Abstract
Objective
Bruxism is a repetitive masticatory muscle activity. This study investigates dental practitioners’ approaches to bruxism assessment and treatment in practices.
Methods
A brief 5 question questionnaire (“Quick Poll”) on bruxism was conducted.
Results
A total of 397 practitioners responded. More than half (55%) initiated treatment for bruxism on one to three patients per month. The majority believed that stress (97%) and sleep patterns (82%) affected bruxism in their patients. Interestingly, 96% offered an occlusal guard/appliance and 46% made occlusal adjustments.
Conclusion
This study highlights inconsistencies in practitioner approaches to bruxism assessment and management in clinical settings, suggesting gaps in practitioner knowledge evidenced by the varied responses.
Graphical Abstract
Introduction
Bruxism is defined as a repetitive masticatory muscle activity (MMA) associated with teeth clenching, grinding and/or bracing, or thrusting of the mandible.1 There are two circadian manifestations: the behavior during sleep, referred to as sleep bruxism (SB), or while awake, referred to as awake bruxism (AB).2 The MMA that occurs during sleep is rhythmic (phasic) or non-rhythmic (tonic).2 During AB, the MMA is repeated or continuous with tooth contact and/or by bracing or thrusting the mandible.2 Based on self-reported data, the prevalence of SB in adults ranges from 8% to 16% in the United States.3 The prevalence of self-reported AB in adults ranges from 22% to 30%. Nearly 20% of people experience both forms of MMA, viz., SB and AB.2,3
The etiology of bruxism is multifactorial.4,5 Different types of MMA may have different etiologies and may be associated with varying health outcomes.3,6 First, it can have negative consequences (harmful), i.e., resulting in, e.g., severe masticatory muscle pain, temporomandibular joint (TMJ) pain, pathological mechanical tooth wear, and sometimes prosthodontic complications.6 Secondly, it can have protective (beneficial) effects by decreasing the chance of a negative health outcome. Examples include ending an episode of respiratory arousals, preventing collapse or restore the patency of the upper airway while asleep, or reducing the risk of detrimental chemical tooth wear by increasing salivation in case of gastroesophageal reflux.6 Lastly, it can also be neutral (neither harmless nor beneficial) where the behavior neither protects nor poses risks to the individual.6 Increasing evidence suggests the combination of several underlying mechanisms in bruxism’s physiopathology, such as psychosocial (e.g., stress and anxiety), physiological (e.g., genetics and sleep arousal), and exogenous (e.g., alcohol consumption, medication use, and tobacco use) factors.3,6 Existing knowledge is limited, but associated factors are distinct regarding both circadian manifestations of bruxism.3 Where psychosocial aspects appear to influence AB, autonomic/central nervous system activations are probable primary factors involved in SB origins.3
It is important to recognize that the management of bruxism has three aspects. First, bruxism is a behavior that may not mandate treatment. Secondly, treatment should only be recommended when severe negative consequences outweigh positive consequences (weighted decision). Lastly, unless the specific cause (the underlying mechanism) is identified, treatment is oriented to managing implied clinical consequences.3,7 The authors of a qualitative systematic literature review on SB suggested that, in the absence of known causes, management should be based on common sense conservative approaches, referring to the so-called ‘Multiple-P’ approach as the standard of reference: Pep talk (counseling), Psychology (cognitive-behavioral strategies), Physiotherapy (exercises of the jaw muscles), Plates (oral appliances), and Pills (medicines/drugs).3,7 The ‘Multiple-P’ approach may also be extended to AB, with minor differences (e.g., different instructions regarding the use of oral appliances).3,7 Importantly, performing irreversible occlusal changes to reduce bruxism activities or decrease pain symptoms in the jaw muscles and/or the TMJ is not recommended.3,7
Multiple and diverse strategies are in place to assess and manage bruxism, yet no standardized approach exists.1,7 Consequently, a dental practitioner should ascertain the presence of the behavior and, if present, come to a weighted decision on if and how to proceed. These new insights represent a paradigm shift and are likely unknown in general dental practices. It should be noted that presently these paradigm shifts are being taught in several dental school curriculums. However, dental curriculums can be further enhanced with evolving new evidence in this field and more clinical case-based scenarios to increase the next generation of practitioners’ confidence in assessing and managing patients with bruxism. An effort is also being made to raise awareness of more medical and dental education integration on topics such as bruxism.8,9 Considering this, a brief preliminary questionnaire (“Quick Poll”) was conducted in the National Dental Practice-Based Research Network (Network) to understand current approaches used by Network dental practitioners for bruxism assessment and management. The Network comprises a diverse group of ‘real-world’ dentists and dental hygienists in active community practices.10–12 One of the Network’s purposes is to identify gaps in the knowledge of dental practitioners, provide information and education around treatment options, and foster quality improvement through participation in research and translation of new knowledge into everyday clinical practice.10,11 The Network is integral to understanding practitioners’ perspectives on varied aspects of clinical topics, including bruxism, and this Quick Poll provides valuable information for developing a standardized approach for assessing bruxism.
The aim of the study was to investigate dental practitioners’ approaches to bruxism assessment and treatment in practices by gathering preliminary information from Network dental practitioners about initiating treatment for bruxism per month in their patient populations, factors practitioners believe affect bruxism, intervention criteria for bruxism treatment, and treatment options they offer their patients.
Materials and Methods
Quick Polls are conducted as a simple, low-cost means to engage Network members in clinical topics of interest, with an expectation that findings will inform the design of subsequent, rigorously-designed, full-scale questionnaires or clinical studies and publications. The Network has conducted over 40 Quick Polls based on practitioner interest.10 Members of the Southwest Region frequently cited bruxism as an area of interest in annual meetings. Therefore, a draft was developed by Southwest Region Network members for the Bruxism Quick Poll questions at their 2015 Regional Meeting. The questions were designed given the criteria of a Network Quick Poll, which is to limit to a maximum of 5 brief questions. The questions gather preliminary data on the bruxism topic that would guide/support the need for further research and represent the view of a private/community practitioner that wants to engage in research. Important in practice-based research is the involvement of the practitioner in the development of the question for Quick Polls as an ecological substantiation of the inquiry. The Southwest Region Directors/investigators further refined the draft, and in October 2015, a Quick Poll on bruxism was conducted by the Network. A single invitation to complete the poll was sent to all 4,355 Network dentists via email through the monthly newsletter, which informs members of various Network activities (Image 1). No follow-up of non-respondents was done because all data capture was anonymous. The Quick Poll on bruxism was constructed with five questions, with questions 2–4 being multiple response options (respondents were asked to “check all that apply”) (for response options, see Figures 1–3):
In how many patients do you initiate treatment for bruxism per month?
Which of the following factors do you believe affect bruxism?
What are your criteria for intervening for bruxism treatment?
Which of the following treatment options do you offer when treating patients with bruxism?
Would a study about bruxism be important to you and your patients?
Figure 1.
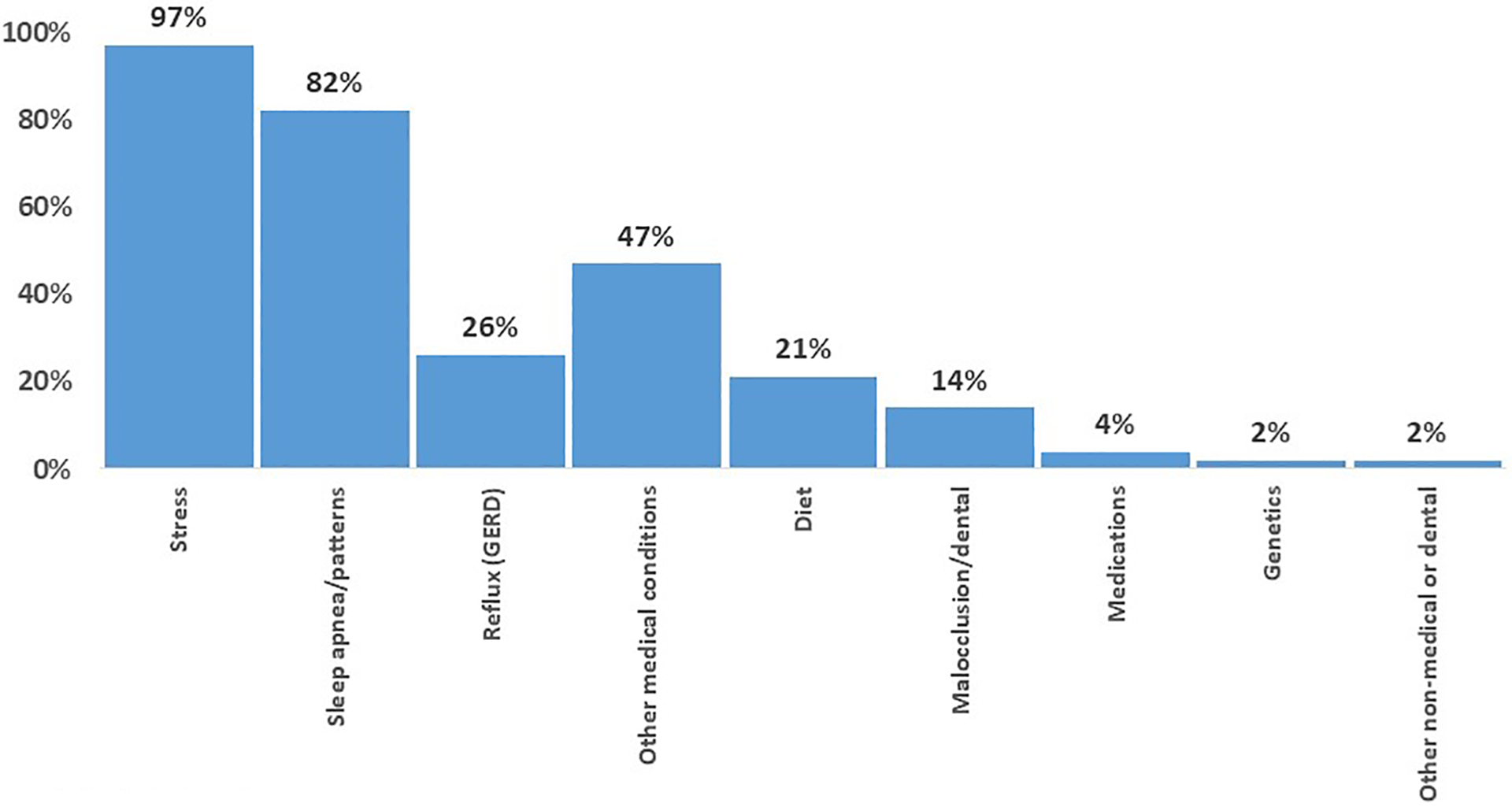
Factors affecting bruxism* (N=397)
*Check all that apply
Figure 3.
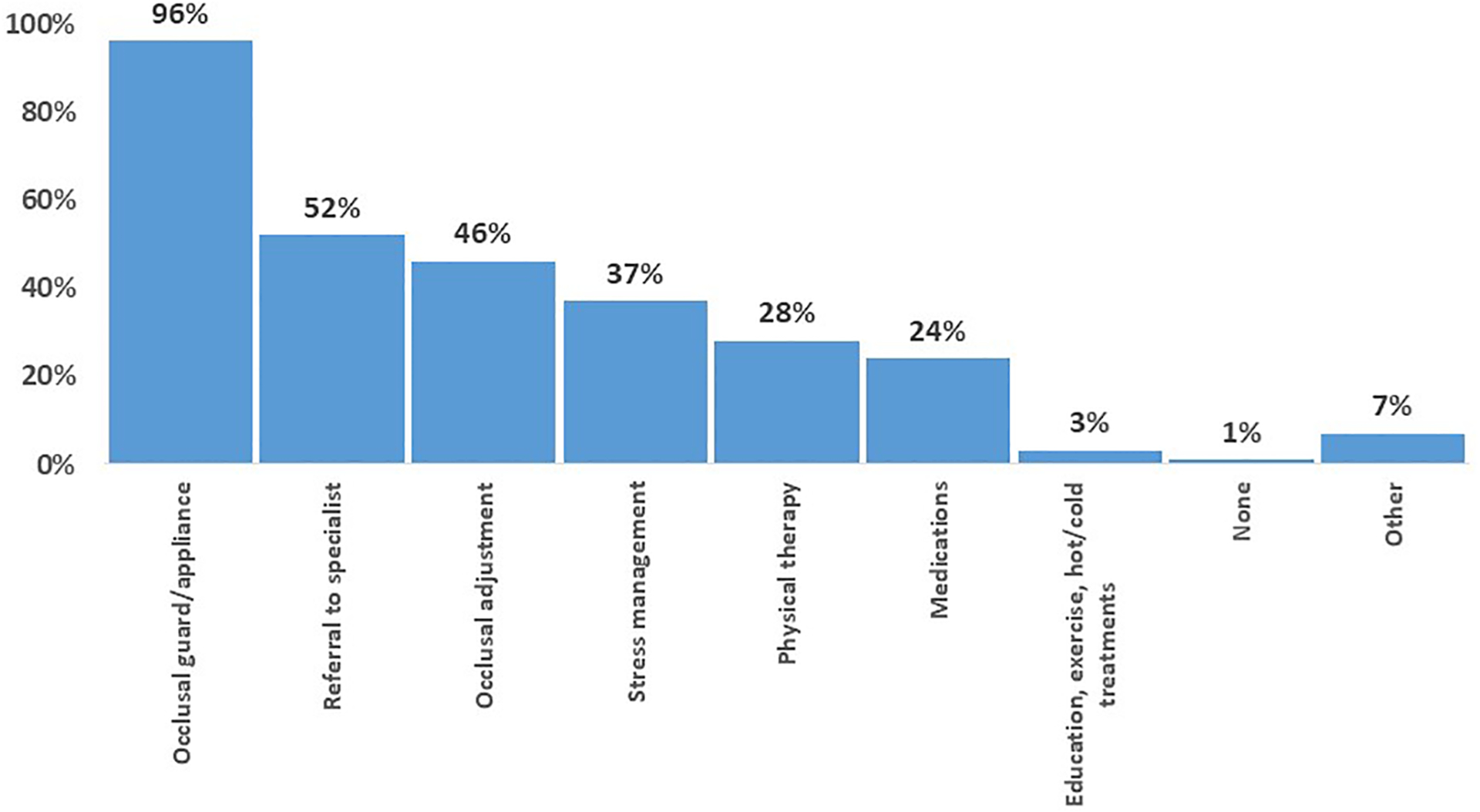
Treatments offered when treating bruxism* (N=396)
*Check all that apply
Furthermore, the study conformed to recognized standards of the US Federal Policy for the Protection of Human Subjects by obtaining Institutional Review Board (IRB) approval for the Network -National Dental PBRN Administrative & Resource Center, obtained from the University of Alabama at Birmingham (IRB-040903006).
Results
A total of 397 practitioners responded out of 4,355 (9% response rate) to the Quick Poll. In total, 55% (n=218) of the respondents indicated that they initiated treatment for bruxism on one to three patients per month, and 17% (n=69) indicated more than seven patients per month. Only 8% (n=30) of practitioners reported not initiating bruxism treatment at all.
Nearly all practitioners believed that stress (97%, n=384) and sleep patterns, including sleep apnea (82%, n=324), were factors that affect bruxism, followed by other medical conditions (47%, n=188). Other responses included reflux (26%, n=102), diet (21%, n=82), or malocclusion or other dental reasons (14%, n=54). Few practitioners indicated that medications (4%, n=17) or genetic factors (2%, n=9) could affect bruxism (Figure 1).
When practitioners were asked which criteria are of influence when deciding to treat bruxism (negative consequences), nearly all indicated that patient complaints (94%, n=373), objective signs such as tooth wear (93%, n=366), and severe or worsening of symptoms (89%, n=352) were criteria for clinical intervention. Practitioners also indicated that associated medical conditions such as sleep apnea (30%, n=119) were criteria for initiating bruxism treatment. Only three percent of respondents (n=10) said they treat patients with bruxism if the patients have cracked or fractured teeth, TMJ pain, or other reasons (e.g., abfraction, altered occlusion, sensitivity) (Figure 2).
Figure 2.
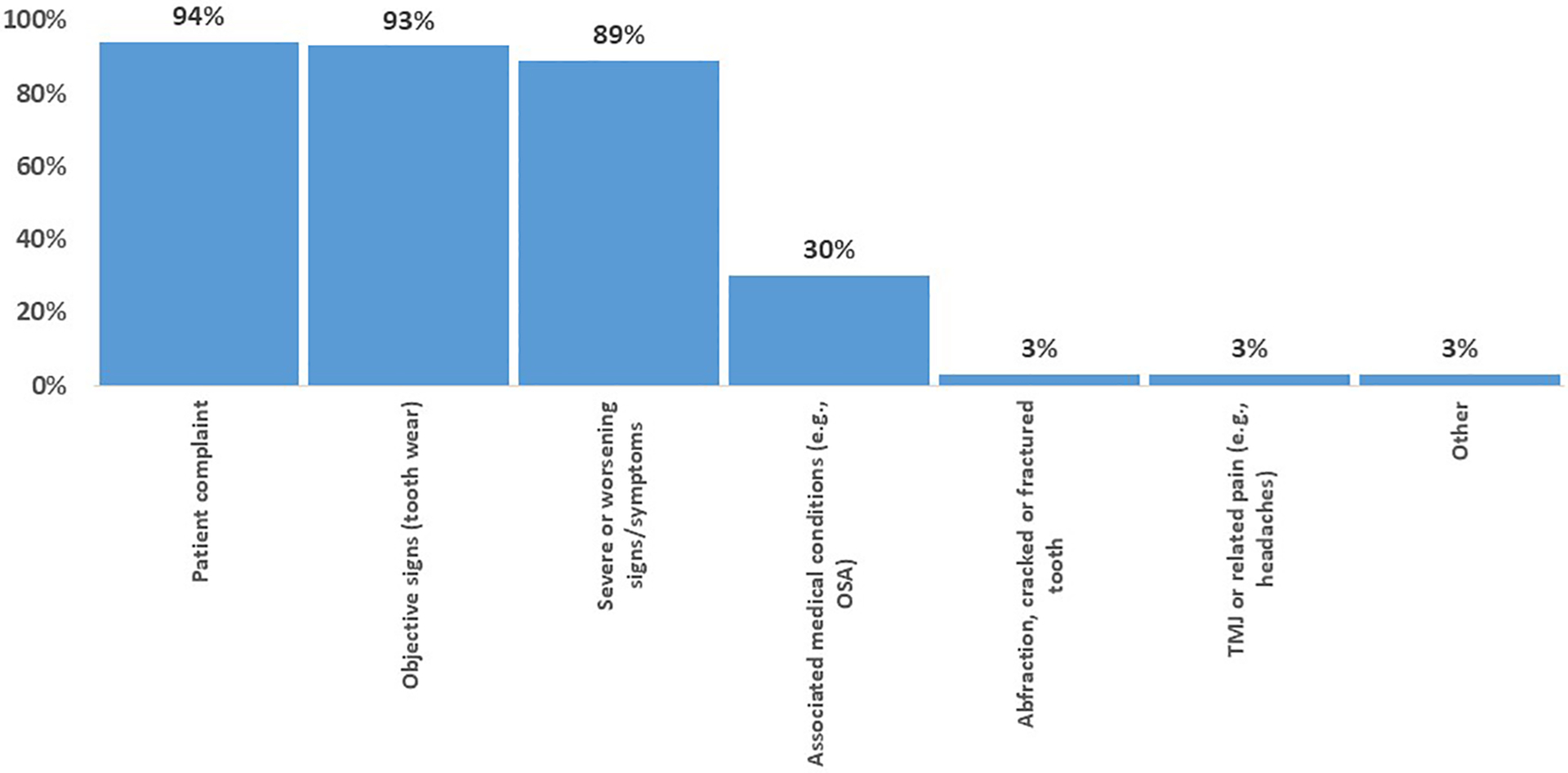
Criteria for intervening for bruxism treatment* (N=395)
*Check all that apply
Nearly all practitioners offered occlusal guards or appliances (96%, n=379) as the primary treatment option for patients with bruxism. More than half of the respondents (52%, n=207) stated they would refer a patient to a specialist (e.g., sleep specialist, orofacial pain specialist, chiropractor), followed by 46% of the practitioners (n=182) who would perform an occlusal adjustment. Also, 37% (n=146) and 28% (n=112) of the respondents stated, respectively, that stress management and physical therapy were indicated, and 24% (n=95) responded that medication could be an option. A few (3%, n=10) indicated that they offered their patients education, exercise, hot/cold treatments, or other treatments not listed in the questionnaire (7%, n=27) (Figure 3). Lastly, most (83%, n=329) participants agreed that a study about bruxism would be important to them and their patients (Figure 3).
Discussion
This study aimed to investigate dental practitioners’ approaches regarding bruxism and their encounters with bruxism within their practices. Perspectives regarding etiological factors, decision-making regarding bruxism treatment, and the importance of future research were queried. The questionnaire indicated that 1) over one-third of the practitioners initiated treatment for bruxism on four or more patients a month; 2) a large majority of patients’ stress levels and sleep patterns/apnea were believed to affect bruxism by practitioners; 3) patient complaints, objective signs such as tooth wear and worsening of signs/symptoms were criteria for treating; 4) occlusal guards were a treatment they offered frequently; 5) a study about bruxism would be important to them and their patients. The overall purpose of this research is to utilize the data collected from this poll to develop educational strategies and future research studies, intending to develop a standardized protocol for assessing and managing bruxism in general dental practices.
Treatment for Bruxism Initiated Monthly by Dental Practitioners
These Quick Poll results show that many respondents treat a significant number of new bruxism patients per month (up to seven patients). This is important because it reflects the level of experience practitioners have with recognizing/addressing bruxism cases and treating them clinically. Since this Quick Poll was conducted in 2015, dental practitioners may currently recognize more or fewer bruxism patients in their practices. Therefore, these numbers may have changed and may not accurately reflect bruxism today. Hence the study is representative of a historical state than of the current situation yet provides valuable data from PBRN Network dental practitioners. Furthermore, in 2020, the Google search volume for bruxism and its related keywords increased during the COVID-19 pandemic, indicating the increasing public demand and concern about the topic.13 Due to this growing awareness of bruxism among patients, practitioners must be trained in evolving evidence to assess and manage patients with bruxism confidently.
Factors Dental Practitioners Believe Affect Bruxism
This Quick Poll question was intended to understand practitioners’ opinions on the factors that affect bruxism. One etiological factor recognized by most practitioners is certain sleep patterns. This demonstrates an understanding of when sleep bruxism behavior occurs. In a study attempting to determine the relationship between obstructive sleep apnea (OSA) and SB, investigators concluded that the relationship depends on the severity of OSA.14 Results from the study’s Quick Poll indicated that most respondents understand the relationship between sleep apnea and bruxism behavior as supported by the literature. However, since this was not asked in the questionnaire, the overall answers did not indicate whether practitioners actually understood that bruxism associated with OSA could benefit the individual patient, with a possible role for MMA in maintaining upper airway patency.15
The Quick Poll findings are consistent with conclusions made from a literature review that explains how stress and other pathological emotional experiences could influence the development of bruxism.16,17 This insight reinforces the importance of addressing the psychosocial factors affecting bruxism when practitioners consider the different treatments to offer to patients. Interestingly, the Quick Poll identified that psychosocial factors (stress), sleep patterns, and sleep apnea were treated with an occlusal guard/appliance (widely referred to as oral splints), while fewer than half were recommended for behavioral therapy. Only 4% (n=17) of respondents indicated that medications could affect bruxism, consistent with literature that suggests that there is insufficient evidence‐based data to draw definite conclusions concerning medications and addictive substances inducing, aggravating, or attenuating SB and or AB.18
Dental Practitioner’s Criteria for Intervening for Bruxism Treatment
Most practitioners assess bruxism by evaluating objective signs (e.g., tooth wear). Furthermore, most practitioners offered the interventional use of occlusal splints. The goal possibly was to prevent further damage, yet it does not address the bruxism behavior. This is supported by a survey conducted in Sweden which demonstrated that dental practitioners considered the first indication for hard interocclusal appliances was to protect dentition from wear.19,20 However, these appliances are not curative or effective in treating bruxism behavior; they only reduce the destructive effects of the behavior on the dentition.19,21,22 Surprisingly, 7% (n=27) of practitioners did not examine the tooth wear of a patient with bruxism, possibly because some patients don’t show signs of tooth wear, and for some, “bruxism” refers to grinding/sleep-related behaviors known to damage teeth. Furthermore, 3% (n=10) of the practitioner’s TMJ or related pain (e.g., headaches) was a criterion for treating bruxism. This is well supported by science that indicates further research is needed in this area and that no clear cause-and-effect relationship is demonstrated between bruxism and TMD.23–25
Treatment Dental Practitioners Offer When Treating Patients with Bruxism
Nearly half of the respondents reported performing occlusal adjustments, which contrasts with the recommendation in the literature against performing irreversible occlusal changes.7 In the past, occlusal imbalance was considered the main etiological factor for bruxism, so practitioners made occlusal adjustments to manage bruxism.26 According to multiple sources, irreversible occlusal adjustments have no supporting evidence from research about how best to manage bruxism.7, 27, 28 With little evidence to support this treatment option, it is difficult to deem it an effective management strategy for bruxism. Yet, many practitioners continue to perform it on their bruxism patients. This drives the need for a standardized protocol to assess and evaluate the management of bruxism in the dental field.
A significant number of the Network dental practitioners direct their patients elsewhere if they cannot, or choose not to, treat the patients themselves within their practice. This could be due to time constraints, assessment difficulties, or other reasons. Other approaches not mentioned in the Quick Poll include sleep hygiene and counseling, which are also treatment measures taken by some practitioners, as mentioned in the literature. These measures could be time-consuming, and practitioners may refer to specialists if indicated. These forms of therapy provide practical routines and habits to limit the risk factors for bruxing.5
Pharmacologic therapy has also been a heavily studied treatment strategy for SB. In a study presented by Lobbezoo et al., levodopa was administered to ten severe bruxers with a noticeable decrease in masticatory movement.29 However, levodopa is not considered a valid treatment option due to the lack of supporting research. Other tested treatments, including amitriptyline, bromocriptine, and propranolol, have been used in research studies and have been shown to be ineffective management for bruxism.5,30,31
Interestingly only 1% (n=3) of practitioners indicated that they offer doing-nothing (“none”) as a treatment option. According to the authors’ current understanding of bruxism, treatment should only be recommended when severe negative consequences outweigh positive consequences (weighted decision). Hence, this number should be much higher, which could indicate overtreatment.3,7 Given the wide variety of treatments offered to manage bruxism, the Quick Poll findings are consistent with the notion that no standardized approach exists and that future studies are needed.
Importance and Need for Bruxism Research
Quick Polls are developed to gauge interest and inform future studies. Hence, there are limitations to Quick Polls. Some questions were phrased in a way that may have been unclear or cause inconsistencies in responses among Network dental practitioners. There were also limitations in the collection and analysis of the data. For example, there was no confirmation of who received the newsletter and had an opportunity to respond. Also, there were categories of membership, one being “informational only”. Newsletters are sent to these members, but there is no expectation of a response. Because of these factors, the present study can only estimate a response rate. The 9% (397/4,355) is an underestimate of the true response rate, but it is an acknowledgment that the response rate is low. The number that responded (n=397) is comparable to what is typically received in the Quick Polls conducted by the Network. It is sufficient to quantify anecdotal information gleaned from discussions at Network’s regional meetings, primarily those that were conducted in the Southwest Region. As the responses to the Quick Poll were kept anonymous and lacked demographic data, the authors could not identify trends in individual responses and perform crosstabulations to identify groups and sub-groups among the respondents. The lack of demographic data also affected the ability to assess the sample’s representativeness. In addition, no information was collected on respondents’ age or years in practice. This information would allow us to look at the rates of treatment use by age groups, as dental schools have deemphasized invasive treatments like occlusal adjustments over the years.
Lastly, there were gaps in the information collected from this Quick Poll. For example, in the interest of the National Dental PBRN’s more extensive future study, it would have been beneficial to see how practitioners assess the presence and severity of bruxism. In addition, it is unclear whether respondents had children, adolescents, or adults in mind when answering questions about their patients. Furthermore in Question 4, it was unclear from the results obtained whether respondents used a range of multiple treatments or a select few within their expertise. Nonetheless, the Quick Poll successfully gauged Network practitioners’ interests and collected sufficient data to inform future studies.
Conclusion
There are many areas where the Quick Poll results are consistent with current research. Still, the study’s diverse responses among Network dental practitioners for factors they believe affect bruxism and treatment choices/offered reveal and reflect the inconsistencies in practitioner approaches. Hence, the preliminary results obtained from this Quick Poll are a crucial first step to prepare for future studies intending to develop a standardized protocol for assessing and managing bruxism in general dental practices. Further, the Quick Poll shows the need to address the gaps in practitioners’ approach on bruxism to improve the efficiency of providing dental care.
Acknowledgments:
Funding information:
This work was supported by NIH grant U19-DE-28717. Opinions and assertions contained herein are those of the authors. They are not to be construed as necessarily representing the views of the respective organizations or the National Institutes of Health. An Internet site devoted to details about the nation’s Network is located at http://NationalDentalPBRN.org. Finally, the authors gratefully acknowledge all the Network practitioners who responded to the Quick Poll, of which the results were used in this work.
Abbreviations:
- PBRN
Practice-Based Research Network
- MMA
Masticatory muscle activity
- SB
Sleep bruxism
- AB
Awake bruxism
- TMJ
Temporomandibular joint
- OSA
Obstructive sleep apnea
Footnotes
Disclosure of interest: The authors report no conflict of interest.
Data availability statement:
The data that support the findings of this study are openly available at nationaldentalpbrn.org
References:
- 1.Lobbezoo F, Ahlberg J, Raphael KG, Wetselaar P, Glaros AG, Kato T, et al. International consensus on the assessment of bruxism: Report of a work in progress. J Oral Rehabil. 2018;45(11):837–844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ahlberg J, Piirtola M, Lobbezoo F, Manfredini D, Korhonen T, Aarab G, et al. Correlates and genetics of self-reported sleep and awake bruxism in a nationwide twin cohort. J Oral Rehabil. 2020;47(9):1110–1119. [DOI] [PubMed] [Google Scholar]
- 3.Manfredini D, Colonna A, Bracci A, & Lobbezoo F. Bruxism: A summary of current knowledge on aetiology, assessment, and management. Oral Surg. 2020;13(4), 358–370. [Google Scholar]
- 4.Lobbezoo F, Naeije M. Bruxism is mainly regulated centrally, not peripherally. J Oral Rehabil. 2001;28(12):1085–1091. [DOI] [PubMed] [Google Scholar]
- 5.Shetty S, Pitti V, Satish Babu CL, Surendra Kumar GP, Deepthi BC. Bruxism: a literature review. J Indian Prosthodont Soc. 2010;10(3):141–148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Raphael KG, Santiago V, Lobbezoo F. Is bruxism a disorder or a behaviour? Rethinking the international consensus on defining and grading of bruxism. J Oral Rehabil. 2016;43(10):791–798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Manfredini D, Ahlberg J, Winocur E, Lobbezoo F. Management of sleep bruxism in adults: a qualitative systematic literature review. J Oral Rehabil. 2015;42(11):862–874. [DOI] [PubMed] [Google Scholar]
- 8.Lobbezoo F, Aarab G. The global oral health workforce. Lancet. 2021. Dec 18;398(10318):2245. [DOI] [PubMed] [Google Scholar]
- 9.Lobbezoo F, Aarab G. Medicine and dentistry working side by side to improve global health equity. J Dent Res 2022;101(10):1133–1134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mungia R, Funkhouser E, Makhija SK, Reyes SC, Cohen RA, Cochran DL, et al. Practitioner Engagement in Activities of the National Dental Practice-Based Research Network (PBRN): 7-Year Results. J Am Board Fam Med. 2020;33(5):687–697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mungia R, Funkhouser E, Buchberg Trejo MK, Cohen R, Reyes SC, Cochran DL, et al. Practitioner Participation in National Dental Practice-based Research Network (PBRN) Studies: 12-Year Results. J Am Board Fam Med. 2018;31(6):844–856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gilbert GH, Fellows JL, Allareddy V, Cochran DL, Cunha-Cruz J, Gordan VV, McBurnie MA, Meyerowitz C, Mungia R, Rindal DB, National Dental PBRN Collaborative Group. Structure, function, and productivity from the National Dental Practice-Based Research Network. J Clin Transl Sci. 2022;6(1):e87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kardeş E, Kardeş S. Google searches for bruxism, teeth grinding, and teeth clenching during the COVID-19 pandemic [published online ahead of print, 2021 Jun 29]. Google-Suchanfragen zu Bruxismus, Zähneknirschen und Zähnepressen während der COVID-19-Pandemie [published online ahead of print, 2021 Jun 29]. J Orofac Orthop. 2021;1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Martynowicz H, Gac P, Brzecka A, Poreba R, Wojakowska A, Mazur G, et al. The Relationship between Sleep Bruxism and Obstructive Sleep Apnea Based on Polysomnographic Findings. J Clin Med. 2019;8(10):1653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Manfredini D, Guarda-Nardini L, Marchese-Ragona R, Lobbezoo F. Theories on possible temporal relationships between sleep bruxism and obstructive sleep apnea events. An expert opinion. Sleep Breath. 2015;19(4):1459–1465. [DOI] [PubMed] [Google Scholar]
- 16.Wieckiewicz M, Paradowska-Stolarz A, Wieckiewicz W. Psychosocial aspects of bruxism: the most paramount factor influencing teeth grinding. BioMed Res Int. 2014;2014:469187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Manfredini D, Lobbezoo F. Role of psychosocial factors in the etiology of bruxism. J Orofac Pain. 2009;23(2):153–166. [PubMed] [Google Scholar]
- 18.de Baat C, Verhoeff M, Ahlberg J, Manfredini D, Winocur E, Zweers P, Rozema F, Vissink A, Lobbezoo F. Medications and addictive substances potentially inducing or attenuating sleep bruxism and/or awake bruxism. J Oral Rehabil. 2021. Mar;48(3):343–354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Johansson A, Omar R, Carlsson GE. Bruxism and prosthetic treatment: a critical review. J Prosthodont Res. 2011;55(3):127–136. [DOI] [PubMed] [Google Scholar]
- 20.Lindfors E, Magnusson T, Tegelberg A. Interocclusal appliances – indications and clinical routines in general dental practice in Sweden. Swed Dent J. 2006;30(3):123–134. [PubMed] [Google Scholar]
- 21.Hardy RS, Bonsor SJ. The efficacy of occlusal splints in the treatment of bruxism: A systematic review. J Dent. 2021;108:103621. [DOI] [PubMed] [Google Scholar]
- 22.Jagger R The effectiveness of occlusal splints for sleep bruxism. Evid Based Dent. 2008;9(1):23. [DOI] [PubMed] [Google Scholar]
- 23.Lobbezoo F, Lavigne GJ. Do bruxism and temporomandibular disorders have a cause-and-effect relationship? J Orofac Pain. 1997;11(1):15–23. [PubMed] [Google Scholar]
- 24.Manfredini D, Lobbezoo F. Relationship between bruxism and temporomandibular disorders: a systematic review of literature from 1998 to 2008. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010. Jun;109(6):e26–50. [DOI] [PubMed] [Google Scholar]
- 25.Manfredini D, Lobbezoo F. Sleep bruxism and temporomandibular disorders: A scoping review of the literature. J Dent. 2021. Aug;111:103711. [DOI] [PubMed] [Google Scholar]
- 26.Mesko ME, Hutton B, Skupien JA, Sarkis-Onofre R, Mohr D, Pereira-Cenci T. Therapies for bruxism: a systematic review and network meta-analysis (protocol). Syst Rev 6. 2017;6(1):4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Beddis H, Pemberton M, Davies S. Sleep bruxism: an overview for clinicians. Br Dent J. 2018;225(6):497–501. [DOI] [PubMed] [Google Scholar]
- 28.Lobbezoo F, Ahlberg J, Manfredini D, Winocur E. Are bruxism and the bite causally related? J Oral Rehabil. 2012;39(7):489–501. [DOI] [PubMed] [Google Scholar]
- 29.Lobbezoo F, Lavigne GJ, Tanguay R, Montplaisir JY. The effect of catecholamine precursor L-dopa on sleep bruxism: a controlled clinical trial. Mov Disord. 1997;12(1):73–78. [DOI] [PubMed] [Google Scholar]
- 30.Mohamed SE, Christensen LV, Penchas J. A randomized double-blind clinical trial of the effect of amitriptyline on nocturnal masseteric motor activity (sleep bruxism). Cranio. 1997;15(4):326–332. [DOI] [PubMed] [Google Scholar]
- 31.de Baat C, Verhoeff M, Ahlberg J, Manfredini D, Winocur E, Zweers P, et al. Medications and addictive substances potentially inducing or attenuating sleep bruxism and/or awake bruxism. J Oral Rehabil. 2021;48(3):343–354. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are openly available at nationaldentalpbrn.org


