Abstract
The burden of chronic kidney disease and associated risk of kidney failure are increasing in Africa. The management of people with chronic kidney disease is fraught with numerous challenges because of limitations in health systems and infrastructures for care delivery. From the third iteration of the International Society of Nephrology Global Kidney Health Atlas, we describe the status of kidney care in the ISN Africa region using the World Health Organization building blocks for health systems. We identified limited government health spending, which in turn led to increased out-of-pocket costs for people with kidney disease at the point of service delivery. The health care workforce across Africa was suboptimal and further challenged by the exodus of trained health care workers out of the continent. Medical products, technologies, and services for the management of people with nondialysis chronic kidney disease and for kidney replacement therapy were scarce due to limitations in health infrastructure, which was inequitably distributed. There were few kidney registries and advocacy groups championing kidney disease management in Africa compared with the rest of the world. Strategies for ensuring improved kidney care in Africa include focusing on chronic kidney disease prevention and early detection, improving the effectiveness of the available health care workforce (e.g., multidisciplinary teams, task substitution, and telemedicine), augmenting kidney care financing, providing quality, up-to-date health information data, and improving the accessibility, affordability, and delivery of quality treatment (kidney replacement therapy or conservative kidney management) for all people living with kidney failure.
Keywords: Africa, chronic kidney disease, kidney failure, kidney replacement therapy, nephrology workforce, out-of-pocket spending
There is a high burden of chronic kidney disease (CKD) in Africa1 despite efforts to increase capacity for kidney care with clear roadmaps.2 The burden from the major causes of CKD continues to increase, including hypertension, diabetes mellitus, chronic glomerulonephritis, genetic conditions (such as sickle cell disease, autosomal dominant polycystic kidney disease, and Apolipoprotein L1 risk alleles), and infections (such as HIV, chronic schistosomiasis, and hepatitis B and C).3, 4, 5 Lack of awareness about kidney disease, abuse of traditional herbal and pain medications, and lower socioeconomic status have also contributed to the growing burden of kidney disease in Africa.6 This has been further compounded by limitations in the various health systems and the infrastructures for care delivery in most parts of Africa,7 a spike in acute kidney injury (AKI), and disruption of routine medical care associated with the recent COVID-19 pandemic.8
Low health expenditure in most African countries has had a crippling effect on kidney care as a “neglected” noncommunicable disease.9 Kidney replacement therapy (KRT) (hemodialysis [HD], peritoneal dialysis [PD], and kidney transplantation) is neither readily available nor affordable in most parts of Africa. This leads to excessive premature and preventable mortality.10 Given the limited capacity for African countries to deliver optimum kidney care, there is a pressing need for early identification and prevention strategies supported by government, nongovernmental organizations, and community initiatives.11,12 The devastating effects of the financially driven “brain drain” phenomenon among health care workers on health service delivery across Africa continue to affect the delivery of optimum kidney care.13
The International Society of Nephrology-Global Kidney Health Atlas (ISN-GKHA) is in its third global iteration and second Africa-specific report. In this second Africa-specific report, we aim to understand and update the status of the regional capacity for kidney health care delivery in Africa. This will be described using the building blocks for health services as defined by the World Health Organization. The methodology for this study is described in detail elsewhere.14
Results
The ISN-GKHA results are broadly categorized as literature review (Table 1,15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34 Table 2,35, 36, 37, 38, 39 and Supplementary Table S140) and survey response (Figure 1, Figure 2, Figure 3, Figure 4, Figure 5 and Supplementary Figures S1–S4).
Table 1.
Demographics, health expenditure, and cost of kidney replacement therapy in the ISN African region15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34
| Country | World Bank income level | Area (km2) | Total population | Prevalence of CKD % (95% CI) | DALYs to CKD per 100,000 rate (95% CI) | Death attributable to CKD % (95% CI) | GDP (PPP), ($ billion) | Govt spending per person (US$ 2021) (95% CI) | Total health expenditures (% of GDP) | Annual cost KRT (US$) and out-of-pocket/% paid by patient from total cost (2021) |
||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| HD | PD | KT (first year) | ||||||||||
| Global | – | 130,483,015 | 7,802,702,984 | 9.5 [5.9–11.7]a | 491.4 [359.9–636.0]a | 2.4 [1.6–3.9]a | 133.8a | – | 6.2a | 19,380.30a | 18,959.20a | 26,903.20a |
| Africa | – | 28,606,970 | 1,386,928,000 | 4.2 [3.5–5.2]a | 464.4 [389.9–528.5]a | 1.8 [1.4–2.3]a | 47.4a | – | 4.6a | 13,792.50a | 14,191.60a | 20,713.90a |
| Algeria | LMIC | 2,381,741 | 44,178,884 | 9.5 (8.9–10.2) | 560.9 (453.1–712.2) | 4.1 (3.4–5.2) | 535.8 | 142 (126–159) | 6.2 | 10,115/– | – | – |
| Angola | LMIC | 1,246,700 | 34,795,287 | 3.4 (3.1–3.7) | 325.4 (236.3–407.2) | 1.3 (1.0–1.5) | 224.0 | 24 (20–29) | 2.5 | –/0% | – | – |
| Benin | LMIC | 112,622 | 13,754,688 | 3.8 (3.5–4.1) | 483.8 (355.5–643.4) | 1.7 (1.4–2.0) | 47.4 | 7 (5–8) | 2.4 | –/0% | – | – |
| Botswana | UMIC | 581,730 | 2,384,246 | 6.1 (5.6–6.6) | 651.1 (460.3–878.3) | 2.1 (1.6–2.7) | 42.2 | 353 (326–379) | 6.1 | –/1%–25% | –/1%–25% | –/1%–25% |
| Burkina Faso | LIC | 274,200 | 21,935,389 | 3.6 (3.4–3.9) | 511.8 (403.1–634.0) | 1.4 (1.2–1.6) | 52.9 | 17 (1–20) | 5.5 | 1646/1%–25% | – | –/100% |
| Burundi | LIC | 27,830 | 12,696,478 | 3.2 (2.9–3.5) | 332.6 (258.6–420.6) | 1.3 (1.1–1.5) | 9.7 | 6 (5–7) | 8.0 | 13,793/1%–25% | – | – |
| Cabo Verde | LMIC | 4033 | 596,707 | 6.4 (5.9–6.8) | 476.7 (411.9–544.0) | 3.0 (2.7–3.3) | 3.9 | 138 (126–152) | 4.9 | –/0% | – | – |
| Cameroon | LMIC | 475,440 | 29,321,637 | 4.7 (4.4–5.0) | 636.0 (468.1–835.8) | 2.3 (1.9–2.8) | 110.6 | 3 (2–3) | 3.6 | 1724/1%–25% | – | – |
| Chad | LIC | 1,284,000 | 17,963,211 | 3.2 (2.9–3.4) | 445.1 (338.0–585.7) | 1.2 (0.9–1.5) | 26.9 | 6 (5–7) | 4.4 | – | – | –/100% |
| Congo, Democratic Republic | LIC | 2,344,858 | 108,407,721 | 3.5 (3.2–3.8) | 341.5 (271.8–421.8) | 1.4 (1.2–1.6) | 113.1 | 3 (2–3) | 3.5 | 32,538/100% | 45,571/100% | – |
| Congo, Republic | LMIC | 342,000 | 5,546,307 | 4.4 (4.0–4.7) | 456.6 (321.6–602.9) | 2.0 (1.4–2.4) | 20.7 | 19 (16–23) | 2.1 | –/>75% | –/100% | – |
| Cote d'Ivoire | LMIC | 322,463 | 28,713,423 | 4.2 (3.9–4.6) | 518.5 (385.9–661.9) | 1.9 (1.5–2.3) | 160.7 | 21 (18–24) | 3.3 | –/1%–25% | – | – |
| Djibouti | LMIC | 23,200 | 957,273 | 4.5 (4.1–4.9) | 412.8 (304.9–553.5) | 1.8 (1.5–2.1) | 6.0 | 28 (24–34) | 1.8 | – | – | – |
| Egypt | LMIC | 1,001,450 | 107,770,524 | 8.0 (7.4–8.6) | 662.4 (432.0–908.2) | 3.9 (2.5–5.3) | 1388.3 | 43 (39–48) | 4.7 | 2707/0% | 2772/– | 8318/1%–25% |
| Eritrea | LIC | 117,600 | 6,209,262 | 3.6 (3.3–3.9) | 389.8 (274.1–537.9) | 1.5 (1.1–1.9) | – | 3 (2–3) | 4.5 | – | – | – |
| Ethiopia | LIC | 1,104,300 | 113,656,596 | 3.3 (3.1–3.6) | 306.4 (268.8–349.6) | 1.8 (1.5–2.0) | 306.4 | 6 (5–7) | 3.2 | 4737/– | – | –/100% |
| Gabon | UMIC | 267,667 | 2,340,613 | 5.1 (4.7–5.5) | 628.4 (426.1–816.9) | 3.1 (2.1–3.9) | 35.5 | 158 (143–172) | 2.8 | –/1%–25% | – | – |
| Gambia | LIC | 11,300 | 2,413,403 | 4.1 (3.8–4.4) | 464.4 (358.1–592.4) | 2.3 (1.9–2.7) | 6.0 | 9 (7–10) | 3.8 | – | – | – |
| Ghana | LMIC | 238,533 | 33,107,275 | 4.6 (4.3–5.0) | 526.0 (391.0–661.3) | 2.3 (1.7–2.7) | 196.1 | 35 (29–43) | 3.4 | –/100% | – | 18,614/100% |
| Guinea | LIC | 245,857 | 13,237,832 | 3.8 (3.6–4.1) | 562.5 (437.0–718.7) | 1.7 (1.5–2.0) | 39.3 | 7 (6–8) | 4.0 | –/1%–25% | – | – |
| Kenya | LMIC | 580,367 | 55,864,655 | 3.8 (3.5–4.1) | 324.1 (274.0–380.5) | 1.6 (1.4–1.9) | 276.2 | 41 (37–45) | 4.6 | 20,254/26%–50% | 15,190/26%–50% | –/26%–50% |
| Liberia | LIC | 111,369 | 5,358,483 | 4.2 (3.9–4.5) | 488.9 (356.3–669.7) | 2.2 (1.7–2.9) | 8.1 | 9 (7–11) | 8.5 | – | – | – |
| Libya | UMIC | 1,759,540 | 7,137,931 | 9.4 (8.7–10.0) | 602.4 (443.2–774.2) | 4.3 (3.0–5.7) | 162.5 | 580 (462–711) | – | – | – | – |
| Madagascar | LIC | 587,041 | 28,172,462 | 3.5 (3.2–3.8) | 287.9 (228.6–362.7) | 1.2 (1.0–1.4) | 46.5 | 10 (8–13) | 3.7 | –/100% | – | – |
| Malawi | LIC | 118,484 | 20,794,353 | 5.3 (4.1–7.3) | 354.8 (290.6–429.0) | 1.5 (1.3–1.7) | 32.6 | 12 (10–14) | 7.4 | –/1%–25% | – | – |
| Mali | LIC | 1,240,192 | 20,741,769 | 3.5 (3.2–3.8) | 490.3 (370.7–639.2) | 1.3 (1.1–1.6) | 51.0 | 10 (9–12) | 3.9 | –/1%–25% | – | – |
| Mauritania | LMIC | 1,030,700 | 4,161,925 | 4.7 (4.4–5.1) | 454.7 (334.3–597.0) | 2.8 (2.2–3.4) | 26.9 | 23 (21-25) | 3.3 | –/1%–25% | – | – |
| Mauritius | – | – | – | 18.1 (16.8–19.4) | 2717.3 (2239.9–3272.0) | 11.8 (10.9–12.5) | – | – | – | –/0% | –/0% | –/0% |
| Morocco | LMIC | 446,550 | 36,738,229 | 9.6 (9.0–10.3) | 724.1 (574.2–881.4) | 4.1 (3.4–5.0) | 333.2 | 81 (73–89) | 5.3 | 13,901/26%–50% | 7503/1%–25% | 91,760/1%–25% |
| Mozambique | LIC | 799,380 | 31,693,239 | 3.3 (3.0–3.6) | 357.8 (279.4–441.0) | 1.0 (0.9–1.2) | 43.2 | 7 (6–9) | 7.8 | –/1%–25% | – | – |
| Namibia | UMIC | 824,292 | 2,727,409 | 5.2 (4.9–5.6) | 431.9 (311.5–583.4) | 1.9 (1.5–2.5) | 25.4 | 181 (162–201) | 8.5 | 31,014/1%–25% | 31,014/0% | –/1%–25% |
| Niger | LIC | 1,267,000 | 24,484,587 | 3.5 (3.2–3.8) | 408.2 (303.5–542.0) | 1.1 (0.9–1.3) | 32.9 | 9 (8–10) | 5.7 | –/100% | – | – |
| Nigeria | LMIC | 923,768 | 225,082,083 | 3.9 (3.6–4.2) | 357.4 (284.3–447.5) | 1.3 (1.0–1.5) | 1154.1 | 11 (9–14) | 3.0 | 23,576/100% | 29,830/– | 38,046/100% |
| Rwanda | LIC | 26,338 | 13,173,730 | 3.9 (3.5–4.2) | 348.0 (277.0–428.6) | 1.9 (1.5–2.1) | 33.1 | 18 (15–22) | 6.4 | – | – | – |
| Senegal | LMIC | 196,722 | 17,923,036 | 4.2 (3.9–4.5) | 528.5 (392.3–696.8) | 2.7 (2.2–3.4) | 64.8 | 17 (14–21) | 4.1 | 11,818/1%–25% | 13,826/1%–25% | – |
| Sierra Leone | LIC | 71,740 | 8,692,606 | 4.1 (3.8–4.4) | 490.3 (366.8–642.9) | 1.5 (1.2–1.8) | 14.9 | 9 (7–11) | 8.8 | – | – | – |
| Somalia | LIC | 637,657 | 12,386,248 | 3.0 (2.8–3.3) | 392.3 (304.6–503.6) | 1.0 (0.9–1.2) | 21.3 | 2 (1–2) | – | – | – | – |
| South Africa | UMIC | 1,219,090 | 57,516,665 | 7.3 (6.7–7.8) | 659.2 (606.8–714.6) | 2.4 (2.2–2.5) | 868.6 | 270 (245–297) | 9.1 | 15,154/100% | 8068/0% | 27,619/0% |
| Sudan | LIC | 1,861,484 | 47,958,856 | 5.6 (5.2–6.0) | 406.4 (299.7–557.8) | 2.4 (1.7–3.5) | 185.6 | 9 (7–10) | 4.6 | 4185/1%–25% | 14,557/1%–25% | 18,269/0% |
| Swaziland | LMIC | 17,364 | 1,121,761 | 5.4 (5.0–5.9) | 818.5 (580–1068.4) | 2.3 (1.9–2.7) | – | 97 (90–106) | 6.8 | –/1%–25% | –/0% | –/0% |
| Tanzania | LMIC | 947,300 | 63,852,892 | 3.6 (3.3–3.9) | 390.5 (322.6–469.3) | 1.8 (1.6–2.0) | 175.0 | 16 (13–19) | 3.8 | 31,571/>75% | – | –/>75% |
| Togo | LIC | 56,785 | 8,492,333 | 4.3 (4.0–4.6) | 479.6 (372.2–601.9) | 1.9 (1.6–2.2) | 20.2 | 9 (7–11) | 5.7 | –/51%–75% | – | –/>75% |
| Tunisia | LMIC | 163,610 | 11,896,972 | 11.8 (11.1–12.5) | 594.6 (461.0–754.8) | 3.9 (3.2–4.6) | 138.4 | 163 (147–179) | 7.0 | 6609/1%–25% | 6101/1%–25% | 20,714/1%–25% |
| Uganda | LIC | 241,038 | 46,205,893 | 3.0 (2.7–3.3) | 303.4 (232.3–381.3) | 1.4 (1.1–1.7) | 113.2 | 8 (7–10) | 3.8 | –/1%–25% | – | –/0% |
| Zambia | LIC | 752,618 | 19,642,123 | 3.5 (3.2–3.8) | 416.9 (334.5–511.9) | 1.6 (1.3–1.8) | 69.2 | 16 (13–21) | 5.3 | –/1%–25% | –/1%–25% | –/51%–75% |
| Zimbabwe | LMIC | 390,757 | 15,121,004 | 4.9 (4.5–5.3) | 520.1 (385.4–740.4) | 1.8 (1.4–2.5) | 37.2 | 13 (11–17) | 7.7 | 32,331/1%–25% | –/1%–25% | – |
–, data not reported or unavailable; CI, confidence interval; CKD, chronic kidney disease; DALY, disability-adjusted life year; GDP, gross domestic product; Govt, government; HD, hemodialysis; ISN, International Society of Nephrology; KRT, kidney replacement therapy; KT, kidney transplant; LIC, low-income country; LMIC, lower-middle-income country; PD, peritoneal dialysis; PPP, purchasing power parity; UMIC, upper-middle income country.
Data are presented as median [interquartile range].
Table 2.
Availability of kidney replacement therapy and workforce for kidney care in the ISN Africa region15,35, 36, 37, 38, 39
| Country | World Bank income level | Treated KF (PMP) | Prevalence of long-term dialysis |
Long-term dialysis centers (PMP)a |
Kidney transplantation (PMP) |
Nephrology workforcea |
Health care professional per 10,000 population |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| HD | PD | Total (HD + PD) | HD | PD | Incidence | Centersa | Nephrologist(PMP) | Nephrology trainees (PMP) | Female nephrologist (%) | Medical doctors | Specialist physicians | Nurse | |||
| Global | – | 822.8 | 322.7 | 21.0 | 396.6 | 5.1 | 1.6 | 12.2 | 0.5 | 11.8 | 1.2 | 35.0 | – | – | – |
| Africa | – | 541.0 | 12.2 | 0.2 | 15.4 | 0.8 | 0.1 | 2.1 | 0.1 | 1.1 | 0.2 | 25.0 | – | – | – |
| Algeria | LMIC | – | 240.3 | 11.1 | 251.4 | – | – | 2.1 | – | – | – | – | 17.2 | 17.2 | 15.5 |
| Angola | LMIC | – | 23.6 | 0.0 | 23.6 | 0.4 | 0.0 | – | – | 1.5 | 0.5 | 71.5 | 2.1 | 2.2 | 4.1 |
| Benin | LMIC | – | 30.2 | 0.0 | 30.2 | 0.3 | – | – | – | 1.1 | 0.0 | 20.0 | 0.7 | 0.8 | 3.0 |
| Botswana | UMIC | – | – | 18.3 | 18.3 | 2.1 | 2.1 | – | – | 2.1 | 1.3 | 25.0 | 3.8 | 5.3 | 54.6 |
| Burkina Faso | LIC | – | – | – | – | 0.3 | – | – | – | 1.4 | 1.2 | 29.0 | 0.9 | 0.9 | 9.3 |
| Burundi | LIC | – | – | – | – | 0.4 | – | – | – | 0.2 | 0.2 | 0.0 | 0.7 | 1.0 | 6.5 |
| Cabo Verde | LMIC | – | – | – | – | 3.4 | – | – | – | 3.4 | 0.0 | 50.0 | 8.3 | 7.8 | 13.0 |
| Cameroon | LMIC | – | 12.2 | 0.0 | 23.6 | 0.2 | – | – | – | 0.5 | 0.2 | 37.5 | 1.3 | 0.9 | 3.6 |
| Chad | LIC | – | – | – | – | 0.1 | – | – | – | 0.2 | 0.0 | 0.0 | 0.6 | 0.4 | 2.0 |
| Congo, Democratic Republic | LIC | – | 0.3 | 0.3 | 0.6 | 0.2 | 0.0 | – | – | 0.3 | 0.1 | 18.0 | 3.8 | 0.7 | 11.1 |
| Congo, Republic | LMIC | – | 0.4 | 0.3 | 8.5 | 1.3 | 0.2 | – | – | 1.8 | 0.7 | 20.0 | 1.0 | 1.7 | 9.7 |
| Cote d'Ivoire | LMIC | – | 23.3 | 0.0 | 23.3 | 0.3 | – | 0.0 | 1.2 | 0.3 | 33.0 | 1.6 | 2.3 | 6.6 | |
| Djibouti | LMIC | – | – | – | – | – | – | – | – | – | – | – | 2.2 | 2.2 | 7.3 |
| Egypt | LMIC | 624.0 | 517.7 | 0.1 | 610.0 | 5.5 | 0.0 | 15.5 | 0.3 | 32.9 | 3.7 | 25.0 | 7.5 | 4.5 | 19.3 |
| Eritrea | LIC | – | – | – | – | – | – | – | – | – | – | – | 0.8 | 0.6 | 14.4 |
| Ethiopia | LIC | – | 5.8 | 0.0 | 5.8 | 0.2 | – | 0.1 | 0.0 | 0.2 | 0.1 | 21.0 | 1.1 | 0.8 | 7.8 |
| Gabon | UMIC | – | 103.0 | 0.0 | 103.0 | 3.8 | – | – | – | 6.8 | 6.4 | 53.0 | 6.5 | 6.8 | 21.1 |
| Gambia | LIC | – | – | – | – | 0.8 | – | – | – | 2.1 | 0.0 | 2.0 | 0.8 | 1.0 | 9.5 |
| Ghana | LMIC | – | 4.4 | 0.0 | 4.4 | 0.9 | – | 0.1 | – | 0.4 | 0.1 | 36.4 | 1.7 | 1.4 | 36.2 |
| Guinea | LIC | – | – | – | – | 0.4 | – | – | – | 1.1 | 0.6 | 1.0 | 2.3 | 0.8 | 5.8 |
| Kenya | LMIC | – | 9.2 | 1.1 | 10.3 | 3.8 | 0.1 | 2.9 | 0.1 | 0.9 | 0.1 | 7.8 | 1.6 | 1.6 | 11.7 |
| Liberia | LIC | – | – | – | – | – | – | – | – | – | – | – | 0.5 | 0.4 | 19.5 |
| Libya | UMIC | – | 347.1 | 8.3 | 360.1 | – | – | 0.8 | – | – | – | – | 20.9 | 20.9 | 65.3 |
| Madagascar | LIC | – | 5.1 | 0.0 | 5.1 | 0.4 | – | – | – | 0.1 | 0.2 | 33.3 | 2.0 | 1.8 | 3.0 |
| Malawi | LIC | – | – | – | – | 0.2 | – | – | – | 0.0 | 0.0 | 0.0 | 0.5 | 0.4 | 7.1 |
| Mali | LIC | – | 3.9 | 0.0 | 3.9 | 0.6 | – | – | – | 1.8 | 0.2 | 8.0 | 1.3 | 1.3 | 4.4 |
| Mauritania | LMIC | – | 80.5 | 0.0 | 80.5 | 3.8 | – | – | – | 2.6 | 0.7 | 1.0 | 1.9 | 1.9 | 9.3 |
| Mauritius | UMIC | – | 648.8 | 0.0 | 648.8 | 11.5 | 3.8 | 10.8 | – | 7.6 | 2.3 | 0.0 | – | – | – |
| Morocco | LMIC | 541.0 | 185.0 | 0.6 | 185.6 | 11.4 | 0.2 | 0.4 | 0.2 | 15.2 | 2.7 | 65.0 | 7.3 | 7.3 | 13.9 |
| Mozambique | LIC | – | 0.9 | 0.9 | 0.9 | 0.1 | – | – | – | 0.1 | 0.0 | 100.0 | 0.9 | 0.8 | 4.9 |
| Namibia | UMIC | – | 16.8 | 9.6 | 16.8 | 5.1 | – | – | 0.4 | 1.1 | 0.0 | 100.0 | 5.9 | 4.2 | 19.5 |
| Niger | LIC | – | – | – | – | 0.2 | – | – | – | 0.3 | 0.0 | 8.0 | 0.4 | 0.4 | 2.2 |
| Nigeria | LMIC | – | 7.4 | 0.0 | 7.4 | 0.8 | 0.0 | 0.8 | 0.1 | 1.6 | 0.2 | 40.0 | 3.8 | 3.8 | 15.0 |
| Rwanda | LIC | 4.4 | – | – | 2.8 | – | – | – | – | – | – | – | 1.2 | 1.3 | 9.5 |
| Senegal | LMIC | – | 9.7 | 1.6 | 11.3 | 1.5 | 0.3 | – | – | 2.3 | 3.1 | 30.0 | 0.9 | 0.7 | 5.4 |
| Sierra Leone | LIC | – | – | – | – | – | – | – | – | – | – | – | 0.7 | 0.3 | 7.5 |
| Somalia | LIC | – | – | – | – | – | – | – | – | – | – | – | 0.2 | 0.2 | 1.1 |
| South Africa | UMIC | 169.0 | 134.3 | 23.3 | 156.0 | 5.2 | – | 15.0 | 0.1 | 2.6 | 0.2 | – | 7.9 | 9.1 | 49.7 |
| Sudan | LIC | – | 67.9 | 2.5 | 70.4 | 1.9 | 0.1 | 3.2 | 0.1 | 1.0 | 0.2 | 45.0 | 2.6 | 2.6 | 11.5 |
| Swaziland | LMIC | – | 15.4 | 0.0 | 15.4 | 3.6 | 0.9 | – | – | 1.8 | 0.0 | 50.0 | 1.4 | 3.3 | 25.1 |
| Tanzania | LMIC | – | 0.5 | 0.0 | 0.5 | 0.7 | 0.1 | 0.1 | 0.0 | 0.5 | 0.1 | 42.0 | 0.5 | 0.1 | 5.7 |
| Togo | LIC | – | 8.3 | 0.0 | 8.3 | 1.1 | – | – | – | 0.4 | 1.2 | – | 0.8 | 0.8 | 5.1 |
| Tunisia | LMIC | 1018.0 | 722.8 | 36.8 | 759.6 | 15.9 | 0.8 | 11.1 | 0.5 | 18.5 | 5.5 | 66.0 | 13.0 | 13.0 | 25.1 |
| Uganda | LIC | – | 1.2 | 0.7 | 1.2 | 0.3 | – | – | – | 0.3 | 0.0 | 28.6 | 1.5 | 1.7 | 16.4 |
| Zambia | LIC | – | 1.7 | 1.7 | 2.9 | 0.5 | 0.1 | – | 0.1 | 0.3 | 0.0 | 16.0 | 1.2 | 11.9 | 10.2 |
| Zimbabwe | LMIC | – | 2.8 | 2.8 | 2.8 | 1.3 | 0.1 | – | – | 0.4 | 0.1 | 4.0 | 2.0 | 2.1 | 21.4 |
–, data not reported or unavailable; HD, hemodialysis; ISN, International Society of Nephrology; KF, kidney failure; LIC, low-income country; LMIC, lower-middle-income country; PD, peritoneal dialysis; PMP, per million population; UMIC, upper-middle-income country.
Survey response data.
Figure 1.
Countries in the International Society of Nephrology Africaregion.
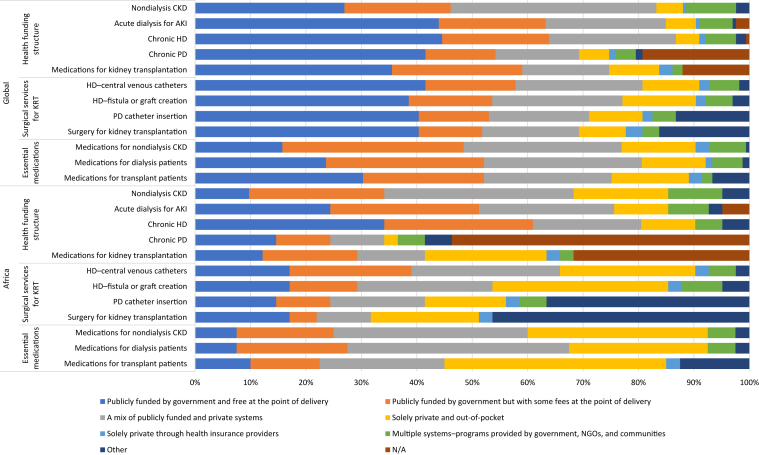
Figure 2.
Funding structures for nondialysis chronic kidney disease (CKD) and kidney replacement therapy (KRT), globally and in the International Society of Nephrology Africa region. Values represent the absolute number of countries in each category expressed as a percentage of the total number of countries. AKI, acute kidney injury; HD, hemodialysis; N/A, not applicable; NGO, nongovernment organization; PD, peritoneal dialysis.
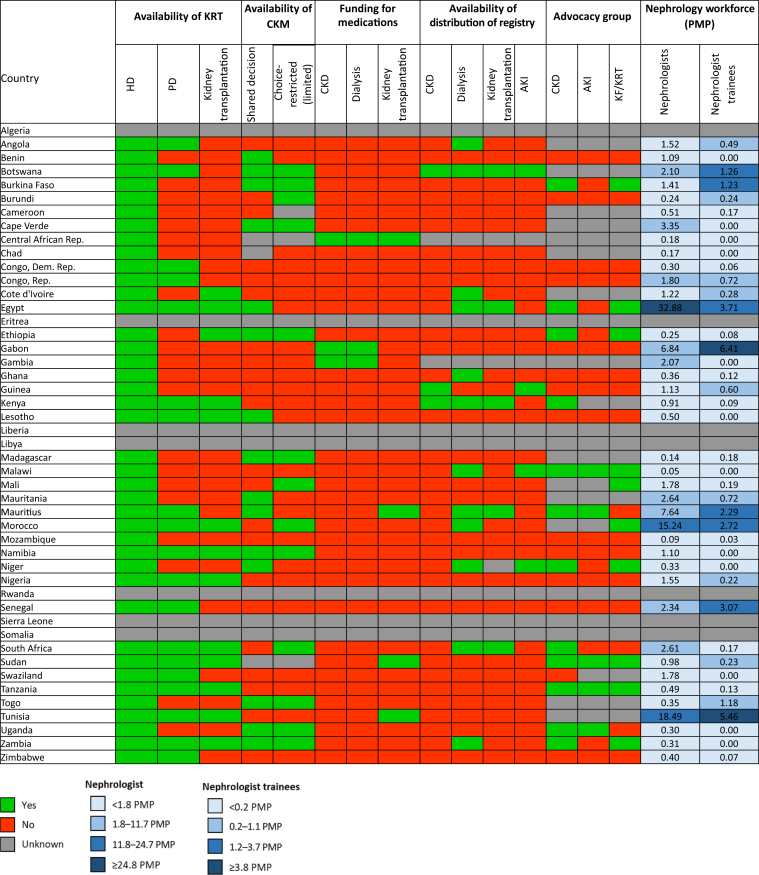
Figure 3.
Country level scorecard showing availability of kidney replacement therapy (KRT), funding of medications, registries, and advocacy groups of countries in the International Society of Nephrology Africa region. Funding for medications refers to 100% publicly funded by the government (free at the point of delivery). AKI, acute kidney injury; CKD, chronic kidney disease; CKM, conservative kidney management; Dem, Democratic; HD, hemodialysis; KF, kidney failure; PD, peritoneal dialysis; PMP, per million population; Rep, Republic.
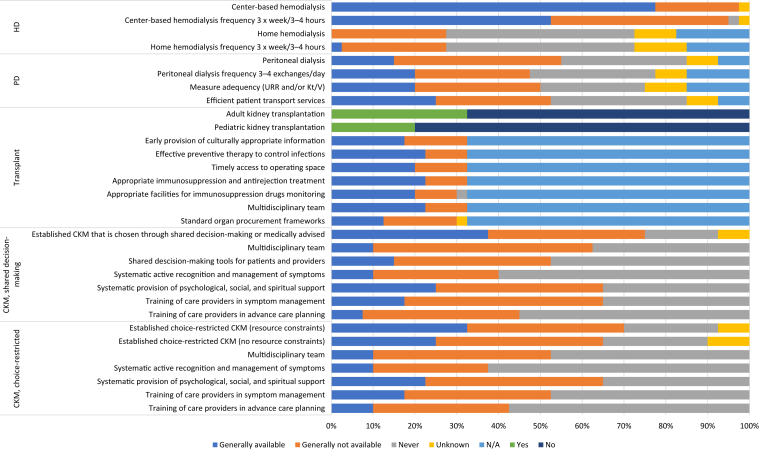
Figure 4.
Availability of choice in kidney replacement therapy or conservative kidney management (CKM) for people living with kidney failure in the International Society of Nephrology Africa region. Values represent the absolute number of countries in each category expressed as a percentage of the total number of countries. HD, hemodialysis; Kt/V, measure of dialysis adequacy; N/A, not applicable; PD, peritoneal dialysis; URR, urea reduction ratio.
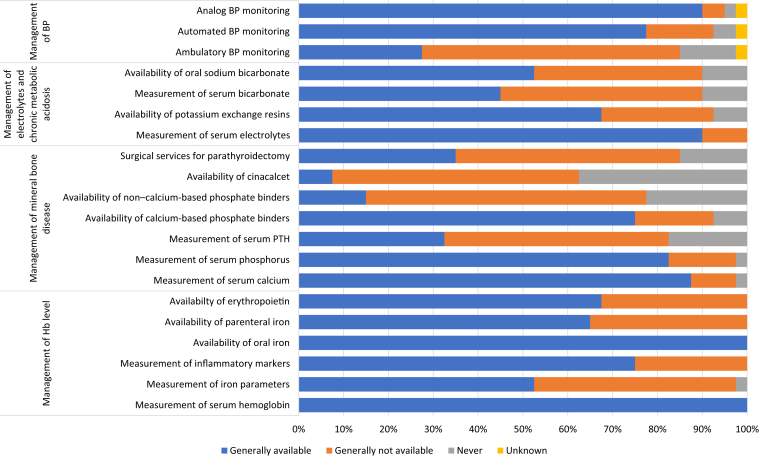
Figure 5.
Available services to diagnose and treat complications of kidney failure in the International Society of Nephrology Africa region. Values represent the absolute number of countries in each category expressed as a percentage of the total number of countries. BP, blood pressure; Hb, hemoglobin; PTH, parathyroid hormone.
Study setting
Africa is second only to Asia as the largest and most populous continent in the world.16 It has a landmass of approximately 30.3 million km2 including adjacent islands, occupying 20% of Earth’s land mass and 6% of the total surface area.41 With 1.4 billion people41as of 2021, it is home to approximately 18% of the world’s population and has the youngest population globally with a median age of 18.8 years.42 It is rife with numerous communicable diseases and a rising prevalence and mortality from noncommunicable diseases.43
Africa has 54 countries divided into 5 geographic and economic regions. There are also territories and independent states with limited recognition on the continent including Sahrawi Arab Democratic Republic, Republic of Somaliland, French Southern Territories, Mayotte, Saint Helena, Ascension and Tristan da Cunha, Reunion, Madeira, Melilla, and Canary Islands. Algeria has the largest surface area in Africa (2.4 million km2), whereas Nigeria has the largest population (224 million).44 Africa encompasses a rich diversity of ethnicities, cultures, religions, and languages including English, French, and numerous indigenous languages.
Although Africa has abundant natural resources, it is the world’s poorest and least developed continent in terms of the current economic ranking. Its total nominal gross domestic product (GDP) put together is lower than that of many individual countries (e.g., United States, China, Japan, Germany, United Kingdom, India, and France). According to the World Bank, >50% of the extremely poor (living on less than US $1.90 per day) lived in sub-Saharan Africa from 2010 to 2016.45 By 2017, the World Bank estimated that 9.2% (689 million people) of the world population were extremely poor.46 Sub-Saharan Africa and South Asia collectively accounted for 85% of the total number of people living in poverty. More than half of this population lived in 5 countries: Nigeria, Democratic Republic of Congo, and Ethiopia in Africa, and India and Bangladesh, outside of Africa.47,48 The number of poor people in sub-Saharan Africa increased from 276 to 413 million between 1990 and 2015.49
Government spending on health care is low in Africa. In 2017, the World Health Organization reported a 70-fold difference in health care spending between high-income and lower-income countries, with the lowest spending in the West, Central, and East African countries. In the same year, more than half of donor funding for health went to 14 countries, and one-fifth went to 4 countries, 3 of which were in Africa (Kenya, Nigeria, and Uganda).50
Current status of kidney care
Kidney health care in Africa is mostly characterized by limited availability of high-quality data, poor funding, low workforce density, and limited accessibility and affordability to KRT.51 There have been efforts by the African Association of Nephrology (AFRAN) to augment and improve kidney registries on the continent, but this is inchoate and limited to a few countries.52,53 The recent COVID-19 pandemic has further strained already weak health systems, thereby widening the already large gaps in health care infrastructure and financing.54 The prevalence of CKD in Africa has previously been reported to be 15.8%1 and 13.9%55 in systematic reviews and meta-analyses, respectively.
Literature review data for countries in the ISN Africa region
Burden of CKD, risk factors, and health care workforce
There are 54 United Nations member states in Africa, 51 of which are affiliated with the ISN; however, literature review data were based on 46 countries for which data were available at the time of analysis.
The median prevalence of CKD in Africa was 4.2% based on Global Burden of Disease data,17 which was lower than the global median prevalence of 9.5%. Tunisia had the highest median prevalence of CKD in Africa (11.8%), whereas Uganda had the lowest (3.0%). The median percentage of deaths attributable to CKD in Africa was 1.8% (vs. global 2.4%) and ranged from 1% in Mozambique to 4.1% in Morocco. The disability-adjusted life years attributed to CKD per 100,000 ranged from 287.9 in Madagascar to 818.5 in Swaziland, with a median of 464.4 (vs. 491.4 globally; Table 1).17
Among the CKD risk factors in Africa, obesity was most prevalent in Libya (31.8%) and lowest in Ethiopia (3.6%; Supplementary Table S1).40 High blood pressure was most prevalent in Niger (33.4%) and lowest in Tunisia (23.2%), whereas the prevalence of smoking ranged from 1% in Sudan to 19.9% in Tunisia (Supplementary Table S1).40 Data on the prevalence of treated kidney failure were available in 5 countries with a median value of 541 per million population (pmp) (interquartile range: 169.0–624.0 pmp) (vs. 822.8 pmp globally), ranging from 4.4 pmp in Rwanda to 1018 pmp in Tunisia (Table 2).35, 36, 37, 38
The median specialist physician prevalence in Africa was 0.16 per 1000 population (vs. 1.95 globally; Table 2).39 The specialist physician prevalence ranged from 0.01 in Tanzania to 1.3 per 1000 in Tunisia. The doctor prevalence in Africa was 1.54 per 1000 (vs. 17.74 per 1000 globally), ranging from 0.23 per 1000 in Somalia to 13.03 per 1000 in Tunisia. The nurse prevalence in Africa was 9.48 per 1000 (vs. 36.20 per 1000 globally). Tunisia again had the highest nurse prevalence of 13.03 per 1000 and the lowest was 0.23 per 1000 in Somalia (Table 2).39
Overview of GDP and government health expenditure by individual countries
The GDP in billion dollars was lowest in Cabo Verde (US $3.95) and highest in Egypt (US $1388.33; Table 1).16 The annual total health spending per person in Africa was US $54 (vs. US $353 globally). It was lowest in Somalia (US $2) and highest in Botswana (US $353). The median government health spending per person in Africa was US $16 (vs. US $216 globally) (Table 1).18 The median total health expenditure as a percentage of GDP was 4.6% (interquartile range: 3.5%–6.4%) and ranged from 1.8% in Djibouti to 9.1% in Sierra Leone. The median out-of-pocket (OOP) spending was US $20 (vs. US $92 globally; Table 1).16,18
Cost of KRT in Africa
The median annual cost of in-center HD in the ISN Africa region was US $13,793 (vs. US $19,380.30 globally) and ranged from US $1646.45 in Burkina Faso to US $32,537.77 in the Democratic Republic of Congo, both low-income countries (Table 1).15,19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34 The median annual cost of continuous ambulatory PD was US $14,192 (vs. US $18,959 globally), ranging from US $2772 in Egypt, a lower-middle-income country, to US $45,571 in Democratic Republic of Congo, a low-income country. The first-year median cost of kidney transplantation was US $20,713.9 (vs. US $26.903.2 globally) and ranged from US $8318 in Egypt to US $91,761 in Morocco (Table 1).15,19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34
Survey response data for the ISN Africa region
Characteristics of participating countries
Responses were received from 41 of 54 countries in the ISN Africa region with a response rate of 75.9%, representing 1.31 billion (92.8%) of the region’s population (Figure 1).
Africa had the highest number of respondents in the 2023 ISN-GKHA, representing 24.6% of all global survey respondents. Of the 41 countries, 5 (12.2%) were upper-middle-income countries, 17 (41.5%) were lower-middle-income countries, and 19 (46.3%) were low-income countries.15 Respondents included 49 (80%) adult nephrologists, 5 (8%) non-nephrologists/physicians, 1 (2%) pediatric nephrologist, and 6 (10%) hospital administrators/policymakers/civil servants.
Health finance and service delivery for kidney care
Kidney care for nondialysis CKD in Africa was mainly funded by a mix of public and private structures in 14 countries (34%) and government/public funding with OOP copayment in 10 (24%). In 7 countries (17%), such care was solely funded through private OOP payments, and in 4 countries (10%), it was funded through public government funds and was free at the point of delivery. Few countries in Africa covered the cost of kidney care using public government funds with no fee at the point of service delivery; this included 10 countries (24%) for acute dialysis (HD or PD), 14 (34%) for chronic HD, and 6 (15%) for continuous ambulatory PD. Kidney transplant was mainly funded by private OOP payment in 9 countries (22%) and public funding in 5 countries (12%; Figure 2).
Health care workforce in kidney care
In most countries (n = 34; 83%), nephrologists were primarily responsible for the medical care of people with kidney failure. The median nephrologist prevalence in the ISN Africa region was 1.12 pmp (vs. 11.8 pmp globally), which was the lowest of all the ISN regions. In addition, nephrology trainee prevalence was low at 0.18 pmp (vs. 1.2 pmp globally). Malawi had the lowest prevalence of nephrologists (0.04 pmp) followed by Mozambique (0.09 pmp; Figure 1).
All countries reported a shortage of health care providers for the medical care of people with kidney failure including transplantation surgeons, access surgeons (HD and PD), dietitians, vascular access coordinators, transplantation coordinators, and dialysis nurses. The highest reported shortages were pediatric nephrologists (n = 40; 98%), vascular surgeons (n = 36; 88%), and transplant surgeons (n = 36; 88%). The least reported shortages were for laboratory technicians (n = 8; 20%) and radiologists to interpret kidney ultrasounds (n = 11; 27%; Supplementary Figure S1).
Capacity for KRT service provision
The prevalence of long-term HD was 12.2 pmp (vs. 322.7 pmp globally). It was available in all countries with a median number of 0.8 HD treatment centers pmp (vs. 5.1 pmp globally). The countries with the lowest median numbers of HD centers were Mozambique (0.09 pmp) and Chad (0.10 pmp). The highest prevalence of chronic dialysis (HD and PD) was found in Tunisia (759.6 pmp) and the lowest in Tanzania (0.5 pmp; Table 2).
Chronic PD was available in 19 (48%) countries. The chronic PD prevalence was 0.2 pmp (vs. global 21.0 pmp). The median number of PD centers was 0.1 pmp (vs. 1.6 pmp globally). Nigeria had the lowest number of PD treatment centers (0.02 pmp), and the highest numbers were reported in Lesotho (6.84 pmp) and Mauritius (3.82 pmp; Table 2).
Kidney transplantation services were available in 13 countries (33%). The median availability of kidney transplantation centers was 0.1 pmp (vs. 0.5 pmp globally). The incidence of kidney transplantation was 2.1 pmp (vs. 12.2 pmp globally) with the lowest occurring in Ethiopia (0.07 pmp) and the highest in Egypt (15.5 pmp; Table 2).
Conservative kidney management (CKM), chosen through shared decision-making, was generally available in 15 countries (38%; vs. 87 [53%] globally) and choice-restricted CKM was available in 13 countries (33%; vs. 65 countries [39%] globally; Figure 3).
Although all countries had reported some availability for HD services, the capacity to provide adequate dialysis (i.e., 3 sessions per week, 3–4 hours/session) was only available in 21 countries (53%). The capacity to provide adequate PD (i.e., 3–4 exchanges/d) was available in 8 countries (20%; Figure 4).
The availability of services to diagnose and treat kidney failure complications varied. The measurement of serum hemoglobin and oral iron preparations were available in all countries for the management of anemia. Cinacalcet was generally available in only 3 countries (8%), whereas non–calcium phosphate binders (e.g., sevelamer) were available in 6 countries (15%) for the management of mineral bone disease (Figure 5).
Health information systems, statistics, and national health policies
Health information reporting was generally low. Few countries reported having official registries for CKD (n = 3; 8%), chronic dialysis (n = 12; 31%), kidney transplantation (n = 5; 13%), AKI (n = 4; 10%), and CKM (n = 2; 4.9%). Only Botswana had a registry for all levels of kidney disease. Overall, 12 countries (31%) had a dialysis registry (Angola, Botswana, Cote d’Ivoire, Egypt, Ghana, Kenya, Malawi, Mauritius, Morocco, Niger, South Africa, and Zambia), whereas 5 countries (13%) had a kidney transplant registry (Botswana, Egypt, Kenya, Mauritius, and South Africa; Figure 3).
Outcomes among people treated with dialysis
Twelve countries (31%) reported that 11% to 50% of people treated with HD died within 1 year of commencement, whereas 11 countries (28%) reported 1% to 10% deaths within 1 year. The most frequently reported causes of death in people treated with HD were cardiovascular diseases in 13 countries (33%) and infections in 11 (28%). Eleven countries (28%) reported that 21% to 30% of people treated with HD required at least 1 hospitalization in their first year of treatment, whereas 9 countries (23%) reported that over 50% of people treated with HD required at least 1 hospitalization in the first year of dialysis. Twenty-one countries (54%) reported access-related infections as the most common cause of hospitalization, followed by access malfunction reported by 5 countries (13%) in people treated with HD. PD-related infections were the most common cause of death among people treated with PD in 5 countries (26%) with hospitalization reported in 11 countries (58%; Supplementary Figure S2A–D).
Barriers to optimal kidney care
The reporting of barriers to optimal kidney care varied across countries including geographical distance from point of care (n = 35; 85%), physician availability and accessibility (n = 32; 78%), patients’ knowledge and attitude (n = 33; 80%), availability of nephrologists (n = 34; 83%), health system access and availability (n = 31; 76%), and lack of political will and enabling policies (n = 26; 63%; Supplementary Figure S3).
Strategies for kidney advocacy
Despite the high burden of kidney disease in the region, it was not formally recognized by governments as a health priority. Less than half of countries (n = 19; 49%) recognized CKD as a health priority, and less than one-fifth recognized AKI (n = 7; 18%) as a priority (Supplementary Figure S4). Few advocacy groups existed for AKI, CKD, kidney failure, and KRT. There was a CKD advocacy group in 12 countries (46.2%), an AKI advocacy group in 3 (12%), and a KRT advocacy group in 9 (34.6%; Supplementary Figure S4). In addition, only 23 countries (59%) had a national strategy for noncommunicable diseases and 5 (13%) had national CKD-specific strategies (Supplementary Figure S4).
Discussion
CKD has attained public health significance in Africa and continues to increase due to a rise in the burden of contributing noncommunicable diseases (such as diabetes mellitus, hypertension, and glomerulonephritis) and communicable diseases (such as HIV and hepatitis B).56 Measures to control these risk factors, especially diabetes mellitus projected to increase in prevalence by 143% (from 2019 to 204557), are warranted to reduce the burden of CKD in the region. Africa is particularly challenged in its capacity to deliver optimum kidney health care due to extreme poverty in many countries (23 of the 28 poorest nations in the world are in Africa),58 low literacy rate, and reliance on indigenous health care systems including herbal remedies.59 Late detection, poor accessibility, and unaffordability of quality kidney care worsen the prognosis of people with CKD and kidney failure, claiming the lives of patients largely in their economically productive age in Africa.4
This report, from the 2023 ISN-GKHA, focuses on the ISN Africa region and highlights the significant gaps in the capacity to provide optimum and quality kidney care. Our report showed that (i) there was limited availability and quality of diagnosis and delivery of KRT, (ii) use of public (government) funding for KRT remained low, (iii) there were very few registries across all levels of kidney disease severity, (iv) there were critical health care workforce shortages across all cadres, and (v) there was a lack of advocacy and recognition of kidney disease as a public health priority.
Although the 2023 ISN-GKHA reported the prevalence of CKD in the ISN Africa region to be 4.2% (the lowest across all regions), systematic reviews and meta-analyses have reported much higher prevalence rates of 13.9% and 15.8%.1,55 These disparities could be due to the varying methodologies used in ascertaining CKD prevalence and lack of robust population-based or representative studies. The 2023 ISN-GKHA low prevalence of CKD may be under-reporting the true prevalence considering the contrasting evidence from studies reporting increasing prevalence of the major risk factors/causes of CKD.4,60 The Global Burden of Disease also reported an increase in kidney-related deaths from 1.3% to 2.5% from 2009 to 2019.61
Optimum medical kidney care can be delivered only in the presence of an adequate nephrology workforce of health care professionals. Although nephrologist prevalence generally increased from 0.92 pmp in the 2019 ISN-GKHA62 to 1.12 pmp in the 2023 survey, some countries such as Sudan and South Africa experienced decreases in both nephrologists and nephrology trainees. The Africa region has benefited greatly from the ISN Fellowships program since its inception in 1985, which has increased nephrology workforce in the continent by over 200 fellows.63 Nevertheless, this has not been sufficient to meet the demands of the continent. It is possible that in many countries in the region, more than 90% of nephrologists were former ISN Fellows;64 however, several trained kidney care providers (including nephrologists, dialysis nurses, and dialysis technologists) continue to leave the continent for greener pastures. The low density of nephrology workforce in the region has been largely attributed to a lack of nephrology exposure among medical students, inflexible work schedules, inadequate training, competition with more attractive specialties, and lack of local training infrastructure such that trainees may be required to travel out of their home country65 to gain the necessary skills.63
Although nephrology medical care was primarily delivered by nephrologists, in 34 countries (83%), there is also a need for professional expertise in all other kidney care cadres to deliver optimum health care. This includes kidney nurses, dietitians, transplant surgeons, transplant coordinators, vascular surgeons, kidney pathologists, technicians, and other health care workers involved directly and indirectly in the provision of kidney care.60 This is further worsened by the exodus of health care providers seeking better working conditions and higher level of renumeration in high-income countries after completing training,66 which has increased recently after the COVID-19 pandemic. In Nigeria, for example, 13,000 health workers migrated to the UK in 1 year alone.67
There was limited capacity to provide KRT. HD prevalence varied across the continent with Mozambique and Chad having the lowest. HD was reported to be universally available, but PD and kidney transplantation were less so, being available in 19 (48%) and 13 (33%) countries, respectively. This was despite kidney transplantation demonstrating better quality of life, improved survival, and being more cost-effective than long-term dialysis.68 Low transplant rates continue to persist because of poor public knowledge, organ shortages, limited acceptability to deceased organ donation, cultural and religious barriers, unavailability of the required kidney care workforce, insufficient health expenditure, and absence of an established legal framework.69,70
PD remains underused as a KRT modality. The lowest rate of PD treatment centers was in Nigeria (0.02 pmp)—the most populated country in the ISN Africa region. Although PD has many advantages over HD, such as being a home-based therapy, convenient, cost-effective, offering better or comparable clinical outcomes, and requiring less expensive equipment, it is still significantly underused. Challenges with PD as a treatment modality include unavailability or high cost of PD fluids, unavailable workforce trained in PD delivery, and challenges in identifying and treating PD-related complications. However, there are calls to improve PD uptake in lower-middle-income countries.71
Although HD was universally available in Africa, the annual cost varied widely ranging from US $2721.76 in Egypt to as high as US $45,571.33 in the Democratic Republic of Congo. This variability in cost may have been due to a lack of government subventions, high taxes, and high private provider costs. These factors coupled with high OOP costs make HD unaffordable in most countries. This in turn leads to increased mortality due to inadequate dialysis as only 4 countries (10%) use public/government funding or free dialysis at the point of delivery. Furthermore, this is worsened by the inequitable geographical distribution of the HD services in those countries where it is available.72
In addition to the limited capacity to provide KRT in Africa, the provision of kidney supportive/palliative care, that is, CKM, to those unable to access KRT was not readily available. The provision of CKM services is imperative in low-resource settings to address the high symptom burden and suffering of those with kidney failure who have no other treatment options.
Africa is endowed with rich natural resources but is chronically poor due to political instability, poor leadership, corruption, and poor health spending with the lowest GDP globally.73 Government health spending varies widely, with Somalia being the lowest (US $2) and Botswana resembling the global median of US $353. This might be influenced by political will, political stability, and country GDP leading to high OOP costs. Most countries are not abiding by the Abuja declaration, signed over 22 years ago, which states that 15% of the national budget should be allocated to health care.74 This has contributed to significant limitations in health systems affecting all facets of chronic disease care including kidney care across the spectrum, particularly for KRT with its attendant high costs. Governments in Africa should see health spending as an “investment” and not a “consumption” as kidney disease in Africa affects people in their reproductive and economically active ages.11,74
Data on kidney disease management are generally scarce in Africa. Only Botswana has registries for all levels of kidney disease. Dialysis registries were the most commonly available (n = 12; 31%), whereas CKM the least available (n = 2; 4.9%). Registries were available in Angola, Botswana, Cote d’Ivoire, Egypt, Ghana, Kenya, Malawi, Mauritius, Morocco, Niger, South Africa, and Zambia. There are calls by the AFRAN to ensure that all member countries establish local kidney disease registries that contribute to a continent-wide registry. Registry data help to guide efforts aimed at prevention, detection, and management of kidney diseases and provide critical information for planning, delivery, evaluating, and advocacy to convince government and policymakers to invest more in kidney care.53 For example, Botswana may be investing more in health because they have a registry for all levels of kidney disease. The South African registry has been the lead and has consistently published its annual reports since 201553 and encouraged others like Ghana to publish their first in 2021.52 More effort should be put in by the AFRAN into registries to draw governments’ attention to ensure timely and accurate Africa-wide data to inform policies and advocate for improved investment in kidney care in Africa.75
It is essential to focus on prevention to decrease kidney disease burden due to challenges in providing optimum kidney care. Prevention is the cheapest option to reduce the burden of kidney disease as we continue to engage government and policymakers to increase funding in kidney health care. This requires advocacy that may be effective when championed by nephrologists with community participation, awareness creation, and early targeted screening.12 Taking advantage of ISN initiatives (e.g., the Sister Renal Center Program, Fellowships, and Mentorship) and others such as the World Kidney Day activities may help achieve the goal of kidney health for all in Africa.59 Policies and strategies for accountability, leadership, and knowledge exchange are needed to deliver optimum care. Advocacy may help increase government prioritization directly for kidney health in the light of competing priorities such as clean water supply and basic sanitation, maternal and child health, malnutrition, and infections such as malaria, HIV, and tuberculosis that may all indirectly improve kidney care in low-income settings.76
In conclusion, this report highlighted substantial gaps in the structure and capacity for kidney care despite the huge burden of kidney disease in the ISN Africa region. There is an urgent need to focus on prevention efforts, nephrology workforce augmentation as well as task shifting, and advocacy for more government funding to decrease OOP costs among people with kidney disease, particularly those requiring KRT associated with unaffordable costs to many in the region. There were some limitations to the 2023 ISN-GKHA; these have been discussed.14 However, this work is important for guiding kidney care policy in the ISN Africa region.
Funding Source
This article is published as part of a supplement sponsored by the International Society of Nephrology with grant funding to the University of Alberta (RES0033080).
Role of the Funder/Sponsor
The International Society of Nephrology provided administrative support for the design and implementation of the study, survey, and data collection activities. The authors were responsible for data management, analysis, and interpretation, as well as manuscript preparation, review, and approval, and the decision to submit the manuscript for publication.
Disclosures
MRD reports personal fees (consultancy) from National Renal Care, outside the submitted work, and is the chair of the African Renal Registry and co-chair of the South African Renal Registry. NP-K reports personal fees (salary) from Africa Healthcare Network, outside the submitted work. LV reports personal fees (salary) and stock or stock options from Africa Healthcare Network, outside the submitted work. SA reports personal fees (salary) from the International Society of Nephrology, outside the submitted work. AKB reports other (consultancy and honoraria) from AMGEN Incorporated and Otsuka, other (consultancy) from Bayer and GSK, and grants from Canadian Institute of Health Research and Heart and Stroke Foundation of Canada, outside the submitted work; he is also an associate editor of the Canadian Journal of Kidney Health and Disease and co-chair of the ISN-Global Kidney Health Atlas. SD reports personal fees (salary) from the International Society of Nephrology, outside the submitted work. J-AD reports personal fees (salary) from the International Society of Nephrology, outside the submitted work. VJ reports personal fees from GSK, AstraZeneca, Baxter Healthcare, Visterra, Biocryst, Chinook, Vera, and Bayer, paid to his institution, outside the submitted work. DWJ reports consultancy fees, research grants, speaker’s honoraria, and travel sponsorships from Baxter Healthcare and Fresenius Medical Care; consultancy fees from AstraZeneca, Bayer, and AWAK; speaker’s honoraria from ONO and Boehringer Ingelheim & Lilly; and travel sponsorships from ONO and Amgen, outside the submitted work. He is also a current recipient of an Australian National Health and Medical Research Council Leadership Investigator Grant, outside the submitted work. CM reports personal fees (salary) from the International Society of Nephrology, outside the submitted work. MN reports grants and personal fees from KyowaKirin, Boehringer Ingelheim, Chugai, Daiichi Sankyo, Torii, JT, and Mitsubishi Tanabe; grants from Takeda and Bayer; and personal fees from Astellas, Akebia, AstraZeneca, and GSK, outside the submitted work. All other authors declared no competing interests.
Acknowledgments
The authors appreciate the support from the International Society of Nephrology’s (ISN’s) Executive Committee, regional leadership, and Affiliated Society leaders at the regional and country levels for their help with the ISN–Global Kidney Health Atlas.
Footnotes
Supplementary Table S1. Burden of chronic kidney disease and risk factors in the ISN Africa region.
Supplementary Figure S1. Workforce shortages for medical kidney care in the ISN Africa region.
Supplementary Figure S2. Outcomes (hospitalization and death) in people on dialysis in the ISN Africa region. (A) Proportion of people living with kidney failure on hemodialysis and die in the first year; (B) proportion of people living with kidney failure on peritoneal dialysis and die in the first year; (C) proportion of people living with kidney failure on hemodialysis and at least 1 hospitalization in the first year; (D) proportion of people living with kidney failure on peritoneal dialysis and at least 1 hospitalization in the first year.
Supplementary Figure S3. Barriers to optimum kidney failure care globally and in the ISN Africa region.
Supplementary Figure S4. Strategies for advocacy efforts globally and in the ISN Africa region. (A) National NCD strategy (% of total number of countries responded); (B) national strategy for improved care (% of total number of countries responded); (C) population covered by a national CKD-specific strategy (% of total number countries responded “Yes” in [B]) and a general NCD strategy (% of total number countries responded “Yes, but incorporated in NCD strategy” in [B]); (D) national advocacy for CKD.
Contributor Information
Fatiu Abiola Arogundade, Email: fatiu3@yahoo.com.
Regional Board and ISN-GKHA Team Authors:
Mohammed Abdel Gawad, Ezzedine Abderrahim, Ahmed Akl, Eyram Makafui Yoan Amekoudi, Atefeh Amouzegar, Jacob Olugbenga Awobusuyi, Omran Bakoush, Elsa R. Chissico, Yeoungjee Cho, Joshua Coker, Brett Cullis, Rumbidzai Dahwa, Rasha Ahmed Darwish, Sara N. Davison, Smita Divyaveer, Isabelle Ethier, Kevin Fagoonee, Aboubacar Sidiki Fofana, Robert Freercks, Winston Wing-Shing Fung, Pierre Eric Gandzali-Ngabe, Anukul Ghimire, Zaghloul Elsafy Gouda, Oswald Habyarimana, Htay Htay, Davy Ip Min Wan, Georgina Irish, Wesam Ismail, Abubacarr Jagne, Faiçal Jarraya, Kailash Jindal, Babikir G. Kabllo, Ahmed Y. Kalebi, François F. Kaze Folefack, Dearbhla M. Kelly, Rowena Lalji, Ben Lomatayo, Sidi Mohamed Mah, Guillaume Zalba Mahamat Abderraman, Mignon McCulloch, Yewondwossen Tadesse Mengistu, Mothusi Walter Moloi, Chisambo Mwaba, Brendon L. Neuen, John Ngigi, Abdou Niang, Joseph Nyandwi, Emad Odeh, Mohamed A. Osman, Cédric Patrick Le Grand Ouanekpone, Anna Petrova, Eliane M. Ranivoharisoa, Parnian Riaz, Syed Saad, Emily See, Ahmed Sokwala, Adaobi Uzoamaka Solarin, Stephen M. Sozio, Tarik Sqalli Houssani, Ernest Sumaili Kiswaya, Weu Melanie Tia, Sophanny Tiv, Thabang Ts'enoli, Somkanya Tungsanga, Ifeoma I. Ulasi, Ssentamu John Vanglist, Andrea Viecelli, Shoyab Wadee, Marina Wainstein, Nicola Wearne, Emily K. Yeung, and Deenaz Zaidi
Appendix
Regional Board and ISN-GKHA Team Authors
Mohammed Abdel Gawad: Nephrology Unit, School of Medicine, Newgiza University, Giza, Egypt; Nephrology, Mansoura University, Mansoura, Egypt
Ezzedine Abderrahim: Department of Nephrology and Internal Medicine, Charles Nicolle Hospital, Tunis, Tunisia; Faculty of Medicine of Tunis, El Manar University, Tunis, Tunisia
Ahmed Akl: Nephrology Unit, Urology and Nephrology Center, Mansoura University, Mansoura, Egypt
Eyram Makafui Yoan Amekoudi: Faculty of Health Sciences, University of Kara, Lome, Togo
Atefeh Amouzegar: Division of Nephrology, Department of Medicine, Firoozgar Clinical Research Development Center, Iran University of Medical Sciences, Tehran, Iran
Jacob Olugbenga Awobusuyi: Nephrology Unit, Department of Medicine, Lagos State University College of Medicine, Ikeja, Lagos, Nigeria
Omran Bakoush: Department of Internal Medicine, College of Medicine and Health Science, United Arab Emirates University, Al Ain, Abu Dhabi, United Arab Emirates; Department of Internal Medicine, Zliten Central Hospital, Zliten, Libya
Elsa R. Chissico: Nephrology Department, Hospital Central de Maputo, Maputo, Mozambique
Yeoungjee Cho: Department of Kidney and Transplant Services, Princess Alexandra Hospital, Brisbane, Queensland, Australia; Australasian Kidney Trials Network at the University of Queensland, Brisbane, Queensland, Australia
Joshua Coker: Department of Medicine, Connaught Hospital, University of Sierra Leone Teaching Hospitals Complex, Freetown, Sierra Leone
Brett Cullis: Department of Nephrology and Child Health, University of Cape Town, Cape Town, South Africa
Rumbidzai Dahwa: Unit of Internal Medicine, Faculty of Medicine and Health Sciences, University of Zimbabwe, Harare, Zimbabwe; The George Institute for Global Health, University of New South Wales, Sydney, New South Wales, Australia
Rasha Ahmed Darwish: Internal Medicine and Nephrology, Kasr Al Einy, Cairo University, Cairo, Egypt
Sara N. Davison: Division of Nephrology and Immunology, University of Alberta Faculty of Medicine and Dentistry, Edmonton, Alberta, Canada
Smita Divyaveer: Department of Nephrology, Postgraduate Institute of Medical Education and Research, Chandigarh, India
Isabelle Ethier: Division of Nephrology, Centre Hospitalier de l’Université de Montréal, Montréal, Québec, Canada; Health Innovation and Evaluation hub, Centre de Recherche du Centre Hospitalier de l’Université de Montréal, Montréal, Québec, Canada
Kevin Fagoonee: Nephrology Unit, Dr A G Jeetoo Hospital, Port Louis, Mauritius
Aboubacar Sidiki Fofana: Nephrology and Hemodialysis Unit, Kayes Hospital, Kayes, Mali
Robert Freercks: Division of Nephrology and Hypertension, Department of Medicine, School of Medicine, Nelson Mandela University, Gqeberha (Port Elizabeth), South Africa
Winston Wing-Shing Fung: Department of Medicine & Therapeutics, Prince of Wales Hospital, The Chinese University of Hong Kong, Hong Kong SAR, China
Pierre Eric Gandzali-Ngabe: Department of Nephrology and Hemodialysis, General Teaching Hospital, Brazzaville, Republic of Congo
Anukul Ghimire: Division of Nephrology, Department of Medicine, University of Calgary, Calgary, Alberta, Canada
Zaghloul Elsafy Gouda: Nephrology Department, Damanhur Teaching Hospital, General Organization of Teaching Hospitals and Institutes, Damanhur City, Elbuhira Governorate, Egypt
Oswald Habyarimana: Nephrology Unit, Department of Internal Medicine, Kigali University Teaching Hospital, University of Rwanda, Kigali, Rwanda
Ghenette Houston: Division of Nephrology and Immunology, Faculty of Medicine and Dentistry, University of Alberta, Edmonton, Alberta, Canada
Htay Htay: Department of Renal Medicine, Singapore General Hospital, Singapore; Duke-NUS Medical School, Singapore
Davy Ip Min Wan: Nephrology Unit, SSR National Hospital, Pamplemousses, Mauritius
Georgina Irish: Australia and New Zealand Dialysis and Transplant (ANZDATA) Registry, South Australia Health and Medical Research Institute, Adelaide, South Australia, Australia; Faculty of Health and Medical Sciences, University of Adelaide, Adelaide, South Australia, Australia; Central and Northern Adelaide Renal and Transplantation Service, Royal Adelaide Hospital, South Australia Health, Adelaide, South Australia, Australia
Wesam Ismail: Pathology Department, Medical School, Beni- Suef University, Beni- Suef, Egypt
Abubacarr Jagne: Internal Medicine Department, Edward Francis Small Teaching Hospital, Banjul, The Gambia
Faiçal Jarraya: Renal Pathology, Faculty of Medicine, Sfax University, Sfax, Tunisia
Kailash Jindal: Division of Nephrology and Immunology, Faculty of Medicine and Dentistry, University of Alberta, Edmonton, Alberta, Canada
Babikir G. Kabllo: Faculty of Medicine, Karary University Military Hospital, Omdurman, Khartoum, Sudan
Ahmed Y. Kalebi: Dr Ahmed Kalebi Consultancy Limited, Pathology Department, Nairobi, Kenya
François F. Kaze Folefack: Faculty of Medicine and Biomedical Sciences, University of Yaounde I, Yaounde, Cameroon
Dearbhla M. Kelly: Wolfson Centre for the Prevention of Stroke and Dementia, University of Oxford, John Radcliffe Hospital, Oxford, UK; Department of Intensive Care Medicine, John Radcliffe Hospital, Oxford, UK
Rowena Lalji: Centre for Kidney Disease Research, University of Queensland, Brisbane, Queensland, Australia; Department of Nephrology, Queensland Children's Hospital, Brisbane, Queensland, Australia; Metro South and Integrated Nephrology and Transplant Services (MINTS), Princess Alexandra Hospital, Brisbane, Queensland, Australia
Ben Lomatayo: Department of Internal Medicine, Aga Khan Hospital, Kisumu, Kenya
Sidi Mohamed Mah: Department of Nephrology and Dialysis, Grand National Hospital, Nouakchott, Mauritania
Guillaume Zalba Mahamat Abderraman: Nephrology Department, Renaissance University Hospital Center, University of N'Djamena, Chad
Mignon McCulloch: Pediatric Nephrology, Red Cross War Memorial Children’s Hospital, University of Cape Town, Cape Town, South Africa
Yewondwossen Tadesse Mengistu: School of Medicine, Addis Ababa University, Addis Ababa, Ethiopia
Mothusi Walter Moloi: Department of Medicine, Faculty of Medicine, University of Botswana, Gaborone, Botswana
Chisambo Mwaba: Department of Paediatrics and Child Health, University of Zambia Medical School, Lusaka, Zambia
Brendon L. Neuen: Kidney Trials Unit, Royal North Shore Hospital, Sydney, New South Wales, Australia; The George Institute for Global Health, Sydney, New South Wales, Australia
John Ngigi: Renal Department, Kenyatta National Hospital, Nairobi, Kenya
Abdou Niang: Nephrology Department, Cheikh Anta Diop University, CHU Dalal Jamm, Dakar, Senegal
Joseph Nyandwi: National Institute of Public Health, Nephrology & Immunology, Faculty of Medicine, University of Burundi, Burundi
Emad Odeh: Department of Nephrology, Al-Basheer Hospital, Ministry of Health. Amman, Jordan
Mohamed A Osman: Department of Family Medicine, University of Ottawa, Ottawa, Ontario, Canada
Cédric Patrick Le Grand Ouanekpone: Nephrology Department, University Hospital Center of Bangui, Bangui, Central African Republic
Anna Petrova: Department of Propaedeutics of Internal Medicine, Bogomolets National Medical University, Kyiv, Ukraine; Department of Nephrology,"Diavita Institute," Kyiv, Ukraine
Eliane M. Ranivoharisoa: Nephrology service and Hemodialysis Center, University Hospital of Befelatanana, Antananarivo, Madagascar
Parnian Riaz: Division of Nephrology, Department of Medicine, McMaster University, Hamilton, Ontario, Canada
Syed Saad: Division of Nephrology and Immunology, Faculty of Medicine and Dentistry, University of Alberta, Edmonton, Alberta, Canada
Emily See: Department of Nephrology, Royal Melbourne Hospital, Parkville, VIC, Australia; Department of Nephrology, Royal Children's Hospital, Parkville, VIC, Australia; Department of Critical Care, University of Melbourne, Melbourne, Australia
Ahmed Sokwala: Nephrology Division, Department of Medicine, Aga Khan University Hospital, Nairobi, Kenya
Adaobi Uzoamaka Solarin: Department of Paediatrics & Child Health, Faculty of Clinical Sciences, Lagos State University College of Medicine, Ikeja, Lagos State, Nigeria
Stephen M. Sozio: Department of Medicine, Johns Hopkins School of Medicine, Baltimore, Maryland, USA; Department of Epidemiology, Johns Hopkins Bloomberg School of Public Health, Baltimore, Maryland, USA
Tarik Sqalli Houssani: Epidemiology and Health Sciences Research Laboratory, Faculty of Medicine, Pharmacy and Dentistry, Sidi Mohamed Ben Abdellah University, Fez, Morocco
Ernest Sumaili Kiswaya: Renal Unit, Kinshasa University Hospital, Kinshasa, Democratic Republic of Congo
Weu Melanie Tia: Division of Nephrology, University Alassane Ouattara, Bouake, Côte d’Ivoire
Sophanny Tiv: Division of Nephrology and Immunology, Faculty of Medicine and Dentistry, University of Alberta, Edmonton, Alberta, Canada
Thabang Ts'enoli: Nephrology Division, Internal Medicine Department, Queen ‘Mamohato Memorial Hospital, Maseru, Lesotho
Somkanya Tungsanga: Division of Nephrology and Immunology, Faculty of Medicine and Dentistry, University of Alberta, Edmonton, Alberta, Canada; Division of General Internal Medicine-Nephrology, Department of Medicine, Faculty of Medicine, Chulalongkorn University, Bangkok, Thailand
Ifeoma I. Ulasi: Renal Unit, Department of Medicine, College of Medicine, University of Nigeria, Ituku Ozalla, Enugu State, Nigeria; Department of Medicine, University of Nigeria Teaching Hospital Ituku Ozalla, Enugu State, Nigeria; Department of Internal Medicine, Alex Ekwueme Federal University Teaching Hospital Abakaliki (AEFUTHA), Ebonyi State, Nigeria
Ssentamu John Vanglist: Division of Clinical Services, Department of Internal Medicine, JJ Dossen Hospital, Harper City, Maryland County, Liberia; Partners in Health-Liberia
Andrea Viecelli: Department of Kidney and Transplant Services, Division of Medicine, Princess Alexandra Hospital, Woolloongabba, Queensland, Australia; University of Queensland, Queensland, Australia; Australasian Kidney Trials Network at the University of Queensland, Brisbane, Queensland, Australia
Shoyab Wadee: Division of Nephrology, Wits Donald Gordon Medical Centre, University of the Witwatersrand, Johannesburg, South Africa
Marina Wainstein: Faculty of Medicine, University of Queensland, Brisbane, Queensland, Australia; West Moreton Kidney Health Service, Ipswich Hospital, Brisbane, Queensland, Australia
Nicola Wearne: Division of Nephrology and Hypertension, Department of Medicine, Groote Schuur Hospital, University of Cape Town, South Africa
Emily K. Yeung: Department of Nephrology, Monash Health, Clayton, Victoria, Australia
Deenaz Zaidi: Division of Nephrology and Immunology, Faculty of Medicine and Dentistry, University of Alberta, Edmonton, Alberta, Canada
Regional Board and ISN-GKHA Team Author disclosures
YC reports grants and other from Baxter Healthcare, outside the submitted work. RAD reports other (travel support) from the International Society of Nephrology, and a fiduciary role in AFRAN as a treasurer, outside the submitted work. SND reports research funding from Canadian Institutes of Health Research, Alberta Innovates, and Alberta Health services, outside the submitted work. IE reports grants from Fonds de Recherche du Québec—Santé, outside the submitted work. HH reports personal fees from AWAK Technology and Baxter Healthcare, and nonfinancial support from Mologic company, outside the submitted work. DIMW reports personal fees from Pfizer and a leadership role with the Renal Association of Mauritius, outside the submitted work. FJ reports travel support from Servier, AstraZeneca, Pfizer, and Fresenius, and a fiduciary role with the African Association of Nephrology, outside the submitted work. BLN reports personal fees (advisory boards, speaker honoraria) from AstraZeneca and Boehringer and Ingelheim, personal fees (advisory boards) from Alexion, Bayer, and Cambridge Healthcare Research, and personal fees (speaker honoraria) from Cornerstone Medical Education, Medscape, and the Limbic, outside the submitted work, with all fees paid to the George Institute for Global Health. ST reports fellowship grants from the International Society of Nephrology-Salmasi Family and the Kidney Foundation of Thailand, outside the submitted work. IU reports personal fees from AstraZeneca, Sanofi, and Boehringer Ingelheim, and other from AstraZeneca, outside the submitted work. All other authors declared no competing interests.
Supplementary Material
Supplementary Table S1. Burden of chronic kidney disease and risk factors in the ISN Africa region.
Supplementary Figure S1. Workforce shortages for medical kidney care in the ISN Africa region.
Supplementary Figure S2. Outcomes (hospitalization and death) in people on dialysis in the ISN Africa region. (A) Proportion of people living with kidney failure on hemodialysis and die in the first year; (B) proportion of people living with kidney failure on peritoneal dialysis and die in the first year; (C) proportion of people living with kidney failure on hemodialysis and at least 1 hospitalization in the first year; (D) proportion of people living with kidney failure on peritoneal dialysis and at least 1 hospitalization in the first year.
Supplementary Figure S3. Barriers to optimum kidney failure care globally and in the ISN Africa region.
Supplementary Figure S4. Strategies for advocacy efforts globally and in the ISN Africa region. (A) National NCD strategy (% of total number of countries responded); (B) national strategy for improved care (% of total number of countries responded); (C) population covered by a national CKD-specific strategy (% of total number countries responded “Yes” in [B]) and a general NCD strategy (% of total number countries responded “Yes, but incorporated in NCD strategy” in [B]); (D) national advocacy for CKD.
References
- 1.Kaze A.D., Ilori T., Jaar B.G., et al. Burden of chronic kidney disease on the African continent: a systematic review and meta-analysis. BMC Nephrol. 2018;19:125. doi: 10.1186/s12882-018-0930-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Okpechi I., Niang A., Hafez M., et al. A roadmap for kidney care in Africa. Afr J Nephrol. 2022;25:82–100. [Google Scholar]
- 3.Matsha T.E., Erasmus R.T. Chronic kidney disease in sub-Saharan Africa. Lancet Glob Health. 2019;7:e1587–e1588. doi: 10.1016/S2214-109X(19)30467-X. [DOI] [PubMed] [Google Scholar]
- 4.Naicker S. End-stage renal disease in sub-Saharan Africa. Ethn Dis. 2009;19(suppl 1):S1–S13-5. [PubMed] [Google Scholar]
- 5.Arogundade F.A., Hassan M.O., Omotoso B.A., et al. Spectrum of kidney diseases in Africa: malaria, schistosomiasis, sickle cell disease, and toxins. Clin Nephrol. 2016;86:53–60. doi: 10.5414/CNP86S120. [DOI] [PubMed] [Google Scholar]
- 6.Luyckx V.A. Nephrotoxicity of alternative medicine practice. Adv Chronic Kidney Dis. 2012;19:129–141. doi: 10.1053/j.ackd.2012.04.005. [DOI] [PubMed] [Google Scholar]
- 7.Okpechi I.G., Bello A.K., Luyckx V.A., et al. Building optimal and sustainable kidney care in low resource settings: the role of healthcare systems. Nephrology (Carlton) 2021;26:948–960. doi: 10.1111/nep.13935. [DOI] [PubMed] [Google Scholar]
- 8.Naicker S., Yang C.W., Hwang S.J., et al. The Novel Coronavirus 2019 epidemic and kidneys. Kidney Int. 2020;97:824–828. doi: 10.1016/j.kint.2020.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tannor E.K. Chronic kidney disease—the ‘neglected’ non-communicable disease in Ghana. Afr J Curr Med Res. 2018;2(1) [Google Scholar]
- 10.Ashuntantang G., Osafo C., Olowu W.A., et al. Outcomes in adults and children with end-stage kidney disease requiring dialysis in sub-Saharan Africa: a systematic review. Lancet Glob Health. 2017;5:e408–e417. doi: 10.1016/S2214-109X(17)30057-8. [DOI] [PubMed] [Google Scholar]
- 11.Arogundade F.A., Barsoum R.S. CKD prevention in sub-Saharan Africa: a call for governmental, nongovernmental, and community support. Am J Kidney Dis. 2008;51:515–523. doi: 10.1053/j.ajkd.2007.12.006. [DOI] [PubMed] [Google Scholar]
- 12.Tannor E.K., Calice-Silva V. Kidney health for all-efforts in low-income settings to enhance community engagement, kidney health awareness, and screening. Kidney Int Rep. 2021;7:359–362. doi: 10.1016/j.ekir.2021.12.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Swanepoel C.R., McCulloch M.I., Abraham G., et al. Challenges for sustainable end-stage kidney disease care in low-middle-income countries: the problem of the workforce. Kidney Int Suppl. 2020;10:e49–e54. doi: 10.1016/j.kisu.2019.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Okpechi I.G., Bello A.K., Levin A., Johnson D.W. Update on variability in organization and structures of kidney care across world regions. Kidney Int Suppl. 2024;13:6–11. [Google Scholar]
- 15.The World Bank World Development Indicators. The world by income and region. https://datatopics.worldbank.org/world-development-indicators/the-world-by-income-and-region.html
- 16.Central Intelligence Agency The World Factbook. https://www.cia.gov/the-world-factbook/
- 17.Institute for Health Metrics and Evaluation (IHME) Global Burden of Disease Collaborative Network. Global Burden of Disease Study 2019 (GBD 2019) Results. 2020. https://vizhub.healthdata.org/gbd-results/
- 18.The Institute for Health Metrics and Evaluation Global Health Data Exchange. Global Expected Health Spending 2019-2050. https://ghdx.healthdata.org/record/ihme-data/global-expected-health-spending-2019-2050
- 19.Abu-Aisha H., Elamin S. Peritoneal dialysis in Africa. Perit Dial Int. 2010;30:23–28. doi: 10.3747/pdi.2008.00226. [DOI] [PubMed] [Google Scholar]
- 20.Bahadi A., Benbria S., Elkabbaj D. Cost of dialysis therapy by modality in Morocco: cost-minimization study comparing peritoneal dialysis to hemodialysis. Ther Apher Dial. 2022;26:1052–1053. doi: 10.1111/1744-9987.13838. [DOI] [PubMed] [Google Scholar]
- 21.Boima V., Agyabeng K., Ganu V., et al. Willingness to pay for kidney transplantation among chronic kidney disease patients in Ghana. PLoS One. 2020;15 doi: 10.1371/journal.pone.0244437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Elsharif M.E., Elsharif E.G., Gadour W.H. Costs of hemodialysis and kidney transplantation in Sudan: a single center experience. Iran J Kidney Dis. 2010;4:282–284. [PubMed] [Google Scholar]
- 23.Haddiya I., Radoui A., Benamar L., et al. Ten years of renal transplantation in a Moroccan hospital: results and constraints. Transplant Proc. 2012;44:2976–2981. doi: 10.1016/j.transproceed.2012.02.038. [DOI] [PubMed] [Google Scholar]
- 24.Izeidi P.P.M., Nlandu Y.M., Lepira F.B., et al. Cost estimate of chronic hemodialysis in Kinshasa, the Democratic Republic of the Congo: a prospective study in two centers. Hemodial Int. 2020;24:121–128. doi: 10.1111/hdi.12802. [DOI] [PubMed] [Google Scholar]
- 25.Kassa D.A., Mekonnen S., Kebede A., et al. Cost of hemodialysis treatment and associated factors among end-stage renal disease patients at the tertiary hospitals of Addis Ababa city and Amhara region, Ethiopia. Clinicoecon Outcomes Res. 2020;12:399–409. doi: 10.2147/CEOR.S256947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lang J.J., Lombardi C.V., James I.A., et al. A payer's perspective: a comparison and simulation of the costs of hemodialysis versus living donor kidney transplant for patients with end-stage renal disease in Nigeria. Transpl Int. 2022;35 doi: 10.3389/ti.2022.10662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mushi L., Krohn M., Flessa S. Cost of dialysis in Tanzania: evidence from the provider's perspective. Health Econ Rev. 2015;5:28. doi: 10.1186/s13561-015-0064-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Obadiah M., Carl S., Ahmed H. Kidney transplantation versus dialysis in Zimbabwe: a systematic review of the cost-effectiveness. J Egypt Soc Nephrol Transplant. 2022;22:71–85. [Google Scholar]
- 29.Okafor C., Kankam C. Future options for the management of chronic kidney disease in Nigeria. Gend Med. 2012;9(suppl):S86–S93. doi: 10.1016/j.genm.2011.10.002. [DOI] [PubMed] [Google Scholar]
- 30.Soliman A.R., Fathy A., Roshd D. The growing burden of end-stage renal disease in Egypt. Ren Fail. 2012;34:425–428. doi: 10.3109/0886022X.2011.649671. [DOI] [PubMed] [Google Scholar]
- 31.Sumaili E.K., Cohen E.P., Zinga C.V., et al. High prevalence of undiagnosed chronic kidney disease among at-risk population in Kinshasa, the Democratic Republic of Congo. BMC Nephrol. 2009;10:18. doi: 10.1186/1471-2369-10-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Toure A.O., Balde M.D., Diallo A., et al. The direct cost of dialysis supported by families for patients with chronic renal failure in Ouagadougou (Burkina Faso) BMC Nephrol. 2022;23:222. doi: 10.1186/s12882-022-02847-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.van der Tol A., Lameire N., Morton R.L., et al. An international analysis of dialysis services reimbursement. Clin J Am Soc Nephrol. 2019;14:84–93. doi: 10.2215/CJN.08150718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yousif A.O., Idris A.K.M., Awad M.M., et al. Out-of-pocket payments by end-stage kidney disease patients on regular hemodialysis: cost of illness analysis, experience from Sudan. Hemodial Int. 2021;25:123–130. doi: 10.1111/hdi.12895. [DOI] [PubMed] [Google Scholar]
- 35.Davids M.R., Jardine T., Marais N., et al. South African Renal Registry Annual Report 2019. Afr J Nephrol. 2021;24:95–106. [Google Scholar]
- 36.Jain A.K., Blake P., Cordy P., et al. Global trends in rates of peritoneal dialysis. J Am Soc Nephrol. 2012;23:533–544. doi: 10.1681/ASN.2011060607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Liyanage T., Ninomiya T., Jha V., et al. Worldwide access to treatment for end-stage kidney disease: a systematic review. Lancet. 2015;385:1975–1982. doi: 10.1016/S0140-6736(14)61601-9. [DOI] [PubMed] [Google Scholar]
- 38.WHO-ONT Global Observatory on Donation and Transplantation. http://www.transplant-observatory.org/data-charts-and-tables/
- 39.World Health Organization. Global Health Observatory Health workforce. 2021. https://www.who.int/data/gho/data/themes/health-workforce
- 40.World Health Organization Global Health Observatory. https://www.who.int/data/gho
- 41.United Nations World Population Prospects. 2022. https://population.un.org/wpp/
- 42.Worldometer. Africa. 2023. https://www.worldometers.info/world-population/africa-population/
- 43.GBD 2016 Causes of Death Collaborators Global, regional, and national age-sex specific mortality for 264 causes of death, 1980-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390:e38. doi: 10.1016/S0140-6736(17)32152-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.UNFPA. United Nations Population Fund World population dashboard. https://www.unfpa.org/data/world-population-dashboard
- 45.Baloch M.A., Danish, Khan S.U., et al. Analyzing the relationship between poverty, income inequality, and CO2 emission in sub-Saharan African countries. Sci Total Environ. 2020;740 doi: 10.1016/j.scitotenv.2020.139867. [DOI] [PubMed] [Google Scholar]
- 46.World Bank Poverty. https://www.worldbank.org/en/topic/poverty/overview
- 47.Agayi C.O., Karakayaci O. Exploring the rural poverty prevalence and eradication strategies for rural development: the case of Kenya. Selcuk J Agr Food Sci. 2022;36:63–73. [Google Scholar]
- 48.Katayama R., Wadhwa D. World Bank Blogs. Half of the world’s poor live in just 5 countries. https://blogs.worldbank.org/opendata/half-world-s-poor-live-just-5-countries
- 49.Food and Agriculture Organization of the United Nations Ending extreme poverty in rural areas—sustaining livelihoods to leave no one behind. 2018. https://www.fao.org/3/ca1908en/CA1908EN.pdf
- 50.World Health Organization Global spending on health: a world in transition. 2019. https://www.who.int/publications/i/item/WHO-HIS-HGF-HFWorkingPaper-19.4
- 51.Osman M.A., Alrukhaimi M., Ashuntantang G.E., et al. Global nephrology workforce: gaps and opportunities toward a sustainable kidney care system. Kidney Int Suppl. 2018;8:52–63. doi: 10.1016/j.kisu.2017.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Boima V., Tannor E.K., Osafo C., et al. The Ghana Renal Registry—a first annual report. Afr J Nephrol. 2021;24(1) [Google Scholar]
- 53.Davids M.R., Eastwood J.B., Selwood N.H., et al. A renal registry for Africa: first steps. Clin Kidney J. 2016;9:162–167. doi: 10.1093/ckj/sfv122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Tannor E.K., Bajpai D., Nlandu Y.M., et al. COVID-19 and kidney disease: progress in health inequity from low-income settings. Semin Nephrol. 2022;42 doi: 10.1016/j.semnephrol.2023.151318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Stanifer J.W., Jing B., Tolan S., et al. The epidemiology of chronic kidney disease in sub-Saharan Africa: a systematic review and meta-analysis. Lancet Glob Health. 2014;2:e174–e181. doi: 10.1016/S2214-109X(14)70002-6. [DOI] [PubMed] [Google Scholar]
- 56.Hodel N.C., Hamad A., Praehauser C., et al. The epidemiology of chronic kidney disease and the association with non-communicable and communicable disorders in a population of sub-Saharan Africa. PLoS One. 2018;13 doi: 10.1371/journal.pone.0205326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.International Diabetes Federation IDF Diabetes Atlas (9th edition) 2019. https://diabetesatlas.org/atlas/ninth-edition
- 58.Institute for Security Studies (ISS) Africa is losing the battle against extreme poverty. https://issafrica.org/iss-today/africa-is-losing-the-battle-against-extreme-poverty
- 59.Tannor E.K., Nlandu Y.M., Elrggal M.E., et al. Kidney health for all—bridging the gap to better kidney care in Africa. Afr J Nephrol. 2022;25:108–115. [Google Scholar]
- 60.Abd ElHafeez S., Bolignano D., D'Arrigo G., et al. Prevalence and burden of chronic kidney disease among the general population and high-risk groups in Africa: a systematic review. BMJ Open. 2018;8 doi: 10.1136/bmjopen-2016-015069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Feng X., Hou N., Chen Z., et al. Secular trends of epidemiologic patterns of chronic kidney disease over three decades: an updated analysis of the Global Burden of Disease Study 2019. BMJ Open. 2023;13 doi: 10.1136/bmjopen-2022-064540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Oguejiofor F., Kiggundu D.S., Bello A.K., et al. International Society of Nephrology Global Kidney Health Atlas: structures, organization, and services for the management of kidney failure in Africa. Kidney Int Suppl. 2021;11:e11–e23. doi: 10.1016/j.kisu.2021.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Harris D.C., Dupuis S., Couser W.G., et al. Training nephrologists from developing countries: does it have a positive impact? Kidney Int Suppl. 2012;2:275–278. doi: 10.1038/kisup.2012.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Okpechi I.G., Eddy A.A., Jha V., et al. Impact of training nephrologists from developing nations and strategies for sustaining a training program in its fourth decade. Kidney Int. 2021;99:1073–1076. doi: 10.1016/j.kint.2021.02.029. [DOI] [PubMed] [Google Scholar]
- 65.Sharif M.U., Elsayed M.E., Stack A.G. The global nephrology workforce: emerging threats and potential solutions! Clin Kidney J. 2016;9:11–22. doi: 10.1093/ckj/sfv111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Eastwood J.B., Conroy R.E., Naicker S., et al. Loss of health professionals from sub-Saharan Africa: the pivotal role of the UK. Lancet. 2005;365:1893–1900. doi: 10.1016/S0140-6736(05)66623-8. [DOI] [PubMed] [Google Scholar]
- 67.Lawal L., Lawal A.O., Amosu O.P., et al. The COVID-19 pandemic and health workforce brain drain in Nigeria. Int J Equity Health. 2022;21:174. doi: 10.1186/s12939-022-01789-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Czyżewski L., Sańko-Resmer J., Wyzgał J., et al. Assessment of health-related quality of life of patients after kidney transplantation in comparison with hemodialysis and peritoneal dialysis. Ann Transplant. 2014;19:576–585. doi: 10.12659/AOT.891265. [DOI] [PubMed] [Google Scholar]
- 69.Elrggal M.E., Gokcay Bek S., Shendi A.M., et al. Disparities in access to kidney transplantation in developing countries. Transplantation. 2021;105:2325–2329. doi: 10.1097/TP.0000000000003585. [DOI] [PubMed] [Google Scholar]
- 70.Muller E. Transplantation in Africa—an overview. Clin Nephrol. 2016;86:90–95. doi: 10.5414/CNP86S125. [DOI] [PubMed] [Google Scholar]
- 71.Okpechi I.G., Jha V., Cho Y., et al. The case for increased peritoneal dialysis utilization in low- and lower-middle-income countries. Nephrology (Carlton) 2022;27:391–403. doi: 10.1111/nep.14024. [DOI] [PubMed] [Google Scholar]
- 72.Tannor E., Awuku Y., Boima V., et al. The geographical distribution of dialysis services in Ghana. Ren Replace Ther. 2018;4:1–7. [Google Scholar]
- 73.African Development Bank Africa’s natural resources: the paradox of plenty. https://www.afdb.org/fileadmin/uploads/afdb/Documents/Publications/%28E%29%20AfricanBank%202007%20Ch4.pdf
- 74.World Health Organization The Abuja declaration: ten years on. 2010. https://iris.who.int/handle/10665/341162
- 75.Okpechi I.G. ESKD in sub-Saharan Africa: will governments now listen? Lancet Glob Health. 2017;5:e373–e374. doi: 10.1016/S2214-109X(17)30070-0. [DOI] [PubMed] [Google Scholar]
- 76.Jha V., Arici M., Collins A.J., et al. Understanding kidney care needs and implementation strategies in low- and middle-income countries: conclusions from a “Kidney Disease: Improving Global Outcomes" (KDIGO) Controversies Conference. Kidney Int. 2016;90:1164–1174. doi: 10.1016/j.kint.2016.09.009. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.