ABSTRACT
Purpose/Background:
Nasal obstruction is a significant issue influencing the patient’s quality of life. Chronic nasal obstruction is frequently associated with other symptoms such as headache, sleep disturbance, and daytime sleepiness. This study aims to investigate the prevalence of nasal obstruction in Saudi Arabia and examine its effect on patients’ quality of life.
Methods:
This is a cross-sectional study conducted in Saudi Arabia. Data were collected using a self-administered combination of two previously validated questionnaires (the NOSE scale and the WHOQOL-BREF) translated into Arabic. The Mann–Whitney test was used to investigate the association between nasal obstruction prevalence and the participants’ QOL.
Results:
The study included 1039 participants from different regions of Saudi Arabia. The prevalence of nasal obstruction was 60.3% among the participants. Several factors significantly affected the prevalence of nasal obstruction, including sex, suffering from a chronic disease, having a family member with nasal obstruction, and using medications (P < 0.001 for all factors). A better score was shown in the four domains of the WHOQOL-BREF questionnaire by the participants who had no nasal obstruction: the physical health domain, psychological health, social relationships, and environment (P < 0.001 for all factors).
Conclusions:
Quality of life is affected by nasal obstruction. The subjective assessment is essential in evaluating the severity of nasal obstruction disease. It is recommended that healthcare providers use subjective tools combined with objective tools to assess the degree of nasal obstruction severity.
Keywords: Nasal obstruction, NOSE scale, quality of life, Saudi Arabia
Introduction
Nasal obstruction is a feeling of discomfort that may be associated with other symptoms such as headache, irregular sleep, and a poor health-related quality of life (QOL).[1,2]
The subjective assessment of obstructive nasal symptoms can be conducted using the nasal obstruction symptom evaluation (NOSE) scale[3] and the WHOQOL-BREF scale.[4,5]
The prevalence of nasal obstruction has not been extensively studied in the general population. It has been assumed that up to one-third of the population has some nasal obstruction due to septal deviation.[6] In Sweden, one-quarter of surveyed people suffered from nose complaint, including obstruction, sneezing, and discharge.[7] In French patients with rhinosinusitis, nasal obstruction was seen in 66% of patients.[8] In 2018, a study conducted in Northern Saudi Arabia revealed that nasal obstruction is prevalent during the period of 2014 to 2016, generally as the presentation of having deviated nasal septum.[9]
Prior research has shown a reduction in quality of life (QoL) with nasal obstruction disorders. Besides, relieving of nasal obstruction has led to substantial improvement in QoL (QoL).[10]
In Saudi Arabia, the prevalence of nasal obstruction and its effect on patients’ quality of life is not clearly defined. Therefore, this study aims to investigate the prevalence of nasal obstruction in Saudi Arabia and to examine the nasal obstruction effect on the QOL of patients.
Subjects and Methods
Study design
This was a cross-sectional, observational, population-based, survey-based study. The data were collected between August and September 2022 using a Google form that was shared with the population in Saudi Arabia through social media platforms (e.g. Twitter, Instagram, Linked-in, and WhatsApp).
Study population
All adult populations from Saudi Arabia were eligible to participate in this study.
Inclusion criteria: Adult males and females living in Saudi Arabia.
Exclusion criteria: Adults not welling to participate in the study.
Sample size
It was calculated using the Raosoft online sample size calculator; considering a marginal error of 5%, a confidence level of 95%, and maximum uncertainty (50% of positive responses), a minimum of 377 participants from the Kingdom of Saudi Arabia were needed to be included in this study.
Data collection
Data were collected using a self-administered combination of two previously validated Arabic questionnaires (the NOSE scale[11,12] and the WHOQOL-BREF[5,13]).
Nasal Obstruction Symptom Evaluation Scale (NOSE): The NOSE scale was designed to evaluate the nasal obstruction’s influence on the quality of life. It contains five items scored with a 5-point scale (0–4), in which 0 represents “not a problem” and 4 “severe problem.” The total score of NOSE is calculated by multiplying the raw score by 5, ranging from 0 to 100.[11] The internal consistency of the Arabic version of the NOSE questionnaire was assessed using Cronbach’s test, which showed an α value of 0.932 in patients and 0.911 in the control individuals, confirming good internal consistency of the scale.[12]
WHO’s QOL scale (WHOQOL-BREF): This instrument is derived from the WHOQOL-100. The WHOQOL-BREF questionnaire contains two items from the Overall QOL and General Health and 24 items of satisfaction that are divided into four domains: Physical health with seven items (Domain1), psychological health with six items (Domain2), social relationships with three items (Domain3), and environmental health with eight items (Domain4). The point values for the questions were summed corresponding to each domain as (1 = Not at all, 2 = Not much, 3 = Moderately, 4 = A great deal, and 5 = Completely) except for questions 3, 4, and 26, which are negatively phrased items. Then, the scores were transformed to a 0- to 100-point interval according to guidelines.[5] The finalized version of the questionnaire was pretested among 20 participants to solve any obstacles. The internal consistency of the Arabic WHO-QOL BREF questionnaire was tested in a previous study where good internal consistency (Cronbach’s α =0.92) for the questionnaire, and its four domains was observed.[13]
Statistical analysis
The normality of numerical data was tested. If normally distributed, data were statistically described in terms of mean ± SD, whereas the median and IQR were used to describe categorical data. Frequencies (number of participants) and valid percentages were used for categorical variables.
Chi-square or Fisher’s exact test was performed for categorical variables between the subgroups. P values less than 0.05 were considered statistically significant. The Mann–Whitney test was used to investigate the association between nasal obstruction prevalence and the participants’ QOL. Furthermore, the Kruskal–Wallis test was used to explore the association between nasal obstruction severity and the participants’ QOL. All statistical calculations were performed using the SPSS program (IBM Corp, Armonk, NY, USA), release 26 for Microsoft Windows.
Results
In total, 1039 subjects from different regions in Saudi Arabia filled out the questionnaire, and their complete characteristics are shown in Tables 1-3. The largest proportion (31.6%) were from the northern region, followed by the southern region (17.8%), the western region (17.4%), the eastern region (16.6%), and the central region (16.5%). The majority of the participants who completed the questionnaire were Saudi (94.1%), females (64.5%), aged from 18 to 30 years (63%), and had a family member with nasal obstruction (41.5%). Approximately 79.8% of the participants had a university degree or higher, about half were single, and 66.1% suffered from chronic diseases. Out of 33.8% of the participants mentioned that they had a nasal obstruction, and nearly half of the participants reported using medications to treat several diseases.
Table 1.
Socio-demographic characteristics of the participants
| Parameters | Category | Count (n=1039) | Percentage |
|---|---|---|---|
| Age (years) | 18 to 30 | 655 | 63 |
| 31 to 40 | 162 | 15.6 | |
| 41 to 50 | 143 | 13.8 | |
| 51 to 60 | 62 | 6.0 | |
| >60 | 17 | 1.6 | |
| Gender | Female | 670 | 64.5 |
| Male | 369 | 35.5 | |
| Nationality | Non-Saudi | 61 | 5.9 |
| Saudi | 978 | 94.1 | |
| Marital status | Divorced | 33 | 3.2 |
| Married | 390 | 37.5 | |
| Single | 602 | 57.9 | |
| Widowed | 12 | 1.3 | |
| Educational level | Primary school | 12 | 1.2 |
| Preparatory school | 15 | 1.4 | |
| Secondary school | 183 | 17.6 | |
| University or higher | 829 | 79.8 | |
| Employment status | Non-employed | 179 | 17.2 |
| Retired | 47 | 4.5 | |
| Student | 418 | 40.2 | |
| Employed | 395 | 38 | |
| Medication use | Using medications | 579 | 55.7 |
| Not using medications | 460 | 44.3 |
Table 3.
Comorbidities among participants
| Parameters | Category | Count (n=1039) | Percentage |
|---|---|---|---|
| Have asthma | Yes | 79 | 7.6 |
| No | 960 | 92.4 | |
| Have cardiovascular diseases | Yes | 11 | 1.1 |
| No | 1028 | 98.9 | |
| Have hepatic diseases | Yes | 5 | 0.5 |
| No | 1034 | 99.5 | |
| Have hyperlipidemia | Yes | 37 | 96.4 |
| No | 1002 | 3.6 | |
| Have skin sensitivity | Yes | 58 | 5.6 |
| No | 981 | 94.4 | |
| Have diabetes mellitus | Yes | 78 | 7.5 |
| No | 961 | 92.5 | |
| Have hypertension | Yes | 87 | 91.6 |
| No | 952 | 8.4 | |
| Have thyroid gland disorders | Yes | 44 | 4.2 |
| No | 995 | 95.8 | |
| Have kidney diseases | Yes | 11 | 1.1 |
| No | 1028 | 98.9 | |
| Have cancer | Yes | 11 | 1.1 |
| No | 1028 | 98.9 | |
| Have psychological disorders | Yes | 23 | 2.2 |
| No | 1016 | 97.8 | |
| Have immunodeficiency disease | Yes | 9 | 0.9 |
| No | 1030 | 99.1 |
Table 2.
Disorders related to nasal obstruction among participants
| Parameters | Category | Count (n=1039) | Percentage |
|---|---|---|---|
| Have allergic rhinitis | Yes | 321 | 30.9 |
| No | 718 | 69.1 | |
| Have Chronic sinusitis | Yes | 166 | 16 |
| No | 873 | 84 | |
| Suffering from nasal obstruction | Yes | 351 | 33.8 |
| No | 688 | 66.2 |
Participants reported the findings associated with nasal obstruction, congestion (as a result of allergic rhinitis, sinusitis, or cold and flu episodes), and deviated septum were the major causes of nasal obstruction (72.4% and 28.8%, respectively). More details are described in Table 4.
Table 4.
Findings associated with nasal obstruction
| Parameters | Count (n=1039) | Percentage |
|---|---|---|
| Nasal polyps | 11 | 3.1 |
| Adenoids hypertrophy | 54 | 15.4 |
| Inferior turbinate hypertrophy | 38 | 10.8 |
| Nasal congestion | 254 | 72.4 |
| Deviated septum | 101 | 28.8 |
After interpreting the results of the NOSE scale questionnaire, it was estimated that the prevalence of nasal obstruction was 60.3% among the participants. Moreover, regarding nasal obstruction severity, approximately half of the participants had moderate (30 to 50) and severe (>50) nasal obstruction. Full details are in Figures 1 and 2.
Figure 1.
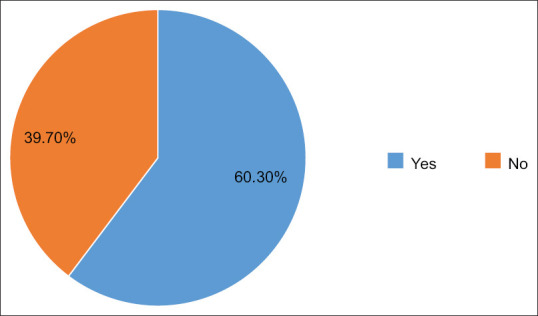
Prevalence of nasal obstruction
Figure 2.
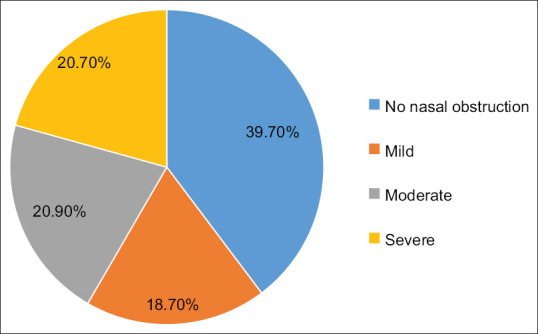
Severity of nasal obstruction
By comparing the associated factors with the prevalence of nasal obstruction [Table 5], no statistically significant differences were found except for male gender, having a chronic disease, using concomitant medications, and having a family member with nasal obstruction that was associated with a significantly higher prevalence of nasal obstruction (P < 0.001).
Table 5.
Factors affecting the prevalence of nasal obstruction
| Factors | Nasal obstruction | P | ||
|---|---|---|---|---|
|
|
|
|||
| Categories | No nasal obstruction (≤10) | Nasal obstruction (15–100) | ||
| Sex | Male | 111 (30.1) | 258 (69.9) | <0.001* |
| Female | 302 (45.1) | 368 (54.9) | ||
| Education | University degree or higher | 328 (39.7) | 501 (60.4) | 0.810 |
| Doesn’t hold a university degree | 85 (40.5) | 125 (59.5) | ||
| Age | ≤50 years | 383 (39.9) | 577 (60.1) | 0.737 |
| >50 years | 30 (38) | 49 (62) | ||
| Nationality | Saudi | 389 (39.8) | 589 (60.2) | 0.947 |
| Non-Saudi | 24 (39.3) | 37 (60.7) | ||
| Marital status | Un-married | 249 (38.4) | 400 (61.6) | 0.240 |
| Married | 164 (42.1) | 226 (57.9) | ||
| Employment status | Non-employed | 266 (41.3) | 378 (58.7) | 0.191 |
| Employed | 147 (37.2) | 248 (62.8) | ||
| Have chronic diseases | No | 319 (46.4) | 368 (53.6) | <0.001* |
| Yes | 94 (26.7) | 258 (73.3) | ||
| Anyone from your family has nasal obstruction disease | No | 318 (52.3) | 290 (47.7) | <0.001* |
| Yes | 95 (22) | 336 (78) | ||
| Medication use | No | 303 (52.3) | 276 (47.7) | <0.001* |
| Yes | 110 (23.9) | 350 (76.1) | ||
By comparing the participants’ answers regarding having nasal obstruction or not with the results of the NOSE Scale, approximately half of the participants who reported they did not have nasal obstruction actually had a nasal obstruction on NOSE Scale (43.6%).
By comparing the total score of the four domains of quality of life with the prevalence of nasal obstruction, all participants who did not have nasal obstruction had a higher score than those who had nasal obstruction (P < 0.001). Full details are described in Table 6.
Table 6.
Nasal Obstructive prevalence and Quality of Life domains
| Factors Category |
Total score of | P | ||
|---|---|---|---|---|
|
| ||||
| Median | Interquartile Range | |||
| Domain 1 (Physical health) | No nasal obstruction | 81 | 31 | <0.001* |
| Nasal obstruction | 63 | 27 | ||
| Domain 2 (Psychological health) | No nasal obstruction | 75 | 25 | <0.001* |
| Nasal obstruction | 63 | 31 | ||
| Domain 3 (Social relationships) | No nasal obstruction | 75 | 44 | <0.001* |
| Nasal obstruction | 56 | 37 | ||
| Domain 4 (Environmental health) | No nasal obstruction | 75 | 25 | <0.001* |
| Nasal obstruction | 63 | 25 | ||
By comparing the severity of nasal obstruction with the total score of the four domains of quality of life, there were significant differences among the four domains of the quality of life with the nasal obstruction degree (P < 0.001), Table 7.
Table 7.
Nasal obstruction severity and quality-of-life domains
| Factors Category |
Total score of | P | ||
|---|---|---|---|---|
|
| ||||
| Median | Interquartile range | |||
| Domain 1 (Physical health) | No nasal obstruction | 81 | 31 | <0.001* |
| Mild nasal obstruction | 69 | 32 | ||
| Moderate nasal obstruction | 56 | 81 | ||
| Severe nasal obstruction | 56 | 25 | ||
| Domain 2 (Psychological health) | No nasal obstruction | 75 | 25 | <0.001* |
| Mild nasal obstruction | 69 | 87 | ||
| Moderate nasal obstruction | 56 | 31 | ||
| Severe nasal obstruction | 56 | 25 | ||
| Domain 3 (Social relationships) | No nasal obstruction | 75 | 44 | <0.001* |
| Mild nasal obstruction | 69 | 31 | ||
| Moderate nasal obstruction | 56 | 38 | ||
| Severe nasal obstruction | 56 | 37 | ||
| Domain 4 (Environmental health) | No nasal obstruction | 75 | 25 | <0.001* |
| Mild nasal obstruction | 69 | 25 | ||
| Moderate nasal obstruction | 63 | 31 | ||
| Severe nasal obstruction | 63 | 25 | ||
Discussion
This study aimed to assess the prevalence of nasal obstruction in Saudi Arabia and to investigate the nasal obstruction effect on patients’ quality of life. The study enrolled 1039 participants from diverse regions of Saudi Arabia and revealed a prevalence of nasal obstruction at 60.3% among the participants. Noteworthy factors influencing the occurrence of nasal obstruction included gender, presence of a chronic illness, familial history of nasal obstruction, and medication use (P < 0.001 for all factors). Participants without nasal obstruction displayed superior scores across four domains of the WHOQOL-BREF questionnaire: physical health, psychological health, social relationships, and environment (P < 0.001 for all factors), which indicated that nasal obstruction detrimentally impacts individuals’ quality of life. Subjective evaluations play a pivotal role in assessing the severity of nasal obstruction. It is advisable for healthcare providers to employ a combination of subjective and objective tools to gauge the degree of nasal obstruction severity since the nose and the nasal airway are complex structures.[14]
Our study used the NOSE Scale, a disease-specific tool used to measure nasal obstruction. The questionnaire is short and simple to fill out and places little burden on the respondent. In addition, it is dependable, genuine, and adaptable in clinical status. It may also be used in conjunction with generic or global quality-of-life measures to evaluate the relative effects of a specific disease on several aspects of overall quality of life.[11]
Our study results revealed that approximately two-thirds of the participants in Saudi Arabia had a nasal obstruction. Likewise, in a study in Saudi Arabia conducted by Alanazy S et al.,[15] the prevalence of nasal obstruction among the participants was slightly higher than our findings (75.5%). On the difference, the prevalence of nasal obstruction in an American study was 98% among the participants.[16]
Furthermore, we compared the answers of the participants regarding suffering from nasal obstruction with the NOSE Scale results. Approximately half of the participants who perceive themselves as not having nasal obstruction actually exhibit nasal obstruction when evaluated using the NOSE Scale. These results assumed the importance of objective evaluations with one of the assessment-validated tools in disease diagnosis.
Turbinate hypertrophy, internal or external nasal valve collapse, and septal abnormalities, congenital or acquired, are some anatomic reasons for nasal blockage. The presence of foreign objects inside the nose and benign or cancerous tumors are uncommon causes of nasal blockage. Allergic rhinitis (AR; IgE-mediated) and nonallergic rhinitis, including inflammatory, infectious (viral or bacterial), hormonal, autonomic, drug-induced, systemic disease linked, or occupational reasons, are among the physiological causes of nasal blockage.[17] Our findings showed that the participants mentioned that congestion (as a result of allergic rhinitis, sinusitis, or cold and flu episodes) and deviated septum were the major causes of nasal obstruction.
The patient’s physical or mental state, ability to concentrate, level of stress, and ability to work may all be impacted by nasal obstruction at work or school. These issues could have a negative impact on the patients’ lives and have an effect on their health and social well-being does not always get better even after nasal surgery.[18,19,20,21]
Concerning the NOSE scale, 18.70% of participants had mild nasal obstruction, 20.9% had moderate nasal obstruction, and 20.7% had severe nasal obstruction. In another study in the USA, only 11% of the patients had mild nasal obstruction, most (63%) patients had severe nasal obstruction, and 24% mentioned moderate nasal obstruction.[16]
Moreover, the results of our study estimated that the nasal obstruction affected the participants’ quality of life, and the participants who did not suffer from nasal obstruction showed significantly higher scores on the quality of life assessment. Our result indicates that nasal obstruction may negatively impact the quality of life.
To our knowledge, most previous studies assessed the nasal obstruction severity associated with the outcome of surgeries or with one of the disease causes.[22,23,24,25]
The study lacks a correlation between the subjective and objective diagnoses, and the results depended on the participants’ points of view. Furthermore, there is no strong attention to the symptoms that may be the reason for nasal obstruction.
Conclusions
Quality of life is affected by nasal obstruction and correlates with its severity, including physical, psychological, social, and environmental domains. The subjective assessment is essential in evaluating the severity of nasal obstruction disease. It is recommended that healthcare providers use subjective tools with objective tools to assess the degree of nasal obstruction severity. Further awareness programs regarding subjective tools will be valuable in nasal obstruction diagnosis and treatment decisions.
Ethical approval
The study was approved by the ethics committee at Taif University (approval number 44-019, September 4, 2022).
Key message
The prevalence of nasal obstruction in Saudi Arabia and its association with patient’s quality of life.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We want to thank Ahmed Naif Ghannam Almutairi (Unaizah College of Medicine Male), Anwar Mustafa Ali Alsaeed (King Faisal University), Abdulbari Ahmed Alzahrani (King Khalid University), Sarah Anwar Almulla (King Faisal University), Rawand Ali Alrwuili (Al Jouf University), Shahad Jamaan Alzahrani (Taif university), Linah Saleh Alduraibi (Sulaiman Alrajhi University), Abdullrahman Saeed Abdullah Alshahrani (King Khalid University), Meshari Mosleh Alenzi (Al Jouf University), and Shatha Abdulrahman L Alanazi (Northern Borders University) for their efforts in data collection.
References
- 1.Udaka T, Suzuki H, Kitamura T, Shiomori T, Hiraki N, Fujimura T, et al. Relationships among nasal obstruction, daytime sleepiness, and quality of life. Laryngoscope. 2006;116:2129–32. doi: 10.1097/01.mlg.0000239111.24094.a3. [DOI] [PubMed] [Google Scholar]
- 2.Rhee JS, Book DT, Burzynski M, Smith TL. Quality of life assessment in nasal airway obstruction. Laryngoscope. 2003;113:1118–22. doi: 10.1097/00005537-200307000-00004. [DOI] [PubMed] [Google Scholar]
- 3.Kahveci OK, Miman MC, Yucel A, Yucedag F, Okur E, Altuntas A. The efficiency of Nose Obstruction Symptom Evaluation (NOSE) scale on patients with nasal septal deviation. Auris Nasus Larynx. 2012;39:275–9. doi: 10.1016/j.anl.2011.08.006. [DOI] [PubMed] [Google Scholar]
- 4.Dağistan H, Turan Y. The effect of septoplasty on endothelial function in patients with marked nasal septal deviation. J Craniofac Surg. 2022;33:e242–5. doi: 10.1097/SCS.0000000000008027. [DOI] [PubMed] [Google Scholar]
- 5.World Health Organization. WHOQOL-BREF: Introduction, Administration, Scoring and Generic Version of the Assessment: Field Trial Version, December 1996. World Health Organization. 1996 [Google Scholar]
- 6.Bateman N, Woolford T. Informed consent for septal surgery: The evidence-base. J Laryngol Otol. 2003;117:186–9. doi: 10.1258/002221503321192476. [DOI] [PubMed] [Google Scholar]
- 7.Jessen M, Janzon L. Prevalence of non-allergic nasal complaints in an urban and a rural population in Sweden. Allergy. 1989;44:582–7. doi: 10.1111/j.1398-9995.1989.tb04204.x. [DOI] [PubMed] [Google Scholar]
- 8.Pessey J, Reitz C, Los F. Acute rhinosinusitis in the adult: national survey of general practice management. Rev Laryngol Otol Rhinol (Bord) 2000;121:237–41. [PubMed] [Google Scholar]
- 9.Alotaibi A, Almutlaq B, Alshammari F, Gadelkarim A. The common clinical presentation of patients selected for septoplasty in Northern Saudi Arabia. Int J Otolaryngol 2018. 2018 doi: 10.1155/2018/8536387. 8536387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Alotaibi A. Quality of life in patients with nasal obstruction after one year of septoplasty. Res Otolaryngol. 2017;6:81–7. [Google Scholar]
- 11.Stewart MG, Witsell DL, Smith TL, Weaver EM, Yueh B, Hannley MT. Development and validation of the nasal obstruction symptom evaluation (NOSE) scale. Otolaryngol Head Neck Surg. 2004;130:157–63. doi: 10.1016/j.otohns.2003.09.016. [DOI] [PubMed] [Google Scholar]
- 12.Elwany S, Atef A, Ismail AS, Hussein WK, Ibrahim AA, Abdelnaby M, et al. Arabic translation and validation of the nasal obstruction symptom evaluation (NOSE) scale. Egypt J Otolaryngol. 2021;37:1–4. [Google Scholar]
- 13.Dalky HF, Meininger JC, Al-Ali NM. The reliability and validity of the Arabic world health organization quality of life-BREF instrument among family caregivers of relatives with psychiatric illnesses in Jordan. J Nurs Res. 2017;25:224–30. doi: 10.1097/JNR.0000000000000146. [DOI] [PubMed] [Google Scholar]
- 14.Keeler J, Most SP. Measuring nasal obstruction. Facial Plast Surg Clin North Am. 2016;24:315–22. doi: 10.1016/j.fsc.2016.03.008. [DOI] [PubMed] [Google Scholar]
- 15.Alanazy S, Alenezi M, Al-Quniabut I, Al-Juraifani I, Alburayh M, Altuaysi A, et al. Patterns of allergic rhinitis among adults in Qassim region, Saudi Arabia: A cross sectional study. Pan Afr Med J. 2021;40:70. doi: 10.11604/pamj.2021.40.70.30719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Clark DW, Del Signore AG, Raithatha R, Senior BA. Nasal airway obstruction: Prevalence and anatomic contributors. Ear Nose Throat J. 2018;97:173–6. doi: 10.1177/014556131809700615. [DOI] [PubMed] [Google Scholar]
- 17.Moche JA, Palmer O. Surgical management of nasal obstruction. Oral Maxillofac Surg Clin North Am. 2012;24:229–37. doi: 10.1016/j.coms.2012.01.013. viii. [DOI] [PubMed] [Google Scholar]
- 18.Garbutt J, Spitznagel E, Piccirillo J. Use of the modified SNOT-16 in primary care patients with clinically diagnosed acute rhinosinusitis. Arch Otolaryngol Head Neck Surg. 2011;137:792–7. doi: 10.1001/archoto.2011.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Valls-Mateus M, Marino-Sanchez F, Ruiz-Echevarría K, Cardenas-Escalante P, Jiménez-Feijoo R, Blasco-Lozano J, et al. Nasal obstructive disorders impair health-related quality of life in adolescents with persistent allergic rhinitis: A real-life study. Pediatr Allergy Immunol. 2017;28:438–45. doi: 10.1111/pai.12724. [DOI] [PubMed] [Google Scholar]
- 20.Bulut OC, Wallner F, Hohenberger R, Plinkert PK, Baumann I. Quality of life after primary septorhinoplasty in deviated- and non-deviated nose measured with ROE, FROI-17 and SF-36. Rhinology. 2017;55:75–80. doi: 10.4193/Rhino16.243. [DOI] [PubMed] [Google Scholar]
- 21.Siegel NS, Gliklich RE, Taghizadeh F, Chang Y. Outcomes of septoplasty. Otolaryngol Head Neck Surg. 2000;122:228–32. doi: 10.1016/S0194-5998(00)70244-0. [DOI] [PubMed] [Google Scholar]
- 22.Ramesh K, Rajendrakumar B, Raj P. To study the effect of septoplasty in relieving nasal obstruction and on quality of life. Eur J Mol Clin Med. 2022;4:175–9. [Google Scholar]
- 23.Nguyen DT, Guillemin F, Arous F, Jankowski R. Assessment of quality-of-life outcomes after surgery for nasal polyposis with the DyNaChron questionnaire. Eur Arch Otorhinolaryngol. 2015;272:367–75. doi: 10.1007/s00405-014-3109-0. [DOI] [PubMed] [Google Scholar]
- 24.Udaka T, Suzuki H, Fujimura T, Hiraki N, Ohkubo J, Shiomori T, et al. Chronic nasal obstruction causes daytime sleepiness and decreased quality of life even in the absence of snoring. Am J Rhinol. 2007;21:564–9. doi: 10.2500/ajr.2007.21.3087. [DOI] [PubMed] [Google Scholar]
- 25.Yamasaki A, Levesque PA, Bleier BS, Busaba NY, Gray ST, Holbrook EH, et al. Improvement in nasal obstruction and quality of life after septorhinoplasty and turbinate surgery. Laryngoscope. 2019;129:1554–60. doi: 10.1002/lary.27859. [DOI] [PubMed] [Google Scholar]


