Summary
Healthcare professionals (HCPs) experienced prolonged stressful conditions during the coronavirus disease 2019 pandemic, and the global situation (particularly in the United Kingdom) meant that they continue to sustain mental stress related to the subsequent cost-of-living and healthcare budgeting crises. The psychological toll on HCPs may lead to increased staff attrition, adversely impacting the quality of patient care and work security. To help mitigate this psychological impact, the current evidence is strongly supportive of healthcare providers consistently adopting programmes fostering improvement in coping and resilience, facilitating healthy lifestyle, and allocating some resources for therapeutic strategies (e.g. cognitive behavioural therapy-based strategies and other strategies specified to trauma-related issues) which can be delivered by trained professionals. We stress that some approaches are not a one-size-fits-all strategy, and we also highlight the need to encourage treatment-seeking among those who need it. These strategies are highly relevant to healthcare employers and policymakers to support all HCPs in settings marked by prolonged periods of stress. The investment in these strategies are expected not only to reduce staff attrition in the long-term, but are likely to add to the cost-effectiveness of overall healthcare budgetary allocation.
Keywords: Healthcare professionals, Mental health, Burnout, Psychological stress, Strategies, Coronavirus, Depression, Prevention, Occupational stress
Introduction
It is more than three years since the SARS-CoV-2 pathogen was first reported to the World Health Organisation, marking the start of the coronavirus disease 2019 (COVID-19) pandemic. Whilst mental health did not considerably worsen in the general population,1 healthcare professionals (HCPs) were especially vulnerable due to the unique psychological stressors faced: pooled estimates show that 28.5% of HCPs had clinically significant symptoms of depression, 28.7% had anxiety, 25.5% had post-traumatic stress disorder (PTSD), and 24.4% had insomnia during the pandemic.2 Furthermore, patient facing HCPs (vs non-patient facing HCPs) were at significantly higher risk of burnout, and this difference in risk exacerbated over time during the pandemic.3 It is debatable to what extent the rates of adverse mental health worsened compared to before the pandemic, nonetheless it is generally accepted that HCPs were particularly vulnerable to adverse mental health even before the pandemic and that pandemic bared those factors to significant degrees, such that they further exacerbated those existing vulnerabilities.2 Although vaccination programmes were effective in mitigating the pandemic, the subsequent cost-of-living and National Health Service (NHS) budgeting crises in the United Kingdom (UK) continues to place immense strain on HCPs4: the Royal College of Nursing strike—the largest nurses strike ever—as well as the British Medical Association junior doctor and consultant strikes attest to this. Indeed, the economic and mental health impact of the pandemic were also worldwide issues.5,6 Since adverse mental health and burnout are increasingly reasons for staff sickness7 and attrition,8 and can impact on the quality of patient care,9 there is an urgent need to reflect on the current evidence for strategies to support all HCPs’ mental wellbeing during the COVID-19 pandemic and moving forward.
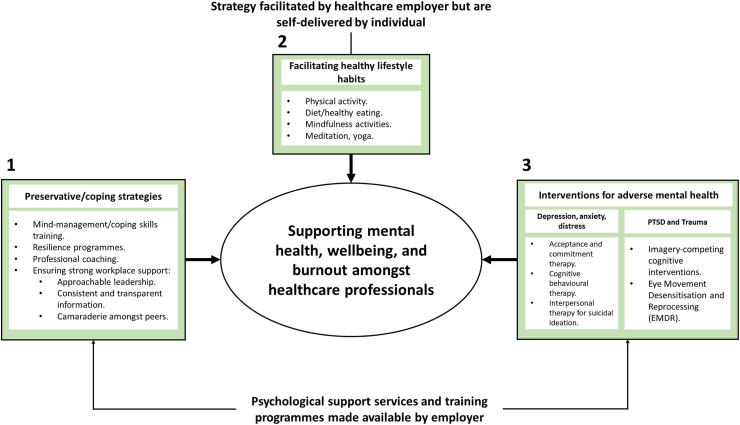
Whilst multiple rapid reviews have been conducted on this topic,10, 11, 12, 13 these generally focus on studies conducted in pre-COVID-19 pandemic scenarios,10,12 or are based on cross-sectional or observational study data.11,13 In this viewpoint article, we offer to provide an overview of strategies that have been shown to be effective interventions in a controlled clinical trial setting, together with evidence from own observations.14 Since mental health is a spectrum, we structure this viewpoint by first positing the strategies and resources implemented or facilitated by employers to support all HCPs regardless of mental illness symptom severity, before positing therapeutic strategies delivered by trained professionals to help mitigate adverse mental health symptomology. We believe the evidence related to effective mitigating strategies can be grouped into three categories: (i) preservative strategies via support programmes implemented by the employer, (ii) healthy lifestyle facilitated by the employer and self-delivered by the individual, and (iii) early and easy access to the therapeutic interventions on individual basis delivered by trained mental health professionals (Fig. 1). The latter may need to include tailored therapeutic strategies depending on the extent and type of mental illness, and strategies that will encourage treatment-seeking behaviours amongst HCPs and reduce the stigma that is often attached to that.
Fig. 1.
Strategies that have been shown to be effective in reducing the risk of adverse mental health impact amongst healthcare professionals. The diagram summarises the three strategies (non-hierarchical) that can be organised by healthcare employers to support the mental health and mental wellbeing of healthcare professionals: (1) preservative strategies via support programmes implemented by the employer, (2) healthy lifestyle facilitated by the employer and self-delivered by the individual, and (3) early and easy access to the tailored therapeutic interventions on an individual basis delivered by trained mental health professionals.
Preservative strategies: ‘mind-management’ and resiliency programmes, and professional coaching
Preservative strategies refer to the strategies which can be implemented by healthcare employers to equip HCPs with the necessary resources to prevent the development or worsening of mental health and burnout symptomology. Here we focus on three aspects, based on supporting evidence, to protect against adverse mental health and burnout amongst HCPs: (i) ‘mind-management’, resilience, and coping skills, (ii) professional coaching, and (iii) overall good quality workplace support.
Firstly, ‘mind-management’, resilience, and coping skills programmes have been shown to be effective against burnout, stress, and adverse mental impact, and should be implemented for all HCPs regardless of mental health status. These programmes can be delivered via several methods including digital apps, online modules, or group face-to-face sessions. The efficacy of these interventions is variable, but still reasonable and appears most relevant to improving mental wellbeing and, to an extent, reducing burnout. For example, the Mind Management Skills for Life Programme (an 8-week programme with one 90-min session per week) improved mental wellbeing by, on average, 3.71 points relative to a waitlist control group and reduced average burnout scores with a medium between-groups effect size (d = 0.60).15 Furthermore, programmes focused on resiliency training16,17 can improve mental wellbeing amongst HCPs16,17: for example, although mental wellbeing improved in a control group over a three-month period with a small effect size (d = 0.25), by contrast the experimental group (who received a single one-shot Community Resilience Model session) experienced improved mental wellbeing with a large effect size (d > 0.60).16 Other psychoeducational programmes aiming to change cognitive appraisals of stress and helping healthcare workers cope with the stressors have been found to reduce occupational stress substantially amongst nurses during the pandemic, relative to waitlist controls.18
Secondly, in comparison, professional coaching is shown to have particularly effective mitigating impact against burnout. They often are delivered by professionals and offer coaching either one to one or group to the HCPs in navigating professional choices and behaviours. These do not have to be delivered by coaches skilled in a specific area of healthcare, but rather the coaches can guide HCPs in obtaining ‘greater meaning in work, manage workload more effectively, and improve work efficiency, teamwork, sense of autonomy, social connections at work, and leadership skills’.19 For example, 3.5 h of professional coaching over a 6-month period reduced burnout by 2.5% amongst surgeons during the pandemic, while in contrast the surgeons who did not receive coaching experienced increased burnout by 2.5%.19 Relative to controls, group-based professional coaching also significantly improved emotional exhaustion by 4.33 points amongst Female physician residents20 and by 4.13 points amongst Female trainee physicians21 during the pandemic. We stress that a one-shot coaching session may not be sufficient and that continued professional coaching (e.g. once a month) should be offered to HCPs to sustain the benefits to burnout in the long-term.19
The third aspect relates to overall workplace support as an additional systemic strategy. Indeed, randomised controlled trials (RCTs) (likely in a cluster design) are required to robustly validate the effectiveness of improved workplace support, nevertheless our own prospective cohort research found that the level of perceived workplace support was consistently associated with mental health, wellbeing, and burnout amongst HCPs, and that improved perceived workplace support was associated with improved depression, anxiety, and wellbeing scores over a four month study period during the pandemic.22 Qualities such as visible and approachable leadership, consistent and transparent information sent on a timely manner, adequate staffing, and camaraderie and solidarity amongst peers constituted good quality workplace support.22 Similar studies also found that clear and consistent communication from leaders and adequate training for COVID-19-related tasks were preservative factors for mental health amongst nurses and midwives,23 and another study found that emotional support and feeling valued by leaders was associated with persistent distress amongst frontline HCPs.24 We posit that similar workplace support qualities should be made available to managers or healthcare leaders.
Facilitating healthy lifestyle habits
In this section, we highlight some of the lifestyle-based strategies which can be facilitated by the employer but self-implemented by the individual to help improve different facets of mental health (primarily depression, anxiety, and general mental wellbeing) and burnout. We further categorise these strategies as: (i) aspects traditionally associated with healthy lifestyle (namely physical activity and healthy eating), and (ii) mindfulness which can also be incorporated into a healthy lifestyle.
Physical activity and healthy eating
Strategies supporting and fostering the adoption and sustenance of the healthy lifestyle amongst the work force is often thought as an effective strategy for improving physical health, but it is now clear that it has significant benefit for improving mental health and reducing burnout. Ironically, despite that, this is not a uniformly adopted strategy nor is targeting towards all HCPs. This strategy can be enabled and facilitated in many ways, including using digital apps to facilitate healthy lifestyle habits which can be self-delivered by HCPs to support their mental wellbeing. For example, the Foundations digital application, provides users with an array of techniques such as breathing exercises, working with thoughts (e.g. cognitive behavioural therapy-based cognitive restructuring), positive thinking, mindfulness and meditation, sleep relaxations, sleep hygiene and scheduling, and physical activity recommendations to incorporate into everyday life.25 Relative to wait-list controls, the Foundations application improved general psychiatric morbidity (reduced on average by 1.39 points), mental wellbeing (improved on average by 0.54 points), and reduced the odds of insomnia by 64% amongst HCPs during the COVID-19 pandemic.25
While digital apps such as Foundations aim to facilitate multiple aspects of healthy lifestyle, we are aware of very few RCTs which have specifically investigated singular aspects such as physical activity and healthy eating in HCPs during the COVID-19 pandemic. Regarding physical activity, a recent RCT demonstrated that a 12-week self-initiated exercise intervention (via a digital application consisting of body weight interval training, yoga, running, and barre; minimum of four 20-min sessions per week) improved depression and burnout symptoms amongst HCPs with a small-to-medium treatment effect (−0.41 for depression and up to −0.39 for burnout) relative to waitlist controls.26 Similar benefits, especially for those with increased depressive symptoms at baseline, have been observed using the same digital exercise application in a non-HCP sample.27 Supporting this, our COVID-19 disease and Physical and Emotional Wellbeing of Health Care Professionals (CoPE-HCP) cohort study found that improved overall lifestyle (consisting of improved physical activity, increased healthy eating, and reduced smoking, alcohol consumption, and vaping) was associated with significantly improved depression, anxiety, and wellbeing amongst 613 UK-based HCPs over a four-month period during the pandemic.28 We advocate that healthcare systems give provision for exercise routinely to staff. Specifically, HCPs could be given subsidised access to a gym or swimming pools, digital exercise-focused applications, or leaders could encourage regular Park Run participation (a free, weekly, 5-km event on Saturday mornings). Indeed, prescribed exercise is already in use amongst some cardiology units in London hospitals but for patients specifically. If successfully incorporated into weekly routines, we anticipate that both regular aerobic29,30 and resistance training programmes30 will lead to mental health benefits based on pre-pandemic evidence in non-HCP samples. One can argue that adherence to exercise interventions will be low amongst those with adverse mental health, but there is evidence from the pandemic that baseline mental health status is unrelated to adherence to digital exercise app use,26 which requires self-administration. As such, prescribed exercise should be made available to all HCPs regardless of mental health status.
In terms of healthy eating, although diet (in particular the Mediterranean diet) and probiotics have been proposed as a potentially effective strategy to promote mental health during a pandemic setting31 or otherwise,32 we are aware of very few RCTs which have examined this amongst HCPs in a pandemic setting. One study found no significant difference in perceived stress between nurses taking probiotic supplement daily and a placebo group,33 while supplementing with cannabidiol (150 mg twice per day for 28 days) may reduce burnout, depression, and anxiety when used with standard care compared to standard care alone34 with benefits sustained up to 1-month after treatment.35 Further RCTs are required to evaluate the effectiveness of nutrition-based supplements and diet in mitigating specific domains of mental health amongst HCPs in a pandemic/post-pandemic setting. None the less, we believe that diet is an integral part of healthy lifestyle, and we recommend that a balanced healthy diet is supported for HCPs by providing subsidies for healthy meal or providing education/skills to encourage adoption of healthy eating routinely is important. Like physical activity, encouraging healthy eating strategies are cost-effective and self-implemented.
Mindfulness
Most lifestyle-based strategies evaluated in a RCT design are mindfulness-based. As detailed above, resilience and ‘mind-management’ programmes often include a mindfulness component. Mindfulness digital applications (such as the Headspace application) may support mental wellbeing by reducing the fear of COVID-19 and promoting sleep quality amongst HCPs during the pandemic.36 Given that such digital applications often require a paid subscription, we recommend that employers provide subsidies to all HCPs for these apps, however we believe that other strategies for delivering mindfulness interventions may be more effective. For example, a 4-week therapist-guided meditation programme via digital messaging application was found to reduce stress, depression, and anxiety37 with moderate-to-very large effect sizes (up to 1.42) immediately after the intervention, and these effect sizes were sustained (up to 0.98) an additional 4-weeks post-intervention in HCPs with moderate-to-high baseline levels of stress or burnout. As such, therapist-guided meditation programmes may also be particularly beneficial to HCPs experiencing high levels of stress.
Whilst self-administered digital mindfulness apps can be useful, our view is that non-digital and more traditional forms of mindfulness, such as 1:1 meditation sessions and face-to-face group meditation sessions, could be more effective but may incur additional costs if therapists are required to lead the sessions or provide training to HCPs. For example, Transcendental Meditation programmes are likely effective in reducing burnout and anxiety38 with small-to-medium effect sizes amongst HCPs during the pandemic, with some evidence for reducing depression in a pre-pandemic setting,39 but training/education in this form of meditation will be required. Breathing exercises such as progress muscle relaxation can also be taught to HCPs to help mitigate stress and anxiety symptomology with large effect sizes (d = 1.47 and 1.61, respectively).40 Less costly but creative forms of mindfulness such as mandala colouring, which are self-administered and require no training, may improve perceived stress amongst HCPs in a pandemic setting but we believe this will be dependent on being motivated to engage in colouring regularly and is unlikely to be an effective strategy for all HCPs.41 We advocate that, if mindfulness is delivered as an intervention to support HCPs, then it should be delivered by trained professionals in the form of guided meditation since this has the strongest evidence base, and preferably conducted in face-to-face settings, although online sessions should be offered given the variable work schedule of HCPs.
Pitfalls of mindfulness interventions
Drawing on this, since most RCTs evaluating the impact of mindfulness (or other lifestyle interventions) on mental health involve HCP samples not marked by a mental illness, it is difficult to advocate for these interventions for HCPs with mental illness or clinically-relevant symptoms and we stress that we should not make a one-size-fits-all approach. Taking suicidal ideation as an example, although brief mindfulness interventions can reduce suicidal ideation (immediately after the intervention) amongst non-HCP samples,42 we are unaware of any RCTs conducted with HCPs in a COVID-19 pandemic setting to demonstrate this. Factors such as exposure to potentially morally injurious events, lack of confidence about raising safety concerns and these concerns being addressed, feeling unsupported by managers, and providing a reduced standard of care are factors unique to HCPs which contribute to increased suicidal ideation amongst HCPs in the COVID-19 setting.43 Psychological therapies such as interpersonal therapy are valuable in reducing suicidal ideation via reducing general depression symptomology and should be prioritised, despite not specifically targeting suicidal ideation as a symptom.44 We speculate, given those workplace-related factors listed above,43 that improvements in systemic workplace support may also yield some benefit via the same mechanism. This is not to negate the value of mindfulness-based digital apps for severe mental health symptomology amongst HCPs: some mindfulness-based digital applications (such as Lift) can be useful by alerting mental health staff to connect the user with additional mental health services if suicidal ideation is reported.45
Access to therapeutic interventions
Noted above, some HCPs will be symptomatic and may have clinically-relevant symptoms of mental illness. Often, these symptoms are less expressed by these HCPs, mainly because of the stigma attached. Additionally, the generic strategies that are discussed above are unlikely to benefit those with clinically-relevant symptoms. This section focuses on the therapeutic strategies which should be prioritised for those with clinically-relevant symptoms. We advocate that there needs to be provision in any healthcare policy to ensure that therapies and trauma-focused strategies are made accessible to HCPs, both online and in person. Online cognitive behavioural therapy (CBT)-based interventions appear promising. For example, the ‘For Recovery from Stress’ (FOREST) programme, which involves individualized messaging-based feedback from psychologists and psychologists' support on-demand, improved perceived stress, depression, and psychological wellbeing amongst nurses, with benefits retained up to 3 months later.46 The value of online interventions, such as those based on CBT and acceptance and commitment therapy, are also supported by single-arm trials.47,48
Novel cognitive interventions may be required for trauma-related issues such as PTSD. For example, imagery-competing tasks49 and eye movement desensitization and reprocessing therapy (EMDR50; are likely effective in mitigating PTSD symptomology amongst frontline healthcare or emergency staff. Indeed, EMDR can be delivered online or in person by a trained lead. The benefits of EMDR in this context may be retained up to 6-months post-intervention50 and may bring additional benefits by reducing burnout amongst HCPs exposed to traumatic events.51 Besides these novel cognitive interventions, creative arts therapy (CAT) may also improve PTSD symptomology,52 although the exact mechanism for mitigating PTSD symptoms remains uncertain because the social aspect alone of group CAT may be therapeutic.
To supplement these interventions, and reduce the stigma associated with these conditions, we feel that it is imperative that there is wide-spread visible support and emphasis to increase the health seeking behaviour amongst HCPs. One strategy is to deliver relatable videos of HCPs describing their own mental health issues and describing how therapy benefitted them53 as part of a combat against mental health stigma. These videos should be tailored to specific professional roles, genders, and age.53 Drawing on this, an increased understanding of mental illness and an increased awareness of the systemic or workplace drivers of adverse mental health is likely to reduce stigma and increase treatment-seeking. Whilst there has been considerable advancement in reducing stigma regarding burnout, there is still work to be done to reduce stigma regarding mental illnesses, most notably, regarding depression.54 This is largely due to depression being regarded as an individual problem as opposed to burnout as an organisational problem, despite workplace perceptions (workload satisfaction and learning environment satisfaction) being strongly associated with both depression and burnout amongst medical interns,55 and the inverse association between hours worked per week and depression amongst physicians.56 Reframing depression (and psychological stress more generally) as both an organisational-level problem and an individual-level problem will hopefully increase treatment seeking and inform organisational approaches (e.g. improved workplace support) to help mitigate both depression and burnout. This reframing requires a top-down, systemic effort by leaders across healthcare services.
Take home messages for policymakers and researchers
The COVID-19 pandemic proved a natural experiment of psychological stress for HCPs and led to numerous clinical trials evaluating support strategies which we base our recommendations on (Fig. 1). Arranging for training programmes for all HCPs to improve resilience and effective coping strategies will help buffer against the onset of adverse mental health and burnout, in addition to employers encouraging healthy lifestyle habits amongst HCPs by subsidising subscriptions to mindfulness digital applications, gym memberships, and healthy eating programmes. Despite the wealth of observational studies reporting consistent associations between these lifestyle aspects and mental health or burnout, we need robust study designs to understand the efficacy of lifestyle improvements (diet in particular) as a cost-effective, self-administered intervention for mitigating adverse mental health and burnout. Furthermore, given that these self-administered lifestyle interventions do not provide a one-size-fits-all approach for all HCPs depending on mental health status, access to relevant psychological support services must be provided by the employer to help combat clinical levels of adverse mental health (e.g. depression, PTSD) or high levels of psychological distress. It also would be valuable to encourage treatment-seeking by increasing awareness of mental illness and both the individual-level and organisational-level drivers of mental health to combat stigma. Indeed, organisational-level factors including provisions for adequate staff, availability of regular supervision, reasonable work environment and working conditions may impact on mental health and burnout amongst HCPs.57,58 These factors may also in-part explain the differential impact amongst HCPs performing different roles. For example, patient-facing HCPs,3 and nurses in general,59 are at more risk of adverse mental health impact which can be explained by differences in working condition, long hours, financial incentives, job security, and provisions of resources and support.59 These work-related disparities should be addressed by healthcare employers. As the pandemic continues amidst cost-of-living and healthcare budgeting crises around the world, it is critical for policymakers and healthcare organisations to invest in these strategies to support the mental health and wellbeing, and to help mitigate burnout amongst HCPs. We expect a return-on-investment by funding these strategies to reduce staff attrition in the long-term: while more studies need to be done on this field, early evidence from two cost-benefit analyses studies have found considerable return-on-investment when hospitals implemented support programmes for HCPs.60,61 We strongly believe that to ensure longevity in these cost benefits and bring additional return-on-investment, initial corporate strategy should be to re-invest any financial savings into the mental health and burnout support strategies.
Outstanding questions
Finally, we recognise that most of the evidence for these strategies is from the Western world, and that there is a need for more studies from Africa and Asia to examine the relative effectiveness of these interventions in the context of culture differences. Drawing on this, we appreciate that there will be additional barriers to implementing such strategies in low-middle income countries (LMICs) due to the pandemic exacerbating the existing economic and health challenges in those countries. A more global effort is required to support those countries, and further research is required to identify the unique barriers to implementing these recommended support systems in LMICs.
Contributors
Conceptualisation: GC, AG.
Literature search: GC, AG.
Supervision: AG.
Writing-original draft: all authors equally.
Writing-review & editing: all authors equally.
Declaration of interests
The authors have no conflicts of interests to declare.
Acknowledgements
Funding: This work was supported by Barts Charity seed funding grant (G-002045).
References
- 1.Sun Y., Wu Y., Fan S., et al. Comparison of mental health symptoms before and during the covid-19 pandemic: evidence from a systematic review and meta-analysis of 134 cohorts. BMJ. 2023;380 doi: 10.1136/bmj-2022-074224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lee B.E.C., Ling M., Boyd L., Olsson C., Sheen J. The prevalence of probable mental health disorders among hospital healthcare workers during COVID-19: a systematic review and meta-analysis. J Affect Disord. 2023;330:329–345. doi: 10.1016/j.jad.2023.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kapil V., Collett G., Godec T., et al. Longitudinal comparisons of mental health, burnout and well-being in patient-facing, non-patient-facing healthcare professionals and non-healthcare professionals during the COVID-19 pandemic: findings from the CoPE-HCP study. BJPsych Open. 2022;8(5):e173. doi: 10.1192/bjo.2022.579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McBride M., Martin C.A., Teece L., et al. Investigating the impact of financial concerns on symptoms of depression in UK healthcare workers: data from the UK-REACH nationwide cohort study. BJPsych Open. 2023;9(4):e124. doi: 10.1192/bjo.2023.520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kaye A.D., Okeagu C.N., Pham A.D., et al. Economic impact of COVID-19 pandemic on healthcare facilities and systems: international perspectives. Best Pract Res Clin Anaesthesiol. 2021;35(3):293–306. doi: 10.1016/j.bpa.2020.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Aymerich C., Pedruzo B., Perez J.L., et al. COVID-19 pandemic effects on health worker's mental health: systematic review and meta-analysis. Eur Psychiatry. 2022;65(1):e10. doi: 10.1192/j.eurpsy.2022.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Edge R., van der Plaat D.A., Parsons V., et al. Changing patterns of sickness absence among healthcare workers in England during the COVID-19 pandemic. J Public Health. 2022;44(1):e42–e50. doi: 10.1093/pubmed/fdab341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hou H., Pei Y., Yang Y., et al. Factors associated with turnover intention among healthcare workers during the coronavirus disease 2019 (COVID-19) pandemic in China. Risk Manag Healthc Policy. 2021;14:4953–4965. doi: 10.2147/RMHP.S318106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Salyers M.P., Bonfils K.A., Luther L., et al. The relationship between professional burnout and quality and safety in healthcare: a meta-analysis. J Gen Intern Med. 2017;32(4):475–482. doi: 10.1007/s11606-016-3886-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kisely S., Warren N., McMahon L., Dalais C., Henry I., Siskind D. Occurrence, prevention, and management of the psychological effects of emerging virus outbreaks on healthcare workers: rapid review and meta-analysis. BMJ. 2020;369:m1642. doi: 10.1136/bmj.m1642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Muller A.E., Hafstad E.V., Himmels J.P.W., et al. The mental health impact of the covid-19 pandemic on healthcare workers, and interventions to help them: a rapid systematic review. Psychiatry Res. 2020;293 doi: 10.1016/j.psychres.2020.113441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Callus E., Bassola B., Fiolo V., Bertoldo E.G., Pagliuca S., Lusignani M. Stress reduction techniques for health care providers dealing with severe coronavirus infections (SARS, MERS, and COVID-19): a rapid review. Front Psychol. 2020;11 doi: 10.3389/fpsyg.2020.589698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.De Kock J.H., Latham H.A., Leslie S.J., et al. A rapid review of the impact of COVID-19 on the mental health of healthcare workers: implications for supporting psychological well-being. BMC Public Health. 2021;21(1):104. doi: 10.1186/s12889-020-10070-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Khanji M.Y., Maniero C., Ng S., et al. Early and mid-term implications of the COVID-19 pandemic on the physical, behavioral and mental health of healthcare professionals: the CoPE-HCP study protocol. Front Psychol. 2021;12 doi: 10.3389/fpsyg.2021.616280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Laker V., Simmonds-Buckley M., Delgadillo J., Palmer L., Barkham M. Pragmatic randomized controlled trial of the mind management skills for life programme as an intervention for occupational burnout in mental healthcare professionals. J Ment Health. 2023;32:1–9. doi: 10.1080/09638237.2023.2182423. [DOI] [PubMed] [Google Scholar]
- 16.Duva I.M., Higgins M.K., Baird M., Lawson D., Murphy J.R., Grabbe L. Practical resiliency training for healthcare workers during COVID-19: results from a randomised controlled trial testing the community resiliency model for well-being support. BMJ Open Qual. 2022;11(4) doi: 10.1136/bmjoq-2022-002011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Henshall C., Davey Z., Srikesavan C., Hart L., Butcher D., Cipriani A. Implementation of a web-based resilience enhancement training for nurses: pilot randomized controlled trial. J Med Internet Res. 2023;25 doi: 10.2196/43771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Alkhawaldeh J.M. Psychoeducational interventional programme during the COVID-19 pandemic for nurses with severe occupational stress: a randomized controlled trial. Int J Nurs Pract. 2023;29 doi: 10.1111/ijn.13129. [DOI] [PubMed] [Google Scholar]
- 19.Dyrbye L.N., Gill P.R., Satele D.V., West C.P. Professional coaching and surgeon well-being: a randomized controlled trial. Ann Surg. 2023;277(4):565–571. doi: 10.1097/SLA.0000000000005678. [DOI] [PubMed] [Google Scholar]
- 20.Fainstad T., Mann A., Suresh K., et al. Effect of a novel online group-coaching program to reduce burnout in Female resident physicians: a randomized clinical trial. JAMA Netw Open. 2022;5(5) doi: 10.1001/jamanetworkopen.2022.10752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mann A., Shah A.N., Thibodeau P.S., et al. Online well-being group coaching program for women physician trainees: a randomized clinical trial. JAMA Netw Open. 2023;6(10) doi: 10.1001/jamanetworkopen.2023.35541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Siddiqui I., Gupta J., Collett G., et al. Perceived workplace support and mental health, well-being and burnout among health care professionals during the COVID-19 pandemic: a cohort analysis. CMAJ Open. 2023;11(1):E191–E200. doi: 10.9778/cmajo.20220191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Marsden K.M., Robertson I.K., Porter J. Stressors, manifestations and course of COVID-19 related distress among public sector nurses and midwives during the COVID-19 pandemic first year in Tasmania, Australia. PLoS One. 2022;17(8) doi: 10.1371/journal.pone.0271824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Peccoralo L.A., Pietrzak R.H., Feingold J.H., et al. A prospective cohort study of the psychological consequences of the COVID-19 pandemic on frontline healthcare workers in New York City. Int Arch Occup Environ Health. 2022;95(6):1279–1291. doi: 10.1007/s00420-022-01832-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gnanapragasam S.N., Tinch-Taylor R., Scott H.R., et al. Multicentre, England-wide randomised controlled trial of the 'Foundations' smartphone application in improving mental health and well-being in a healthcare worker population. Br J Psychiatry. 2023;222(2):58–66. doi: 10.1192/bjp.2022.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Boucher V.G., Haight B.L., Hives B.A., et al. Effects of 12 Weeks of at-home, application-based exercise on health care workers' depressive symptoms, burnout, and absenteeism: a randomized clinical trial. JAMA Psychiatry. 2023;80(11):1101–1109. doi: 10.1001/jamapsychiatry.2023.2706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Puterman E., Hives B., Mazara N., et al. COVID-19 Pandemic and Exercise (COPE) trial: a multigroup pragmatic randomised controlled trial examining effects of app-based at-home exercise programs on depressive symptoms. Br J Sports Med. 2022;56(10):546–552. doi: 10.1136/bjsports-2021-104379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Khanji M.Y., Collett G., Godec T., et al. Improved lifestyle is associated with improved depression, anxiety and well-being over time in UK healthcare professionals during the COVID-19 pandemic: insights from the CoPE-HCP cohort study. Gen Psychiatr. 2023;36(1) doi: 10.1136/gpsych-2022-100908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Goldstein E., Topitzes J., Brown R.L., Barrett B. Mediational pathways of meditation and exercise on mental health and perceived stress: a randomized controlled trial. J Health Psychol. 2020;25(12):1816–1830. doi: 10.1177/1359105318772608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.LeBouthillier D.M., Asmundson G.J.G. The efficacy of aerobic exercise and resistance training as transdiagnostic interventions for anxiety-related disorders and constructs: a randomized controlled trial. J Anxiety Disord. 2017;52:43–52. doi: 10.1016/j.janxdis.2017.09.005. [DOI] [PubMed] [Google Scholar]
- 31.Shabbir M.A., Mehak F., Khan Z.M., et al. Delving the role of nutritional psychiatry to mitigate the COVID-19 pandemic induced stress, anxiety and depression. Trends Food Sci Technol. 2022;120:25–35. doi: 10.1016/j.tifs.2021.12.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Firth J., Gangwisch J.E., Borisini A., Wootton R.E., Mayer E.A. Food and mood: how do diet and nutrition affect mental wellbeing? BMJ. 2020;369:m2382. doi: 10.1136/bmj.m2382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Slykerman R.F., Li E. A randomized trial of probiotic supplementation in nurses to reduce stress and viral illness. Sci Rep. 2022;12(1) doi: 10.1038/s41598-022-19104-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Crippa J.A.S., Zuardi A.W., Guimaraes F.S., et al. Efficacy and safety of cannabidiol plus standard care vs standard care alone for the treatment of emotional exhaustion and burnout among frontline health care workers during the COVID-19 pandemic: a randomized clinical trial. JAMA Netw Open. 2021;4(8) doi: 10.1001/jamanetworkopen.2021.20603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Souza J.D.S., Zuardi A.W., Guimaraes F.S., et al. Maintained anxiolytic effects of cannabidiol after treatment discontinuation in healthcare workers during the COVID-19 pandemic. Front Pharmacol. 2022;13 doi: 10.3389/fphar.2022.856846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Keng S.L., Chin J.W.E., Mammadova M., Teo I. Effects of mobile app-based mindfulness practice on healthcare workers: a randomized active controlled trial. Mindfulness (N Y) 2022;13(11):2691–2704. doi: 10.1007/s12671-022-01975-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Luangapichart P., Saisavoey N., Viravan N. Efficacy and feasibility of the minimal therapist-guided four-week online audio-based mindfulness program 'mindful senses' for burnout and stress reduction in medical personnel: a randomized controlled trial. Healthcare (Basel) 2022;10(12):2532. doi: 10.3390/healthcare10122532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Joshi S.P., Wong A.I., Brucker A., et al. Efficacy of transcendental meditation to reduce stress among health care workers: a randomized clinical trial. JAMA Netw Open. 2022;5(9) doi: 10.1001/jamanetworkopen.2022.31917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Loiselle M., Brown C., Travis F., Gruener G., Rainforth M., Nidich S. Effects of transcendental meditation on academic physician burnout and depression: a mixed methods randomized controlled trial. J Contin Educ Health Prof. 2023;43(3):164–171. doi: 10.1097/CEH.0000000000000472. [DOI] [PubMed] [Google Scholar]
- 40.Ganjeali S., Farsi Z., Sajadi S.A., Zarea K. The effect of the demonstration-based progressive muscle relaxation technique on stress and anxiety in nurses caring for COVID-19 patients: a randomized clinical trial. BMC Psychiatry. 2022;22(1):791. doi: 10.1186/s12888-022-04456-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Fong J.S.Y., Hui A.N.N., Ho K.M., Chan A.K.M., Lee A. Brief mindful coloring for stress reduction in nurses working in a Hong Kong hospital during COVID-19 pandemic: a randomized controlled trial. Medicine (Baltimre) 2022;101(43) doi: 10.1097/MD.0000000000031253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wu R., Zhong S.Y., Wang G.H., et al. The effect of brief mindfulness meditation on suicidal ideation, stress and sleep quality. Arch Suicide Res. 2023;27(2):215–230. doi: 10.1080/13811118.2021.1982800. [DOI] [PubMed] [Google Scholar]
- 43.Padmanathan P., Lamb D., Scott H., et al. Suicidal thoughts and behaviour among healthcare workers in England during the COVID-19 pandemic: a longitudinal study. PLoS One. 2023;18(6) doi: 10.1371/journal.pone.0286207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Weitz E., Hollon S.D., Kerkhof A., Cuijpers P. Do depression treatments reduce suicidal ideation? The effects of CBT, IPT, pharmacotherapy, and placebo on suicidality. J Affect Disord. 2014;167:98–103. doi: 10.1016/j.jad.2014.05.036. [DOI] [PubMed] [Google Scholar]
- 45.Pratt E.H., Hall L., Jennings C., et al. Mobile mindfulness for psychological distress and burnout among frontline COVID-19 nurses: a pilot randomized trial. Ann Am Thorac Soc. 2023;20(10):1475–1482. doi: 10.1513/AnnalsATS.202301-025OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Dumarkaite A., Truskauskaite I., Andersson G., et al. The efficacy of the internet-based stress recovery intervention FOREST for nurses amid the COVID-19 pandemic: a randomized controlled trial. Int J Nurs Stud. 2023;138 doi: 10.1016/j.ijnurstu.2022.104408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Finucane A.M., Hulbert-Williams N.J., Swash B., et al. Feasibility of RESTORE: an online acceptance and commitment therapy intervention to improve palliative care staff wellbeing. Palliat Med. 2023;37(2):244–256. doi: 10.1177/02692163221143817. [DOI] [PubMed] [Google Scholar]
- 48.Trottier K., Monson C.M., Kaysen D., Wagner A.C., Liebman R.E., Abbey S.E. Initial findings on RESTORE for healthcare workers: an internet-delivered intervention for COVID-19-related mental health symptoms. Transl Psychiatry. 2022;12(1):222. doi: 10.1038/s41398-022-01965-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ramineni V., Millroth P., Iyadurai L., et al. Treating intrusive memories after trauma in healthcare workers: a Bayesian adaptive randomised trial developing an imagery-competing task intervention. Mol Psychiatry. 2023;28:1–10. doi: 10.1038/s41380-023-02062-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Farrell D., Moran J., Zat Z., et al. Group early intervention eye movement desensitization and reprocessing therapy as a video-conference psychotherapy with frontline/emergency workers in response to the COVID-19 pandemic in the treatment of post-traumatic stress disorder and moral injury-An RCT study. Front Psychol. 2023;14 doi: 10.3389/fpsyg.2023.1129912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Iyadurai L., Highfield J., Kanstrup M., et al. Reducing intrusive memories after trauma via an imagery-competing task intervention in COVID-19 intensive care staff: a randomised controlled trial. Transl Psychiatry. 2023;13(1):290. doi: 10.1038/s41398-023-02578-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Moss M., Edelblute A., Sinn H., et al. The effect of creative arts therapy on psychological distress in health care professionals. Am J Med. 2022;135(10):1255–12562.e5. doi: 10.1016/j.amjmed.2022.04.016. [DOI] [PubMed] [Google Scholar]
- 53.Amsalem D., Lazarov A., Markowitz J.C., Smith T.E., Dixon L.B., Neria Y. Video intervention to increase treatment-seeking by healthcare workers during the COVID-19 pandemic: randomised controlled trial. Br J Psychiatry. 2022;220(1):14–20. doi: 10.1192/bjp.2021.54. [DOI] [PubMed] [Google Scholar]
- 54.Sen S. Is it burnout or depression? Expanding efforts to improve physician well-being. N Engl J Med. 2022;387(18):1629–1630. doi: 10.1056/NEJMp2209540. [DOI] [PubMed] [Google Scholar]
- 55.Rotenstein L.S., Zhao Z., Mata D.A., Guille C., Sen S. Substantial overlap between factors predicting symptoms of depression and burnout among medical interns. J Gen Intern Med. 2021;36(1):240–242. doi: 10.1007/s11606-020-05664-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Fang Y., Lodi S., Hughes T.M., Frank E., Sen S., Bohnert A.S.B. Work hours and depression in U.S. First-year physicians. N Engl J Med. 2022;387(16):1522–1524. doi: 10.1056/NEJMc2210365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Denning M., Goh E.T., Tan B., et al. Determinants of burnout and other aspects of psychological well-being in healthcare workers during the Covid-19 pandemic: a multinational cross-sectional study. PLoS One. 2021;16(4) doi: 10.1371/journal.pone.0238666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Morawa E., Schug C., Geiser F., et al. Psychosocial burden and working conditions during the COVID-19 pandemic in Germany: the VOICE survey among 3678 health care workers in hospitals. J Psychosom Res. 2021;144 doi: 10.1016/j.jpsychores.2021.110415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Tian H., Qiao T., Teng J., et al. Factors associated with depression among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Psychol Med. 2023:1–10. doi: 10.1017/S0033291723002271. [DOI] [PubMed] [Google Scholar]
- 60.Moran D., Wu A.W., Connors C., et al. Cost-benefit analysis of a support program for nursing staff. J Patient Saf. 2020;16(4):e250–e254. doi: 10.1097/PTS.0000000000000376. [DOI] [PubMed] [Google Scholar]
- 61.Wijnen B.F.M., Lokkerbol J., Boot C., Havermans B.M., van der Beek A.J., Smit F. Implementing interventions to reduce work-related stress among health-care workers: an investment appraisal from the employer's perspective. Int Arch Occup Environ Health. 2020;93(1):123–132. doi: 10.1007/s00420-019-01471-y. [DOI] [PMC free article] [PubMed] [Google Scholar]