Abstract
Objective
Femoral neck fractures (FNFs) are among the most common fractures in elderly individuals. Surgery is the main treatment for FNFs, and osteonecrosis of the femoral head (ONFH) is one of the unacceptable complications. This study aimed to assess both the clinical and radiological outcomes in patients with FNFs treated with three parallel cannulated screws and to identify relationship between screws position and ONFH.
Patients and methods
A total of 100 patients who were treated with closed reduction and fixed with 3 parallel cannulated screws met the inclusion criteria between January 2014 and December 2020 at authors’ institution. The follow-up duration, age, sex, affected side, and injury-to-surgery interval were collected; the neck-shaft angle of both hips, screw-apex distance (SAD) and the tip-apex distance (TAD)were measured; and the Garden classification, quality of reduction and presence of ONFH were evaluated.
Results
The sample consisted of 37 males and 63 females, with 60 left and 40 right hips affected. The mean age of patients was 54.93 ± 12.24 years, and the mean follow-up was 56.3 ± 13.38 months. The overall incidence of ONFH was 13%. No significant difference was observed in the incidence of ONFH by affected side, age, fracture displacement, injury-to-surgery interval, neck-shaft angle deviation, or reduction quality. The SAD was significantly shorter in ONFH patients than in normal patients for all three screws (p = 0.02, 0.02, and 0.01, respectively).
Conclusions
The short SAD of all screws is associated with femoral head necrosis of FNFs treated with 3 cannulated screws. The short SAD indicated that screws malpositioning in the weight-bearing area of the femoral head, potentially harming the blood supply and compromising the anchorage of the primary compressive trabeculae in this region.
Keywords: Femoral neck fracture, Osteonecrosis, Cannulated screws, Screw-apex distance, Weight-bearing area
Introduction
Femoral neck fractures (FNFs) are among the most common fractures in elderly individuals, accounting for approximately 50% of all hip fractures [1]. These fractures pose a serious threat to the health and quality of life of patients [2–4]. Surgery is the main treatment for FNFs, as it allows patient mobilization and reduces the risk of complications. A variety of implants, including cannulated screws, dynamic hip screws, full-thread headless compression screws, the Targon system, and hip prostheses, femoral neck system are used in FNF treatment [5–7]. Cannulated screw fixation is the classical treatment option for FNFs because of its advantages, such as minimal invasiveness, reduced operative time, and sufficient stability [8]. However, the optimal positioning and volume of screws in the femoral neck remain controversial [9]. Traditionally, three cannulated screws are implanted in a parallel inverted triangle configuration [10]. This configuration provides the advantage of allowing compression within the fracture gap and enabling some collapses during the fracture heals, which has been demonstrated to be biomechanically superior to other implants [11].
Complications of this treatment, including postoperative nonunion, screw cut-out or fixation failure, femoral neck shortening, and osteonecrosis of the femoral head (ONFH), have been reported. ONFH is a severe and prevalent postoperative complication of FNFs. ONFH is thought result from the impairment of the unique blood supply to the femoral head. The overall incidence of ONFH ranges from 14.8–30% [12, 13], and it frequently manifests 2–3 years after treatment [14]. Although numerous studies have focused on factors influencing ONFH, its underlying pathophysiological mechanism remains incompletely understood. Independent risk factors, such as chronic disease, delayed surgery, fracture displacement, age, and sex, remain controversial [15, 16]. Furthermore, the potential impact of screw spatial positioning on the development of ONFH has not been investigated. The aim of this retrospective study was to assess both the clinical and radiological outcomes of FNF patients who underwent closed reduction and fixation with three parallel cannulated screws and to identify relationship between screws position and ONFH.
Patients and methods
Study Population
We retrospectively reviewed the records of patients who underwent surgical treatment for FNFs between January 2014 and December 2020 at our institutions. This study was approved by the ethics committees of the participating hospitals. The inclusion criteria included: (1) patients diagnosed FNFs treated with closed reduction and surgical placement of 3 parallel cannulated screws; (2) patients aged over than 18 years at the time of injury; (3) availability of complete clinical and radiological data; and (4) a minimum follow-up duration of 2 years. The exclusion criteria included: (1) fracture treated with an internal fixation construct other than three parallel cannulated screws, including fully threaded parallel conical screws, four cannulated screws with a cross screw, and a femoral neck system (FNS); (2) fracture treated with open reduction or over 2 weeks after injury; (3) pathological fracture; (4) concomitant systemic immune disease requiring long-term steroid use or alcoholism; (5) follow-up duration shorter than two years; and (6) insufficient clinical data or incomplete radiographs.
Finally, a total of 100 patients treated by closed reduction and 3 parallel cannulated screws met the inclusion criteria. The cohort were divided into ONFH and normal groups.
Radiographic measurements
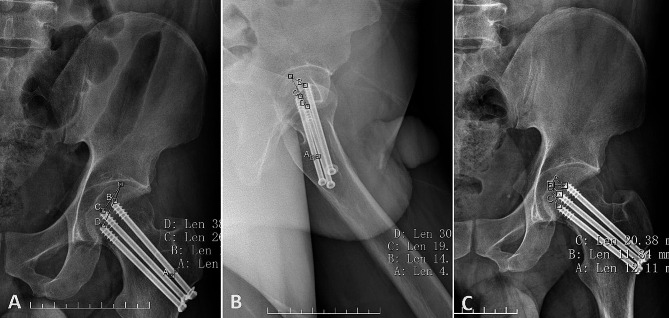
Anteroposterior (AP) and lateral radiographs of the hip were obtained to measure parameters at the first month of followup. The neck-shaft angle of both hips, the screw-apex distance (SAD) and the tip-apex distance (TAD) were measured using a Picture Archiving and Communication System (PACS; GE Healthcare, Chicago, Illinois). The Garden classification, and the quality of reduction were assessed, which included the presence of neutral support (anatomical reduction), positive support, and negative support (Fig. 1A-C) [17], and the presence of ONFH was evaluated by two experienced orthopaedic surgeons (XXZ and SYG). At each follow-up appointment, AP and lateral radiographs were routinely obtained for monitoring complications. ONFH was characterized by the emergence of subchondral osteolysis, accompanied by cystic alterations or sclerosis, and the occurrence of segmental collapse as evident on postoperative radiographs. However, patients continued to experience persistent hip pain and an inability to bear weight [18–22].
Fig. 1.
Schematic diagram showing the quality of femoral neck fracture reduction, including neutral support (anatomic reduction) of the fracture fragment (A), positive support (B), and negative support (C). Positive support indicates medial cortical support of the distal edge of the femoral neck fragment (B), and negative support indicates no medial cortical support of the distal edge (C)
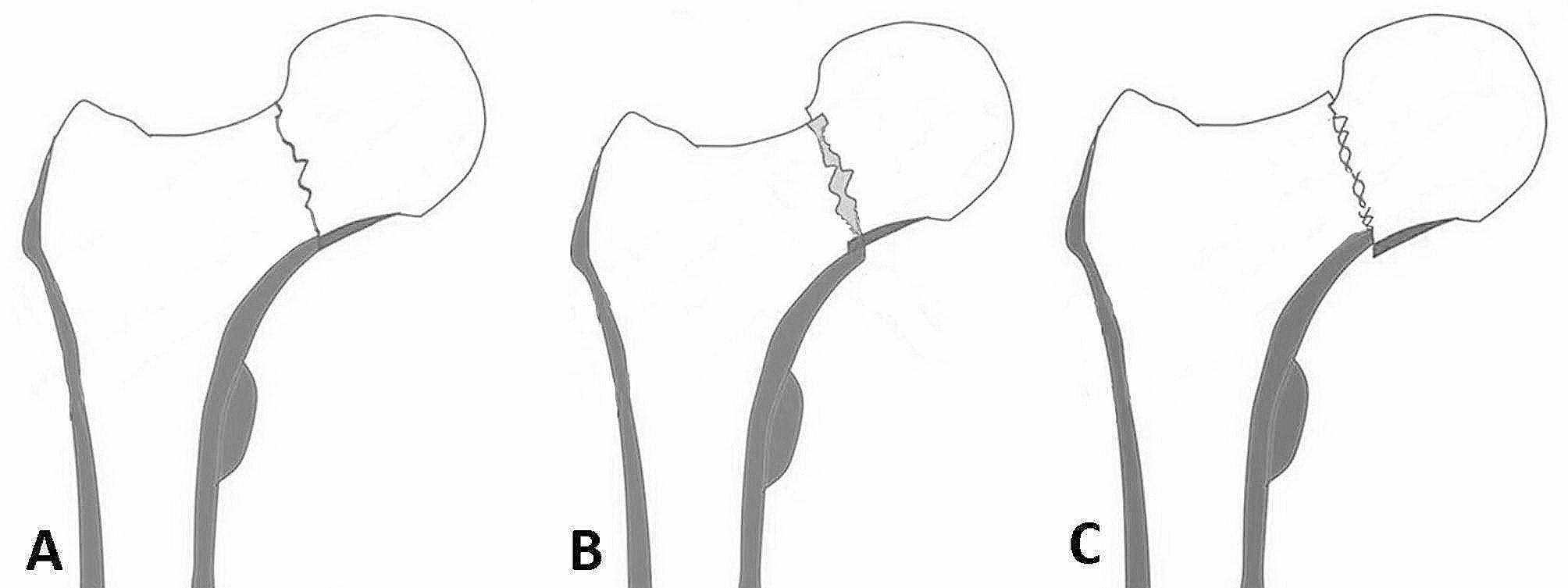
The SAD of the weight-bearing area was defined as the distance between the apex and the end of each screw, measured on both AP and lateral radiographs of the hip (Fig. 2A and B). The TAD of the medial femoral head was defined as the distance between the fossa capitis femoris and the tip of each screw, measured on both AP and lateral radiographs of the hip(Fig. 2B and C) [23]. The known diameter of the cannulated screws was used for calibrating all parameter measurements. On AP radiographs of the hip, the screw closest to the apex of the weight-bearing area was defined as the 1st screw, followed sequentially by the 2nd and 3rd screws.
Fig. 2.
Schematic diagram showing the definition of the screw-apex distance (SAD) and the tip-apex distance (TAD). The SAD was measured as the distance between the apex of the weight-bearing area and the end of each screw on anteroposterior (AP) and conventional lateral radiographs of the hip (A and B). The TAD was measured as the distance between the apex of the medial femoral head and the tip of each screw on AP and lateral radiographs of the hip (C and B). All images were calibrated using the known diameter of the screw
Closed reduction and percutaneous screw fixation
Surgery was performed promptly after diagnosis, typically within 24 h, by experienced orthopaedic surgeons. The patient was positioned in a supine position on a speciallized orthopaedic traction bed. The affected lower limb was initially abducted and externally rotated to enlarge the space of fractures, then adducted and internally rotated under longitudinal traction for reduction until the patella oriented horizontally. The reduction quality was verified in the AP and lateral planes with a cross-table view using a C-arm X-ray machine. After reduction, three Kirschner wires were usually used as guide pins, and cannulated screws were percutaneously inserted using a freehand technique. The primary goal was Neutral support (anatomical reduction), with positive support as the secondary aim. Negative support was also deemed acceptable if stable reduction of the fracture has been achieved (Fig. 1A-C). Sometimes, a Kirschner wire was inserted into the femoral head, serving as a joystick to control the head to assist the reduction. Subsequently, three partially threaded parallel cannulated screws (φ = 6.5 mm, Smith & Nephew, UK) were placed; the first implant was inserted along the femoral calcar (inferior), and the other two were placed superiorly (posterosuperior, anterosuperior) to form an inverse triangular configuration. The choice between a regular or an inverse triangle configuration was at the surgeon’s discretion.
Rehabilitation and follow-up
All patients followed a standardized postoperative protocol, which included the following: refraining from putting weight on the affected limb for the initial 3 months, transitioning to partial weight-bearing after bone union, and advancing to full weight-bearing after 6 months post-operation [24]. The following demographic and clinical data were collected: follow-up duration; age; sex; affected side; and injury-to-surgery interval.
Statistical analysis
Statistical analysis was conducted using SPSS 23.0 software (SPSS, Inc., IBM Corporation, Armonk, NY, USA). Continuous variables were presented as the mean ± standard deviation. The independent-samples t-test was used to compare differences between the ONFH group and the normal group. Categorical variables, presented as numbers and percentages, were anlyzed using the chi-square test or Fisher’s exact test when the expected count was less than 5. The significance level was set at 0.05.
Results
This sample consisted of 37 males and 63 females. The mean patient age was 54.93 ± 12.24 (23 to 82) years, and the mean follow-up duration was 56.3 ± 13.38 (27 to 72) months. This study involved 60 left hips and 40 right hips; 34 patients presented with nondisplaced Garden class I–II FNFs, and 66 patients with displaced Garden class III–IV FNFs. The overall incidence of ONFH was 13% (13/100). The mean time of fracture to ONFH was 27.75 ± 10.24 months (range, 13 to 46 months), with all cases of ONFH occurring between 1 and 4 years after surgery.
There was no significant difference between the ONFH and normal groups with regard to affected side, age, displacement (Garden classification), injury-to-surgery interval, neck-shaft angle deviation, or reduction quality. In the ONFH group, there were 13 females and no males, with a significant difference in the incidence of ONFH observed between male and female patients (p < 0.01) (Table 1).
Table 1.
Summary of the main demographic data of the two groups
| Basic characteristics | ONFH patients (n = 13) |
Normal patients (n = 87) |
P value |
|---|---|---|---|
| Age(years) |
58.38 ± 11.03 (38–78) |
54.74 ± 14.35 (23–82) |
0.38 |
| Sex | |||
| Male(n, %) | 0(0%) | 37(42.5%) | < 0.01 |
| Female(n, %) | 13(100%) | 50(57.5%) | |
| Operative side | 0.56 | ||
| Left(n, %) | 9(69.2%) | 51(58.6%) | |
| Right(n, %) | 4(30.8%) | 36(41.4%) | |
| Garden classification | 0.53 | ||
| I + II(n, %) | 3(23.1%) | 31(35.6%) | |
| III + IV(n, %) | 10(76.9%) | 56(64.4%) | |
| Reduction quality | 0.32 | ||
| negative(n, %) | 3(23.1%) | 8(9.2%) | |
| positive(n, %) | 2(15.4%) | 13(14.9%) | |
| neutral support(n,%) | 8(61.5%) | 66(75.9%) | |
|
Injury-to-surgery interval (days) |
2.38 ± 1.04 (1–4) |
2.80 ± 1.85 (1–14) |
0.43 |
|
Follow-up duration (months) |
59.38 ± 13.47 (29–72) |
55.84 ± 13.38 (27–72) |
0.38 |
| Deviation of neck-shaft angle (°) |
1.74 ± 6.97 (-12.13-13.63) |
4.33 ± 7.68 (-11.41-20.94) |
0.26 |
ONFH, osteonecrosis of the femoral head. Continuios data are presented as the mean ± standard deviation(range) and categorical data are present as percentage. The significance level was set at 0.05
The TAD of the 1st screw and the 1st screw plus 2nd screw in AP view were significantly longer in ONFH group, compared to the normal group(p < 0.001, p < 0.01, respectively). No significant difference was found regarding of the sum value of the 1st, 2nd and 3rd screws in the AP view. The cumulative TAD values in both AP view and lateral view showed no significant difference between the ONFH group and the normal group (Table 2).
Table 2.
Comparison of the TAD between the two groups
| AP view | Lateral view | TAD | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Items | ONFH group (n = 13) |
Normal group (n = 87) |
P value | ONFH group (n = 13) |
Normal group (n = 87) |
P value | ONFH group (n = 13) |
Normal group (n = 87) |
P value |
| 1st screw(mm) |
21.35 ± 5.46 (14.28–29.13) |
15.95 ± 4.52 (5.02–28.42) |
< 0.001 |
13.13 ± 5.80 (6.60-21.79) |
14.90 ± 4.73 (1.88–28.16) |
0.22 |
34.48 ± 6.36 (23.07–43.04) |
30.85 ± 7.36 (13.51–53.29) |
0.10 |
| 1st + 2nd screw(mm) |
37.51 ± 6.59 (25.66–51.38) |
31.70 ± 6.42 (22.34–55.48) |
< 0.01 |
31.06 ± 11.05 (19.40-54.54) |
34.17 ± 9.18 (3.96–61.51) |
0.27 |
68.57 ± 14.00 (47.93–94.40) |
65.87 ± 13.01 (33.71-106.14) |
0.49 |
| 1st + 2nd + 3rd screw(mm) |
56.99 ± 9.00 (43.34–70.90) |
52.13 ± 9.86 (32.69–87.20) |
0.10 |
52.84 ± 16.76 (34.63–89.35) |
58.36 ± 14.19 (6.37–96.91) |
0.20 |
109.81 ± 20.29 (80.00-160.25) |
110.49 ± 20.73 (60.26-164.33) |
0.91 |
ONFH, osteonecrosis of the femoral head; TAD, tip-apex distance; AP, anteroposterior
Data are presented as the mean ± standard deviation(range) or number of patients. Differences are considered significant at p < 0.05
The SAD, the distance from the tip of the screw to the apex in the weight-bearing area of the femoral head, was significantly shorter in the ONFH group compared to the normal group. Specifically, the SAD of the 1st screw in the ONFH group(13.48 ± 6.73 mm; range, 4.54–31.77 mm) was significantly shorter than in the normal group (18.47 ± 6.49 mm; range, 3.12–36.63 mm) in AP radiographs. Similar trends were observed for the combined SAD of the 1st and 2nd screws (p = 0.01), as well as the 1st, 2nd, and 3rd screws combined (p = 0.01), as indicated in AP radiographs (Table 3).
Table 3.
Comparison of the SAD between the two groups
| AP view | Lateral view | SAD | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Items | ONFH group (n = 13) |
Normal group (n = 87) |
P value | ONFH group (n = 13) |
Normal group (n = 87) |
P value | ONFH group (n = 13) |
Normal group (n = 87) |
P value |
| 1st screw(mm) |
13.48 ± 6.73 (4.54–31.77) |
18.47 ± 6.49 (3.12–36.63) |
0.01 |
13.13 ± 5.80 (6.60-21.79) |
14.90 ± 4.73 (1.88–28.16) |
0.22 |
26.61 ± 10.32 (11.73–53.56) |
33.37 ± 9.33 (12.13–60.70) |
0.02 |
| 1st + 2nd screw(mm) |
34.95 ± 13.52 (13.78–70.49) |
44.80 ± 12.44 (17.10-77.86) |
0.01 |
31.06 ± 11.05 (19.40-54.54) |
34.17 ± 9.18 (3.96–61.51) |
0.27 |
66.01 ± 21.86 (34.79-125.02) |
78.97 ± 17.68 (43.96-130.26) |
0.02 |
| 1st + 2nd + 3rd screw(mm) |
67.38 ± 18.80 (40.10-113.63) |
81.54 ± 17.66 (40.81-128.83) |
0.01 |
52.84 ± 16.76 (34.63–89.35) |
58.36 ± 14.19 (6.37–96.91) |
0.20 |
120.20 ± 30.03 (77.60-202.98) |
139.90 ± 25.87 (87.73-217.02) |
0.01 |
ONFH, osteonecrosis of the femoral head; SAD, screw-apex distance; AP, anteroposterior
Data are presented as the mean ± standard deviation(range) or number of patients. Differences are considered significant at p < 0.05
Although there were no significant differences in these distances in lateral radiographs between two groups (p = 0.22, 0.27, and 0.20, respectively), the corresponding total SADs of the three screws in AP and lateral radiographs were significantly shorter in the ONFH group than in the normal group (p = 0.02, 0.02, and 0.01, respectively) (Table 3).
Discussion
The most significant finding of this study was the markedly shorter SAD of the first screw, the combined first screw and second screw, and the sum of all three screws in the ONFH group compared to the normal group. Conversely, the TAD of the first screw, the combined first screw and second screw, and the sum of all three screws in the ONFH group showed no significant difference when compared to the normal group. A reduced SAD implies that the screw tip is closer to the weight-bearing area of the femoral head, potentially correlating with ONFH in femoral neck fractures treated with three cannulated screws.
Multiple factors have been identified as contributors to ONFH, including fracture displacement, segmental rotation, delayed time to surgery, postoperative malposition, and fracture patterns [15, 25, 26]. Achieving satisfactory reduction and rigid fixation is crucial in reducing the incidence of ONFH. Although various fixation devices are currently available, the use of three cannulated screws in a inverted triangle configuration is the most prevalent method in FNF treatment, owing to its excellent mechanical strength, rigid fixation, minimal invasiveness, and technical simplicity [27, 28]. The precise insertion of the three screws were key point to avoid ONFH.
The pathophysiological mechanisms underlying osteonecrosis of ONFH have been a subject of debate for many years, with significant gaps in understanding its pathogenesis yet to be addressed. There is a strong argument for vascular hypotheses in the aetiology of ONFH, which posit that a reduction in blood perfusion within the femoral head is critical to its pathogenesis [29]. The lateral epiphyseal vessels are of paramount importance, accounting for vascular supply to 80% of the proximal and weight-bearing areas of the femoral head [30, 31]. Their vulnerability to damage, compression, or occlusion positions these vessels as central in the pathogenesis of osteonecrosis, particularly in areas anatomically prone to such conditions, like the anterosuperior segment of the femoral head [32]. It has been argued that the force of the initial trauma determines the fate of vascularity in these fractures and the development of ONFH [33]. Furthermore, stress on the retinacular vessels has been identified as a primary factor in the development of ONFH [34], with the absence of these vessels being a significant contributor to its pathogenesis [35]. In displaced FNFs, tearing or kinking of these vessels can severely limit blood supply, potentially leading to nonunion and ONFH [36]. Consequently, the epiphysis and articular surface are especially prone to circulatory insufficiency [37], especially in weight-bearing areas. A digital subtraction angiography study revealed that vessel damage rates in Garden class III and IV fractures could reach 72.7-100% [38]. Nonetheless, 95% of patients in Garden class III and 80% in Garden class IV retained intact superior retinacular artery blood supplies, without showing signs of ischemia [39]. Another study suggested that higher Garden classifications do not necessarily correlate with increased ONFH risk [25], and some researchers have postulated that intraosseous healing may compensate for part of the devascularised head [40].
The proximal femur comprises five trabecular groups, displaying highly asymmetric distribution, which may lead to diverse pathomechanisms [41]. In the femoral head’s upper and central areas, principal compressive trabeculae are prominent, transmitting weight from the articular surface to the neck and fulcrum (Fig. 3). The principal tensile trabeculae, which exhibit a more horizontal orientation, intersect and extend into the lower medial, non-weight-bearing region [42]. Research suggests that both the elastic modulus and functions of these trabeculae are comparable to cortical bone [43]. Trabecular degeneration has been identified as a crucial factor in the incidence of hip fragility fractures, predominantly occurring in the femoral neck and intertrochanteric regions [44]. However, the exact role of trabecular injury in ONFH remains unclear.
Fig. 3.
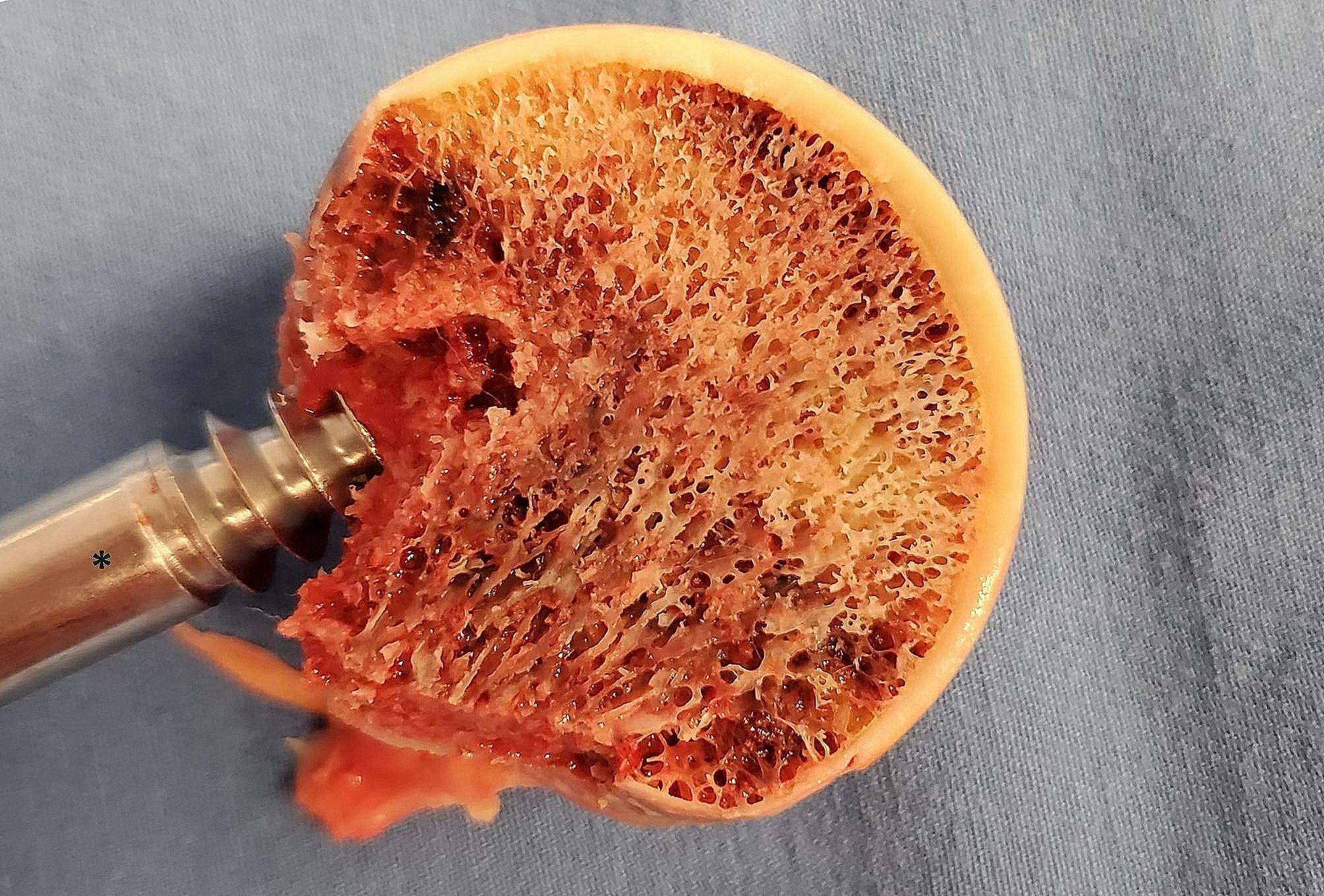
An 81-year-old female patient suffering from a right femoral neck fracture was treated with artificial hip replacement. The femoral head was cut with a saw near the centre on the coronal plane after the femoral head was removed, with the weight-bearing region just above the femoral head. Here, we aim to show the principal compressive trabecular structure. * Extractor
As delineated by the vascular pathophysiological mechanisms, the femoral head endures both static and dynamic weight-bearing biomechanical demands, resulting in uneven distribution of mechanical forces on its surface [45]. Notably, areas subjected to maximal loading demonstrate a discernible 25% increase in vessel density within the subchondral bone [46]. Research has further investigated the relationship between mechanical loading and bone perfusion, indicating that regions subjected to increased mechanical stress exhibit reduced perfusion [47]. This indicates that trabeculae located under the weight-bearing region need more blood supply and demonstrate increased sensitivity to ischemia. According to our results, a higher incidence of ONFH was associated with a shorter SAD, the tips of the screws were closer to the apex of the superolateral aspect of the femoral head. Consequently, FNFs-induced damage to the retinacular vessels would exacerbate the circulatory insufficiency, especially in the epiphysis and weight-bearing area. Meanwhile, damage to the screw anchorage in the principal compressive trabeculae on the articular surface may be another important factor. Such damage could reduce the structural integrity of the anchorage, leading to subchondral microfractures, accompanied by a minor extent of bone cell death, thereby impairing normal reparative processes in the femoral head. This impairment, along with osteocytes ischemic necrosis, could eventually lead to structural collapse of the femoral head. However, the collapse phenomenon can be further explicated by the imbalance between the slower rate of bone formation and the more rapid resorption rate in the subchondral bone, resulting in a net bone loss, compromised structural integrity, and eventual subchondral fracture [48].
This study’s limitations include its small sample size and retrospective design. Additionally, the monocentric data collection and absence of randomization introduce potential for selection bias. The short follow-up duration in this study, although the mean follow-up was 56.3 ± 13.38 months, may underestimate the actual incidence of ONFH. Asnis et al. reported ONFH in 11% of their patients after two years, increasing to 22% at eight years, and almost 25% of their patients had nondisplaced Garden I or II fractures [41]. Additionally, the use of radiographs and CT scans to diagnose osteonecrosis likely leads to further underreporting. Magnetic resonance imaging (MRI) is more sensitive for detecting osteonecrosis, but postoperative MRI is not routinely performed. Additionally, hip rotation during measurements can introduce significant errors in screw positioning [9], especially in TAD measurements. The absence of data on nonunion, screw cut-out or fixation failure, and femoral neck shortening also represents a notable limitation. However, despite these limitations, we believe that our findings are robust and provide empirical evidence that the spatial malpositioning of screws may increase the risk of ONFH in FNFs patients.
Conclusions
In conclusion, the short SAD of all screws is potentially associated with femoral head necrosis of FNFs treated with 3 cannulated screws. The short SAD indicated that screws malpositioning in the weight-bearing area of the femoral head, which may result in harm to the unique blood supply and compromise the anchorage of the primary compressive trabeculae in this region. This damage may lead to ischaemic necrosis of bone cells and loss of structural integrity of the principal compressive trabeculae, eventually leading to structural collapse of the femoral head.
Acknowledgements
Not applicable.
Abbreviations
- FNFs
Femoral neck fractures
- ONFH
osteonecrosis of the femoral head
- SAD
screw-apex distance
- TAD
tip-apex distance
- AP
anteroposterior
- MRI
Magnetic resonance imaging
Author contributions
ZXX, YY, and WJP designed the project and wrote the manuscript. JHL, WJP and GSY performed the parameter measurements. JHL, GSY, and ZLY analysed the data. All authors participated in the review and discussion of the manuscript.
Funding
Not applicable.
Data availability
All data will be available upon motivated request to the corresponding author of the present paper.
Declarations
Ethics approval and consent to participate
This study was approved by the institutional review board of Shanghai university of medicine & health Sciences Affiliated Zhoupu hospital (2022-A-10). Written informed consent was waived by the Institutional Ethics Committee of Zhoupu Hospital, Affiliated to Shanghai University of Medicine & Health Sciences.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Xiaoxiao Zhou, Shengyang Guo, and Wenjun Pan co-first authors.
References
- 1.Haubruck P, Heller RA. Tanner Femoral neck fractures: current evidence, controversies and arising challenges Orthop. Traumatol Surg Res. 2020;106(4):597–600. doi: 10.1016/j.otsr.2020.03.006. [DOI] [PubMed] [Google Scholar]
- 2.Maffulli N. R Aicale Proximal femoral fractures in the Elderly: a few things to know, and some to Forget Medicina (Kaunas, Lithuania). 58(10).2022 10.3390/medicina58101314. [DOI] [PMC free article] [PubMed]
- 3.Chen YP, Kuo YJ, Hung SW et al. Loss of skeletal muscle mass can be predicted by Sarcopenia and reflects poor functional recovery at one year after surgery for geriatric hip fractures Injury. 52(11): 3446–52.2021 10.1016/j.injury.2021.08.007. [DOI] [PubMed]
- 4.Quaranta M, Miranda L, Oliva F, et al. Haemoglobin and transfusions in elderly patients with hip fractures: the effect of a dedicated orthogeriatrician. J Orthop Surg Res. 2021;16(1):387. doi: 10.1186/s13018-021-02524-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Marsillo E, Pintore A, Asparago G et al. Cephalomedullary nailing for reverse oblique intertrochanteric fractures 31A3 (AO/OTA) orthopedic reviews. 14(6): 38560.2022 10.52965/001c.38560. [DOI] [PMC free article] [PubMed]
- 6.Gargano G, Poeta N, Oliva F, et al. Zimmer Natural Nail and ELOS nails in pertrochanteric fractures. J Orthop Surg Res. 2021;16(1):509. doi: 10.1186/s13018-021-02634-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cai L, Zheng W, Chen C et al. Comparison of young femoral neck fractures treated by femoral neck system, multiple cancellous screws and dynamic hip screws: a retrospectively comparison study BMC musculoskeletal disorders. 25(1): 188.2024 10.1186/s12891-024-07319-y. [DOI] [PMC free article] [PubMed]
- 8.Zhang LL, Zhang Y, Ma X et al. Multiple cannulated screws vs. dynamic hip screws for femoral neck fractures: a meta-analysis Orthopade. 46(11): 954-10.1007/s00132-017-3473-8. [DOI] [PubMed]
- 9.Lindequist S. Cortical screw support in femoral neck fractures. A radiographic analysis of 87 fractures with a new mensuration technique. Acta Orthop Scand. 1993;64(3):289–93. doi: 10.3109/17453679308993627. [DOI] [PubMed] [Google Scholar]
- 10.Walker E, Mukherjee DP, Ogden AL et al. A biomechanical study of simulated femoral neck fracture fixation by cannulated screws: effects of placement angle and number of screws am J orthop (Belle Mead NJ). 36(12): 680–4.2007. [PubMed]
- 11.Madsen F, Linde F, Andersen E, et al. Fixation of displaced femoral neck fractures. A comparison between sliding screw plate and four cancellous bone screws. Acta Orthop Scand. 1987;58(3):212–6. doi: 10.3109/17453678709146468. [DOI] [PubMed] [Google Scholar]
- 12.Liu Y, Li M, Zhang M, et al. Femoral neck fractures: prognosis based on a new classification after superselective angiography. J Orthop Sci. 2013;18(3):443–50. doi: 10.1007/s00776-013-0367-4. [DOI] [PubMed] [Google Scholar]
- 13.Ye Y, Chen K, Tian K, et al. Medial buttress plate augmentation of cannulated screw fixation in vertically unstable femoral neck fractures: Surgical technique and preliminary results. Injury. 2017;48(10):2189–93. doi: 10.1016/j.injury.2017.08.017. [DOI] [PubMed] [Google Scholar]
- 14.Florschutz AV, Langford JR, Haidukewych GJ, et al. Femoral neck fractures: current management. J Orthop Trauma. 2015;29(3):121–9. doi: 10.1097/BOT.0000000000000291. [DOI] [PubMed] [Google Scholar]
- 15.Cui S, Zhao L, Wang Y et al. Using Naive Bayes Classifier to predict osteonecrosis of the femoral head with cannulated screw fixation Injury. 49(10): 1865–70.2018 10.1016/j.injury.2018.07.025. [DOI] [PubMed]
- 16.Li H, Li F, Liu N et al. Risk Prediction of Femoral Head Necrosis: A Finite Element Analysis Based on Fracture Mechanics 17(06): 1121-1127.2020.
- 17.Xiong WF, Chang SM, Zhang YQ, et al. Inferior calcar buttress reduction pattern for displaced femoral neck fractures in young adults: a preliminary report and an effective alternative. J Orthop Surg Res. 2019;14(1):70. doi: 10.1186/s13018-019-1109-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Upadhyay A, Jain P, Mishra P, et al. Delayed internal fixation of fractures of the neck of the femur in young adults. A prospective, randomised study comparing closed and open reduction. J Bone Joint Surg Br. 2004;86(7):1035–40. doi: 10.1302/0301-620x.86b7.15047. [DOI] [PubMed] [Google Scholar]
- 19.Bray TJ. Femoral neck fracture fixation. Clinical decision making Clin Orthop Relat Res. 339): 20–31.1997 10.1097/00003086-199706000-00004. [DOI] [PubMed]
- 20.Tripathy SK, Goyal T. Sen Management of femoral head osteonecrosis: current concepts. Indian J Orthop. 2015;49(1):28–45. doi: 10.4103/0019-5413.143911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nikiforidis P, Babis GC, Papaioannou N et al. The role of primary total hip replacement for the treatment of the displaced femoral neck fractures.1997.
- 22.Bachiller FG, Caballer AP. L F Portal avascular necrosis of the femoral head after femoral neck fracture Clin Orthop Relat Res. 399): 87–109.2002 10.1097/00003086-200206000-00012. [DOI] [PubMed]
- 23.Baumgaertner MR, Curtin SL, Lindskog DM, et al. The value of the tip-apex distance in predicting failure of fixation of peritrochanteric fractures of the hip. J Bone Joint Surg Am. 1995;77(7):1058–64. doi: 10.2106/00004623-199507000-00012. [DOI] [PubMed] [Google Scholar]
- 24.Hasegawa K, Takegami Y, Tokutake K et al. Early versus delayed weight bearing after internal fixation for femoral neck fracture in younger adults: a multicenter retrospective study Injury. 55(2): 111292.2024 10.1016/j.injury.2023.111292. [DOI] [PubMed]
- 25.Zheng J, Wang H, Gao Y, et al. A study on the evaluation of a risk score of osteonecrosis of the femoral Head based on. Survival Anal J Arthroplasty. 2021;36(1):62–71. doi: 10.1016/j.arth.2020.07.046. [DOI] [PubMed] [Google Scholar]
- 26.Jin Z, Chen L, Wang D et al. A prediction model for osteonecrosis of femoral head after internal fixation with multiple cannulated compression screws for adult femoral neck fractures joint diseases and related surgery. 35(1): 20–6.2024 10.52312/jdrs.2024.975. [DOI] [PMC free article] [PubMed]
- 27.Tian P, Kuang L, Li ZJ et al. Comparison between femoral Neck systems and cannulated cancellous screws in treating femoral Neck fractures: a Meta-analysis geriatric orthopaedic surgery & rehabilitation. 13(10.1177/21514593221113533. [DOI] [PMC free article] [PubMed]
- 28.Cui Y, Ren G, Peng C et al. A novel Navigation device for Precise Percutaneous Placement of the Guidewire in femoral Neck fracture cannulated screw fixation surgery. IEEE J Translational Eng Health Med 12(10.1109/jtehm.2023.3332453. [DOI] [PMC free article] [PubMed]
- 29.De Camargo FP, De Godoy RM Jr. R Tovo Angiography in Perthes’ disease Clin Orthop Relat Res. 191): 216–20.1984. [PubMed]
- 30.Johnson EO, Soultanis K. P N Soucacos vascular anatomy and microcirculation of skeletal zones vulnerable to osteonecrosis: vascularization of the femoral head. Orthop Clin North Am. 35(3): 285–91, viii.2004 10.1016/j.ocl.2004.03.002. [DOI] [PubMed]
- 31.Gautier E, Ganz K. N Krügel, Anatomy of the medial femoral circumflex artery and its surgical implications the Journal of bone and joint surgery British volume. 82(5): 679–83.2000 10.1302/0301-620x.82b5.10426. [DOI] [PubMed]
- 32.Jacobs B. Epidemiology of traumatic and nontraumatic osteonecrosis. Clin Orthop Relat Res. 1978;130:51–67. [PubMed] [Google Scholar]
- 33.Tooke SM. Favero femoral neck fractures in skeletally mature patients, fifty years old or less. J Bone Joint Surg Am. 1985;67(8):1255–60. doi: 10.2106/00004623-198567080-00018. [DOI] [PubMed] [Google Scholar]
- 34.Soto-Hall R, Johnson LH. R A Johnson Variations in the Intra-articular pressure of the Hip Joint in Injury and Disease. A probable factor in avascular necrosis. J Bone Joint Surg Am. 46(509-516.1964. [PubMed]
- 35.Atsumi T. Role of impairment of blood supply of the femoral head in the pathogenesis of idiopathic osteonecrosis. Clin Orthop Relat Res. 1992;277:22–30. doi: 10.1097/00003086-199204000-00004. [DOI] [PubMed] [Google Scholar]
- 36.Rawall S, Bali K, Upendra B, et al. Displaced femoral neck fractures in the young: significance of posterior comminution and raised intracapsular pressure. Arch Orthop Trauma Surg. 2012;132(1):73–9. doi: 10.1007/s00402-011-1395-1. [DOI] [PubMed] [Google Scholar]
- 37.Gelberman RH, Gross MS. The vascularity of the wrist. Identification of arterial patterns at risk. Clin Orthop Relat Res. 1986;202:40–9. doi: 10.1097/00003086-198601000-00006. [DOI] [PubMed] [Google Scholar]
- 38.Orthopaedics Kodali siva r K P J C, R Research® CORR Insights®. Epiphyseal Arterial Network and Inferior Retinacular Artery seem critical to femoral Head Perfusion in Adults With Femoral Neck Fractures.2017. [DOI] [PMC free article] [PubMed]
- 39.Papadakis SA, Segos D, Kouvaras I et al. Integrity of posterior retinaculum after displaced femoral neck fractures Injury. 40(3): 277–9.2009 10.1016/j.injury.2008.07.024. [DOI] [PubMed]
- 40.Asnis SE, Wanek-Sgaglione L. Intracapsular fractures of the femoral neck. Results of cannulated screw fixation. J Bone Joint Surg Am. 1994;76(12):1793–803. doi: 10.2106/00004623-199412000-00005. [DOI] [PubMed] [Google Scholar]
- 41.Skedros JG, Baucom SL. Mathematical analysis of trabecular ‘trajectories’ in apparent trajectorial structures: the unfortunate historical emphasis on the human proximal femur. J Theor Biol. 2007;244(1):15–45. doi: 10.1016/j.jtbi.2006.06.029. [DOI] [PubMed] [Google Scholar]
- 42.Whitehouse WJ. E D Dyson scanning electron microscope studies of trabecular bone in the proximal end of the human femur. J Anat. 1974;118(Pt 3):417–44. [PMC free article] [PubMed] [Google Scholar]
- 43.Sverdlova N. Tensile trabeculae–myth or reality? J Musculoskelet Neuronal Interact. 2011;11(1):1–7. [PubMed] [Google Scholar]
- 44.Lu Y, Wang L, Hao Y et al. Analysis of trabecular distribution of the proximal femur in patients with fragility fractures. BMC Musculoskelet Disord 14(10.1186/1471-2474-14-130. [DOI] [PMC free article] [PubMed]
- 45.Daniel M, Iglic A, Kralj-Iglic V. The shape of acetabular cartilage optimizes hip contact stress distribution. J Anat. 2005;207(1):85–91. doi: 10.1111/j.1469-7580.2005.00425.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lane LB, Villacin A. Bullough the vascularity and remodelling of subchondrial bone and calcified cartilage in adult human femoral and humeral heads. An age- and stress-related phenomenon. J Bone Joint Surg Br. 1977;59(3):272–8. doi: 10.1302/0301-620X.59B3.893504. [DOI] [PubMed] [Google Scholar]
- 47.Budzik JF, Lefebvre G, Behal H et al. Assessment of the zonal variation of perfusion parameters in the femoral head: a 3-T dynamic contrast-enhanced MRI pilot study skeletal Radiol. 47(2): 261–70.2018 10.1007/s00256-017-2802-7. [DOI] [PubMed]
- 48.Jones JP Jr. Coagulopathies and osteonecrosis Acta Orthop Belg. 65 Suppl 1(5-8.1999. [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data will be available upon motivated request to the corresponding author of the present paper.