Scholar]
- 19. Domb BG, Shindle MK, McArthur B et al. Iliopsoas impingement: a newly identified cause of labral pathology in the hip. HSS J 2011; 7: 145–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Fabricant PD, Bedi A, De La Torre K et al. Clinical outcomes after arthroscopic psoas lengthening: the effect of femoral version. Arthroscopy 2012; 28: 965–71. [DOI] [PubMed] [Google Scholar]
- 21. Hain KS, Blankenbaker DG, De Smet AA et al. MR appearance and clinical significance of changes in the hip muscles and iliopsoas tendon after arthroscopic iliopsoas tenotomy in symptomatic patients. HSS J 2013; 9: 236–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Garala K, Prasad V, Jeyapalan K et al. Medium-term and long-term outcomes of interventions for primary psoas tendinopathy. Clin J Sport Med 2014; 24: 205–10. [DOI] [PubMed] [Google Scholar]
- 23. Ilizaliturri VM, Buganza-Tepole M, Olivos-Meza A et al. Central compartment release versus lesser trochanter release of the iliopsoas tendon for the treatment of internal snapping hip: a comparative study. Arthroscopy 2014; 30: 790–5. [DOI] [PubMed] [Google Scholar]
- 24. El Bitar YF, Stake CE, Dunne KF et al. Arthroscopic iliopsoas fractional lengthening for internal snapping of the hip. Am J Sports Med 2014; 42: 1696–703. [DOI] [PubMed] [Google Scholar]
- 25. Hwang D-S, Hwang J-M, Kim P-S et al. Arthroscopic treatment of symptomatic internal snapping hip with combined pathologies. Clin Orthop Surg 2015; 7: 158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Brandenburg JB, Kapron AL, Wylie JD et al. The functional and structural outcomes of arthroscopic iliopsoas release. Am J Sports Med 2016; 44: 1286–91. [DOI] [PubMed] [Google Scholar]
- 27. Mardones R Arthroscopic release of iliopsoas tendon in patients with femoro-acetabular impingement: clinical results at mid-term follow-up. Muscles Ligaments Tendons J 2016; 6: 378–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Hartigan DE, Perets I, Close MR et al. Arthroscopic treatment of iliopsoas snapping in patients with radiographic acetabular dysplasia using iliopsoas fractional lengthening and capsular plication. Arthroscopy 2018; 34: 1841–50. [DOI] [PubMed] [Google Scholar]
- 29. Maldonado DR, Krych AJ, Levy BA et al. Does iliopsoas lengthening adversely affect clinical outcomes after hip arthroscopy? A multicenter comparative study. Am J Sports Med 2018; 46: 2624–31. [DOI] [PubMed] [Google Scholar]


