Abstract
Families with children who have access and mobility challenges, chronic illness, or intellectual or developmental disabilities require targeted messages before, during, and after disasters to ensure that they understand risks to their children’s health and can take measures to avoid harm and build resilience. A scoping review was conducted to assess current evidence for optimal ways to address the disaster information needs and communication preferences of families with children and youth with special healthcare needs. The disaster information needs of such families remain understudied, with few published evidence-based practices. Much of the relevant research focuses on information content, specifically the preparedness needs of these families; disaster recovery information for them remains a major gap. The few studies that have been performed suggest that parents with children and youth with special healthcare needs require additional information, education, and training to develop an effective disaster preparedness plan for their children. They are also largely unaware of schools’ disaster plans, and schools are often unable to meet parents’ expectations for timely, accurate information during a disaster. Several guidance documents highlighted the importance of completing an emergency information form before an event. Several studies suggested that one-on-one education or counseling was a strategy for encouraging preparedness planning; others highlighted potential value in incorporating families directly into disaster risk reduction planning. Evidence about channel preferences and their effectiveness in this population was generally lacking. Future studies should expand the evidence basis for optimal communication during all disaster phases both with parents of children and youth with special healthcare needs and with children directly.
Keywords: Public health preparedness/response, Risk communication, At-risk populations, Children and youth with special healthcare needs
Children and youth with special healthcare needs, including access and mobility challenges, chronic illness, and intellectual or developmental disabilities, are at high risk for severe health consequences in the wake of disasters. An estimated 200 million children worldwide experience some form of disability.1 In the United States alone, roughly 20% of households have a child with special healthcare needs, equating to roughly 11 million children.2 Children with medical complexity—defined as children with chronic, severe health conditions and major functional limitations—account for over one-third of pediatric healthcare costs, mostly arising from inpatient care.3 A nationwide survey found that nearly 50% of children with a disability require at least 5 or more specific healthcare services or have specialized medical equipment needs.4 These children are at high risk for severe outcomes during disasters.
Despite the vulnerabilities of this population, research on children with disabilities is lacking in the area of disaster preparedness and response.5,6 Research to date has focused largely on children in general, or adults with special healthcare needs, seldom focusing on the unique needs of children and youth with special healthcare needs.1 Additionally, when this population has been studied, families of these children and youth have been found to be no more prepared for disasters, and less so in some cases, compared to the general population.2,7 This is particularly concerning given that children and youth with special healthcare needs are more vulnerable to the effects of disruptions in electrical power and running water and interruptions in access to medications. They are also more likely to have communication challenges that complicate taking protective actions when necessary.8,9 As a result, families with children and youth with special healthcare needs have unique disaster information requirements that must be met to ensure that they understand the risks to their child’s health and can take measures to avoid harm and build resilience. However, little is known about the communication needs during disasters of vulnerable individuals and their families.10
To address this gap, we conducted a scoping review of the literature to identify the current evidence for optimal ways to address the disaster information needs and communication preferences of families with children and youth with special healthcare needs. The scoping review framework, which provides a systematic search methodology while allowing for a broad range of evidence, allowed us to both summarize and disseminate relevant research findings, as well as to identify research gaps in the existing literature.11 Our review examined the current evidence to date, based on research performed with families and stakeholders, systematic literature reviews, and expert opinion. This article describes the findings with respect to communication with parents and other stakeholders and with direct communication to children with differing health challenges.
Methods
To identify published peer-reviewed literature related to the disaster information needs of families of children and youth with special healthcare needs, we began with a search of 5 relevant indexed databases: CINHAL, PsychINFO, PubMed, Scopus, and Web of Science. We developed a keyword search string (see Figure 1) and adapted the search to each of the 5 databases. The development of the search string was an iterative process, and additional terms were considered for inclusion in the search. For example, we considered including disaster-specific keywords (eg, pandemic, earthquake, hurricane, etc), but we found that, although new articles were added to the sample, none fit the inclusion/exclusion criteria required to fit the final sample. Thus, these terms were not included in our final search string. Keywords such as “emergency room” and “emergency department” were also excluded from the search because of the large number of false-positives (ie, articles that did not meet the inclusion criteria) they generated. Our search did not include any date restrictions.
Figure 1.
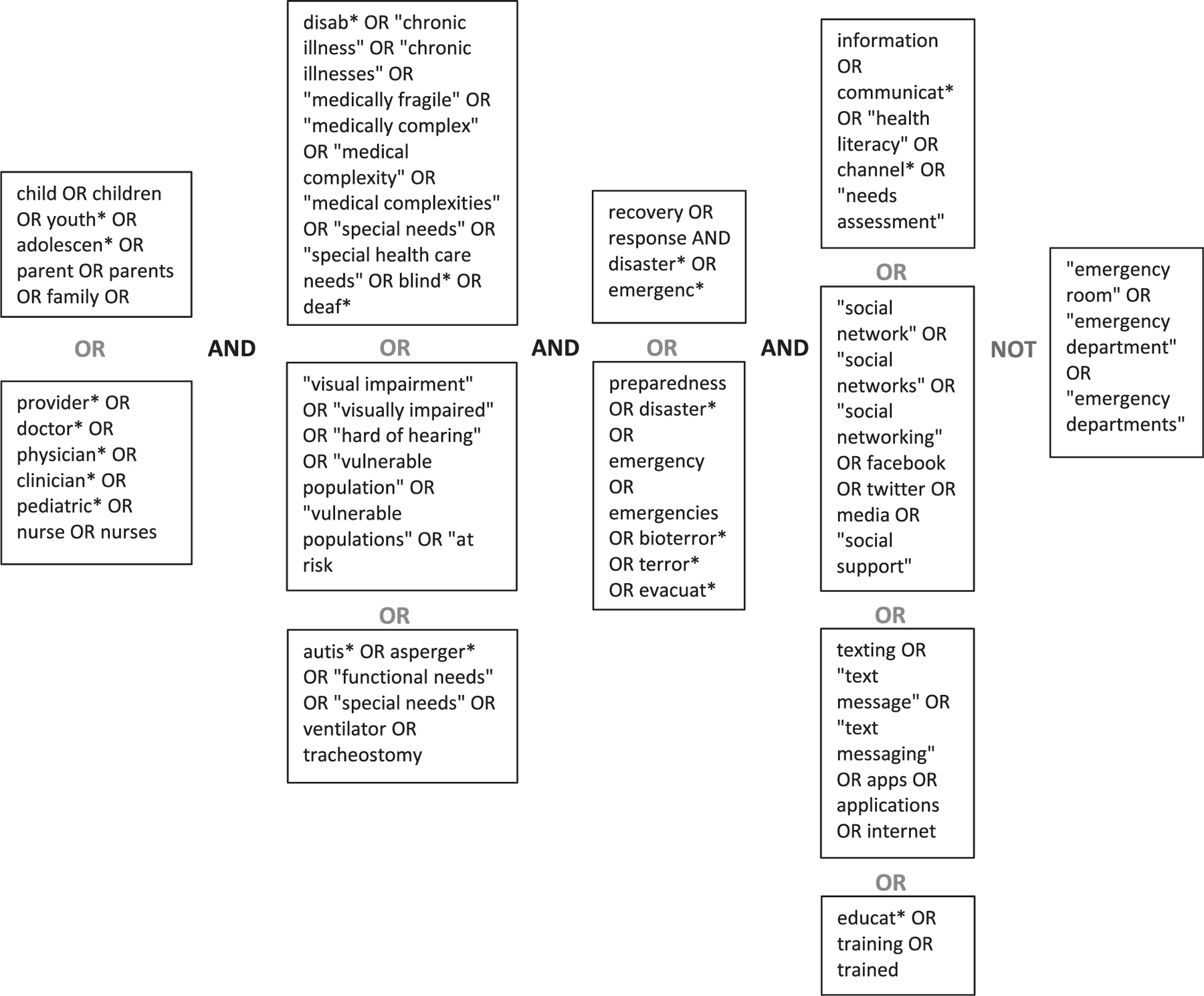
Search Strings
We anticipated that evidence would also exist outside of peer-reviewed literature, and we supplemented the initial search to capture relevant grey literature. We conducted searches in Google and the National Library of Medicine’s Disaster Lit Database, using keywords from our initial search string. Additionally, we searched the websites of relevant government agencies, emergency preparedness research centers, professional societies, and community-based organizations. Every organization whose website we searched was US-based, except the United Nations Office for Disaster Risk Reduction and the World Health Organization.
Inclusion criteria were developed prior to screening. Inclusion criteria stated that the article must: (1) be available in English; and (2) address some aspect of the disaster information needs of children with special healthcare needs, including content, channel, and/or source preferences. Exclusion criteria were developed after an initial review of the literature. The exclusion criteria stated that articles would be excluded if: (1) the article pertained only to adults with special healthcare needs or children in general (ie, not specific to children with special healthcare needs); and (2) they were in a format other than one of the following:
Peer-reviewed journal article
Conference presentation
Dissertation
Guidance document, white paper, or report from a government agency, think tank, NGO, or academic research center (eg, websites and blog posts were excluded from the final sample)
The initial search of the 5 indexed databases, completed between August 16 and October 20, 2017, produced 1,741 unique results after duplicates were removed (see Figure 2). Three reviewers screened these articles based on title and abstract, searching for any content relevant to children and disasters; 1,648 articles did not address these broad criteria or were not available in English and, as a result, were excluded.
Figure 2.
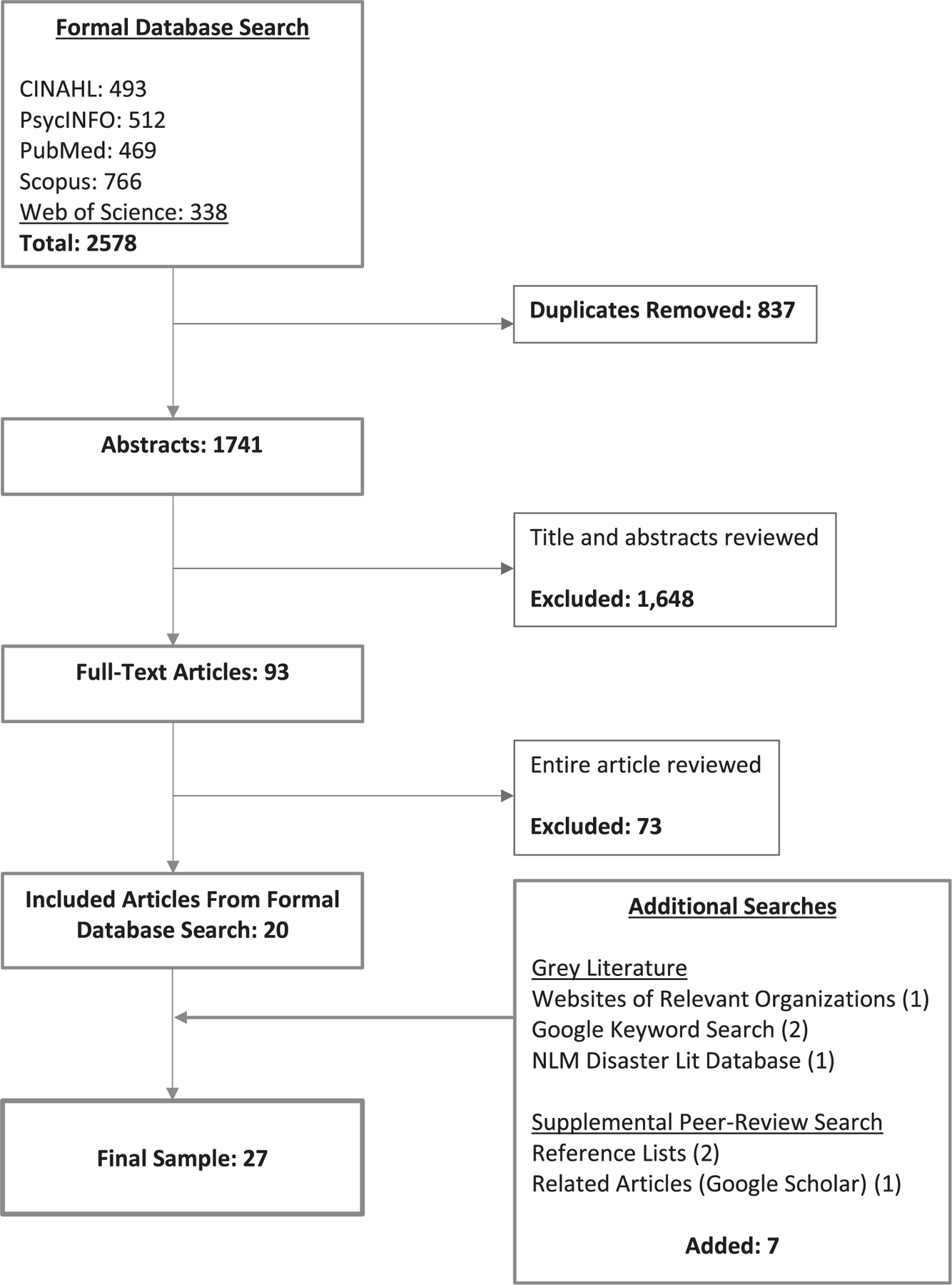
Flowchart of Search and Review Process
Two reviewers then conducted a full-text review of the remaining 93 articles, resulting in 20 articles that met the criteria. When any disagreements occurred, a consensus was reached through discussion. Following the indexed database search, we conducted the grey literature search using the same inclusion and exclusion criteria. Finally, to ensure a comprehensive review of the literature, we reviewed the reference lists and conducted a “related articles” search in Google Scholar for each of the articles included in our sample. Along with the grey literature search, this process added 7 new articles, resulting in a final sample of 27 articles.
Articles in the final sample were reviewed and coded based on a number of categories:
study type: original research, review article, or other (which encompassed guidance documents, commentaries, and expert opinion)
type of special healthcare need on which the article focused (eg, autism spectrum disorders)
type of disaster (eg, winter storm)
phase of disaster (preparedness, response, recovery)
Articles that focused broadly on children and youth with special healthcare needs (eg, addressed children with different types of healthcare needs, including physical disabilities, intellectual or developmental disabilities, or technology or medication dependency) were coded as “broad children and youth with special healthcare needs,” and articles that focused on disasters in general were coded as “all-hazards.” We coded for disaster phase based only on findings relevant to the information needs of children and youth with special healthcare needs, not whether a phase was considered at any point in the article. Three investigators (TH, EC, RD) descriptively coded each article based on its finding and key recommendations. These codes were then organized by themes (content, channel, and source preferences), which align with measures commonly used in the health information–seeking literature.12 Specifically, content refers to the information conveyed in a communication; source refers to the person or agency from which the communication comes; and channel refers to the mechanism or format for the communication. Summaries were produced for each of these themes, compared with each other, and consolidated for this review. Discrepancies were resolved by discussion.
Results
Study Characteristics
Our search methodology and the application of our inclusion/exclusion criteria yielded 27 articles; the dates of publication for articles in the final sample ranged from 2002 to 2017. Table 1 details the distribution of studies by article type. Twenty of the articles (74%) were from peer-reviewed journals, while 7 (26%) were grey literature, including white papers from nonprofit organizations, a technical report and policy statement from a professional society, unpublished research presented at a national conference, and a dissertation. Twelve of the articles (44%) described the results of original research studies, including 6 survey-based studies, 5 qualitative studies, and 1 mixed-methods study. Three articles in the final sample were review articles (11%), while 12 of the articles were guidance documents or commentaries that did not incorporate original data (46%). With respect to article type, the grey literature featured the same even distribution of original research articles and guidance documents as the peer-reviewed literature. Most of the articles from the overall sample (78%) focused broadly on children with a wide range of healthcare needs. Six articles (22%) focused on a specific group, with 3 articles focused on children with autism spectrum disorders or developmental disabilities, 1 on children with cognitive or language processing challenges, 1 on chronic illnesses, and 1 on children with hearing impairments.
Table 1.
Overview of Article Type
| Original Research | Review Article | Guidance Document | Subtotal | |
|---|---|---|---|---|
| Article Type | ||||
| Peer-reviewed | 9 | 2 | 9 | 20 (74%) |
| Grey literature | 3 | 1 | 3 | 7 (26%) |
| Subtotal | 12 (44%) | 3 (11%) | 12 (44%) | N = 27 |
| Type of special healthcare needs | ||||
| Broad | 10 | 3 | 8 | 21 (78%) |
| Specific healthcare needs | 2 (autism spectrum disorders; developmental disabilities) | 0 | 4 (autism spectrum disorders; cognitive or language processing challenges; chronic illnesses; hearing-impaired) | 6 (22%) |
| Disaster type | ||||
| All-hazards | 8 | 3 | 8 | 19 (70%) |
| Specific hazard | 4 (natural disasters) | 0 | 4 (terrorism [2]; infectious disease; humanitarian emergencies) | 8 (30%) |
| Disaster phase a | ||||
| Preparedness | 10 (83%) | 3 (100%) | 10 (83%) | 23 (85%) |
| Response | 3 (25%) | 2 (67%) | 7 (58%) | 12 (44%) |
| Recovery | 0 | 1 (33%) | 2 (17%) | 3 (11%) |
| Number of articles by type (denominator) | 12 | 3 | 12 | N = 27 |
Several studies addressed more than 1 phase of disaster. See Table 2 for additional details.
Regarding disaster type, 19 articles (70%) focused broadly on disasters in general, taking an “all-hazards” approach to disaster communication. Four of the articles focused on natural disasters, and 2 focused on terrorism. Additionally, 1 focused on an infectious disease outbreak and 1 on humanitarian emergencies. Most of the articles in the sample (85%) focused on the disaster preparedness phase (eg, planning prior to a disaster to improve outcomes). Twelve of the articles (44%) presented findings related to the response phase (eg, activities taken during a disaster to prevent injury), in which the focus was on communicating during a disaster. Only 3 articles (11%) provided relevant findings pertaining to the recovery phase (eg, actions taken after a disaster to facilitate return to normal or safer situation), in which the focus was on communication following a disaster. Five of the articles addressed disaster communications in international settings; the remainder focused on US-based disaster communications. Of the 5 articles that focused on disaster communications outside of the United States, 2 addressed communications during disasters that affect low- and middle-income nations. Table 2 provides a summary of all the articles included in this review sample, with detailed information on article type, study design (as relevant), target audience, and phase and type of disaster.
Table 2.
Summary of Included Articles in Scoping Review Sample
| Author, Year | Article Type | Research Design | Type of Healthcare Needs | Disaster Phase | Disaster Type | |
|---|---|---|---|---|---|---|
| 1 | Amer Acad Peds, 2010 | Guidance | N/A | Broad | Preparedness | All hazards |
| 2 | Asher A, 2009 | Guidance | N/A | Broad | Preparedness | All hazards |
| 3 | Bagwell HB, 2016 | Research | Survey of caregivers (n = 223) | Broad | Preparedness | All hazards |
| 4 | Baker, 2010 | Research | Survey of caregivers (n = 145) | Broad | Preparedness | All hazards |
| 5 | Baker, 2012 | Research | Survey of caregivers, pre/post preparedness intervention (n = 238) | Broad | Preparedness | All hazards |
| 6 | Baker, 2012 | Research | Survey of caregivers, pre/post preparedness intervention (n = 210) | Broad | Preparedness | All hazards |
| 7 | Barnes, 2013 | Research | Interviews of parents and professionals (n = 22) | Broad | Preparedness, Response | All hazards |
| 8 | Cancro, 2009 | Guidance | N/A | Broad | Response | All hazards |
| 9 | Claessens, 2016 | Research | Case study: report review, interviews, and focus groups (n = 1,853 children) | Broad | Response | Earthquake |
| 10 | Committee on Pediatric Emergency Medicine, 2012 | Guidance | N/A | Broad | Preparedness | All hazards (rural impact) |
| 11 | Edmonds, 2017 | Guidancea | N/A | Autism spectrum disorders | Preparedness, Response | All hazards |
| 12 | Fifolt, 2017 | Research | Interviews of professionals, service organization leaders (n = 22) | Broad | Response | Natural disaster |
| 13 | Friehe, 2002 | Guidance | N/A | Cognitive or language processing challenges | Recovery | Terrorism |
| 14 | Hamann, 2016 | Research | Survey of caregivers (n = 287); RCT of preparedness intervention | Broad | Preparedness | All hazards |
| 15 | Hill-Patterson, 2010 | Guidance | N/A | Hearing impaired | Preparedness, Response | All hazards |
| 16 | Lou, 2007 | Research | Survey of parents and professionals; interviews of parents (n = 65), professionals (n = 23); evaluation of education intervention | Autism spectrum disorders | Preparedness | All hazards |
| 17 | Markenson, 2006 | Guidance | N/A | Broad | Preparedness, Response | All hazards (terrorism focus) |
| 18 | Meredith LS, 2008 | Reviewb | Review of literature; case study entailed interviews with professionals in 4 jurisdictions (n = 50) including government, community organizations | Broad | Preparedness | All hazards (focus on natural disaster, terrorism) |
| 19 | Murray, 2011 | Review | N/A | Broad | Preparedness, Response | All hazards |
| 20 | Natl Assn School Psychologists, 2002 | Guidance | N/A | Broad (specific guidance for autism; learning disabilities; cognitive limitations; visual, hearing, and physical challenges) | Preparedness, Response, Recovery | Terrorism |
| 21 | Peacock, 2012 | Guidance | N/A | Broad | Preparedness, Response | Influenza pandemic |
| 22 | Ronoh, 2015 | Research | Focus groups with children and youth with special healthcare needs (n = 10); interviews with caregivers, teachers, emergency response organization representatives (n = 5) | Broad | Preparedness | Earthquake |
| 23 | Ronoh, 2017 | Research | Focus groups with children and youth with special healthcare needs (n = 20) in 2 jurisdictions with different disaster risks; interviews with teachers, parents, emergency response organization representatives (n = 14) | Broad | Preparedness | Natural disaster |
| 24 | Stallwood, 2006 | Guidance | N/A | Chronic illnesses | Preparedness | All hazards |
| 25 | Stough, 2017 | Review | N/A | Broad | Preparedness, Response, Recovery | All hazards (specific inclusion of terrorism) |
| 26 | UNICEF, 2017 | Guidance | N/A | Broad | Preparedness, Response | Humanitarian emergencies |
| 27 | Wolf-Fordham, 2015 | Research | Survey of parents, caregivers (n = 314) | Developmental disabilities (included autism) | Preparedness | All hazards |
Edmonds, 2017, was coded as a guidance document given its primary focus, although it did include original research in the form of expert review of materials.
Meredith, 2008, was coded as a review article, given its primary focus, although it did incorporate a case study approach in which professionals were interviewed.
Thematic Analysis
Our review found few publications that presented original research or evidence-based recommendations on the best ways to meet the information needs of these high-risk families during emergencies. Much of the content in the literature referred to activities related to preparedness before disasters, generally with a broad, all-hazards approach that was not customized for children with different types of healthcare challenges. Specific findings related to content needs, channel preferences, and source preferences of families of children and youth with special healthcare needs are summarized below.
Content: Needs and Recommendations
Preparedness Education
Most of the relevant findings with respect to content needs and recommendations pertained to improving preparedness of families with children and youth with special healthcare needs. A number of studies corroborated findings from the broader disaster literature, indicating that these families are poorly prepared for disasters.13–17 Disaster preparedness among families living in rural areas, with reduced access to health and emergency response resources, was also low, although 1 study showed that rural families whose children had physical disabilities were more likely to have emergency plans than were families with children with developmental or intellectual disabilities.18 Parents also identified that they were unaware of community resources that might be helpful during emergencies.17 As a result, preparedness education was cited as an important need for families of children and youth with special healthcare needs.
More specific to communication, multiple studies showed that only roughly 10% of these families had a family emergency communication plan—that is, a plan to reach family members when networks may be disrupted, including a paper copy of contact information for family and other key support individuals, such as doctors and service providers.14,15 Additionally, parents were largely unaware of their child’s school disaster plan and were unlikely to have spoken with their child’s school or healthcare provider about a plan.17,19 Parental expectation for immediate communication during disasters outstrips most schools’ ability to provide accurate, approved communication,20 and several studies highlighted the importance of getting information regarding school-based emergency response plans in advance of disasters.17,19–21 Recommendations for how best to inform parents of these plans included emphasizing how children will be cared for during a disaster, providing precise details on how parents will be reunited with their children following a disaster, and offering parents an opportunity to participate in disaster drills so they can familiarize themselves with these plans firsthand.20
Parents also expressed a need for preparedness education and training. They indicated an interest in a wide variety of topics, including an understanding of local emergency resources; strategies for discussions with schools and with their child’s healthcare providers; help developing family emergency plans, with a focus on the specific needs of their child; strategies for approaching local emergency officials to discuss the needs of their child; and information on using local shelter sites.13,16,17 These findings suggest that parents, a key target audience in this context, recognize the need for additional education and have provided specific content areas on which future training efforts should focus.
Messaging and Interventions that Increase Preparedness
A number of studies highlighted specific ways in which information could help to address the preparedness education needs among families with children and youth with special healthcare needs. One study found that although parents wanted to complete preparedness tasks, a lack of knowledge about how to do so was the primary reason they were not completing these tasks.14 Another study conducted with rural families found that parents of children and youth with special healthcare needs with higher levels of self-efficacy, as measured by their confidence in their abilities to complete disaster-related tasks without assistance, also had the highest levels of disaster preparedness.18 These findings suggest that when addressing the need for disaster preparedness education, effective interventions are those that increase parents’ knowledge of specific preparedness tasks and increase their belief that they are capable of performing those tasks. Parents’ perceived level of social support and perceived ability to receive assistance from external sources (including relatives, friends, neighbors, community-based agencies, family doctors, and emergency medical services) were also tied to increased levels of preparedness, suggesting additional variables to target in future education interventions.18
Other studies found that providing a brief counseling session with educational materials led to an increase in preparedness levels. One 10- to 20-minute intervention conducted by trained health educators provided parents with preparedness information, including potential barriers that might inhibit completion of preparedness tasks and guidance for completing an emergency information form (EIF) with their providers, and significantly improved parents’ preparedness levels.15 Another intervention provided parents with a disaster starter kit that included supplies and handouts with preparedness information, including a blank emergency information form and instructions for how to complete it. Following the intervention, 79% of families had completed an emergency information form, compared to only 43% beforehand.13 While sustained and ongoing efforts may be necessary to ensure that families of children and youth with special healthcare needs are prepared for disasters, each of these interventions points to efficient and effective ways to increase disaster awareness and preparedness.
The emergency information form is an important component of preparedness for families of children and youth with special healthcare needs and has been used by many interventions.22–25 A completed form provides a summary of a child’s medical conditions, medications, and special healthcare conditions in order to optimize the provision of emergency medical care by a provider who is not familiar with the child’s medical needs.22
In addition to facilitating the communication of complex medical management considerations, completing the emergency information form can initiate the process of preparedness planning for families, allowing pediatricians to educate them on power-loss contingency plans, medication supply and medical equipment maintenance, and how household members can assume the role of in-home healthcare providers when necessary.23 Similar frameworks that could be tailored to the unique needs of individual families were also mentioned, including individual emergency and evacuation plans.26,27
Another area of focus was an emphasis on the need to incorporate children and youth with special healthcare needs themselves into the development of content intended to help them and their families prepare for disasters. Children with disabilities are often not included in emergency planning or training, as these initiatives are typically aimed at adult caregivers, including parents and teachers.16,28 A number of studies cited the need for tailored content for children, including ability- and age-appropriate resources,25,29,30 and the importance of input from children in the development of this content.28,31 Suggestions included involving children and youth with special healthcare needs in school-based drills and exercises32 and including them in the design, review, and dissemination of communication materials.33 Children with both intellectual and physical disabilities who engaged in pre-event emergency preparedness planning have demonstrated good awareness of natural hazards and self-protective actions for disasters.31 A common theme from the literature was that communication interventions should be targeted to the unique needs of children and youth with special healthcare needs,28–32 and input from children themselves could help in this regard. Table 3 summarizes the content needs as well as preferred channels and sources for providing preparedness-related information for families with children and youth with special healthcare needs.
Table 3.
Disaster Communication Preferences for Families with Children and Youth with Special Healthcare Needs
| Preferred content | ● Education and training in family emergency planning ● Information on local emergency resources ● Use of emergency information form (EIF) ● School emergency plan information ● Content directed specifically to children’s needs; developmental level, tailored to communication challenges ● Content informed by children and youth with special healthcare needs—risk perceptions and challenges with protective behaviors, customized to age and disability ● Mental health of children following disasters |
| Preferred sources | ● Healthcare professionals, including pediatricians, occupational therapists ● School personnel, including administrators, nurses, teachers ● Local government officials |
| Preferred channels | ● In-person meetings, one-on-one training ● Hybrid (in-person/online) forums hosted by schools, service organizations ● Brochures, videos, web-based resources—for use by medical practices ● Text messages from schools to parents/families (during emergencies) ● Social media (during emergencies) |
Content for Response and Recovery: Communicating Directly
While most of the literature focused on the disaster preparedness phase, some findings were relevant to the response and, to a lesser extent, recovery phases. Findings pertaining to the response phase centered around the need to communicate with children with specific disabilities during disasters. One study examined the 2015 Nepal earthquake and found that information provided during the event was not inclusive of children with disabilities; the study stressed the need for more targeted and accessible information.34 Recommended practices for children with communication challenges such as autism,26,29 hearing impairments,26,35 and visual impairments26 included use of specific alerting devices; visual depictions of appropriate behaviors and response activities, including the use of communication boards; creating “social stories” that reinforce appropriate behaviors during disasters; and encouraging children to carry “in case of emergency” cards that instruct responders and others in how best to communicate with them.20,34
Table 4 summarizes recommendations for communicating with children and youth with special healthcare needs during disasters, abstracted from the articles in this review. For the most part, the audiences for these recommendations are parents, caregivers, schools, and teachers who work directly with these children before, during, and after emergencies. However, they are relevant for health and social service professionals as well as emergency response organization representatives who are engaged in emergency preparedness and response activities that involve children and youth with special healthcare needs. Content related to communicating post-disaster was relatively sparse but focused on ways to address the mental healthcare needs of children and youth with special healthcare needs following a terrorism event, including helping students feel safe and learn how to cope with their emotions.16,26,36
Table 4.
Recommendations for Communicating During Disasters with Children and Youth with Special Healthcare Needs
| Pre-event communication planning | ● Engage children and youth with special healthcare needs in disaster risk reduction planning to understand perceptions of risk, challenges28,31,33 ● Engage children and youth with special healthcare needs as disaster communication plans are being developed, to understand how they access and use resources31–33 ● Involve children and youth with special healthcare needs in drills and exercises32 ● Develop communication resources that are appropriate for age, developmental stage, and abilities, communication challenges28–32 ● Agree on warning signals for potential hazards and associated protective actions31,35 ● Agree on evacuation strategies and a plan for reunification, and ensure parents are aware that their children will be cared for during a disaster20,28 ● Use “social stories” to reinforce appropriate behaviors during disasters for children with autism or intellectual or developmental disabilities29 ● Encourage use of “in-case-of-emergency” communication tools by children who may not be able to communicate their needs during disasters29,35 |
| Communication during disasters | ● Use communication materials in different formats to reach children with physical, intellectual, hearing, and visual challenges: ○ Simple language and visual depictions of appropriate behaviors and response activities, including use of pictograms, communication boards, drawings, and photographs for children with intellectual disabilities26,29 ○ Large print, text messages with free voice-over applications, Braille, radio and audio announcements for children with visual impairments26 ○ Print, text messages, captions, and sign language interpretations for children with hearing impairments26,35 ● Integrate photographs, images of children and youth with special healthcare needs into disaster-related information, depicting children with disabilities among groups of children (rather than separated) and actively participating in appropriate response activities34 |
Preferred Sources
Studies cited a variety of important sources of disaster information for families of children and youth with special healthcare needs. In a number of studies, primary care providers were suggested as effective sources of disaster information for these families,23,25 including as a source of preparedness education and disaster planning.13,24,37 With respect to preparedness training needs, parents of children with autism indicated that they wanted to receive emergency preparedness training from autism specialists, school personnel, and representatives from local government.19 Occupational therapists were also identified as potentially effective sources of information for children and youth with special healthcare needs for emergency evacuation planning, particularly for children with access and mobility as well as behavioral challenges.27
Schools were cited as an important source of information for families of children and youth with special healthcare needs, across all phases of disasters. Several studies in this review identified schools as key venues to provide education and training in disaster preparedness to these families. School-based preparedness planning, including exercises and drills that engage children and youth, have been used successfully to improve preparedness.32 Additionally, school nurses and childcare health consultants were cited as important sources of information who can assist schools, childcare facilities, and parents in planning what to do during an emergency.30 During disasters, schools serve as an important source of information for both children and their parents and caregivers.21 Teachers, including those devoted to special education, were found to be effective providers of information to parents during disasters and effective providers of emotional support to children and youth, helping to make them feel safe during disasters and to recover following disasters.16 Additionally, locating mental health services in school facilities in the wake of disasters may help to normalize these services and lessen stigma associated with using them.16
Preferred Channels
A number of channels were mentioned, both as a means to deliver pre-event training and education as well as a mechanism to communicate with parents and caregivers during disasters. Customized one-on-one education sessions to promote preparedness have been effective, particularly when accompanied by interventions such as providing emergency supplies and assisting with the completion of emergency information forms.13,15,38 In surveys on preferred preparedness training formats, families with children and youth with special healthcare needs indicated preferences for combined online/in-person strategies (group) and receiving training in schools with other parents and in combination with DVD viewing.17,19 One author speculated that the preference for in-person training in group sessions might reflect the importance of parent-to-parent mutual support and the value of connecting with parents who have similar challenges.17
During disasters, mass media (eg, television, radio) have been the traditional channels used to convey information, but they may not be effective in reaching families with children and youth with special healthcare needs.38,39 One study interviewed leaders of organizations who cared for such children and youth during a 2014 winter storm and found that media outlets had limited capacity to provide sufficient detail related to facility closures to parents, which led to confusion among families.39 The same study cited the use of social media by hospitals and schools to respond to questions, request needed supplies, and reassure families that their children were well cared for by posting photographs of children eating and engaging in activities. Another article cited the effectiveness of an emergency messaging platform that enabled schools to send real-time alerts to parents via email and SMS texts during the H1N1 outbreak.21 The importance of communicating across multiple formats in order to increase the likelihood that families receive the information was also mentioned.34 Though these findings suggest the potential of a number of channels, evidence about channel preferences and the effectiveness of specific channels was generally lacking for families with children and youth with special healthcare needs.
Discussion
The objectives of this scoping review were to summarize and disseminate the research findings and expert recommendations for communicating with families who have special healthcare needs in the context of disasters, and to identify research gaps that can be addressed in this area. Fewer than half of the 27 articles in our sample reported on findings from primary data collected from families, children, and other stakeholders in the special healthcare needs community; the remaining articles summarized reviews of published literature or expert opinions regarding their communication needs and preferences during emergencies. Thus, there is little evidence for the optimal ways to communicate with families with children and youth with special healthcare needs during disasters. The findings from the few relevant research articles need to be corroborated by additional studies that define outcomes and focus on the impact of communication during all phases of disasters. Most articles identified in this review focused specifically on preparedness-related information for “all-hazards,” and they were directed broadly to children with a wide range of special healthcare needs. The optimal communication content, preferred sources, and channels necessary to reach families and children with different types of disabilities remain understudied. Moreover, all but 2 of the articles in this review addressed disaster communications in high-income countries, mainly in the United States. Our findings may be less relevant to low- and middle-income countries, which bear the brunt of most disasters and where access to new communication technologies and health system infrastructure may be more limited.
Our review identified that families believe they need better information related to how to prepare for disasters. Successful efforts to improve emergency preparedness for families with children and youth with special healthcare needs have involved one-on-one sessions with educators who assist with completion of emergency information forms—a major component of preparedness planning for children and youth with special healthcare needs—and demonstrate the need to improve caregivers’ knowledge and self-efficacy with respect to preparedness tasks. The literature also identifies examples of specific content about which parents desire more information and training, providing important insight for future communication interventions. Healthcare professionals and service providers who are familiar with a child’s specific medical needs have great potential to serve as trusted sources of information and effective advisors for families with children and youth with special healthcare needs. Family-centered care coordination that occurs through medical homes that provide interdisciplinary and enhanced care to children with complex medical needs may be optimal settings to provide emergency planning support for these families and to customize communication plans, evacuation plans, and other important preparedness activities.40–42 Emergency response organizations that serve these populations might collaborate more closely with trusted professionals as they work to improve the preparedness of at-risk children and increase their capacity to reach families during emergencies. Additionally, while parents and caregivers represent a primary audience for disaster information in this context, the literature also demonstrates the need to involve children and youth with special healthcare needs in preparedness planning and education, a strategy that has not occurred often to date but that shows promise in addressing the overall lack of preparedness in this population. Studies are needed to assess effective ways to accomplish these activities and to assess their impact.
Given the amount of time that children spend out of home and in childcare and school settings, our findings that schools are recognized as important sources of emergency preparedness information is perhaps not surprising. Families identified that they needed more information about their children’s school emergency plan and generally have high expectations for school-to-parent communication during emergencies. However, studies have shown that school and childcare center disaster plans are typically neither comprehensive nor inclusive of children and youth with special healthcare needs.6,43–45 Thus, schools should be assured of sufficient resources to improve their capacity to meet the needs of these families before, during, and after disasters.
Limitations
There are several limitations worth noting in this review. Studies were included only if they were written and published in English. It is thus possible that some relevant publications may have been excluded. However, our review used a broad approach to capture published literature in 5 structured databases that encompass literature in the health sciences, as well as grey literature relevant to this area.
Second, our focus on literature that specifically addressed the disaster communication needs of children with special healthcare challenges also narrowed the sample; the number of actual research studies with evidence-based recommendations for this population were few, and the total number of participants in the surveys, interviews, and focus groups that were reported here reflect a very small percentage of the families and children with special healthcare needs in the general population.
Finally, it is important to note that the majority of research included in this review was not focused primarily on the information needs of families with children and youth with special healthcare needs, but instead focused on their general needs during disasters. This contributed to the relative lack of relevant findings pertaining to the specific emergency communication needs of these families.
Research Gaps and Suggestions for Future Studies
A common theme from the literature was that communication interventions should be targeted to the unique needs of children and youth with special healthcare needs.28–32 This group represents a diverse audience with unique healthcare needs, and, as a result, they have unique information needs during a disaster. Similarly, natural disasters pose different risks than pandemics or terrorist events, and each phase of a disaster requires that different types of information needs be met. Despite this, most of the existing literature focuses broadly on all children with disabilities and on disasters in general and focuses primarily on their preparedness needs. Additional research is needed to better understand the needs generated by particular disabilities and contexts so that targeted interventions for children and youth with special healthcare needs can be developed for different disaster situations and across all phases of the disaster lifecycle. In particular, children with technology dependence or physical disabilities have different needs than children with communication challenges or intellectual disabilities; these differences will likely affect both information content and channels during disasters.
This review identified several specific gaps with respect to the content, source, and channel preferences of families with children and youth with special healthcare needs. The information and specific messages needed during the pre-event or preparedness phase of disasters have received the most attention, but additional work is required to address specific concerns of families whose children have different types of disabilities. Knowledge of their content needs and information preferences as disasters are unfolding and during the recovery phase remain a significant gap. Studies that explore these needs during different phases of disasters would allow emergency response organizations and healthcare and other professionals to meet them in a more targeted fashion, and perhaps more effectively.
With respect to sources, while many articles point to the potential of healthcare providers as trusted sources of information, there is also a need to identify the capacity of these providers to communicate with patients before, during, and after disasters. Specifically, do they have the knowledge required to convey critical information, and do they have the technological resources necessary to reach families? Additionally, there were few articles in this sample that addressed optimal platforms for communicating with families with children and youth with special healthcare needs. Several studies suggested that mass media is less effective for this purpose and demonstrated the potential of social media channels and text messaging systems, particularly from trusted sources. However, additional research is needed both in terms of the effectiveness of these channels in reaching families of children and youth with special healthcare needs during disasters and regarding channels that these families prefer to use before, during, and following disasters.
More evidence-based research is needed that is explicitly devoted to the information needs and information-seeking behaviors of families with children and youth with special healthcare needs before, during, and after disasters. Related areas of research may provide an effective blueprint for better understanding these information needs. For example, there is considerably more published literature and a more robust evidence base for optimal communication practices for meeting the health information needs of families with children and youth with special healthcare needs outside of the disaster context. These studies focus explicitly on the information-seeking behaviors of these families and suggest that healthcare providers and peer networks are trusted sources of information46–48 and that the internet, including online forums and social media channels, are important channels for both information and social support.49,50 Future research should explore whether these preferences apply to families with children and youth with special healthcare needs during emergencies.
Conclusion
The disaster communication and information needs and preferences of families with children and youth with special healthcare needs remain understudied. Targeted communication before, during, and after disasters has the potential to improve their preparedness and overall outcomes. This review suggests that healthcare providers and schools are important sources of information for these families before and during emergencies and that they can facilitate key preparedness activities such as completion of an emergency information form. Future studies should expand the body of evidence for optimal communication during all disaster phases both with parents of children and youth with special healthcare needs and with children directly.
Contributor Information
Thomas J. Hipper, Center for Public Health Readiness and Communication, Department of Environmental and Occupational Health.
Renee Davis, Program Coordinator/Research Associate, Maternal and Child Health Program, Department of Community Health and Prevention.
Philip M. Massey, Department of Community Health and Prevention; all are at Drexel University Dornsife School of Public Health, Philadelphia, PA.
Renee M. Turchi, Section Chief, General Pediatrics, St. Christopher’s Hospital for Children, Drexel University, College of Medicine, Department of Pediatrics, Philadelphia, PA.
Keri M. Lubell, Division of Emergency Operations, Office of Public Health Preparedness and Response, Centers for Disease Control and Prevention, Atlanta, GA.
Laura E. Pechta, Division of Emergency Operations, Office of Public Health Preparedness and Response, Centers for Disease Control and Prevention, Atlanta, GA.
Dale A. Rose, Division of Emergency Operations, Office of Public Health Preparedness and Response, Centers for Disease Control and Prevention, Atlanta, GA.
Amy Wolkin, Office of Public Health Preparedness and Response, Centers for Disease Control and Prevention, Atlanta, GA.
Lisa Briseño, Division of Emergency Operations, Office of Public Health Preparedness and Response, Centers for Disease Control and Prevention, Atlanta, GA.
Jessica L. Franks, Health Communications Fellow, Division of Human Development & Disability, Centers for Disease Control and Prevention, Atlanta, GA, and Oak Ridge Institute for Science and Education, CDC Research Participation Programs, Oak Ridge, TN.
Esther Chernak, Center for Public Health Readiness and Communication, and Associate Clinical Professor, Department of Environmental and Occupational Health, Drexel University Dornsife School of Public Health, and Drexel University College of Medicine, Philadelphia, PA.
References
- 1.Peek L, Stough LM. Children with disabilities in the context of disaster: a social vulnerability perspective. Child Dev 2010; 81(4):1260–1270. [DOI] [PubMed] [Google Scholar]
- 2.Baker LR, Cormier LA. Disasters and Vulnerable Populations: Evidence-Based Practice for the Helping Professions New York: Springer Publishing Company; 2014. [Google Scholar]
- 3.Berry JG, Hall M, Neff J, et al. Children with medical complexity and Medicaid: spending and cost savings. Health Aff (Millwood) 2014;33(12):2199–2206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.National Survey of Children with Special Healthcare Needs (NC-CSHCN). Child and adolescent health measurement initiative 2009/2010. http://www.childhealthdata.org/learn/NS-CSHCN. Accessed April 27, 2018. [Google Scholar]
- 5.Ronoh S, Gaillard JC, Marlowe J. Children with disabilities and disaster risk reduction: a review. Int J Disaster Risk Reduct 2015;6(1):38–48. [Google Scholar]
- 6.Boon HJ, Brown LH, Tsey K, et al. School disaster planning for children with disabilities: a critical review of the literature. Int J Spec Educ 2011;26(3):223–237. [Google Scholar]
- 7.Goodhue CJ, Demeter NE, Burke RV, Toor KT, Upperman JS, Merritt RJ. Mixed-methods pilot study: disaster preparedness of families with children followed in an intestinal rehabilitation clinic. Nutr Clin Pract 2016;31(2):257–265. [DOI] [PubMed] [Google Scholar]
- 8.Dolan MA, Krug SE. Pediatric disaster preparedness in the wake of Katrina: lessons to be learned. Clin Pediatr Emerg Med 2006;7(1):59–66. [Google Scholar]
- 9.Mace SE, Doyle CJ. Patients with access and functional needs in a disaster. South Med J 2017;110(8):509–515. [DOI] [PubMed] [Google Scholar]
- 10.Uscher-Pines L, Hausman AJ, Powell S, DeMara P, Heake G, Hagen MG. Disaster preparedness of households with special needs in southeastern Pennsylvania. Am J Health Behav 2009;37(3):227–230. [DOI] [PubMed] [Google Scholar]
- 11.Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol 2005;8(1):19–32. [Google Scholar]
- 12.Anker AE, Reinhart AM, Feeley TH. Health information seeking: a review of measures and methods. Patient Educ Couns 2011;82(3):346–354. [DOI] [PubMed] [Google Scholar]
- 13.Bagwell HB, Liggin R, Thompson T, et al. Disaster preparedness in families with children with special healthcare needs. Clin Pediatr 2016;55(11):1036–1043. [DOI] [PubMed] [Google Scholar]
- 14.Baker LR, Baker MD. Disaster preparedness among families of children with special healthcare needs. Disaster Med Public Health Prep 2010;4(3):240–245. [DOI] [PubMed] [Google Scholar]
- 15.Baker LR, Cormier LA. Disaster preparedness and families of children with special needs: a geographic comparison. J Community Health 2013;38(1):106–112. [DOI] [PubMed] [Google Scholar]
- 16.Stough LM, Ducy EM, Kang D. Addressing the needs of children with disabilities experiencing disaster or terrorism. Curr Psychiatry Rep 2017;19(4):24. [DOI] [PubMed] [Google Scholar]
- 17.Wolf-Fordham S, Curtin C, Maslin M, Bandini L, Hamad CD. Emergency preparedness of families of children with developmental disabilities: what public health and safety emergency planners need to know. J Emerg Manag 2015; 13(1):7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hamann CJ, Mello E, Wu H, Yang J, Waldron D, Ramirez M. Disaster preparedness in rural families of children with special healthcare needs. Disaster Med Public Health Prep 2016;10(2):225–232. [DOI] [PubMed] [Google Scholar]
- 19.Lou J, Braun M, De J, Fox A, Rokusek CF, Howell JT. Emergency preparedness for children with autism: a needs assessment for a vulnerable population [PowerPoint slides] Washington, DC: American Public Health Association; November 2007. [Google Scholar]
- 20.Barnes JM. School disaster needs for students with disabilities: voices from the field Los Angeles: University of California, Los Angeles; 2013. [Google Scholar]
- 21.Cancro BL. Schools with special needs students connect with parents in a crisis. Exceptional Parent 2009;39(8):49–50. [Google Scholar]
- 22.American Academy of Pediatrics, Committee on Pediatric Emergency Medicine, Council on Clinical Information Technology, American College of Emergency Physicians, Pediatric Emergency Medicine Committee. Emergency information forms and emergency preparedness for children with special healthcare needs. Pediatrics 2010;125(4):829–837. [DOI] [PubMed] [Google Scholar]
- 23.Markenson D, Reynolds S. The pediatrician and disaster preparedness. Pediatrics 2006;117(2):e340–e362. [DOI] [PubMed] [Google Scholar]
- 24.Committee on Pediatric Emergency Medicine. The role of the pediatrician in rural emergency medical services for children. Pediatrics 2012;130(5):978–982. [DOI] [PubMed] [Google Scholar]
- 25.Murray JS. Disaster preparedness for children with special healthcare needs and disabilities. J Spec Pediatr Nurs 2011; 16(3):226–232. [DOI] [PubMed] [Google Scholar]
- 26.National Association of School Psychologists. Coping with terrorism—helping children with special needs: tips for school personnel and parents. Commun Disord Q 2002; 23(2):100–102. [Google Scholar]
- 27.Asher A Planning emergency evacuations for students with unique needs: role of occupational therapy. OT Pract 2009; 14(21):1–8. [Google Scholar]
- 28.Ronoh S, Ronoh S. Disability through an inclusive lens: disaster risk reduction in schools. Disaster Prev Manag 2017; 26(1):105–119. [Google Scholar]
- 29.Edmonds CO. Designing emergency preparedness resources for children with autism. Intl J Disabil Dev Educ 2017;64(4): 404–419. [Google Scholar]
- 30.Peacock G, Moore C, Uyeki T. Children with special healthcare needs and preparedness: experiences from seasonal influenza and the 2009 H1N1 influenza pandemic. Disaster Med Public Health Prep 2012;6(2):91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ronoh S, Gaillard JC, Marlowe J. Children with disabilities and disaster preparedness: a case study of Christchurch. Kōtuitui: New Zealand Journal of Social Sciences Online 2015;10(2):91–102. [Google Scholar]
- 32.Meredith LS, Shugarman LR, Chandra A, et al. Analysis of Risk Communication Strategies and Approaches with At-Risk Populations to Enhance Emergency Preparedness, Response, and Recovery. Final Report Santa Monica, CA: RAND Corp.; 2009. https://www.rand.org/pubs/working_papers/WR598.html. Accessed April 27, 2018. [Google Scholar]
- 33.Claessens L, Forsberg O. Communicating with Disaster-Affected Children: A Case Study from the 2015 Nepal Earthquake Response Stockholm: Plan International Sweden; 2016. [Google Scholar]
- 34.UNICEF. Guidance: Including children with disabilities in humanitarian action 2017. http://training.unicef.org/disability/emergencies/index.html. Accessed April 27, 2018.
- 35.Hill-Patterson T In case of emergency: eight ways to make sure your child knows what to do. Volta Voices 2010;17(1): 36–37. [Google Scholar]
- 36.Friehe MJ, Swain KD. Helping students with disabilities deal with acts of terrorism. Commun Disord Q 2002;23(2):87–90. [Google Scholar]
- 37.Stallwood LG. Assessing emergency preparedness of families caring for young children with diabetes and other chronic illnesses. J Spec Pediatr Nurs 2006;11(4):227–233. [DOI] [PubMed] [Google Scholar]
- 38.Baker MD, Baker LR, Flagg LA. Preparing families of children with special healthcare needs for disasters: an education intervention. Soc Work Health Care 2012;51(5):417–429. [DOI] [PubMed] [Google Scholar]
- 39.Fifolt M, Wakelee J, Eldridge-Auffant L, Carpenter R, Hites L. Addressing the needs of adults and children with disabilities through emergency preparedness and organizational improvisation. Nonprofit Manag Leadersh 2017;27(3):423–434. [Google Scholar]
- 40.Cené CW, Johnson BH, Wells N, Baker B, Davis R, Turchi R. A narrative review of patient and family engagement: the “foundation” of the medical “home.” Med Care 2016;54(7): 697–705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Council on Children with Disabilities and Medical Home Implementation Project Advisory Committee. Patient-and family-centered care coordination: a framework for integrating care for children and youth across multiple systems. Pediatrics 2014;133(5):1451–1460. [DOI] [PubMed] [Google Scholar]
- 42.McAllister J Achieving a Shared Plan of Care with Children and Youth with Special Healthcare Needs Palo Alto, CA: Lucile Packard Foundation for Children’s Health; May 2014. [Google Scholar]
- 43.Boon H, Brown L, Pagliano P. Emergency planning for students with disabilities: a survey of Australian schools. Australian J Emerg Manag 2014;29:45–49. [Google Scholar]
- 44.Chang MT, Bradin S, Hashikawa AN. Disaster preparedness among Michigan’s licensed child care programs. Pediatr Emerg Care 2016. Aug 1. [DOI] [PubMed]
- 45.Graham J, Shirm S, Liggin R, Aitken ME, Dick R. Mass-casualty events at schools: a national preparedness survey. Pediatrics 2006;117(1):e8–e15. [DOI] [PubMed] [Google Scholar]
- 46.Alsem MW, Ausems F, Verhoef M, Jongmans MJ, Meily-Visser JM, Ketelaar M. Information seeking by parents of children with physical disabilities: an exploratory qualitative study. Res Dev Disabil 2017;60:125–134. [DOI] [PubMed] [Google Scholar]
- 47.Khoo K, Bolt P, Babl FE, Jury S, Goldman RD. Health information seeking by parents in the internet age. J Paediatr Child Health 2008;44(7–8):419–423. [DOI] [PubMed] [Google Scholar]
- 48.Singer GH, Marquis J, Powers LK, et al. A multi-site evaluation of parent to parent programs for parents of children with disabilities. J Early Interv 1999;22(3):217–229. [Google Scholar]
- 49.Ammari T, Morris MR, Schoenebeck SY. Accessing social support and overcoming judgment on social media among parents of children with special needs Proceedings of the 8th International AAAI Conference on Weblogs and Social Media; June 1, 2014. https://www.aaai.org/ocs/index.php/ICWSM/ICWSM14/paper/viewFile/8032/8102. Accessed April 30, 2018. [Google Scholar]
- 50.Knapp C, Madden V, Marcu M, et al. Information seeking behaviors of parents whose children have life-threatening illnesses. Pediatr Blood Cancer 2011;56(5):805–811. [DOI] [PubMed] [Google Scholar]


