ABSTRACT
Background:
Breast cancer awareness and early detection are critical for reducing the global burden of the disease. This study assessed breast cancer awareness among women in a high-altitude sub-Himalayan region of North India.
Materials and Methods:
A cross-sectional survey was conducted among women attending the gynecology outpatient clinic in a district hospital. A structured questionnaire was used to collect data on breast cancer knowledge, attitudes, and practices. Participants received posttest health education and counseling on breast cancer prevention strategies.
Result:
The study included 188 participants with a mean age of 31.0 ± 8.8 years. The findings revealed inadequate knowledge about breast cancer among a significant portion of the cohort. Misconceptions about risk factors, such as breastfeeding, oral contraceptive use, and past wrongdoings, were observed. Only half of the participants believed early-stage breast cancer could be effectively treated. Limited awareness of screening methods, including self-breast examination and mammography, was noted. Barriers to breast self-examination (BSE) included considering it unnecessary and lacking knowledge about its execution.
Conclusion:
This study highlights insufficient breast cancer awareness in the high-altitude sub-Himalayan region. Targeted interventions, including health campaigns and electronic media, should be prioritized to improve knowledge and promote early detection practices.
Keywords: Breast cancer awareness, breast self-examination, early detection, high-altitude region, knowledge gaps
Introduction
Cancer is a leading cause of morbidity and mortality worldwide and is responsible for one in six global deaths.[1] In 2018, there were 18.1 million new cases of cancer and 9.6 million deaths. Breast cancer accounted for 11.6% of all cancer cases and 24.2% of cases in women, representing the highest incidence among all cancers and the leading cause of mortality (6.6%) in women worldwide.[2] A meticulous analysis of development indicators and mortality-to-incidence ratios reveals noteworthy disparities across nations, with low–middle-income countries (LMICs) demonstrating lower (albeit increasing) breast cancer incidence rates and higher mortality rates relative to their high-income countries counterparts.[3] Indeed, it is in resource-limited settings where the majority of breast cancer cases and fatalities are anticipated to arise in the coming decades. According to Global Breast Cancer Initiative (GBCI) estimates, LMICs are projected to account for over 60% of newly diagnosed breast cancer cases and 70% of associated fatalities by 2040.[4] This underscores the urgent need for concerted efforts to decrease the impact of the disease.
Breast cancer awareness and early detection play a vital role in enhancing outcomes for individuals affected by breast cancer. The timely identification of breast cancer enables prompt treatment and can substantially enhance survival rates. Nevertheless, there exists considerable variation in awareness and early detection rates across diverse regions and populations. Individuals residing in high-altitude areas face a myriad of challenges in the realm of cancer care. These challenges encompass geographical isolation, elevated levels of poverty and associated financial constraints, scarce healthcare infrastructure,[5] reduced literacy rates, limited educational opportunities, distinct cultural beliefs,[6] and stigmas surrounding cancer.[7]
The purpose of this study was to evaluate the existing knowledge, attitudes, and practices gap regarding breast cancer awareness among women who sought care at the gynecology outpatient clinic situated in a high-altitude sub-Himalayan region of North India. This study bears critical significance for family physicians and primary healthcare providers, as understanding these local contexts is pivotal for them to tailor their clinical approaches effectively.
Materials and Methods
The research was a hospital-based cross-sectional survey conducted at a district hospital in a sub-Himalayan region. Institutional ethics committee approval was obtained before the commencement of the study. To evaluate breast cancer awareness among women visiting the gynecology outpatient clinic, a pretested structured questionnaire was used. The questionnaire was developed and validated based on a thorough literature review and underwent pretesting with a group of 10 women attending the same clinic. It comprised a combination of open-ended and closed-ended questions. The survey was conducted by trained female health workers who were proficient in the local language (Hindi).
The study included all women aged 18 years and above, who visited the gynecology outpatient clinic during the study period. Women who were critically ill or had cognitive impairment were excluded from the study. Following the acquisition of informed consent, women were interviewed using the pretested questionnaire, which included questions on breast cancer awareness, risk factors, warning signs, and screening.
After the completion of the interviews, all study participants received posttest health education sessions on breast cancer. These sessions were delivered in the local language and encompassed a comprehensive range of topics, including breast cancer risk factors, warning signs, self-examination techniques, screening modalities, and available treatment options. To further reinforce the health education provided, participants were furnished with educational materials, such as brochures and pamphlets focusing on breast cancer.
Descriptive statistics was used to summarize and present the data collected from the participants. Nominal quantitative data were displayed as mean ± standard deviation (SD), while proportions (percentages) were used to display the qualitative data.
Results
The study included a total of 188 participants with a mean age of 31.0 ± 8.8 years (range 18–65). The majority of participants were married (95.7%, n = 180) and had lower levels of education (illiterate = 14.8%, n = 28; below graduation = 57.4%, n = 108).
Table 1 provides a comprehensive overview of the knowledge, attitudes, and practices observed among the study participants. A notable portion of the cohort demonstrated insufficient knowledge regarding breast cancer. Family and friends emerged as the primary source of information on breast cancer (62.5%), followed by health professionals (32.5%) and print or electronic media (45%). Only a small minority (5%) relied on alternative sources of information. Notably, within the participant group, 36.1% expressed uncertainty regarding the noncontagious nature of breast cancer, while 27.6% lacked awareness of the potential for early detection, leading to successful treatment outcomes.
Table 1.
Knowledge, attitude, and practice patterns of study participants
| Yes | No | Not sure | ||
|---|---|---|---|---|
| 1 | Have you heard of breast cancer? | 168 (89.4%) | 8 (4.3%) | 12 (6.4%) |
| 2 | Do you have anybody in your family or neighborhood who has/had breast cancer | 16 (8.5%) | 160 (85.1%) | 12 (6.4%) |
| 3 | Is breast cancer a communicable disease? | 0 (0.0%) | 120 (63.8%) | 68 (36.2%) |
| 4 | Can breast cancer be detected early? | 124 (66.0%) | 8 (4.3%) | 56 (29.8%) |
| 5 | Can early detection improve chances of survival? | 136 (72.3%) | 4 (2.1%) | 48 (25.5%) |
| 6 | Is early-stage breast cancer curable? | 100 (53.2%) | 0 (0.0%) | 88 (46.8%) |
| 7 | Breast cancer patients should be isolated | 8 (4.3%) | 180 (95.7%) | - |
| Breast cancer is punishment from God | 20 (10.6%) | 148 (78.7%) | 20 (10.6%) | |
| 8 | Breast cancer patient should not breastfeed | 116 (61.7%) | 64 (34.0%) | 8 (4.3%) |
| 9 | Breast cancer patients can never become mother | 146 (77.7%) | 36 (19.1%) | 6 (3.2%) |
| 10 | Breast cancer patients cannot have normal sexual intercourse | 170 (90.4%) | 8 (4.3%) | 10 (5.3%) |
| 11 | Have you ever performed breast self-examination? | 40 (21.3%) | 148 (78.7%) | - |
| 12 | If you are diagnosed with breast cancer, will you share this news with your family? | 98 (52.1%) | 22 (11.7%) | 68 (36.2%) |
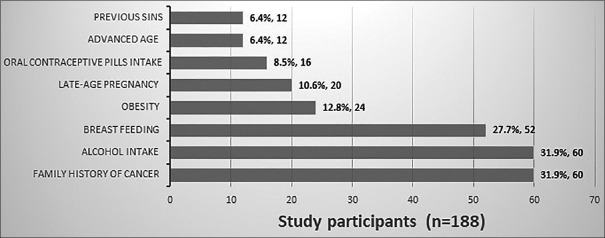
Figure 1 presents the perceived risk factors for breast cancer as reported by the participants. A significant proportion of participants held misconceptions regarding risk factors, including breastfeeding (27.7%), oral contraceptive use (8.5%), and past wrongdoings (6.4%). Among the participants, 55.3% (n = 104) expressed their views on breast cancer reduction strategies. Alarmingly, 73.1% of patients (n = 76) suggested avoiding breastfeeding as a strategy, while other mentioned strategies included increased physical activity (34.6%, n = 36) and the avoidance of alcohol (23.1%, n = 24).
Figure 1.
Perceived risk factors for breast cancer by the study participants
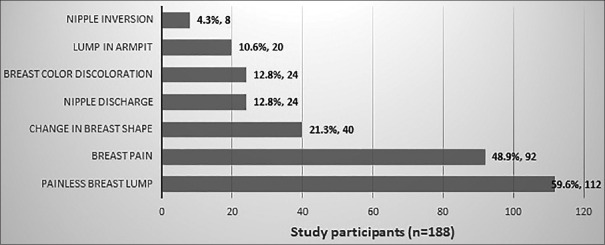
Figure 2 displays the warning signs of breast cancer as perceived by the participants. A majority of participants identified painless breast lump (59.6%, n = 112) and breast pain (48.9%, n = 92) as common warning signs of cancer. However, only a small percentage (4.3%, n = 8) believed that nipple retraction, inversion or nipple discharge could be warning signs.
Figure 2.
Perceived warning signs of breast cancer by the study participants
Regarding beliefs about early-stage breast cancer, only half of the participants (n = 100, 53.2%) subscribed to the notion that it can be effectively treated. However, in the entire participant pool, a substantial 61.7% (n = 116) emphasized the importance of early detection, indicating widespread consensus on the role of recognizing warning signs in facilitating timely diagnosis. Additionally, 24.1% of respondents endorsed self-breast examination as a means of early detection, while a mere 6.9% (n = 8) demonstrated awareness of screening mammography as a screening tool.
Furthermore, 21.3% (n = 40) of participants reported having performed a self-breast examination at least once in their lifetime. Among the remaining respondents (68.1%, n = 128), reasons for not engaging in self-breast examination included considering it unnecessary (71.9%, n = 92), lacking knowledge on how to perform it (21.9%, n = 28), finding it inconvenient or uncomfortable (3.1%, n = 4), and other reasons (6.3%, n = 8).
A significant majority of participants (81.6%) expressed their appreciation and trust in direct health campaigns conducted by healthcare professionals for breast cancer awareness. Additionally, a substantial proportion (60.5%) advocated for the utilization of electronic media, including social media platforms, as an effective means for disseminating information and promoting breast cancer awareness.
Discussion
Breast cancer is a significant global health issue that affects millions of women every year. To effectively combat the rising menace of breast cancer, especially in LMICs, it is crucial to understand the knowledge, attitudes, and practices of the population regarding breast cancer awareness.
The findings of the present study shed light on an important issue concerning the knowledge levels of individuals residing in high-altitude areas regarding breast cancer. The study revealed that a significant proportion of the participants displayed a lack of adequate knowledge about breast cancer. The results indicated that family and friends were the primary sources of information for many individuals. This finding underscores the significance of social networks and interpersonal relationships in shaping an individual’s understanding of health-related matters. It suggests that disseminating accurate and up-to-date information about breast cancer to these influential networks can have a far-reaching impact on raising awareness within the population. Furthermore, the study indicated that print and electronic media also played a role in disseminating information about breast cancer to the participants. This finding highlights the potential of mass media channels, such as newspapers, magazines, television, and the Internet, in reaching a wide audience and raising awareness about breast cancer. There is definitely an unmet need for accurate and evidence-based information to be effectively communicated through these channels to ensure that the population receives reliable and trustworthy information. Mobile phone usage, particularly for accessing Internet-based health information, can play a significant role in improving cancer awareness among the population. They can be utilized as valuable sources for delivering cancer awareness tools and interventions to reach a wider audience and promote prevention and early detection efforts.[8]
The study identified several misconceptions and gaps in knowledge regarding breast cancer risk factors. A significant proportion of participants held misconceptions about breastfeeding, oral contraceptive use, and past wrongdoings as risk factors. This underscores the need for targeted educational interventions to address and correct such misconceptions. Furthermore, the study found that a majority of participants believed avoiding breastfeeding to be a breast cancer reduction strategy, despite evidence suggesting its protective effect.
The participants displayed a reasonable understanding of common warning signs of breast cancer, such as painless breast lump and breast pain. However, there was a lack of awareness regarding nipple retraction or inversion or nipple discharge as warning signs. This emphasizes the importance of enhancing knowledge about the diverse range of warning signs associated with breast cancer.
While only half of the participants believed that early-stage breast cancer can be effectively treated, a substantial majority recognized the importance of early detection in facilitating timely diagnosis. However, awareness of screening methods, such as self-breast examination and screening mammography, was limited. The study revealed that a minority of participants (21.3%) reported having performed breast self-examination (BSE) at least once in their lifetime. Barriers to engaging in self-breast examination included considering it unnecessary, lacking knowledge on how to perform it, finding it inconvenient or uncomfortable, and other reasons. This highlights the need for targeted educational campaigns to address misconceptions, provide clear instructions, and alleviate concerns surrounding self-breast examination. BSE is a cost-effective and minimally invasive screening method for early detection of breast cancer. Education programs and community outreach efforts have shown promising results in increasing BSE practice rates. Studies have demonstrated the effectiveness of BSE training in improving knowledge and practice rates. BSE should be considered a suitable screening tool, particularly in LMICs due to its affordability and potential to contribute to a decline in breast cancer mortality rates.
Participants expressed trust in direct health campaigns conducted by healthcare professionals and emphasized the potential of electronic media, including social media platforms, for disseminating information and promoting breast cancer awareness. These findings underscore the importance of utilizing diverse communication channels to reach a wider audience and improve breast cancer awareness among the population. Effective communication strategies[9] should be developed to reach women with low levels of education and literacy, as these women are particularly vulnerable to inadequate awareness and late-stage diagnosis, resulting in poor outcomes. Community health workers, who play a crucial role in delivering healthcare services in rural areas, could be trained to deliver breast cancer education and promote breast cancer screening among women in these regions. Moreover, a periodic clinical breast examination by primary health workers may result in a significant 30% reduction in breast cancer-related mortality among women aged 50 and older.[10]
The study’s findings are crucial for family physicians and healthcare providers in hilly regions. Understanding local knowledge gaps allows them to create targeted awareness campaigns using social networks and media. With this knowledge, they can actively raise cancer awareness, dispel cancer myths and misconceptions, and promote early cancer detection, significantly impacting breast cancer outcomes in their communities.
Conclusion
This study highlights the urgent need for breast cancer awareness-raising programs in high-altitude areas of sub-Himalayan regions. The findings highlight the presence of knowledge gaps, misconceptions, and limited awareness of screening methods, including BSE, among the participants. The development of effective communication strategies to reach women with low levels of education and literacy is crucial for promoting breast cancer screening and early detection. Targeted educational interventions, utilizing a variety of communication channels, are essential to address these gaps and improve breast cancer awareness, with a specific focus on empowering women to perform regular and effective BSE. Failure to address these issues will result in continued high rates of morbidity and mortality due to breast cancer in these regions. Future research should focus on evaluating the effectiveness of specific interventions in enhancing knowledge, promoting early detection practices, and dispelling misconceptions related to breast cancer.
Data availability
The data that support the findings of this study are contained in the published article.
Authors contribution
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this manuscript, take responsibility for the integrity of the work, and have given final approval for the version to be published.
Ethics approval and consent to participate
The study was approved by the institutional ethics committee. All participants in the research provided voluntary explicit informed written consent before their inclusion in the study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209–49. doi: 10.3322/caac.21660. [DOI] [PubMed] [Google Scholar]
- 2.Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61:69–90. doi: 10.3322/caac.20107. [DOI] [PubMed] [Google Scholar]
- 3.Lima SM, Kehm RD, Terry MB. Global breast cancer incidence and mortality trends by region, age-groups, and fertility patterns. EClinicalMedicine. 2021;38:100985. doi: 10.1016/j.eclinm.2021.100985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Anderson BO, Ilbawi AM, Fidarova E, Weiderpass E, Stevens L, Abdel-Wahab M, et al. The global breast cancer initiative: A strategic collaboration to strengthen health care for non-communicable diseases. Lancet Oncol. 2021;22:578–81. doi: 10.1016/S1470-2045(21)00071-1. [DOI] [PubMed] [Google Scholar]
- 5.Global Burden of Disease Cancer Collaboration. Fitzmaurice C, Dicker D, Pain A, Hamavid H, Moradi-Lakeh M, et al. The Global Burden of Cancer 2013. JAMA Oncol. 2015;1:505–27. doi: 10.1001/jamaoncol.2015.0735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kaul P, Kumar R, Singh MP, Garg PK. Social taboos: A formidable challenge in cancer care. BMJ Case Rep. 2021;14:e236095. doi: 10.1136/bcr-2020-236095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Garg PK. What plagues cancer: Does it spread? Oncologist. 2015;20:1099. doi: 10.1634/theoncologist.2014-0346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yadav K, Hariprasad R, Gupta R, Upadhayay S, Sharma V, Kumari M, et al. Cancer awareness &its association with demographic variables &mobile phone usage among the rural population of a district in north India. Indian J Med Res. 2022;156:94–103. doi: 10.4103/ijmr.IJMR_3145_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kaul P, Choudhary D, Garg PK. Deciphering the optimum doctor-patient communication strategy during COVID-19 pandemic. Indian J Surg Oncol. 2021;12((Suppl 2)):240–1. doi: 10.1007/s13193-021-01301-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mittra I, Mishra GA, Dikshit RP, Gupta S, Kulkarni VY, Shaikh HKA, et al. Effect of screening by clinical breast examination on breast cancer incidence and mortality after 20 years: Prospective, cluster randomised controlled trial in Mumbai. BMJ. 2021;372:n256. doi: 10.1136/bmj.n256. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are contained in the published article.