Abstract
Aims
Studies have suggested relationships between obesity and cardiovascular disease (CVD) morbidity. However, little is known about whether substantial weight reduction affects the risk of CVD-related acute care use in obese patients with CVD. The objective of this study was to determine whether bariatric surgery is associated with decreased risk of CVD-related acute care use.
Methods and results
We performed a self-controlled case series study of obese adults with CVD who underwent bariatric surgery, using population-based emergency department (ED), and inpatient samples in California, Florida, and Nebraska from 2005 to 2011. The primary outcome was ED visit or unplanned hospitalization for CVD. We used conditional logistic regression to compare the risk during sequential 12-month periods, using pre-surgery months 13–24 as the reference period. We identified 11 106 obese adults with CVD who underwent bariatric surgery. During the reference period, 20.6% [95% confidence interval (CI), 19.8–21.3%] of patients had an ED visit or unplanned hospitalization for CVD. The risk did not significantly change in the subsequent 12-month pre-surgery period [adjusted odds ratio (aOR) 0.98; 95% CI, 0.93–1.04; P = 0.42]. By contrast, in the first 12-month period after bariatric surgery, the risk significantly decreased (aOR 0.91; 95% CI, 0.86–0.96; P = 0.002). The risk remained reduced in the subsequent 13–24 months post-bariatric surgery (aOR 0.84; 95% CI, 0.79–0.89; P < 0.001). There was no reduction in the risk in separate obese populations that underwent non-bariatric surgery (i.e. cholecystectomy, hysterectomy). By CVD category, the risk of acute care use for coronary artery disease (CAD), heart failure (HF), and hypertension decreased after bariatric surgery, whereas that of dysrhythmia and venous thromboembolism transiently increased (Bonferroni corrected P < 0.05 for all comparisons).
Conclusion
Bariatric surgery is associated with a lower risk of overall CVD-related ED visit or unplanned hospitalization. The decline was mainly driven by reduced risk of acute care use for CAD, HF, and hypertension after bariatric surgery.
Keywords: Bariatric surgery, Cardiovascular disease, Obesity, Self-controlled case series study
1. Introduction
Cardiovascular disease (CVD) is the leading public health problem in the US, affecting approximately one-third (92 million) of American adults.1 The burden of healthcare utilization for CVD within the US healthcare system is substantial, accounting for 4.4 million emergency department (ED) visits and 5.8 million hospitalizations in 2010 alone.1 The estimated direct and indirect costs of CVD were $316 billion in 2012.1 At the same time, the nation has also experienced an obesity epidemic—approximately 35% of men and 40% of women are obese.2
Obese patients often have multiple cardiovascular comorbidities given that obesity is an established risk factor for various CVDs [e.g. coronary artery disease (CAD), heart failure (HF), hypertension, dysrhythmia, and venous thromboembolism (VTE)].1 Bariatric surgery is the most effective method to achieve substantial and sustained weight loss.3 However, past studies on the effects of bariatric surgery on CVD have mainly focused on ischaemic cardiovascular outcomes (e.g. myocardial infarction) and atherosclerotic risk factors such as hypertension, dyslipidaemia, and diabetes mellitus.4–7 No studies have examined the effectiveness of bariatric surgery on the overall CVD morbidities inclusive of ischaemic and non-ischaemic outcomes. Additionally, bariatric surgery may have different effects on the risk of each category of CVD. While bariatric surgery can theoretically decrease the risk of ischaemic cardiovascular events, surgery in general is known to increase the risk of non-ischaemic cardiovascular events such as dysrhythmia and VTE postoperatively.8,9 However, the effectiveness of bariatric surgery on the risk of acute care use (e.g. ED visit, unplanned hospitalization) for individual CVD categories is largely unknown.
To address these major knowledge gaps in the literature, we designed this study to investigate whether bariatric surgery is associated with a reduction in the risk of ED visit or unplanned hospitalization for all CVD among obese adults. We also aimed to determine changes in the risk of individual CVD categories after bariatric surgery.
2. Methods
2.1. Study design and setting
We performed a self-controlled case series study in obese adults who experienced both the exposure (bariatric surgery) and the outcome (ED visit or unplanned hospitalization for CVD). The present study fulfils the required assumptions of the self-controlled case series design because the exposure is transient and discrete and the outcome is an acute event.10 We selected this study design because it enables intra-person comparisons where every patient serves as his or her own control.10 Therefore, a control group was not necessary. This study design also minimizes confounding by unmeasured factors as all time-invariant variables are implicitly controlled.10
We used the Healthcare Cost and Utilization Project (HCUP) State Emergency Department Databases (SEDD) and State Inpatient Databases (SID) in three states (California, Florida, and Nebraska) from 1 January 2005 to 31 December 2011.11,12 We chose these states because of geographic diversity and unique patient identifiers that enabled us to perform longitudinal follow-up throughout the study years. The HCUP is the largest longitudinal hospital care data collection available in the US.11,12 In the participating states, all ED visits regardless of disposition are captured in the HCUP SEDD,11 and all inpatient discharges regardless of source of hospitalization are recorded in the SID.12 By integrating the HCUP SEDD and SID, we identified all ED visits and hospitalizations within the three study states.11,12 Details of the self-controlled case series study design and databases have been published previously.5–7,11–14 The institutional review boards of Massachusetts General Hospital and Columbia University Medical Center approved this study.
2.2. Study population
To identify all obese adults with CVD who underwent bariatric surgery and also experienced an ED visit or unplanned hospitalization for CVD within the study states, we took the following steps. First, we identified adults aged >_18 years with obesity by using the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) diagnosis codes 278.0–278.1, V77.8, V85.3x, and V85.4.5–7,13–15 Second, we selected patients who had at least one hospitalization for bariatric surgery by using the ICD-9-CM procedure codes 43.89, 44.31, 44.38, 44.39, 44.50, 44.68, 44.69, 44.93, 44.95, 44.99, 45.51, and 45.90.5–7,13–15 We excluded patients with diagnostic codes for gastrointestinal cancer (ICD-9-CM codes, 150.0–159.9).5–7,13–15 We only included patients who had bariatric surgery between 1 January 2007 and 31 December 2009 to collect data on the outcome event within 2 years before and after surgery. Last, we further identified patients with at least one ED visit or unplanned hospitalization for CVD between 1 January 2005 and 31 December 2011 among these obese adults who underwent bariatric surgery by using the Clinical Classifications Software (CCS) codes 96–121 in the primary CCS field.16 We excluded residents outside the study states and patients who died during the hospitalization for bariatric surgery, died in-hospital within 2 years after bariatric surgery, or had two or more bariatric surgeries during the study period.5–7,13–15
2.3. Measurements and outcomes
We retrieved data from the HCUP SEDD and SID on demographics (age, sex, and race/ethnicity), primary insurance type, quartiles for estimated median household income of residents in the patient’s ZIP code, ICD-9-CM diagnosis, procedures, season of surgery, and state. We used the baseline characteristics information recorded during the index hospitalization for bariatric surgery.
The primary outcome measure was an ED visit or an unplanned hospitalization with a primary diagnosis of CVD. As an additional analysis, we further examined the five most common CVD categories individually (i.e. CAD, HF, hypertension, dysrhythmia, and VTE). These five categories were chosen based on the number of patients with an ED visit or unplanned hospitalization during the reference period (i.e. pre-surgery months 13–24) according to the CCS categories for CVDs (i.e. CCS category 96–121).16
2.4. Statistical analysis
Adjusted odds ratios (aORs) were calculated by fitting a conditional logistic regression model—using pre-surgery months 13–24 as the reference period—for 1–12 months before surgery, 0–12 months after surgery, and 13–24 months after surgery. Each patient was matched to his or her own reference period. Several sensitivity analyses were performed to test the robustness of our inferences. First, the main analysis was repeated by stratifying by age group (18–44 years, 45–59 years, and >_60 years), sex, or race/ethnicity (non-Hispanic white, non-Hispanic black, and Hispanic).17 Second, by fitting a negative binomial regression model, the number of ED visits and unplanned hospitalizations for CVD was modelled as a count, instead of a binary, variable. Third, a sensitivity analysis was performed including patients who died in-hospital during the 2-year post-surgery period. To account for the shorter follow-up duration than 12 months in each 12-month period due to death, the off-set function (i.e. log[patient-years within each 12-month period]) was used with the Poisson regression analysis. Fourth, to address the possibility of loss to follow-up (e.g. out-of-hospital deaths, emigration from the study states), which would downwardly bias the post-surgery estimates, and a subgroup analysis was conducted by limiting the population to those with any ED visit or hospitalization during post-surgery 25–36 months. Fifth, two separate populations were also examined—obese adults who underwent other types of elective abdominal surgery: (i) cholecystectomy (ICD-9-CM procedure codes, 51.21–51.24, and 51.41–51.59) and (ii) hysterectomy (ICD-9-CM procedure codes, 68.31–68.79, and 68.9).5,7,13 These two non-bariatric surgeries were selected because of a large sample size, similar characteristics (i.e. common abdominal elective surgery), and no biological plausibility to affect weight or risks of the primary outcome.5,7,13 Additionally, a formal test for interaction between time (before vs. after surgery) and type of surgery (bariatric vs. non-bariatric surgery) was performed to examine whether changes in the risk differed between bariatric and non-bariatric surgery. Finally, another sensitivity analysis was performed to examine if the risk of ED visit or unplanned hospitalization for any reason changed before and after bariatric surgery.
All analyses were performed at a two-sided significance level of 0.05. All confidence intervals (CIs) were reported as two-sided values with a confidence level of 95%. For the analyses of the five most common CVD categories, P-values were corrected according to the Bonferroni method to account for multiple comparisons. Statistical analyses were performed with R software, version 3.3.2. (www.r-project.org).
3. Results
Among adult patients with obesity who underwent bariatric surgery and had at least one ED visit or unplanned hospitalization for CVD, 246 patients died in-hospital and 281 had multiple bariatric surgeries; the remaining 11 106 patients were included in the analysis. The baseline characteristics are described in Table 1. Overall, the median age was 48 years (interquartile range, 40–57 years), 73.6% were female, and 63.7% were non-Hispanic white.
Table 1.
Baseline characteristics of obese adults with cardiovascular disease who underwent bariatric surgery
| Characteristics | n = 11 106 |
|---|---|
| Age (years), median (IQR) | 48 (40–57) |
| Female sex | 8171 (73.6) |
| Race/ethnicitya | |
| Non-Hispanic white | 7071 (63.7) |
| Non-Hispanic black | 1406 (12.7) |
| Hispanic | 1628 (14.7) |
| Other | 308 (2.8) |
| Primary insurance | |
| Medicare | 2232 (20.1) |
| Medicaid | 880 (7.9) |
| Private | 6993 (63.0) |
| Other | 1001 (9.0) |
| Quartiles for median household income of patient’s ZIP code | |
| 1 (lowest) | 2799 (25.2) |
| 2 | 3020 (27.2) |
| 3 | 2816 (25.4) |
| 4 (highest) | 2251 (20.3) |
| Season of bariatric surgery | |
| January–March | 2518 (22.7) |
| April–June | 2691 (24.2) |
| July–September | 2963 (26.7) |
| October–December | 2934 (26.4) |
| State | |
| California | 7285 (65.6) |
| Florida | 3608 (32.5) |
| Nebraska | 213 (1.9) |
Data were expressed as n (%), unless otherwise indicated.
IQR, interquartile range.
Analyzed for 10 413 (93.8%) patients with race/ethnicity data. Race/ethnicity data were not available in Nebraska.
The risk of ED visit or unplanned hospitalization for overall CVD is summarized in Table 2. During the reference period of pre-bariatric surgery 13–24 months, 20.6% (95% CI 19.8–21.3%) experienced an ED visit or unplanned hospitalization for CVD. The risk remained unchanged at 20.3% (95% CI 19.6–21.1%) during the subsequent 1–12 months prior to bariatric surgery with aOR of 0.98 (95% CI 0.93–1.04; P = 0.42). By contrast, the risk was significantly lower after bariatric surgery. Within 0–12 months following surgery, 18.9% (95% CI 18.1–19.6%) had an ED visit or unplanned hospitalization for CVD (aOR 0.91, 95% CI 0.86–0.96; P = 0.002). The risk remained lower during 13–24 months after bariatric surgery at 17.4% (95% CI 16.7–18.2%), corresponding to an aOR of 0.84 (95% CI 0.79–0.89; P < 0.001).
Table 2.
Number of patients and risk of emergency department visit or unplanned hospitalization for cardiovascular disease
| Time interval | Number of patients | Risk (%) (95% CI) | aOR (95% CI)a | P-value |
|---|---|---|---|---|
| ED visit or unplanned hospitalizationb | (n = 11 106) | |||
| 13–24 months before bariatric surgery | 2284 | 20.6 (19.8–21.3) | Reference | – |
| 1–12 months before bariatric surgery | 2259 | 20.3 (19.6–21.1) | 0.98 (0.93–1.04) | 0.42 |
| 0–12 months after bariatric surgery | 2096 | 18.9 (18.1–19.6) | 0.91 (0.86–0.96) | 0.002 |
| 13–24 months after bariatric surgery | 1937 | 17.4 (16.7–18.2) | 0.84 (0.79–0.89) | <0.001 |
aOR, adjusted odds ratio; CI, confidence interval; ED, emergency department.
Adjusted odds ratios are for each 12 months of period vs. the reference period (i.e. 13–24 months before bariatric surgery), as calculated with conditional logistic regression.
Composite of at least one ED visit or unplanned hospitalization for cardiovascular disease.
The sensitivity analyses demonstrated the robustness of the findings. The stratified analyses by age group (Supplementary material online, Figure S1), sex (Supplementary material online, Figure S2), and race/ethnicity (Supplementary material online, Figure S3) showed a similar temporal risk pattern. When the outcome was modelled as a count variable as opposed to a binary variable with the use of negative binomial regression model, the risk of primary outcome also decreased during 0–12 months and 13–24 months after bariatric surgery (both P < 0.001; Supplementary material online, Table S1). The sensitivity analysis including those who died after surgery was also consistent with the main analysis (Supplementary material online, Table S2). Subgroup analysis limiting to those with any healthcare utilization during 25–36 months after bariatric surgery replicated the results with a reduced statistical power (Supplementary material online, Table S3). Contrary to the findings in the population with bariatric surgery, the risk of ED visit or unplanned hospitalization for CVD did not decrease in obese populations that underwent an elective non-bariatric abdominal surgery (Table 3, Supplementary material online, Tables S4 and S5). There was a significant interaction between time period (before vs. after surgery) and type of surgery (bariatric vs. non-bariatric) with P-interaction of <0.001, indicating that the risk reduction after surgery was significantly different between bariatric and non-bariatric surgery. The sensitivity analysis including all ED visits and unplanned hospitalizations for any reason showed no decrease in the risk after bariatric surgery (Supplementary material online, Table S6).
Table 3.
Number of patients and risk of emergency department visit or unplanned hospitalization for cardiovascular disease, among obese patients with cardiovascular disease who underwent non-bariatric surgery
| Time interval and surgery | Number of patients | Risk (%) (95% CI)a | aOR (95% CI)b | P-value |
|---|---|---|---|---|
| Cholecystectomy | (n = 10 554) | |||
| 13–24 months before surgery | 2174 | 20.6 (19.8–21.4) | Reference | – |
| 1–12 months before surgery | 3013 | 28.5 (27.7–29.4) | 1.42 (1.34–1.50) | <0.001 |
| 0–12 months after surgery | 2602 | 24.7 (23.8–25.5) | 1.23 (1.16–1.30) | <0.001 |
| 13–24 months after surgery | 2485 | 23.5 (22.7–24.4) | 1.17 (1.10–1.24) | <0.001 |
| Hysterectomy | (n = 6194) | |||
| 13–24 months before surgery | 1127 | 18.2 (17.2–19.2) | Reference | – |
| 1–12 months before surgery | 1381 | 22.3 (21.3–23.4) | 1.24 (1.14–1.34) | <0.001 |
| 0–12 months after surgery | 1385 | 22.4 (21.3–23.4) | 1.25 (1.15–1.35) | <0.001 |
| 13–24 months after surgery | 1472 | 23.8 (22.7–24.8) | 1.34 (1.24–1.45) | <0.001 |
aOR, adjusted odds ratio; CI, confidence interval.
Adjusted odds ratios are for each 12 months of period vs. the reference period (i.e. 13–24 months before surgery), as calculated with conditional logistic regression.
Composite of at least one emergency department visit or unplanned hospitalization for cardiovascular disease.
With further classification of CVDs according to the CCS category, the five most common CVD categories were CAD, HF, hypertension, dysrhythmia, and VTE (Table 4). Compared with the reference period of 13–24 months before bariatric surgery, the risk of ED visit or unplanned hospitalization for CAD, HF, and hypertension decreased significantly after bariatric surgery (Figure 1A–C). By contrast, there was an increase in the risk of dysrhythmia and VTE during the 3-month post-surgery period, which returned to the baseline level during 3–6 months after surgery (Figure 1D and E).
Table 4.
Number of patients and risk of emergency department visit or unplanned hospitalization for five most common categories of cardiovascular disease
| Time interval and CVD categorya | Number of patients (n = 11 106) | Risk (%) (95% CI)b | aOR (95% CI)c | Bonferroni-corrected P-valued |
|---|---|---|---|---|
| Coronary artery disease | ||||
| 13–24 months before surgery | 190 | 1.7 (1.5–2.0) | Reference | – |
| 1–12 months before surgery | 170 | 1.5 (1.3–1.8) | 0.88 (0.71–1.08) | 0.99 |
| 0–12 months after surgery | 83 | 0.7 (0.6–0.9) | 0.42 (0.32–0.54) | <0.001 |
| 13–24 months after surgery | 99 | 0.9 (0.7–1.1) | 0.51 (0.40–0.65) | <0.001 |
| Heart failure | ||||
| 13–24 months before surgery | 138 | 1.2 (1.0–1.5) | Reference | – |
| 1–12 months before surgery | 104 | 0.9 (0.8–1.1) | 0.75 (0.58–0.97) | 0.14 |
| 0–12 months after surgery | 52 | 0.5 (0.3–0.6) | 0.37 (0.27–0.51) | <0.001 |
| 13–24 months after surgery | 60 | 0.5 (0.4–0.7) | 0.42 (0.31–0.57) | <0.001 |
| Hypertension | ||||
| 13–24 months before surgery | 127 | 1.1 (1.0–1.3) | Reference | – |
| 1–12 months before surgery | 151 | 1.4 (1.2–1.6) | 1.19 (0.94–1.51) | 0.73 |
| 0–12 months after surgery | 82 | 0.7 (0.6–0.9) | 0.64 (0.49–0.85) | 0.01 |
| 13–24 months after surgery | 94 | 0.8 (0.7–1.0) | 0.74 (0.57–0.97) | 0.14 |
| Dysrhythmia | ||||
| 13–24 months before surgery | 271 | 2.4 (2.2–2.7) | Reference | – |
| 1–12 months before surgery | 322 | 2.9 (2.6–3.2) | 1.20 (1.02–1.41) | 0.13 |
| 0–12 months after surgery | 351 | 3.2 (2.8–3.5) | 1.31 (1.12–1.54) | 0.004 |
| 13–24 months after surgery | 315 | 2.8 (2.5–3.5) | 1.17 (1.00–1.38) | 0.27 |
| Venous thromboembolism | ||||
| 13–24 months before surgery | 74 | 0.7 (0.5–0.8) | Reference | – |
| 1–12 months before surgery | 51 | 0.5 (0.3–0.6) | 0.69 (0.48–0.98) | 0.20 |
| 0–12 months after surgery | 162 | 1.5 (1.2–1.7) | 2.20 (1.67–2.90) | <0.001 |
| 13–24 months after surgery | 73 | 0.7 (0.5–0.8) | 0.98 (0.71–1.36) | 0.99 |
aOR, adjusted odds ratio; CI, confidence interval; CVD, cardiovascular disease.
Five most common CVD categories were determined according to the number of patients with an emergency department visit or unplanned hospitalization during 13–24 months before bariatric surgery. The other tables include all CVD categories.
Composite of at least one emergency department visit or unplanned hospitalization.
Adjusted odds ratios are for each 12 months of period vs. the reference period (i.e. 13–24 months before the index bariatric surgery), as calculated with conditional logistic regression.
Corrected for comparisons of five categories.
Figure 1.
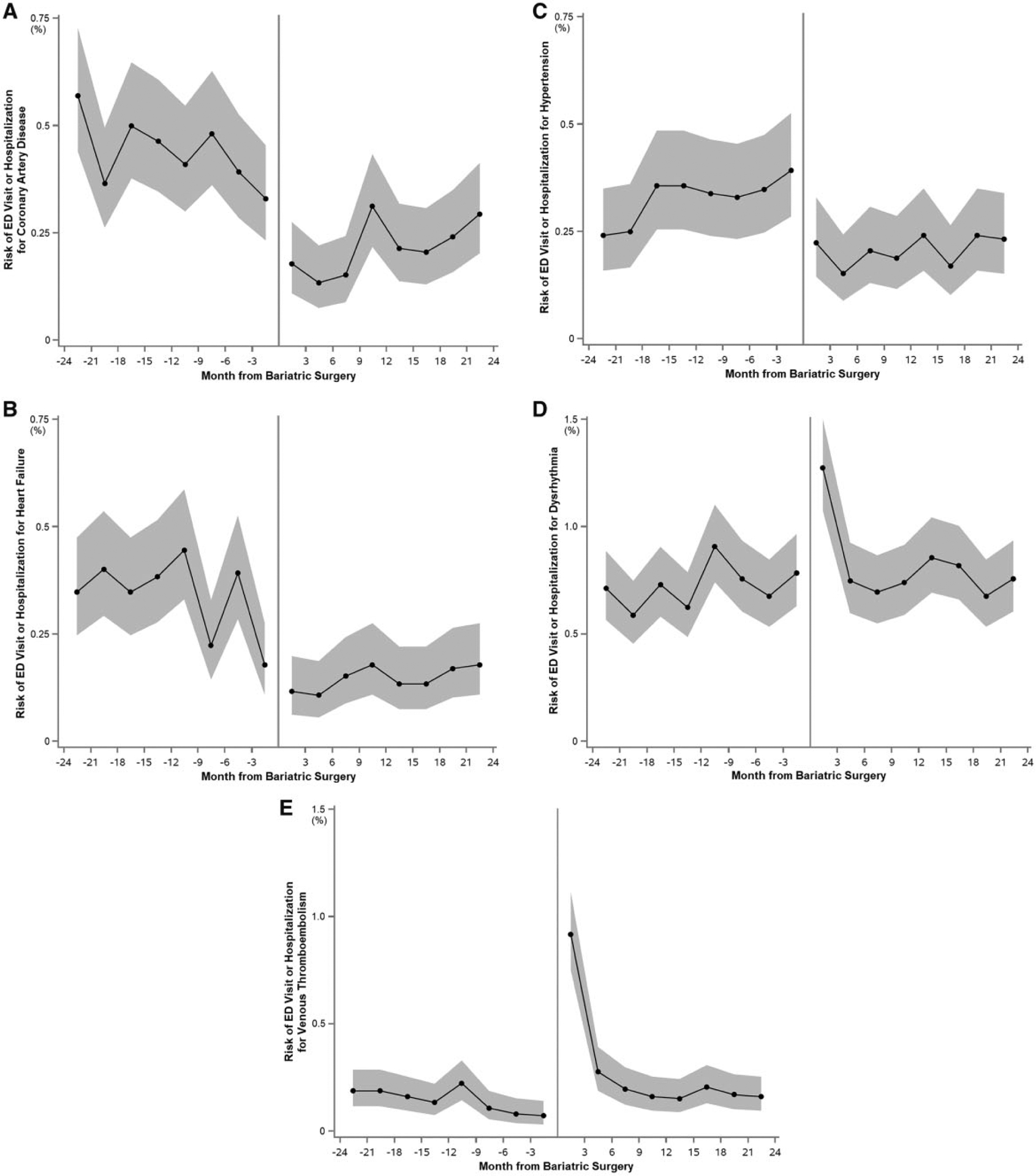
Risk of emergency department visit or unplanned hospitalization for individual categories of cardiovascular disease before and after bariatric surgery in 3 months of interval. Proportion of patients with an ED visit or unplanned hospitalization for (A) coronary artery disease, (B) heart failure, (C) hypertension, (D) dysrhythmia, and (E) venous thromboembolism, with the 95% CIs for the 2 years before and after bariatric surgery in 3 months of intervals (n = 11 106). The periods were centred on the date of bariatric surgery of each patient. CI, confidence interval; ED, emergency department.
4. Discussion
4.1. Principal findings
In this self-controlled case series study using population-based data of 11 106 patients with obesity and CVD, we found that the risk of acute care use for CVD was significantly reduced after bariatric surgery, and the lower risk lasted for at least 2 years. The significant temporal changes in the risk persisted across several subpopulations and analytical assumptions. Additionally, the observed decline in the risk was primarily driven by the lower risk of acute CVD events related to CAD, HF, and hyper-tension. By contrast, we observed a transiently increased risk of dysrhythmia and VTE after bariatric surgery. This is the first study that has investigated the association of bariatric surgery with acute care use for the overall (inclusive of ischaemic and non-ischaemic) and individual CVDs.
4.2. Results in context
There is emerging evidence that supports the effectiveness of bariatric surgery to prevent CVD-related healthcare utilization.4–6 For example, in a cohort study of 2010 obese adults who underwent bariatric surgery and 2037 controls who received usual care, bariatric surgery was associated with lower incidence of a composite of cardiovascular death, myocardial infarction, and stroke.4 However, prior studies on bariatric surgery have examined its effects exclusively on ischaemic cardiovascular outcomes and atherosclerotic risk factors (e.g. hypertension, dyslipidaemia, and diabetes mellitus) except for our recent report on HF exacerbation.4–7 Furthermore, the risk reduction associated with bariatric surgery observed in ischaemic CVD and HF may not be universal in all categories of CVD. Surgery in general increases the risk of dysrhythmia and VTE post-operatively, particularly in obese individuals.8,9 Indeed, the effect size of the present study on the overall CVD (aOR 0.84) was smaller than that in the prior reports on myocardial infarction and stroke (aOR 0.67),4 CAD (aOR 0.33),6 HF (aOR 0.57),5 and hypertension-related acute care use (aOR 0.71).7 This apparent discrepancy in the effect size may be attributable to the concurrent increase in the risk of dysrhythmia and VTE. Our study builds on these prior reports, and extends them by demonstrating the favourable association of bariatric surgery with the all-inclusive CVD as well as the divergent effectiveness on the individual CVD categories.
4.3. Advantages of the study design and databases
The influence of residual confounding by unmeasured variables is inherent in the traditional case-control or other cohort study designs. By contrast, the self-controlled case series design controls for all time-invariant confounders (e.g. patient characteristics, genetic background), both measured and unmeasured, because each patient serves as his or her own control.10 This study design augments the internal validity by eliminating inter-personal variations to accurately determine the effects of the exposure (i.e. bariatric surgery in the present study).10 These advantages of the self-controlled case series design have let to successful demonstration of the associations between surgical weight reduction and morbidity in a variety of cardiopulmonary conditions (e.g. asthma, stable angina, HF, hypertension, and atrial fibrillation).5–7,13,14
A large-scale, high-quality randomized controlled trial would be required to further delineate the efficacy of bariatric surgery on the risk of acute cardiovascular events. However, the financial and logistic burden associated with such a trial can be substantial. Moreover, the external validity of randomized controlled trials is sometimes limited because the participants may be selected and motivated individuals or may behave differently in the highly controlled environment.18,19 In most of randomized controlled trials on bariatric surgery, for example, less than 10% of screened patients were enrolled and they had to be compliant with dietary and exercise instructions as well as follow-up visits.20,21 By contrast, the external validity of the present study is strengthened because the HCUP SEDD and SID captured all ED visits and hospitalizations that occurred within the study states, thereby allowing for collection of large general population-based data of patient care in the natural setting. Further, our study population was racially/ethnically, socioeconomically, and geographically diverse. The comprehensiveness of the databases and inclusion of diverse populations in the real world enhance the external validity of the inferences derived from our study.
4.4. Potential limitations
Our study has several potential limitations. First, misclassification can occur with any study using administrative data. However, the HCUP databases and the ICD-9-CM codes have been extensively utilized and the quality has been tested in multiple prior studies.5–7,13,14,22 For example, our method to identify obese patients was reported to have specificity of 99.4%.23 With respect to the outcome, it has been shown that administrative data to identify HF- and hypertension-related acute care use perform well with a high specificity and positive predictive value, most reporting values of >95%.24–26 Second, due to the observational nature of the present study, it does not prove causality or yield the same strength of evidence as a randomized controlled trial would. Third, patients might have lost to follow-up or died after bariatric surgery, thereby downwardly biasing our estimates during the post-surgery period. However, the sensitivity analysis showed consistent findings when we limited the population to patients who were confirmed to be alive for at least 2 years after surgery. Fourth, the observed decrease in the risk may be attributable to intensified management during the peribariatric surgery period, which may not be unique to bariatric surgery. However, it would be difficult to postulate that the reduction in the risk after bariatric surgery is fully attributable to intensified non-invasive treatment for the following reasons: (i) the substantial and immediate weight reduction after bariatric surgery reported in the literature3 was paralleled by a significant decline in the risk in our study and (ii) no reduction in the risk was observed with elective non-bariatric surgery. Further, the formal test for interaction revealed that the change in the risk after surgery was significantly different between bariatric and non-bariatric populations. Fifth, our database did not include some potentially useful clinical data such as body mass index. Last, our study population of interest was obese adults with an ED visit or hospitalization for CVDs. Thus, our findings might not be generalizable to those with well-controlled CVDs. Yet, our study population contributes a large healthcare burden, and hence is the one for which targeted interventions are urgently needed.
5. Conclusions
In this self-controlled case series study with the use of large population-based data from three states in the US, we found that bariatric surgery is associated with a significantly lower risk of CVD-related acute healthcare utilization among obese adults with CVD. The risk reduction was mainly driven by the lower risk of morbidities related to CAD, HF, and hypertension after bariatric surgery. Our study also demonstrated a post-surgical increase in the risk of dysrhythmia and VTE. The present study provides the best evidence to date on the effectiveness of bariatric surgery on morbidities associated with CVD. Yet, many obese patients with CVD choose non-surgical weight reduction interventions due to concerns for peri-operative complications or other reasons (e.g. lack of insurance coverage, cost, and compliance). Our data stress the importance of developing safe and effective weight loss strategies, both surgical and non-surgical, to mitigate the large societal burden of CVD in obese patients.
Supplementary Material
Funding
This work was supported in part by an unrestricted grant from the American Heart Association National Clinical and Population Research Award [award number 15CRP22930001 and 17MCPRP33670415 to Y.J.S.], the American Heart Association Career Development Award [award number 18CDA34110245 to Y.J.S.], Honjo International Scholarship Foundation, and the Korea Institute of Oriental Medicine [award number K18190 to Y.J.S.]. The funding organizations had no role in design or conduct of the study; collection, management, analysis, or interpretation of the data; preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication. The researchers were independent from the funding organizations.
Footnotes
Supplementary material
Supplementary material is available at Cardiovascular Research online.
Conflict of interest: none declared.
References
- 1.Benjamin EJ, Virani SS, Callaway CW, Chamberlain AM, Chang AR, Cheng S, Chiuve SE, Cushman M, Delling FN, Deo R, de Ferranti SD, Ferguson JF, Fornage M, Gillespie C, Isasi CR, Jiménez MC, Jordan LC, Judd SE, Lackland D, Lichtman JH, Lisabeth L, Liu S, Longenecker CT, Lutsey PL, Mackey JS, Matchar DB, Matsushita K, Mussolino ME, Nasir K, O’Flaherty M, Palaniappan LP, Pandey A, Pandey DK, Reeves MJ, Ritchey MD, Rodriguez CJ, Roth GA, Rosamond WD, Sampson UKA, Satou GM, Shah SH, Spartano NL, Tirschwell DL, Tsao CW, Voeks JH, Willey JZ, Wilkins JT, Wu JH, Alger HM, Wong SS, Muntner P. Heart disease and stroke statistics-2018 update: a report from the American Heart Association. Circulation 2018;137:e67–e492. [DOI] [PubMed] [Google Scholar]
- 2.Flegal KM, Kruszon-Moran D, Carroll MD, Fryar CD, Ogden CL. Trends in obesity among adults in the United States, 2005 to 2014. JAMA 2016;315:2284–2291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gloy VL, Briel M, Bhatt DL, Kashyap SR, Schauer PR, Mingrone G, Bucher HC, Nordmann AJ. Bariatric surgery versus non-surgical treatment for obesity: a systematic review and meta-analysis of randomised controlled trials. BMJ 2013;347:f5934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sjostrom L, Peltonen M, Jacobson P, Sjostrom CD, Karason K, Wedel H, Ahlin S, Anveden A, Bengtsson C, Bergmark G, Bouchard C, Carlsson B, Dahlgren S, Karlsson J, Lindroos AK, Lonroth H, Narbro K, Naslund I, Olbers T, Svensson PA, Carlsson LM. Bariatric surgery and long-term cardiovascular events. JAMA 2012;307: 56–65. [DOI] [PubMed] [Google Scholar]
- 5.Shimada YJ, Tsugawa Y, Brown DF, Hasegawa K. Bariatric surgery and emergency department visits and hospitalizations for heart failure exacerbation: population-based, self-controlled series. J Am Coll Cardiol 2016;67:895–903. [DOI] [PubMed] [Google Scholar]
- 6.Shimada YJ, Tsugawa Y, Iso H, Brown DF, Hasegawa K. Association between bariatric surgery and rate of hospitalisations for stable angina pectoris in obese adults. Heart 2017;103:1009–1014. [DOI] [PubMed] [Google Scholar]
- 7.Shimada YJ, Tsugawa Y, Iso H, Brown DFM, Hasegawa K. Association of bariatric surgery with risk of acute care use for hypertension-related disease in obese adults: population-based self-controlled case series study. BMC Med 2017;15:161–169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Heintz KM, Hollenberg SM. Perioperative cardiac issues: postoperative arrhythmias. Surg Clin North Am 2005;85:1103–1114, viii. [DOI] [PubMed] [Google Scholar]
- 9.Sweetland S, Green J, Liu B, Berrington de Gonzalez A, Canonico M, Reeves G, Beral V. Duration and magnitude of the postoperative risk of venous thromboembolism in middle aged women: prospective cohort study. BMJ 2009;339: b4583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Whitaker HJ, Farrington CP, Spiessens B, Musonda P. Tutorial in biostatistics: the self-controlled case series method. Stat Med 2006;25:1768–1797. [DOI] [PubMed] [Google Scholar]
- 11.Overview of the State Emergency Department Databases (SEDD). Healthcare Cost and Utilization Project. http://www.hcup-us.ahrq.gov/seddoverview.jsp (20 June 2018, date last accessed).
- 12.Overview of the State Inpatient Databases (SID). Healthcare Cost and Utilization Project. http://www.hcup-us.ahrq.gov/sidoverview.jsp (20 June 2018, date last accessed).
- 13.Hasegawa K, Tsugawa Y, Chang Y, Camargo CA Jr., Risk of an asthma exacerbation after bariatric surgery in adults. J Allergy Clin Immunol 2015;136:288–294.e8. [DOI] [PubMed] [Google Scholar]
- 14.Shimada YJ, Tsugawa Y, Camargo CA Jr, Brown DFM, Hasegawa K. Effect of bariatric surgery on emergency department visits and hospitalizations for atrial fibrillation. Am J Cardiol 2017;120:947–952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nguyen GC, Patel AM. Racial disparities in mortality in patients undergoing bariatric surgery in the U.S.A. Obes Surg 2013;23:1508–1514. [DOI] [PubMed] [Google Scholar]
- 16.HCUP CCS. Healthcare Cost and Utilization Project (HCUP). https://www.hcup-us.ahrq.gov/toolssoftware/ccs/ccs.jsp (27 August 2018, date last accessed).
- 17.Morgenstern LB, Smith MA, Sanchez BN, Brown DL, Zahuranec DB, Garcia N, Kerber KA, Skolarus LE, Meurer WJ, Burke JF, Adelman EE, Baek J, Lisabeth LD. Persistent ischemic stroke disparities despite declining incidence in Mexican Americans. Ann Neurol 2013;74:778–785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Maasland L, van Oostenbrugge RJ, Franke CF, Scholte Op Reimer WJ, Koudstaal PJ, Dippel DW. Patients enrolled in large randomized clinical trials of antiplatelet treatment for prevention after transient ischemic attack or ischemic stroke are not representative of patients in clinical practice: the Netherlands Stroke Survey. Stroke 2009; 40:2662–2668. [DOI] [PubMed] [Google Scholar]
- 19.Van Spall HG, Toren A, Kiss A, Fowler RA. Eligibility criteria of randomized controlled trials published in high-impact general medical journals: a systematic sampling review. JAMA 2007;297:1233–1240. [DOI] [PubMed] [Google Scholar]
- 20.Halperin F, Ding SA, Simonson DC, Panosian J, Goebel-Fabbri A, Wewalka M, Hamdy O, Abrahamson M, Clancy K, Foster K, Lautz D, Vernon A, Goldfine AB. Roux-en-Y gastric bypass surgery or lifestyle with intensive medical management in patients with type 2 diabetes: feasibility and 1-year results of a randomized clinical trial. JAMA Surg 2014;149:716–726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ikramuddin S, Korner J, Lee WJ, Connett JE, Inabnet WB, Billington CJ, Thomas AJ, Leslie DB, Chong K, Jeffery RW, Ahmed L, Vella A, Chuang LM, Bessler M, Sarr MG, Swain JM, Laqua P, Jensen MD, Bantle JP. Roux-en-Y gastric bypass vs intensive medical management for the control of type 2 diabetes, hypertension, and hyperlipidemia: the Diabetes Surgery Study randomized clinical trial. JAMA 2013;309: 2240–2249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hasegawa K, Tsugawa Y, Brown DF, Camargo CA Jr. A population-based study of adults who frequently visit the emergency department for acute asthma. California and Florida, 2009–2010. Ann Am Thorac Soc 2014;11:158–166. [DOI] [PubMed] [Google Scholar]
- 23.Goff SL, Pekow PS, Markenson G, Knee A, Chasan-Taber L, Lindenauer PK. Validity of using ICD-9-CM codes to identify selected categories of obstetric complications, procedures and co-morbidities. Paediatr Perinat Epidemiol 2012;26: 421–429. [DOI] [PubMed] [Google Scholar]
- 24.Saczynski JS, Andrade SE, Harrold LR, Tjia J, Cutrona SL, Dodd KS, Goldberg RJ, Gurwitz JH. A systematic review of validated methods for identifying heart failure using administrative data. Pharmacoepidemiol Drug Saf 2012;21: 129–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McNaughton CD, Self WH, Zhu Y, Janke AT, Storrow AB, Levy P. Incidence of hypertension-related emergency department visits in the United States, 2006 to 2012. Am J Cardiol 2015;116:1717–1723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Birman-Deych E, Waterman AD, Yan Y, Nilasena DS, Radford MJ, Gage BF. Accuracy of ICD-9-CM codes for identifying cardiovascular and stroke risk factors. Med Care 2005;43:480–485. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


