Key Points
Question
Is exposure to green space associated with internalizing (eg, anxiety and depression) and externalizing (eg, aggression and rule-breaking) symptoms among children?
Findings
In this cohort study of 2103 children in 41 states across the US, greater residential green space exposure was associated with fewer internalizing symptoms in early childhood but not in middle childhood.
Meaning
These findings suggest that green space initiatives may help reduce the risk of early anxiety and depressive symptoms in children across the US.
This cohort study of children born between 2007 and 2013 examines associations between residential green space exposure and internalizing and externalizing symptoms in early and middle childhood.
Abstract
Importance
Evidence suggests that living near green space supports mental health, but studies examining the association of green space with early mental health symptoms among children are rare.
Objective
To evaluate the association between residential green space and early internalizing (eg, anxiety and depression) and externalizing (eg, aggression and rule-breaking) symptoms.
Design, Setting, and Participants
Data for this cohort study were drawn from the Environmental Influences on Child Health Outcomes cohort; analysis was conducted from July to October 2023. Children born between 2007 and 2013 with outcome data in early (aged 2-5 years) and/or middle (aged 6-11 years) childhood who resided in 41 states across the US, drawing from clinic, hospital, and community-based cohorts, were included. Cohort sites were eligible if they recruited general population participants and if at least 30 children had outcome and residential address data to measure green space exposure. Nine cohorts with 13 sites met these criteria. Children diagnosed with autism or developmental delay were excluded, and 1 child per family was included.
Exposures
Green space exposure was measured using a biannual (ie, summer and winter) Normalized Difference Vegetation Index, a satellite image–based indicator of vegetation density assigned to monthly residential history from birth to outcome assessment.
Main Outcome and Measures
Child internalizing and externalizing symptoms were assessed using the Child Behavior Checklist for Ages 1½ to 5 or 6 to 18. The association between green space and internalizing and externalizing symptoms was modeled with multivariable linear regression using generalized estimating equations, adjusting for birthing parent educational level, age at delivery, child sex, prematurity, and neighborhood socioeconomic vulnerability. Models were estimated separately for early and middle childhood samples.
Results
Among 2103 children included, 1061 (50.5%) were male; 606 (29.1%) identified as Black, 1094 (52.5%) as White, 248 (11.9%) as multiple races, and 137 (6.6%) as other races. Outcomes were assessed at mean (SD) ages of 4.2 (0.6) years in 1469 children aged 2 to 5 years and 7.8 (1.6) years in 1173 children aged 6 to 11 years. Greater green space exposure was associated with fewer early childhood internalizing symptoms in fully adjusted models (b = −1.29; 95% CI, −1.62 to −0.97). No associations were observed between residential green space and internalizing or externalizing symptoms in middle childhood.
Conclusions and Relevance
In this study of residential green space and children’s mental health, the association of green space with fewer internalizing symptoms was observed only in early childhood, suggesting a sensitive period for nature exposure. Policies protecting and promoting access to green space may help alleviate early mental health risk.
Introduction
The mental health of children in the US is a national emergency.1 Up to 40% of children will meet the criteria for a mental disorder by adulthood,2 an epidemic that has only accelerated in recent years.3 Impaired mental health is even more common below diagnostic thresholds,4 with notable increases in internalizing (eg, anxiety and depression) and externalizing (eg, aggression and rule-breaking) symptoms.5 Identifying environmental factors that buffer children from internalizing and externalizing symptoms offers the potential for modifiable pathways to offset risk.
Exposure to nature may be one such pathway. Forests, parks, backyards, and other green spaces offer children opportunities to restore emotional and physiologic resources; build regulatory capacities through risk-taking, physical activity, and play; and reduce harm from environmental stressors, such as heat or air pollution.6 Experimental research notes short-term benefits of green space on improved mood and physiologic and perceived indicators of stress.7,8 Longitudinal evidence indicates links between green space and mental health7,9,10; adolescents and adults raised in low levels of green space have up to a 55% greater risk for mental disorders than those raised in high levels of green space.11 However, studies examining early emerging internalizing and externalizing symptoms are rare. This is a notable gap: plasticity in emotional, physiologic, and behavioral regulation peaks in early childhood and is shaped by environmental experiences,12,13 and early emerging symptoms have prolonged effects on functioning.14,15 Additionally, research to date is predominantly cross-sectional, focused within single or small groups of cities, and typically fails to account for neighborhood socioeconomic vulnerability, a co-occurring environmental risk.10,16,17 Evidence suggests that green space and socioeconomic vulnerability have independent links with health outcomes18 despite disparities in availability17; the protective benefits of green space may be greater in low-income areas, offsetting social and environmental stressors.19 No studies to date have examined the associations between residential green space exposure from birth, neighborhood socioeconomic vulnerability, and early and middle childhood internalizing and externalizing symptoms across the US. Such research could inform feasible interventions and policy changes to promote the development of children in the US, reducing the rising burden of mental illness.
To address this gap, the current study leveraged data from the Environmental Influences on Child Health Outcomes (ECHO) cohort, a National Institutes of Health–funded consortium of socioeconomically and geographically diverse cohort sites across the US studying the environmental factors contributing to child health, to examine associations between residential green space exposure and internalizing and externalizing symptoms in early (ages 2-5 years) and middle (ages 6-11 years) childhood. A secondary aim was to examine whether neighborhood socioeconomic vulnerability or child sex modified observed associations between green space and internalizing or externalizing symptoms.
Methods
Study Population
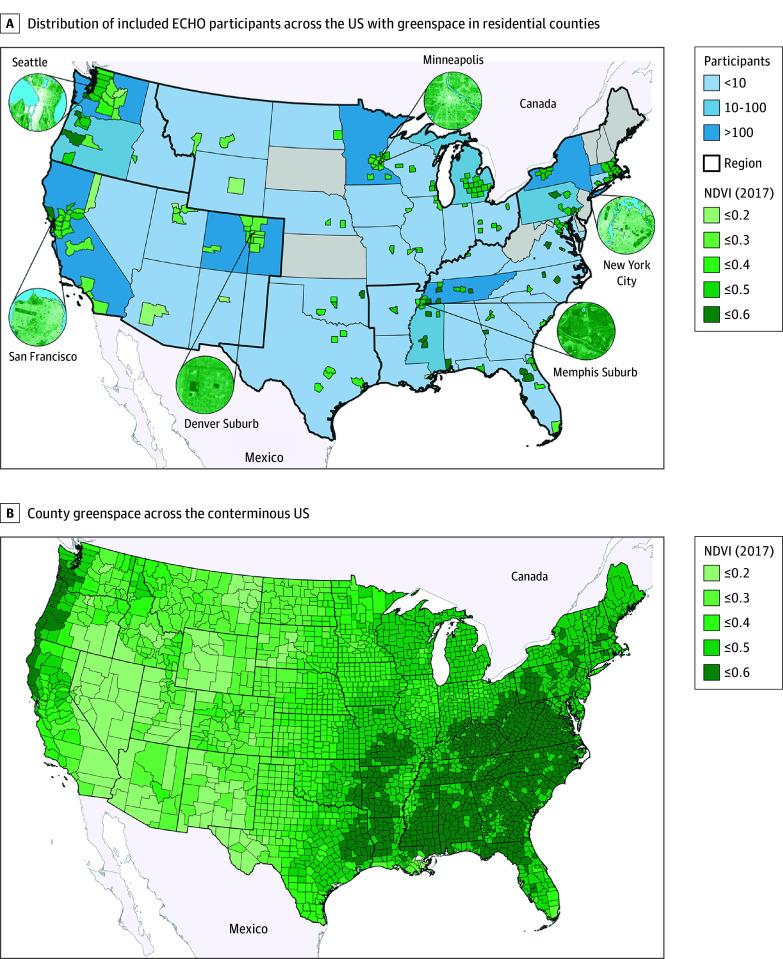
The ECHO cohort comprises 69 ongoing cohorts across the US.20 Children born between 2007 and 2013 who recruited to a general cohort (ie, not selected on medical risk or adoption status) were eligible for the current analysis if they had 1 birthing parent report of internalizing and/or externalizing symptoms via the Child Behavior Checklist for Ages 1½ to 5 years or 6 to 18 years (CBCL 1½-5 or 6-18)21,22 before March 15, 2020 (1 child per family), and a high-quality-match geocoded residential address (point or specific street address, >85% of geocoded addresses) for more than 75% of months from birth to outcome assessment. Children diagnosed with autism spectrum disorder or developmental delay were excluded (n = 240); associations between green space and mental health may be more complex within these populations.23 Cohort enrollment sites with fewer than 30 eligible participants were excluded (9 sites, n = 90; eFigure 1 in Supplement 1). Nine cohorts met these criteria, representing 13 clinic, hospital, and community sites and 2103 children (eTable 1 in Supplement 1); children resided in 199 counties across 41 states (Figure, A). The early childhood (ages 2-5 years) sample included 1469 children from 6 cohorts (7 sites) with 1 measure of internalizing or externalizing symptoms. The middle childhood (ages 6-11 years) sample included 1173 children from 7 cohorts (10 sites); 539 participants (25.6%) who had CBCL data in both early and middle childhood were included in both sets of analyses, almost exclusively from a single cohort (523 [97.0%]). Child race and ethnicity were included as descriptors; these data were provided by the caregiver and harmonized across samples as ethnicity being Hispanic or non-Hispanic and primary race being Black, White, more than 1 race, or other (Alaska Native, American Indian, Asian, Native Hawaiian or other Pacific Islander, or other). The study protocol was reviewed and approved by the local (or single ECHO) institutional review board. Written informed parental consent or permission was obtained along with child assent as appropriate for ECHO-wide and cohort participation. This manuscript follows the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline.
Figure. Maps of Included Environmental Influences on Child Health Outcomes (ECHO) Participants and County-Level Summer and Winter Green Space Across the Conterminous US.
Mean summer and winter Normalized Difference Vegetation Index (NDVI) values in 2017 for residential counties of ECHO participants and counties across the conterminous US.
Measures
Green Space
A monthly residential address history file was generated for each child, accounting for moves from birth to the outcome assessment. Addresses were geocoded using ArcGIS Streetmap Premium, version 3.0 (Esri), generating latitude and longitude for addresses to link with green space data. Monthly green space was estimated using the summer and winter Normalized Difference Vegetation Index (NDVI), a satellite image–based indicator of relative live vegetation density widely used in epidemiologic research.24,25 The NDVI values range from −1 to 1; higher values represent dense vegetation (eg, forests), values close to 0 represent areas without live vegetation, and negative values represent water bodies. Google Earth Engine was used to generate cloud-free ultra-high-resolution (30 m) NDVI values from Landsat satellite data across the conterminous US using XIS (XGBoost-IDW Synthesis26); select ultra-high-resolution images within sample counties (insets) and national county-level summer and winter average NDVI values are presented in the Figure, A and B, respectively. Residential greenness was processed using Python software, version 3.9.11 (Python Software Foundation) and ArcGIS, with average NDVI values estimated in buffers of 270, 510, and 1230 m around home addresses to evaluate the immediate residential area, nearby neighborhood, and extended walkable areas. Consistent with prior research,17 negative NDVI values were set to 0 (<5 children), and raw NDVI values were rescaled by multiplying values greater than 0 by 10 for modeling and interpretability. The NDVI values were assigned to monthly address history to create time-weighted average green space from birth to outcome accounting for residential mobility; NDVI measures (summer) were highly correlated over time within children (intraclass correlation coefficients of 0.84 and 0.81 in early and middle childhood samples, respectively). The NDVI values in buffers of 270 m are reported in the main analyses.
Child Internalizing and Externalizing Symptoms
Preschool (early) or school-aged (middle) CBCL 1½-5 or 6-18 assessed internalizing (ie, anxiety, depression, withdrawal, and somatic concerns) and externalizing (ie, rule-breaking and aggressive behavior) symptoms,21,22 which include 100 and 119 items, respectively. The CBCL 1½-5 or 6-18 is extensively used as a reliable and valid assessment of internalizing and externalizing symptoms27 associated with concurrent and adult clinical health28,29; given significant discrepancies across parental reports on the CBCL,30 we used birthing parent ratings of symptoms observed in the past 6 months, with item responses ranging from 0 (not true) to 2 (very true or often true). Nationally normed T scores based on age and sex were used in the current analysis.
Confounders
Neighborhood- and individual-level confounders were identified a priori based on theory, research, and data availability. Neighborhood socioeconomic status (SES) vulnerability was assessed using the SES theme of the Social Vulnerability Index,31 which includes rankings of census tracts based on census-reported levels of poverty, unemployment, housing cost burden, no high school diploma, and no health insurance. Scores reflect the proportion of national tracts less vulnerable than the residential tract (higher scores reflect greater vulnerability based on low SES). Social Vulnerability Index values averaged for the exposure period were categorized into tertiles established by national data representing low, medium, and high vulnerability based on US norms.32 At the individual level, we adjusted for birthing parent age at delivery (continuous) and educational level (highest attained: less than high school, high school or equivalent, or more than high school) as well as child sex assigned at birth and preterm status (<37 vs ≥37 weeks’ gestation).
Statistical Analysis
Analyses were conducted from July to October 2023 using Stata software, version 17 (StataCorp LLC)33 and ArcGIS Pro, version 3.0.3 (Esri).34 We examined outcome distributions to ensure normality and the functional form of the association between NDVI and outcomes with scatterplots and Lowess lines. Because most cohorts had CBCL assessments in either early or middle childhood (but not both), all analyses were run separately for the early and middle childhood samples. Because ECHO data are clustered by design, we used multivariable linear regression with generalized estimating equation (exchangeable correlation structure and robust variance) estimates to account for clustering of participants within cohort enrollment sites. We first examined unadjusted models of associations between NDVI (per 0.1 increments) and internalizing or externalizing symptoms, then adjusted for individual-level confounders, and finally adjusted for individual- and area-level SES vulnerability. Because more than 99% of the sample had complete covariate data, we used complete case analysis for adjusted models. To aid in interpretation, we used model estimates to calculate the difference in estimated CBCL for individuals residing at relatively high green space compared with low (90th vs 10th percentile NDVI for sample).
We conducted 2 sets of a priori exploratory analyses examining effect measure modification by child sex assigned at birth and by average neighborhood SES vulnerability; interaction terms were added in the fully adjusted models. We considered an interaction term 2-sided P = .10 as the threshold for effect measure modification.
We evaluated the robustness of the results through sensitivity analyses. We examined associations between NDVI and internalizing and externalizing symptoms in buffers of 510 and 1230 m to evaluate the sensitivity of associations to the size of the buffer used. Next, the relative contribution to the estimates from a single cohort enrollment site were evaluated using the leave-one-out approach.
Results
Among 2103 children included (1469 in the early childhood sample, 1173 in the middle childhood sample, and 539 children in both samples), 1061 (50.5%) were male and 1042 (49.5%) female; 203 (9.7%) were preterm and 1900 (90.3%) were not; 606 (29.1%) were Black, 1094 (52.5%) were White, 248 (11.9%) were of more than 1 race, and 137 (6.6%) were of other races (Alaska Native, American Indian, Asian, Native Hawaiian or other Pacific Islander, or caregiver-reported “other” race); and 1761 (84.0%) were non-Hispanic and 336 (16.0%) Hispanic. Most birthing parents (1795 [85.4%]) had more than a high school education, with a mean (SD) age of 29.0 (6.0) years at delivery. Descriptive statistics for the early and middle childhood samples are presented in Table 1 (eTables 2-3 in Supplement 1). Symptoms were reported at a mean (SD) age of 4.2 (0.6) years for the early childhood sample and 7.8 (1.6) years for the middle childhood sample. Most children moved at least once between birth and outcome assessment (855 [58.2%] and 799 [68.1%] in the early and middle childhood samples, respectively). There were not notable differences in demographics between the early and middle childhood analytic samples.
Table 1. Child, Parental, and Residential Characteristics by Early and Middle Childhood Study Populationsa.
| Characteristic | Early childhood (n = 1469) | Middle childhood (n = 1173) | Total (N = 2103) |
|---|---|---|---|
| Child characteristics | |||
| Age at CBCL 1½-5 or 6-18 assessment, mean (SD), y | 4.2 (0.6) | 7.8 (1.6) | 5.0 (1.5) |
| CBCL 1½-5 or 6-18 internalizing symptoms T score, median (IQR) | 45 (37-53) | 48 (41-54) | 45 (39-54) |
| CBCL 1½-5 or 6-18 externalizing symptoms T score, median (IQR) | 44 (39-51) | 48 (41-56) | 46 (39-53) |
| Sex assigned at birth | |||
| Male | 745 (50.7) | 581 (49.5) | 1061 (50.5) |
| Female | 724 (49.3) | 592 (50.5) | 1042 (49.5) |
| Child raceb | |||
| Black | 528 (36.3) | 416 (35.6) | 606 (29.1) |
| White | 697 (47.9) | 558 (47.8) | 1094 (52.5) |
| >1 Race | 139 (9.5) | 143 (12.3) | 248 (11.9) |
| Otherc | 92 (6.3) | 50 (4.3) | 137 (6.6) |
| Child ethnicityb | |||
| Non-Hispanic | 1215 (83.0) | 1068 (91.1) | 1761 (84.0) |
| Hispanic | 249 (17.0) | 104 (8.9) | 336 (16.0) |
| Preterm (<37 completed weeks) | |||
| No | 1354 (92.2) | 1038 (88.5) | 1900 (90.3) |
| Yes | 115 (7.8) | 135 (11.5) | 203 (9.7) |
| Birthing parent characteristics | |||
| Age at delivery, mean (SD), y | 29.0 (6) | 29.0 (6.0) | 29.0 (6.0) |
| Educational attainment | |||
| Less than high school | 59 (4.0) | 27 (2.3) | 77 (3.7) |
| High school, GED, or equivalent | 181 (12.3) | 132 (11.3) | 229 (10.9) |
| Some college or more | 1228 (83.7) | 1013 (86.4) | 1795 (85.4) |
| Residential characteristics | |||
| Average neighborhood SES (SVI) | |||
| High | 536 (36.5) | 497 (42.4) | 885 (42.1) |
| Medium | 339 (23.1) | 266 (22.7) | 489 (23.3) |
| Low | 594 (40.4) | 410 (35.0) | 729 (34.7) |
| Region | |||
| West | 413 (28.1) | 194 (16.5) | 606 (28.8) |
| Northwest | 84 (5.7) | 184 (15.7) | 268 (12.7) |
| Midwest or Central | 87 (5.9) | 117 (10.0) | 204 (9.7) |
| East | 885 (60.2) | 678 (57.8) | 1025 (48.7) |
| NDVI at 270 m from birth to outcome, mean (SD) | 0.32 (0.08) | 0.35 (0.08) | 0.32 (0.09) |
| Movers | |||
| No (1 residential location) | 614 (41.8) | 374 (31.9) | 988 (37.4) |
| Yes (>1 residential location) | 855 (58.2) | 799 (68.1) | 1654 (62.6) |
Abbreviations: CBCL 1½-5 or 6-18, Child Behavior Checklist for Ages 1½ to 5 or 6 to 18; GED, General Educational Development; NDVI, Normalized Difference Vegetation Index; SES, socioeconomic status; SVI, Social Vulnerability Index.
Data are presented as number (percentage) of participants unless otherwise indicated. Covariate data are complete or are missing at less than 1%; 539 participants are included in both the early and middle childhood samples.
Child race and ethnicity were identified through caregiver report.
Other includes Alaska Native, American Indian, Asian, Native Hawaiian or other Pacific Islander, or caregiver-reported “other.”
Most children were recruited from cohort sites in the Eastern US (885 [60.2%] and 678 [57.8%] for early and middle childhood samples, respectively). More than one-third (885 [42.1%]) of the children resided in neighborhoods classified as high SES vulnerability. Green space was negatively correlated with internalizing and externalizing symptoms in early childhood (r = −0.12 and P < .001 and r = −0.08 and P = .002, respectively) but not in middle childhood (r = 0.01 and P = .78 and r = 0.02 and P = .59, respectively).
Unadjusted and adjusted models are presented in Table 2. A 0.1-unit higher NDVI at 270 m was associated with 1.28-unit lower internalizing (b = −1.28; 95% CI, −1.62 to −0.95) and 0.77-unit lower externalizing (b = −0.77; 95% CI, −11.53 to −0.02) T scores in early childhood (Table 2), adjusting for child sex assigned at birth, preterm status, birthing parent educational level, and age at delivery. The association held for internalizing symptoms after adjustment for neighborhood SES vulnerability (b = −1.29; 95% CI, −1.62 to −0.97) but was attenuated for externalizing symptoms (b = −0.66; 95% CI, −1.38 to 0.06); estimates for covariates in fully adjusted models are presented in eTable 4 in Supplement 1. In fully adjusted models, children residing at relatively high green space (90th percentile NDVI = 0.42) had mean CBCL T scores 2.62 points lower for internalizing and 1.34 points lower for externalizing symptoms compared with children residing in lower levels (10th NDVI = 0.22); example counties with average NDVI values at the 90th and 10th percentiles are shown in eFigure 2 in Supplement 1. In middle childhood, analyses revealed no associations between green space and internalizing or externalizing scores, which did not change after adjustment for individual- and/or area-level factors.
Table 2. Adjusted Association Between Residential Green Space and Children’s Internalizing and Externalizing Symptoms (CBCL 1½-5 or 6-18 T Score)a.
| NDVI | b (95% CI) | |||||
|---|---|---|---|---|---|---|
| Internalizing symptoms | Externalizing symptoms | |||||
| Unadjusted | Individual-level covariates | Individual-level covariates and average SVI | Unadjusted | Individual-level covariates | Individual-level covariates and average SVI | |
| Early childhood (aged 2-5 y) | ||||||
| No. | 1469 | 1463 | 1463 | 1469 | 1463 | 1463 |
| Average NDVI within 270 m | −1.59 (−2.28 to −0.87)b | −1.28 (−1.62 to −0.95)b | −1.29 (−1.62 to −0.97)b | −1.16 (−2.10 to −0.22)b | −0.77 (−11.53 to −0.02)b | −0.66 (−1.38 to 0.06) |
| Average NDVI within 510 mc | −1.59 (−2.40 to −0.79)b | −1.26 (−0.69 to −0.84)b | −1.27 (−1.67 to −0.87)b | −1.25 (−2.19 to −0.30)b | −0.83 (−1.62 to −0.05)b | −0.69 (−1.47 to 0.08) |
| Average NDVI within 1230 mc | −1.38 (−2.29 to −0.47)b | −1.10 (−1.59 to −0.60)b | −1.10 (−1.58 to −0.62)b | −1.05 (−2.00 to −0.10)b | −0.62 (−1.40 to 0.17) | −0.48 (−1.22 to 0.27) |
| Middle childhood (aged 6-11 y) | ||||||
| No. | 1172 | 1170 | 1170 | 1171 | 1169 | 1169 |
| Average NDVI within 270 m | 0.16 (−0.80 to 1.12) | 0.11 (−0.81 to 1.03) | 0.11 (−0.70 to 0.92) | 0.18 (−0.34 to 0.71) | 0.19 (−0.44 to 0.82) | 0.20 (−0.51 to 0.91) |
| Average NDVI within 510 mc | 0.22 (−0.82 to 1.26) | 0.15 (−0.85 to 1.16) | 0.12 (−0.79 to 1.02) | 0.20 (−0.31 to 0.70) | 0.22 (−0.40 to 0.84) | 0.25 (−0.45 to 0.96) |
| Average NDVI within 1230 mc | 0.26 (−0.69 to 1.21) | 0.16 (−0.79 to 1.11) | 0.09 (−0.81 to 0.99) | 0.07 (−0.55 to 0.69) | 0.09 (−0.63 to 0.80) | 0.13 (−0.64 to 0.90) |
Abbreviations: CBCL 1½-5 or 6-18, Child Behavior Checklist for Ages 1½ to 5 or 6 to 18; NDVI, Normalized Difference Vegetation Index; SVI, Social Vulnerability Index.
Coefficients (per 0.1 higher NDVI) from generalized estimating equation linear regression of the association between average green space exposure from birth and internalizing and externalizing symptoms. Models are (1) unadjusted and then adjusted for (2) individual-level confounders (birthing parent’s educational level, age at delivery, child sex, and preterm birth status) and (3) individual confounders and tract-level Social Vulnerability Index from birth. High social vulnerability corresponds with low socioeconomic status.
Statistically significant based on P < .05.
Sensitivity analysis of different buffer sizes for comparability with previous literature.
No evidence of effect measure modification by child sex emerged for internalizing or externalizing symptoms. Associations were also similar across high vs low neighborhood SES vulnerability. Although there was a significant interaction between moderate SES vulnerability and green space compared with low SES vulnerability for middle childhood externalizing symptoms, we were unable to run analyses stratified by neighborhood SES vulnerability due to sparseness across cells.
Sensitivity analyses were conducted to investigate the robustness of associations. In early childhood, a similar pattern emerged at 510-m and 1230-m buffers, although the magnitude of associations was attenuated at 1230 m. Sensitivity analyses for middle childhood similarly found no association of green space with internalizing or externalizing symptoms at larger buffers. To assess whether associations were robust and not driven by any single site, fully adjusted models were reestimated, leaving 1 enrollment site out at a time. Forest plots of estimates for early and middle childhood internalizing and externalizing symptoms are summarized in eFigure 3 in Supplement 1.
Discussion
To our knowledge, this is the first study to examine the association of green space exposure on early internalizing and externalizing symptoms in children across the US. Our results suggest that higher levels of residential green space are associated with fewer internalizing symptoms in early childhood (aged 2-5 years) before and after adjusting for child sex, prematurity, birthing parent educational level and age at delivery, and neighborhood socioeconomic vulnerability. Although green space was also associated with externalizing problems in early childhood, this association was attenuated after accounting for neighborhood socioeconomic vulnerability. We did not find evidence of associations between residential green space and internalizing or externalizing symptoms in middle childhood (aged 6-11 years). Leveraging data from multiple diverse cohorts with substantial regional, demographic, and economic diversity, these findings extend our understanding of nature as a protective factor for mental health risk.
Our finding that green space is associated with fewer early childhood internalizing symptoms is consistent with evidence of the benefits of nature on children’s functioning10 and work, suggesting that early childhood may be a sensitive period for green space exposure.32 In fully adjusted models, residing in relatively low vs high levels of green space was associated with 2.62-point higher internalizing T scores; this association is greater in magnitude than risks such as exceeding the recommended threshold of screentime (>2 hours per day) or the benefit of more than 2 hours per week of organized physical activity on early internalizing scores.35 Rapid neural maturation and foundational regulatory skill development make early childhood a sensitive window for environmental influences. With the home as a central context for early development, nearby nature may offer unique opportunities for positive emotions, stress reduction, and the restoration of emotional resources through evolutionarily determined pathways; areas directly around the residence may be particularly salient for young children given the restorative influence of green space within visible distances around the home.6 Additionally, green space may reduce the impact of environmental stressors such as heat or air pollution, increase exposure to diverse microbiomes, and offer opportunities for play and physical activity,36,37 providing multiple pathways to offset mental health risk. The protection and extension of natural environments to young children may offer widespread benefits.
Notably, associations between green space and early childhood internalizing symptoms were stronger than for externalizing symptoms. This discrepancy was more pronounced after accounting for neighborhood socioeconomic vulnerability; because there are notable socioeconomic disparities in green space17 and neighborhood poverty has stronger links with externalizing than internalizing symptoms,38 this finding is not entirely surprising. Nationally representative studies from Australia and Europe have also reported stronger associations between green space and children’s internalizing symptoms,39 depression diagnoses,40 and internalizing disorders into adulthood,11 although findings are mixed within adolescence.41 Although externalizing symptoms were not examined, Bezold et al42 found links between higher greenness and lower risk for depressive symptoms in more than 11 000 adolescents and adults across the US. In one of the only longitudinal studies focused on preschool, green space similarly supported resilience for boys’ emotional symptoms.43 Because early internalizing symptoms may have a prolonged and severe developmental course,15 the protective role of green space within this period may have long-term implications.
The lack of associations between residential green space and middle childhood internalizing or externalizing symptoms is counter to the broader body of green space research to date. However, middle childhood mental health research is lagging in general44; research from school age through adolescence suggests that the magnitude of green space associations vary across development.45 The transition to school represents a notable change in the environment for children, and school green space exposure may be an important influence.46 For example, Liao et al47 found that the combination of concurrent school and residential greenness was linked with kindergarten mental health symptoms, but residential green space alone was not. Time-use data may offer more accurate exposure estimates, with free-play at home decreasing across childhood48 and participation in extracurricular activities at home or elsewhere varying according to parental values and SES.49 Additionally, inclusion of self-report or teacher report could improve outcome assessment in middle childhood, particularly for internalizing symptoms,50 and the middle childhood sample had differences in both regional characteristics and socioeconomic vulnerability. Improving the accuracy of exposure and outcome measurement across diverse samples is an important area for investigation.
With data pooled across all sites, green space near the home had similar and independent associations with early internalizing symptoms across child sex and across the most vs the least socioeconomically disadvantaged neighborhoods. Consistent protective linkages with green space are in line with prior work indicating unique associations of SES and green space on child outcomes11; the potential for universal benefits of nearby natural areas on early childhood mental health is promising.
Limitations
Confounding factors may have influenced our results, such as exposure to environmental hazards, parenting quality, or neighborhood cohesion or violence. Although neighborhood SES vulnerability and individual characteristics were included in our models, choice of residence may be driven by historical social class, residential segregation, or additional factors not included. The NDVI does not indicate the quality, accessibility, or use of nearby nature, and we did not assess childcare or school green space. Similarly, characteristics of green space that may be important for mental health were not assessed, such as woodland composition, water, or biodiversity. The sample predominantly resided in the East and metropolitan areas; these findings may not generalize across rural or other areas. Associations between green space and internalizing symptoms were modest; social or genetic factors may have stronger implications for early symptoms. Although our assessment of average green space exposure from birth to the outcome assessment incorporated shifts in NDVI values due to residential moves or urbanization over time, longitudinal research is needed to examine the dynamic changes in green space and the development of internalizing and externalizing symptoms across childhood.
Conclusions
Residential green space exposure was associated with fewer early childhood internalizing symptoms within the national ECHO-wide cohort, even after accounting for neighborhood socioeconomic vulnerability. These findings suggest that green initiatives (eg, parks, urban forest programs, and protected natural areas) have the potential to reduce risk for early anxiety and depressive symptoms in children across the US. At a time of crisis in children’s mental health and dwindling natural environments, policies that protect and promote green space could have widespread benefits for children, society, and the environment.
eTable 1. Included ECHO Cohort Descriptions
eTable 2. Distribution of Child, Parental, and Residential Characteristics for Early Childhood Study Population by Quartiles of NDVI (n = 1469)
eTable 3. Distribution of Child, Parental, and Residential Characteristics for Middle Childhood Study Population by Quartiles of NDVI (n = 1173)
eTable 4. Fully Adjusted Associations Between Residential Green Space, Individual and Area-Level Confounders, and Children’s Internalizing and Externalizing Symptoms (CBCL 1½-5/6-18 t-Score)
eFigure 1. Flowchart for Final Analytic Sample of 2103 Children Included in the Analysis of Residential Green Space and Internalizing and Externalizing Symptoms
eFigure 2. Example Counties With Average NDVI Values at Relatively High Levels of Greenspace (at the 90th Percentile of NDVI) for the Early Childhood Sample Compared to Relatively Low Levels (the 10th Percentile)
eFigure 3. Leave-One-Out (Cohort Enrollment Site) Coefficient Plots for Association Between Green Space (270m) Internalizing and Externalizing Symptoms for Early and Middle Childhood Samples
Nonauthor Collaborators
Data Sharing Statement
References
- 1.American Academy of Pediatrics . AAP-AACAP-CHA Declaration of a National Emergency in Child and Adolescent Mental Health. Published October 19, 2021. Accessed May 2023. https://www.aap.org/en/advocacy/child-and-adolescent-healthy-mental-development/aap-aacap-cha-declaration-of-a-national-emergency-in-child-and-adolescent-mental-health/
- 2.Shim R, Szilagyi M, Perrin JM. Epidemic rates of child and adolescent mental health disorders require an urgent response. Pediatrics. 2022;149(5):e2022056611. doi: 10.1542/peds.2022-056611 [DOI] [PubMed] [Google Scholar]
- 3.Deng J, Zhou F, Hou W, et al. Prevalence of mental health symptoms in children and adolescents during the COVID-19 pandemic: a meta-analysis. Ann N Y Acad Sci. 2023;1520(1):53-73. doi: 10.1111/nyas.14947 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Copeland W, Shanahan L, Costello EJ, Angold A. Cumulative prevalence of psychiatric disorders by young adulthood: a prospective cohort analysis from the Great Smoky Mountains Study. J Am Acad Child Adolesc Psychiatry. 2011;50(3):252-261. doi: 10.1016/j.jaac.2010.12.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Levante A, Martis C, Bianco F, Castelli I, Petrocchi S, Lecciso F. Internalizing and externalizing symptoms in children during the COVID-19 pandemic: a systematic mixed studies review. Front Psychol. 2023;14:1182309. doi: 10.3389/fpsyg.2023.1182309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Markevych I, Schoierer J, Hartig T, et al. Exploring pathways linking greenspace to health: theoretical and methodological guidance. Environ Res. 2017;158:301-317. doi: 10.1016/j.envres.2017.06.028 [DOI] [PubMed] [Google Scholar]
- 7.Fyfe-Johnson AL, Hazlehurst MF, Perrins SP, et al. Nature and children’s health: a systematic review. Pediatrics. 2021;148(4):e2020049155. doi: 10.1542/peds.2020-049155 [DOI] [PubMed] [Google Scholar]
- 8.Jones R, Tarter R, Ross AM. Greenspace interventions, stress and cortisol: a scoping review. Int J Environ Res Public Health. 2021;18(6):2802. doi: 10.3390/ijerph18062802 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Collins R, Spake R, Brown K, Ogutu B, Smith D, Eigenbrod F. A systematic map of research exploring the effect of greenspace on mental health. Landsc Urban Plan. 2020;201:103823. doi: 10.1016/j.landurbplan.2020.103823 [DOI] [Google Scholar]
- 10.Zare Sakhvidi MJ, Knobel P, Bauwelinck M, et al. Greenspace exposure and children behavior: a systematic review. Sci Total Environ. 2022;824:153608. doi: 10.1016/j.scitotenv.2022.153608 [DOI] [PubMed] [Google Scholar]
- 11.Engemann K, Pedersen CB, Arge L, Tsirogiannis C, Mortensen PB, Svenning JC. Residential green space in childhood is associated with lower risk of psychiatric disorders from adolescence into adulthood. Proc Natl Acad Sci U S A. 2019;116(11):5188-5193. doi: 10.1073/pnas.1807504116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Blair C, Raver CC. Child development in the context of adversity: experiential canalization of brain and behavior. Am Psychol. 2012;67(4):309-318. doi: 10.1037/a0027493 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Davidson RJ, Jackson DC, Kalin NH. Emotion, plasticity, context, and regulation: perspectives from affective neuroscience. Psychol Bull. 2000;126(6):890-909. doi: 10.1037/0033-2909.126.6.890 [DOI] [PubMed] [Google Scholar]
- 14.Arslan İB, Lucassen N, van Lier PAC, de Haan AD, Prinzie P. Early childhood internalizing problems, externalizing problems and their co-occurrence and (mal)adaptive functioning in emerging adulthood: a 16-year follow-up study. Soc Psychiatry Psychiatr Epidemiol. 2021;56(2):193-206. doi: 10.1007/s00127-020-01959-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sterba SK, Prinstein MJ, Cox MJ. Trajectories of internalizing problems across childhood: heterogeneity, external validity, and gender differences. Dev Psychopathol. 2007;19(2):345-366. doi: 10.1017/S0954579407070174 [DOI] [PubMed] [Google Scholar]
- 16.Liu J, Green R. The effect of exposure to nature on children’s psychological well-being: a systematic review of the literature. Urban For Urban Green. 2023;81:127846. doi: 10.1016/j.ufug.2023.127846 [DOI] [Google Scholar]
- 17.Klompmaker JO, Hart JE, Bailey CR, et al. Racial, ethnic, and socioeconomic disparities in multiple measures of blue and green spaces in the United States. Environ Health Perspect. 2023;131(1):17007. doi: 10.1289/EHP11164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wan S, Rojas-Rueda D, Pretty J, Roscoe C, James P, Ji JS. Greenspace and mortality in the U.K. Biobank: Longitudinal cohort analysis of socio-economic, environmental, and biomarker pathways. SSM Popul Health. 2022;19:101194. doi: 10.1016/j.ssmph.2022.101194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rigolon A, Browning MHEM, McAnirlin O, Yoon HV. Green space and health equity: a systematic review on the potential of green space to reduce health disparities. Int J Environ Res Public Health. 2021;18(5):2563. doi: 10.3390/ijerph18052563 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Knapp EA, Kress AM, Parker CB, et al. The Environmental Influences on Child Health Outcomes (ECHO)-wide cohort. Am J Epidemiol. 2023;192(8):1249-1263. doi: 10.1093/aje/kwad071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Achenbach TM. Manual for the Child Behavior Checklist/4-18 and 1991 Profile. Dept of Psychiatry, University of Vermont; 1991. [Google Scholar]
- 22.Achenbach T, Rescorla L. Child behavior checklist for ages 1 1/2-5. Reporter. 2000;10:20. [Google Scholar]
- 23.Larson LR, Barger B, Ogletree S, et al. Gray space and green space proximity associated with higher anxiety in youth with autism. Health Place. 2018;53:94-102. doi: 10.1016/j.healthplace.2018.07.006 [DOI] [PubMed] [Google Scholar]
- 24.Jimenez MP, DeVille NV, Elliott EG, et al. Associations between nature exposure and health: a review of the evidence. Int J Environ Res Public Health. 2021;18(9):4790. doi: 10.3390/ijerph18094790 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.James P, Banay RF, Hart JE, Laden F. A review of the health benefits of greenness. Curr Epidemiol Rep. 2015;2(2):131-142. doi: 10.1007/s40471-015-0043-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Just AC, Arfer KB, Rush J, et al. Advancing methodologies for applying machine learning and evaluating spatiotemporal models of fine particulate matter (PM2.5) using satellite data over large regions. Atmos Environ (1994). 2020;239:117649. doi: 10.1016/j.atmosenv.2020.117649 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Achenbach TM, Ruffle TM. The Child Behavior Checklist and related forms for assessing behavioral/emotional problems and competencies. Pediatr Rev. 2000;21(8):265-271. doi: 10.1542/pir.21.8.265 [DOI] [PubMed] [Google Scholar]
- 28.Biederman J, DiSalvo M, Vaudreuil C, et al. Can the Child Behavior Checklist (CBCL) help characterize the types of psychopathologic conditions driving child psychiatry referrals? Scand J Child Adolesc Psychiatr Psychol. 2020;8(1):157-165. doi: 10.21307/sjcapp-2020-016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hofstra MB, van der Ende J, Verhulst FC. Child and adolescent problems predict DSM-IV disorders in adulthood: a 14-year follow-up of a Dutch epidemiological sample. J Am Acad Child Adolesc Psychiatry. 2002;41(2):182-189. doi: 10.1097/00004583-200202000-00012 [DOI] [PubMed] [Google Scholar]
- 30.Schroeder J, Hood M, Hughes H. Inter-parent agreement on the syndrome scales of the Child Behavior Checklist (CBCL): correspondence and discrepancies. J Child Fam Stud. 2010;19:646-653. doi: 10.1007/s10826-010-9352-0 [DOI] [Google Scholar]
- 31.Geospatial Research, Analysis, and Services Program, Agency for Toxic Substances and Disease Registry, Centers for Disease Control and Prevention. CDC/ATSDR Social Vulnerability Index [2018, 2016, 2014, 2010, 2000] Database [US]. Accessed February 22, 2024. https://www.atsdr.cdc.gov/placeandhealth/svi/data_documentation_download.html
- 32.Jimenez MP, Aris IM, Rifas-Shiman S, et al. Early life exposure to greenness and executive function and behavior: an application of inverse probability weighting of marginal structural models. Environ Pollut. 2021;291:118208. doi: 10.1016/j.envpol.2021.118208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Stata. Release 17. StataCorp LLC; 2021.
- 34.ArcGIS. Version 3.0.3. Environmental Systems Research Institute Inc; 2010. [Google Scholar]
- 35.Tamana SK, Ezeugwu V, Chikuma J, et al. ; CHILD Study Investigators . Screen-time is associated with inattention problems in preschoolers: results from the CHILD birth cohort study. PLoS One. 2019;14(4):e0213995. doi: 10.1371/journal.pone.0213995 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Nieuwenhuijsen MJ. Urban and transport planning pathways to carbon neutral, liveable and healthy cities; a review of the current evidence. Environ Int. 2020;140:105661. doi: 10.1016/j.envint.2020.105661 [DOI] [PubMed] [Google Scholar]
- 37.Selway CA, Mills JG, Weinstein P, et al. Transfer of environmental microbes to the skin and respiratory tract of humans after urban green space exposure. Environ Int. 2020;145:106084. doi: 10.1016/j.envint.2020.106084 [DOI] [PubMed] [Google Scholar]
- 38.Maxwell M, Taylor R, Barch D. Relationship between neighborhood poverty and externalizing symptoms in children: mediation and moderation by environmental factors and brain structure. Child Psychiatry Hum Dev. 2022;54(6):1710-1722. doi: 10.1007/s10578-022-01369-w [DOI] [PubMed] [Google Scholar]
- 39.Feng X, Astell-Burt T. Residential green space quantity and quality and child well-being: a longitudinal study. Am J Prev Med. 2017;53(5):616-624. doi: 10.1016/j.amepre.2017.06.035 [DOI] [PubMed] [Google Scholar]
- 40.Maas J, Verheij RA, de Vries S, Spreeuwenberg P, Schellevis FG, Groenewegen PP. Morbidity is related to a green living environment. J Epidemiol Community Health. 2009;63(12):967-973. doi: 10.1136/jech.2008.079038 [DOI] [PubMed] [Google Scholar]
- 41.Lee M, Kim S, Ha M. Community greenness and neurobehavioral health in children and adolescents. Sci Total Environ. 2019;672:381-388. doi: 10.1016/j.scitotenv.2019.03.454 [DOI] [PubMed] [Google Scholar]
- 42.Bezold CP, Banay RF, Coull BA, et al. The association between natural environments and depressive symptoms in adolescents living in the United States. J Adolesc Health. 2018;62(4):488-495. doi: 10.1016/j.jadohealth.2017.10.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Flouri E, Midouhas E, Joshi H. The role of urban neighborhood green space in children’s emotional and behavioral resilience. J Environ Psychol. 2014;40:179-186. doi: 10.1016/j.jenvp.2014.06.007 [DOI] [Google Scholar]
- 44.Voss ML, Claeson M, Bremberg S, Peterson SS, Alfvén T, Ndeezi G. The missing middle of childhood. Glob Health Action. 2023;16(1):2242196. doi: 10.1080/16549716.2023.2242196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Li D, Menotti T, Ding Y, Wells NM. Life course nature exposure and mental health outcomes: a systematic review and future directions. Int J Environ Res Public Health. 2021;18(10):5146. doi: 10.3390/ijerph18105146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Vanaken GJ, Danckaerts M. Impact of green space exposure on children’s and adolescents’ mental health: a systematic review. Int J Environ Res Public Health. 2018;15(12):2668. doi: 10.3390/ijerph15122668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Liao J, Yang S, Xia W, et al. Associations of exposure to green space with problem behaviours in preschool-aged children. Int J Epidemiol. 2020;49(3):944-953. doi: 10.1093/ije/dyz243 [DOI] [PubMed] [Google Scholar]
- 48.Hofferth S, Sandberg J. Changes in American children’s time, 1981–1997. Adv Life Course Res. 2001;6:193-229. doi: 10.1016/S1040-2608(01)80011-3 [DOI] [Google Scholar]
- 49.Weininger E, Lareau A, Conley D. What money doesn’t buy: class resources and children’s participation in organized extracurricular activities. Soc Forces. 2015;94(2):479-503. doi: 10.1093/sf/sov071 [DOI] [Google Scholar]
- 50.Mesman J, Koot HM. Child-reported depression and anxiety in preadolescence, I: associations with parent- and teacher-reported problems. J Am Acad Child Adolesc Psychiatry. 2000;39(11):1371-1378. doi: 10.1097/00004583-200011000-00011 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Included ECHO Cohort Descriptions
eTable 2. Distribution of Child, Parental, and Residential Characteristics for Early Childhood Study Population by Quartiles of NDVI (n = 1469)
eTable 3. Distribution of Child, Parental, and Residential Characteristics for Middle Childhood Study Population by Quartiles of NDVI (n = 1173)
eTable 4. Fully Adjusted Associations Between Residential Green Space, Individual and Area-Level Confounders, and Children’s Internalizing and Externalizing Symptoms (CBCL 1½-5/6-18 t-Score)
eFigure 1. Flowchart for Final Analytic Sample of 2103 Children Included in the Analysis of Residential Green Space and Internalizing and Externalizing Symptoms
eFigure 2. Example Counties With Average NDVI Values at Relatively High Levels of Greenspace (at the 90th Percentile of NDVI) for the Early Childhood Sample Compared to Relatively Low Levels (the 10th Percentile)
eFigure 3. Leave-One-Out (Cohort Enrollment Site) Coefficient Plots for Association Between Green Space (270m) Internalizing and Externalizing Symptoms for Early and Middle Childhood Samples
Nonauthor Collaborators
Data Sharing Statement