Sarcoidosis is a chronic, multi-system disease characterized by the presence of non-caseating granulomatous inflammation, often affecting the lungs, lymph nodes, and skin (1,2). Cutaneous manifestations are among the most common extrapulmonary manifestations of sarcoidosis (1). Approximately 25-40% of patients with sarcoidosis exhibit skin involvement, which can present with papules, plaques, and lupus pernio, as well as less common manifestations such as alopecia and ulcers (1-3). Herein, we discuss scalp sarcoidosis with alopecia, a rare cutaneous manifestation of sarcoidosis, to enhance awareness and facilitate early recognition.
Scalp sarcoidosis is uncommon, yet when it occurs can have a profound impact on quality of life considering the potential for scarring and may serve as a sign of systemic disease (2-5). The clinical presentation of scalp sarcoidosis varies, but is typically characterized by atrophic, indurated, annular, scaly, erythematous plaques or nodules, frequently accompanied by alopecia (3,6). Alopecia secondary to sarcoidosis can be cicatricial (scarring) or non-cicatricial (non-scarring) depending on the extent of hair follicle involvement, although cicatricial alopecia is more common (Figure 1) (3,4,6,7). Differentiating alopecic sarcoidosis from other conditions through biopsy is critical both to confirm granulomatous inflammation and to differentiate from mimickers and other scarring alopecias, including discoid lupus erythematosus, lichen planopilaris, and necrobiosis lipoidica (2,3,6,7).
Figure 1.

Scalp with atrophic depigmented alopecic plaques with scarring.
The diagnosis of sarcoidosis relies on histopathologic evidence of non-caseating granulomas, clinical or radiographic signs of sarcoidosis, and the exclusion of other potential causes of disease (1,3). Clinicians must perform a thorough physical examination of the scalp and body when sarcoidosis is suspected (Figure 2) (3). Cutaneous lesions provide easily accessible sites for histologic analysis, which can aid in prompt diagnosis and identification of systemic sarcoidosis, often found in association with scalp disease (1-4,7). Trichoscopy (i.e. polarized light microscopy) of scalp lesions may also aid in the diagnosis of sarcoidosis, typically revealing perifollicular or follicular orange spots, which correspond to granulomas in the superficial dermis with prominent telangiectasis (2,6,7).
Figure 2.
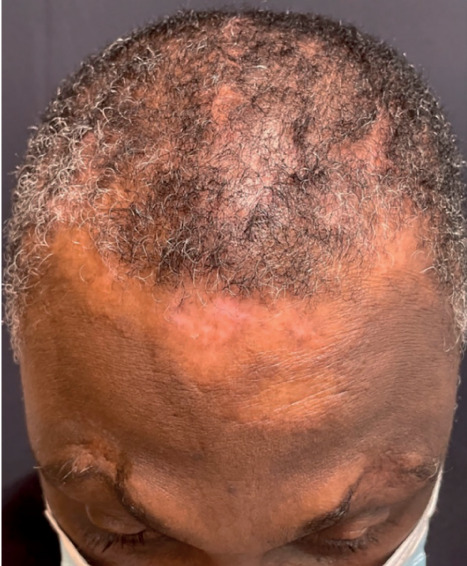
Patient with scarring alopecia on the scalp.
Currently, there is a lack of consensus regarding the treatment of scalp sarcoidosis, as it often proves refractory to various therapies (2-4,7). Considering the high burden of scarring alopecic sarcoidosis, halting the progression of hair loss is a main goal of treatment (2,7). Given its resistance to treatments and the potential for permanent alopecia, early recognition becomes paramount for effective management (2,3). Treatment options include the use of intralesional corticosteroids, topical corticosteroids, oral corticosteroids, antimalarial therapy, and immunosuppressive agents (1-4,7).
A second important goal of early identification of cutaneous sarcoidosis is to identify undiagnosed extracutaneous disease, as skin lesions frequently appear at disease onset and may be the presenting sign of systemic sarcoidosis (2,6,8). In patients with cutaneous and systemic sarcoidosis, skin findings are present before or at the time of systemic diagnosis in 80% of patients (2,8). It is therefore crucial for physicians to be knowledgeable about extrapulmonary manifestations, including those affecting the scalp, to provide comprehensive care to patients. When sarcoidosis is confirmed, further work up for systemic disease, including chest radiography, pulmonary function tests, electrocardiograms, and ophthalmologic examination, is warranted (2-4).
Sarcoidosis can affect individuals from all backgrounds, however, the epidemiology, clinical presentation, and patient outcomes associated with sarcoidosis vary depending on factors such as age, sex, race, and geographic location (1,8-10). Scalp involvement is more frequent in African American women and is often associated with systemic involvement (9,10). In the United States, African American patients with sarcoidosis tend to experience more extensive multi-organ involvement, severe pulmonary disease, and an overall poorer prognosis, marked by higher rates of hospitalization and mortality (9,10). Given the higher incidence and worse outcomes of sarcoidosis in African American populations, recognition of cutaneous sarcoidosis involving the scalp, especially in patients with skin of color, is paramount (9,10).
A collaborative approach in treating sarcoidosis encourages the recognition of diverse clinical presentations, leading to more accurate and timely identification of various organ system manifestations (2). Overall, increasing awareness and knowledge about the diverse manifestations of sarcoidosis, including rare presentations on the scalp, are essential for enhancing patient care, quality of life, and clinical outcomes.
Funding:
This article has no funding source.
Conflicts of Interest:
The authors have no conflicts of interest to declare. These images have not been previously published.
References
- Ezeh N, Caplan A, Rosenbach M, Imadojemu S. Cutaneous Sarcoidosis. Dermatol Clin. 2023;41(3):455–470. doi: 10.1016/j.det.2023.02.012. doi:10.1016/j.det.2023.02.012. [DOI] [PubMed] [Google Scholar]
- Starace M, Brandi N, Baraldi C, Piraccini BM, Alessandrini A. Scalp Sarcoidosis with Systemic Involvement: A Case Report and Literature Review. EMJ. 2019;4(3):63–67. doi: 10.33590/emj/10312099. [Google Scholar]
- Katta R, Nelson B, Chen D, Roenigk H. Sarcoidosis of the scalp: A case series and review of the literature. J Am Acad Dermatol. 2000;42(4):690–692. doi:10.1067/mjd.2000.104679. [PubMed] [Google Scholar]
- La Placa M, Vincenzi C, Misciali C, Tosti A. Scalp sarcoidosis with systemic involvement. J Am Acad Dermatol. 2008;59(5 SUPPL):S126–S127. doi: 10.1016/j.jaad.2008.07.041. doi:10.1016/j.jaad.2008.07.041. [DOI] [PubMed] [Google Scholar]
- Singh R, Wilborn D, Lintzeri DA, Blume-Peytavi U. Health-related quality of life (hrQoL) among patients with primary cicatricial alopecia (PCA): A systematic review. J Eur Acad Dermatol Venereol. 2023 Dec;37(12):2462–2473. doi: 10.1111/jdv.19381. doi: 10.1111/jdv.19381. [DOI] [PubMed] [Google Scholar]
- Torres F, Tosti A, Misciali C, Lorenzi S. Trichoscopy as a clue to the diagnosis of scalp sarcoidosis. Int J Dermatol. 2011;50(3):358–361. doi: 10.1111/j.1365-4632.2010.04711.x. doi:10.1111/J.1365-4632.2010.04711.X. [DOI] [PubMed] [Google Scholar]
- House NS, Welsh JP, English J. Sarcoidosis-induced alopecia. Dermatol Online J. 2012;18(8):4. doi:10.5070/D30FP92370. [PubMed] [Google Scholar]
- Sève P, Pacheco Y, Durupt F, et al. Sarcoidosis: A Clinical Overview from Symptoms to Diagnosis. Cells. 2021;10(4):766. doi: 10.3390/cells10040766. Published 2021 Mar 31. doi:10.3390/cells10040766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hena KM. Sarcoidosis Epidemiology: Race Matters. Front Immunol. 2020;11:537382. doi: 10.3389/fimmu.2020.537382. Published 2020 Sep 15. doi:10.3389/fimmu.2020.537382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rybicki BA, Major M, Popovich J, Jr, Maliarik MJ, Iannuzzi MC. Racial differences in sarcoidosis incidence: a 5-year study in a health maintenance organization. Am J Epidemiol. 1997;145(3):234–241. doi: 10.1093/oxfordjournals.aje.a009096. doi:10.1093/oxfordjournals.aje.a009096. [DOI] [PubMed] [Google Scholar]


