Abstract
Background
Higher scores for the American Heart Association Life's Essential 8 (LE8) metrics, blood pressure, cholesterol, glucose, body mass index, physical activity, smoking, sleep, and diet, are associated with lower risk of chronic disease. Socioeconomic status (SES; employment, insurance, education, and income) is associated with LE8 scores, but there is limited understanding of potential differences by sex. This analysis quantifies the association of SES with LE8 for each sex, within Hispanic Americans, non‐Hispanic Asian Americans, non‐Hispanic Black Americans, and non‐Hispanic White Americans.
Methods and Results
Using cross‐sectional data from the National Health and Nutrition Examination Survey, years 2011 to 2018, LE8 scores were calculated (range, 0–100). Age‐adjusted linear regression quantified the association of SES with LE8 score. The interaction of sex with SES in the association with LE8 score was assessed in each racial and ethnic group. The US population representatively weighted sample (13 529 observations) was aged ≥20 years (median, 48 years). The association of education and income with LE8 scores was higher in women compared with men for non‐Hispanic Black Americans and non‐Hispanic White Americans (P for all interactions <0.05). Among non‐Hispanic Asian Americans and Hispanic Americans, the association of SES with LE8 was not different between men and women, and women had greater LE8 scores than men at all SES levels (eg, high school or less, some college, and college degree or more).
Conclusions
The factors that explain the sex differences among non‐Hispanic Black Americans and non‐Hispanic White Americans, but not non‐Hispanic Asian Americans and Hispanic Americans, are critical areas for further research to advance cardiovascular health equity.
Keywords: equity, health disparities, Life's Essential 8, sex, socioeconomic status
Subject Categories: Epidemiology, Women
Nonstandard Abbreviations and Acronyms
- CVH
cardiovascular health
- HA
Hispanic American
- LE8
Life's Essential 8
- NHAA
non‐Hispanic Asian American
- NHANES
National Health and Nutrition Examination Survey
- NHBA
non‐Hispanic Black American
- NHWA
non‐Hispanic White American
Clinical Perspective.
What Is New?
The association of socioeconomic status with cardiovascular health is of greatest magnitude among non‐Hispanic White and Black American women compared with non‐Hispanic White and Black American men, with few sex differences among non‐Hispanic Asian Americans and Hispanic Americans.
What Are the Clinical Implications?
Improving socioeconomic status is beneficial for both men and women of all races and ethnicities, but women of some races and ethnicities may have a greater association of socioeconomic status with cardiovascular health than men; thus, multifaceted approaches may be required to advance sex‐based cardiovascular health equity.
Cardiovascular disease (CVD) is the leading cause of death in the United States among men and women. 1 Age‐adjusted CVD mortality rates declined for many years, then hit an inflection point in 2011, and have since remained stable for premature CVD (age, <65 years). 2 , 3 There are disparities in incident premature CVD among Black women and men compared with White women and men, with the former having a 144% and 59% higher risk, respectively. 4 The disparities in incident CVD disappeared after adjustment for clinical, lifestyle, depression, socioeconomic, and neighborhood factors. 4 In women, clinical factors (eg, blood pressure, glucose, lipids, cardiometabolic medications, and forced vital capacity) contributed to 87% of the disparity between Black and White women, followed by neighborhood (32%) and socioeconomic (23%) factors, when examining these factors individually. Similarly, in Black and White men, clinical factors contributed to 64% of the disparity, followed by socioeconomic (50%) and lifestyle (34%) factors, when examining these factors individually. Thus, to eliminate disparities in premature CVD across racial and ethnic groups, it is critical to advance our understanding of socioeconomic status (income, education, and occupation) and clinical and lifestyle factors across racial and ethnic groups. It is also important to consider the role of sex, given the sex‐based variance in CVD prevalence in the United States. 1
In 2010, the American Heart Association developed Life's Simple 7, which consisted of 7 factors that are critical in cardiovascular health (CVH), including diet, physical activity, smoking, body mass index, cholesterol, blood pressure, and blood glucose, 5 and in 2022, the American Heart Association revamped the scoring and added an eighth metric, sleep. 6 This new group of risk factors, Life's Essential 8 (LE8), has disparate attainment across racial and ethnic and sex groups, with non‐Hispanic Black Americans (NHBAs; Americans used to mean US residents) and men having the lowest (worst) CVH scores. 7 , 8
Socioeconomic status (SES) has been posited as a potential explanatory factor for the racial and ethnic disparities in CVH, as SES is associated with attainment of CVH, although we have previously shown that these associations may be limited in some populations, including Black men. 9 The objective of the current analysis was to quantify the association of SES (income, education, insurance status, and employment) with CVH (using the updated LE8 definition) among men and women, stratified by self‐reported racial and ethnic group. On the basis of our prior work, 9 we hypothesized that SES would have a greater magnitude of association on CVH in women compared with men, across racial and ethnic groups.
Methods
Sample Characteristics
The National Health and Nutrition Examination Survey (NHANES) is a multistage, cross‐sectional, stratified, clustered probability sample of US civilian, noninstitutionalized residents organized by the National Center for Health Statistics of the Centers for Disease Control and Prevention. All data and guidance on analytical approaches are freely and publicly available from the US Centers for Disease Control and Prevention's National Center for Health Statistics and can be found at https://www.cdc.gov/nchs/nhanes/index.htm. The analyzed NHANES data were gathered in 4 waves from 2011 to 2018 (2011–2012, 2013–2014, 2015–2016, and 2017–2018). These waves involved oversampling of non‐Hispanic Asian Americans (NHAAs). The included waves were combined and sample weights were transformed following National Center for Health Statistics guidelines. 10 Participants answered questions and underwent physical examination, including blood draws. For this investigation, we included adults aged ≥20 years who self‐identified as Asian, Black, Hispanic, or White and who were not missing any metrics of the LE8 score, SES variables, or covariates (n=13 529; Figure S1). All participants gave written informed consent. The NHANES study protocol was approved by the National Center for Health Statistics Institutional Review Board. This analysis of secondary data was exempted from approval by The Ohio State University Institutional Review Board, because the use of deidentified secondary data is not human subjects research.
SES Variables (Exposures)
The categorization of the exposures, the scoring of the outcome, and analysis of the data were conducted in a similar manner to previously published work. 11 These methods are described in detail below.
Educational Level
NHANES published data on education status, with levels: less than 9th grade, 9th to 11th grade (includes 12th grade with no diploma), high school graduate/general educational development or equivalent, some college or associate's degree, and college graduate or above. Because of the small number of observations, and consistent with our prior publications, 9 the lower levels of education were combined. The 3 categories used in this analysis were high school graduate/general educational development or less, some college or associate's degree, and college graduate or above.
Income
Annual family income divided by the applicable (based on family size) poverty line was the formula used to calculate the income/poverty line ratio. In NHANES, income/poverty line ratio is reported continuously, ranging from 0 (no income) to 5 (≥5 times the poverty line). Regression models featured continuous income/poverty line ratio.
Employment
Employment status options were student, retired, employed, unemployed, homemaker, and unable to work for health reasons/disability.
Health Insurance Status
Health insurance options were private, uninsured, Medicare, Medicaid, military, combination, and other. Combination insurance is any combination of insurance types.
LE8 Scoring (Outcome)
LE8 score (on a scale from 0 to 100) was the average of the scores for the 8 individual health behaviors and factors explained below. 6 Low CVH is an average score of 0 to 49, moderate CVH is a score of 50 to 79, and high CVH is a score of 80 to 100. 6 In regression analyses, LE8 score was modeled continuously.
Body Mass Index
For non‐Asian participants, body mass index (BMI) of <25 kg/m2 received a score of 100 points, BMI of 25 to 29.9 kg/m2 received a score of 70 points, BMI of 30 to 34.9 kg/m2 received a score of 30 points, BMI of 35 to 39.9 kg/m2 received a score of 15 points, and BMI of ≥40 kg/m2 received a score of 0 points. NHAA participants were scored as shown in Table 1.
Table 1.
Measurement and Scoring of LE8
| CVH metric | Method of measurement | Scoring | |
|---|---|---|---|
| Diet | Two 24‐h recalls, intakes averaged | Points | Quantile of DASH score |
| 100 | ≥95th Percentile | ||
| 80 | 75th–94th Percentile | ||
| 50 | 50th–74th Percentile | ||
| 25 | 25th–49th Percentile | ||
| 0 | 1st–24th Percentile | ||
| Physical activity | NHANES Physical Activity Questionnaire | Points | Minutes |
| 100 | ≥150 | ||
| 90 | 120–149 | ||
| 80 | 90–119 | ||
| 60 | 60–89 | ||
| 40 | 30–59 | ||
| 20 | 1–29 | ||
| 0 | 0 | ||
| Smoking | NHANES Smoking and Tobacco Use Questionnaire | Points | Status |
| 100 | Never smoker | ||
| 75 | Quit ≥5 y | ||
| 50 | Quit 1 to <5 y | ||
| 25 | Quit <1 y, or current NDS use | ||
| 0 | Current smoker | ||
| Subtract 20 (if score ≥25) for living with active indoor smoker | |||
| Sleep |
2011 and 2013 cycles: average sleep per night 2015 and 2017 cycles: average weekday sleep per night |
Points | Hours of sleep |
| 100 | 7 to <9 | ||
| 90 | 9 to <10 | ||
| 70 | 6 to <7 | ||
| 40 | 5 to <6 or ≥10 | ||
| 20 | 4 to <5 | ||
| 0 | <4 | ||
| Body mass index | Weight in kg/height in m squared | Points | Body mass index, kg/m2 |
| Non–Asian Americans | |||
| 100 | <25 | ||
| 70 | 25.0–29.9 | ||
| 30 | 30.0–34.9 | ||
| 15 | 35.0–39.9 | ||
| 0 | ≥40.0 | ||
| Asian Americans | |||
| 100 | <23.0 | ||
| 70 | 23.0–24.9 | ||
| 50 | 25.0–29.9 | ||
| 25 | 30.0–34.9 | ||
| 0 | ≥35.0 | ||
| Non–HDL‐C | Enzymatically measured total cholesterol minus HDL‐C | Points | Non–HDL‐C, mg/dL |
| 100 | <130 | ||
| 60 | 130–159 | ||
| 40 | 160–189 | ||
| 20 | 190–219 | ||
| 0 | ≥220 | ||
| If drug‐treated level, subtract 20 (if score ≥20) | |||
| Blood glucose | Glycated hemoglobin | Points | Glycated hemoglobin, % |
| 100 | <5.7, No diabetes | ||
| 60 | 5.7–6.4, No diabetes | ||
| 40 | <7.0, With diabetes | ||
| 30 | 7.0–7.9, With diabetes | ||
| 20 | 8.0–8.9, With diabetes | ||
| 10 | 9.0–9.9, With diabetes | ||
| 0 | ≥10.0, With diabetes | ||
| Blood pressure | Appropriately measured systolic and diastolic blood pressure | Points | Blood pressure, mm Hg |
| 100 | <120/<80 | ||
| 75 | 120–129/<80 | ||
| 50 | Systolic 130–139 or diastolic 80–89 | ||
| 25 | Systolic 140–159 or diastolic 90–99 | ||
| 0 | Systolic ≥160 or diastolic ≥100 | ||
| If drug‐treated level, subtract 20 (if score ≥20) | |||
Reproduced from Williams et al 11 with permission. Copyright ©2023, John Wiley and Sons. CVH indicates cardiovascular health; DASH, Dietary Approaches to Stop Hypertension; HDL‐C, high‐density lipoprotein cholesterol; LE8, Life's Essential 8; NDS, nicotine delivery system; and NHANES, National Health and Nutrition Examination Survey.
Blood Pressure
Blood pressure was measured ≥3 times. The mean of all measurements was used in this analysis, after excluding implausible values. Blood pressure scores ranged from 0 to 100, as shown in Table 1.
Smoking
Current tobacco users received 0 points. If participants reported quitting, they received a score of 25 to 75 points, depending on how long it had been since quitting, as shown in Table 1. Participants who never smoked received 100 points. For the 2013 to 2017 cycles, e‐cigarette use decreased the score by 20 points (if the score was ≥20). E‐cigarette use was not measured in the 2011 cycle, but e‐cigarette use was rare at that time.
Physical Activity
Self‐reported physical activity was measured via the NHANES Physical Activity Questionnaire. Number of weekly leisure moderate and vigorous physical activity bouts were multiplied by mean bout duration in minutes. The product was weekly physical activity minutes. A total of ≥150 weekly physical activity minutes received a score of 100 points, and 0 weekly physical activity minutes was scored as 0 points. Values in between 0 and 150 minutes received scores between 0 and 100, as shown in Table 1.
Diet
Two days' (averaged) 24‐hour recall data were transformed into the Dietary Approaches to Stop Hypertension score, as described by Fung et al. 12 The 24‐hour recall from day 1 was collected at the Mobile Examination Center using the automated multiple pass method. The recall from day 2 was collected over the telephone 3 to 10 days later with the same method. Ounce and cup equivalents for the required Dietary Approaches to Stop Hypertension food groups were downloaded from the US Department of Agriculture Agricultural Research Service. 13 Consumption levels were then adjusted on the basis of caloric targets for each age/sex group (Table S1–S5). The US Department of Agriculture did not separate low‐fat dairy, so total dairy was used. The US Department of Agriculture did not report sugar‐sweetened beverage intake, so kilocalories from sugar‐sweetened beverages were calculated and then averaged from the 2 days' recall. Quantile cutoff points for the Dietary Approaches to Stop Hypertension score were used to calculate the LE8 diet score, as described in Table 1.
Cholesterol
Total cholesterol was measured enzymatically by hydrolyzing cholesterol esters and producing H2O2, which was then quantified chromatically with paraquinone. Total cholesterol, high‐density lipoprotein cholesterol, and self‐reported prescription of hypercholesterolemia medications were used to calculate the cholesterol score. Total cholesterol minus high‐density lipoprotein cholesterol (non– high‐density lipoprotein cholesterol) <130 mg/dL without hypercholesterolemia medication received a score of 100 points. Non– high‐density lipoprotein cholesterol of ≥220 mg/dL received a score of 0 points. Values in between 130 and 220 mg/dL received scores between 0 and 100, as shown in Table 1.
Blood Glucose
The glycemia score was based on diabetes status (self‐reported diagnosis, hemoglobin A1c [HbA1c] ≥6.5, or use of diabetes medication) and HbA1c. High‐performance liquid chromatography was used to measure HbA1c. An HbA1c of <5.7% in the absence of diabetes received a score of 100 points. For participants with diabetes, the highest score possible was 40 points (HbA1c <7.0%). Participants with an HbA1c ≥10.0% received a score of 0 points. Values of HbA1c between 7.0% and 10.0% received scores between 0 and 40, as shown in Table 1.
Sleep
Self‐reported hours of average weekday sleep were used for cycles 2015 and 2017, and self‐reported mean hours of sleep per night were used for cycles 2011 and 2013. A total of 7 to <9 hours of sleep per night received a score of 100 points, and 0 points were awarded for sleep <4 hours per night. Other sleep durations received points between 0 and 100, as shown in Table 1.
Demographic Variables (Covariates)
Race and Ethnicity
Race and ethnicity were self‐reported from the available categories of non‐Hispanic White, non‐Hispanic Black, non‐Hispanic Asian, non‐Hispanic other, Mexican American, and other Hispanic. For this assessment, participants who identified as non‐Hispanic other were excluded (n=1646), and participants who identified as other Hispanic or Mexican American were combined into the Hispanic American (HA) group. The 4 included groups were HA, NHAA, NHBA, and non‐Hispanic White American (NHWA).
Age
Age at time of data collection was calculated in years from the participant's self‐reported or imputed date of birth. Participants aged >80 years were coded as 80 to minimize risk of identification.
Sex
Sex was self‐reported at the time of the survey, with male or female being the only options.
Statistical Analysis
Linear regression was used to quantify the association of SES variables (exposure) with LE8 score (outcome). An interaction term was included in the model to test the interaction of sex with SES variables in the association with LE8 score among men and women of each racial and ethnic group (see conceptual model, Figure S2). Univariate models contained only the sex×SES variable interaction term describing LE8 score (the software automatically adds the main effects of SES and sex to the model).
Age‐adjusted models contained the interaction term, main effects, and age. Multivariable models were adjusted for age and all SES variables not included in the interaction term. Statistical analyses were performed in R, version 4.0.3 (R Foundation for Statistical Computing, Vienna, Austria). All analyses were performed accounting for NHANES sample weights, primary sampling units, and strata, in R, using the survey package. 14 , 15 , 16 , 17 , 18 Models were computed using the glm function of the survey package, and predicted LE8 scores were extracted from these models with the predict function of the stats package. Statistical significance for all analyses was defined as 2‐sided α <0.05 for main effects of the models, and a 2‐sided α<0.1 for interaction terms, as in previous studies. 19
Results
Sample Characteristics
The overall weighted sample (n=13 529) was 15% HA, 11% NHBA, 5% NHAA, 69% NHWA, 49% men, and representative of the US population. Median age was 48 years. In all racial and ethnic groups, there was a greater proportion of women in the high CVH category than men, with the most prominent difference being among HAs, where only 36% of participants with high CVH are men (Table 2).
Table 2.
Sample Characteristics of Male and Female Adult Participants by Race and Ethnicity
| Characteristics | Hispanic Americans | Non‐Hispanic Asian Americans | Non‐Hispanic Black Americans | Non‐Hispanic White Americans | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Male | Female | Male | Female | Male | Female | Male | Female | |||||||||||||||||
| Obs. | N | % | Obs. | N | % | Obs. | N | % | Obs. | N | % | Obs. | N | % | Obs. | N | % | Obs. | N | % | Obs. | N | % | |
| Age, y | ||||||||||||||||||||||||
| 20–30 | 269 | 4033 | 51 | 323 | 3933 | 49 | 167 | 1408 | 54 | 161 | 1212 | 46 | 268 | 2392 | 47 | 297 | 2743 | 53 | 443 | 11 888 | 52 | 450 | 10 784 | 48 |
| 31–50 | 512 | 6106 | 51 | 583 | 5805 | 49 | 303 | 2023 | 51 | 287 | 1979 | 49 | 414 | 3140 | 43 | 544 | 4173 | 57 | 882 | 21 107 | 51 | 912 | 20 605 | 49 |
| 51–65 | 459 | 2775 | 49 | 496 | 2908 | 51 | 192 | 1082 | 45 | 186 | 1320 | 55 | 464 | 2484 | 46 | 518 | 2925 | 54 | 673 | 19 136 | 49 | 731 | 20 129 | 51 |
| 66+ | 241 | 1015 | 45 | 280 | 1253 | 55 | 80 | 429 | 41 | 94 | 618 | 59 | 297 | 1055 | 45 | 267 | 1285 | 55 | 875 | 13 153 | 46 | 861 | 15 183 | 54 |
| Income/poverty line ratio | ||||||||||||||||||||||||
| 0–1.00 | 390 | 3153 | 45 | 509 | 3847 | 55 | 82 | 635 | 48 | 87 | 689 | 52 | 317 | 2060 | 39 | 454 | 3176 | 61 | 429 | 5558 | 43 | 486 | 7255 | 57 |
| 1.01–2.00 | 464 | 4345 | 51 | 513 | 4212 | 49 | 108 | 724 | 51 | 101 | 704 | 49 | 375 | 2392 | 44 | 445 | 3081 | 56 | 785 | 11 007 | 47 | 797 | 12 591 | 53 |
| 2.01–3.00 | 241 | 2287 | 53 | 261 | 2043 | 47 | 99 | 679 | 49 | 105 | 695 | 51 | 242 | 1447 | 46 | 258 | 1674 | 54 | 417 | 9979 | 51 | 443 | 9704 | 49 |
| 3.01–4.00 | 155 | 1839 | 55 | 155 | 1530 | 45 | 111 | 729 | 47 | 111 | 835 | 53 | 179 | 1075 | 48 | 166 | 1185 | 52 | 310 | 7923 | 46 | 344 | 9432 | 54 |
| 4.01–5.00+ | 231 | 2305 | 50 | 244 | 2266 | 50 | 342 | 2174 | 50 | 324 | 2205 | 50 | 330 | 2097 | 51 | 303 | 2010 | 49 | 932 | 30 816 | 53 | 884 | 27 720 | 47 |
| Employment | ||||||||||||||||||||||||
| Disability | 130 | 947 | 48 | 140 | 1025 | 52 | 8 | 67 | 36 | 19 | 116 | 64 | 168 | 972 | 46 | 176 | 1120 | 54 | 262 | 4009 | 46 | 285 | 4641 | 54 |
| Employed | 1012 | 10 658 | 57 | 852 | 7970 | 43 | 573 | 3852 | 55 | 441 | 3140 | 45 | 805 | 5680 | 46 | 933 | 6723 | 54 | 1614 | 44 588 | 55 | 1434 | 36 822 | 45 |
| Homemaker | 12 | 70 | 3 | 302 | 2200 | 97 | 12 | 88 | 10 | 112 | 765 | 90 | 11 | 54 | 9 | 84 | 553 | 91 | 21 | 447 | 7 | 252 | 5860 | 93 |
| Retired | 198 | 854 | 42 | 220 | 1174 | 58 | 77 | 427 | 43 | 83 | 557 | 57 | 273 | 995 | 42 | 265 | 1364 | 58 | 772 | 12 732 | 46 | 783 | 14 760 | 54 |
| Student | 13 | 216 | 37 | 32 | 373 | 63 | 34 | 287 | 58 | 30 | 204 | 42 | 36 | 281 | 56 | 28 | 217 | 44 | 35 | 619 | 39 | 35 | 953 | 61 |
| Unemployed | 116 | 1185 | 51 | 136 | 1157 | 49 | 38 | 221 | 39 | 43 | 345 | 61 | 150 | 1089 | 49 | 140 | 1148 | 51 | 169 | 2888 | 44 | 165 | 3666 | 56 |
| Educational level | ||||||||||||||||||||||||
| HS | 930 | 8061 | 52 | 975 | 7384 | 48 | 130 | 939 | 48 | 134 | 1013 | 52 | 704 | 4292 | 50 | 633 | 4280 | 50 | 1084 | 20 583 | 51 | 1002 | 19 515 | 49 |
| Some college | 356 | 3834 | 47 | 477 | 4367 | 53 | 134 | 942 | 44 | 167 | 1223 | 56 | 475 | 3202 | 42 | 638 | 4336 | 58 | 941 | 20 569 | 47 | 1112 | 23 165 | 53 |
| College+ | 195 | 2035 | 49 | 230 | 2147 | 51 | 478 | 3061 | 51 | 427 | 2892 | 49 | 264 | 1578 | 39 | 355 | 2509 | 61 | 848 | 24 131 | 50 | 840 | 24 021 | 50 |
| Insurance | ||||||||||||||||||||||||
| Combination | 149 | 833 | 50 | 158 | 820 | 50 | 36 | 242 | 45 | 47 | 292 | 55 | 213 | 862 | 44 | 213 | 1096 | 56 | 655 | 10 757 | 48 | 637 | 11 715 | 52 |
| Medicaid | 94 | 731 | 30 | 200 | 1744 | 70 | 38 | 305 | 53 | 43 | 267 | 47 | 111 | 914 | 32 | 267 | 1942 | 68 | 134 | 2161 | 40 | 211 | 3236 | 60 |
| Medicare | 136 | 578 | 50 | 129 | 588 | 50 | 40 | 210 | 42 | 41 | 284 | 58 | 143 | 528 | 43 | 133 | 700 | 57 | 280 | 4449 | 45 | 306 | 5384 | 55 |
| Military | 17 | 132 | 50 | 11 | 131 | 50 | 4 | 34 | 24 | 10 | 109 | 76 | 62 | 379 | 66 | 24 | 196 | 34 | 81 | 1265 | 55 | 38 | 1047 | 45 |
| Other | 79 | 713 | 39 | 135 | 1112 | 61 | 50 | 409 | 56 | 39 | 323 | 44 | 86 | 573 | 40 | 117 | 868 | 60 | 117 | 2734 | 47 | 150 | 3114 | 53 |
| Private | 519 | 5807 | 52 | 566 | 5318 | 48 | 469 | 3022 | 49 | 457 | 3190 | 51 | 519 | 3543 | 46 | 621 | 4237 | 54 | 1194 | 35 810 | 50 | 1283 | 35 908 | 50 |
| Uninsured | 487 | 5135 | 55 | 483 | 4186 | 45 | 105 | 721 | 52 | 91 | 663 | 48 | 309 | 2272 | 52 | 251 | 2086 | 48 | 412 | 8107 | 56 | 329 | 6296 | 44 |
| LE8 | ||||||||||||||||||||||||
| Low | 337 | 2746 | 61 | 275 | 1767 | 39 | 70 | 411 | 57 | 41 | 316 | 43 | 420 | 2462 | 50 | 402 | 2485 | 50 | 651 | 11 676 | 54 | 552 | 9814 | 46 |
| Moderate | 1012 | 9379 | 51 | 1109 | 8982 | 49 | 486 | 3293 | 53 | 422 | 2966 | 47 | 906 | 5702 | 43 | 1057 | 7443 | 57 | 1862 | 43 168 | 53 | 1769 | 38 755 | 47 |
| High | 132 | 1804 | 36 | 298 | 3149 | 64 | 186 | 1238 | 40 | 265 | 1846 | 60 | 117 | 907 | 43 | 167 | 1198 | 57 | 360 | 10 439 | 37 | 633 | 18 133 | 63 |
% Indicates weighted percentage; HS, high school or less; LE8, Life's Essential 8; N, weighted number (in 1000s); and Obs., number of participants (observations).
Predicted LE8 Scores
Figure 1 shows that at lower levels of education and income, predicted LE8 scores were not appreciably different between men and women among NHBAs and NHWAs, holding age constant. Appreciable sex differences among NHBAs and NHWAs appeared at higher income and education levels, with women having the higher scores. Among HAs and NHAAs, women generally had higher LE8 scores than men at all levels of SES. One notable exception is the higher scores of NHAA men compared with women when retired or with Medicare insurance.
Figure 1. Predicted Life's Essential 8 (LE8) values for each level of socioeconomic status by sex and race and ethnicity, with age held constant at the median (48 years).
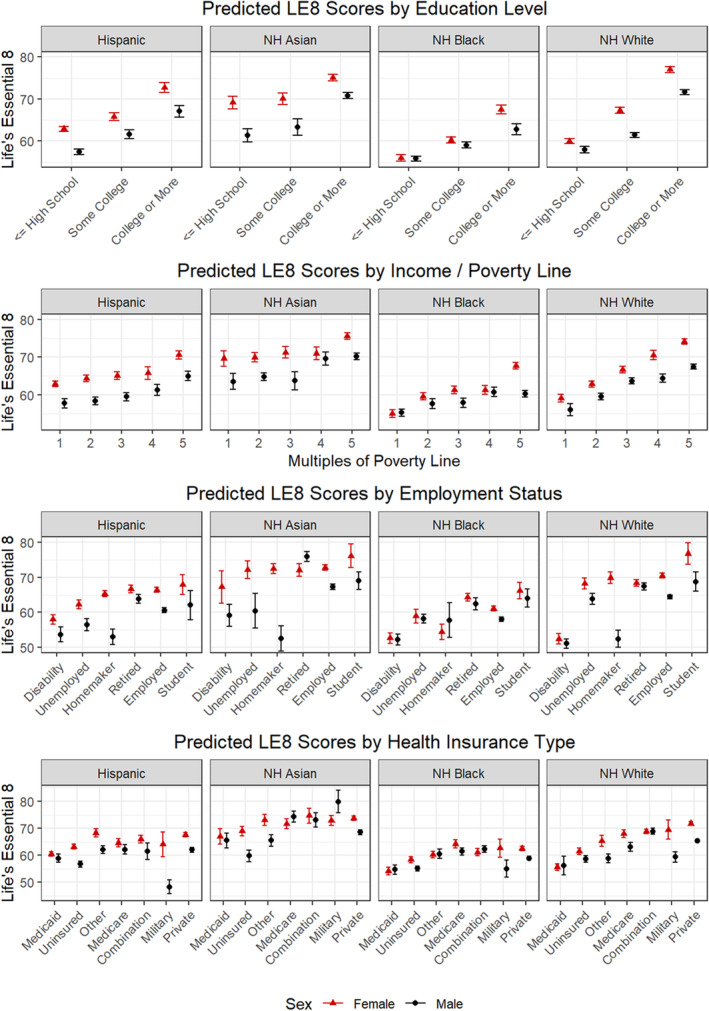
Predicted LE8 scores for women are in red, and scores for men are in black. Radio masts indicate SE of the predicted scores. NH indicates non‐Hispanic.
Education and LE8 Scores
Among NHBAs and NHWAs, women had a greater magnitude of positive association of college degree or more (compared with high school or less) with LE8 scores than men after adjusting for age (interaction P=0.013 among NHBAs and P=0.006 among NHWAs). There was no difference between HA or NHAA men and women in this association in age‐adjusted models (Figure 2 and Table S2).
Figure 2. Association of socioeconomic status measures with Life's Essential 8 scores by race and ethnicity and sex, with sex interaction P values indicated.
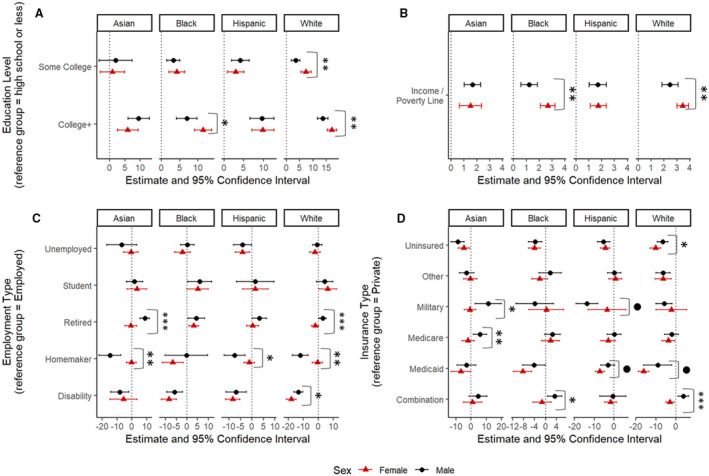
Estimates represent the difference in Life's Essential 8 score for the indicated group compared with the reference group of the same sex, race, and ethnicity. Error bars are 95% CIs of this difference. Interaction P values are indicated by the following symbols: ● indicates P<0.1, *P<0.05, **P<0.01, **P<0.001. Estimates are from models adjusted for age. A, The association of educational level with Life's Essential 8 score. B, The association of income/poverty line ratio with Life's Essential 8 score. C, The association of employment type with Life's Essential 8 score. D, The association of insurance type with Life's Essential 8 score. Interpretation: Black women have a greater magnitude of association of college or more education (compared with high school or less education) with cardiovascular health than Black men (12 vs 7 LE8 points; P=0.01). White women have a greater magnitude of association of income/poverty line ratio with cardiovascular health than White men (3.4 vs 2.5; P=0.002). Asian women have a negative association of Medicare health insurance (compared with private insurance) with cardiovascular health, and Asian men have a positive association (−2 vs 6; P=0.005). Hispanic men have a greater magnitude of association of homemaker employment status (compared with employed) with cardiovascular health score than Hispanic women (−8 vs −1; P=0.02).
Income/Poverty Line Ratio and LE8 Scores
Among NHBAs and NHWAs, women had a greater magnitude of positive association of income/poverty line ratio with LE8 scores than men after adjusting for age (interaction P=0.001 among NHBAs and P=0.002 among NHWAs). Among HAs and NHAAs, there was no difference between men and women in this age‐adjusted association (Figure 2 and Table S3).
Insurance
The most common combination of insurances was Medicare and private insurance. Among NHWAs and NHBAs in age‐adjusted models, men with a combination of insurances had numerically higher LE8 scores than men with private insurance only, whereas women with a combination of insurances had lower scores than women with private insurance only. These sex differences resulted in significant interaction term P values (P=0.011 among NHBAs and P<0.001 among NHWAs). Among NHAAs and HAs, there were no significant sex differences in the association of combination insurance with LE8 scores; however, the same pattern of higher scores among men and lower scores among women was seen among NHAAs with Medicare insurance compared with private insurance (P=0.005; Figure 2 and Table S4).
Employment
Among NHAAs and NHWAs, men who were retired had higher LE8 scores than men who were employed, whereas women who were retired had lower scores than women who were employed after adjusting for age. These sex differences resulted in significant interaction term P values (P<0.001 for NHAAs and NHWAs; Figure 2 and Table S5).
Discussion
Summary
In this US representative sample, NHBA and NHWA populations had a greater magnitude of association of education and income with LE8 in women compared with men. The greater magnitude was a reflection of higher LE8 scores in women in higher education and income categories while having similar LE8 scores to men at the lowest education and income categories. The current analysis shows that there are greater sex differences as income and education increase in NHWA and NHBA populations. In general, women had higher LE8 scores than men in HA and NHAA populations. Thus, no sex disparity existed when comparing higher with lower levels of SES with LE8. Potential explanations for the sex differences in the NHWA and NHBA populations include sex norms around seeking health care, caregiver burden, survivor bias, perceived discrimination, the sex‐based pay gap, and the glass ceiling, which are explained below.
Greater Willingness to Visit a Physician: A Potential Factor Leading to Higher LE8 in Women With High SES Compared With Men
A study of Medical Expenditure Panel Survey data from 1996 found that 60% of men and 77% of women visited a physician in that year. 20 In addition, 26% of men compared with 16% of women did not have a usual source of health care. These trends exist despite men in Medical Expenditure Panel Survey having higher SES and being more likely to work ≥40 h/wk than women. These patterns are not isolated to this sample; others have found women have higher health care use than men, even after adjusting for services like gynecologic examinations. 21 Higher health care use among high SES women compared with high SES men may contribute to women having better preventive care and control of chronic medical conditions than men, leading to higher LE8 scores at higher SES.
Potential Factors Leading to Lower LE8 With Low SES in NHBA and NHWA Women
Caregiver Burden
Women, particularly low SES women, are more likely than men to be caregivers. 22 Caregiver burden is a stress, and stress is associated with poor CVH scores. 23 Among NHBAs and NHWAs, caregiver burden may affect low SES women more than higher SES women, who may be able to afford to reduce caregiver burden through additional paid resources. This difference in caregiver burden may contribute to the lower LE8 scores experienced by lower SES women compared with higher SES women. Among NHAAs and HAs, caregiving may not be a task predominantly performed alone, and instead, a task performed by the entire (extended) family. 24 This may partially explain why no sex differences by income or education were found among NHAAs and HAs.
Perceived Discrimination
Ample research has described the association between perceived discrimination and poorer mental and physical health, but much of it has been focused on race‐ or ethnicity‐based discrimination. 25 Research on sex‐based discrimination is scarcer and often focuses on workplace discrimination. Some studies report similar general discrimination scores by sex, 26 , 27 but studies measuring sex‐specific discrimination have found the opposite. 28 , 29 One may conclude that women experience more sex‐based discrimination, but experience overall discrimination similarly to men. In addition, women may experience poor health outcomes related to discrimination at lower levels of discrimination than men. 27 Limited evidence suggests that perceived race‐ and sex‐based discrimination increases as SES increases among women. 30 , 31 If discrimination leads to poorer health, and women perceive more discrimination as SES increases, one would expect women of high SES to have worse CVH than men of high SES and there to be little difference between men and women of low SES. Instead, this analysis showed men of high SES had lower CVH than women of high SES. More research is needed to explain sex differences in perceived discrimination (or lack thereof) and their relationship to sex differences in CVH by SES.
Sex‐Based Pay Gap and the Glass Ceiling
This and previous analyses show that women earn less income than men, even when adjusting for education and occupation. 32 In addition, women are underrepresented in higher‐paying occupations, like C‐suite level executives, suggesting the existence of what is termed the “glass ceiling.” 32 There are many factors that may explain these gaps, including sex‐based discrimination, career and educational field choice differences, sex differences in risk aversion, and sex‐related norms around nonmarket work. 32 In light of the sex‐related pay gap that persists within education and occupation strata, one would expect women to have lower LE8 scores than men within each stratum of education and occupation, but this analysis revealed the opposite, especially in higher SES strata among NHBAs and NHWAs.
Toxic Stress of Poverty
Poverty, in childhood and in adulthood, is associated with toxic stress, whose effects in children manifest as chronic illnesses in adulthood. 33 The lack of difference in LE8 in the lowest educational attainment, the highest poverty level, and Medicaid as insurance among NHBAs and NHWAs may reflect a more toxic effect of poverty among NHBAs and NHWAs than NHAAs and HAs, and may reflect similar lived experiences and effects of poverty on male and female children that extend into adulthood. More research is needed to understand these observations and relationships.
Survivor Bias
One explanation for the sex differences in LE8 among those who are retired and have Medicare insurance among NHAAs could be survivor bias. It is possible that NHAA men with low scores die at greater rates than NHAA women with low scores. Indeed, men in all age groups have higher rates of myocardial infarction or fatal coronary heart disease than women in those age groups, 34 although there is a dearth of data on sex differences in CVD mortality among NHAAs. In this analysis, 20‐ to 30‐year‐old NHAAs are 54% men, whereas NHAAs aged ≥66 years are only 41% men. This discrepancy is the greatest difference between proportion of men and women at ≥66 years among the studied racial and ethnic groups. This evidence, however, cannot address the question of survivor bias, as it is cross‐sectional. Thus, more longitudinal research is needed.
Factors that influence men's lower LE8 scores than women's in higher strata of SES need to be further explored. We have previously shown that the associations of SES with CVH may be limited in men, particularly in Black men, where education and employment status were not associated with higher attainment of CVH. 9 Mechanistic evaluation of drivers and inhibitors of CVH in men with increasing SES may provide targets for interventions to improve CVH in men.
Strengths and Limitations
The strengths of this study include census‐based definitions of race and ethnicity, the use of a nationally representative sample, gold standard ascertainment of diet (two 24‐hour recalls on nonconsecutive days), a validated physical activity questionnaire, and reliably measured laboratory values. Results should be considered in light of a few limitations. Participants were able to choose only between male or female sex. The study is cross‐sectional in design, so causation and temporality can neither be ascertained nor inferred. For employment status, the employed category was not further subdivided in this analysis, as there was no clear SES gradient among the industry codes supplied by NHANES. Participants who identified themselves as Indigenous or multiracial were not included in this analysis. As is convention, self‐reported data were used for sleep, diet, physical activity, and smoking. Limited overlap in ages between Medicare and private insurances may lead to residual confounding attributable to age, even after adjustment. Multiple models were fit to generate these results, which increases the probability of false‐positive results. Finally, participants of different national origin and immigration statuses are grouped together within the racial and ethnic groups described. These groups could not be further subdivided because of power considerations.
Conclusions
CVH scores were greater in higher SES strata than in lower strata for all sex, race, and ethnicity groups. Women have the greatest magnitude of association of SES with LE8 scores among NHBAs and NHWAs, but not NHAAs and HAs. Improving SES may improve CVH in all groups; however, given the greater magnitude of difference in NHBA and NHWA women compared with men and the higher overall CVH at higher levels of SES in women across racial and ethnic groups, interventions focused on addressing inequities in men's health should consider the intersectional role of SES.
Sources of Funding
This study was funded by the Robert Wood Johnson Foundation Harold Amos Medical Faculty Development Program Award (Dr Joseph; identifier 76236) and the American Heart Association Strategically Focused Research Network on Biologic Pathways of Chronic Psychosocial Stressors on Cardiovascular Health (Dr Joseph; identifier 23SFRNPCS1067039). This publication was supported, in part, by the National Center for Advancing Translational Sciences of the National Institutes of Health under grant UL1TR002733. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Disclosures
None.
Supporting information
Tables S1–S5
Figures S1–S2
This article was sent to Mahasin S. Mujahid, PhD, MS, Associate Editor, for review by expert referees, editorial decision, and final disposition.
Supplemental Material is available at https://www.ahajournals.org/doi/suppl/10.1161/JAHA.123.030805
For Sources of Funding and Disclosures, see page 11.
References
- 1. Tsao CW, Aday AW, Almarzooq ZI, Alonso A, Beaton AZ, Bittencourt MS, Boehme AK, Buxton AE, Carson AP, Commodore‐Mensah Y, et al. Heart disease and stroke statistics—2022 update: a report from the American Heart Association. Circulation. 2022;145:e153–e639. doi: 10.1161/CIR.0000000000001052 [DOI] [PubMed] [Google Scholar]
- 2. Shah NS, Lloyd‐Jones DM, Kandula NR, Huffman MD, Capewell S, O'Flaherty M, Kershaw KN, Carnethon MR, Khan SS. Adverse trends in premature cardiometabolic mortality in the United States, 1999 to 2018. J Am Heart Assoc. 2020;9:e018213. doi: 10.1161/JAHA.120.018213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Lee K, Huang X, Wang MC, Shah NS, Khan SS. Age at diagnosis of CVDs by race and ethnicity in the U.S., 2011 to 2020. JACC Adv. 2022;1:100053. doi: 10.1016/j.jacadv.2022.100053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Shah NS, Ning H, Petito LC, Kershaw KN, Bancks MP, Reis JP, Rana JS, Sidney S, Jacobs DR, Kiefe CI, et al. Associations of clinical and social risk factors with racial differences in premature cardiovascular disease. Circulation. 2022;146:201–210. doi: 10.1161/CIRCULATIONAHA.121.058311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Lloyd‐Jones DM, Hong Y, Labarthe D, Mozaffarian D, Appel LJ, Van Horn L, Greenlund K, Daniels S, Nichol G, Tomaselli GF, et al. Defining and setting national goals for cardiovascular health promotion and disease reduction. Circulation. 2010;121:586–613. doi: 10.1161/CIRCULATIONAHA.109.192703 [DOI] [PubMed] [Google Scholar]
- 6. Lloyd‐Jones DM, Allen NB, Anderson CAM, Black T, Brewer LC, Foraker RE, Grandner MA, Lavretsky H, Perak AM, Sharma G, et al. Life's Essential 8: updating and enhancing the American Heart Association's construct of cardiovascular health: a presidential advisory from the American Heart Association. Circulation. 2022;146:e18–e43. doi: 10.1161/CIR.0000000000001078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Lloyd‐Jones DM, Ning H, Labarthe D, Brewer L, Sharma G, Rosamond W, Foraker RE, Black T, Grandner MA, Allen NB, et al. Status of cardiovascular health in US adults and children using the American Heart Association's new “Life's Essential 8” metrics: prevalence estimates from the National Health and Nutrition Examination Survey (NHANES), 2013–2018. Circulation. 2022;146:822–835. doi: 10.1161/CIRCULATIONAHA.122.060911 [DOI] [PubMed] [Google Scholar]
- 8. Egan BM, Li J, Sutherland SE, Jones DW, Ferdinand KC, Hong Y, Sanchez E. Sociodemographic determinants of Life's Simple 7: implications for achieving cardiovascular health and health equity goals. Ethn Dis. 2020;30:637–650. doi: 10.18865/ed.30.4.637 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Azap RA, Nolan TS, Gray DM, Lawson K, Gregory J, Capers Q, Odei JB, Joseph JJ. Association of socioeconomic status with ideal cardiovascular health in Black men. J Am Heart Assoc. 2021;10:e020184. doi: 10.1161/JAHA.120.020184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. NHANES tutorials . Centers for Disease Control and Prevention. Published March 15, 2020. Accessed December 21, 2021. https://wwwn.cdc.gov/nchs/nhanes/tutorials/default.aspx
- 11. Williams A, Nolan TS, Brock G, Garner J, Brewer LC, Sanchez EJ, Joseph JJ. Association of socioeconomic status with Life's Essential 8 varies by race and ethnicity. J Am Heart Assoc. 2023;12:e029254. doi: 10.1161/JAHA.122.029254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Fung TT, Chiuve SE, McCullough ML, Rexrode KM, Logroscino G, Hu FB. Adherence to a DASH‐style diet and risk of coronary heart disease and stroke in women. Arch Intern Med. 2008;168:713–720. doi: 10.1001/archinte.168.7.713 [DOI] [PubMed] [Google Scholar]
- 13. Food patterns equivalents database. USDA Agricultural Research Service. Accessed December 8, 2021. https://www.ars.usda.gov/northeast‐area/beltsville‐md‐bhnrc/beltsville‐human‐nutrition‐research‐center/food‐surveys‐research‐group/docs/fped‐databases/
- 14. R: A language and environment for statistical computing . Version 4.0.3. The R project for statistical computing. 2021. Accessed November 9, 2020. https://www.r‐project.org/
- 15. Survey: Analysis of complex survey samples. Version 4.0. 2020. Accessed November 9, 2020. https://cran.r‐project.org/web/packages/survey/index.html
- 16. Lumley T. Analysis of complex survey samples. J Stat Softw. 2004;9:1–19. doi: 10.18637/jss.v009.i08 [DOI] [Google Scholar]
- 17. Lumley T. Complex Surveys: A Guide to Analysis Using R. John Wiley & Sons; 2010. doi: 10.1002/9780470580066 [DOI] [Google Scholar]
- 18. svyVGAM: Design‐based inference in vector generalised linear models. Version 1.0. 2021. Accessed March 10, 2021. https://cran.r‐project.org/web/packages/svyVGAM/index.html
- 19. Joseph JJ, Echouffo Tcheugui JB, Effoe VS, Hsueh WA, Allison MA, Golden SH. Renin‐angiotensin‐aldosterone system, glucose metabolism and incident type 2 diabetes mellitus: MESA. J Am Heart Assoc. 2018;7:e009890. doi: 10.1161/JAHA.118.009890 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Xu KT, Borders TF. Gender, health, and physician visits among adults in the United States. Am J Public Health. 2003;93:1076–1079. doi: 10.2105/AJPH.93.7.1076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Briscoe ME. Why do people go to the doctor? Sex differences in the correlates of GP consultation. Soc Sci Med. 1987;25:507–513. doi: 10.1016/0277-9536(87)90174-2 [DOI] [PubMed] [Google Scholar]
- 22. Adelman RD, Tmanova LL, Delgado D, Dion S, Lachs MS. Caregiver burden: a clinical review. JAMA. 2014;311:1052–1060. doi: 10.1001/jama.2014.304 [DOI] [PubMed] [Google Scholar]
- 23. Brewer LC, Redmond N, Slusser JP, Scott CG, Chamberlain AM, Djousse L, Patten CA, Roger VL, Sims M. Stress and achievement of cardiovascular health metrics: the American Heart Association Life's Simple 7 in blacks of the Jackson Heart Study. J Am Heart Assoc. 2018;7:e008855. doi: 10.1161/JAHA.118.008855 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Chan SW‐C. Family caregiving in dementia: the Asian perspective of a global problem. Dement Geriatr Cogn Disord. 2010;30:469–478. doi: 10.1159/000322086 [DOI] [PubMed] [Google Scholar]
- 25. Pascoe EA, Smart RL. Perceived discrimination and health: a meta‐analytic review. Psychol Bull. 2009;135:531–554. doi: 10.1037/a0016059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Levin S, Sinclair S, Veniegas RC, Taylor PL. Perceived discrimination in the context of multiple group memberships. Psychol Sci. 2002;13:557–560. doi: 10.1111/1467-9280.00498 [DOI] [PubMed] [Google Scholar]
- 27. Hahm HC, Ozonoff A, Gaumond J, Sue S. Perceived discrimination and health outcomes: a gender comparison among Asian‐Americans nationwide. Womens Health Issues. 2010;20:350–358. doi: 10.1016/j.whi.2010.05.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Gutek BA, Cohen AG, Tsui A. Reactions to perceived sex discrimination. Hum Relat. 1996;49:791–813. doi: 10.1177/001872679604900604 [DOI] [Google Scholar]
- 29. Kobrynowicz D, Branscombe NR. Who considers themselves victims of discrimination?: individual difference predictors of perceived gender discrimination in women and men. Psychol Women Q. 1997;21:347–363. doi: 10.1111/j.1471-6402.1997.tb00118.x [DOI] [Google Scholar]
- 30. Watson JM, Scarinci IC, Klesges RC, Slawson D, Beech BM. Race, socioeconomic status, and perceived discrimination among healthy women. J Womens Health Gend Based Med. 2002;11:441–451. doi: 10.1089/15246090260137617 [DOI] [PubMed] [Google Scholar]
- 31. Andersson MA, Harnois CE. Higher exposure, lower vulnerability? The curious case of education, gender discrimination, and women's health. Soc Sci Med. 2020;246:112780. doi: 10.1016/j.socscimed.2019.112780 [DOI] [PubMed] [Google Scholar]
- 32. Bertrand M. The glass ceiling. 2017. Becker Friedman Institute for Research in Economics Working Paper No. 2018‐38. https://ssrn.com/abstract=3191467 or https://papers.ssrn.com/sol3/papers.cfm?abstract_id=3191467
- 33. Braveman P, Barclay C. Health disparities beginning in childhood: a life‐course perspective. Pediatrics. 2009;124:S163–S175. doi: 10.1542/peds.2009-1100D [DOI] [PubMed] [Google Scholar]
- 34. Mosca L, Barrett‐Connor E, Kass WN. Sex/gender differences in cardiovascular disease prevention. Circulation. 2011;124:2145–2154. doi: 10.1161/CIRCULATIONAHA.110.968792 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Tables S1–S5
Figures S1–S2


