Abstract
Objectives
To assess social determinants of stunting and the shifts in contributions of socio-demographic factors to national prevalence trends in India between 2005 and 2021.
Methods
We leveraged data from three rounds of the National Family Health Survey (NFHS-3: 2005–2006, NFHS-4: 2015–2016, NFHS-5: 2019–2021) for 443 038 children under 5 years. Adjusted logistic regression models and a Kitigawa-Oaxaca-Blinder decomposition were deployed to examine how wealth, residence, belonging to a marginalised social group, maternal education and child sex contributed to changes in stunting prevalence.
Results
The decrease in stunting prevalence was notably slower between NFHS-4 and NFHS-5 (annual average rate of reduction (AARR): 1.33%) than between NFHS-3 and NFHS-4 (AARR: 2.20%). The protective effect of high wealth diminished from 2015 onwards but persisted for high maternal education. However, an intersection of higher household wealth and maternal education mitigated stunting to a greater extent than either factor in isolation. Residence only predicted stunting in 2005–2006 with an urban disadvantage (adjusted OR: 1.18; 95% CI: 1.07 to 1.29). Children from marginalised social groups displayed increased likelihoods of stunting, from 6–16% in 2005–2006 to 11–21% in 2015–2016 and 2020–2021. Being male was associated with 6% and 7% increased odds of stunting in 2015–2016 and 2019–2021, respectively. Increased household wealth (45%) and maternal education (14%) contributed to decreased stunting prevalence between 2005 and 2021.
Conclusions
Stunting prevalence in India has decreased across social groups. However, social disparities in stunting persist and are exacerbated by intersections of low household wealth, maternal education and being from a marginalised social group. Increased survival must be accompanied by needs-based interventions to support children and mitigate mutually reinforcing sources of inequality.
Keywords: Malnutrition
WHAT IS ALREADY KNOWN ON THIS TOPIC
Stunting is associated with suboptimal development, diminished human capital and reduced economic productivity.
WHAT THIS STUDY ADDS
This study found that the rate of decline in stunting has slowed in recent years in India and that it is influenced by intersecting factors, primarily household wealth, marginalised social group status and maternal education.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
Greater policy action is required to mitigate stunting in children impacted by multiple interacting factors.
Introduction
Stunting, or low height-for-age, is the consequence of a child experiencing chronic malnutrition. It has been associated with impaired neurological, cognitive, physiological and psychosocial development.1 The adverse impact of stunting at the individual level has wide-ranging implications for society, including diminished human capital and economic productivity.2 Furthermore, an intergenerational effect of stunting has caused concern.3 The United Nations Sustainable Development Goals Target 2.2 sets out to ‘end all forms of malnutrition’ by 2030.4 Significant progress has been made in reducing stunting globally, with a 10.7% decrease in prevalence between 2000 and 2022. However, socioeconomic inequalities between and within countries continue to be ubiquitous. Stunting prevalence is also associated with economic development, and 64% of children affected by stunting reside in lower-middle-income countries.5 Most of the world’s stunted children live in Sub-Saharan Africa (38.3%), followed by Central and Southern Asia (36.6%).
India has the largest population of children under 5 years in the world and has almost one-quarter (24.2%) of the world’s stunted children.6 7 There is a notable disparity in stunting prevalence among the nation’s 28 states and 8 union territories (Meghalaya—46.5%; Puducherry—20%) (20%).8 Extant research in India has demonstrated prominent gaps in stunting by different subgroups. Low household wealth, residing in rural areas, low maternal educational attainment and belonging to a marginalised social group have been associated with increased prevalence and risk of stunting.9–12 Additionally, the impact of a child’s sex on stunting in India has undergone a shift from a female disadvantage in the early 1990s to a male disadvantage.12
India has experienced substantial increases in per capita income and educational attainment among both men and women.13 Increased wealth and levels of maternal education are important drivers of the decline in child stunting across several countries.14 Increased wealth enables improved food security and easier access to healthcare, whereas higher levels of education allow mothers to benefit from information to promote health and nutrition. Furthermore, the Indian government has made considerable efforts to improve the nutrition outcomes of children. The Integrated Child Development Services (ICDS) Scheme currently provides supplemental nutrition, health and antenatal check-ups, nutrition and basic education, and immunisation to over 90.6 million women and child beneficiaries.15 Additionally, the National Nutrition Mission was relaunched in 2018 to reduce India’s stunting prevalence by 2 percentage points per annum.16
Despite the implementation of wide-reaching national policies and interventions, there is a paucity of research utilising recent data to examine how intersecting social determinants of stunting at the individual level have changed and contributed to national trends in stunting prevalence. Therefore, we aimed to fill this gap by analysing data collected between 2005 and 2021. Findings from the analyses have implications for national policy and interventions that support early childhood development. We predict that a reduction in prevalence across all social groups will co-occur with a significantly higher likelihood of stunting among children from low-income families, with less educated mothers and belonging to marginalised social groups. This disadvantage will be more prominent at the intersections of these groups. Moreover, given decreased sex differences in stunting, we expect a rising trend of growing disadvantages for males. We also foresee that changes in household wealth and maternal education will mainly contribute to nationwide reductions in stunting prevalence.
Methods
Data source and study population
This study leveraged data from the three most recent rounds of the National Family Health Survey (NFHS) carried out in 2005–2006 (NFHS-3), 2015–2016 (NFHS-4) and 2019–2021 (NFHS-5).8 17 18 The NFHS collects robust nationally representative cross-sectional data on population and health indicators across numerous socio-demographic domains in all of India’s states and union territories. The eligibility criteria include women between 15 and 49 years, men between 15 and 59 years and living children. Data across NFHS rounds were collected in two stages to achieve better coordination and supervision. The Indian Census served as the sampling frame for selecting primary sampling units (PSUs) in rural areas and census enumeration blocks (CEBs) in urban areas in the first stage. In the second stage, 22 PSUs and CEBs were randomly selected in each district. Across the three NFHS rounds, the household response rates were 97.7% for NFHS-3 and 98% for both NFHS-4 and NFHS-5.
Outcome
Stunting in children under 5 years was the outcome variable of interest. It is based on whether a child’s sex-specific height/length-for-age z-score is 2 or more SD below the WHO Child Growth Standards median.19 We used binary classification to denote stunting. Children’s height was measured in millimetres by health investigators.
Predictor variables
We concentrate on household wealth, belonging to a marginalised social group, urban/rural residence, maternal education and the sex of the child. Household wealth was derived from a Harmonised Wealth Index created by pooling information on the ownership of several assets from the three rounds of NFHS household population data.20 Subsequently, a principal component analysis was deployed to calculate the wealth index score for each household, which was then divided into five quintiles (poorest, poor, middle, richer and richest). Children in the sample were then assigned to the appropriate wealth quintile based on their household score relative to the population. We used sampling weights of mothers to control for possible disproportionate representation of wealth quintiles.
Marginalised social groups refer to a social category comprising historically marginalised communities. This includes individuals from a tribal community or a lower-ranked group in the Indian caste system. Marginalised social groups were categorised into Scheduled Castes (SCs), Scheduled Tribes (STs), Other Backward Class (OBC) and a residual category, unreserved caste. A binary classification was used to denote urban/rural residence and the sex of the child. Maternal education was categorised into illiterate, primary, secondary, and higher education.
Statistical analyses
We described changes in stunting prevalence over time by calculating the annual average rate of reduction (AARR) between survey rounds. One-way analyses of variance (ANOVAs) were used to compare absolute differences in the national stunting prevalence between NFHS rounds across levels of the selected social predictors.
Binary logistic regression models determined the extent to which social factors predict national-level stunting. A Poisson regression was executed as a sensitivity analysis to account for the possible overestimation in predictions from the logistic regression. Furthermore, we conducted a logistic regression using NFHS-5 data to examine stunting predictions across 64 intersecting groups. These were every combination of two household wealth levels (poor and non-poor, where the former refers to children with a harmonised wealth index score in the lowest two quintiles), four levels of maternal education, four marginalised social groups and two types of residence. The reference category for intersectional comparisons was non-poor, having a mother with higher education, belonging to an unreserved caste and residing in an urban area. Additional factors were added as controls for all regression analyses. This was done to account for confounders shown to be proximal and distal determinants of stunting.14 21 Controls included household religion, child’s age, ICDS utilisation in the last 12 months, private institutional delivery, delivery by skilled attendants, mother’s body mass index, mother’s age (years), mother’s media exposure, mother’s height, mother’s diet diversity, mother’s diet balance, mother’s age at first birth, household size, toilet facility, safe water sources, sex of the household head, fuel source, and state and union territories as the PSU-level factor.
The Kitigawa-Oaxaca-Blinder (KOB) decomposition method was executed using the same predictors and controls to determine how the selected social factors contributed to the change in stunting prevalence between 2005 and 2021.22 23 Using a counterfactual approach, this method decomposes the change in prevalence into two distinct effects: (1) those arising from changes in the distribution of the predictor variables (explained effect); and (2) those arising from the changes in returns to each predictor variable (unexplained effect). We present the main results of the KOB decomposition based on linear probability modelling using NFHS-3 coefficients as counterfactuals. We ran a series of robustness checks, including using a logit mode, and an alternative counterfactual with NFHS-5 coefficients. Sampling weights of mothers were used across analyses. Analyses were performed with Stata V.17.0.
Results
After removing missing data and flagged observations for both the outcome and predictor variables, our final analytical sample comprised 38 996, 211 729 and 192 314 children under 5 years from the NFHS-3, NFHS-4 and NFHS-5, respectively (see table 1 and online supplemental table S1). The percentage of omission from the full sample was 19% in NFHS-3, 13.4% in NFHS-4 and 13.1% in NFHS-5. Sample characteristics for the selected predictor variables are provided in table 2.
Table 1.
Sample representation from NFHS-3 to NFHS-5 for children under 5 years
| NFHS-3 (2005–2006) children under 5 years (% of total sample) |
NFHS-4 (2015–2016) children under 5 years (% of total sample) |
NFHS-5 (2019–2021) children under 5 years (% of total sample) |
|
| Total pre-analytic sample (513 855) |
48 084 (9.36) | 244 508 (47.6) | 221 263 (43.1) |
| Sample of NFHS round (%) | Sample of NFHS round (%) | Sample of NFHS round (%) | |
| Number of flagged observations for the stunting outcome variable | 6778 (14.1) | 19 506 (7.98) | 15 238 (6.89) |
| Sample size after omitting flagged observations of stunting (471 333) |
41 306 (85.9) | 225 002 (92.0) | 206 025 (93.1) |
| Number of flagged and missing observations for the selected predictor and control variables | 2310 (4.8) | 13 273 (5.4) | 13 711 (6.20) |
| Total number of omitted observations | 9088 (19.0) | 32 779 (13.4) | 28 949 (13.1) |
| Final analytic sample size (443 039) |
38 996 (81.0) | 211 729 (86.6) | 192 314 (87.0) |
Flagged observations are data points that have been excluded because they do not correspond to any observable value for the variable being studied. Missing observations are data points that have not been reported or are unavailable.
NFHS, National Family Health Survey.
Table 2.
Sample characteristics for the selected predictor variables across NFHS-3 to NFHS-5 for children under 5 years (%)
| NFHS-3 (2005–2006) (%) |
NFHS-4 (2015–2016) (%) |
NFHS-5 (2019–2021) (%) |
|
| Sample representation in (%) | |||
| Wealth quintile | |||
| Poorest | 56.59 | 29.29 | 13.75 |
| Poorer | 18.86 | 22.04 | 23.49 |
| Middle | 11.58 | 19.48 | 22.70 |
| Richer | 7.53 | 15.84 | 22.37 |
| Richest | 5.43 | 13.35 | 17.69 |
| Marginalised social group | |||
| Schedule Caste (SC) | 20.63 | 21.96 | 23.82 |
| Scheduled Tribe (ST) | 9.26 | 10.28 | 10.33 |
| Other Backward Class (OBC) | 40.99 | 43.89 | 42.42 |
| Unreserved caste | 25.89 | 19.75 | 17.93 |
| Residence | |||
| Rural | 75.29 | 72.23 | 73.83 |
| Urban | 24.71 | 27.77 | 26.17 |
|
Maternal education | |||
| Illiterate | 49.17 | 29.69 | 21.01 |
| Primary | 14.24 | 14.05 | 12.29 |
| Secondary | 31.56 | 45.83 | 51.16 |
| Higher | 5.03 | 10.43 | 15.53 |
| Sex of the child | |||
| Female | 47.72 | 48.10 | 48.19 |
| Male | 52.28 | 51.90 | 51.81 |
NFHS, National Family Health Survey.
bmjnph-2023-000648supp001.pdf (647.6KB, pdf)
Stunting prevalence
The national prevalence of stunting decreased by 19.88% with an AARR of 2.20% between NFHS-3 and NFHS-4 (see table 3). However, between NFHS-4 and NFHS-5, stunting only decreased by 7.75%, with a slower annual rate of decline (AARR: 1.33%).
Table 3.
National stunting prevalence, annual average rate or reduction and percentage change of decline across NFHS-3 to NFHS-5
| NFHS-3 (2005–2006) |
NFHS-4 (2015–2016) |
NFHS-5 (2019–2021) |
|
| Stunting prevalence (%) | 48.3 | 38.7 | 35.7 |
| NFHS-3 to NFHS-5 | NFHS-3 to NFHS-4 | NFHS-4 to NFHS-5 | |
| Annual average rate of reduction (%) | 1.88 | 2.20 | 1.33 |
| Percentage change of decline (%) | 26.09 | 19.88 | 7.75 |
NFHS, National Family Health Survey.
Stunting prevalence across levels of the selected predictor variables with p values from the one-way ANOVA is shown in table 4. A wealth gradient of stunting prevalence was observed across all rounds. However, stunting prevalence decreased most in the poorest quintile (8.7 pp, p<0.0001) and increased in the richest wealth quintile (3.2 pp, p<0.0001).
Table 4.
National stunting prevalence (%) across levels of the selected predictors and associated p values derived from one-way ANOVAs for NFHS-3 to NFHS-5
| NFHS-3 (2005–2006) (95% CI) |
NFHS-4 (2015–2016) (95% CI) |
NFHS-5 (2019–2021) (95% CI) |
P values | |
| Wealth quintile | ||||
| Poorest | 56.48 (55.781 to 57.180) | 50.63 (50.259 to 50.991) | 47.77 (47.224 to 48.308) | <0.0001 |
| Poorer | 45.08 (44.021 to 46.137) | 42.92 (42.497 to 43.335) | 42.54 (42.123 to 42.961) | <0.0001 |
| Middle | 38.34 (37.097 to 39.592) | 35.51 (35.057 to 35.966) | 36.72 (36.281 to 37.152) | <0.0001 |
| Richer | 29.07 (27.695 to 30.444) | 28.26 (27.767 to 28.762) | 29.54 (29.108 to 29.979) | 0.0007 |
| Richest | 20.67 (19.325 to 22.016) | 22.56 (22.049 to 23.073) | 23.82 (23.342 to 24.295) | <0.0001 |
| Marginalised social group | ||||
| Scheduled Caste (SC) | 53.99 (52.855 to 55.135) | 43.14 (42.668 to 43.603) | 39.45 (38.993 to 39.915) | <0.0001 |
| Scheduled Tribe (ST) | 53.97 (52.764 to 55.179) | 44.11 (43.644 to 44.567) | 41.16 (40.697 to 41.628) | <0.0001 |
| Other Backward Caste (OBC) | 49.09 (48.257 to 49.931) | 39.01 (38.688 to 39.333) | 35.05 (34.711 to 35.387) | <0.0001 |
| Unreserved caste | 40.85 (39.967 to 41.733) | 31.12 (30.664 to 31.573) | 29.27 (28.785 to 29.765) | <0.0001 |
| Residence | ||||
| Rural | 50.98 (50.370 to 51.584) | 41.53 (41.297 to 41.763) | 37.61 (37.375 to 37.843) | <0.0001 |
| Urban | 39.97 (39.191 to 40.746) | 31.37 (30.978 to 31.765) | 30.39 (29.943 to 30.830) | <0.0001 |
| Maternal education | ||||
| Illiterate | 57.46 (56.707 to 58.216) | 51.08 (50.709 to 51.456) | 46.62 (46.156 to 47.083) | <0.0001 |
| Primary | 48.87 (47.610 to 50.133) | 43.76 (43.225 to 44.298) | 41.89 (41.297 to 42.485) | <0.0001 |
| Secondary | 38.32 (37.559 to 39.084) | 33.07 (32.780 to 33.357) | 33.58 (33.300 to 33.867) | <0.0001 |
| Higher | 19.59 (18.204 to 20.969) | 21.1 (20.544 to 21.648) | 23.11 (22.622 to 23.606) | <0.0001 |
| Sex of the child | ||||
| Female | 48.25 (47.554 to 48.945) | 38.14 (37.849 to 38.426) | 34.86 (34.559 to 35.151) | <0.0001 |
| Male | 48.33 (47.662 to 48.999) | 39.16 (38.881 to 39.442) | 36.52 (36.231 to 36.810) | <0.0001 |
NFHS, National Family Health Survey.
The most notable decrease in stunting prevalence occurred across all marginalised social groups, particularly in SCs (14.5 pp, p<0.0001) and Other Backward Class (OBC) (14.0 pp, p<0.0001) communities. Yet, a prevalence gap between marginalised social groups and the unreserved caste group persisted across all three NFHS rounds.
The marked decrease in rural areas (13.4 pp, p<0.0001) with a lower decline in urban areas (9.6 pp, p<0.0001) indicates the closing of the urban–rural prevalence gap. For stunting prevalence according to levels of maternal education, the most significant decrease occurred for children with illiterate mothers (10.8 pp, p<0.0001). At the same time, there was a 3.5 pp increase (p<0.0001) for children with mothers who received higher education. Stunting prevalence was marginally lower among females than males across all three rounds, with the difference increasing with each survey round.
Association of selected social factors in predicting stunting
The results of the logistic regression analysis are shown in table 5 and online supplemental table S2. Children from the richest wealth quintile were consistently the least likely to be stunted (NFHS-3 AOR: 0.363; 95% CI: 0.292 to 0.450, NFHS-4 AOR: 0.619; 95% CI: 0.565 to 0.678, NFHS-5 AOR: 0.636; 95% CI: 0.588 to 0.688). However, the protective effect of household wealth decreased noticeably from NFHS-4 onwards, particularly for the richest wealth quintile.
Table 5.
Logistic regression results for selected predictor variables
| NFHS-3 (2005–2006) (n=38 996) | NFHS-4 (2015–2016) (n=211 728) | NFHS-5 (2019–2021) (n=192 314) | ||||
| OR (95% CI) | AOR (95% CI) | OR (95% CI) | AOR (95% CI) | OR (95% CI) | AOR (95% CI) | |
| Wealth quintile | ||||||
| Poorest | Ref | Ref | Ref | Ref | Ref | Ref |
| Poorer | 0.633*** (0.588 to 0.682) | 0.775*** (0.710 to 0.846) | 0.733*** (0.710 to 0.758) | 0.905*** (0.872 to 0.939) | 0.809 (0.777 to 0.843) | 0.924*** (0.884 to 0.964) |
| Middle | 0.481*** (0.440 to 0.527) | 0.675*** (0.598 to 0.762) | 0.537*** (0.516 to 0.559) | 0.803*** (0.765 to 0.844) | 0.634*** (0.608 to 0.662) | 0.834*** (0.794 to 0.876) |
| Richer | 0.318*** (0.285 to 0.354) | 0.497*** (0.420 to 0.589) | 0.384*** (0.365 to 0.404) | 0.701*** (0.652 to 0.753) | 0.459*** (0.438 to 0.481) | 0.706*** (0.665 to 0.749) |
| Richest | 0.201*** (0.176 to 0.230) | 0.363*** (0.292 to 0.450) | 0.284*** (0.268 to 0.300) | 0.619*** (0.565 to 0.678) | 0.341*** (0.323 to 0.359) | 0.636*** (0.588 to 0.688) |
| Marginalised social group | ||||||
| Unreserved caste | Ref | Ref | Ref | Ref | Ref | Ref |
| Scheduled Caste (SC) | 1.702*** (1.547 to 1.872) | 1.16*** (1.05 to 1.28) | 1.683*** (1.606 to 1.764) | 1.21*** (1.15 to 1.27) | 1.580*** (1.502 to 1.663) | 1.21*** (1.15 to 1.27) |
| Scheduled Tribe (ST) | 1.698*** (1.520 to 1.898) | 1.14** (1.00 to 1.30) | 1.753*** (1.665 to 1.846) | 1.16*** (1.09 to 1.22) | 1.694*** (1.600 to 1.794) | 1.19*** (1.12 to 1.27) |
| Other Backward Class (OBC) | 1.400*** (1.286 to 1.523) | 1.06 (0.970 to 1.16) | 1.418*** (1.361 to 1.479) | 1.11*** (1.06 to 1.16) | 1.307*** (1.246 to 1.371) | 1.11*** (1.06 to 1.16) |
| Residence | ||||||
| Rural | Ref | Ref | Ref | Ref | Ref | Ref |
| Urban | 0.642*** (0.593 to 0.695) | 1.18*** (1.07 to 1.29) | 0.641*** (0.616 to 0.667) | 1.04 (0.99 to 1.08) | 0.725*** (0.695 to 0.755) | 1.02 (0.970 to 1.06) |
| Maternal education | ||||||
| Illiterate | Ref | Ref | Ref | Ref | Ref | Ref |
| Primary | 0.708*** (0.654 to 0.765) | 0.868*** (0.795 to 0.948) | 0.745*** (0.716 to 0.776) | 0.895*** (0.857 to 0.934) | 0.825*** (0.789 to 0.863) | 0.926*** (0.883 to 0.972) |
| Secondary | 0.460*** (0.431 to 0.491) | 0.795*** (0.730 to 0.867) | 0.473*** (0.459 to 0.487) | 0.774*** (0.746 to 0.804) | 0.579*** (0.560 to 0.599) | 0.814*** (0.782 to 0.848) |
| Higher | 0.180*** (0.157 to 0.207) | 0.637*** (0.530 to 0.767) | 0.256*** (0.241 to 0.272) | 0.641*** (0.596 to 0.688) | 0.344*** (0.328 to 0.362) | 0.698*** (0.657 to 0.743) |
| Sex of the child | ||||||
| Female | Ref | Ref | Ref | Ref | Ref | Ref |
| Male | 1.003 (0.954 to 1.055) | 1.00 (0.949 to 1.06) | 1.044*** (1.019 to 1.070) | 1.07*** (1.04 to 1.10) | 1.075*** (1.049 to 1.102) | 1.08*** (1.05 to 1.11) |
AORs were produced after controlling for all included covariates. SEs are robust and clustered at the primary sampling unit level.
*p<0.10, **p<0.05, ***p<0.01.
AOR, adjusted odds ratio; NFHS, National Family Health Survey.
Relative to a child in an unreserved caste, children from a marginalised social group were more likely to be stunted across all three NFHS rounds. Children from the SC community were consistently the most likely to be stunted (NFHS-3 AOR: 1.16; 95% CI: 1.05 to 1.28, NFHS-4 AOR: 1.21; 95% CI: 1.15 to 1.27, NFHS-5 AOR: 1.21; 95% CI: 1.15 to 1.27). Stunting was only significantly predicted by residence in NFHS-3 after controlling for all covariates (AOR: 1.18; 95% CI: 1.07 to 1.29).
The likelihood of stunting predicted by each level of maternal education remained relatively stable, with a greater protective effect for increasing levels of maternal education. Children with mothers who received higher education were consistently the least likely to be stunted (NFHS-3 AOR: 0.637; 95% CI: 0.530 to 0.767, NFHS-4 AOR: 0.641; 95% CI: 0.596 to 0.688, NFHS-5 AOR: 0.698; 95%CI: 0.657 to 0.743).
Male children were more likely to be stunted than female children in NFHS-4 and NFHS-5 (NFHS-4 AOR: 1.07; 95% CI: 1.04 to 1.1, NFHS-5 AOR: 1.08; 95% CI: 1.05 to 1.11). The results of the Poisson Regression sensitivity analysis were generally concordant with the above results. However, urban/rural residences did not significantly predict stunting across all survey rounds (online supplemental table S3).
The results for the logistic regression exploring 64 intersecting groups of household wealth, maternal education, marginalised social groups and urban/rural residence for NFHS-5 data are in online supplemental table S4 and figure S1. Children who were poor and had illiterate mothers were the most disadvantaged across marginalised social groups and urban/rural residences, with the OR ranging from 3.60 to 5.3 (p<0.0001) (online supplemental table S4 and figure S2). Higher levels of maternal education were generally associated with a lower likelihood of stunting across intersections of household wealth, marginalised social groups and urban/rural residence. Children with mothers who received higher education had a lower likelihood of stunting if they were non-poor (online supplemental table S4, figure S1 and figure S3).
Contribution of selected social factors to the change in stunting prevalence
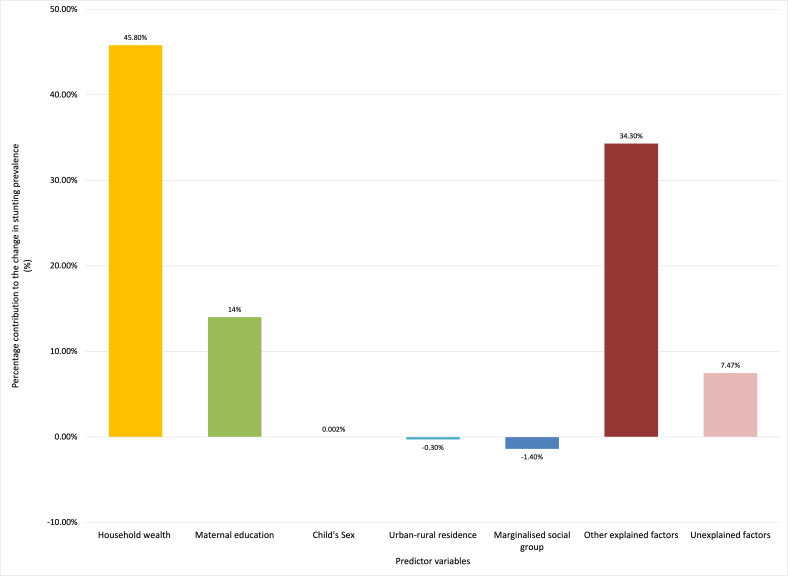
Table 6 shows the explained and unexplained contributions of the change in the distribution of the selected predictor variables and control variables to the change in the mean national stunting prevalence between NFHS-3 and NFHS-5. Changes in the distribution of the predictor variables explained 92.5% (SE=6.23, p<0.0001) of the decrease in stunting. The other 7.47% (SE=6.23, p=0.23) was unexplained. Of the explained contributions, 58.1% of the decrease in stunting was explained by the selected social factors, and 34.3% by the additional covariates accounted for in the analysis (figure 1).
Table 6.
Results for the Kitigawa-Oaxaca-Blinder decomposition
| Changes in mean prevalence | All India aggregate | |
| Coefficients/contributions (SEs) |
P values | |
| Stunting in NFHS-5 | 0.357 (0.002) | <0.0001 |
| Stunting in NFHS-3 | 0.484 (0.004) | <0.0001 |
| Total change | −0.127 (0.005) | <0.0001 |
| Explained | −0.117 (0.007) | <0.0001 |
| Explained contribution (%) | 92.5 (6.23) | <0.0001 |
| Unexplained | −0.009 (0.008) | 0.24 |
| Unexplained contribution (%) | 7.47 (6.23) | 0.23 |
SEs are clustered at the primary sampling unit (PSU) level. Decompositions are clustered at the PSU level and weighted by NFHS survey weights.
NFHS, National Family Health Survey.
Figure 1.
Percentage of the explained and unexplained contributions in stunting prevalence change between 2005 and 2021 from the Oaxaca-Blinder decomposition analysis.
Figure 1 shows the explained and unexplained contributions of the selected predictor variables to the changes in the mean stunting prevalence between NFHS-3 and NFHS-5. Household wealth (45.8%, SE=5.10, p<0.0001) and maternal education (14.0 %, SE=2.57, p<0.0001) contributed significantly to decreases in stunting. Belonging to a marginalised social group did not contribute substantially to the decrease in stunting prevalence (−1.42%, SE=0.577, p=0.013). The contribution to the change in stunting prevalence on account of residence (−0.26%, SE=0.309, p=0.41) and a child’s sex (0.002%, SE=0.018, p=0.93) was not significant. Findings from the sensitivity analyses aligned with these results (online supplemental table S7–S9).
Discussion
This study investigated social determinants of stunting and examined changes in the contributions of socio-demographic elements to national prevalence trends from 2005 to 2021. In line with our predictions, we found that household wealth, maternal education and marginalised social group status were strong predictors of stunting across all three NFHS rounds. Changes in household wealth and maternal education contributed predominantly to the decrease in stunting prevalence between 2005 and 2021. Furthermore, urban–rural disparities in stunting have been minimised, and male children have become increasingly disadvantaged.
Strengths and limitations of this study
We utilised three large datasets with nationally representative data. This study is one of the first to use NFHS-5 data to conduct a detailed examination of trends in the impact of social determinants on stunting at the national level in India. However, our study has limitations. We had a notable reduction in our sample size due to omitting missing and flagged observations in the data. Additionally, the use of cross-sectional data prohibits causal inference. We do not examine subnational nuances or trends of inequality. However, the current results pave the way for future research to examine regional differences in social determinants of stunting. The WHO growth standards used in this study do not account for possible intergenerational and gene-environment effects of height-for-age. This may have led to an overestimation of malnutrition estimates.24 A portion of the data for the NFHS-5 was collected after the COVID-19 nationwide lockdown in India. This could have led to a bias in our observations of the impact of wealth on stunting prevalence. However, stunting is a chronic condition generally unresponsive to short-term influences, especially after the age of 2. The pandemic disproportionately impacted low-income families; however, the reduced significance of wealth in predicting stunting could be attributed to the fact that all households, irrespective of their financial status, were affected by the pandemic.
Previous studies examining the prevalence and social determinants of stunting in India primarily use data preceding the NFHS-5. Using an intersectional approach, as used in this study, Kochupurackal and colleagues25 found low household wealth and being from an SC or ST to be associated with increased odds of anthropometric failure.25 Previous studies examining stunting in India using a decomposition approach have consistently found household wealth and maternal education to contribute predominantly to decreasing stunting prevalence at the national and subnational levels.26–28 Avula and colleagues29 found that improvements in maternal factors, including educational attainment, explained between 15% and 30% of the decrease in stunting prevalence between NFHS-3 and NFHS-4 across four Indian states.29 Increased household wealth and maternal education are also important contributors to reductions in stunting prevalence in various countries, including Bangladesh, Nepal, Senegal, and Zambia.30
Interpretations and implications
The sharper decline in stunting between NFHS-3 and NFHS-4 coincides with substantial policy action to mitigate undernutrition. The Supreme Court of India ordered the universalisation of the ICDS in 2006, and it has since rapidly expanded.31 Additionally, the Indian government implemented the National Food Security Act (NFSA) in 2013, which entails the provision of subsidised food grains through a targeted public distribution system and covers 75% of the rural population and 50% of the urban population.32 However, the slower decline in stunting prevalence between NFHS-4 and NFHS-5 indicates the nation is not on track to meeting the goal of reducing stunting by at least 2 percentage points annually or SDG target 2.2. There have been concerns about a lack of investment in the quality and quantity of the food provided in supplemental nutrition programmes in India, resulting in a discordance between supply and demand. For example, only 41% of the required budget for the supplemental nutrition programme under the ICDS was approved for the 2022–2023 financial year.33
Household wealth remained a significant predictor and primarily contributed to the change in stunting prevalence. Still, data from NFHS-4 onwards indicate that high household wealth no longer plays the same role in protecting children from stunting. This could be due to a decrease in absolute poverty, economic development and improved food security. Indeed, the Human Development Index of the country increased by 18.5% between 2005 and 2020.34 Improved nutritional status could have contributed to better physiological and psychological functioning, promoting productivity and reducing poverty.35 Increasing levels of maternal education were consistently associated with decreased odds of stunting. Maternal education remains as important in determining stunting as it was 16 years ago. Higher levels of maternal education are linked to increased health-seeking behaviours and utilisation of healthcare services.21 Our intersectional analysis of NFHS-5 data revealed an intersection of high household wealth and high maternal education, which mitigated stunting to a greater extent than either factor in isolation. This suggests that a multisectoral approach that addresses co-occurring disadvantages could be more effective in mitigating stunting than targeting a particular social group. Additionally, the notable contribution of maternal education to the decrease in stunting between 2005 and 2021 could be attributable to increases in women’s educational attainment in the nation. The percentage of women who have received over 10 years of education has increased by 18.6% between NFHS-3 and NFHS-5.36 37
The elimination of urban–rural gaps in predicting stunting by NFHS-4 suggests that policies and programmes promoting rural health, nutrition and education have been effective. The prevalence and likelihood of stunting for children from marginalised social groups was significantly higher than for children from the unreserved caste, with a trend of increasing likelihood across NFHS rounds. Intersectional analyses revealed the disadvantage was intensified by being poor and having mothers with low educational attainment. This suggests that greater efforts are necessary to ensure children and families from marginalised social groups are supported in accessing and engaging in interventions. India has a history of son preference that has been shown to manifest in poorer nutrition outcomes for girls in the past.12 However, our findings indicate a shift away from this. A meta-analysis that included 47 studies in over 30 countries found a concordant male disadvantage and suggests this could be due to an intersection of biological and social factors, such as the introduction of vaccines for diseases that affect girls more than boys.38
Policy and programmes have had a vital role in ameliorating stunting in India. The generally slow decline in stunting prevalence may be explained by the nation having experienced a sharp decrease in infant and under-five mortality rates. NFHS data reveals that under-5 mortality rates dropped from 74.3 deaths per 1000 live births in 2005–2006 to 41.9 deaths per 1000 live births in 2019–2021.36 37 India has strongly emphasised integrating nutrition interventions into prenatal and postnatal programmes, including in the ICDS, thus increasing child survival rates.39 Therefore, the slow decline in stunting suggests that surviving children are not flourishing. The Nurturing Care Framework advocates optimal Early Childhood Development through the concurrence of services promoting survival and thriving.40
Conclusions
Children from families that are poor, who have mothers with low educational attainment or who belong to a marginalised social group have been and continue to be more vulnerable to stunting. Their social disadvantages preclude their optimal development. Interventions to promote nurturing care are warranted. Furthermore, focusing on social justice is necessary through the equitable provision of services and resources based on the needs of intersecting social groups. Proportionate universalism ensures resources are provided on a needs basis and may be a preferred strategy. Universalism in isolation can undermine the needs of disadvantaged social groups, and targeting can exacerbate the marginalisation of disadvantaged groups.41
Footnotes
Contributors: NRao, NRanganathan and SD conceptualised and designed the study. SD and UA performed the analyses. MB wrote the first draft with the support of NRao. JCC and AMW critically commented on the conceptualisation and analyses. All authors critically reviewed this draft and approved the final draft for submission, with final responsibility for publication. NRao is the guarantor of this paper.
Funding: The work described in this paper is based on two grants received by NRao from the Research Grants Council, Hong Kong SAR China. They are Project No. HKU-17602519, 'Are young children developmentally on track? Comparison between adult ratings and direct assessment in China and India' and Project No. HKU-17609521 - 'Enhancing Early Childhood Development in China and India: Understanding the Contributions of Maternal Education and Policy Variations'.
Competing interests: All authors have completed the ICMJE uniform disclosure form at http://www.icmje.org/disclosure-of-interest/ and declare that the work was supported by two grants from the Research Grants Council, Hong Kong.
Provenance and peer review: Not commissioned; externally peer reviewed by Ankita Mukherjee, United Kingdom of Great Britain and Northern Ireland.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available in a public, open access repository. Data are available upon reasonable request. Data described in this study is from the NFHS. NFHS datasets are freely available from https://dhsprogram.com/data/available-datasets.cfm. Stata codes are available via NRao upon reasonable request.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
Ethical approval was not required for the research conducted. Data collection for the NFHS was conducted under the purview of the institution ethical review board of the Indian Institute of Population Sciences.
References
- 1. de Onis M, Branca F. Childhood stunting: a global perspective. Matern Child Nutr 2016;12 Suppl 1:12–26. 10.1111/mcn.12231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Victora CG, Adair L, Fall C, et al. Maternal and child undernutrition: consequences for adult health and human capital. Lancet 2008;371:340–57. 10.1016/S0140-6736(07)61692-4 Available: https://pubmed.ncbi.nlm.nih.gov/18206223/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Prendergast AJ, Humphrey JH. The stunting syndrome in developing countries. Paediatr Int Child Health 2014;34:250–65. 10.1179/2046905514Y.0000000158 Available: https://www.tandfonline.com/action/journalInformation?journalCode=ypch20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. United Nations General Assembly . Transforming our world: the 2030 agenda for sustainable development | Department of economic and social affairs. Transforming our world: the 2030 agenda for sustainable development. New York. 2015. Available: https://sdgs.un.org/2030agenda
- 5. United Nations Children’s Fund (UNICEF), World Health Organization (WHO), The World Bank . Levels and trends in child malnutrition UNICEF / WHO / World Bank group joint child malnutrition estimates key findings of the 2023 edition. World Heal Organ; 2023. Available: https://www.who.int/publications/i/item/9789240025257 [Google Scholar]
- 6. Population Division UND of E and SA . World population prospects 2022: data sources; 2022.
- 7. United Nations Children’s Fund (UNICEF), World Health Organization, World Bank . Levels and trends in child malnutrition: UNICEF / WHO / the World Bank group joint child malnutrition estimates: key findings of the 2021 edition. New York; 2021.
- 8. [dataset] Indian Institute for Population Sciences, ICF . National Family Health Survey (NFHS5). Denoar, Mumbai. 2022. Available: http://www.rchiips.org/nfhs
- 9. Karlsson O, Kim R, Sarwal R, et al. Trends in underweight, stunting, and wasting prevalence and inequality among children under three in Indian States, 1993–2016. Sci Rep 2021;11:14137. 10.1038/s41598-021-93493-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Subramanyam MA, Kawachi I, Berkman LF, et al. Socioeconomic inequalities in childhood undernutrition in India: analyzing trends between 1992 and 2005. PLoS ONE 2010;5:e11392. 10.1371/journal.pone.0011392 Available: https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0011392 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Bharti R, Dhillon P, Narzary PK. A spatial analysis of childhood stunting and its contextual correlates in India. Clin Epidemiol Glob Heal 2019;7:488–95. 10.1016/j.cegh.2019.04.005 Available: http://cegh.net/article/S2213398418301702/fulltext [DOI] [Google Scholar]
- 12. Tarozzi A, Mahajan A. Child nutrition in India in the nineties. Econ Dev Cult Change 2007;55:441–86. Available: https://www.readcube.com/articles/10.1086/511195 [Google Scholar]
- 13. OECD . Education at a glance 2021: India. Paris: OECD Publishing; 2021. Available: https://www.oecd-ilibrary.org/education/education-at-a-glance-2021_b35a14e5-en [Google Scholar]
- 14. Vaivada T, Akseer N, Akseer S, et al. Stunting in childhood: an overview of global burden, trends, determinants, and drivers of decline. Am J Clin Nutr 2020;112:777S–791S. 10.1093/ajcn/nqaa159 Available: https://academic.oup.com/ajcn/article/112/Supplement_2/777S/5898920 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Ministry of Women and Child Development G . Integrated child development services rapid reporting system. 2021. Available: https://wcd.dashboard.nic.in/scheme_detail/eyJpdiI6Ilp1S2xrcXh4SXNmV0FxOXpna0xYXC9nPT0iLCJ2YWx1ZSI6InE4eVNlc1wvaHA5R2h6T2JiTDdONkVRPT0iLCJtYWMiOiIyYWIwZjg2N2Q5ZGZkYWRjMjZiYWNlMzE2ZTNhYjg4Yzc4YzgxNGIzM2VkNTQ4MzlkYmNlMjg3YTljOTEyMGNhIn0=
- 16. Ministry of Women and Child Development Government of India . Poshan Abhiyaan. 2022. Available: http://poshanabhiyaan.gov.in/#/
- 17. [dataset] Indian Institute for Population Sciences, ICF . National Family Health Survey (NFHS-3). Denoar, Mumbai; 2007.
- 18. [dataset] Indian Institute for Population Sciences, ICF . National Family Health Survey (NFHS-4). Denoar, Mumbai; 2017.
- 19. WHO Multicentre Growth Reference Study Group . WHO child growth standards based on length/height, weight and age. Acta Paediatr Int J Paediatr 2006;95:76–85. 10.1111/j.1651-2227.2006.tb02378.x [DOI] [PubMed] [Google Scholar]
- 20. Staveteig S, Mallick L. Intertemporal comparisons of poverty and wealth with DHS data: a harmonized asset index approach. DHS Methodological Reports; 2014. [Google Scholar]
- 21. Black RE, Victora CG, Walker SP, et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet 2013;382:427–51. 10.1016/S0140-6736(13)60937-X [DOI] [PubMed] [Google Scholar]
- 22. Oaxaca R. Male-female wage differentials in urban labor markets. Int Econ Rev 1973;14:693. 10.2307/2525981 Available: https://www.jstor.org/stable/2525981?casa_token=2KMW06zovAYAAAAA:myiKVQgPgDuk8JYNHL4D-PK4wKKEFxHcwQp4K23o3hzGmx5M-k8UzrmiQMZZgb8knHJtqBJksue8MRBo8uvWVRUKdmux_b7Tkj_cNRWlmu_u0fvBvsyTlA [DOI] [Google Scholar]
- 23. Blinder AS. Wage discrimination: reduced form and structural estimates. J Hum Resour 1973;8:436–55. 10.2307/144855 Available: https://www.jstor.org/stable/pdf/144855.pdf?casa_token=AeEbQMgqDQgAAAAA:VwIwzSZ7gj8VL9fDbOQ2zG-XW0fgaNQT26VOJE16o4W6GdFfAG0tgQaJaj7XHLQV0kXeSVN-Z-CW5oMm9epVot6_6UoINyPjStiJ2oiXJIAlyU8aB9y1pg [DOI] [Google Scholar]
- 24. Subramanian SV, Karlsson O, Kim R. Revisiting the stunting metric for monitoring and evaluating nutrition policies. Lancet Glob Heal 2022;10:e179–80. 10.1016/S2214-109X(21)00504-0 Available: http://www.thelancet.com/article/S2214109X21005040/fulltext [DOI] [PubMed] [Google Scholar]
- 25. Kochupurackal SU, Channa Basappa Y, Vazhamplackal SJ, et al. An intersectional analysis of the composite index of anthropometric failures in India. Int J Equity Health 2021;20:155. 10.1186/s12939-021-01499-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Nie P, Rammohan A, Gwozdz W, et al. Changes in child nutrition in India: a decomposition approach. Int J Environ Res Public Health 2019;16:1–22. 10.3390/ijerph16101815 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Srivastava S, Upadhyay AK. A success story of reduction in childhood stunting and underweight in India: analysis of pooled data from three rounds of Indian demographic and health surveys (1998–2016). J Biosoc Sci 2022;54:106–23. 10.1017/S002193202000070X Available: https://www.cambridge.org/core/journals/journal-of-biosocial-science/article/abs/success-story-of-reduction-in-childhood-stunting-and-underweight-in-india-analysis-of-pooled-data-from-three-rounds-of-indian-demographic-and-health-surveys-19982016/2A52AB4F425B5EF76DC80E51DCC448C1 [DOI] [PubMed] [Google Scholar]
- 28. Menon P, Headey D, Avula R, et al. Understanding the geographical burden of stunting in India: a regression-decomposition analysis of district-level data from 2015–16. Matern Child Nutr 2018;14:e12620. 10.1111/mcn.12620 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Avula R, Nguyen PH, Tran LM, et al. Reducing childhood stunting in India: insights from four subnational success cases. Food Sec 2022;14:1085–97. 10.1007/s12571-021-01252-x Available: https://link.springer.com/article/10.1007/s12571-021-01252-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Headey D, Hoddinott J, Park S. Accounting for nutritional changes in six success stories: a regression-decomposition approach. Glob Food Sec 2017;13:12–20. 10.1016/j.gfs.2017.02.003 [DOI] [Google Scholar]
- 31. Ministry of Women and Child Development G of I . ICDS mission. 2013. Available: https://wcd.nic.in/sites/default/files/IcdsMissionBroad Framework.pdf
- 32. Department of Food & Public Distribution G of I . National Food Security Act (NFSA). 2023. Available: https://dfpd.gov.in/nfsa.htm
- 33. Accountability Initiative, Research C for P . Saksham Anganwadi and POSHAN 2.0 Goi, 2022-23. Vol. 14. Budget Briefs; 2017. [Google Scholar]
- 34. United Nations Development Programme . Trends in India’s HDI 1990-2019. 2022. Available: https://hdr.undp.org/data-center/specific-country-data#/countries/IND
- 35. Siddiqui F, Salam RA, Lassi ZS, et al. The intertwined relationship between malnutrition and poverty. Front Public Health 2020;8:453. 10.3389/fpubh.2020.00453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Indian Institute for Population Sciences . Key indicators for India from NFHS-3. Mumbai. 2006. Available: http://rchiips.org/nfhs/pdf/India.pdf
- 37. Indian Institute for Population Sciences . National Family Health Survey-5 India fact sheet. Mumbai. 2021.
- 38. Thurstans S, Opondo C, Seal A, et al. Boys are more likely to be undernourished than girls: a systematic review and meta-analysis of sex differences in undernutrition. BMJ Glob Health 2020;5:1–17. 10.1136/bmjgh-2020-004030 Available: https://www.readcube.com/articles/10.1136%2Fbmjgh-2020-004030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Rai RK, Kumar SS, Parasannanavar DJ, et al. Tipping the scale: the role of a national nutritional supplementation programme for pregnant mothers in reducing low birth weight and neonatal mortality in India. Br J Nutr 2022;127:289–97. 10.1017/S0007114521000982 Available: 10.1017/S0007114521000982 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. World Health Organization . Nurturing care for early child development: a framework for helping children survive and thrive to transform health and human potential. Geneva. 2018. Available: http://apps.who.int/iris/bitstream/handle/10665/272603/9789241514064-eng.pdf?ua=1
- 41. Marmot M, Bell R. Fair society, healthy lives. Public Health 2012;126 Suppl 1:S4–10. 10.1016/j.puhe.2012.05.014 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjnph-2023-000648supp001.pdf (647.6KB, pdf)
Data Availability Statement
Data are available in a public, open access repository. Data are available upon reasonable request. Data described in this study is from the NFHS. NFHS datasets are freely available from https://dhsprogram.com/data/available-datasets.cfm. Stata codes are available via NRao upon reasonable request.