ABSTRACT
Objective:
This study aimed to introduce and evaluate the feasibility and outcomes of a novel surgical technique, robot-assisted Foley tie ureteric tapering (RAFUT) and reimplantation, specifically designed for intravesical ureteral tapering during pediatric robotic-assisted ureteric reimplantation.
Materials and Methods:
A retrospective analysis was conducted on pediatric patients diagnosed with primary vesicoureteric reflux (VUR), who underwent RAFUT between January 2019 and July 2021. Patient records were reviewed to assess preoperative characteristics, operative details, and postoperative outcomes. RAFUT involved meticulous patient positioning, precise port placement with a 6 mm separation, and bladder anchoring to maintain pneumovesicum. Ureteric tapering was performed with the Foley tie technique to enhance surgical precision. The primary outcome measures included operative time, complications, and postoperative VUR resolution.
Results:
All four patients underwent successful intravesical RAFUT without any intraoperative or postoperative complications. The age of the patients ranged from 3 to 12 years, with varying bladder capacities (range: 210–550 mL). The operating times ranged from 180 to 210 min, and the estimated blood loss was 35–50 mL. None of the patients required conversion to open surgery. Patients demonstrated resolution of VUR on postoperative imaging, and none experienced recurrent urinary tract infections during follow-up, which ranged from 1.5 to nearly 4 years.
Conclusion:
RAFUT represents a safe and effective surgical technique for intravesical ureteral tapering during pediatric robotic-assisted ureteric reimplantation. This innovative approach addresses the challenges posed by intravesical surgery for dilated ureters, maintains anatomical orientation, and offers precise excision and suturing capabilities.
KEYWORDS: Foley tie, intravesical ureteric reimplantation, robotic surgery, ureteric tapering
INTRODUCTION
Ureteric reimplantation, a surgical procedure for the correction of vesicoureteric reflux (VUR) and primary obstructive megaureter, has seen significant advancements in recent years particularly with the introduction of laparoscopy and robotic techniques. A significant challenge is encountered while reimplanting massively dilated ureters that lack coaptation owing to the large diameter of the ureters. While various techniques for ureteral tapering and reimplantation have been described, they are primarily designed for extravesical reimplantation, leaving a significant gap in the literature for effective intravesical tapering methods.[1,2,3,4]
Traditionally, intravesical ureteral tapering has been challenging due to inherent limitations posed by the pediatric bladder’s confined working space, and extravesical reimplantation is more popular. Although excisional tapering can be performed laparoscopically, the extravesical approach is associated with complications such as bladder spasms and bladder dysfunction, particularly when done bilaterally.[4] Intracorporeal-extravesical excisional tapering involves dissecting and tapering the ureter outside the bladder, which can be technically demanding and may not be suitable for all cases. The robotic approach facilitates tapering and suturing owing to the ergonomic advantage of the robot. However, excisional tapering in robotic-assisted intravesical ureteric reimplantation is again challenging due to the limitations of the working space.
Recognizing the need for an innovative and patient-specific approach, this research article introduces a novel technique in pediatric robotic ureteric reimplantation known as robot-assisted Foley tie ureteric tapering (RAFUT) and reimplantation. RAFUT is specifically tailored to address the challenges posed by intravesical reimplantation and not only liberates both robotic working arms but also significantly enhances maneuverability within the confined surgical field of the pediatric bladder.
MATERIALS AND METHODS
Patient selection and data collection
We conducted a retrospective review of patient records from our center’s hospital information system spanning from January 2019 to July 2021. The primary objective was to evaluate the preoperative and video graphic records of four pediatric patients who underwent RAFUT and reimplantation. This study cohort comprised three male patients and one female patient, with ages ranging from 3 to 12 years. The primary pathology in all cases was primary VUR. The preoperative evaluation included renal and bladder ultrasonography, voiding cystourethrogram (VCUG), and mandatory preoperative cystoscopy to establish the prerequisites for inserting the first robotic port.
Patient position and cystoscopy
Following induction under general anesthesia with caudal block, patients were positioned in the lithotomy position. Adequate padding was applied to pressure points. The initial cystoscopy served to exclude any obstructive pathology and reconfirm bladder capacity as predicted by the prior VCUG. Under cystoscopic guidance, the first transvesicoscopic robotic port was placed at the highest point of the dome of the full bladder. Surface markings of bony landmarks were then made to determine the approximate positions for subsequent port placements, with an aim to achieve at least 6 cm separation between ports [Figure 1].
Figure 1.
Bladder marking and port planning. (a) Bladder outline is marked during cystoscopy. (b) Adequate (minimum 6 mm) space is ensured between the camera port and the working ports. (c) Port planning for a typical patient (inset: actual image after port insertion). ASIS: Anterior superior iliac spine
Bladder hitch and port placement
A prerequisite for transvesicoscopic surgery was the creation of an individual bladder hitch at each port site to prevent bladder collapse leading to loss of pneumovesicum. To achieve this, the bladder was suspended from the abdominal wall when fully filled with normal saline under cystoscopic guidance. This was done using a 1-0 Polypropylene Loop passed through an 18-G cannula [Figure 2], which retrieved a hitch stitch of the same material passed through another similar cannula inserted adjacent to the first. Once the robust hitch stitch was confirmed, an incision was made to enter the bladder directly while ensuring suture integrity. The first 8-mm robotic port was then placed under the cystoscopic vision and secured in place using the intact Polypropylene hitch stitch.
Figure 2.
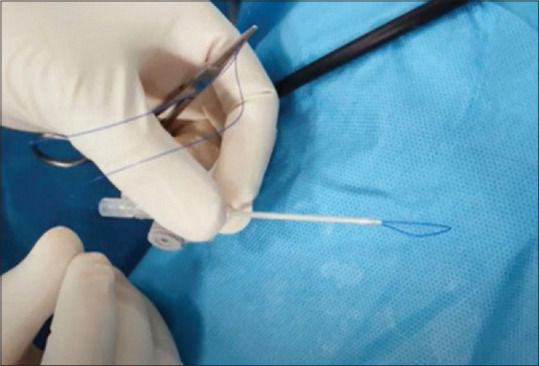
1-0 Polypropylene Loop passed through an 18-G cannula to retrieve the hitch stitch
Intraoperative setup and ureteric cannulation
The cystoscope was replaced with a Foley catheter at the bladder neck, keeping the balloon deflated and clamped after removing the saline completely. CO2 insufflation was initiated at 1–2 L/min through the robotic port. The robotic endoscope was employed to guide the placement of the two remaining robotic ports in the best possible triangulation with Prolene hitch stays, as illustrated in Figure 3a. A 5-mm suprapubic assistant port was placed finally [Figure 3b], and the clamped Foley catheter remained connected to a suction device, used sparingly to maintain a clear operative field as needed.
Figure 3.
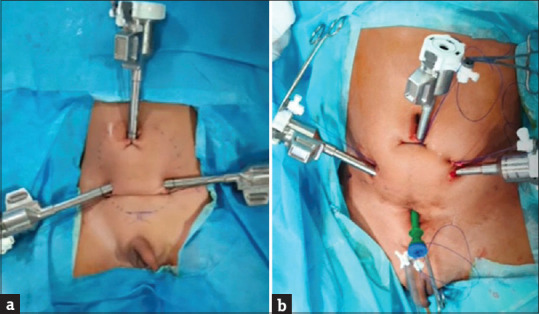
Final appearance after port placement: (a) Camera port in the center and working ports on the sides, (b) suprapubic assistant port opposite to the camera port
Ureteric manipulation and tapering
The procedure commenced with ureteric cannulation using a 5-Fr Infant feeding tube secured to the ureteric orifice with a 5-0 Polyglactin suture. After making an initial circumscribing incision, the ureter was dissected off the hiatus while staying outside the detrusor muscle adventitia. Subsequently, the distal end of the ureter was tied to the previously placed Foley catheter, as depicted in Figure 4. This maneuver served to straighten and stabilize the dissected portion of the ureter, allowing for precise excision and subsequent suturing of the cut margins, as shown in Figure 5. Excisional tapering was achieved with reasonable ease. The margins of the ureter were approximated using 5-0 polyglactin sutures.
Figure 4.
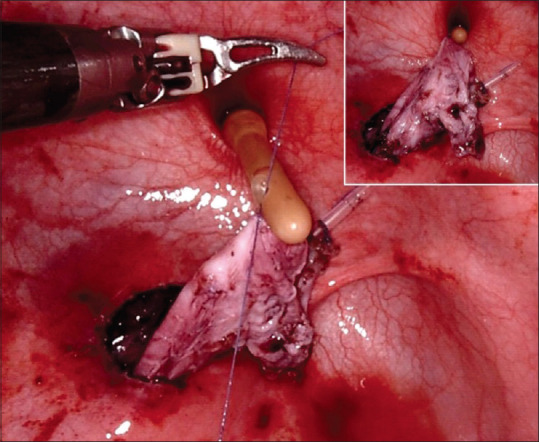
Foley tie to the ureter followed by ureteric alignment and stabilization with Foley tie (inset)
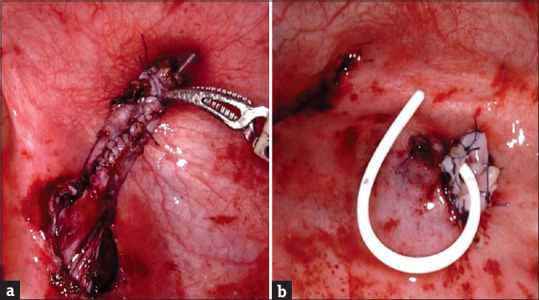
Figure 5.
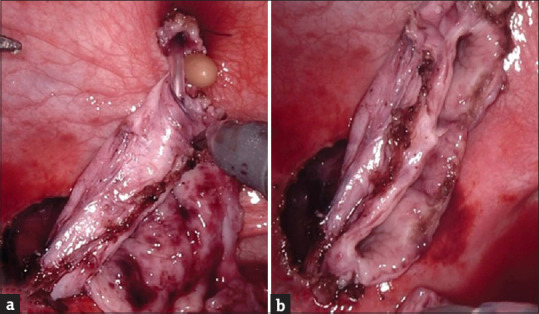
Ureteric tapering: (a) anterior wall, (b) posterior wall
Ureteric reimplantation and closure
Following ureteric manipulation and tapering, the ureteric reimplantation was completed using the Cross Cohen reimplantation technique [Figure 6] while maintaining Paquin’s ratio of 5:1 tunnel length to ureteral diameter; the usual length of the tunnel was around 4 cm. The plication line was positioned posteriorly toward the detrusor. Subsequently, a suprapubic catheter was placed through the 5-mm assistant port site. All other robotic port sites were meticulously closed in layers – the bladder was first closed using 3-0 polyglactin, followed by the closure of the muscle layer and skin.
Figure 6.
(a) Appearance after reconstruction of the ureter. (b) Final appearance after ureteric reimplantation
RESULTS
Four children underwent intravesical RAFUT and reimplantation at our center between 2019 and 2021. The age range of the patients varied from 3 years to 12 years. Notably, the bladder capacity of the youngest patient was 210 cc, while the oldest patient’s bladder approached adult volumes [Table 1]. The operative time for these procedures ranged from 180 to 210 min, and no intraoperative or postoperative complications were encountered. The average volume of blood loss during the procedure ranged from 35 to 50 mL. None of the patients required conversion to open surgery, and there were no significant collisions of robotic instruments during the surgeries. It was observed that the ease of movement of robotic arms was better in the female patient, probably due to the pelvic anatomy (oval shape of the pelvic inlet compared to boys with a triangular pelvic inlet). Notably, no complications were encountered in the male patients. However, in the female patient, a subtle gas leak occurred as the Foley tie occasionally approached the external urinary sphincter. This was effectively addressed by increasing the flow rate. This technique preserved the vascular and anatomical orientation of the ureter without axial twisting, ensuring precision in excision and suturing within the limited available space.
Table 1.
Summary of the cases undergoing ureteric reimplantation using robot-assisted Foley tie ureteric tapering
| Case number | Age/sex | Diagnosis | Investigations | Surgical procedure | Operating time | Estimated blood loss | Hospital stay | Outcome at 1 year |
|---|---|---|---|---|---|---|---|---|
| Case 1 | 3 years, male | Bilateral primary VUR, left PFK | USG: Right kidney - 5.4 cm with raised echoes. Left kidney - 9.3 cm, gross hydroureteronephrosis with marked cortical thinning VCUG: Bilateral VUR (left - grade 5, right - grade 2), bladder capacity 210 mL DMSA: Left kidney 23%, scars + | Robotic bilateral intravesical ureteric reimplantation with excisional tapering of the left ureter | 180 min | 50 mL | 5 days | Resolution of VUR; no UTI |
| Case 2 | 12 years, male | Left PFK with grade V VUR | Contrast-enhanced CT: Gross left hydroureteronephrosis up to the lower end of the ureter DMSA: Left PFK (30%), scars + VCUG: Left grade 5 VUR; bladder capacity 450 mL | Robotic intravesical left ureteric reimplantation with excisional tapering | 200 min | 35 mL | 5 days | Resolution of VUR; no UTI |
| Case 3 | 12 years, male | Bilateral grade 5 VUR | USG: Bilateral gross hydroureteronephrosis; left distal ureter - 2 cm, right distal ureter - 1.8 cm VCUG: Bilateral grade 5 VUR; bladder capacity 550 mL DMSA: Left kidney 60%, right kidney 40% | Robotic bilateral intravesical ureteric reimplantation with Cohen’s technique and tapering of the left ureter | 210 min | 50 mL | 6 days | Resolution of VUR; no UTI |
| Case 4 | 6 years, female | Right PFK with ectopic ureter and grade 5 VUR | USG: Small right kidney (5.5 cm × 2.3 cm) with moderate hydroureteronephrosis) VCUG: Right grade 5 VUR; bladder capacity 250 mL DMSA: Right kidney 17%, scars + | Robot right intravesical ureteric reimplantation with tapering of the right ureter | 200 min | 40 mL | 5 days | Resolution of VUR; no UTI |
DMSA: Dimercaptosuccinic acid, PFK: Poorly functioning kidney, USG: Ultrasonography, UTI: Urinary tract infection, VCUG: Voiding cystourethrogram, VUR: Vesicoureteral reflux, CT: Computed tomography
Case 1
A 3-year-old boy presented with recurrent febrile urinary tract infection (UTI) every month for the past 2 years. Ultrasonography showed a small right kidney (5.4 cm) with raised echoes. The left kidney was 9.3 cm long, grossly hydroureteronephrotic with marked cortical thinning. Anteroposterior renal pelvic diameter was 2.6 cm. The right retrovesical ureter (RVU) diameter was 6 mm, and the left RVU was 16 mm. VCUG revealed primary VUR (left grade 5 and right grade 2), and dimercaptosuccinic acid (DMSA) scan showed a poorly functioning left kidney. Robotic-assisted bilateral intravesical ureteric reimplantation was done with excisional tapering of the left ureter. Postoperative VCUG at 6 months confirmed resolution of VUR. On follow-up of nearly 4 years now, the child has no UTIs.
Case 2
A boy aged 12 years presented with pain abdomen with nausea and vomiting and episodes of febrile UTI. He was evaluated elsewhere, and the physician ordered a contrast-enhanced computerized tomography which showed gross left hydroureteronephrosis up to the lower end of the ureter. DMSA scan and VCUG revealed a poorly functioning left kidney with grade 5 VUR. His bladder capacity was 450 mL. Robot-assisted intravesical left ureteric reimplantation was done after excisional tapering using the RAFUT technique. There were no intraoperative or postoperative complications. On 2 years of follow-up, the child is doing well, with no further history of febrile UTI.
Case 3
A 12-year-old boy presented with a history of febrile UTI and difficulty in voiding since birth, and multiple consultations with different physicians were evaluated for his symptoms. There was a history of cystoscopy which did not reveal any obstructive lesion of the urethra. VCUG showed bilateral grade 5 VUR with bilateral hydroureteronephrosis and a bladder capacity of 550 mL. The urodynamic study revealed a compliant bladder with phasic detrusor overactivity during the filling phase and unsustained detrusor pressure during the voiding phase. He was able to empty the bladder with double voiding. Bilateral intravesical ureteric reimplantation was done with Cohen’s technique and tapering of the left ureter. He is currently doing well at 1.5 years of follow-up with the resolution of symptoms.
Case 4
A 6-year-old female child presented to us with left flank pain and high-grade fever. There was no history of urinary complaints. On ultrasonography, the right kidney measured 5.5 cm × 2.3 cm with moderate hydroureteronephrosis and abrupt narrowing of the lower ureter and ectopic opening proximal to the bladder neck. The left kidney was unremarkable. Preoperative VCUG revealed grade 5 VUR on the right side. DMSA scan revealed a poorly functioning right kidney with multiple cortical scars. Robot-assisted right intravesical ureteric reimplantation was done with right-sided ureteric tapering. She is currently asymptomatic at 1.5 years of follow-up.
DISCUSSION
RAFUT represents an innovative approach to addressing primary VUR in pediatric patients. While the gold standard for managing VUR has historically been open ureteric reimplant, this study explores the potential advantages of RAFUT in the context of pediatric patients.
One of the primary considerations when evaluating the adoption of RAFUT is the question of why robotic intravesical reimplantation has not gained traction at the rate of technological advancements. This can be attributed, in part, to the intricate technical challenges associated with intravesical surgery.[5] However, RAFUT offers a compelling solution that does not compromise on outcomes while simultaneously enhancing the surgical experience for both patients and surgeons. Notably, the evolution of robotic intravesical reimplantation appears to have plateaued after 2012, unlike laparoscopic intravesical reimplantation, where ergonomic challenges had been addressed effectively by robotic instruments.[6] The remaining barrier to widespread acceptance remains the cost associated with robotic surgery. As the cost of robotic systems gradually decreases, particularly as these systems become more accessible across various medical centers, it is anticipated that RAFUT may become a more economically viable option for pediatric patients. Currently, open surgery holds a cost advantage, costing approximately 33% less than its robotic counterpart.[7]
Patient age and bladder capacity play pivotal roles in determining the suitability of intravesical robotic surgery. While laparoscopic intravesical reimplantation is recommended for children older than 2 years with a bladder capacity of at least 130 mL,[8] robotic-assisted intravesical reimplantation typically sets the bar higher, requiring patients to be at least 4 years old and possess a bladder capacity of 200 mL.[9] Although performing surgery on smaller bladders can be challenging, we observed that RAFUT demonstrated its ability to overcome this hurdle, facilitated by meticulous port placement and strategic technique. RAFUT aids in atraumatic intravesical stabilization of the ureter, thereby allowing anatomical orientation without any axial twisting, besides precise excision and suturing. It is crucial to recognize that RAFUT may not be suitable for extremely small bladders, where maintaining the required distance between ports becomes practically impossible. While operating times for RAFUT may appear long, with increasing experience, these times are likely to decrease.
RAFUT’s success in achieving high rates of VUR resolution is a significant highlight. Published studies on robot-assisted intravesical ureteric reimplantation have reported success rates ranging from 92% to 100%.[9,10,11] However, due to the limited volume of literature on robotic intravesical reimplantation, further research is required to comprehensively define the true success rate of this procedure. Nonetheless, the preliminary results are undeniably promising and underscore RAFUT’s potential as a valuable option. In such scenarios, where concerns regarding extravesical approaches persist and open surgery may be excessively invasive, RAFUT emerges as an appealing alternative.
CONCLUSION
RAFUT represents a pioneering approach in addressing primary VUR in pediatric patients. As robotic technology continues to evolve and become more cost-effective, RAFUT’s role in pediatric urology is likely to expand. Future research endeavors should focus on further substantiating the effectiveness of RAFUT, refining the surgical technique, and assessing long-term outcomes to solidify its position as a valuable option in the management of VUR in pediatric patients.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts wildl be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Khan A, Rahiman M, Verma A, Bhargava R. Novel technique of laparoscopic extravesical ureteric reimplantation in primary obstructive megaureter. Urol Ann. 2017;9:150–2. doi: 10.4103/0974-7796.204182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Teng J, Jia Z, Ai X, Guan Y, Gao F. A modified transurethral stenting technique for (robot-assisted) laparoscopic ureteral reimplantation. Urol Int. 2019;102:385–9. doi: 10.1159/000496470. [DOI] [PubMed] [Google Scholar]
- 3.Li B, Lindgren BW, Liu DB, Gong EM. Robot-assisted laparoscopic megaureter tapering with ureteral reimplantation: Tips and tricks. J Pediatr Urol. 2017;13:637–8. doi: 10.1016/j.jpurol.2017.09.013. [DOI] [PubMed] [Google Scholar]
- 4.Ansari MS, Mandhani A, Khurana N, Kumar A. Laparoscopic ureteral reimplantation with extracorporeal tailoring for megaureter: A simple technical nuance. J Urol. 2006;176:2640–2. doi: 10.1016/j.juro.2006.08.025. [DOI] [PubMed] [Google Scholar]
- 5.Chang C, Steinberg Z, Shah A, Gundeti MS. Patient positioning and port placement for robot-assisted surgery. J Endourol. 2014;28:631–8. doi: 10.1089/end.2013.0733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Baek M, Koh CJ. Lessons learned over a decade of pediatric robotic ureteral reimplantation. Investig Clin Urol. 2017;58:3–11. doi: 10.4111/icu.2017.58.1.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schober MS, Jayanthi VR. Vesicoscopic ureteral reimplant: Is there a role in the age of robotics? Urol Clin North Am. 2015;42:53–9. doi: 10.1016/j.ucl.2014.09.005. [DOI] [PubMed] [Google Scholar]
- 8.Kutikov A, Guzzo TJ, Canter DJ, Casale P. Initial experience with laparoscopic transvesical ureteral reimplantation at the children's hospital of Philadelphia. J Urol. 2006;176:2222–5. doi: 10.1016/j.juro.2006.07.082. [DOI] [PubMed] [Google Scholar]
- 9.Marchini GS, Hong YK, Minnillo BJ, Diamond DA, Houck CS, Meier PM, et al. Robotic assisted laparoscopic ureteral reimplantation in children: Case matched comparative study with open surgical approach. J Urol. 2011;185:1870–5. doi: 10.1016/j.juro.2010.12.069. [DOI] [PubMed] [Google Scholar]
- 10.Peters CA, Woo R. Intravesical robotically assisted bilateral ureteral reimplantation. J Endourol. 2005;19:618–21. doi: 10.1089/end.2005.19.618. [DOI] [PubMed] [Google Scholar]
- 11.Chan KW, Lee KH, Tam YH, Sihoe JD. Early experience in robotic-assisted laparoscopic bilateral intravesical ureteral reimplantation for vesicoureteral reflux in children. J Robot Surg. 2012;6:259–62. doi: 10.1007/s11701-011-0288-1. [DOI] [PubMed] [Google Scholar]



