Abstract
The International Society of Nephrology Global Kidney Health Atlas charts the availability and capacity of kidney care globally. In the North America and the Caribbean region, the Atlas can identify opportunities for kidney care improvement, particularly in Caribbean countries where structures for systematic data collection are lacking. In this third iteration, respondents from 12 of 18 countries from the region reported a 2-fold higher than global median prevalence of dialysis and transplantation, and a 3-fold higher than global median prevalence of dialysis centers. The peritoneal dialysis prevalence was lower than the global median, and transplantation data were missing from 6 of the 10 Caribbean countries. Government-funded payments predominated for dialysis modalities, with greater heterogeneity in transplantation payor mix. Services for chronic kidney disease, such as monitoring of anemia and blood pressure, and diagnostic capability relying on serum creatinine and urinalyses were universally available. Notable exceptions in Caribbean countries included non-calcium-based phosphate binders and kidney biopsy services. Personnel shortages were reported across the region. Kidney failure was identified as a governmental priority more commonly than was chronic kidney disease or acute kidney injury. In this generally affluent region, patients have better access to kidney replacement therapy and chronic kidney disease–related services than in much of the world. Yet clear heterogeneity exists, especially among the Caribbean countries struggling with dialysis and personnel capacity. Important steps to improve kidney care in the region include increased emphasis on preventive care, a focus on home-based modalities and transplantation, and solutions to train and retain specialized allied health professionals.
Keywords: chronic kidney disease, dialysis nurses, hemodialysis, kidney care funding, kidney transplantation, peritoneal dialysis
The International Society of Nephrology (ISN) North America and the Caribbean (NAC) region has one of the highest overall prevalences of kidney disease and kidney replacement therapy (KRT; hemodialysis [HD], peritoneal dialysis [PD], and kidney transplantation [KT]) in the world.1 Yet, tremendous variation in systematic data collection exists within the region, especially among the Caribbean nations. For example, Canada captures detailed metrics on nearly every person with kidney failure, and can assess prevalence, incidence, and quality of care.2 In contrast, the English-speaking Caribbean islands lack population-representative estimates of chronic kidney disease (CKD) prevalence and a KRT registry.
Recognizing that lack of epidemiologic data in turn obscures the need for resources and hampers advocacy for patients with kidney disease, the ISN-Global Kidney Health Atlas (ISN-GKHA) aims to provide on-the-ground insights from in-country experts (nephrologists, policymakers, and administrators). Three rounds of surveys spanning 6 years have been reported (2017–2023) and can further track trends in care over time. The present report seeks to describe both the current status of kidney care availability and delivery in the ISN NAC region and strategies for maintaining and improving care delivery in the region. The methodology for the 2023 survey is described in detail elsewhere.3
Results
The ISN-GKHA results are broadly categorized as literature review (Tables 14, 5, 6, 7, 8, 9, 10, 11 and 24,12, 13, 14, 15; Supplementary Tables S116,17 and S218) and survey response (Figure 1, Figure 2, Figure 3, Figure 4, Figure 5; Supplementary Figures S1–S6), used to describe the state of kidney care in the ISN NAC region.
Table 1.
General demographic and economic indicators of 12 countries of the ISN NAC region, which participated in the ISN-GKHA4, 5, 6, 7, 8, 9, 10, 11
| Country/territory | World Bank ranking | Area (km2) | Total population (2022) | GDP (PPP; $ billion, est. 2021 US$) |
Government health spending per person (2021 US$) | Annual cost KRT (2021 US$) |
||
|---|---|---|---|---|---|---|---|---|
| In-center HD | CAPD | Kidney transplant first year | ||||||
| Global median [IQR] | — | 130,483,015 | 7,802,702,984 | 133.8 [39.7–545.0] | 216 [23–908] | 19,380.3 [11,817.6–38,005.4] | 18,959.2 [10,891.4–31,013.8] | 26,903.2 [15,424.5–70,749.2] |
| NAC median [IQR] | — | 19,849,895 | 380,577,311 | 13.5 [2.0–38.6] | 584 [284–1216] | 39,825.9 [28,095.6–42,146.7] | 39,825.9 [25,224.4–90,937.8] | 265,045.3 [78,392.6–451,697.9] |
| Antigua and Barbuda | HIC | 443 | 100,335 | 1.96 | 623 | — | — | — |
| Aruba | HIC | — | — | — | — | 83,617.11 | 90,937.75 | — |
| The Bahamas | HIC | 13,880 | 355,608 | 13.54 | 1216 | — | — | — |
| Barbados | HIC | 430 | — | — | — | 28,095.58 | — | — |
| Bermuda | HIC | 54 | — | 5.63 | — | — | — | — |
| Canada | HIC | 9,984,670 | 38,232,593 | 1992.05 | 4705 | 42,146.73 | 25,224.38 | 78,392.65 |
| Jamaica | UMIC | 10,991 | 2,818,596 | 29.81 | 211 | 17,622.45 | — | — |
| St. Lucia | UMIC | 616 | 167,122 | 2.57 | 284 | — | — | — |
| St. Vincent and the Grenadines | UMIC | 389 | 100,969 | 1.57 | 225 | — | — | — |
| Trinidad and Tobago | HIC | 5128 | 1,405,646 | 38.61 | 584 | — | — | — |
| Turks and Caicos Islands | HIC | 948 | — | — | — | — | — | — |
| United States | HIC | 9,833,517 | 337,341,954 | 22,996.1 | 6578 | 39,825.88 | 39,825.88 | 451,697.93 |
–, data not reported or unavailable; CAPD, continuous ambulatory peritoneal dialysis; est., estimated; GDP, gross domestic product; GKHA, Global Kidney Health Atlas; HD, hemodialysis; HIC, high-income country; ISN, International Society of Nephrology; IQR, interquartile range; KRT, kidney replacement therapy; NAC, North America and the Caribbean; PPP, purchasing power parity; UMIC, upper-middle–income country.
Table 2.
Kidney replacement therapy and nephrology workforce statistics in the 12 NAC countries participating in the ISN-GKHA12, 13, 14, 15
| Country/territory | World Bank ranking for income status | Published epidemiologic data |
Survey response data |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Treated kidney failure (pmp) |
Chronic dialysis prevalence (pmp) |
Kidney TX (pmp) |
Dialysis and transplant centers (pmp) |
||||||||
| Incidence | Prevalence | Total | HD | PD | Incidence | Prevalence | HD | PD | TX | ||
| Global median (IQR) | — | 145.5 (107.0–212.5) | 822.8 (556.0–1114.0) | 396.6 (105.7–687.0) | 322.7 (76.3–648.8) | 21.0 (1.5–62.4) | 12.2 (3.0–27.8) | 279.0 (58.0–492.0) | 5.07 (1.56–11.12) | 1.57 (0.45–3.10) | 0.46 (0.23–0.75) |
| NAC Median (IQR) |
— | 309.1 (208.1–410.0) | 666.8 (334.6–1415.9) | 620.3 (334.6–805.6) | 515.4 (321.0–678.8) | 11.5 (0.0–114.2) | 40.3 (2.1–76.6) | 6.8 (3.7–610.3) | 18.42 (13.87–26.82) | 9.95 (2.81–19.81) | 0.71 (0.42–3.30) |
| Antigua and Barbuda | HIC | — | — | 515.40 | 515.40 | 0 | — | — | 29.90 | — | 9.97 |
| Aruba | HIC | — | — | — | — | — | — | — | 16.35 | 16.35 | 0 |
| The Bahamas | HIC | — | 651.10 | 620.30 | 506.10 | 114.20 | — | 3.10 | 19.68 | 2.81 | — |
| Barbados | HIC | — | 682.50 | 678.80 | 678.80 | 0 | — | 3.70 | 16.52 | 3.30 | 3.30 |
| Bermuda | HIC | — | — | — | — | — | — | — | 41.47 | 41.47 | — |
| Canada | HIC | 208.10 | 1415.90 | 805.60 | 639.60 | 166.00 | 40.27 | 610.30 | 8.50 | 1.57 | 0.42 |
| Jamaica | UMIC | — | 137.40 | 131.50 | 192.70 | 11.50 | — | 6.80 | 7.81 | 1.42 | 0.71 |
| St. Lucia | UMIC | — | — | 321.00 | 321.00 | 0 | — | — | 23.93 | — | — |
| St. Vincent and the Grenadines | UMIC | — | — | — | — | — | — | — | 29.71 | 19.81 | — |
| Trinidad and Tobago | HIC | — | 334.60 | 334.61 | 278.60 | 56.02 | 2.14 | — | 11.38 | 3.56 | 0.71 |
| Turks and Caicos Islands | HIC | — | — | 1882.40 | 1882.40 | 0 | — | — | 17.16 | 17.16 | — |
| United States | HIC | 410.00 | 2465.00 | 1736.00 | 1552.95 | 197.20 | 76.57 | 729.00 | 22.23 | 20.75 | 0.74 |
–, data not reported or unavailable; ISN, International Society of Nephrology; GKHA, Global Kidney Health Atlas; HD, hemodialysis; HIC, high-income country; IQR, interquartile range: NAC, North America & the Caribbean; PD, peritoneal dialysis; pmp, per million population; TX, transplantation; UMIC, upper-middle–income country.
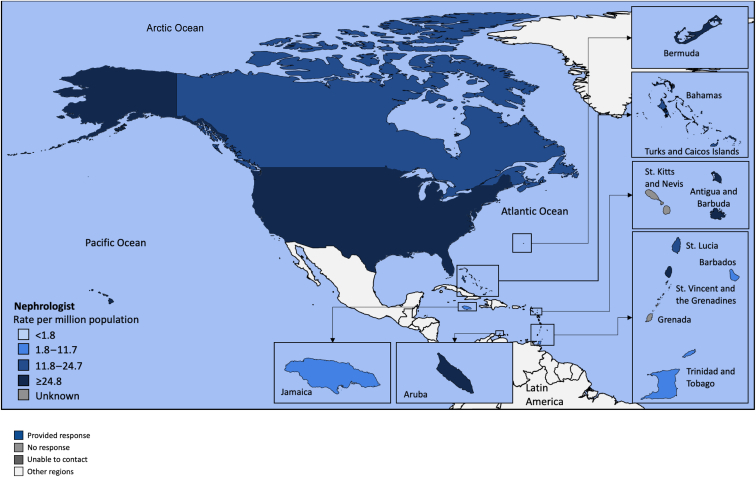
Figure 1.
Countries in the International Society of Nephrology North America and the Caribbean region, with quartiles of nephrologist prevalence in each country shown.
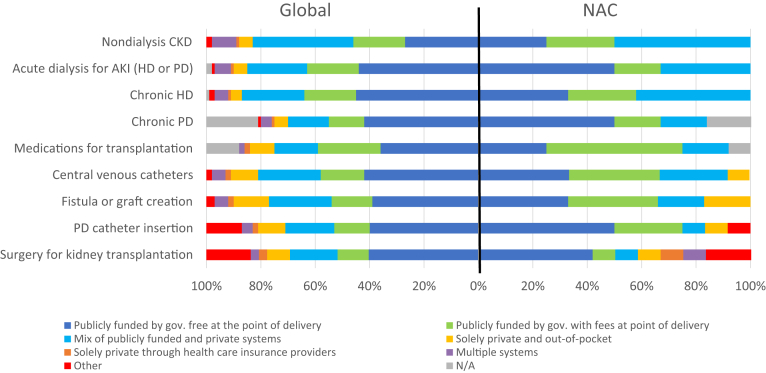
Figure 2.
Funding structures for nondialysis chronic kidney disease (CKD) and kidney replacement therapy care, globally and in the International Society of Nephrology North America and the Caribbean (NAC) region. Values represent absolute number of countries in each category expressed as a percentage of total number of countries. gov., government; HD, hemodialysis; N/A: not available; PD, peritoneal dialysis.
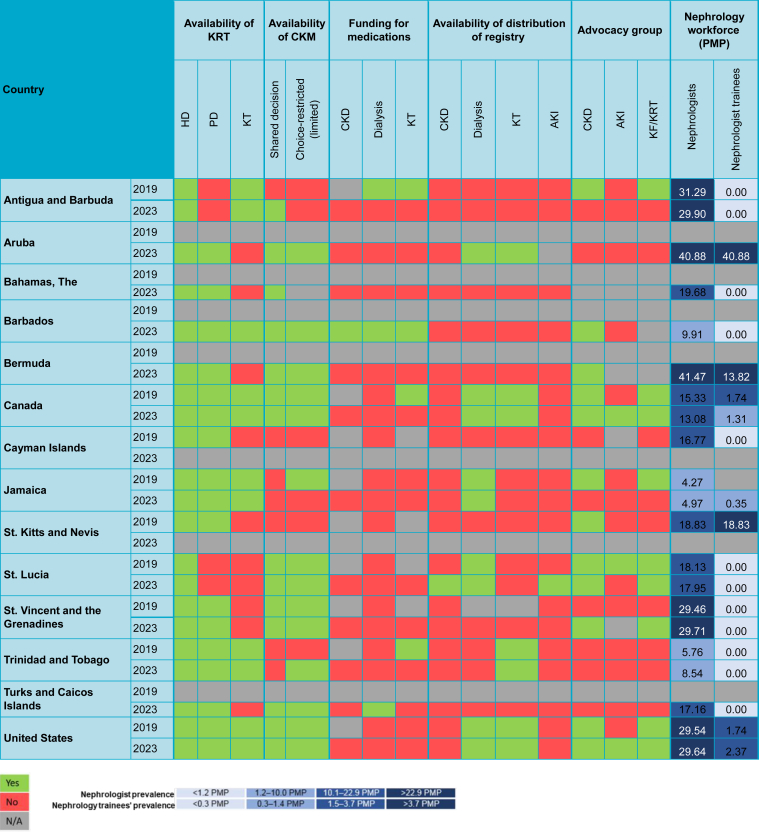
Figure 3.
Country-level scorecard showing availability of kidney replacement therapy (KRT), funding of medications, registry, and advocacy groups in the International Society of Nephrology North America and the Caribbean region, 2019 and 2023. Funding for medications refers to 100% public funding by the government (free at the point of delivery). AKI, acute kidney injury; CKD, chronic kidney disease; CKM, conservative kidney management; HD, hemodialysis; KF, kidney failure; KRT, kidney replacement therapy; N/A, not available; PD, peritoneal dialysis; PMP, per million population.
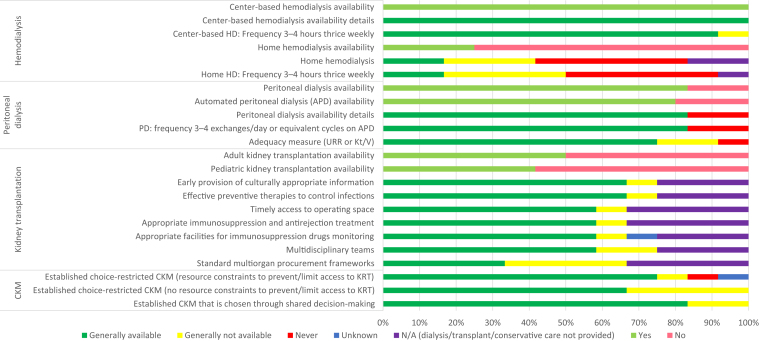
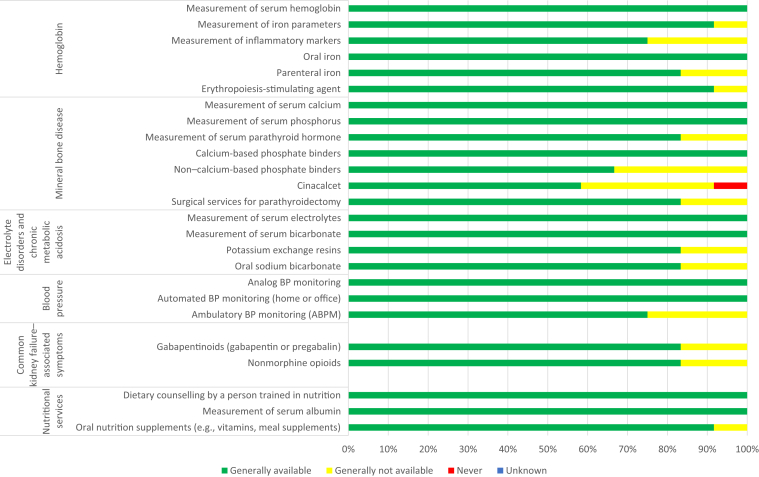
Figure 4.
Availability of choice in kidney replacement therapy or conservative kidney management (CKM) for people living with kidney failure in the North America and the Caribbean region. Values represent absolute number of countries in each category expressed as a percentage of total number of countries. HD, hemodialysis; Kt/V, clearance time per volume; N/A, not available; PD, peritoneal dialysis; URR, urea reduction ratio.
Figure 5.
Availability of services for kidney care in the International Society of Nephrology North America and the Caribbean region. Values represent absolute number of countries in each category expressed as a percentage of total number of countries. BP, blood pressure.
Study setting
The ISN NAC region, as categorized for the purposes of the ISN-GKHA, includes 2 large countries (Canada and the United States [US]) and numerous islands forming an additional 16 countries (Figure 1). Canada and the US each represent over 9 million km2 of surface area. However, Canada is home to around 38 million people, whereas the US is almost 10 times more populous (337 million). In contrast, countries in the Caribbean region have small total surface areas, ranging from 54 km2 (Bermuda) to 13,880 km2 (Bahamas; Table 1).5
Over the past decade, the region increasingly has experienced the effects of climate change. Vast regions of the US and Canada have suffered wildfires, and the Caribbean countries have weathered hurricanes and record droughts. The Southwestern US has experienced drought since 2000 (now termed “megadrought”). The Caribbean region is among the most vulnerable, with costs of climate change expected to exceed $20 billion per year by 2050; governments are acting in the face of tremendous escalating cost to human life and infrastructure, but they are limited by debt.19
Mortality rates from the COVID-19 pandemic were staggeringly high in the US, exceeding one million people as of March 2023, the second-highest number reported across the globe.20 Significantly fewer deaths were reported in Jamaica and the Bahamas (<10,000), but the mortality rate per 100,000 population was similar to that in Canada. Long-lasting effects include an erosion of public trust in public health surveillance, a low level of vaccine acceptance, especially past the primary series, and dramatic increases in healthcare worker burnout.21
Current status of kidney care in the NAC region
In general, in the US and Canada, access to KRT is universal, and the main concerns are cost-containment, reducing dialysis-related mortality despite “adequate” treatment, and improving quality of life for persons receiving dialysis. Preventive care efforts are gaining momentum. Randomized controlled trials evaluating promising therapeutic strategies in kidney preventive care, such as stricter blood pressure targets, sodium-glucose transporter inhibitors, and glucagon-like peptide analogues, have drawn significant numbers of participants from the US and Canada. Rapid access to therapies is available, though not universally. Furthermore, initiatives to identify disease subphenotypes (including the Nephrotic Syndrome Study Network [NEPTUNE] and the Kidney Precision Medicine Project) and integrate innovative trial designs into nephrology practice (e.g., the Time to Reduce Mortality in ESRD [TIME] trial22 and the Major Outcomes with Personalized Dialysate TEMPerature [myTEMP]study23) originate from this region.
Yet heterogeneity is evident, with a lag in both innovation and capacity for kidney care in many countries within the Caribbean. Until the 1970s, public health efforts were focused primarily on infectious disease and maternal–child care.24 Primary healthcare and noncommunicable disease–care infrastructure became a priority relatively recently, despite the fact that diabetes and hypertension are the most common causes of death,9 and that the cause of kidney disease is most commonly ascribed to these conditions. With a lack of systematic registry data, tracking trends in kidney-failure incidence is challenging, but no doubt remains that capacity for kidney care needs to grow, both for prevention of progression and for care of people needing KRT.
Narrative literature review data for countries in the ISN NAC region
Burden of CKD, risk factors, and health workforce
Based on existing data review, the prevalence of CKD in the region was 11.4% (interquartile range [IQR]: 10.5%–11.7%; Supplementary Table S1).16 The regional prevalence was higher than the global prevalence of 9.5% (IQR: 5.9%–11.7%). CKD prevalence ranged from 9.8% (IQR: 9.2%–10.5%) in the Bahamas to 12.9% (IQR: 12.1%–13.8%) in the US. The region had the highest incidence of mortality attributable to CKD, at a median of 4.8%, compared to the global mortality incidence of 2.4%, with 6 Caribbean countries reporting mortality incidence exceeding 4%. The number of disability-adjusted life-years per 100,000 attributed to CKD in NAC was 1169.7, versus 491.4 globally, representing the highest number of disability-adjusted life-years of all the regions. Canada was the only country in which the number of disability-adjusted life-years was lower than the global median.16
Regarding the CKD risk factors in the NAC region, obesity was most prevalent in the US (37.3%) and was lowest in Antigua and Barbuda (19.1%), whereas high blood pressure was most prevalent in St. Lucia (27.1%) and lowest in the US (12.9%; Supplementary Table S2).18 The median prevalence of specialist physicians in the NAC region was 2.3 per 1000 population (vs. 1.95 globally), whereas that of medical doctors was 24.4 per 1000 population (compared to 17.7 globally). The median prevalence of nurses in the region was 45.7 per 1000 population; the US had the highest prevalence (156.9), and Jamaica had the lowest (9.4; Supplementary Table S1).17
Concordant with trends noted in CKD, Canada and the US reported incident and prevalent treated kidney-failure rates that were nearly two-fold or more higher than that of the global median, including for chronic dialysis and transplantation (Table 2).12, 13, 14, 15 The Caribbean countries lacked incident data. Available prevalence data indicated higher than global median prevalence for dialysis in Turks and Caicos Islands, and lower than global and regional median prevalence for dialysis in Jamaica. Notably, transplantation data were available from only 4 of 10 Caribbean countries, and prevalence was drastically lower, ranging from 3.1 per million population (pmp) in The Bahamas to 6.8 pmp in Jamaica, compared with a global median of 279 pmp.
Overview of gross domestic product (GDP) and government health expenditure by individual countries
The NAC region is one of the wealthiest in the world: the per capita GDP (expressed as purchasing power parity in current international $) was highest in the US ($22,996 billion) and lowest in St. Lucia ($1.57 billion; Table 1).5 Government health spending per capita in the region was higher than the global median ($584 vs. $216) with the US, Canada, and the Bahamas being the top 3 countries with the highest government health spending per capita (Table 1).6
Cost of KRT in the NAC region
The median annual costs of in-center HD, PD, and first-year KT in the region were $39,826, $39,826, and $265,045, respectively. Among countries with available cost data, Jamaica had the lowest annual cost of in-center HD ($17,622), whereas Aruba had the highest ($83,617) and also had the highest annual cost of PD ($90,937). Data on the annual cost of the first year of KT were available for Canada ($78,392) and the US ($451,698; Table 1).7, 8, 9, 10, 11
Survey response data for the ISN NAC region
Characteristics of participating countries
A total of 25 respondents (92% nephrologists and 8% others) from 12 countries responded to the survey (Table 1). The number of respondents varied across participating countries: Antigua and Barbuda (n = 2); Aruba (n = 2); The Bahamas (n = 1); Barbados (n = 1); Bermuda (n = 2); British Virgin Islands (n = 1); Canada (n = 2); Curacao (n = 1); Jamaica (n = 3); St. Lucia (n = 1); St. Vincent and the Grenadines (n = 1); Trinidad and Tobago (n = 1); Turks and Caicos Islands (n = 1); US (n = 5); and the Virgin Islands (n = 1). The World Bank classifies 9 countries as being high-income countries, and the remainder as upper-middle–income countries.4 Of note, Cayman Islands, Guyana, Suriname, Dominica, Belize, Puerto Rico, and the US and UK Virgin Islands were surveyed as part of the ISN Latin America region. Grenada, Montserrat, St. Kitts, and Nevis did not respond to the survey.
Health-system financing and service delivery for kidney care
Figure 2 summarizes the funding structures for kidney care in the NAC region. PD surgery and care, and dialysis for acute kidney injury received the greatest proportion of funding from government-funded (free) services alone or a combination of government services and point-of-care fees, compared with other therapies, including nondialysis CKD, presumably encompassing preventive measures to slow progression to kidney failure. KT surgery and medications had the most heterogeneity in payor mix.
Health workforce in kidney care
The oversight of medical kidney care was handled primarily by individual hospitals, trusts, or organizations in 67% of countries (n = 8) in the region, and by a national body for 25% of countries (n = 3). Medical care for people with kidney disease is provided primarily by nephrologists in 83% of countries (n = 10) and by multidisciplinary teams in the remainder (17%; n = 2). The nephrologist workforce of 18.8 pmp (IQR: 11.5–29.8), is comprised mostly of adult nephrologists (19.7 pmp; IQR: 11.8–29.9), and few pediatric nephrologists (0.0 pmp; IQR: 0.0–1.3; Table 2). The number of nephrologists in the NAC region was greater than the global median of 11.8 pmp (IQR: 1.8–24.8), but lower than the median in high-income countries of 25.3 pmp (IQR: 17.9–35.4; Table 2). Three countries in the region (Barbados, Jamaica, and Trinidad and Tobago) had fewer than 10 nephrologists pmp.
Shortages of kidney care providers were reported by all respondents. Specifically, a shortage of surgeons and interventional radiologists to create arteriovenous HD access was most commonly reported (n = 8; 67%), followed by shortages of pediatric nephrologists (n = 7; 58%), transplant surgeons (n = 7; 58%), surgeons and/or interventional radiologists to place PD access (n = 7; 58%), vascular access coordinators (n = 7; 58%), transplant coordinators (n = 7; 58%), dialysis technicians (n = 7; 58%), and palliative care physicians (n = 7; 58%). A shortage of nephrologists was reported in 5 Caribbean countries.
Capacity of KRT provision and availability of conservative kidney management (CKM)
Long-term in-center HD was available in all countries in the region and was the predominant form of dialysis, with a prevalence ranging from 192.7 to 1882.4 pmp (Figures 3 and 4; Table 2). The median number of HD centers was higher in the NAC region than globally (18.4 vs. 5.1 pmp), ranging from 7.8 pmp in Jamaica to 41.5 pmp in Bermuda. Notably, home HD, PD, particularly automated PD, and KT were not universally available in responding countries. Long-term PD was unavailable in Antigua and Barbuda and St. Lucia, and transplantation was unavailable in Aruba, Bermuda, The Bahamas, St. Vincent and the Grenadines, St. Lucia, and Turks and Caicos Islands (Figures 3 and 4; Table 2). Similarly, CKM, chosen through shared decision-making, was not universally available. Even where CKM was reported to be available, core CKM care components were not accessible, highlighting care gaps (Figures 3 and 4). The quality of dialysis and transplantation measures across the region are summarized in Supplementary Figure S1.
Overall, 4 countries (33%) reported within-country variation in the organization of kidney-failure care, and 3 countries (25%) reported within-country variation in the cost of kidney-failure care in their country (Supplementary Figure S2). One third of countries (n = 4; 33%) reported differences in kidney-failure care delivery for children versus adults, with 7 countries (58%) reporting differences in KRT access (Supplementary Figure S2). These differences in access were more marked for PD than for HD, with 3 countries (60%) reporting that children had more access than adults to PD. Sixty percent of countries reported that adults had more access than children to KT.
Availability of services for CKD monitoring and management
Although the ISN NAC region had generally comprehensive availability of services to monitor and treat complications of CKD, some countries in the region lacked availability of treatment for bone-mineral disorders (in the form of noncalcium phosphate binders and calcimimetic agents) and symptoms of kidney failure (Figure 5).
Capacity for identification and management of CKD
The majority of services for CKD diagnostics were available in the region at both the primary and secondary and/or tertiary care levels, with the exception of a crucial diagnostic service (pathology review of kidney biopsies), which was available in 8 of 12 responding countries (67%; Supplementary Figure S3).
Outcomes of hospitalizations and death among people utilizing HD and PD
Seven responding countries of the region reported relatively low first-year HD mortality (1%–10%), mirroring global estimates (Supplementary Figure S4). Four of the 10 countries where PD was available (40%) reported having low mortality rates (1%–10%) within the first year of initiating PD. However, these data were unknown in 5 countries (50%), thereby making comparison with global estimates difficult (Supplementary Figure S4). Similar to the global estimates, cardiovascular disease was the most common of cause of death in the majority of countries in the region, regardless of modality. In addition, approximately 30% of countries (n = 4) reported that 31%–50% of the people receiving KRT would require hospitalization within the first year of HD or PD. Access-related infection was the most common cause of hospitalization for people utilizing HD, and cardiovascular disease for people utilizing PD.
Health information systems
Official registries of CKD (nondialysis) and acute kidney injury were available only in St. Lucia, on a mandatory basis. No official registry for CKM was available in the region. Official registries of dialysis were available in five countries (42%; Aruba, Canada, Jamaica, St. Lucia, the US), whereas 4 countries (33%) had a transplantation registry (Aruba, Canada, Trinidad and Tobago, the US; Figure 3; Supplementary Figure S5).
Barriers to optimal care
The most commonly reported barriers to optimal kidney care across countries in the ISN NAC region were patient knowledge or attitude (n = 12; 100%), followed by healthcare system availability, access, and capability (n = 9; 75%), and economic factors (n = 8; 67%). Physician availability, access, knowledge, and/or attitude, and nephrologist availability, were reported as barriers by 6 countries (50%) and 5 countries (42%), respectively.
Advocacy and policy
A majority of countries reported having a strategy for noncommunicable diseases that had either been implemented (n = 7; 58%) or was under development (n = 3; 25%). However, only 3 countries (25%) reported having CKD-specific strategies, whereas 4 countries (33%) had a CKD strategy incorporated into a general noncommunicable diseases strategy that included other diseases. Seven countries (58%) recognized CKD as a health priority, and only 3 (25%) viewed acute kidney injury as a health priority. Comparatively, kidney failure and/or its treatment by KRT seemed to be higher on the list of government interests, with 10 countries (83%) recognizing it as a health priority (Supplementary Figure S6). Five countries (42%) did not have advocacy groups for any of the 3 categories of CKD, kidney failure, and acute kidney injury (Antigua, Aruba, Jamaica, Trinidad, and Turks and Caicos Islands). Only the US and Canada had advocacy groups for all 3 categories (Figure 3).
Discussion
The third iteration of the ISN-GKHA again highlights the heterogeneity in kidney care across the ISN NAC region. Although this region is composed of primarily high-income and upper-middle–income countries and is largely equipped with reasonable diagnostic and CKD management capacity, it still struggles to generate policies and practices that align with the cohesive kidney care programs recommended by experts.25 Evident from the data is that in most of the 12 responding countries, the very costly treatment of kidney failure is prioritized, whereas systematic strategies for the prevention and management of CKD are lacking. Furthermore, even within the realm of kidney-failure management, in-center HD, the most medically and resource-intensive form of KRT, surpasses all other forms of KRT in terms of prevalence and volume of patients, as well as need for treatment centers.
Efforts to “reverse the tide” toward a more home-based approach are underway in the US and Canada, 2 of the world’s largest users of KRT. In the US, the federal government enacted the Advancing American Kidney Health Executive Order in 2019 with the ambitious target of having 80% of KRT delivery be home-based dialysis or through transplantation.26 The Centers for Medicare and Medicaid Services has changed reimbursement incentives to align with this priority.27 Downstream effects of these policies are yet to be captured. In Canada, innovative assisted PD programs and approaches to reduce disparities in transplantation are under study.28, 29, 30
Policymakers in Caribbean countries could follow the initiatives underway in the US and Canada by focusing capacity-building efforts toward home-based and KT efforts. As data from the 2023 ISN-GKHA demonstrate, the prevalence of CKD is similar in Caribbean countries, compared with that in the US and Canada, yet the KRT incidence, prevalence, center prevalence, and nephrologist capacity are all drastically lower, indicating likely a lack of capacity for care of persons with kidney failure. In Jamaica, 5 public hospital-based units and a little over 20 private units are available to dialyze about 890 patients, once (20%) to twice (70%) weekly, with some (10%) receiving the recommended thrice-weekly treatment. All public units are at capacity, so those without health insurance have to pay an out-of-pocket average of $90–$117 per session.31 In some countries, such as Grenada, dialysis capacity is being newly built,32 and rather than an ad hoc unregulated growth in dialysis capacity, active policy management with incentives toward home therapies and transplantation may achieve a better mix of therapies. For example, home HD is not available in the Caribbean, owing to a lack of personnel training and exorbitant patient-borne costs of purchasing the machine, a financial disincentive that could be revised. Other PD initiatives in the region include a unique nurse-led PD clinic in Bermuda that encourages education, independence, and autonomy with dialysis treatment, and the rolling out of a PD program in the Turks & Caicos Islands shortly.
The COVID-19 pandemic highlighted another advantage of focusing on home-based therapies: in the face of personnel and supply shortages, home HD or PD enables a relatively easier pivot to telehealth services and a reduction in the need for healthcare or interpersonal contact, which has the added benefit of reducing infection transmission.33,34 Similar benefits could be experienced during environmental disasters, especially with advanced planning, and are thus particularly relevant for Caribbean countries,35 where residents have experienced rising temperatures and droughts, in parallel with sea-level rise, and 1 category-4 and 2 category-5 hurricanes in just the past 6 years.36
Unlike in the US and Canada, where deceased-donor kidney transplantation predominates, capacity for transplantation in the Caribbean is largely limited to living-donor transplantation, with surgical capacity available in Jamaica, Trinidad and Tobago, and Barbados. In Trinidad and Tobago, a 15-year review of the National Organ Transplant Unit showed that 195 transplants were done between 2005 and 2020, with 24% from deceased donors, which nonetheless represented a dramatic increase in deceased-donor transplantation over time.37 The authors highlighted the need for additional resources to support the deceased-donor registry and the organ-procurement process.
Limiting the surgical capacity for transplantation may represent a reasonable strategy, as developing high-volume centers of excellence may yield better outcomes38; however, cooperative intercountry agreements that underline clear pathways to surgery would be required to enable equitable access. Furthermore, post-transplantation care pathways are essential to realizing the upfront investment for the surgical procedure and organ procurement. Data on healthcare financing of both the surgical procedure and post-transplant care demonstrate high variability in payor mix, creating a chaotic situation on-the-ground where simplified pathways would enable access to and longevity of the best treatment option for KRT.
Despite the existence of numerous renowned training programs, all countries in the region reported having shortages of medical kidney-care professionals. In the US, a perennial ∼10% deficit of HD nurses occurs,39 with nearly 2000 open positions. Not only was this deficit worsened by the COVID-19 pandemic, but more strikingly, the nurse workforce is aging, and among new nurses, the levels of job turnover and dissatisfaction are high.39 This situation likely feeds the interregional “brain drain” phenomenon, of which the Caribbean has a long history. Nearly 1 in 5 specialized nurses were emigrating from Jamaica, even prior to the pandemic.40 Registered nurses are enticed by recruiters to migrate and are offered employment packages that Caribbean employers cannot match. The days of being bonded to a place of employment, based on receiving government scholarship and/or sponsorship, are dwindling, as nurses are able to pay back their bond with their newfound foreign salaries. At the moment, only one training institute in the Caribbean is dedicated to certifying nephrology nurses.41 The program was launched in 2007, through the Ministry of Health & Wellness In-Service Department in Jamaica; a registered nurse there completes a 9-month didactic and clinical rotation in all areas of nephrology. After acquiring some experience, nurses have sought employment in North America or in another island jurisdiction that offers comparable, if not better, salary compensation than that in the US and Canada. A 3-semester dialysis technician program at the University of Technology, Jamaica that trained technicians has been closed for a few years. Therefore, interested persons from Jamaica and the Turks & Caicos Islands must complete a dialysis technician program in Texas in the US to meet their local accreditation process. No specialty-trained dietitians, clinical pharmacists, or social workers are dedicated to solely kidney care in the Caribbean. Unlike Canada and the US, which typically attract physicians from across the world, the Caribbean countries struggle to retain physicians. In 2019, the Pan American Health Organization (PAHO) highlighted that poor working conditions, low wages, lack of promotions, and poor healthcare infrastructure contributed to this issue.42 A concerted effort was made to increase the number of employment posts for doctors, as many hospitals in the rural areas became accredited to provide internship opportunities. Over time, an increasing number of medical graduates could not obtain local postgraduate training, owing to a lack of such positions. Consequently, an increasing number of doctors undertake completion of an overseas medical licensing examination to enter their system as specialists. In addition to nephrologist shortages, only one fellowship-trained nephropathologist is available in the Caribbean (Jamaica), where samples for electron microscopy are shipped to Canada for analysis. The Caribbean also has a general lack of transplant surgeons, with those involved having trained overseas, where they often decide to remain. A transplant surgical fellow is currently training in the US and plans to return to Jamaica. Urgent innovative solutions to retain nephrologists and nurses,43 such as reverse aid from recruiting countries or in-country time commitments, are needed to improve the access to and quality of care in the Caribbean countries.40,44
Although kidney failure is seen as a health priority in most countries in the ISN NAC region, formal health policies and advocacy groups targeting prevention and progression are both lacking in the region. With the advent of new treatments, such as sodium-glucose transporter inhibitors, which are broadly available and significantly reduce the risk of progression among persons with CKD, resources intentionally spent on improving uptake and access to these and other preventive therapies should form the backbone of kidney care. In addition to advocacy groups, networks of patients, scientists, and healthcare professionals, such as the Canadian Can-SOLVE-CKD initiative (Canadians Seeking Solutions and Innovations to Overcome Chronic Kidney Disease), work toward the creation of innovative kidney-care solutions with patients at the center.45 Such initiatives are important for engagement of people with kidney failure and are a key avenue to improving kidney care.
In conclusion, this third iteration of the ISN-GKHA demonstrates that the ISN NAC region is among those that host the highest density of KRT programs in the world, and reasonably comprehensive CKD diagnostic and management capacity, compared with global programs, although heterogeneity exists, with significantly lower capacity in the Caribbean countries, compared to that in the US and Canada. Areas for improvement in kidney care, applicable across the region but to a varying degree, include programming to prioritize home-based modalities and transplantation as KRT, systems to train and retrain specialized nurses and physicians, and policies that funnel resources to CKD care and thereby invest in the most cost-efficient means to prevent kidney failure, rather than continually struggle to manage it. The 2023 ISN-GKHA had some limitations; these have been discussed.3 However, this work is important for guiding kidney-care policy in the ISN NAC region.
Funding Source
This article is published as part of a supplement sponsored by the International Society of Nephrology with grant funding to the University of Alberta (RES0033080).
Role of the Funder/Sponsor
The International Society of Nephrology provided administrative support for the design and implementation of the survey and data collection activities. The authors were responsible for data management, analysis, and interpretation, as well as manuscript preparation, review, and approval, and the decision to submit the manuscript for publication.
Disclosure
RLJ reports consultation fees from Ministry of Health & Wellness (Jamaica) Hypertension Guideline Development Group; honoraria from AstraZeneca and Cari-Med, outside the submitted work. IE reports grants from Fonds de Recherche du Québec—Santé, outside the submitted work. SND reports research funding from Canadian Institutes of Health Research, Alberta Innovates, and Alberta Health services, outside the submitted work. LF reports personal fees (speaking) from Dr. Reddy's Pharamaceutical and Servier Latin America and the Caribbean, outside the submitted work. ST reports fellowship grants from the International Society of Nephrology-Salmasi Family and the Kidney Foundation of Thailand, outside the submitted work. MMYW reports grants from Michael Smith Health Research BC and Kidney Foundation of Canada; personal fees from George Clinical, Bayer, and AstraZeneca advisory board: CKD early identification and intervention in primary care, outside the submitted work. SA reports personal fees (salary) from The International Society of Nephrology (ISN), outside the submitted work. AKB reports other (consultancy and honoraria) from AMGEN Incorporated and Otsuka; other (consultancy) from Bayer and GSK; and grants from Canadian Institutes of Health Research and Heart and Stroke Foundation of Canada, outside the submitted work; and serving as Associate Editor of the Canadian Journal of Kidney Health and Disease and Co-chair of the ISN-Global Kidney Health Atlas. SD reports personal fees (salary) from ISN, outside the submitted work. JD reports personal fees (salary) from ISN, outside the submitted work. VJ reports personal fees from GSK, AstraZeneca, Baxter Healthcare, Visterra, Biocryst, Chinook, Vera, and Bayer, paid to his institution, outside the submitted work. DWJ reports consultancy fees, research grants, speaker honoraria and travel sponsorships from Baxter Healthcare and Fresenius Medical Care; consultancy fees from AstraZeneca, Bayer, and AWAK; speaker honoraria from ONO and Boehringer Ingelheim & Lilly; travel sponsorships from ONO and Amgen, outside the submitted work; and being a current recipient of an Australian National Health and Medical Research Council Leadership Investigator Grant, outside the submitted work. CM reports personal fees (salary) from the ISN, outside the submitted work. MN reports grants and personal fees from KyowaKirin, Boehringer Ingelheim, Chugai, Daiichi Sankyo, Torii, JT, and Mitsubishi Tanabe; grants from Takeda and Bayer; and personal fees from Astellas, Akebia, AstraZeneca, and GSK, outside the submitted work. SA reports grants from Doris Duke Award and Stanford Center for Innovation in Global Health, during the conduct of the study; personal fees from HealthPals, Inc, and Vera Therapeutics, outside the submitted work. All the other authors declared no competing interests.
Acknowledgments
The authors appreciate the support from the International Society of Nephrology's (ISN’s) Executive Committee, regional leadership, and Affiliated Society leaders at the regional and country levels for their help with the ISN–Global Kidney Health Atlas.
Footnotes
Supplementary Table S1. Burden of chronic kidney disease (CKD) in the International Society of Nephrology (ISN) North America and the Caribbean region.
Supplementary Table S2. Risk factors for chronic kidney disease (CKD) in the International Society of Nephrology (ISN) North America and the Caribbean region.
Supplementary Figure S1. Quality of dialysis and transplantation: (A) proportion of centers routinely measuring and reporting outcomes and (B) proportion of people initiating dialysis with an incremental start, in the International Society of Nephrology (ISN) North America and the Caribbean region.
Supplementary Figure S2. Within-country variation in the organization, delivery, and cost of kidney-failure care and access to kidney replacement therapy (KRT) in the International Society of Nephrology (ISN) North America and the Caribbean region.
Supplementary Figure S3. Availability of services for chronic kidney disease (CKD) monitoring and management (proportion of countries) at the primary and secondary and/or tertiary care level in the International Society of Nephrology (ISN) North America and the Caribbean region.
Supplementary Figure S4. Proportion of death and hospitalization in people living with kidney failure on dialysis in the first year of dialysis, globally and in the International Society of Nephrology (ISN) North America and the Caribbean region.
Supplementary Figure S5. Availability and basis of participation of “official” registries for conditions and treatments (proportion of countries) in the International Society of Nephrology (ISN) North America and the Caribbean region.
Supplementary Figure S6. Proportion of countries in which kidney disease is recognized as a health priority by the government in the International Society of Nephrology (ISN) North America and the Caribbean region.
Contributor Information
Racquel Lowe-Jones, Email: racquel.lowejones@gmail.com.
Isabelle Ethier, Email: iethier@hotmail.com.
Regional Board and ISN-GKHA Team Authors:
Anil K. Agarwal, Atefeh Amouzegar, Carmen Avila-Casado, Everard N. Barton, Suman Behera, Melvin Bonilla Felix, Jorge Cerda, Yeoungjee Cho, Andrey V. Cybulsky, M. Razeen Davids, María Esther Diaz-González de Ferris, Hassane M. Diongole, Smita Divyaveer, Udeme E. Ekrikpo, Agnes B. Fogo, David Friedman, Winston Wing-Shing Fung, Susan L. Furth, John Gill, Ghenette Houston, Li-Li Hsiao, Chi-yuan Hsu, Htay Htay, Kwaifa Salihu Ibrahim, Georgina Irish, Sabine Karam, Dearbhla M. Kelly, Rowena Lalji, Edgar V. Lerma, Fabrice Mac-Way, Etienne Macedo, Hassina Mohammed, Devika Nair, Aisha M. Nalado, Brendon L. Neuen, Timothy O. Olanrewaju, Xavier Fernanco Vela Parada, Roberto Pecoits-Filho, Anna Petrova, Bhanu Prasad, Lisa Radix, Rupesh Raina, Avinash Rao Ullur, Mitchell H. Rosner, Aminu Muhammad Sakajiki, Emily See, Surya V. Seshan, Isaac Teitelbaum, Ian Thomas, Sophanny Tiv, Michele Trask, Tushar J. Vachharajani, Andrea Viecelli, Marina Wainstein, Michael Walsh, Christina Wyatt, Karen Yeates, Emily K. Yeung, Sandrica Young-Peart, and Deenaz Zaidi
Appendix
Regional Board and GKHA Team Authors
Anil K. Agarwal: Department of Medicine, VA Central California Health Care System, Fresno, California, USA; Department of Medicine, University of California, San Francisco Fresno, California, USA
Atefeh Amouzegar: Division of Nephrology, Department of Medicine, Firoozgar Clinical Research Development Center, Iran University of Medical Sciences, Tehran, Iran
Carmen Avila-Casado: Department of Laboratory Medicine & Pathology, University Health Network, University of Toronto, Toronto, Ontario, Canada
Everard N. Barton: Department of Medicine, University of the West Indies, Mona, Kingston, Jamaica
Suman Behera: Division of Nephrology, William Osler Health System, Ontario, Canada; Department of Medicine, Faculty of Health Sciences, McMaster University, Hamilton, Ontario, Canada
Melvin Bonilla Felix: Division of Pediatric Nephrology, Department of Pediatrics, University of Puerto Rico—Medical Sciences Campus, San Juan, Puerto Rico
Jorge Cerda: Division of Nephrology, Department of Medicine, Albany Medical College, Albany, New York, USA
Yeoungjee Cho: Department of Kidney and Transplant Services, Princess Alexandra Hospital, Brisbane, Queensland, Australia; Australasian Kidney Trials Network at the University of Queensland, Brisbane, Queensland, Australia
Andrey V. Cybulsky: Division of Nephrology, Department of Medicine, McGill University Health Centre Research Institute, McGill University, Montreal, Quebec, Canada
M. Razeen Davids: Division of Nephrology, Department of Medicine, Stellenbosch University and Tygerberg Hospital, Cape Town, South Africa
María Esther Diaz-González de Ferris: Department of Pediatrics, The University of North Carolina at Chapel Hill, Chapel Hill, North Carolina, USA
Hassane M. Diongole: Division of Nephrology, Department of Medicine, National Hospital Zinder, Zinder, Niger; Faculty of Health Sciences, University of Zinder, Zinder, Niger
Smita Divyaveer: Department of Nephrology, Postgraduate Institute of Medical Education and Research, Chandigarh, India
Udeme E. Ekrikpo: Department of Internal Medicine, University of Uyo/University of Uyo Teaching Hospital, Uyo, Nigeria
Agnes B. Fogo: Department of Pathology, Microbiology and Immunology, Vanderbilt University Medical Center, Nashville, Tennessee, USA
David Friedman: Division of Nephrology, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, Massachusetts, USA
Winston Wing-Shing Fung: Department of Medicine & Therapeutics, Prince of Wales Hospital, The Chinese University of Hong Kong, Hong Kong SAR, China
Susan L. Furth: Division of Nephrology, Department of Pediatrics, Children’s Hospital of Philadelphia, Perelman School of Medicine at the University of Pennsylvania, Philadelphia, Pennsylvania, USA
John Gill: Division of Nephrology, Department of Medicine, University of British Columbia, Vancouver, British Columbia, Canada
Ghenette Houston: Division of Nephrology and Immunology, Faculty of Medicine and Dentistry, University of Alberta, Edmonton, Alberta, Canada
Li-Li Hsiao: Renal Division, Department of Medicine, Brigham and Women’s Hospital, Harvard Medical School, Boston, Massachusetts, USA
Chi-yuan Hsu: Division of Nephrology, University of California, San Francisco, California, USA
Htay Htay: Department of Renal Medicine, Singapore General Hospital, Singapore, Singapore; Duke-NUS Medical School, Singapore, Singapore
Kwaifa Salihu Ibrahim: Nephrology Unit, Department of Medicine, Wuse District Hospital, Abuja, Nigeria; Department of Internal Medicine, College of Health Sciences, Nile University, Federal Capital Territory, Abuja, Nigeria
Georgina Irish: Australia and New Zealand Dialysis and Transplant (ANZDATA) Registry, South Australia Health and Medical Research Institute, Adelaide, South Australia, Australia; Faculty of Health and Medical Sciences, University of Adelaide, Adelaide, South Australia, Australia; Central and Northern Adelaide Renal and Transplantation Service, Royal Adelaide Hospital, South Australia Health, Adelaide, South Australia, Australia
Sabine Karam: Division of Nephrology and Hypertension, Department of Medicine, University of Minnesota, Minneapolis, Minnesota, USA; Division of Nephrology and Hypertension, Department of Internal Medicine, American University of Beirut, Beirut, Lebanon
Dearbhla M. Kelly: Wolfson Centre for the Prevention of Stroke and Dementia, University of Oxford, John Radcliffe Hospital, Oxford, UK; Department of Intensive Care Medicine, John Radcliffe Hospital, Oxford, UK
Rowena Lalji: Centre for Kidney Disease Research, University of Queensland, Brisbane, Queensland, Australia; Department of Nephrology, Queensland Children's Hospital, Brisbane, Queensland, Australia; Metro South and Integrated Nephrology and Transplant Services (MINTS), Princess Alexandra Hospital, Brisbane, Queensland, Australia
Edgar V. Lerma: Section of Nephrology, University of Illinois at Chicago, Chicago, Illinois USA; Section of Nephrology, Advocate Christ Medical Center, Oak Lawn, Illinois, USA
Fabrice Mac-Way: CHU de Québec Research Center, Hôtel-Dieu de Québec Hospital, Québec City, Québec, Canada; Division of Nephrology, Faculty and Department of Medicine, Université Laval, Québec City, Québec, Canada
Etienne Macedo: University of California San Diego, San Diego, California, USA
Hassina Mohammed: Department of Anaesthesia and Intensive Care, Eric Williams Medical Sciences Complex, Champs Fleurs, Trinidad and Tobago
Devika Nair: Division of Nephrology and Hypertension, Department of Medicine, Vanderbilt University Medical Center, Nashville, Tennessee, USA
Aisha M. Nalado: Department of Medicine, Bayero University Kano, Kano, Nigeria
Brendon L. Neuen: Kidney Trials Unit, Royal North Shore Hospital, Sydney, New South Wales, Australia; The George Institute for Global Health, Sydney, New South Wales, Australia
Timothy O. Olanrewaju: Division of Nephrology, Department of Medicine, College of Health Sciences, University of Ilorin, Ilorin, Nigeria; Julius Global Health, Julius Center for Health Sciences and Primary Care, University Medical Center Utrecht, Utrecht University, Utrecht, The Netherlands
Xavier Fernanco Vela Parada: Department of Medicine, Berkshire Medical Center, Pittsfield, Massachusetts, USA
Roberto Pecoits-Filho: School of Medicine, Pontificia Universidade Catolica do Paraná, Curitiba, Brazil; Arbor Research Collaborative for Health, Ann Arbor, Michigan, USA
Anna Petrova: Department of Propaedeutics of Internal Medicine, Bogomolets National Medical University, Kyiv, Ukraine; Department of Nephrology,"Diavita Institute," Kyiv, Ukraine
Bhanu Prasad: Section of Nephrology, Department of Medicine, University of Saskatchewan, Saskatoon, Saskatchewan, Canada; Section of Nephrology, Department of Medicine, Regina General Hospital, Saskatchewan Health Authority, Regina, Saskatchewan, Canada
Lisa Radix: Universal Health and Wellness Foundation, Memphis, Tennessee, USA
Rupesh Raina: Akron Nephrology Associates/Cleveland Clinic Akron General Medical Center, Akron, Ohio, USA; Department of Nephrology, Akron Children’s Hospital, Akron, Ohio, USA
Avinash Rao Ullur: Nephrology Division, Department of Medicine, The University of Toronto, Toronto, Ontario, Canada
Mitchell H. Rosner: Department of Medicine, University of Virginia Health, Charlottesville, Virginia, USA
Aminu Muhammad Sakajiki: Department of Medicine, Usmanu Danfodiyo University and Usmanu Danfodiyo University Teaching Hospital, Sokoto, Nigeria
Emily See: Department of Nephrology, Royal Melbourne Hospital, Parkville, VIC, Australia; Department of Nephrology, Royal Children's Hospital, Parkville, VIC, Australia; Department of Critical Care, University of Melbourne, Melbourne, Victoria, Australia
Surya V. Seshan: Department of Pathology and Laboratory Medicine, Weill Cornell Medicine, Cornell University, New York, New York, USA
Isaac Teitelbaum: Division of Kidney Diseases and Hypertension, Department of Medicine, University of Colorado School of Medicine, Aurora, Colorado, USA
Ian Thomas: Medical Subspecialties Division, Sir Lester Bird Medical Centre, Michael’s Mount, St Johh’s, Antigua
Sophanny Tiv: Division of Nephrology and Immunology, Faculty of Medicine and Dentistry, University of Alberta, Edmonton, Alberta, Canada
Michele Trask: School of Nursing, University of British Columbia, Vancouver, British Columbia, Canada; Vancouver Coastal Health, Vancouver, British Columbia, Canada
Tushar J. Vachharajani: Department of Medicine, John D. Dingell Veterans Affairs Medical Center & Wayne State University School of Medicine, Detroit, Michigan, USA
Andrea Viecelli: Department of Kidney and Transplant Services, Division of Medicine, Princess Alexandra Hospital, Woolloongabba, Queensland, Australia; University of Queensland, Queensland, Australia; Australasian Kidney Trials Network at the University of Queensland, Brisbane, Queensland, Australia
Marina Wainstein: Faculty of Medicine, University of Queensland, Brisbane, Queensland, Australia; West Moreton Kidney Health Service, Ipswich Hospital, Brisbane, Queensland, Australia
Michael Walsh: Department of Medicine, McMaster University, Hamilton, Ontario, Canada; Department of Health Research Methods, Evidence & Impact, McMaster University, Hamilton, Ontario, Canada; and Population Health Research Institute, McMaster University/Hamilton Health Sciences, Hamilton, Ontario, Canada
Christina Wyatt: Division of Nephrology, Department of Medicine, Duke University School of Medicine, Durham, North Carolina, USA
Karen Yeates: Division of Nephrology, Department of Medicine, Queen's University, Kingston, Ontario, Canada
Emily K. Yeung: Department of Nephrology, Monash Health, Clayton, Victoria, Australia
Sandrica Young-Peart: Department of Paediatric Nephrology, Bustamante Hospital for Children, Kingston, Jamaica; Department of Child & Adolescent Medicine, University of the West Indies, Mona, Kingston, Jamaica
Deenaz Zaidi: Division of Nephrology and Immunology, Faculty of Medicine and Dentistry, University of Alberta, Edmonton, Alberta, Canada
Regional Board and ISN-GKHA Team Author disclosures
YC reports grants and other from Baxter Healthcare, outside the submitted work. MRD reports personal fees (consultancy) from National Renal Care, outside the submitted work; and serving as the Chair of the African Renal Registry and Co-chair of the South African Renal Registry. MBF reports personal fees (consulting) from Natera and Novartis; personal fees (speaker fees) from the Association of American Medical Colleges; and a leadership role as the President of the Latin American Association of Pediatric Nephrology, outside the submitted work. MDGDF reports personal fees from ProKidney; and grants from The Renal Research Institute, MONDO/Pediatric Investigation and Close Collaborative Consortium for Ongoing Life Outcomes for MONitoring Dialysis Outcomes (PICCOLO MONDO) Registries, outside the submitted work. DF reports grants or contracts from the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), Department of Defense, and Vertex, paid to his institution; royalties for patents related to APOL1 paid to his institution; consulting fees and payment for participation on the Data Safety Monitoring or Advisory Board from Vertex; payment and/or honoraria for lectures, presentations, or speaker bureaus from Sanofi Genzyme; and unpaid participation on the NIDDK Data Safety Monitoring or Advisory Board, outside the submitted work. CYH reports grants from Satellite Healthcare, royalties from UpToDate, consulting fees from Allen Shepherd & Lewis, King and Spalding, Triangle Insights Group, Lewis Brisbois, Aria Pharma, and McMasters Keith Butler; travel support from Satellite Healthcare, and participation on the LG Chem advisory board. HH reports personal fees from AWAK technology and Baxter Healthcare; and nonfinancial support from Mologic company, outside the submitted work. SK reports consulting fees for George Clinical, outside the submitted work. EVL reports royalties or licenses from Elsevier, McGraw-Hill, and Springer; consulting fees from AstraZeneca, Boehringer Ingelheim, GSK, Novartis, Calliditas, Otsuka, Travere, and Vifor; personal fees from AstraZeneca, Calliditas, Vifor, and GSK; and other financial or nonfinancial interests of joint venture with Fresenius (as partner of Associates in Nephrology, S.C.), outside the submitted work. EM reports grants from the National Institutes of Health (NIH), participation on the Data Safety Monitoring Board or Advisory Board for CKDu in Sri Lanka, outside the submitted work. BLN reports personal fees (advisory boards, speaker honoraria) from AstraZeneca and Boehringer and Ingelheim; personal fees (advisory boards) from Alexion, Bayer, and Cambridge Healthcare Research; and personal fees (speaker honoraria) from Cornerstone Medical Education, Medscape, and The Limbic, outside the submitted work, with all fees paid to The George Institute for Global Health. RPF reports grants from the National Council for Scientific and Technological Development and Fresenius Medical Care; consulting fees from Fresenius Medical Care, Bayer, AstraZeneca, Fibrigen, and Akebia, all paid to his employer; payment or honoraria for lectures, presentations, speaker bureaus, manuscript writing, or educational events from Fresenius Medical Care, Bayer, AstraZeneca, Novo Nordisk, Fibrigin, and Akebia, all paid to his employer; and has a leadership or fiduciary role with Kidney Disease: Improving Global Outcomes (KDIGO), the ISN and International Society of Peritoneal Dialysis (ISPD); and employment by Arbor Research Collaborative for Health, which runs the Dialysis Outcomes and Practice Patterns Study (DOPPS) programs (global support for the ongoing DOPPS Programs is provided without restriction by a variety of funders and is provided to Arbor Research Collaborative for Health and not to RPF). IT reports other (stock) from liberDi, outside the submitted work. MW reports grants from Canadian Institutes of Health Research, British Heart Foundation, Medical Research Future Fund, National Health and Medical Research Council, Health Research Council, Hamilton Academic Health Sciences Organization, and Vifor; other from Otsuka; nonfinancial support from Otsuka; other from Bayer, Pharmaceuticals, Novo Nordisk, Medical Research Council, Roche, and National Institutes of Health Research, outside the submitted work.
Supplementary Material
Supplementary Table S1. Burden of chronic kidney disease (CKD) in the International Society of Nephrology (ISN) North America and the Caribbean region.
Supplementary Table S2. Risk factors for chronic kidney disease (CKD) in the International Society of Nephrology (ISN) North America and the Caribbean region.
Supplementary Figure S1. Quality of dialysis and transplantation: (A) proportion of centers routinely measuring and reporting outcomes and (B) proportion of people initiating dialysis with an incremental start, in the International Society of Nephrology (ISN) North America and the Caribbean region.
Supplementary Figure S2. Within-country variation in the organization, delivery, and cost of kidney-failure care and access to kidney replacement therapy (KRT) in the International Society of Nephrology (ISN) North America and the Caribbean region.
Supplementary Figure S3. Availability of services for chronic kidney disease (CKD) monitoring and management (proportion of countries) at the primary and secondary and/or tertiary care level in the International Society of Nephrology (ISN) North America and the Caribbean region.
Supplementary Figure S4. Proportion of death and hospitalization in people living with kidney failure on dialysis in the first year of dialysis, globally and in the International Society of Nephrology (ISN) North America and the Caribbean region.
Supplementary Figure S5. Availability and basis of participation of “official” registries for conditions and treatments (proportion of countries) in the International Society of Nephrology (ISN) North America and the Caribbean region.
Supplementary Figure S6. Proportion of countries in which kidney disease is recognized as a health priority by the government in the International Society of Nephrology (ISN) North America and the Caribbean region.
References
- 1.Liyanage T., Ninomiya T., Jha V., et al. Worldwide access to treatment for end-stage kidney disease: a systematic review. Lancet. 2015;385:1975–1982. doi: 10.1016/S0140-6736(14)61601-9. [DOI] [PubMed] [Google Scholar]
- 2.Government of Canada Canada's health care system. https://www.canada.ca/en/health-canada/services/health-care-system/reports-publications/health-care-system/canada.html
- 3.Okpechi I.G., Bello A.K., Levin A., Johnson D.W. Update on variability in organization and structures of kidney care across world regions. Kidney Int Suppl. 2024;13:6–11. [Google Scholar]
- 4.The World Bank World development indicators. The world by income and region. https://datatopics.worldbank.org/world-development-indicators/the-world-by-income-and-region.html
- 5.US Central Intelligence Agency The world factbook. https://www.cia.gov/the-world-factbook/
- 6.Institute for Health Metrics and Evaluation Global Health Data Exchange Global expected health spending 2019–2050. https://ghdx.healthdata.org/record/ihme-data/global-expected-health-spending-2019-2050
- 7.Adomakoh S.A., Adi C.N., Fraser H.S., et al. Dialysis in Barbados: the cost of hemodialysis provision at the Queen Elizabeth Hospital. Rev Panam Salud Publica. 2004;16:350–355. doi: 10.1590/s1020-49892004001100009. [DOI] [PubMed] [Google Scholar]
- 8.Barnieh L., Yilmaz S., McLaughlin K., et al. The cost of kidney transplant over time. Prog Transplant. 2014;24:257–262. doi: 10.7182/pit2014710. [DOI] [PubMed] [Google Scholar]
- 9.Kramer H., Soyibo A., Forrester T., et al. The burden of chronic kidney disease and its major risk factors in Jamaica. Kidney Int. 2018;94:840–842. doi: 10.1016/j.kint.2018.07.025. [DOI] [PubMed] [Google Scholar]
- 10.van der Tol A., Lameire N., Morton R.L., et al. An international analysis of dialysis services reimbursement. Clin J Am Soc Nephrol. 2019;14:84–93. doi: 10.2215/CJN.08150718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wang J.H., Hart A. Global perspective on kidney transplantation: United States. Kidney360. 2021;2:1836–1839. doi: 10.34067/KID.0002472021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Canadian Organ Replacement Register (CORR) https://www.cihi.ca/en/canadian-organ-replacement-register-corr
- 13.Jain A.K., Blake P., Cordy P., et al. Global trends in rates of peritoneal dialysis. J Am Soc Nephrol. 2012;23:533–544. doi: 10.1681/ASN.2011060607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Soyibo A.K., Barton E.N. Vol. 56. West Indian Med J; 2007. pp. 355–363. (Report from the Caribbean renal registry, 2006). [PubMed] [Google Scholar]
- 15.United States Renal Data System . National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; Bethesda, MD: 2019. 2019 USRDS Annual Data Report.https://www.niddk.nih.gov/about-niddk/strategic-plans-reports/usrds/prior-data-reports/2019 [Google Scholar]
- 16.Institute for Health Metrics and Evaluation 2019 Global Burden of Disease study results. https://vizhub.healthdata.org/gbd-results/ [DOI] [PMC free article] [PubMed]
- 17.World Health Organization Global Health Observatory Health Workforce. https://www.who.int/data/gho/data/themes/health-workforce
- 18.World Health Organization The Global Health Observatory. https://www.who.int/data/gho
- 19.Roy D. How the Caribbean is building climate resilience. https://www.cfr.org/backgrounder/how-caribbean-building-climate-resilience
- 20.COVID-19 Excess Mortality Collaborators Estimating excess mortality due to the COVID-19 pandemic: a systematic analysis of COVID-19-related mortality, 2020-21. Lancet. 2022;399:1513–1536. doi: 10.1016/S0140-6736(21)02796-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Schwalb A., Armyra E., Méndez-Aranda M., et al. COVID-19 in Latin America and the Caribbean: two years of the pandemic. J Intern Med. 2022;292:409–427. doi: 10.1111/joim.13499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dember L.M., Lacson E., Jr., Brunelli S.M., et al. The TiME Trial: a fully embedded, cluster-randomized, pragmatic trial of hemodialysis session duration. J Am Soc Nephrol. 2019;30:890–903. doi: 10.1681/ASN.2018090945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.MyTEMP writing committee Personalised cooler dialysate for patients receiving maintenance haemodialysis (MyTEMP): a pragmatic, cluster-randomised trial. Lancet. 2022;400:1693–1703. doi: 10.1016/S0140-6736(22)01805-0. [DOI] [PubMed] [Google Scholar]
- 24.McCaw-Binns A.M., Moody C.O., Standard K.L. Forty years. An introduction to the development of a Caribbean public health. West Indian Med J. 1998;47(suppl 4):8–12. [PubMed] [Google Scholar]
- 25.Levin A., Tonelli M., Bonventre J., et al. Global kidney health 2017 and beyond: a roadmap for closing gaps in care, research, and policy. Lancet. 2017;390:1888–1917. doi: 10.1016/S0140-6736(17)30788-2. [DOI] [PubMed] [Google Scholar]
- 26.Teitelbaum I., Finkelstein F.O. Why are we not getting more patients onto peritoneal dialysis? Observations from the United States with global implications. Kidney Int Rep. 2023;8:1917–1923. doi: 10.1016/j.ekir.2023.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lin E., Ginsburg P.B., Chertow G.M., et al. The "Advancing American Kidney Health" Executive Order: challenges and opportunities for the large dialysis organizations. Am J Kidney Dis. 2020;76:731–734. doi: 10.1053/j.ajkd.2020.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Oliver M.J., Salenger P. Making assisted peritoneal dialysis a reality in the United States: a Canadian and American viewpoint. Clin J Am Soc Nephrol. 2020;15:566–568. doi: 10.2215/CJN.11800919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bamforth R.J., Beaudry A., Ferguson T.W., et al. Costs of assisted home dialysis: a single-payer Canadian model from Manitoba. Kidney Med. 2021;3:942–950.e1. doi: 10.1016/j.xkme.2021.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Garg A.X., Yohanna S., Naylor K.L., et al. Effect of a novel multicomponent intervention to improve patient access to kidney transplant and living kidney donation: the EnAKT LKD cluster randomized clinical trial. JAMA Intern Med. 2023;183:1366–1375. doi: 10.1001/jamainternmed.2023.5802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fisher L.A., Lowe-Jones R. Global dialysis perspective: Jamaica. Kidney360. 2023;4:1623–1627. doi: 10.34067/KID.0000000000000275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Campbell C. Living with end-stage renal (kidney) disease. https://nowgrenada.com/2019/02/dr-germain-bristol-stanisclaus-living-with-end-stage-renal-disease/
- 33.Brown E.A., Perl J. Increasing peritoneal dialysis use in response to the COVID-19 pandemic: Will it go viral? J Am Soc Nephrol. 2020;31:1928–1930. doi: 10.1681/ASN.2020050729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Albakr R., Bieber B., Aylward R., et al. An ISN-DOPPS survey of the global impact of the COVID-19 pandemic on peritoneal dialysis services. Kidney Int Rep. 2022;7:2196–2206. doi: 10.1016/j.ekir.2022.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yglesias-González M., Palmeiro-Silva Y., Sergeeva M., et al. Code red for health response in Latin America and the Caribbean: enhancing peoples' health through climate action. Lancet Reg Health Am. 2022;11 doi: 10.1016/j.lana.2022.100248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Avilés Mendoza G.J., Finne K.P., Torre Leon F., et al. Observations from the emergency management of dialysis patients evacuated from the US Virgin Islands to Puerto Rico following hurricane Irma. BMC Health Serv Res. 2021;21:1239. doi: 10.1186/s12913-021-07194-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Elcock-Straker B., Manyalich Vidal M., Gomez M.P. Kidney donation and transplant outcomes in Trinidad and Tobago: a 15-year experience of the National Organ Transplant Unit. Exp Clin Transplant. 2022;20:649–656. doi: 10.6002/ect.2022.0163. [DOI] [PubMed] [Google Scholar]
- 38.Contento M.N., Vercillo R.N., Malaga-Dieguez L., et al. Center volume and kidney transplant outcomes in pediatric patients. Kidney Med. 2020;2:297–306. doi: 10.1016/j.xkme.2020.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Boyle S.M., Washington R., McCann P., et al. The nephrology nursing shortage: insights from a pandemic. Am J Kidney Dis. 2022;79:113–116. doi: 10.1053/j.ajkd.2021.07.007. [DOI] [PubMed] [Google Scholar]
- 40.Lofters A.K. The "brain drain" of health care workers: causes, solutions and the example of Jamaica. Can J Public Health. 2012;103:e376–e378. doi: 10.1007/BF03404445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Jamaica Information Service Health Ministry launches nephrology training programme for nurses. https://jis.gov.jm/health-ministry-launches-nephrology-training-programme-for-nurses/
- 42.Pan American Health Organization, World Health Organization Health workers perception and migration in the Caribbean region. https://www.paho.org/en/documents/health-workers-perception-and-migration-caribbean-region
- 43.International Society of Nephrology The post-SARS-CoV-2 pandemic global nephrology nursing workforce. https://www.theisn.org/blog/2023/05/08/the-world-is-a-very-different-place-for-nephrology-nurses-the-isn-kidney-health-professionals-working-group-on-post-global-pandemic-working-conditions-for-nurses/
- 44.Kollar E., Buyx A. Ethics and policy of medical brain drain: a review. Swiss Med Wkly. 2013;143 doi: 10.4414/smw.2013.13845. [DOI] [PubMed] [Google Scholar]
- 45.Can-SOLVE CKD Network Impact Report. https://cansolveckd.ca/
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.