Abstract
PURPOSE:
The purpose of this study was to examine the prevalence of urinary (UI), fecal (FI), and dual incontinence (DI) in older adults and their association with urinary tract infections, dermatitis, slips and falls, and behavioral disturbances based on Medicare fee-for-service (FFS) claims data.
DESIGN:
Retrospective analysis.
SUBJECTS AND SETTINGS:
Data from administrative claims from the CMS Medicare Limited Data Set (5% sample) for all months in 2018 were reviewed. The analysis was limited to FFS Medicare beneficiaries, with minimum of 3-month enrollment in Parts A and B who were at least 65 years old. This cohort included 1.2 million beneficiaries in the United States.
METHODS:
We used diagnosis codes to identify members with incontinence and grouped these members into 3 categories (UI only, FI only, and DI). We also divided claims based on 4 sites of care (nursing home, skilled nursing facility, home health, and self- or family care). We then determined the prevalence of (1) urinary tract infections (UTIs), (2) dermatitis, (3) slips and falls, and (4) behavioral disturbances for each type of incontinence.
RESULTS:
We found that 11.2% of Medicare members had a claims-based diagnosis of incontinence in 2018. On average, those diagnosed with incontinence experienced 5 times more UTIs, 2 times as many dermatitis events, more than twice as many slips and falls, and 2.8 times more behavior disturbances compared to those without an incontinence diagnosis. For those with DI, the prevalence of the 4 outcomes was significantly higher (between 22% and 185%) compared to those with UI only.
CONCLUSIONS:
Findings show that Medicare beneficiaries diagnosed as incontinent experience a much higher prevalence of UTIs, dermatitis, slips and falls, and behavioral disturbances compared to those without a diagnosis of incontinence. Our results suggest that incontinence may be an important indicator diagnosis for multiple other conditions and, if not well-managed, may challenge the desire for those who are incontinent to age at home.
Keywords: Administrative claims, Behavioral disturbances, Fecal incontinence, Incontinence-associated dermatitis, Medicare fee-for-service, Prevalence, Slips and falls, Urinary incontinence, Urinary tract infections
Video Abstract
Video 1 The Prevalence of Incontinence and Its Association With Urinary Tract Infections, Dermatitis, Slips and Falls, and Behavioral Disturbances Among Older Adults in Medicare Fee-for-Service
INTRODUCTION
Urinary incontinence (UI) and fecal incontinence (FI) affect millions of individuals older than 65 years in the United States and are reported to have a larger effect on health-related quality of life than diabetes mellitus, cancer, or arthritis.1 The likelihood of incontinence increases with age, increased body mass index, and diabetes mellitus; rates are also higher in men undergoing any type of prostate surgery and among women following pregnancy or vaginal delivery.2–5 With the exception of serious injuries, surgeries, or childhood diseases such as spina bifida, incontinence often starts as small, intermittent losses of urine that gradually increases in severity over time, particularly when the individual experiences certain comorbid conditions that affect lower urinary tract function or mobility.6
The prevalence of UI in those 65 years or older is as high as 60% for women and 35% for men 65 years or older.7,8 Fecal incontinence is estimated to affect about a quarter to a third of those with UI older than 50 years.9 Urinary incontinence, particularly when paired with FI, is a leading cause of admission to nursing homes and skilled care settings.2,10,11 Although only about 10% of the Medicare population is in an institutional setting (long-term care or skilled nursing facility [SNF]), an estimated 45% to 60% of those Medicare beneficiaries have UI.2,10–12 The prevalence of FI in institutions is less well known, but 3 studies suggest that half to three-fourths of institutional residents who experience UI may also experience FI, with a higher prevalence of FI among men.2,5,7,12
The remaining Medicare population is aging at home independently or being cared for by family or receiving care from a home health agency or hospice care. The prevalence of UI in the home setting is estimated to be 46% for female Medicare beneficiaries and 28% for male beneficiaries, with about 10% experiencing dual incontinence (DI), that is, UI and FI.2 For those under hospice care, the rate of UI is more than 60%, with almost half of those experiencing both UI and FI.2
The most common management strategy for UI is the use of disposable body-worn absorbent products (BWAPs), although surgery, medications, and other types of preventive or collection medical devices are also available. For those using a BWAP, the most common mode of failure is leakage that can result in several complications for the individual including an increase in slips and falls,13 incontinence-associated dermatitis (IAD),14–16 serious wounds or infections including UTIs, and a reduction in sleep quality that can contribute to cognitive decline and behavioral disturbances.17 Incontinence has been associated with both an increased need for care assistance and an increased turnover of caregivers.18,19
Despite the emotional distress and financial burden to the individuals and to the society, incontinence is often underreported.16 Reported incontinence prevalence varies widely due to difference in study designs, the method used to measure incontinence, the definition of incontinence, and sample selection. The primary purpose of this study was to examine the prevalence of UI, FI, and DI in older adults and their association with urinary tract infections (UTIs), dermatitis, slips and falls, and behavioral disturbances based on Medicare fee-for-service (FFS) claims data. Secondarily, we examined the prevalence of incontinence and its association with the 4 outcomes based on 4 sites of care: nursing home, SNF, home health, and self- or family care.
METHODS
This is a retrospective analysis that relied on administrative claims data from the CMS Medicare Limited Data Set (5% sample) to identify the prevalence of incontinence over all months in 2018. The target population was Medicare FFS beneficiaries (ie, we excluded Medicare Advantage [MA] beneficiaries) because of gaps in claims reporting in the MA beneficiary segment. To reduce duration bias caused by beneficiaries who have minimal exposure to Medicare, we also required at least 3 months of enrollment per member. Our analysis includes only the over-65 Medicare population, which we find to represent approximately 75% of the FFS beneficiary group. These criteria yielded approximately 1.2 million FFS beneficiaries with coverage in 2018 in the United States.
Outcome Measures
To identify UI and FI in the longitudinal sample population, we used International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) diagnosis codes captured in their claims experience for utilization analysis. Codes for relevant diagnoses, identified in any position on a claims record, are provided in the Appendix. Incontinent members were grouped into 3 mutually exclusive categories using the code list: UI only, FI only, and DI that included members with both UI and FI.
Member records were then divided into 4 categories based on care setting: nursing home, SNF, home health, and self- or family care according to the most resource-intensive site in which they received care during 2018. The resource intensity was assumed greatest for SNFs, followed by nursing home, home health, and self- or family care. The Centers for Medicare & Medicaid Services (CMS) considers an SNF to be a facility that primarily provides inpatient skilled nursing care and related services to patients who require medical, nursing, or rehabilitative services but does not provide the level of care or treatment available in a hospital. A nursing home, which includes assisted living, can do the same but offers, on a regular basis, health-related care services above the level of custodial care (https://www.cms.gov/medicare/coding/place-of-service-codes).
We also identified 4 healthcare events for each cohort: (1) UTIs; (2) dermatitis (we used multiple codes since the current code for incontinence-associated irritant dermatitis has not been added to ICD-10-CM in 2018); (3) slips, falls, and related fractures; and (4) claims associated with a behavioral disturbance (see the Appendix). The existence of these healthcare events was determined based on the presence of a relevant diagnosis code in the claims experience (see the Appendix). One additional instrument that we used was the risk score for each member. We applied the CMS-HCC Risk Adjustment Model developed by CMS to generate risk scores for each member in our studied population. In the model, a select number of diagnosis codes were grouped into various Hierarchical Chronic Categories (HCCs) and each of the HCCs consists of acute or chronic conditions that are clinically related and have similar pattern in healthcare expenditures. The risk score for each member was calculated based on their demographic factors (age and gender) and the disease factors captured in the HCCs. Higher risk score often associates with more severe health condition of a member.
The Office of Research Human Subjects Department at the University of California, Santa Barbara, reviewed this work and determined that it did not meet the criteria for human subjects research as defined in the Common Rule (45 CFR 46). Institutional Review Board review and oversight were not required because the activity does not involve “human subjects” as defined under 45 CFR 46.102 and the research team is not accessing identifiable patient information.
Data Analysis
All results in this paper were generated using SAS software version 9.4 (SAS Institute Inc, Cary, North Carolina). Within each incontinent cohort, we summarized demographic statistics: average age, gender, and the average risk score. Additionally, we estimated the prevalence and the conditional average of the 4 identified healthcare events by incontinence cohorts and care settings. The prevalence for each event is defined as the number of members within each cohort who experienced at least one event during 2018. The conditional average number of events is the average number of events for members in a cohort who experienced at least one event in 2018. Member characteristics and the occurrence of each event by care settings and cohorts were compared using 2-sample z-tests, where we assumed normality assumption holds due to large sample size. We reported the level of P value from each test, where we set the level of significance to be .05.
RESULTS
Summary statistics of those diagnosed as incontinent in 2018 by site of service and type of incontinence are presented in Table 1. In 2018, 11.2% of the members were diagnosed with UI, FI, or DI. The prevalence of incontinence was higher in places of service that offer more intensive care: 20.6% for SNFs, 16.6% for nursing homes, 24.5% for those receiving formal healthcare at home, and 8.6% under self/family care. In addition, 62% of those with DI were receiving some type of formal care, either institutional or home healthcare, as compared to 36% of those diagnosed with UI alone.
TABLE 1. Summary Statistics for Incontinent and Not Incontinent Populations, 2018a.
| Metrics | Nursing Home (n = 10,635) | SNF (n = 52,168) | Home Health (n = 160,736) | Home: Self- or Family Care (n = 1,019,634) | Total (N = 1,243,173) | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Inco. Cohort | Not Inco. Cohort | Inco. Cohort | Not Inco. Cohort | Inco. Cohort | Not Inco. Cohort | Inco. Cohort | Not Inco. Cohort | Inco. Cohort | Not Inco. Cohort | |
| Urinary incontinence | ||||||||||
| Prevalence | 13.5% of 10,635 | 17.3% of 52,168 | 21.5% of 160,736 | 7.9% of 1,019,634 | 10.1% of 1,243,173 | |||||
| Female | 71.1% | 70.5% | 65.7%*** | 63.7% | 65.6%*** | 61.6% | 63.0%*** | 54.8% | 64.0%*** | 56.0% |
| Average risk score | 2.18** | 1.86 | 3.51*** | 2.95 | 3.17*** | 2.70 | 1.36*** | 1.04 | 2.00*** | 1.28 |
| Average age, y | 83.0 | 84.0 | 81.0** | 82.0 | 81.0*** | 80.0 | 76.0*** | 74.0 | 78.0*** | 75.0 |
| Fecal incontinence | ||||||||||
| Prevalence | 0.5% of 10,635 | 0.8% of 52,168 | 0.9% of 160,736 | 0.4% of 1,019,634 | 0.5% of 1,243,173 | |||||
| Female | 62.9% | 70.5% | 64.9% | 63.7% | 63.8%* | 61.6% | 69.9%*** | 54.8% | 68.2%*** | 56.0% |
| Average risk score | 2.52 | 1.86 | 4.06** | 2.95 | 3.51*** | 2.70 | 1.44*** | 1.04 | 2.07*** | 1.28 |
| Average age, y | 84.0 | 84.0 | 80.0 | 82.0 | 80.0 | 80.0 | 76.0*** | 74.0 | 77.0*** | 75.0 |
| Urinary and fecal incontinence (DI) | ||||||||||
| Prevalence | 2.6% of 10,635 | 2.5% of 52,168 | 2.2% of 160,736 | 0.3% of 1,019,634 | 0.7% of 1,243,173 | |||||
| Female | 71.8% | 70.5% | 63.4% | 63.7% | 64.0%** | 61.6% | 76.8%*** | 54.8% | 69.14%*** | 56.0% |
| Average risk score | 2.34* | 1.86 | 3.90*** | 2.95 | 3.77*** | 2.70 | 1.71*** | 1.04 | 2.95*** | 1.28 |
| Average age, y | 83.0 | 84.0 | 82.0 | 82.0 | 81.0** | 80.0 | 77.0*** | 74.0 | 80.0*** | 75.0 |
| All incontinence | ||||||||||
| Prevalence | 16.6% of 10,635 | 20.6% of 52,168 | 24.5% of 160,736 | 8.6% of 1,019,634 | 11.2% of 1,243,173 | |||||
| Share of UI with FI | 16.1% of 1,710 | 12.5% of 10,329 | 9.1% of 37,961 | 3.7% of 83,502 | 6.1% of 133,502 | |||||
| Female | 71.0% | 70.5% | 65.4% | 63.7% | 65.4% | 61.6% | 63.8% | 54.8% | 64.5% | 56.0% |
| Average risk score | 2.22 | 1.86 | 3.58 | 2.95 | 3.25 | 2.70 | 1.38 | 1.04 | 2.08 | 1.28 |
| Average age, y | 83.0 | 84.0 | 81.1 | 82.0 | 81.1 | 80.0 | 81.0 | 74.0 | 78.1 | 75.0 |
Abbreviations: DI, dual incontinence; FI, fecal incontinence; Inco, incontinent; Not Inco., not incontinent; SNF, skilled nursing facility; UI, urinary incontinence.
aAsterisks represent significant difference between the incontinent and not incontinent groups within each place-of-service setting: ***P < .0001; **P < .05; *P < .10.
We then analyzed the prevalence of documented healthcare events in Table 2. In nearly all settings, the rates of UTIs, dermatitis, slips and falls, and behavioral disturbances were statistically significantly higher in the incontinent cohort than in those without a diagnosis of incontinence. Specifically, those with UI were more likely to have at least one UTI than nonincontinent members (39.2% vs 12.9%; P = .0001). Conditional on having a UTI, urinary incontinent members will have 1.6 more UTIs than someone who has not been identified as incontinent (4.31 vs 2.69; P = .0001). The difference increases for those with DI; beneficiaries with DI were significantly more likely to have at least one UTI (47.9% vs 12.9%; P = .0001) and, conditional on having a UTI, will have significantly more UTIs than beneficiaries not diagnosed with incontinence (5.61 vs 2.69; P = .0001).
TABLE 2. Summary of 2018 Urinary and Fecal Incontinent Groups by Places of Servicea.
| Metrics | Nursing Home | SNF | Home Health | Home/Self-care | Total | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Inco. Cohort | Not Inco. Cohort | Inco. Cohort | Not Inco. Cohort | Inco. Cohort | Not Inco. Cohort | Inco. Cohort | Not Inco. Cohort | Inco. Cohort | Not Inco. Cohort | ||
| Urinary incontinence | |||||||||||
| UTIs | Prevalence | 42.6%*** | 26.0% | 60.5%*** | 38.4% | 54.5%*** | 30.3% | 30.2%*** | 9.4% | 39.2%*** | 12.9% |
| Cond. Average | 3.34*** | 2.66 | 6.16*** | 4.30 | 5.67*** | 3.71 | 2.88*** | 1.96 | 4.31*** | 2.69 | |
| Dermatitis | Prevalence | 7.9%*** | 4.4% | 10.7%*** | 6.4% | 9.2%*** | 6.2% | 6.7%*** | 4.1% | 7.7%*** | 4.5% |
| Cond. Average | 2.02*** | 1.75 | 2.21*** | 2.04 | 1.80*** | 1.67 | 1.47*** | 1.41 | 1.66*** | 1.49 | |
| Slips and falls | Prevalence | 47.1%*** | 39.6% | 66.4%*** | 56.2% | 71.7%*** | 60.8% | 31.6%*** | 22.2% | 45.3%*** | 27.8% |
| Cond. Average | 4.54*** | 3.81 | 7.10*** | 6.29 | 7.25*** | 6.17 | 3.49*** | 3.15 | 5.52*** | 4.12 | |
| Fall-related injuries | Prevalence | 17.6%*** | 13.8% | 27.8%*** | 22.2% | 27.8%*** | 21.4% | 6.6%*** | 3.8% | 14.2%*** | 6.6% |
| Cond. Average | 2.16** | 1.73 | 2.57 | 2.48 | 2.64*** | 2.44 | 1.52*** | 1.43 | 2.29*** | 1.95 | |
| Behavioral disruptions | Prevalence | 19.9% | 19.9% | 21.3% | 21.5% | 10.2%*** | 6.8% | 1.3%*** | 0.6% | 5.4%*** | 2.2% |
| Cond. Average | 6.02** | 5.29 | 6.39 | 6.29 | 4.75*** | 4.46 | 3.16*** | 2.98 | 5.03*** | 4.88 | |
| Fecal incontinence | |||||||||||
| UTIs | Prevalence | 32.1% | 26.0% | 52.3%*** | 38.4% | 45.0%*** | 30.3% | 18.3%*** | 9.4% | 26.8%*** | 12.9% |
| Cond. Average | 3.41 | 2.66 | 4.81** | 4.30 | 5.05*** | 3.71 | 2.35*** | 1.96 | 3.73*** | 2.69 | |
| Dermatitis | Prevalence | 0.0% | 4.4% | 9.30%*** | 6.4% | 10.04%*** | 6.2% | 6.83%*** | 4.1% | 7.68%*** | 4.5% |
| Cond. Average | 0/00 | 1.75 | 2.87*** | 2.04 | 1.97*** | 1.67 | 1.58** | 1.41 | 1.80*** | 1.49 | |
| Slips and falls | Prevalence | 45.3% | 39.6% | 66.8%*** | 56.2% | 73.7%*** | 60.8% | 33.2%*** | 22.2% | 44.9%*** | 27.8% |
| Cond. Average | 7.0** | 3.81 | 6.75 | 6.29 | 6.77** | 6.17 | 3.33** | 3.15 | 5.01*** | 4.12 | |
| Fall-related injuries | Prevalence | 14.3%*** | 12.7% | 28.5%*** | 23.7% | 26.5%*** | 22.7% | 6.8%*** | 4.0% | 12.8%*** | 7.3% |
| Cond. Average | 2.0 | 1.8 | 2.64 | 2.50 | 2.64 | 2.49 | 1.45 | 1.40 | 2.18* | 2.01 | |
| Behavioral disruptions | Prevalence | 11.3% | 19.9% | 19.1% | 21.5% | 9.7%*** | 6.8% | 1.2%*** | 0.6% | 4.5%*** | 2.2% |
| Cond. Average | 3.67*** | 5.29 | 5.55** | 6.29 | 4.52 | 4.46 | 3.14*** | 2.98 | 4.53*** | 4.88 | |
| Urinary and fecal incontinence (DI) | |||||||||||
| UTIs | Prevalence | 35.5%*** | 26.0% | 54.5%*** | 38.4% | 58.7%*** | 30.3% | 34.0%*** | 9.4% | 47.9%*** | 12.9% |
| Cond. Average | 3.68** | 2.66 | 6.34*** | 4.30 | 6.51*** | 3.71 | 3.52** | 1.96 | 5.61*** | 2.69 | |
| Dermatitis | Prevalence | 6.2% | 4.4% | 11.7%*** | 6.4% | 11.5%*** | 6.2% | 8.2%*** | 4.1% | 9.9%*** | 4.5% |
| Cond. Average | 2.59*** | 1.75 | 3.48*** | 2.04 | 2.05*** | 1.67 | 1.66*** | 1.41 | 2.20*** | 1.49 | |
| Slips and falls | Prevalence | 57.3%*** | 39.6% | 68.7%*** | 56.2% | 77.0%*** | 60.8% | 43.3%*** | 22.2% | 62.3%*** | 27.8% |
| Cond. Average | 5.68*** | 3.81 | 7.40*** | 6.29 | 8.18*** | 6.17 | 4.16*** | 3.15 | 6.91*** | 4.12 | |
| Fall-related injuries | Prevalence | 17.7%*** | 14.2% | 26.0%*** | 23.8% | 30.3%*** | 22.6% | 10.8%*** | 4.0% | 22.0%*** | 7.3% |
| Cond. Average | 1.93 | 1.79 | 2.51 | 2.50 | 2.81** | 2.49 | 1.79*** | 1.45 | 2.54*** | 2.00 | |
| Behavioral disturbance | Prevalence | 27.5%*** | 19.9% | 27.9%*** | 21.5% | 19.0%*** | 6.8% | 4.9%*** | 0.6% | 15.4%*** | 2.2% |
| Cond. Average | 5.17 | 5.29 | 5.93** | 6.29 | 5.15*** | 4.46 | 4.01*** | 2.98 | 5.24*** | 4.88 | |
Abbreviations: Cond. Average, conditional average, or the average count conditional on having at least one observation; DI, dual incontinence; FI, fecal incontinence; Inco, incontinent; Not Inco., and not incontinent; SNF, skilled nursing facility; UI, urinary incontinence; UTI, urinary tract infection.
aAsterisks represent significant difference between the incontinent and not incontinent groups within each place-of-service setting: ***P < .0001; **P < .05; *P < .1.
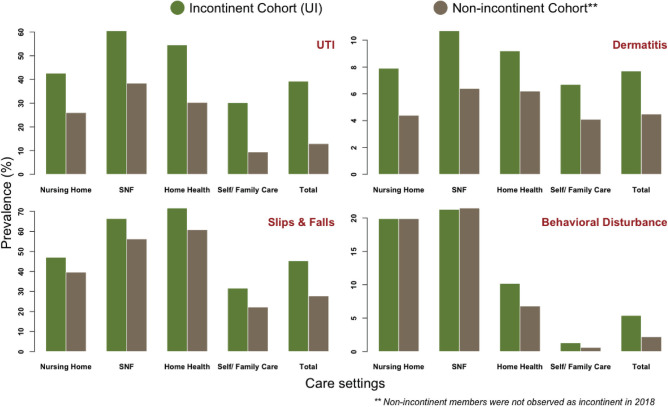
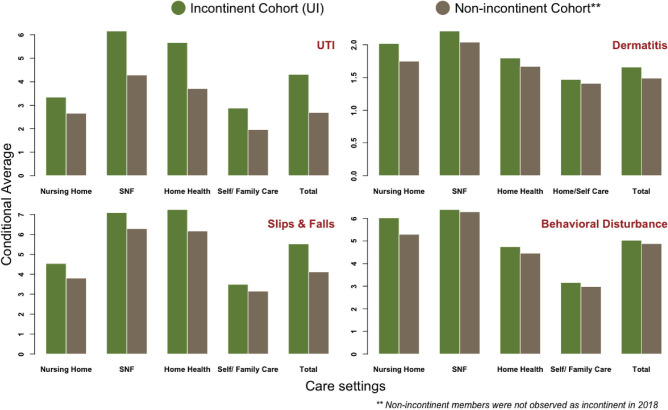
Analysis of dermatitis, slips and falls, and behavioral disturbances revealed similar findings (Figure 1). Those with UI, on average, are 72% more likely to have dermatitis (7.7% vs 4.5%; P = .0001), 63% more likely to experience a slip and fall (45.3% vs 27.8%; P = .0001), and more likely to experience a behavioral disturbance compared to those without an UI diagnosis (5.4% vs 2.2%; P = .0001). Once beneficiaries experience one of these conditions, they, on average, have 12% more dermatitis episodes (1.66 vs 1.49; P = .0001), 34% more slips and falls (5.52 vs 4.12; P = .0001), and 3% more behavioral disruptions than those without observed incontinence (5.03 vs 4.88; P = .0001; Figure 2). Beneficiaries diagnosed with incontinence were more than twice as likely to have fall-related injuries (14.2% vs 6.6%; P = .0001) compared to nonincontinent members. In addition, the frequency of fall-related injuries for incontinent members was significantly higher than beneficiaries without an incontinence diagnosis (2.29 vs 1.95; P = .05).
Figure 1.
Association between urinary incontinence and UTIs, dermatitis, slips and falls, and behavioral disturbances by care setting: prevalence. SNF indicates skilled nursing facility; UI, urinary continence; UTI, urinary tract infection.
Figure 2.
Association between urinary incontinence and UTIs, dermatitis, slips and falls, and behavioral disturbances by care setting: conditional average. SNF indicates skilled nursing facility; UI, urinary continence; UTI, urinary tract infection.
We found that members with a higher prevalence of UTIs, dermatitis, slips and falls, or behavioral disturbances were cared for by places of service with more intensive care. For example, in the most intensive places of service, SNFs, 60.5% of incontinent members in 2018 had at least one UTI, with a conditional average of more than 6 UTIs in 2018. In contrast, for those aging at home under self-care, 30.2% of incontinent members had at least one UTI, with a conditional average of 2.9 UTIs in 2018 (Table 1). Similarly, in 2018, 66.4% of incontinent members in an SNF had at least one slip or fall compared to 31.6% of incontinent members aging at home.
DISCUSSION
To the best of our knowledge, this is the first analysis of Medicare claims data to directly measure the prevalence of incontinence. We found that 11.2% of the members were diagnosed with incontinence in 2018. This percentage falls below estimates of incontinence prevalence in adults 65 years or older.7,8 We hypothesize that the rate we found is lower because CMS claims data on incontinence are incomplete, as found in other data sets.16 A well-known limitation of claims data, including CMS claims data, is the lack of clinical evaluation. Other studies have gone through painstaking effort to evaluate large amounts of clinical data to ascertain the true prevalence of UI.20–22 We hypothesize that the incontinent population identified through claims in the CMS data is likely to miss many of those with light or moderate incontinence because that is less likely to be diagnosed by a clinical professional and less likely to be identified as a comorbidity when compared to more severe incontinence.23,24
The FI results in Table 1 also suggest that CMS data are missing many individuals with FI. The literature predicts that between half and three-fourths of those in SNFs with UI also experience FI. Nelson20 reports that the prevalence of FI in nursing homes may be as high as 50%, while Leung and Schnelle7 estimate this prevalence to be as high as 65%. As reported in Table 1, FI was only documented in 16% of those with UI in nursing homes, 12% in SNFs, and 9% in home health. Identifying the missing urinary and fecal incontinent members is a topic of other research.23
We analyzed the prevalence of pertinent healthcare events and comorbid conditions within the incontinent population. The prevalence of UTIs, dermatitis, slips and falls, and behavioral disturbances was statistically significant higher for those with incontinence compared to those without. On average, those diagnosed with incontinence in 2018 will experience 5 times more UTIs, 2 times as many dermatitis events, more than twice as many slips and falls, and 2.8 times more behavioral disruptions compared to those not diagnosed with incontinence in 2018. We also found, consistent with the literature, that members with a higher incidence of these 4 events were more likely to be receiving care in places of service with higher intensity of care.21,22
Findings from this study indicate that the 4 events are significantly higher among those who experience DI relative to those with only UI. For example, the prevalence of a UTI in 2018 increases from 39% to 48% for those diagnosed with DI compared to those with just a UI diagnosis. Similarly, the prevalence of dermatitis in 2018 increases from 8% to 10%, the prevalence of slips and falls increases from 45% to 62%, and the rate of behavioral disturbances in a nursing home increases from 5% to 15%. These results, ranging from 22% higher to 185% higher, are consistent with the significant increase in risk to skin health posed by the combination of feces and urine.14
Limitations and Considerations
Our approach in using Medicare claims data to assess the prevalence of incontinence is subject to several limitations. First, our database does not contain any drug records, though this limitation may exert only a small influence, given the small proportion of these patients who are managed by drugs.25,26 Second, we identify patients through administrative claims and thus we do not have access to clinical information to determine members' diagnosis and severity. This is particularly relevant in our evaluation of dermatitis. To the extent that dermatitis is associated with exposure to urine and/or feces, it would be classified as IAD, but in 2018, there was not an ICD-10 code for IAD and the codes that were available in 2018 would capture dermatitis events unrelated to such exposures.14–16 Thus, the absence of clinical information precludes our ability to isolate the prevalence of IAD within our sample.
Third, our recorded incontinence prevalence is less than that which has been estimated in the literature, suggesting that incontinence is either not sufficiently severe to result in a formal diagnosis or physicians are not incented to code the incontinence diagnosis. Undercoding is well known in Medicare FFS compared with MA.27,28 Another explanation is that patients may be reluctant to discuss incontinence with their primary care physicians due to the perceived social stigma.29,30 Finally, we note that our analysis does not allow us to claim that incontinence is the cause of the comorbidities analyzed, but only that there is a correlation between incontinence and the comorbidities.
CONCLUSIONS
We evaluated a large cohort of Medicare beneficiaries residing in the United States and found that incontinence is associated with a disproportionately higher incidence of UTIs, dermatitis, slips and falls, and behavioral disturbances relative to those without an incontinence diagnosis. The high frequency of these events can have serious negative health and well-being effects for those with incontinence and may cause a change in the place of service to one of increasing intensity of care. This shift away from self- or family care increases the burden on institutions that already struggle with attracting and retaining staff.31 We found that DI, in particular, is highly correlated with conditions that require more intensive care and may trigger a transition to nursing or skilled nursing care. Consequently, investments in the successful management of incontinence at home are strongly recommended to enable the population to age at home.
ACKNOWLEDGMENT
The authors thank Elaine Zhao, ASA, MAAA, and Maggie Richard, FSA, MAAA, for research assistance. Funding for this article was provided by Principle Business Enterprises Inc.
APPENDIX: ICD-10 Diagnosis Code List for Incontinence and Related Conditions.
| Condition | ICD-9 Diagnosis Code | ICD-10 Diagnosis Code |
|---|---|---|
| Urinary incontinence | 788.30 | R32 Unspecified urinary incontinence |
| 788.63 | R39.15 Urge Incontinence | |
| 788.91 | R39.81 Functional urinary incontinence | |
| 596.54, 596.59 | N31.9 Neurogenic bladder | |
| 596.51 | N32.81 Overactive bladder | |
| 596.6, 596.7, 596.89 | N32.89 Bladder spasm | |
| 625.6, 788.32 | N39.3 Stress incontinence (female) (male) | |
| 788.31 | N39.41 Urge incontinence | |
| 788.34 | N39.42 Incontinence without sensory awareness | |
| 788.33 | N39.46 Stress and urge incontinence | |
| 788.36 | N39.44 Nocturnal urinary Incontinence | |
| N/A | N39.492 postural (urinary) incontinence | |
| 788.39 | N39.498 reflex urinary incontinence | |
| Fecal incontinence | &a | R15 Fecal incontinence |
| &a | R15.0 Incomplete defecation | |
| &a | R15.1 Fecal smearing | |
| &a | R15.2 Fecal urgency | |
| &a | R15.9 Full incontinence of feces | |
| &a | R98.1 Fecal incontinence, nonorganic origin | |
| &a | K59.2 Neurogenic bowel | |
| Urinary tract infections | 599.0 | N39.0 Urinary tract infection, site not specified |
| 595 | N30 Cystitis | |
| 597.0, 099.4, 597.8 | N34 Urethritis and urethral syndrome | |
| Incontinence-associated dermatitis or perineal dermatitis | 691.0 | L22 Diaper dermatitis |
| N/A | L30.9 Dermatitis, unspecified | |
| N/A | L24.9 Irritant contact dermatitis, unspecified cause | |
| 112.3 | B37.2 Candidiasis of skin and nail | |
| 112.1 | B37.3 Candidiasis of vulva and vagina | |
| Slips, falls, and fractures | N/A | R29.6 Repeated falls |
| V15.88 | Z91.81 history of falling | |
| E880-E884, E885.9, E886.0, E887-E888, E917.7, E917.8, E929.3 | W00-W19 Slipping, tripping, stumbling, and falls | |
| 800-826, 830-908, 910-918, 921-929, 950-957, 959, V54.1 | S00-S99 (Injuries of external causes) | |
| Behavioral disturbances | 294.11 | F02.81 Alzheimer's dementia late onset with behavioral disturbance |
| 294.21 | F03.91 Unspecified dementia with behavioral disturbance | |
| 331.19 | G31.09 Dementia with Parkinsonism plus F02.81 dementia with behavioral disturbance | |
| 306.8 | F59 Unspecified behavioral syndromes associated with physiological disturbances and physical factor | |
| 312.9 | F91.9 Conduct disorder |
Abbreviations: ICD-9, International Classification of Diseases, Ninth Revision; ICD-10, International Classification of Diseases, Tenth Revision; N/A, not applicable.
aUsed ICD-9 codes for the analysis of latent incontinence and did not evaluate fecal incontinence.
Footnotes
The authors declare no conflicts of interest.
Contributor Information
Ian Duncan, Email: duncan@pstat.ucsb.edu.
Andrew Stocking, Email: astocking@pbenet.com.
Karen Fitzner, Email: kfitzner@sbactuaries.com.
Tamim Ahmed, Email: kfitzner@sbactuaries.com.
Nhan Huynh, Email: nhuynh@sbactuaries.com.
REFERENCES
- 1.Hawkins K, Pernarelli J, Ozminkowski RJ, et al. The prevalence of urinary incontinence and its burden on the quality of life among older adults with Medicare supplement insurance. Qual Life Res. 2011;20(5):723–732. [DOI] [PubMed] [Google Scholar]
- 2.Gorina Y, Schappert S, Bercovitz A, Elgaddal N, Kramarow E. Prevalence of incontinence among older Americans. In: Vital and Health Statistics Series 3, Analytical and Epidemiological Studies. Atlanta, GA: National Center for Health Statistics, Centers for Disease Control and Prevention; 2014. [PubMed] [Google Scholar]
- 3.Markland AD, Richter HE, Fwu C-W, Eggers P, Kusek JW. Prevalence and trends of urinary incontinence in adults in the United States, 2001 to 2008. J Urol. 2011;186(2):589–593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Menees SB, Almario CV, Spiegel BMR, Chey WD. Prevalence of and factors associated with fecal incontinence: results from a population-based survey. Gastroenterology. 2018;154(6):1672–1681.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Musa MK, Saga S, Blekken LE, Harris R, Goodman C, Norton C. The prevalence, incidence, and correlates of fecal incontinence among older people residing in care homes: a systematic review. J Am Med Dir Assoc. 2019;20(8):956–962.e8. [DOI] [PubMed] [Google Scholar]
- 6.Hagan KA, Erekson E, Austin A, et al. A prospective study of the natural history of urinary incontinence in women. Am J Obstet Gynecol. 2018;218(5):502.e1–502.e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Leung FW, Schnelle JF. Urinary and fecal incontinence in nursing home residents. Gastroenterol Clin North Am. 2008;37(3):697–707, x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Luo Y, Zou P, Wang K, Li X, Wang J. Prevalence and risk factors of urinary incontinence among elderly adults in rural China. J Wound Ostomy Continence Nurs. 2022;49(1):78–86. [DOI] [PubMed] [Google Scholar]
- 9.Wu JM, Mathews CA, Vaughan CP, Markland AD. Urinary, fecal, and dual incontinence in older U.S. adults. J Am Geriatr Soc. 2015;63(5):947–953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tunis SR, Norris A, Simon K.Decision Memo for Biofeedback for Urinary Incontinence (CAG-00020N). Baltimore, MD: CMS.gov; 2000. [Google Scholar]
- 11.Barakat-Johnson M, Barnett C, Lai M, Wand T, White K. Incontinence, incontinence-associated dermatitis, and pressure injuries in a health district in Australia: a mixed-methods study. J Wound Ostomy Continence Nurs. 2018;45(4):349–355. [DOI] [PubMed] [Google Scholar]
- 12.Bliss DZ, Savik K, Harms S, Fan Q, Wyman JF. Prevalence and correlates of perineal dermatitis in nursing home residents. Nurs Res. 2006;55(4):243–251. [DOI] [PubMed] [Google Scholar]
- 13.Chiarelli PE, Mackenzie LA, Osmotherly PG. Urinary incontinence is associated with an increase in falls: a systematic review. Aust J Physiother. 2009;55(2):89–95. [DOI] [PubMed] [Google Scholar]
- 14.Gray M, Guiliano KK. Incontinence-associated dermatitis, characteristics and relationship to pressure injury: a multisite epidemiologic analysis. J Wound Ostomy Continence Nurs. 2018;45(1):63–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ostaszkiewicz J, Tomlinson E, Hunter K. The effects of education about urinary incontinence on nurses' and nursing assistants' knowledge, attitudes, continence care practices, and patient outcomes: a systematic review. J Wound Ostomy Continence Nurs. 2020;47(4):365–380. [DOI] [PubMed] [Google Scholar]
- 16.Kayser SA, Koloms K, Murray A, Khawar W, Gray M. Incontinence and incontinence-associated dermatitis in acute care: a retrospective analysis of total cost of care and patient outcomes from the premier healthcare database. J Wound Ostomy Continence Nurs. 2021;48(6):545–552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ge TJ, Vetter J, Lai HH. Sleep disturbance and fatigue are associated with more severe urinary incontinence and overactive bladder symptoms. Urology. 2017;109:67–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Langa KM, Fultz NH, Saint S, Kabeto MU, Regula Herzog A. Informal caregiving time and costs for urinary incontinence in older individuals in the United States. J Am Geriatr Soc. 2002;50(4):733–737. [DOI] [PubMed] [Google Scholar]
- 19.Wilson L, Brown JS, Shin GP, Luc KO, Subak LL. Annual direct cost of urinary incontinence. Obstet Gynecol. 2001;98(3):398–406. [DOI] [PubMed] [Google Scholar]
- 20.Nelson RL. Epidemiology of fecal incontinence. Gastroenterology. 2004;126(1)(suppl 1):S3–S7. [DOI] [PubMed] [Google Scholar]
- 21.Bliss DZ, Harms S, Garrard JM, et al. Prevalence of incontinence by race and ethnicity of older people admitted to nursing homes. J Am Med Dir Assoc. 2013;14(6):451.e1–451.e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Roe B, Flanagan L, Jack B, et al. Systematic review of the management of incontinence and promotion of continence in older people in care homes: descriptive studies with urinary incontinence as primary focus. J Adv Nurs. 2011;67(2):228–250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Stocking A, Duncan I, Huynh N. Estimating under-diagnosis of patients in chronically-ill populations. N Am Actuar J. 2003. doi:10.1080/10920277.2023.2281471. [Google Scholar]
- 24.Coyne KS, Wein A, Nicholson S, Kvasz M, Chen C-I, Milsom I. Comorbidities and personal burden of urgency urinary incontinence: a systematic review. Int J Clin Pract. 2013;67(10):1015–1033. [DOI] [PubMed] [Google Scholar]
- 25.Thirugnanasothy S. Managing urinary incontinence in older people. BMJ. 2010;341:c3835. [DOI] [PubMed] [Google Scholar]
- 26.Holroyd-Leduc JM, Straus SE. Management of urinary incontinence in women: scientific review. JAMA. 2004;291(8):986–995. [DOI] [PubMed] [Google Scholar]
- 27.Kronick R, Welch WP. Measuring coding intensity in the Medicare Advantage Program. Medicare Medicaid Res Rev. 2014;4(2):mmrr2014.004.02.a06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kronick R. Projected coding intensity in Medicare Advantage could increase Medicare spending by $200 billion over 10 years. Health Aff (Millwood). 2017;36(2):320–327. [DOI] [PubMed] [Google Scholar]
- 29.Bardsley A. An overview of urinary incontinence. Br J Nurs. 2016;25(18):S14–S21. [DOI] [PubMed] [Google Scholar]
- 30.Brown HW, Guan W, Schmuhl NB, Smith PD, Whitehead WE, Rogers RG. If we don't ask, they won't tell: screening for urinary and fecal incontinence by primary care providers. J Am Board Fam Med. 2018;31(5):774–782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gandhi A, Yu H, Grabowski DC. High nursing staff turnover in nursing homes offers important quality information. Health Aff (Millwood). 2021;40(3):384–391. [DOI] [PMC free article] [PubMed] [Google Scholar]