Abstract
Mindfulness-based cognitive therapy (MBCT) offers promise as a group-based intervention to alleviate posttraumatic stress disorder (PTSD) and depression symptoms in traumatized Black adults. Given the high level of barriers that exist for low-income Black adults, virtual delivery of MBCT may be helpful. This pilot randomized controlled trial assessed feasibility and acceptability of an adapted 8-week virtual MBCT group intervention for Black adults screening positive for PTSD and depression. Forty-six participants (89.3% women) recruited from an urban safety net hospital were randomized to MBCT or waitlist control (WLC). Overall feasibility was fair (70%); however, completion rates were higher for WLC than MBCT (90% vs. 54%). Group acceptability was high across quantitative and qualitative measures for study completers. Perceived barriers to psychological treatment were high (>9). While showing potential via improved coping skills and positive health changes, this intervention’s success hinges on mitigating engagement barriers for future delivery; additional studies are warranted.
Keywords: Trauma, Posttraumatic stress, Depression, Mindfulness, Virtual intervention
1. Introduction
Urban-dwelling Black adults are exposed to disproportionate levels of trauma and racial and income-based marginalization [1–3]. Chronic trauma and stress exposure heightens risk of posttraumatic stress disorder (PTSD) and depression and their co-occurrence [4,5]. Thus, finding effective behavioral health treatments for Black adults with low socioeconomic resources who are disproportionally exposed to trauma is critical.
Mindfulness-based cognitive therapy (MBCT; 6) is efficacious in treating depression [7] and directly targets emotion dysregulation and autonomic dysfunction, transdiagnostic factors underlying PTSD and mood symptoms [8–10]. While mindfulness approaches have shown efficacy in treating PTSD [11] and success in low-resourced Black populations [12,13], investigation into feasibility and acceptability of MBCT for PTSD in this population is limited, with only one study led by our team testing the in-person delivery of MBCT for Black adults with PTSD and depression in an urban safety net primary-care setting [14]. Providing remotely delivered MBCT may help reduce barriers to care [15,16] and health disparities exacerbated during the COVID-19 pandemic [17,18]. To our knowledge, no studies have examined feasibility and acceptability of virtual MBCT in trauma-exposed Black adults with PTSD.
This pilot randomized clinical trial (RCT) examined feasibility and acceptability of an 8-week virtual MBCT group in trauma-exposed Black adults with PTSD and depression symptoms who utilize medical care at an urban safety net hospital. The original study protocol [14] was adapted for virtual delivery following the COVID-19 pandemic. Based on retention rates in the in-person trial [14], we predicted a rate of 65% to support adequate feasibility. Quantitative and qualitative approaches were used to assess intervention acceptability across group satisfaction, perceived benefits and barriers, and symptom change. We predicted high satisfaction levels and reduced symptoms.
2. Materials and methods
All procedures and the RCT (NCT03922581) were approved by the Emory Institutional Review Board and the Grady Research Oversight Committee.
2.1. Study participants
Forty-six Black adults (89.3% women) were randomized (Table 1). Inclusion criteria included positive PTSD and depression screens, chronic trauma exposure,1 self-identification as Black or African American, and age 18–65.2 Exclusion criteria included active mania, psychosis, cognitive impairment, or past-month alcohol or substance use disorder.
Table 1.
Sample baseline characteristics.
| Variables | Overall Sample n (%) |
WLC n (%) |
MBCT n (%) |
|---|---|---|---|
|
| |||
| Gender | 40 (87.0) | 19 (95.0) | 21 (80.8) |
| Female | 6 (13.0) | 1 (5.0) | 5 (19.2) |
| Male | |||
| Race | 43 (93.5) | 19 (95.0) | 24 (92.3) |
| Black/African American | |||
| American | |||
| Mixed | 3 (6.5) | 1 (5.5) | 2 (7.7) |
| Marital status | 29 (63.0) | 10 (50.0) | 19 (73.1) |
| Single, never married | 4 (8.7) | 4 (20.0) | – |
| Married | 7 (15.2) | 3 (15.0) | 4 (15.4) |
| Divorced or separated | 3 (6.5) | 2 (10.0) | 1 (3.8) |
| Widowed | 3 (6.5) | 1 (5.0) | 2 (7.7) |
| Domestic partner | |||
| Employed | 16 (34.8) | 5 (25.0) | 11 (42.3) |
| Supported by disability | 21 (45.7) | 9 (45.0) | 12 (46.2) |
| Income | 27 (73.0) | 10 (66.7) | 17 (77.3) |
| Less than $2000 per month | |||
| Mean (SD), Range | Mean (SD), Range | Mean (SD), Range | |
| Age | 44.37 (13.80), 20–63 | 45.45 (14.09), 24–62 | 43.54 (13.78), 20–63 |
| Number of types of trauma exposure | 8.57 (3.02), 2–17 | 8.16 (2.76), 4–15 | 8.87 (3.23), 2–17 |
| PC-PTSD-5 Score | 4.44 (0.69) 3–5 | 4.58(0.69), 3–5 | 4.35 (0.69), 3–5 |
| PHQ-9 Score | 18.17(4.30) 10–27 | 18.80 (3.91), 10–25 | 17.69 (4.58), 10–25 |
| n (%) | n (%) | n (%) | |
| Current PTSD | 28 (68.3) | 9 (45.0) | 19 (73.1) |
| Current MDD | 28 (66.7) | 11 (55.0) | 17 (65.4) |
| Prior reported treatment | |||
| Psychotherapy | 15 (32.6) | 5 (25.0) | 10 (38.5) |
| Psychiatric Medication | 22 (57.9) | 11 (55.0) | 10 (88.5) |
N = 46; percentages vary slightly if missing data exists in any demographic variables
2.2. Procedure
The in-person RCT was halted in March 2020 due to the COVID-19 pandemic and was analyzed in a prior study [14]. Recruitment resumed in September 2020 with a fully virtual model of assessments and interventions. Participants were recruited from medical clinics via provider referrals or electronic medical record identification within an urban public hospital (Fig. 1). Screening assessments were conducted by phone or HIPAA-compliant Zoom. After completing a virtual baseline diagnostic assessment, participants were randomized to MBCT or waitlist control (WLC). Following completion, a post-assessment that mirrored pre-assessment was completed, and symptoms were re-assessed at 1-month. Participants were compensated for their time. See Supplemental Materials for details.
Fig. 1.
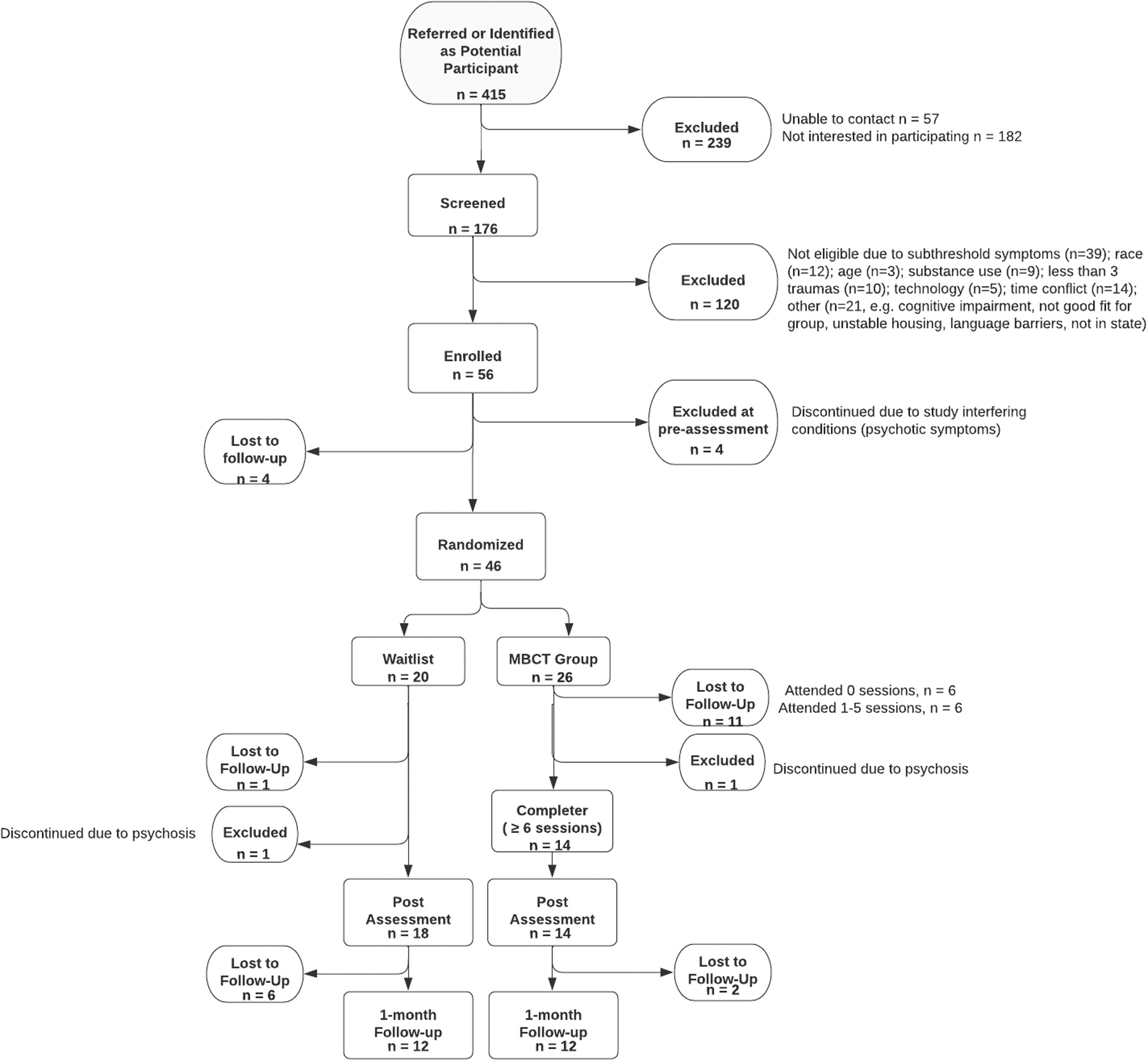
CONSORT flow chart.
2.3. Measures
Lifetime trauma exposure was assessed with the Traumatic Events Inventory (TEI; [19,20]). Current PTSD and depression symptoms were screened using the Primary Care PTSD Screen for DSM-5 (PC-PTSD-5; [21, 22]; cutoff ≥3) and the Patient Health Questionnaire (PHQ-9; [23]; cutoff ≥10). Symptom change was assessed at all time points using the PTSD Checklist for DSM-5 (PCL-5, [24,25]) and the Beck Depression Inventory, II (BDI-II, [26,27]).
Group satisfaction was measured using the Client Satisfaction Questionnaire (CSQ-8; [28]). Barriers to treatment engagement was measured pre- and post-assessment using the Perceived Barriers to Psychological Treatments (PBPT; [29]) across eight subscales: stigma, lack of motivation, emotional concerns, negative evaluations of therapy, misfit of therapy to needs, time constraints, participation restriction,3 and availability of services. In the original psychometric paper, the childcare responsibilities and cost of therapy items did not fit in any of the above subscales so were examined as individual items. A 12-item internal questionnaire assessed participants’ feelings about the MBCT group and changes observed across multiple areas (Supplemental Table 1). Questions were asked verbatim and participant responses were recorded.
2.4. MBCT group intervention
Participants randomized to MBCT attended live, Zoom-based group sessions led by two trained clinicians. MBCT consisted of eight, weekly 90-minute sessions conducted with rolling admission. It was patterned after MBCT for depression [6] but adapted to be trauma-informed and culturally responsive (see Supplemental Materials). Group leaders started each session reminding participants about confidentiality, removal of distractions (e.g., quiet space, muting self when not speaking), and nonjudgmental approach. Manual adherence was assessed using an adapted Group Leader Manual Adherence and Competence Rating Form [30]; adherence was 99.2% based on a randomized review of 30/70 sessions by two independent raters.
2.5. Data analysis
Enrollment, study completion, and participation rates were used to evaluate feasibility. Acceptability was assessed using quantitative and qualitative data at post-assessment. Supplemental Table 1 shows qualitative prompts, consensus codes, and direct quotes; details of coding methods are included in Supplemental Materials. Despite being underpowered, exploratory analyses of within-subjects change in PTSD and depression symptoms were examined using paired samples t-tests separately for the MBCT and WLC groups and descriptives of symptom scores at each time point are provided in Supplemental Table 2.
3. Results
3.1. Feasibility
Of 176 individuals screened, 120 were excluded (Fig. 1). Fifty-six participants were enrolled; 82% (n = 46) of those were randomized (26 virtual MBCT, 20 WLC). Study completion reflected attendance of ≥ 6 virtual sessions with no more than 2 weeks missed between sessions for MBCT or WLC through post-assessment. Thirty-two (70%) participants were study completers (54% for MBCT, 90% for WLC). Additionally, 24 (52%) completed 1-month follow-up (46% for MBCT, 60% for WLC). Fifty-four percent (n = 14) of participants randomized to MBCT completed group (≥6 sessions). Twenty participants (76.9%) randomized to MBCT attended at least one session. Of those who attended ≥ 1 session, 11 (55.0%) attended all sessions. Regarding participation timing, no participants enrolled in 2020 completed the study; completion rates were highest in 2021 (79.0%), followed by 2022 (68.0%) and 2023 (67.0%).
3.2. Acceptability
3.2.1. Satisfaction
Mean CSQ-8 score among MBCT completers (n = 12) was 28.50 (SD=2.88) on a scale of 8–32; 100% endorsed overall satisfaction with the group (see Supplemental Materials for results across items). All participants reported a positive experience with the group, but 46% indicated initial wariness about the group that transformed into fondness over time. When asked what they liked about MBCT, participants reported interacting with group members and leaders (61.5%), gaining strategies to practice mindfulness (46.1%), being able to express feelings (23.1%), and having their experience validated (7.7%). Regarding dislikes, most reported none (61.5%); however, 23.1% reported initial group-related discomfort, and 15.4% endorsed concerns surrounding time (i.e., schedule). Regarding format acceptability, 46.2% of participants preferred group format, 30.8% preferred individual format, and 23.1% noted benefits to both. Most participants liked the size of the group (53.8%); some noted preference for smaller (23.1%) or larger (15.4%) group.
3.2.2. Group benefits
When asked about participation gains, several patterns emerged from narrative analysis, including a new understanding of self (15.4%; n = 2), a new perspective of the trauma (15.4%; n = 2), and enhanced coping strategies (61.5%; n = 8); some reported gaining specific coping strategies, such as grounding and breathing exercises (62.5%; n = 5), while 37.5% (n = 3) mentioned gaining broad coping strategies. Most participants endorsed group-related changes in emotional (84.6%; n = 11); relational (76.9%; n = 10); and physical health (61.5%; n = 6). Only one participant denied group-related changes. Participants spontaneously reported being better able to notice (23.1%; n = 3) and regulate (23.1%; n = 3) emotions, accepting and open to their experience (23.1%; n = 3), and present (7.7%; n = 1). See Supplemental Materials and Supplemental Table 1 for more details.
3.2.3. Treatment engagement barriers
Participants completed the PBPT at pre- and post-assessment (n = 38, n = 31 respectively). Participants indicated an average of 9.82 significant barriers to receiving psychological services at pre-assessment (Supplemental Table 3). The most frequently reported barrier subscale was participation restrictions, followed by stigma and lack of motivation. Supplemental Table 4 shows barriers separated by MBCT completers and non-completers.
Participants (n = 12) were also asked about barriers that interfered with MBCT group participation or practicing skills outside of group in the post-assessment questionnaire. Emotional barriers to engagement were most endorsed (46.1%), followed by practical barriers (30.8%). Notably, 38.5% of participants denied any barriers to participation or practice.
3.2.4. Symptom change
There was a significant within-subjects reduction in PTSD scores from pre-assessment to post-assessment among participants in both MBCT (t[10]=2.06, p = .031) and WLC (t[15]=3.84, p < .001). Additionally, there was a significant within-subjects reduction in depression symptoms from pre-assessment to post-assessment for MBCT (t[10]= 2.96, p = .007) but not WLC participants (t[13]=1.73, p = .054).
4. Discussion
This study examined feasibility and acceptability of an 8-week adapted MBCT intervention delivered virtually for trauma-exposed Black adults who screened positive for PTSD and depression. Feasibility of the overall study was fair, although retention among the MBCT group was below the expected 65% target. Over half of participants randomized to the MBCT group were completers, but dropout rate was high; almost a quarter of MBCT randomized participants never attended a single session, demonstrating the need to identify and address barriers to initial care engagement. Supporting high acceptability, all participants endorsed satisfaction with the intervention, which shows promise for future MBCT programming for medical patients in urban settings. However, significant challenges with retention in the MBCT group means acceptability was only evaluated in completers; thus, challenges to acceptability in non-completers is essential to keep in mind.
Qualitative results showed that most participants endorsed enhanced coping strategies (e.g., grounding, breathing), as well as improvements in emotional, relational, and physical health and emotion regulation and acceptance, elements seen as critical mechanisms of change in MBCT [8]. Despite not prompting trauma-specific discussions, some also noted a transformation in their perspective on their trauma. Group members endorsed liking group interaction, gaining specific strategies for mindfulness practice, and having space to express feelings. Within-person reductions in PTSD and depression were found in group completers, but given similar results for the WLC, efficacy trials are needed.
Perceived barriers to psychological treatment were high, with the most common including participation restrictions (e.g., physical limitations) and personal barriers (e.g., stigma, lack of motivation). Qualitatively, almost half of participants indicated initial hesitance but grew to enjoy the group over time. This hesitancy may have been relevant for participants that never attended a single group, although data on this was not collected. Given the hesitancy of joining the group endorsed by many, stigma and perceived/objective accessibility must be addressed. Lay provider models of care delivery for Black individuals may help address mental health disparities and reduce stigma [31,32], and such models should be considered in the delivery of mindfulness-based interventions in future research. Importantly, while stigma is impactful [33], environmental and systemic factors (e.g., structural racism) that affect access to mental health care and have led to substantial treatment barriers [34,35] must be addressed to ensure treatment feasibility.
This study was conducted following the immediate aftermath of the COVID-19 shutdown. Our shift to a virtual delivery model allowed for accessibility, which is valuable given the increase in racial inequities from COVID-19 [17,18]. There are many positives to virtual delivery of group-based care [36,37], such as reduced time, transportation, and financial barriers. However, while virtual delivery allows the flexibility to engage in the intervention from wherever participants are, it creates challenges to privacy, consistency, and reduction of distractions (e.g., attending in parked car because only private space). Retention was lower in this sample than the pre-pandemic, in-person delivery of this RCT with this patient population [14]; although COVID-19 was a factor in lack of retention in 2020, given that rates of retention in this study was highest in 2021, COVID-19 alone was not the only factor. Flexibility in delivery method may help (e.g., hybrid models). Across this sample and prior study [14], similar patterns emerged regarding acceptability, satisfaction, and observed change, suggesting delivery method itself did not alter how the intervention was experienced.
Major strengths of this study include focus on a high-symptom sample and limited number of exclusions to promote real-world generalizability, inclusion of an understudied population, and mixed-method approach. There are also several limitations. Specificity of the sample to predominantly Black women limits generalizability. We did not capture data regarding adequacy of cultural adaptations or preference toward virtual or in-person delivery mode. At times, group sessions included only one participant; this could have impacted group experience. Clinician satisfaction, usefulness, and barriers to implementing intervention were not collected. Qualitative interview approaches should be considered for future studies.
Overall, adapted MBCT for trauma exposed Black adults is acceptable among those that complete it, but substantial barriers remain. Implementation research is necessary to enhance feasibility and acceptability of mindfulness-based interventions in this population. Promoting access to trauma informed behavioral health services, and virtual (or hybrid) group-based MBCT interventions may be a useful path forward.
Supplementary Material
Funding Source and Acknowledgements
This work was supported by the National Center for Complementary & Integrative Health (K23AT009713) and the Emory School of Medicine Doris Duke Charitable Foundation COVID-19 Fund to Retain Clinical Scientists and the Georgia CTSA NIH award number (UL1-TR002378). We would like to thank Angelo Brown, Natalie Merrill, and the entire Grady Trauma Project team for their assistance and the participants for their study engagement and time.
Footnotes
Presence of 3 or more traumas was used as an inclusion criterion to ensure the presence of multiple trauma exposures.
Age cutoff of 65 was required for the screening study used to enroll participants so was included for this study also.
Participation restrictions include physical symptoms, difficulty walking or getting around, illness, or problems with transportation.
Declaration of Competing Interest
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests: Abigail Powers reports financial support was provided by National Center for Complementary and Integrative Health.
Appendix A. Supporting information
Supplementary data associated with this article can be found in the online version at doi:10.1016/j.xjmad.2024.100048.
References
- [1].Galán CA, Auguste EE, Smith NA, Meza J. An intersectional-contextual approach to racial trauma exposure risk and coping among black youth. J Res Adolesc 2022;32(2):583–95. 10.1111/jora.12757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Gluck R, Hartzell G, Dixon HD, Michopoulos V, Powers A, Stevens J, Fani N, Carter S, Schwartz A, Jovanovic T, Ressler K, Bradley B, Gillespie CF. Trauma exposure and stress-related disorders in a large, urban, predominantly African American female sample. Arch Women’S Ment Health 2021. 10.1007/s00737-021-01141-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Mekawi Y, Carter S, Brown B, Martinez de Andino A, Fani N, Michopoulos V, Powers A. Interpersonal trauma and posttraumatic stress disorder among black women: does racial discrimination matter? J Trauma Dissociation 2021;22(2):154–69. 10.1080/15299732.2020.1869098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Chiu KB, deRoon-Cassini TA, Brasel KJ. Factors identifying risk for psychological distress in the civilian trauma population. Acad Emerg Med 2011;18(11):1156–60. 10.1177/003335491112600211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the national comorbidity survey. Arch Gen Psychiatry 1995;52(12):1048–60. 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- [6].Segal ZV, Williams M, Teasdale J. Mindfulness-Based Cognitive Therapy for Depression. Guilford Publications; 2018. [Google Scholar]
- [7].van der Velden AM, Kuyken W, Wattar U, Crane C, Pallesen KJ, Dahlgaard J, Fjorback LO, Piet J. A systematic review of mechanisms of change in mindfulness-based cognitive therapy in the treatment of recurrent major depressive disorder. Clin Psychol Rev 2015;37:26–39. 10.1016/j.cpr.2015.02.001. [DOI] [PubMed] [Google Scholar]
- [8].Gratz KL, Tull MT. Emotion regulation as a mechanism of change in acceptance- and mindfulness-based treatments. In: Baer RA, editor. Assessing mindfulness and acceptance processes in clients: Illuminating the theory and practice of change. Oakland, CA: New Harbinger Publications; 2010. p. 107–33. [Google Scholar]
- [9].Krygier JR, Heathers JA, Shahrestani S, Abbott M, Gross JJ, Kemp AH. Mindfulness meditation, well-being, and heart rate variability: a preliminary investigation into the impact of intensive Vipassana meditation. Int. J. Psychophysiol. 2013;89(3):305–13. 10.1016/j.ijpsycho.2013.06.017. [DOI] [PubMed] [Google Scholar]
- [10].Bhatnagar R, Phelps L, Rietz K, Juergens T, Russell D, Miller N, Ahearn E. The effects of mindfulness training on post-traumatic stress disorder symptoms and heart rate variability in combat veterans. J Altern Complement Med 2013;19(11):860–1. 10.1056/NEJMms2025396. [DOI] [PubMed] [Google Scholar]
- [11].Hopwood TL, Schutte NS. A meta-analytic investigation of the impact of mindfulness-based interventions on post traumatic stress. Clin Psychol Rev 2017. 1; 57:12–20. 10.1016/j.cpr.2017.08.002. [DOI] [PubMed] [Google Scholar]
- [12].Dutton MA, Bermudez D, Matas A, Majid H, Myers NL. Mindfulness-based stress reduction for low-income, predominantly African American women with PTSD and a history of intimate partner violence. Cogn Behav Pract 2013;20(1):23–32. 10.1016/j.cbpra.2011.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Vallejo Z, Amaro H. Adaptation of mindfulness-based stress reduction program for addiction relapse prevention. Humanist Psychol 2009;37(2):192–206. [Google Scholar]
- [14].Powers A, Lathan EC, Dixon HD, Mekawi Y, Hinrichs R, Carter S, et al. Primary care-based mindfulness intervention for posttraumatic stress disorder and depression symptoms among Black adults: A pilot feasibility and acceptability randomized controlled trial. Psychological Trauma: Theory, Research, Practice, and Policy 2023;15(5):858. 10.1037/tra0001390. [removed for blind review] [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Kaslow NJ, Leiner AS, Reviere S, Jackson E, Bethea K, Bhaju J, Rhodes M, Gantt MJ, Senter H, Thompson MP. Suicidal, abused African American women’s response to a culturally informed intervention. J Consult Clin Psychol 2010;78(4):449. 10.1037//0022-006x.70.2.311. [DOI] [PubMed] [Google Scholar]
- [16].Williams MV, Parker RM, Baker DW, Parikh NS, Pitkin K, Coates WC, Nurss JR. Inadequate functional health literacy among patients at two public hospitals. JAMA 1995;274(21):1677–82. [PubMed] [Google Scholar]
- [17].Hooper MW, Nápoles AM, Pérez-Stable EJ. COVID-19 and racial/ethnic disparities. JAMA 2020. 10.1001/jama.2020.8598. [DOI] [Google Scholar]
- [18].Yancy CW. COVID-19 and African Americans. JAMA 2020. 10.1001/jama.2020.6548. [DOI] [PubMed] [Google Scholar]
- [19].Gillespie C, Bradley B, Mercer K, Smith A, Conneely K, Gapen M, Ressler K. Trauma exposure and stress-related disorders in inner city primary care patients. Gen Hosp Psychiatry 2009;31:505–14. 10.1016/j.genhosppsych.2009.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Mekawi Y, Kuzyk E, Dixon HD, McKenna B, Camacho L, de Andino AM, Stevens J, Michopolous V, Powers A. Characterizing typologies of polytraumatization: a replication and extension study examining internalizing and externalizing psychopathology in an urban population. Clin Psychol Sci 2021;9(6):1144–63. 10.1177/21677026211000723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Prins A, Bovin MJ, Smolenski DJ, Marx BP, Kimerling R, Jenkins-Guarnieri MA, Kaloupek DG, Schnurr PP, Kaiser AP, Leyva YE. The primary care PTSD screen for DSM-5 (PC-PTSD-5): development and evaluation within a veteran primary care sample. J Gen Intern Med 2016;31(10):1206–11. 10.1007/s11606-016-3703-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Lathan EC, Petri J, Haynes T, Mekawi Y, Michopoulos V, Powers A. Evaluating the performance of the primary care posttraumatic stress disorder screen for DSM-5 (PC-PTSD-5) in a trauma-exposed, socioeconomically vulnerable patient population. J Clin Psychol Med Settings 2023:1–13. 10.1007/s10880-023-09941-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Arroll B, Goodyear-Smith F, Crengle S, Gunn J, Kerse N, Fishman T, Falloon K, Hatcher S. Validation of PHQ-2 and PHQ-9 to screen for major depression in the primary care population. Ann Fam Med 2010;8(4):348–53. 10.1370/afm.1139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Blevins CA, Weathers FW, Davis MT, Witte TK, Domino JL. The posttraumatic stress disorder checklist for DSM-5 (PCL-5): development and initial psychometric evaluation. J Trauma Stress 2015;28(6):489–98. 10.1002/jts.22059. [DOI] [PubMed] [Google Scholar]
- [25].Mekawi Y, Silverstein MW, Walker A, Ishiekwene M, Carter S, Michopoulos V, Stevens JS, Powers A. Examining the psychometric properties of the PCL-5 in a black community sample using item response theory. J Anxiety Disord 2022;87:102555. 10.1016/j.janxdis.2022.102555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Beck AT, Steer RA, Brown G Beck depression inventory–II. Psychological Assessment. 1996. Jan 1. [Google Scholar]
- [27].Wang YP, Gorenstein C. Psychometric properties of the beck depression inventory-II: a comprehensive review. Braz J Psychiatry 2013;35:416–31. 10.1590/1516-4446-2012-1048. [DOI] [PubMed] [Google Scholar]
- [28].Attkisson CC, Greenfield TK. The UCSF client satisfaction scales: I. The client satisfaction questionnaire-8. In: Maruish M, editor. The Use of Psychological Testing for Treatment Planning and Outcomes Assessment: Instruments for Adults. Lawrence Erlbaum Associates Publishers; 2004. p. 799–811. [Google Scholar]
- [29].Mohr DC, Hart SL, Howard I, Julian L, Vella L, Catledge C, Feldman MD. Barriers to psychotherapy among depressed and nondepressed primary care patients. Ann Behav Med 2006;32(3):254–8. 10.1207/s15324796abm3203_12. [DOI] [PubMed] [Google Scholar]
- [30].Kaslow NJ, Leiner AS, Reviere S, Jackson E, Bethea K, Bhaju J, Rhodes M, Gantt MJ, Senter H, Thompson MP. Suicidal, abused African American women’s response to a culturally informed intervention. J Consult Clin Psychol 2010;78(4):449. 10.1037/a0019692. [DOI] [PubMed] [Google Scholar]
- [31].Kazdin AE, Rabbitt SM. Novel models for delivering mental health services and reducing the burdens of mental illness. Clin Psychol Sci 2013;1(2):170–91. 10.1177/1745691611418241. [DOI] [Google Scholar]
- [32].Winiarski DA, Rufa AK, Karnik NS. Using layperson-delivered cognitive-behavioral therapy to address mental health disparities. Psychiatr Ann 2019;49(8):353–7. 10.3928/00485713-20190711-02. [DOI] [Google Scholar]
- [33].Budhwani H, De P. Perceived stigma in health care settings and the physical and mental health of people of color in the United States. Health Equity 2019;3(1):73–80. 10.1089/heq.2018.0079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Bailey ZD, Feldman JM, Bassett MT. How structural racism works—racist policies as a root cause of US racial health inequities. N Engl J Med 2021;384(8):768–73. 10.1056/NEJMms2025396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Planey AM, Smith SM, Moore S, Walker TD. Barriers and facilitators to mental health help-seeking among African American youth and their families: a systematic review study. Child Youth Serv Rev 2019;101:190–200. [Google Scholar]
- [36].Appleton R, Williams J, Vera San Juan N, Needle JJ, Schlief M, Jordan H, Sheridan Rains L, Goulding L, Badhan M, Roxburgh E. Implementation, adoption, and perceptions of telemental health during the COVID-19 pandemic: systematic review. J Med Internet Res 2021;23(12):e31746. 10.2196/31746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Madigan S, Racine N, Cooke JE, Korczak DJ. COVID-19 and telemental health: Benefits, challenges, and future directions. Can Psychol 2021;62(1):5. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


