Abstract
Introduction
Travelling for cancer treatment comes with unique challenges, particularly for a young patient and his or her family. The aims of this study were to (1) gain an understanding of the experiences of families and patients who travelled overseas (OS) from Australia for proton beam therapy (PBT) and (2) identify the supportive care needs patients and their families require when living away from home, while having PBT.
Methods
This was a retrospective, qualitative study using semi‐structured interviews, conducted with participants aged under 25 years and their families who travelled OS for PBT between 2017 and 2020. Data were analysed using Microsoft Excel Software, where key themes were identified and coded based on their responses. A total of 17 participants were included in interviews from seven Australian families who travelled to America or Europe for PBT.
Results
The majority of participants reported a lack of coordination with travel and treatment arrangements prior to arrival OS. Families who stayed in hotel accommodation while OS reported greater feelings of isolation compared with those who stayed in share house‐style accommodation. The acuity of cancer diagnosis played a significant part in patient experience, with those patients requiring the greatest amount of supportive care and availability of service provision at stand‐alone centres reporting a lack of appropriate care provision.
Conclusions
This study has identified services, accommodation provisions and care coordination requirements that are largely missing from the travel and treatment experience in patients travelling OS for PBT. Future use of consumer‐led working groups or committees in creating models of care for families travelling for PBT treatment could be advantageous, with many families willing to share their experiences and provide support to others who are travelling for PBT.
Keywords: Oncology, proton therapy, radiation, radiotherapy, travelling for cancer treatment
This study examined the experiences of families and young cancer patients who travelled overseas for proton beam therapy. It identified challenges in the coordinating travel and treatment process. The research highlights the need for improved care provision and support for families travelling for PBT treatment and suggests the use of consumer‐led working groups to create models of care.
Introduction
Proton beam therapy (PBT) is a specialised form of radiation therapy used to treat cancer. Due to its unique physical properties, PBT takes advantage of the Bragg peak in which radiation dose is deposited directly at the tumour location with significantly more sparing of normal tissues. This is compared to conventional photon treatment, which utilises high‐energy x‐ray beams to deliver a therapeutic dose by traversing all tissues, 1 which inadvertently has the potential to deliver higher doses to nearby, uninvolved tissues that may lead to a higher rate of acute and late effects. PBT is particularly useful in the treatment of paediatric, adolescent and young adult (AYA) patients, who are at greater risk of long‐term treatment toxicity due to longer survivorship during which late radiation effects manifest. 2
With no PBT treatment centres open in Australia, cancer patients currently seeking access to PBT either self‐fund or apply to the Medical Treatment Overseas Program (MTOP) for funding. MTOP is an Australian Federal Government program that provides financial assistance for Australian residents with either a life‐threatening or life‐limiting medical condition to enable treatment overseas (OS) when an effective treatment alternative is not available in Australia. Families are able to make an application to MTOP to support the cost of treatment, accommodation and airfares for the patient and one support person. 3 Since 2016, the Royal Adelaide Hospital (RAH) has provided a photon versus proton comparative (radiation therapy treatment) planning service, comparing these two treatment modalities (i.e. demonstrating the benefits of PBT over high‐energy x‐rays) to accompany applications for MTOP financial support. Over a two‐year period, a total of 43 patients were referred to this service, 19 of these referrals resulting in applications to MTOP and following review by MTOP, 16 of these applications received approval and subsequently travelled OS for PBT. 4
Paediatric, AYA patients and their families have a distinct set of challenges they face when given a cancer diagnosis, with research concluding that a supportive care model of practice is required to best support this cohort of patients. 5 , 6 , 7 A systematic literature review identified there are no publications investigating the experiences of Australian patients and their families travelling OS for PBT. Publications within the scope of travelling for treatment reported the economic burden for rural and remote Australian patients travelling to urban centres for radiation or cancer treatment but did not specifically include patients travelling OS. This review identified a significant gap in the literature regarding the perceived experiences of patients and their families who have travelled both OS and nationally for not only PBT but also cancer treatment in general and what support structures were available.
Australia's first PBT centre, the Australian Bragg Centre for Proton Therapy and Research (ABCPTR) is currently under construction in Adelaide, South Australia. It is anticipated that many paediatric and AYA Australian residents and their families will travel interstate to South Australia for this specialised treatment. Patient modelling completed by the ABCPTR indicates that approximately 60% of patients are expected to be under 25 years of age and 10% are likely to be South Australian residents. 8 , 9 , 10 , 11 This highlights an important area of study that needs to be understood if the distinct set of challenges, burden of travel and supportive care needs of these patients is to be met.
The aims of this study were to (1) gain an understanding of the experiences of families and patients who travelled overseas (OS) from Australia for proton beam therapy (PBT) and (2) identify the supportive care needs patients and their families require when living away from home while having PBT.
Materials and Methods
Study design
This was a retrospective, multiple case study, interviewing families who supported a paediatric patient, aged under 18 years at the time of PBT and two patients aged under 25 years and their family members who travelled OS for PBT between 2017 and 2020. Interviews were conducted with semi‐structured questions and themes to elicit organic conversations from patients and their families who had travelled OS. Interviews were conducted by a single researcher, experienced in radiation oncology nursing, care coordination and data management. A critical realist approach was used to engage patients and families and allow them to share their first‐hand experience in order to understand the complexity of providing care to patients travelling for cancer treatment. This approach helped capture the complex and dynamic nature of the patients and family experience, as well as explore the broader provisions of care required when travelling for cancer treatment. 12 To ensure robustness and dependability of the findings, the researcher followed a rigorous methodology. Among measures taken was a consistent application of interview questions and themes to all participants (Appendix S1). By seeking responses to the same themes, the researchers were able to maintain consistency in the data collected and subsequent analysis. This approach reduced potential bias in the study and allowed for more reliable comparisons and conclusions. Sufficient coverage on the research topic was considered when no new information or insights were emerging through the interviews. 13 Reporting and research procedures followed the consolidated criteria for reporting qualitative research guidelines (COREQ). 14
Ethical considerations
The study was reviewed and approved by the Central Adelaide Local Health Network (CALHN) Human Research Ethics Committee (HREC)‐2021 – HREC reference number 14790.
Participants and recruitment
Families were identified from the RAH comparative planning service, who subsequently travelled OS for PBT. Treating clinicians were approached to confirm that patient contact details were still current and that the patient and family were appropriate to approach.
Approved participants were contacted by telephone, informed of the research study and, with verbal consent, emailed the participant information sheet. All participants who received information sheets consented to be interviewed.
Data collection and analysis
Interviews were conducted between June and October 2021. Recorded interviews were subsequently dictated into verbatim scripture transcripts using Microsoft Word dictation software. Participants were assigned a unique identifier, identifiable scripture was removed, and interviews were stored on firewall, password‐protected electronic files. Participants were not provided with transcripts for comment or correction. In order to ensure robustness and methodological rigour, the data collected from participants were coded, based on key themes that encompassed crucial aspects to the responses provided to the questions asked in the interviews and subsequent discussions that took place. These included prior PBT knowledge, length of treatment versus length of stay, accommodation and overall financial, employment and/or educational impact on participants. These common themes were tabled both individually and grouped together as themes and descriptive text used on what was considered participant impact statements.
Results
Participants
A total of nine families were approached, seven families consented to be interviewed, two declined by way of no response to initial telephone call, voice mail message and one further follow‐up telephone call. An additional four families were unable to be approached in time due to a delayed response from the referring clinician and seeking local governance input. It is worth noting that this health service was experiencing governance and operational delays due to the COVID‐19 pandemic, and this impacted their ability to respond in what would usually be considered a timely manner. Data saturation was also considered achieved at this point, and the additional four participants were unlikely to add any further information, change the findings or enhance the research and were omitted from the participants to approach list. 13
Table 1 outlines the participant and interview characteristics; a total of six interviews were completed via online video platforms, depending on the participant preference, and four interviews were completed over the telephone. Written consent was given by 6 participants and 11 provided verbal consent at the start of their voice recording.
Table 1.
Participant and interview characteristics.
| Participant | Interview characteristics |
|---|---|
| 1. AYA patient |
Individual Interviews Via online platform Recorded Patient Mother Father |
| 2. AYA patient |
Individual Interviews Via online platform Recorded Patient Mother |
| 3. Paediatric patient |
Family Interview Via phone Recorded Mother Father |
| 4. Paediatric patient |
Family Interview Via online platform Recorded Mother Father Grandmother |
| 5. Paediatric patient |
Family Interview Via online platform Recorded Mother Father Stepfather |
| 6. Paediatric patient |
Family Interview Via online platform Recorded Mother Father |
| 7. Paediatric patient |
Family Interview Via phone Scribed Mother Father |
In total, 17 participants were included in interviews from 7 families in this study, 10 separate interviews were completed, 5 interviews were conducted with individuals and 5 as a family unit. The breakdown, as described in Table 1, included two adolescent and young adult (AYA) patients and their three parents who travelled with them as a support person. In addition, 11 parents and 1 grandparent of 5 paediatric patients who travelled overseas for their child/grandchild to have proton therapy. All participants, including those in a family unit, provided responses to the themes covered based on their own individual experiences in travelling OS as a family unit. Participants were given the option to have their interviews voice recorded or dictated in verbatim scripture with a total of 15 participants electing to have their interviews recorded and two participants scribed. Average interview times ranged from 45 to 90 min. Interviewed participants either had or were supporting their family member (patient) receiving PBT for a central nervous system (CNS) cancer diagnosis. Patients, who received PBT, ranged in age from 3 to 23 years at the time of treatment, with the median age being 11 years. The average length of time between treatment and interview was 3 years.
Prior PBT experience or knowledge
Only one of the seven families interviewed had any previous experience or knowledge of PBT, with four of the families, suggesting they were made aware of PBT through online cancer support groups and then discussed PBT with their treating team. Additionally, two families were made aware of PBT from their treating radiation oncologist who suggested an MTOP application should be made.
MTOP and funding
All families applied for MTOP funding with six of the seven families interviewed travelling with MTOP support. The average length of time for MTOP application to approval ranged from 4 to 16 weeks, with the median time, 7 weeks. Turnaround times between MTOP approval and subsequent travel OS for PBT was short, with families travelling between 1 and 4 weeks from time of approval. Many of the families interviewed also raised additional funding for their OS travel, utilising an online crowd funding platform. A total of four families raised additional funding using this method.
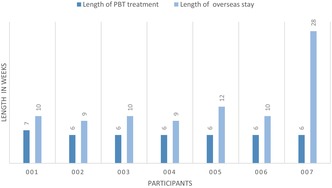
Previous overseas travel experience and length of stay
Of the 17 participants interviewed, 14 had previous experience in travelling OS and did not require passport applications. Average length of PBT for the patient was 6 weeks while average length of OS stay was 12.5 weeks (range 9–28 weeks) (Fig. 1).
Figure 1.
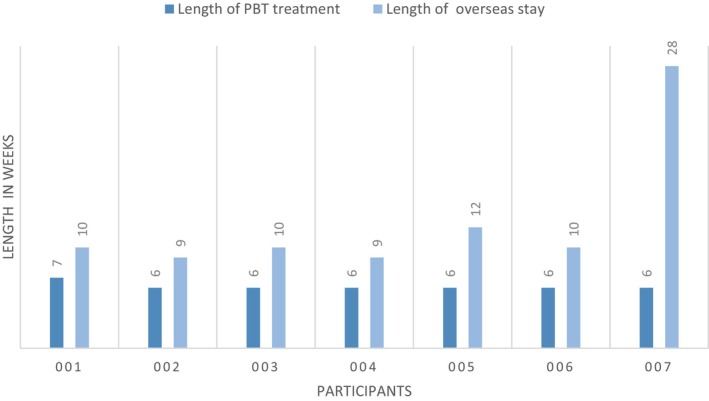
Length of PBT treatment vs Length of Stay (overseas).
MTOP and treatment centre coordination
All families reported a perceived lack of coordination with MTOP and the OS treatment centre prior to arrival. MTOP provided flight details and centres provided a point of contact, usually via email. Emails provided instructions for transport pick up at airport upon arrival, accommodation details and relevant appointment times. Families reported little opportunity to ask questions, leaving families feeling unprepared, which caused significant distress for most participants as outlined in Table 2 – Participant Quotes.
Table 2.
Participant responses to interview questions (Theme).
| Interview Theme | Participant Response As Quote |
|---|---|
| Medical Treatment Overseas Program and Treatment Centre Coordination |
‘There was no pre planning around that (proton treatment overseas) other than organising our hotel for example, there was no other pre planning around our trip, it was quite abrupt’. ‘It was a short timeline, and it was obviously a very stressful time – the time did fly and there wasn't much opportunity for what we might call patient care around the treatment elements and what to expect for treatment, that may have been a support for the anxiety we were feeling’. ‘I could have been better supported if I had known what it is like. But no one can prepare you for that kind of thing’. |
| Transit, Flights and Arrival |
‘I had a miserable traumatic time; it does not really matter how great the team at the end point is if the journey is unorganised and distressing’. ‘I had a meltdown, I just had a meltdown when we got there, it was really overwhelming – crying. I had no idea what we needed to do’. ‘Getting in late from the flight and arriving at the accommodation, we had no milk, we did not know if we could drink the tap water ‐ no nothing and we were not even able to provide breakfast for our child ‐ we did not know where anything was nearby’ |
| Support and isolation |
‘Because they kept changing the treatment times, I'd be meeting different people. I just got too tired talking; you could not build a connection in 10 weeks with anyone cause the times changed’ ‘It was just really hard to try to be strong. I just felt so alone. If it wasn't for the other Australian family that was there, I would've, I just do not know how I would've got through it’ ‘I had to be strong for her and carry her through when she was down depressed or crying, wasn't eating but I had no one I could talk to about it’ |
| Proton Beam Therapy Treatment Centre |
‘Once treatment started it was all good ‐ it was just all the unknowingness prior ‐ leading up to leaving’. ‘All service provisions seemed to be on an asked basis ‐ if you did not ask you did not get’ ‘She was just putting on so much weight from the steroids, it would have been great to speak to a dietitian’ ‘It's taken over a year to come back from our ordeal, but to be fair, I actually do not think that place (treatment centre) was set up for someone so ill, they had mostly men coming in with prostate cancer’ |
Transit, flights and arrival
One family shared an experience in transit to an OS treatment centre, including a lack of adequate mobility provisions organised at the airports. Heightened by a pain crisis due to lengthy periods of sitting and separation from their travelling support person due to airport restriction and mobility access. Other families reported issues with allowable baggage, restrictions on baggage and medication approvals. A lack of coordination and information sharing from MTOP booking flights versus family's needs was identified as a key contributor to this lack of adequate provision. Many of the families shared stories about the ‘unknown’ when they arrived – what to expect from accommodation, treatment centre and the overall impact this had on them feeling ‘prepared’.
Support and Isolation
All of the interviewed participants acknowledged the support they got from other families who they met through the treatment centre or their accommodation, with many reporting these families were a great support for sharing of knowledge and general emotional support. Those families staying in shared accommodation relied greatly on the other families who were also staying in the accommodation for various medical treatments at the nearby hospital or care facilities, while those staying in private hotel accommodation relied on other patients having PBT who they met at the treatment centre. Four of these families travelled as a family unit, two families had additional family members visit for a short period of the treatment time, and one family travelled as a patient and parent. Table 2 describes how the constant change in treatment times affected one participant's ability to seek support through connection.
Accommodation
Of the seven families interviewed, three stayed in shared housing, charity or not‐for‐profit provided accommodation. An additional three families stayed in hotel or apartment‐type accommodation. A family expressed how if they could go back, they would stay in shared accommodation. There was one family who initially stayed in hotel accommodation and moved to shared housing when a room became available for increased support. Those who stayed in hotel accommodation reported greater moments of isolation and a perceived lack of support while those that stayed in shared accommodation felt greater supported.
Bringing small children from the treatment facility to nearby accommodation post‐treatment and general anaesthetic, meant families often had to carry their children. Many of the supported shared housing had prams or trolley's that families could use free of charge, while hotel or apartment accommodation did not provide this.
An advantage to hotel or apartment accommodation was the ability for families to cook for themselves in their rooms with many treatment centres or hotels providing hire or loan kitchen appliance facilities – like blenders, rice cookers or slow cookers. Often these items were left behind and donated by other families, items also included deck chairs, picnic baskets and rugs or leisure activity equipment.
PBT treatment centre
Families expressed an overall positive experience with their treatment centre; however, care provision between families differed greatly, even within the same treatment centre as described in Table 2. Of the seven families interviewed, five had treatment in centres based in the United States of America and two travelled to European centres who are capable of providing PBT to all international patients, not just those with Australian residency. Families welcomed the information sessions held by clinicians that were available during child treatment times on PBT and available tours of the treating facility after hours, allowing families to see ‘behind the scenes’. There was a perceived lack by three families in available support or allied health services within treatment centres. Families requiring physiotherapy, occupational therapy and dietetic input during their treatment found there was no availability of these services within the stand‐alone centres – those not affiliated with an acute care hospital.
All treatment centres provided local tourist‐based free ticketed activities for families, provided daily treatment incentives for young children by the way of a daily decorative bead to add to a necklace, or daily treatment sticker charts and treatment countdowns. Families spoke of the joy end of treatment rituals within centres brought them or their children, including ‘bell ringing’ with what was described as a team celebration for those completing treatment.
Two patients treated with PBT were recruited and treated as part of a clinical trial at an OS PBT centre. A total of three patients treated with PBT had a general anaesthetic each day as part of their course of treatment.
Work, education, family and financial impact
Generally, most families reported very little overall impact to their work situation. All travelling support people were supported by their workplace to either work remotely while OS, had enough paid leave to cover the time off or were already not working.
Of the seven families interviewed, one family had a child who was not of school age. Due to a perceived lack of support from the Australian education system and no support provided while on treatment, two of the participants needed to repeat their school year. It was observed that both patients had other treatment modalities included in their treatment protocol, which likely had an impact on their ability to attend school also. Two other participants were able to continue their schooling at the treatment facility, while another participant deferred their university studies for 1 year. Another young person continued their studies online throughout treatment and indicated it was a welcomed distraction from treatment.
All families reported some variation of disruption to the family unit, with many parents travelling together and leaving other children at home with family. Some of these families described missing significant birthdays, anniversaries or significant events for their other children and the impact this had on their family overall. One family with no other family able to provide care in Australia was forced to send their other small children OS with family for 3 months, while they supported their child OS.
With MTOP booking the flights for the patient and one additional support person, five of the seven families interviewed discussed the burden of matching flights for additional members of their travelling party with the flights booked from MTOP. The inability to liaise with MTOP for flight bookings created another layer of complexity for additional travelling support people, with many struggling to get on matching flights during peak periods.
Overall, many families were able to absorb the financial impact of travelling OS for PBT, with MTOP covering a significant portion of the financial burden, with flights and accommodation covered by the program. Those families who had crowdfunding pages were in a greater position than those who did not. It is worth noting that families usually started crowdfunding pages to raise funds for their child's PBT in the event the application with MTOP was declined. When the MTOP application was approved funds raised covered living expenses while away, supplemented any loss of income and facilitated additional family members to travel, providing much‐needed additional emotional support.
Follow‐up
Once arriving back in Australia, patient follow‐up from the treatment centres was largely completed by the referring Australian specialist, with only two of the families, suggesting they have had any further involvement with their PBT treatment centre. Both of these families were on clinical trials with the treatment centre.
Discussion
The present study reports the first insights into the experiences encountered by Australian families travelling OS for PBT. This extends on previous research of patients travelling to access cancer treatment. 15 , 16 , 17 , 18 , 19 Key findings in this study related to patient education and clinician knowledge of the benefits of PBT or its availability OS. An identified lack of coordination between MTOP approval and subsequent treatment, availability of service provision at the treating centre and the types of accommodation available for families were also common themes.
It is noteworthy that four of the seven families raised PBT with their clinician after being made aware of it through online social media groups. The small number of applications made to MTOP as identified by Hu et al compared with patient modelling done by the ABCPTR data suggests currently very few patients are being considered or applying for PBT through the MTOP process. 4 The reasons for this remain largely unknown, but may be explained by the time to apply for MTOP funding, the challenges associated with obtaining proton versus photon comparative studies to accompany the MTOP application, uncertainty of the MTOP and outcome, and hesitancy of families willing to travel OS, particularly during a global pandemic. The findings herein also highlight the importance of a PBT service locally to ensure greater access and equity of care.
An efficient approach to approval for PBT, eligibility criteria and patient education regarding the treating centre is required to provide a more coordinated approach to care. Notably, this lack of coordinated care had a profound impact on all families prior to their arrival at the treatment centre for PBT. This research suggests that a framework and program to assist families in their travel for PBT should be adopted and delivered in a timely manner, so families can feel an increased sense of understanding before they arrive at the treatment centre for their PBT. The optimisation of a coordinated model of care is an important consideration with patient modelling highlighting 10% of patients treated at the ABCPTR will be South Australian residents, indicating that the vast majority of patients will be travelling for their PBT. 11
PBT is largely given in the outpatient setting making provision of available wrap‐around support services centre specific. Those centres with an affiliation to a large acute care provider had the greatest level of supportive care service provision, with large groups of allied health teams available compared to those centres that were not associated with an acute care provider. Previous research in this area concluded that a lack in adequate service provision in outpatient settings not only creates concerns regarding patient safety but also has an impact on patient outcome and does not apply a holistic patient‐centred approach to care. 20
The type of accommodation families stayed in had a profound impact on their treatment journey, described isolation and perceived lack of support. With almost all families suggesting a preference to stay in shared, not‐for‐profit housing such as those provided by Ronald McDonald House. Previous research in this area shows that meeting accommodation needs of families is an effective way of enabling families to stay together while providing greater support by housing them in purpose‐built accommodation. 21
The main limitation of this study was relying on the historical recollection of family experiences and bares some inherent limitations of a qualitative approach, where findings were taken from a small number of interviewees. While data saturation was considered from the 17 participants, a larger family sample size may provide greater insight. The self‐reporting nature of the study also allows for a margin of feedback bias from the participant, while questions were semi‐structured, and participants were encouraged to discuss their overall experience it is worth recognising this as a potential limitation. Future studies should also consider the use of quantitative methods to validate these findings, including the examination of a consumer‐focused model of care that manages the expectations and needs of patients travelling for cancer treatment 22 Another limiting factor is the heterogeneous diagnoses of the participants in the study and the often‐complex treatment plans for these tumour streams, including systemic treatment. As identified, those patients that had experienced increased supportive care needs were those with greater acuity of care and treatment protocols potentially played a significant part in this.
Conclusion
The findings herein support future research into understanding the challenges associated with accessing and receiving PBT. Specifically, the study highlights two critical areas where significant gaps exist: the limited understanding of PBT among both consumers and clinicians in Australia, particularly in relation to its effective utilisation in specific tumour types, and the insufficient provision of services, accommodation and care coordination within the travel and treatment experience.
Further research is needed to elucidate travel experiences by following the patient journey, encompassing patient referral, end of treatment and treatment follow‐up experience. The use of healthcare facility consumer‐led working groups or committees currently being utilised in many clinical settings could be particularly advantageous, with participants willing to share their experiences and provide support to other families travelling for PBT. This could also provide valuable insight to enable individualised care planning for patients. An increase of support and a greater understanding can be achieved through this shared patient and family experience model of care.
Author Contributions
All authors have made significant contributions to the manuscript.
Conflict of Interest
Authors have declared no conflicts of interest.
Funding Information
There are no declarations of any financial support provided for this research or the manuscript.
Supporting information
Appendix S1 Interview questions/themes.
Acknowledgements
We would like to thank and acknowledge the families who shared their experiences in travelling overseas for proton beam therapy.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request
References
- 1. Targeting Cancer . What is Particle Therapy? [Cited 2023]. Available from: https://www.targetingcancer.com.au/radiation‐therapy/ebrt/proton‐therapy/.
- 2. ANSTO . Particle Therapy. 2020.
- 3. The Department of Health . Medical Treatment Overseas Program [Webpage]. 2016. Available from: https://www1.health.gov.au/internet/main/publishing.nsf/Content/guidelinesMTO.htm.
- 4. Hu Y, Dalfsen R, Penfold SN, et al. Comparative proton versus photon treatment planning for the Medicare Medical Treatment Overseas Program: The Royal Adelaide Hospital experience. J Med Imaging Radiat Oncol 2020; 64: 682–688. [DOI] [PubMed] [Google Scholar]
- 5. Bradford NK, Henney R, Walker R, et al. Queensland Youth Cancer Service: a partnership model to facilitate access to quality care for young people diagnosed with cancer. J Adolesc Young Adult Oncol 2018; 7: 339–348. [DOI] [PubMed] [Google Scholar]
- 6. Kinahan KE, Kircher S, Altman J, et al. Promoting the shared‐care model for adolescent and young adults with cancer: Optimizing referrals and care coordination with primary care providers. J Natl Compr Canc Netw 2017; 15: 38–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Johnson RH, Macpherson CF, Smith AW, Block RG, Keyton J. Facilitating teamwork in adolescent and young adult oncology. J Oncol Pract 2016; 12: 1067–1074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Australian Institute of Health and Welfare . Australia's health 2020 data insights. 2020.
- 9. Australian Institute of Health and Welfare . Cancer data in Australia. 2021. [cited 2021 August 23]. Available from: https://www.aihw.gov.au/reports/cancer/cancer‐data‐in‐australia/contents/cancer‐incidence‐by‐age‐visualisation.
- 10. Cancer Council . Australian Childhood Cancer Statistics Online 2021. [cited 2021 August 23]. Available from: https://cancerqld.org.au/research/queensland‐cancer‐statistics/accr/.
- 11. Jessop S, Penfold S, Gorayski P, et al. If we build it, will they come? Modeling of public hospital care requirements for the Australian Bragg Centre for Proton Therapy and Research. Asia‐Pac J Clin Oncol 2022; 19: 1–8. [DOI] [PubMed] [Google Scholar]
- 12. Mukumbang FC, Marchal B, Van Belle S, van Wyk B. Using the realist interview approach to maintain theoretical awareness in realist studies. Qual Res 2020; 20: 485–515. [Google Scholar]
- 13. Saunders B, Sim J, Kingstone T, et al. Saturation in qualitative research: exploring its conceptualization and operationalization. Qual Quant 2018; 52: 1893–1907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32‐item checklist for interviews and focus groups. Int J Qual Health Care 2007; 19: 349–357. [DOI] [PubMed] [Google Scholar]
- 15. Ugalde A, Blaschke S, Boltong A, et al. Understanding rural caregivers' experiences of cancer care when accessing metropolitan cancer services: a qualitative study. BMJ Open 2019; 9: e028315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Vindrola‐Padros C, Brage E, Chambers P. On the road and away from home: a systematic review of the travel experiences of cancer patients and their families. Support Care Cancer 2018; 26: 2973–2982. [DOI] [PubMed] [Google Scholar]
- 17. Payne S, Jarrett N, Jeffs D. The impact of travel on cancer patients' experiences of treatment: a literature review. Eur J Cancer Care 2000; 197: 197–203. [DOI] [PubMed] [Google Scholar]
- 18. Cockle SG, Ogden J. The 'radiation vacation': Parents' experiences of travelling to have their children's brain tumours treated with proton beam therapy. Health Psychol Open 2016; 3: 2055102916649767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Fitch MI, Gray RE, McGowan T, et al. Travelling for radiation cancer treatment: patient perspectives. Psychooncology 2003; 12: 664–674. [DOI] [PubMed] [Google Scholar]
- 20. Nancy FB, Molly FB, Wanda KN, Mindy S, Richard DU, Sarah CMR. The effect of facility characteristics on patient safety, patient experience, and service availability for procedures in non‐hospital‐affiliated outpatient settings: A systematic review. PloS One 2018; 13: e0190975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Rubin N, Franck L. The Role of Ronald McDonald House Charities® in Keeping Families Close. Pediatr Nurs 2017; 43: 202–205. [Google Scholar]
- 22. Carrigan A, Roberts N, Clay‐Williams R, et al. Innovative models of care for the health facility of the future: a protocol for a mixed‐methods study to elicit consumer and provider views. BMJ Open 2022; 12: e059330. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1 Interview questions/themes.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request


