Abstract
Background
Musculoskeletal conditions are a leading contributor to disability worldwide. The treatment of these conditions accounts for 7% of health care costs in Germany and is often provided by physiotherapists. Yet, an overview of the cost-effectiveness of treatments for musculoskeletal conditions offered by physiotherapists is missing. This review aims to provide an overview of full economic evaluations of interventions for musculoskeletal conditions offered by physiotherapists.
Methods
We systematically searched for publications in Medline, EconLit, and NHS-EED. Title and abstracts, followed by full texts were screened independently by two authors. We included trial-based full economic evaluations of physiotherapeutic interventions for patients with musculoskeletal conditions and allowed any control group. We extracted participants' information, the setting, the intervention, and details on the economic analyses. We evaluated the quality of the included articles with the Consensus on Health Economic Criteria checklist.
Results
We identified 5141 eligible publications and included 83 articles. The articles were based on 78 clinical trials. They addressed conditions of the spine (n = 39), the upper limb (n = 8), the lower limb (n = 30), and some other conditions (n = 6). The most investigated conditions were low back pain (n = 25) and knee and hip osteoarthritis (n = 16). The articles involved 69 comparisons between physiotherapeutic interventions (in which we defined primary interventions) and 81 comparisons in which only one intervention was offered by a physiotherapist. Physiotherapeutic interventions compared to those provided by other health professionals were cheaper and more effective in 43% (18/42) of the comparisons. Ten percent (4/42) of the interventions were dominated. The overall quality of the articles was high. However, the description of delivered interventions varied widely and often lacked details. This limited fair treatment comparisons.
Conclusions
High-quality evidence was found for physiotherapeutic interventions to be cost-effective, but the result depends on the patient group, intervention, and control arm. Treatments of knee and back conditions were primarily investigated, highlighting a need for physiotherapeutic cost-effectiveness analyses of less often investigated joints and conditions. The documentation of provided interventions needs improvement to enable clinicians and stakeholders to fairly compare interventions and ultimately adopt cost-effective treatments.
Supplementary Information
The online version contains supplementary material available at 10.1186/s40798-024-00713-9.
Keywords: Economic evaluation, Physiotherapy, Musculoskeletal condition, Orthopedic
Key Points
Several high-quality economic evaluations of physiotherapeutic treatments for the back and knee exist
Economic evaluations of other joints are rare
Physiotherapeutic interventions are often cost-effective over treatments provided by other health professionals
The description of provided interventions in cost-effectiveness analyses needs improvement, to allow fair treatment comparisons
Supplementary Information
The online version contains supplementary material available at 10.1186/s40798-024-00713-9.
Background
Rationale
Globally about 1.71 billion people suffer from a musculoskeletal condition [1]. Most adults in rehabilitation within Germany present with this diagnosis [2]. These patients have an increased risk of developing additional chronic diseases and mental health problems, which further increase the patients’ burden [3, 4]. Rehabilitation programs, aiming at reducing these patients' burden and their duration of sick leave, are often planned, and implemented by physiotherapists. Their and other therapeutic services account for 7% of the health expenditures in Germany (2021) and thus cause a financial burden for society [5].
Physiotherapeutic treatments have been used before clinical studies were conducted, but in the last decades, several interventions for specific diseases have been evaluated regarding their clinical effectiveness—although some intervention-disease-combinations remain yet unexplored. In recent years, besides their clinical effectiveness, the costs involved with a treatment have become additionally important to the stakeholders. The combined information supports their decision on whether a treatment should be implemented or de-implemented [6]. Full economic evaluations furnish this information on the anticipated costs along with the expected clinical outcomes of an intervention, enabling comparisons between various disease interventions and by this providing insight into possible cost savings. The costs presented in such analyses consider either healthcare costs alone or both healthcare costs and societal costs [6].
Several studies have already demonstrated that physiotherapists offer treatments worth the money [7, 8]. One review provides an overview of economic evaluations for treatments of neurological conditions offered by physiotherapists [9] and another review evaluates the cost-effectiveness of physical exercise, which is one of the treatment modalities offered by physiotherapists, for various health conditions [10]. However, an overview of existing economic evaluations of different physiotherapeutic treatment modalities for patients with musculoskeletal conditions is missing. Such an overview allows physiotherapists to easily identify relevant publications. Furthermore, it enables policymakers to easily identify relevant studies and researchers to plan future investigations.
Objectives
In this review, we therefore aim to:
provide an overview of existing full economic evaluations of interventions for patients with musculoskeletal conditions offered by physiotherapists.
shed light on the cost-effectiveness of physiotherapeutic interventions for specific musculoskeletal health conditions.
highlight for which health conditions further research is needed.
Methods
Protocol and Registration
A protocol for this review was published and additionally registered at Prospero (CRD42021276050) [11]. We followed our protocol but decided to report the findings of the identified trial and model-based economic evaluations separately. This allows us to fully account for and address the heterogeneous aspects of the two study types. Here we present our findings from the trial-based publications. We report our results following the PRISMA statement.
Eligibility Criteria
We included full economic evaluations of physiotherapeutic interventions for patients with musculoskeletal conditions. To specify our inclusion and exclusion criteria, we used the PICOS acronym (population, intervention, control group, outcome, study type).
Our population of interest suffered from a musculoskeletal condition. If the majority had another primary disease or if the participants had intellectual disabilities, we excluded the publication.
We included publications where physiotherapists provided one of the intervention/control group treatments alone. We excluded publications if the treatment of interest was offered by an interdisciplinary team, non-healthcare professionals, or mostly by a different profession. If the physiotherapeutic treatment of interest was combined with another treatment, this needed to be provided in a comparator group as well. Thus, an isolated incremental effect evaluation of a physiotherapeutic intervention needed to be possible. Economic evaluations of E-intervention were excluded.
We allowed any type of control group including wait-and-see, usual care, placebo, and alternative treatments, and excluded publications where no control group was considered.
Our outcome needed to be the result of a full health economic evaluation, including cost-effectiveness ratios, and cost-utility ratios.
Economic evaluations based on models and clinical trials were included during the screening process. We excluded Delete 'study types like' conference abstracts, reviews, books, and articles with no access and studies without results, e.g. protocols. In this publication, we additionally excluded model-based studies during the full-text screening, to reduce heterogeneity of included studies and allow a fair comparison of the study quality.
Finally, the economic evaluation needed to be published in Danish, English, or German.
Information Sources
We searched for relevant publications in the databases Medline (through PubMed), EconLit, and NHS-EED (can only be searched up to March 2015). The initial search was performed at the end of January 2022 and the final update was performed on the 8th of December 2023.
Search Strategy
We used the three main search terms ‘economic evaluation’, ‘physiotherapy’, and ‘orthopedic’ to develop a search matrix. For each of the main search terms we collected synonyms and combined them with an ‘OR’ in a search. Afterwards, we merged the three synonym searches with two ‘AND’. Utilizing asterisks reduced the number of search terms but allowed identifying relevant articles. Our search string in PubMed consequently was: ((((economic analy*) OR (cost analy*) OR (cost benefit*) OR (cost utility) OR (cost effectiveness) OR (economic evaluation))) AND (((orthopaedic rehabilitation) OR (physical rehabilitation) OR (exercise therap*) OR (conservative therap*) OR (conservative management) OR (conservative treatment) OR (exercise training) OR (physiotherap*))) AND (((muskuloskeletal) OR (chirur*) OR (orthop*) OR (osteoarthritis) OR (back pain)))). "Details on the PubMed search" are also available in Additional file 1: Table S1.
Selection Process
After removing duplicates, we applied a two-step study selection process. In the first step, we screened the title and abstracts for our inclusion and exclusion criteria. In the second step, we evaluated the full texts. Both steps were conducted by two independent reviewers at any time (LB, WF, BK). After each step, the involved authors compared their results and resolved disagreements via discussions or consulting a third reviewer (HHK) if needed.
Data Collection Process
The spreadsheet for data extraction was independently tested on three included publications by two authors (LB, BK). The authors discussed uncertainties, adjusted the labeling in the spreadsheet, and repeated the process. The authors agreed in the second round and LB proceeded with the data extraction. WF became involved in the data extraction process after she compared the data extraction results of three publications with LB, and no disagreement occurred.
Data Items
In total, we extracted the following items per publication: authors, year of publication, sample size, mean age, the proportion of female sex, health condition, location, type of economic analysis, cost perspective, economic effect measure, time horizon, study design, setting, and frequency, intensity, duration as well as the type of intervention, further control intervention, cost-effectiveness results, and finally the author’s conclusion. If the modalities of an intervention were not presented in a publication, but a reference was mentioned, we extracted the information from the cited publication. Further, in articles with several physiotherapeutic intervention or control groups, we ordered the interventions of interest as primary, secondary and so on. We prioritized basic interventions as primary, meaning interventions which could be most easily provided by physiotherapists—without further training.
Critical Appraisal of the Included Publications
We utilized the Consensus on Health Economic Criteria checklist for evaluating the quality of the included articles [12]. This tool consists of 19 questions which can be answered with ‘yes’ or ‘no’ each. Each ‘yes’ indicates good quality, whereas a ‘no’ indicates limited quality.
Two authors (LB and HHK) independently assessed the quality of three articles. After discussing uncertainties LB proceeded with the evaluation. WF got involved in the assessment after she and LB agreed on the quality of three, independently evaluated, articles.
Synthesis of Results
We provide a descriptive overview of the available literature. We categorized the economic evaluations based on the affected body parts. Afterwards, we grouped all cost-effectiveness comparisons, which are partly between two physiotherapeutic interventions, and partly between a physiotherapeutic and another intervention, of the included articles according to the four quadrants of a cost-effectiveness plane (I. more costly, more effective; II. more costly, less effective (dominated); III. less costly, less effective; IV. less costly, more effective (dominant)). The IV. quadrant is always assumed to be cost-effective, and the II. quadrant is always dominated, hence not cost-effective in the performed comparison. However, whether the interventions are cost-effective in the other two quadrants (I. and III.), depends on the stakeholder’s willingness to pay for an extra benefit in a health outcome. As an example, if a health system is not willing to pay the additional costs for the gain in health outcomes in the comparison group, our (primary) interventions in the III. quadrant would be cost-effective. However, if the healthcare system is willing to pay the additional costs to achieve the additional benefit in the health outcome, our (primary) interventions grouped in the I. quadrant would be cost-effective. Thus, to determine if interventions of the I. and III. quadrants are cost-effective, we would need to know the amount of money the healthcare system or society is willing to pay for a one-unit gain in the respected health outcome. However, this is beyond the scope of this review. For comparisons between two physiotherapeutic interventions, we defined one intervention as the primary intervention of interest. These primary physiotherapeutic interventions were more likely offered solely by physiotherapists and required least additional training/courses for the physiotherapists.
Results
Selection of Publications
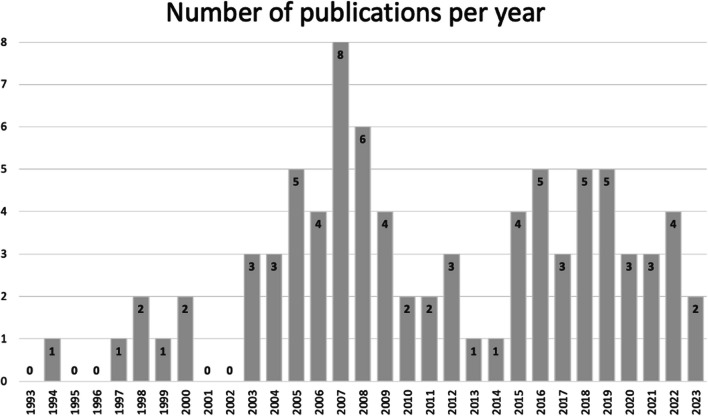
Our search findings and the study selection process are visualized in the flowchart Fig. 1. In total, we identified 5141 eligible publications of which 83 met our inclusion criteria. A list of the publications excluded during the full-text screening process including an indication of the reason for exclusion is provided in Additional file 2: Table S2.
Fig. 1.
Flow chart of the study selection process
Characteristics of the Economic Evaluations
Table 1 summarizes our included 83 articles which were based on 78 clinical trials [13–95]. Niemistö et al., Barker et al., Skargren et al. as well as Hurley et al. published two articles each building on one trial [17, 18, 51, 52, 72, 81, 82, 96]. Abbott et al. and Pinto et al. utilized data from the MOA RCT [13, 74]. All articles were published between 1994 and 2023 (Fig. 2). The majority of the 78 clinical trials were RCTs (n = 71) and 71 of the articles originated from the Western world. The UK (n = 23) and the Netherlands (n = 22) contributed more than 50% of the articles (Fig. 3). The time horizon of the economic evaluations varied between 5 days and 36 months. In Table 1 the included articles are grouped by their addressed body parts: spine (n = 39), upper limb (n = 8), lower limb (n = 30), and other conditions (n = 6). The most frequently investigated conditions were low back pain (n = 25) and hip and knee osteoarthritis (n = 16). In most included samples the mean age was between 45 and 65 and the distribution of female and male participants was between 40 to 60%. If a sample deviated from this, the mean age and female percentage were added in Table 1.
Table 1.
Overview of the included trial-based economic evaluations
| Study ID | Patients' characteristics | Country | Study design, type of economic analysis | Cost perspective | Effect measure | Time horizon |
|---|---|---|---|---|---|---|
| Spine | ||||||
| Back | ||||||
|
A Barker et al. 2019 [17] B Barker et al. 2020 [18] |
n = 615 Mean age: 72 Female: 86% Osteoporotic vertebral fracture |
UK |
RCT (PROVE-trial) Cost-utility |
Healthcare perspective, Societal perspective |
QALY (EQ-5D) | 12 months |
| Müller et al. 2019 [71] |
n = 2324 patients Back pain |
DE |
Prospective cohort study Cost-effectiveness |
Healthcare perspective, sick leave | Pain intensity (Graded chronic back pain status) | 24 months |
| Søgaard et al. 2008 [84] |
n = 90 lumbar spinal fusion |
DK~ |
RCT Cost-effectiveness |
Societal perspective | Pain- and disability index scales of the low back pain rating scale | 24 months |
| Low back pain | ||||||
| Aboagye et al. 2015 [14] |
n = 159 female: (i1) 72% (i2) 62% (c) 80% LBP |
SE |
RCT Cost-effectiveness |
Societal perspective | QALY (EQ -5D) | 12 months |
| Ankjær-Jensen et al. 1994 [15] |
n = 172 Mean age: 44 LBP (herniated disc) |
DK |
Retrospective cohort study Cost-effectiveness |
Societal perspective | Low back pain rating scale |
(i) 12 months c) 22 months |
| Apeldoorn et al. 2012 [16] |
n = 156 Mean age: (i) 43 (c) 42 LBP (chronic) |
NL |
RCT cost-effectiveness |
Societal perspective | QALY (EQ-5D) | 12 months |
| Bello et al. 2015 [21] |
n = 62 Mean age: (i) 43 (c) 45 LBP (chronic) |
GH |
Feasibility intervention NA |
Healthcare perspective | SF-36, numeric rating scale | 3 months |
| Burton et al. 2004 [26] |
n = 1287 LBP (non-specific) |
UK |
RCT Cost-utility, cost-effectiveness |
Healthcare perspective | QALY (EQ -5D) | 12 months |
| Canaway et al. 2018 [27] |
n = 220 Mean age: 42 LBP |
IL |
Prospective cohort study Cost-effectiveness |
Healthcare perspective | QALY (SF-12) | 12 months |
| Carr et al. 2005 [28] |
n = 237 Mean age: (i) 42 (c) 43 LBP |
UK |
RCT Cost-effectiveness |
Healthcare perspective | RMDQ | 12 months |
| Cherkin et al. 1998 [29] |
n = 321, Mean age: 41 LBP (chronic) [12+ weeks] |
US |
RCT Cost-effectiveness |
Healthcare perspective | Bothersomeness of symptoms, RDS |
Short-term: 3 months Long-term: 12–24 months |
| Critchley et al. 2007 [32] |
n = 150 Mean age: 44 Female: (i1) 71% (i2) 62% (c) 69% LBP (acute) [symptoms < 90 days] |
UK |
RCT Cost-effectiveness |
Healthcare perspective | QALY (EQ-5D) | 18 months |
| Fritz et al. 2008 [38] |
n = 471 Mean age: 41 LBP (acute) [without clinical signs of nerve root, symptoms < 16 days] |
US |
Case–control Cost-effectiveness |
Healthcare perspective | OSW, pain rating | 24 months |
| Fritz et al. 2017 [39] |
n = 220 Mean age: (i) 38 (c) 37 LBP [symptoms for 6 weeks to 6 months] |
US |
RCT Cost-effectiveness |
Societal perspective | QALY (EQ-5D) | 12 months |
| Hahne et al. 2017 [43] |
n = 300 Mean age: (i) 43 (c) 46 LBP (chronic) [symptoms 6+ weeks] |
AU |
RCT Cost-utility |
Healthcare perspective | QALY (EQ-5D) | 12 months |
| Herman et al. 2008 [45] |
n = 75 LBP [symptoms for 4+ weeks] |
US |
RCT Cost-effectiveness |
Main: societal perspective; additional: employer, participant | QALY (SF-6D) | 6 months |
| Hlobil et al. 2007 [46] |
n = 134 [sick-listed worker] mean age: (i) 39 (c) 37 LBP (chronic) |
NL |
RCT Cost–benefit |
Societal perspective | Lost productivity days | 36 months |
| Hurley et al. 2015 [50] |
n = 246 LBP [symptoms 3+ months] |
IE |
RCT Cost-utility |
Healthcare perspective | QALY (EQ-5D) | 12 months |
| Johnson et al. 2007 [55] |
n = 234 LBP |
UK |
RCT Cost-utility |
Healthcare perspective | QALY (EQ-5D) | 12 months |
| Karjalainen et al. 2003 [57] |
n = 164 mean age: (i1) 44 (i2) 44 (c) 43 [25–61 y.] LBP |
FI |
RCT Cost–benefit |
Healthcare perspective | Bothersomeness and frequency of pain, daily symptoms, generic health-related quality of life, intensity of pain, ODI, sick leave, | 12 months |
| Kim et al. 2020 [59] |
n = 56 [BMI 17–30] Mean age: (i) 48 (c) 39 Female: (i) 25% (c) 29% LBP (chronic) |
KR |
RCT Cost-effectiveness |
Healthcare perspective | Functional rating index, Multidimensional Personality Questionnaire, VAS | 3 weeks |
|
A Niemistö et al. 2003 [72] B Niemistö et al. 2005 [73] |
n = 204 Mean age: (i) 37 (c) 37 [24–46] LBP (subacute and chronic) [symptoms 6+ weeks] |
FI |
RCT Cost-effectiveness |
Societal perspective |
A VAS B ODI, VAS |
A 12 months B 24 months |
| Rivero-Arias et al. 2006 [77] |
n = 286 mean age: (i) 42 (c) 40 LBP (chronic) [symptoms 3+ months] |
UK |
RCT Cost-utility |
Healthcare perspective, societal perspective | QALY (EQ-5D) | 12 months |
| Smeets et al. 2009 [83] |
n = 160 Mean age: (i1) 43 (i2) 42 (c) 43 LBP |
NL |
RCT Cost-effectiveness, cost-utility |
Societal perspective | RMDQ, QALY (EQ-5D) | 12 months |
| Suni et al. 2018 [87] |
n = 219 [health professionals] Female: 100% LBP (chronic) |
FI |
RCT Cost-effectiveness |
Healthcare perspective, sick leave | QALY (SF-6D) | 12 months |
| van der Roer et al. 2008 [93] |
n = 114 [have a health insurance with company AGIS] LBP [symptoms < 12 weeks] |
NL |
RCT Cost-effectiveness |
Societal perspective | General perceived effect (6-point-scale), pain-rating-scale, EQ-5D, RMDQ | 12 months |
| Whitehurst et al. 2007 [95] |
n = 299 LBP (chronic) |
UK |
RCT cost-effectiveness, cost-utility |
Healthcare perspective | RMDQ, QALY (EQ-5D) | 12 months |
| Neck | ||||||
| Bosmans et al. 2011 [24] |
n = 146 Neck pain (subacute) |
NL |
RCT Cost-effectiveness, cost-utility |
Societal perspective | Patient perceived recovery, QALY (SF-6D) | 12 months |
| Korthals-de Bos et al. 2003 [62] |
n = 183 Neck pain |
NL~ |
RCT Cost-effectiveness, cost-utility |
Societal perspective | EQ, functional disability, pain intensity, patient perceived recovery | 12 months |
| Leininger et al. 2016 [63] |
n = 241 Mean age: 73 Neck pain (chronic) [symptoms 3+ months] |
US |
RCT Cost-effectiveness |
Societal perspective | QALY (SF-6D) | 12 months |
| Lewis et al. 2007 [64] |
n = 350 Female: 63% (in total) Neck disorders (non-specific) |
UK |
RCT Cost-effectiveness, cost-utility |
Healthcare perspective, societal perspective | Northwick Park Questionnaire, QALY (EQ-5D) | 6 months |
| Manca et al. 2006 [68] |
n = 268 Female: (i) 62% (c) 66% Neck pain [musculoskeletal origin, symptoms 2+ weeks] |
UK |
RCT Cost-effectiveness |
Healthcare perspective | QALY (EQ-5D) |
3 months, 12 months |
| Van Dongen et al. 2016 [94] |
n = 181 Female: (i) 62% (c) 62% neck pain (subacute and chronic) |
NL |
RCT cost-effectiveness, cost-utility |
Societal perspective | Neck Disability Index—Dutch Version, patient's perceived recovery | 12 months |
| Others/mixed | ||||||
| Denninger et al. 2018 [34] |
n = 447 Female: 72% Back pain or neck pain |
US |
Retrospective cohort Cost-effectiveness |
Healthcare perspective | EQ-5D, NPRS, Oswestry Disability Index/Neck Disability Index, Patient Health Questionnaire-4 | 24 months |
| Manca et al. 2007 [67] |
n = 315 Back pain or neck pain [non-systematic origin, symptoms 2+ weeks] |
UK |
RCT Cost-effectiveness |
Healthcare perspective | QALY (EQ-5D) | 12 months |
|
A Skargren et al. 1997 [82] B Skargren et al. 1998 [81] |
n = 323 Mean age: (i) 41 c) 41 back or neck pain |
SE |
RCT Cost–benefit |
Healthcare perspective | General Health (scale), ODS, VAS |
A 6 months B 12 months |
| Upper limb | ||||||
| Bergman et al. 2010 [23] |
n = 142 Shoulder complaints |
NL |
RCT Cost-effectiveness |
Societal perspective | Patient perceived recovery | 6 months |
| Commbes et al. 2016 [30] |
n = 154 Female: (i1) 36 (i2) 39 (c1) 38 (c2) 38 epicondylitis lateralis [> 6 weeks duration] |
AU |
RCT Cost-utility |
Societal perspective | QALY (EQ-5D) | 12 months |
| Fernandez-de-Las-penjas et al. 2019 [37] |
n = 120 Female: 100% Carpal tunnel syndrom |
ES |
RCT Cost-effectiveness |
Societal perspective | QALY (EQ-5D) | 12 months |
| Geraets et al. 2006 [41] |
n = 176 Shoulder complaints (chronic) |
NL |
RCT Cost–benefit |
Societal perspective | EQ-5D, main complaints, Shoulder Disability Questionnaire | 12 months |
| Hopewell et al. 2021 [48] |
n = 708 Rotator cuff disease |
UK |
RCT Cost-utility |
Healthcare perspective | QALY (EQ-5D) | 12 months |
| James et al. 2005 [53] |
n = 207 Shoulder pain [new episode] |
UK |
RCT Cost-consequences |
Healthcare perspective | Disability score, EQ-5D | 6 months |
| Korthals-de Bos et al. 2004 [61] |
n = 183 Epicondylitis lateralis |
NL |
RCT Cost-effectiveness, cost-utility |
Societal perspective |
Cost effectiveness: general improvement, pain during the day, PFFQ cost-utility: EQ |
12 months |
| Struijs et al. 2006 [86] |
n = 180 Epicondylitis lateralis [symptoms 6+ weeks] |
NL |
RCT Cost-effectiveness, cost-utility |
Societal perspective | EQ, pain-free function questionnaire, pain most serious complaint, severity of complaint, success rate | 12 months |
| Lower limb | ||||||
| Hip | ||||||
| Fusco et al. 2019 [40] |
n = 80 Female: 0% Hip replacement |
UK |
RCT Cost-effectiveness, cost-utility |
Healthcare perspective | QALY (EQ-5D) | 12 months |
| Griffin et al. 2022 [42] |
n = 358 Mean age: (i) 35 (c) 35 Female: (i) 42% (c) 36% femoroacetabular impingement syndrome |
UK |
RCT (UK FASHioN RCT) Cost-effectiveness |
Healthcare perspective, societal perspective | QALY (EQ-5D) | 12 months |
| Juhakoski et al. 2011 [56] |
n = 118 Mean age: (i) 67 (c) 66 Female: (i) 68% (c) 72% Hip osteoarthritis |
FI |
RCT Cost-effectiveness |
Healthcare perspective | SF-36, WOMAC | 24 months |
| Tan et al. 2016 [88] |
n = 203 Mean age: (i) 65 (c) 67 Female: (i) 62% (c) 55% Hip osteoarthritis |
NL |
RCT Cost-utility |
Healthcare perspective, societal perspective | QALY (EQ-5D) | 12 months |
| Knee | ||||||
| Barton et al. 2009 [20] |
n = 389 Female: 66% (in total) Knee pain [BMI > = 28; age = 45+] |
UK |
RCT Cost-effectiveness |
Healthcare perspective | QALY (EQ-5D) | 24 months |
| Bennell et al. 2016 [22] |
n = 222 [50+] Knee osteoarthritis |
AU |
RCT Cost-effectiveness |
Healthcare perspective | QALY (EQ-5D) | 12 months |
| Eggerding et al. 2021 [35] |
n = 167 Mean age: (i) 31 (c) 31 ACL tear [recent ACL tear, max. 2 month ago] |
NL+ |
RCT Cost-utility |
Healthcare perspective, Societal perspective |
QALY (EQ-5D) | 24 months |
| Ho-Henriksson et al. 2022 [47] |
n = 69 Female: (i) 60% (c) 68% Knee osteoarthritis |
SE |
RCT Cost-effectiveness |
Health care perspective, societal perspective | QALY (EQ-5D) | 12 months |
| Huang et al. 2012 [49] |
n = 243 Mean age: (i) 70 (c) 71 Female: (i) 70% (c) 74% Total knee replacement [unilateral TKA, due to OA] |
TW |
RCT Cost-effectiveness |
Healthcare perspective | Knee ROM, Length of stay, VAS | 5 days |
|
A Hurley et al. 2007 [52] B Hurley et al. 2012 [51] |
n = 418 Mean age: (i1) 66 (i2) 68 (c) 67 [50+] female: (i1) 25% (i2) 22% (c) 23% Knee pain (chronic) [symptoms 6+ months] |
UK |
A RCT (ESCAPE-Knee-Study) Cost-effectiveness, cost-utility B RCT (ESCAPE-Knee-Study) Cost-effectiveness |
Healthcare perspective, social care payer perspective |
A WOMAC, QALY (EQ-5D) B WOMAC |
A 6 months B 30 months |
| Jessep et al. 2009 [54] |
n = 64 Mean age: (i) 66 (c) 67 [> 50] Female: (i) 63% (c) 76% Knee pain (chronic) |
UK |
RCT Cost–benefit |
Healthcare perspective | QALY (EQ-5D) | 12 months |
| Kigozi et al. 2018 [58] |
n = 514 Knee osteoarthritis |
UK |
RCT (BEEP-trial) Cost-effectiveness, cost-utility |
Healthcare perspective | QALY (EQ-5D) | 18 months |
| Knoop et al. 2023 [60] |
n = 328 Mean age: (i) 66 (c) 64 [40–85] Female: (i) 63% (c) 64% Knee osteoarthritis |
NL |
RCT Cost-utility |
Societal perspective | QALY (EQ-5D) | 12 months |
| McCarthy et al. 2004 [69] |
n = 214 Knee osteoarthritis |
UK |
RCT (GRASP-RCT) cost-effectiveness |
Healthcare perspective | QALY (EQ-5D) | 12 months |
| Mitchell et al. 2005 [70] |
n = 114 Mean age: (i) 70 (c) 71 Total knee replacement |
UK |
RCT Cost-effectiveness |
Healthcare perspective | SF-36, WOMAC | 15 months |
| Pryymachenko et al. 2021 [75] |
n = 75 Female: (i1) 63% (i2) 67% (i3) 63% (c) 58% Knee osteoarthritis |
NZ |
RCT (MOA2-Trial) Cost-effectiveness |
Healthcare perspective, societal perspective | QALY (EQ-5D) | 24 months |
| Rhon et al. 2022 [76] |
n = 156 Female: (i) 37% (c) 38% Knee osteoarthritis |
US |
RCT Cost-effectiveness |
Healthcare perspective | QALY (EQ-5D) | 12 months |
| Sevick et al. 2000 (ex) [78] |
n = 439 Mean age: (i1) 69 (i2) 68 (c) 69 [60+] Female: (i1) 69% (i2) 73% (c) 69% Knee osteoarthritis |
US |
RCT Cost-effectiveness |
Healthcare perspective | Car task, lifting and carrying task, Self-reported disability score, stair climb, 6-min walking distance | 18 months |
| Sevick et al. 2009 [80] |
n = 316 Mean age: (i1) 68 (i2) 69 (i3) 69 (c) 69 Female: (i1) 72% (i2) 74% (i3) 74% (c) 68% Knee osteoarthritis |
US~ |
RCT (ADAPT-trial) Cost-effectiveness |
Payer perspective | Stair climb, weight, WOMAC function, WOMAC pain, WOMAC stiffness, 6-min walk | 18 months |
| Stan et al. 2015 [85] |
n = 90 Age mean: (i) 67 (c1) 64 (c2) 65 [60+] Female: 70% (in total) Knee osteoarthritis [varus deformity, Ahlback score 3, 4 or 5] |
RO |
Controlled trial Cost-effectiveness |
Payer perspective | QALY (EQ-5D) | Uncertain |
| Tan et al. 2010 [89] |
n = 131 Mean age: (i) 25 (c) 23 Female: (i) 65% (c) 64% Patellofemoral pain syndrome |
NL |
RCT Cost-utility |
Healthcare perspective, societal perspective | QALY (EQ-5D) | 12 months |
| van de Graaf et al. 2020 [90] |
n = 319 Meniscal tear [non-obstructive] |
NL |
RCT Cost-effectiveness |
Societal perspective | International Knee Documentation Committee, QALY (EQ-5D) | 24 months |
| van der Graaff et al. 2023 [92] |
n = 99 Mean age: (i) 36 (c) 34 [18–45] Female: (i) 26% (c) 23% meniscal tear (traumatic) |
NL |
RCT Cost-utility |
Healthcare perspective, societal perspective | QALY (EQ-5D) | 24 months |
| Others/mixed | ||||||
|
A Abbott et al. 2019 [13] B Pinto et al. 2013 [74] |
n = 206 Mean age: (i1) 67 (i2) 67 (i3) 66 (c) 66 Female: (i1) 32% (i2) 28% (i3) 29% (c) 25% Hip osteoarthritis, knee osteoarthritis |
NZ |
A RCT (MOA-RCT) Cost-effectiveness B RCT (MOA-RCT) Cost-effectiveness, cost-utility |
A Societal perspective B Healthcare perspective, societal perspective |
A QALY (SF-6D) B OMERACT-OARSI responder, QALY (SF-12v2), WOMAC |
A 24 months B 12 months |
| Bulthuis et al. 2008 [25] |
n = 85 Mean age: (i) 69 (c) 69 Female: (i) 42% (c) 28% Hip osteoarthritis, knee osteoarthritis |
NL |
RCT (DAPPER-study) Cost-utility, cost-effectiveness |
Societal perspective | Functional ability, MACTAR and EPMROM | 6 months |
| Coupé et al.‚ 2007 [31] |
n = 200 Female: (i) 75% (c) 79% Hip osteoarthritis, knee osteoarthritis |
NL |
RCT Cost-effectiveness |
Societal perspective | QALY (EQ-5D) | 15 months |
| Fernandes et al. 2017 [97] |
n = 165 Mean age: (i) 68 (c) 67 Total hip replacement, total knee replacement |
DK |
RCT Cost-utility |
Healthcare perspective | HOOS, KOOS, QALY (EQ-5D) | 12 months |
| Lin et al. 2008 [66] |
n = 94 Mean age: (i) 43 (c) 41 Female: (i) 26% (c) 17% Ankle fracture [treated with cast immobilization, with or without surgery before] |
AU |
RCT Cost-effectiveness |
Healthcare perspective, patient perspective | Assessment of Quality of Life, Lower Extremity Functional Scale | 5,5 months |
| Other conditions | ||||||
| Barnhoorn et al. 2018 [19] |
n = 56 Mean age: 44 [18–80] Complex regional pain syndrome type 1 |
NL |
RCT Cost-effectiveness |
Healthcare perspective, travel costs | QALY (EQ-5D) | 9 months |
| Daker-White et al. 1999 [33] |
n = 481 Musculoskeletal problems |
UK |
RCT Cost-effectiveness |
Healthcare perspective, patient perspective | Disease Repercussions Profile, Hospital Anxiety and Depression Scale, Pain—Visual Analogue Scale, SF-36 | 5–6 months |
| Heij et al. 2022 [44] |
n = 292 Female: (i) 60 (c) 62 Mean age: (i) 82 (c) 81 Mobility problems |
NL |
RCT Cost-consequences, cost-utility |
Healthcare perspective | QALY (EQ-5D) | 6 months |
| Lilje et al. 2014 [65] |
n = 78 Mean age: (i) 38 (c) 45 Mixed (on a waiting list for surgery regarding neck, shoulder/arm, back, pelvis/hip, knee or leg/foot condition)+ |
SE |
RCT Cost-consequences |
Healthcare perspective | QALY (SF-6D) | 12 months |
| Sevick et al. 2000 (life) [79] |
n = 235(+) Sedentary adults |
US |
RCT (Project ACTIVE) Cost-effectiveness |
Practicing clinician | Blood pressure, heart rate, peak VO 2 (mL/kg/min), Physical Activity Recall), total treadmill time, weight |
6 months, 24 months |
| Van den Hout et al. 2005 [91] |
n = 300 Female: 79% Rheumatoid arthritis |
NL |
RCT (RAPIT-study) Cost-utility |
Societal perspective | HAQ, MACTAR, QALY (EQ-5D, SF-6D, VAS) | 24 months |
+information found in an additional paper, ~assumption of the authors, […] inclusion criteria, —not applicable, NA not available, (i) intervention, (c) control intervention, A, B publications based on the same conducted study
AU Australia, DE Germany, DK Denmark, ES Spain, FI Finland, GH Ghana, IE Ireland, IL Israel, KR South-Korea, NL Netherlands, NZ New-Zealand, RO Romania, SE Sweden, TW Taiwan, UK United Kingdom, US United States of America, LBP low back pain, EPMROM Escola Paulista de Medicina Range of Motion scale, EQ EuroQol, HAQ Health assessment Questionnaire, HOOS Hip Disability and Osteoarthritis Outcome Score, KOOS The Knee Injury and Osteoarthritis Outcome Score, MACTAR McMaster Toronto Arthritis Patient Preference Questionnaire, NPRS Numeric Pain Rating Scale, ODI Oswestry Disability Index, OMERACT-OARSI Outcome Measures in Rheumatology-Osteoarthritis Research Society International, OSW Osteoporosis Screening in Older Women, PFFQ Pain Free Function Questionnaire, QALY Quality-Adjusted Life Years, RDS Roland Disability score, RDQ Roland‐Morris Disability Questionnaire, ROM Range of motion, SF Short Form questionnaire, VAS Visual Analogue Scale, WOMAC The Western Ontario and McMaster Universities Arthritis Index
Fig. 2.
Years of publication of the included publications
Fig. 3.
Overview of the origin of included publications
The outcomes of the included studies needed to involve a clinical outcome as well as the economic outcome costs. The latter was evaluated from a health-payer perspective in 50 cases and in 36 cases from a societal perspective (Table 1). As the numbers indicate, some studies presented costs for both perspectives. The most frequently utilized clinical outcomes were quality-adjusted life-years (QALYs), which were assessed via the EQ-5D (n = 39) and the SF6 or SF12 (n = 9). Disease-specific disability scores were assessed second most often (n = 9), e.g. via the Roland-Morris Disability Questionnaire. Finally, pain intensity was used in five publications. The remaining publications used individual outcome measures such as bothersomeness of symptoms, a stair climbing task, and blood pressure (Table 1).
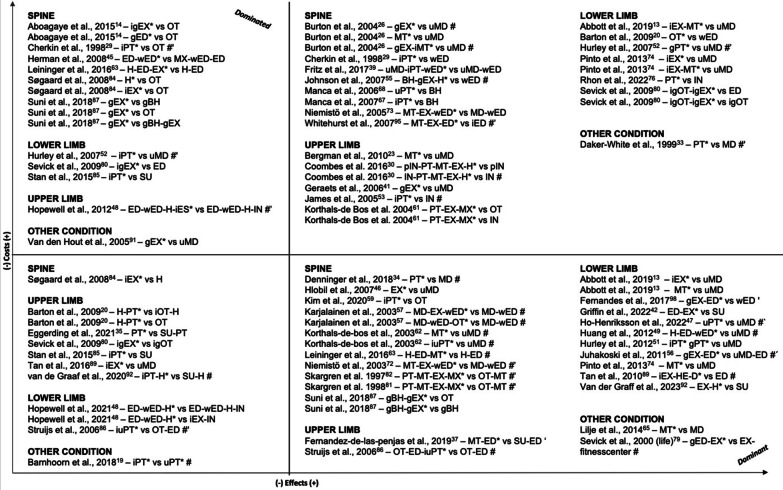
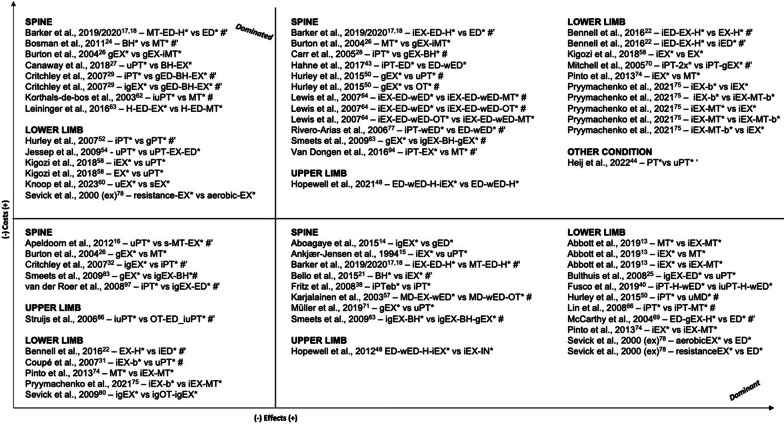
In Table 2, we present details on the interventions and highlight our defined primary intervention. The articles involved 150 comparisons between physiotherapeutic interventions and comparators. Figures 4 and 5 display the results in terms of differences in costs and effects grouped qualitatively according to the four quadrants of the cost-effectiveness plane. Eighty-one comparisons involved one treatment provided by a physiotherapist versus another non-physiotherapeutic intervention (Fig. 4), while 69 of the comparisons were between two physiotherapeutic treatments (Fig. 5).
Table 2.
Overview of interventions provided in the included trial-based economic evaluations
| Study ID | Condition, setting | Intervention(s) and comparator(s) | |||
|---|---|---|---|---|---|
| Frequency | Intensity | Time | Type | ||
| Spine | |||||
| Back | |||||
|
A Barker et al. 2019 [17] B Barker et al. 2020 [18] |
Osteoporotic vertebral fracture Outpatient, rehabilitation |
(i1) Up to 7 sessions over 12 weeks (i2) up to 7 sessions over 12 weeks, home exercises daily (c) 1 session |
(i1) yes (i2) yes (c) – |
(i1) 1 h assessment, following sessions 30 min (manual therapy), 15 min (stretches) (i2) 1 h assessment, following sessions 30 min (exercise therapy), 45 min/day on 3 to 5 days (home exercises) (c) 1 h |
(i1)* manual therapy, home stretching and education (i2)* individual exercise therapy, home exercises and education (c)* education by PT |
| Müller et al. 2019 [71] |
Back pain Outpatient, therapy |
(i) 36 sessions over 6 months (week 1–12: 2x/week, week 13–24: 1x/week) (c) NA |
(i) yes (c) NA |
(i) 1 h (c) NA |
(i)* group exercise therapy (c)* usual physiotherapeutic care |
| Søgaard et al. 2008 [84] |
Lumbar spinal fusion Outpatient, rehabilitation |
(i1) 3 sessions over 8 weeks (i2) 2x/week over 8 weeks (c) 1 session |
(i1) NA (i2) NA (c) – |
(i1) 1,5 h (i2) NA (c) NA |
(i1) group meetings for interpatient exchange of experiences for the promotion of cooping (i2)* individual exercise therapy (c)* oral instruction for home exercises |
| Low back pain | |||||
| Aboagye et al. 2015 [14] |
LBP Outpatient, therapy |
(i1) 2x/week over 6 weeks, afterwards alone at least 2x/week (i2) over 6 weeks, afterwards biweekly group, and alone at least 2x/week (c) NA |
(i1) NA (i2) NA (c) – |
(i1) NA (i2) NA (c) NA |
(i1) group yoga (i2)* individual + group exercise therapy (c)* evidence-based self-care advice group by back specialist # |
| Ankjær-Jensen et al. 1994 [15] |
LBP (herniated disc) Outpatient, rehabilitation |
(i) NA (c) NA |
(i) partly (c) NA |
(i) NA (c) NA |
(i)* group exercise therapy~ (c)* usual physiotherapeutic care~ |
| Apeldoorn et al. 2012 [16] |
LBP (chronic) Outpatient, therapy |
(i) over 4 weeks minimum, afterwards treatment could change (c) NA |
(i) NA (c) NA |
(i) NA (c) NA |
(i)* stratified treatment (adjusted Delitto´s classified treatment approach): either direction specific exercises, spinal manipulation or stabilization exercises (c)* usual physiotherapeutic care |
| Bello et al. 2015 [21] |
LBP (chronic) Outpatient, therapy |
(i) 2x/week over 12 weeks (c) 2x/week over 12 weeks |
(i) yes (c) yes |
(i) 45 min (c) 45 min |
(i)* behavioral graded activity (c)* individual conventional exercise therapy program |
| Burton et al. 2004 [26] |
LBP (non-specific) outpatient, therapy |
(i1) up to 9 sessions over 12 weeks (i2) 8 sessions over 12 weeks (i3) i1 and i2 over six weeks (c) – |
(i1) NA (i2) NA (c) – |
(i1) NA (i2) NA (i3) NA (c) NA |
(i1)* group exercise therapy (i2)* spinal manipulation (i3)* group exercise therapy and individual spinal manipulation (c) usual care in GP |
| Canaway et al. 2018 [27] |
LBP Outpatient, therapy |
(i) min. 2 sessions in total+ (c) NA |
(i) yes (c) NA |
(i) initial session of 40 min, following sessions 20–30 min+ (c) NA |
(i)* individual behavior changes and exercise therapy (c)* usual physiotherapeutic care |
| Carr et al. 2005 [28] |
LBP Outpatient, therapy |
(i) 8 sessions over 4 weeks (c) at the discretion of the physiotherapist |
(i) partly (c) NA |
(i) 1 h (c) NA |
(i)* group exercise therapy incl. cognitive behavioral approach (c)* individual physiotherapy |
| Cherkin et al. 1998 [29] |
LBP Outpatient, therapy |
(i1) up to 8 additional sessions (at the discretion of therapist) (i2) up to 8 additional sessions (at the discretion of therapist) (c) – |
(i) NA (c) – |
(i1) NA (i2) NA (c) – |
(i1) chiropractic (i2)* individual physical therapy (McKenzie) (c) education by booklet |
| Critchley et al. 2007 [32] |
LBP (acute) Outpatient, therapy |
(i1) up to 8 sessions (i2) up to 8 sessions (c) up to 12 sessions |
(i1) partly (i2) partly (c) partly |
(i1) 1,5 h (i2) 1,5 h (c) 30 min |
(i1)* individual and group spinal stabilization (i2)* group education: cognitive-behavioral approach and light exercises (c)* individual physiotherapy |
| Fritz et al. 2008 [38] |
LBP (acute) Outpatient, therapy |
(i) mean: 4.6 sessions over 25.4 days (c) mean: 5.9 sessions over 29.7 days |
(i) NA (c) NA |
(i) NA (c) NA |
(i)* individual physiotherapy following evidence-based guidelines (c)* physiotherapy not following evidence-based guidelines |
| Fritz et al. 2017 [39] |
LBP Outpatient, therapy |
(i) 4 sessions over 4 weeks (c) – |
(i) NA (c) – |
(i) NA (c) NA |
(i)* usual primary care, booklet and early individual physiotherapy (c) usual primary care, booklet and waiting min. 4 weeks before considering additional treatments # |
| Hahne et al. 2017 [43] |
LBP (chronic) Inpatient, therapy |
(i) 10 sessions over 10 weeks (c) 2 sessions over 10 weeks |
(i) partly (c) – |
(i) 30 min (c) 30 min |
(i)* individual physiotherapy (pathoanatomical, psychosocial, neurophysiological) and education by PT (c)* guideline-based education by PT and booklet |
| Herman et al. 2008 [45] |
LBP Outpatient, therapy |
(i) 2x/week over 3 months (c) bi-weekly over 3 months |
(i) NA (c) – |
(i) 30 min (c) 30 min |
(i) individual neuropathic care (acupuncture, exercise and dietary advice, relaxation), education by PT and booklet (c)* standardized education by PT and booklet |
| Hlobil et al. 2007 [46] |
LBP (chronic) Outpatient, therapy |
(i) 2x/week over 3 months or until patient can fully return to previous duties (c) – |
(i) partly (c) – |
(i) 1 h (c) – |
(i)* Graded Activity intervention (c) usual care in GP |
| Hurley et al. 2015 [50] |
LBP Outpatient, therapy |
(i1) weekly phone contact over 8 weeks (i2) 1 session 1x/week over 8 weeks c) NA |
(i1) yes (i2) partly (c) NA |
(i1) NA (i2) 1 h (c) NA |
(i1)* walking program (i2)* group exercise therapy (c)* usual physiotherapeutic care |
| Johnson et al. 2007 [55] |
LBP Outpatient, therapy |
(i) 8 sessions over 6 weeks (c) – |
(i) partly (c) – |
(i) 2 h (group sessions) (c) – |
(i)* cognitive behavorial therapy, group exercise therapy and home exercises (c) education by booklet |
| Karjalainen et al. 2003 [57] |
LBP outpatient/inpatient, therapy |
(i1) 1 session (i2) 1 session (c) – |
(i1) partly (i2) NA (c) NA |
(i1) 1,5 h (i2) 75 min (c) – |
(i1)* GP visit, light mobilization, graded activity exercises, leaflet (i2) GP visit, leaflet, visit of the patient’s work site by PT to review how the patient deals with the information given (c) GP visit, leaflet |
| Kim et al. 2020 [59] |
LBP (chronic) outpatient, therapy |
(i) 6 sessions over 3 weeks (c) 6 sessions over 3 weeks |
(i) NA (c) NA |
(i) 20 min (c) 20 min |
(i)* individual physical therapy: ultrasound, electrotherapy, hot pack (c) massage chair # |
|
A Niemistö et al. 2003 [72] B Niemistö et al. 2005 [73] |
LBP (chronic) Outpatient, therapy |
(i) 4 sessions over 4 weeks (c) reinforced at 5 month follow up |
A (i) yes (c) – B (i) partly (c) – |
(i) 1 h (c) – |
(i)* individual evaluation, manipulative treatment, exercises and booklet (c) physician consultation, education by booklet about low back pain, including exercise and coping advice |
| Rivero-Arias et al. 2006 [77] |
LBP (chronic) Outpatient, therapy |
(i) up to 5 sessions (c) 1 session |
(i) NA (c) – |
(i) initial session 1 h, following sessions 30 min (c) 1 h |
(i)* individual physiotherapy and education by booklet (c)* education by PT and booklet |
| Smeets et al. 2009 [83] |
LBP Outpatient, therapy |
all: 10 weeks intervention (i1) GA: 1-3x/week, 20 sessions (3 group, 17 individual) PST: 10 sessions (i2) PST: 10 sessions GA: start at 3 weeks, 19 sessions APT: 3x/week, 30 min bicycle and 75 min strength/endurance training (c) APT: 3x/week, 30 min bicycle and 75 min strength/endurance training |
(i1) partly (i2) i1 and c combined (c) yes |
(i1) GA: 30 min PST: 1,5 h (i2) APT: 1,75 h PST: 1,5 h GA: 30 min (c) 1,75 h |
(i1)* group and individual graded activity (GA) with problem solving (PST) (i2)* c and i1 combined (c)* group active physical treatment (APT) # |
| Suni et al. 2018 [87] |
LBP (chronic) Outpatient, therapy |
(i1) i2 and i3 combined (i2) in total: 32 sessions; 2x/week over 8 weeks, followed by 1x/week instructed session and 1x/week home session over 16 weeks (i3) 4 sessions 1x/week over 4 weeks, followed by 6 sessions every third week for 24 weeks |
(i1) yes (i2) yes (i3) yes (c) – + |
(i1) 1,75 h (i2) 1 h (i3) 45 min |
(i1)* i2 and i3 combined (i2)* group exercise therapy (i3) group counseling based on cognitive behavioral learning (c) wait and see |
| van der Roer et al. 2008 [93] |
LBP Outpatient, therapy |
(i) in total: 46 sessions over 30 weeks including 3 phases, 1. phase—10 individual sessions and 20 group sessions over 3 weeks 2. phase—group sessions 2x/week over 8 weeks 3. phase—decreased frequency of sessions, more home exercises (c) number of treatment sessions at discretion of the PTs, on average 9 sessions over 6 weeks + |
(i) yes (c) yes |
(i) individual sessions: 30 min, group sessions: 1,5 h (c) NA |
(i)* group and individual exercise therapy and education by back school according to behavioral principles (c)* individual physiotherapy according to the Low Back Pain Guidelines of the Royal Dutch College for Physiotherapy # |
| Whitehurst et al. 2007 [95] |
LBP Outpatient, therapy |
(i) 1 initial session + up to 6 sessions following (c) 1 initial session + up to 6 sessions following |
(i) partly (c) – |
(i) initial session 40 min, following sessions 20 min (c) initial session 40 min, following sessions 20 min |
(i)* manual therapy, individual back-specific exercises, advice (c)* individual brief pain management based on the biopsychosocial model of care # |
| Neck | |||||
| Bosmans et al. 2011 [24] |
Neck pain (subacute) Outpatient, therapy |
(i) up to 18 sessions (c) up to 6 sessions over 6 weeks |
(i) partly (c) NA |
(i) 30 min (c) 30–45 min |
(i)* Behavioral Graded Activity (c)* manual therapy |
| Korthals-de Bos et al. 2003 [62] |
Neck pain Outpatient, therapy |
(i1) up to 6 sessions 1x/week over 6 weeks (i2) up to 12 sessions 2x/week (c) – |
(i1) partly (i2) NA (c) – |
(i1) 45 min (i2) 30 min (c) – |
(i1)* manual therapy (i2)* individual physiotherapy (exercises, optional massage or partly manual therapy) (c) usual care in GP |
| Leininger et al. 2016 [63] |
Neck pain (chronic) Outpatient, therapy |
(i1) 4 sessions of education and up to 20 sessions of SMT over 12 weeks (i2) 4 sessions of education and 20 sessions of SRE over 12 weeks (c) 4 sessions over 12 weeks |
(i) yes (c) NA |
(i1) 1 h (i2) 1 h (c) 1 h |
(i1)* home exercises and advice (HEA) and spinal manipulative therapy (SMT) (i2)* HEA and individual supervised rehabilitative exercises (SRE) (c) home exercise and advice (HEA) # |
| Lewis et al. 2007 [64] |
Neck disorders (non-specific) Outpatient, therapy |
(i1) mean: 5.79 sessions followed by up to 6 sessions over 6 weeks (i2) mean: 6.63 sessions followed by up to 6 sessions over 6 weeks (c) mean: 4.49 sessions followed by up to 6 sessions over 6 weeks |
(i1) partly (i2) partly (c) partly + |
(i1) initial session 40 min, following sessions 20 min (i2) initial session 40 min, following sessions 20 min (c) initial session 40 min, following sessions 20 min |
(i1)* c and manual therapy (i2)* c and pulsed shortwave diathermy c)* individual exercise therapy, advice by PT and booklet (Arthritis Research Campaign's “Pain in the Neck” booklet) |
| Manca et al. 2006 [68] |
Neck pain Outpatient, therapy |
(i) 1–3 sessions (c) according to individual judgment of PT |
(i) – (c) NA |
(i) NA (c) NA |
(i) cognitive-behavioral treatment c)* usual physiotherapeutic care (electrotherapy, manual therapy, advice, acupuncture, other treatments) |
| Van Dongen et al. 2016 [94] |
Neck pain (subacute and chronic) Outpatient, therapy |
(i) up to 6 sessions 1x/week or bi-weekly, determined by PT (c) up to 9 sessions up to 2x/week |
(i) NA (c) NA |
(i) 30 min—1 h (c) 30 min |
(i)* Manual Therapy according to the Utrecht school c)* individual physiotherapy, with at least 20 min of active exercises # |
| Others/mixed | |||||
| Denninger et al. 2018 [34] |
Back or neck pain Outpatient, therapy |
(i) mean: 7 sessions (c) mean: 8 sessions |
(i) NA (c) NA |
(i) NA (c) NA |
(i)* individual initial contact by direct access to a PT (back and neck program) and following physical therapy (c) initial contact by traditional medical referral # |
| Manca et al. 2007 [67] |
Back or neck pain Outpatient, therapy |
(i) mean: 3,1 sessions (SD:2,5), range: 0 to 7+ (c) mean: 4,15 sessions (SD:2,8), range: 0 to 7+ |
(i) NA (c) NA |
(i) NA (c) NA |
(i) individual Solution Finding Approach c)* individual McKenzie therapy # |
|
A Skargren et al. 1997 [82] B Skargren et al. 1998 [81] |
Back or neck pain Outpatient, therapy |
(i) mean: 6 sessions (c) mean: 5 sessions |
(i) NA (c) NA |
(i) NA (c) NA |
(i)* physiotherapy (manipulation, mobilization, traction, soft tissue treatment, McKenzie treatment, TENS, acupuncture, relaxation training, training program) (c) chiropractic (manipulation, mobilization, traction, soft tissue treatment) |
| Upper Limb | |||||
| Bergman et al. 2010 [23] |
Shoulder complaints Outpatient, therapy |
(i) up to 6 sessions over 12 weeks (c) – |
(i) yes (c) – |
(i) NA (c) – |
(i)* manual therapy (manipulative and mobilization of the cervicothoracic spine and adjacent ribs) (c) usual care in GP |
| Commbes et al. 2016 [30] |
Epicondylitis lateralis [> 6 weeks duration] Outpatient, therapy |
(i1) 8 sessions over 8 weeks (physiotherapy) (i2) 8 sessions over 8 weeks (physiotherapy) (c1) 1 session (c2) 1 session |
(i1) yes (i2) yes (c1) yes (c2) yes |
(i1) 30 min (i2) 30 min (c1) – (c2) – |
(i1)* saline injection (placebo) followed by physiotherapy (manual therapy, exercise, home exercises) (i2) corticosteroid injection followed by physiotherapy (manual therapy, exercise, home exercises) c1) saline injection (placebo) # c2) corticosteroid injection # |
| Fernandez-de-Las-penjas et al. 2019 [37] |
Carpal tunnel syndrome Outpatient, therapy |
(i) 3 sessions 1x/week (c) – |
(i) yes (c) – |
(i) 30 min (c) – |
(i)* manual therapy and education for exercises (c) open or endoscopic surgery and education for exercises |
| Geraets et al. 2006 [41] |
Shoulder complaints (chronic) Outpatient, therapy |
(i) up to 18 sessions over 12 weeks (c) – |
(i) yes (c) – |
(i) 1 h (c) – |
(i)* group graded exercise therapy (c) usual care in GP |
| Hopewell et al. 2021 [48] |
Rotator cuff disorder Outpatient, therapy |
(i1) injection and c (i2) up to 6 sessions over 16 weeks (i3) injection and i2 (c) 1 session |
(i1) – (i2) partly (i2) partly (c) – |
(i1) 1 h (i2) initial session 1 h, following sessions 20–30 min (i3) injection and i2 (c) 1 h |
(i1) c and corticosteroid injection (i2)* c and individual exercise therapy (i3) individual exercise therapy and corticosteroid injection (c)* best-practice advice by PT, education by booklet and home exercises # |
| James et al. 2005 [53] |
Shoulder pain Outpatient, therapy |
(i) up to 8 sessions over 6 weeks (c) 1 injection at beginning, if symptoms persisted patients could have 1 additional injection within 4 weeks |
(i) NA (c) – |
(i) 20 min (c) – |
(i)* individual ( ~) physiotherapy (c) corticosteroid injection into subacromial space # |
| Korthals-de Bos et al. 2004 [61] |
Epicondylitis lateralis Outpatient, therapy |
(i) max. 9 sessions 2x/week over 6 weeks (c1) 1 session (c2) 1 session |
(i) partly (c1) yes (c) – |
(i) 30 min (c1) NA (c2) NA |
(i)* physiotherapy (ultrasound, deep friction massage, exercise) (c1) corticosteroid injections # (c2) wait-and-see # |
| Struijs et al. 2006 [86] |
Epicondylitis lateralis Outpatient, therapy |
(i1) 9 sessions over 6 weeks (i2) i1 and c (c) over 6 weeks |
(i1) yes (i2) yes (c) – |
(i1) 30 min (7,5 min ultrasound, 5–10 min friction) (i2) i1 and c combined (c) wearing the brace continuously during the day |
(i1)* individual physiotherapy (ultrasound, friction massage, home exercises, if pain subsided) (i2)* i1 and c (c) brace, 1 initial PT visit for instruction |
| Lower limb | |||||
| Hip | |||||
| Fusco et al. 2019 [40] |
Hip replacement Inpatient, rehabilitation |
(i), (c) 2x/day until hospital discharge, 8 weeks home exercises, 2 weeks after discharge 1 session at home or outpatient |
(i) NA (c) NA |
(i) NA (c) NA |
(i)* individual physiotherapy without 'hip precautions' and home exercises via booklet (c)* individual physiotherapy with 'hip precautions' and home exercises via booklet |
| Griffin et al. 2022 [42] |
Femoroacetabular Impingement syndrome Outpatient, therapy |
(i) – (c) 6–10 sessions over 12–24 weeks |
(i) – (c) yes |
(i) – (c) mean: 30 min |
(i) hip arthroscopy c)* best conservative care (personalized hip therapy: education and exercise therapy, sometimes per telephone or e-mail) |
| Juhakoski et al. 2011 [56] |
Hip osteoarthritis Outpatient, therapy |
(i) 1 session (education), 12 sessions 1x/week, after that 3x/week home exercise over 2 years, 4 booster sessions 1 year later (exercise) (c) 1 session (education) |
(i) yes (c) – |
(i) 1 h (education), 45 min (exercise) (c) 1 h (education) |
(i)* group exercise therapy and education by physician (c) usual care in GP and education by physician |
| Tan et al. 2016 [88] |
Hip osteoarthritis Outpatient, therapy |
(i) max. 12 sessions over the first 3 months, followed by 3 booster sessions at month 5, 6 and 9 (c) – |
(i) NA (c) – |
(i) NA (c) – |
(i)* individual ( ~) exercise therapy (c) usual care in GP |
| Knee | |||||
| Barton et al. 2009 [20] |
Knee pain Outpatient, therapy |
(i1) dietary intervention: 15 sessions over 24 months (monthly until 6th month, then every other month) home exercises: daily, 6 sessions with a PT every 4 months over 24 months (i2) 15 sessions over 24 (i3) daily, 6 sessions with a PT over 24 months (c) – |
(i1) home exercises: partly (i2) – (i3) partly (c) – |
(i1) NA (i2) NA (i3) NA (c) – |
(i1) individual dietary intervention and quadriceps strengthening home exercises (i2) individual dietary intervention (i3)* quadriceps strengthening home exercises with PT visits (c) education by leaflet |
| Bennell et al. 2016 [22] |
Knee osteoarthritis Outpatient, therapy |
(i) 10 sessions over 12 weeks, home program: 4x/week over 12 weeks, followed by 3x/week over 9 months (c1) exercise therapy: 10 sessions home program: 4x/week over 12 weeks, followed by 3x/week over 9 months (c2) 10 sessions 1x/week |
(i) partly (c1) partly (c2) – |
(i) 70 min (c1) 25 min (exercise therapy) (c2) 45 min |
(i)* individual education (pain coping) and exercise therapy and home program (c1)* exercise therapy and home program only (c2)* individual education (pain coping) by PT # |
| Eggerding et al. 2021 [35] |
ACL tear Outpatient, rehabilitation |
(i) until good functional control was achieved + (c) according to the recommendations of the Dutch ACL guideline, min. 3 months |
(i) NA (c) NA |
(i) NA (c) NA |
(i) early ACL reconstruction, within six weeks after randomization, after that referred for individual physical therapy + (c)* supervised individual physical therapy program, then optional reconstruction+# |
| Ho-Henriksson et al. 2022 [47] |
Knee osteoarthritis Outpatient, therapy |
(i) mean: 4 individual and two group sessions; 0,3 physician visits (c) mean: 4 individual and 1,5 group sessions; 1,5 physician visits |
(i) NA (c) NA |
(i) NA (c) NA |
(i)* primary access to individual PT (education, exercise therapy, pain treatment, walking aids) and group treatment (BOA-program: education, exercise therapy) (c) primary access to physician (education, medical prescription, referrals) |
| Huang et al. 2012 [49] |
Total knee replacement Outpatient, prehabilitation |
(i) daily, over 4 weeks before surgery (c) NA |
(i) NA (c) NA |
(i) 40 min/day (c) NA |
(i)* home exercises and education before replacement by PT and booklet (c) conventional pre-TKA care |
|
A Hurley et al. 2007 [52] B Hurley et al. 2012 [51] |
Knee pain (chronic) Outpatient, therapy |
(i1) 12 sessions 2x/week over 6 weeks (i2) 12 sessions 2x/week over 6 weeks (c) – |
(i1) partly (i2) partly (c) – |
(i1) 15–20 min (i2) 15–20 min (c) – |
(i1)* ESCAPE program (exercise and self-management education) (i2)* group rehabilitation program (c) usual primary care |
| Jessep et al. 2009 [54] |
Knee pain (chronic) Outpatient, therapy |
(i) 10 sessions 2x/week over 5 weeks plus booster at 4 month plus home exercises (c) mean: 4 sessions |
(i) partly (c) NA |
(i) approx. 60 min (c) NA |
(i)* adapted ESCAPE program (exercise and self-management education) (c)* usual care by PT (exercise, advice, electrotherapy, MT) |
| Kigozi et al. 2018 [58] |
Knee osteoarthritis Outpatient, therapy |
(i1) 6–8 sessions over 12 weeks (i2) 4 sessions until week 12, 4–6 follow-ups until sixth month (c) up to 4 sessions over 12 weeks |
(i1) partly (i2) partly (c) NA |
(i1) NA (i2) NA (c) NA |
(i1)* individual exercise program (i2)* targeted exercise adherence (c)* usual physiotherapeutic care (individual exercise therapy and education by booklet) |
| Knoop et al. 2023 [60] |
Knee osteoarthritis Outpatient, therapy |
(i) 3–18 sessions individual over 12 weeks plus 1–3 booster sessions (c) mean: 10 sessions over 12 weeks |
(i) NA (c) NA |
(i) NA (c) NA |
(i)* stratified exercise therapy (c)* usual exercise therapy by PT |
| McCarthy et al. 2004 [69] |
Knee osteoarthritis Outpatient, therapy |
(i) 1 initial session (education), 2x/week over 8 weeks (exercise) (c) 1 initial session (education) |
(i) yes (exercise) (c) – |
(i) 45 min (exercise) (c) NA |
(i)* c, group exercise therapy and home exercises (c)* education by PT based on the Research Campaign's information booklet 'Osteoarthritis of the knee' and home exercises # |
| Mitchell et al. 2005 [70] |
Total knee replacement Outpatient/home, prehabilitation/rehabilitation |
(i) min. 3 pre-TKR sessions and up to 6 post-discharge sessions (c) 1-2x/week (group exercise) and at PT's discretion (individual) |
(i) NA (c) NA |
(i) NA (c) NA |
(i)* individual physiotherapy at home pre- and post-TKA (c)* individual physiotherapy and group exercise therapy post-TKA only |
| Pryymachenko et al. 2021 [75] |
Knee osteoarthritis Outpatient, therapy |
(i1) 12 sessions over 1 year (i2) 12 sessions over 9 weeks (i3) 12 sessions over 1 year (c) over 9 weeks |
(i1) partly (i2) partly (i3) partly (c) partly |
(i1) NA (i2) NA (i3) NA (c) NA |
(i1)* individual exercise therapy and booster session (i2)* individual exercise therapy and manual therapy (i3)* individual exercise therapy, manual therapy and booster session (c)* individual exercise therapy # |
| Rhon et al. 2022 [76] |
Knee osteoarthritis Outpatient, therapy + |
(i) 8 sessions over 4–6 weeks, additional 3 sessions between 4 and 9th month (c) 1 session |
(i) yes (c) – |
(i) 1 h (c) – |
(i)* physical therapy (exercises, joint mobilization) (c) glucocorticoid injection |
| Sevick et al. 2000 (ex) [78] |
Knee osteoarthritis Outpatient, therapy |
(i1), (i2) month 1–3: 3x/week of 1 h month 4–6: home exercises of 1 h, bi-weekly contact to PT (4 home visits, 6 telephone calls) month 7–9: home exercises of 1 h, every 3 weeks contact to PT (telephone calls) month 10–18: 1x/month contact to PT (telephone calls) (c) month 1–3: 3 sessions of 1,5 h month 4–6: biweekly nurse contact month 7–18: 1x/month nurse contact |
(i1) yes (i2) yes (c) – |
(i1) and (i2) month 1–3: 1 h month 4–6: home exercises of 1 h month 7–9: home exercises of 1 h month 10–18: NA month 1–3: 1,5 h month 4–6: NA month 7–18: NA |
(i1)* aerobic exercise training (3 months in a group, 15 months homebased individual) (i2)* resistance exercise (3 months in a group, 15 months homebased individual) (c)* health education |
| Sevick et al. 2009 [80] |
Knee osteoarthritis Outpatient, therapy |
(i1) 1 initial visit at home, months 1–4: monthly 3 group sessions, 1 individual session months 5–6: biweekly 3 group sessions, 1 individual months 7+: biweekly telephone call or meeting and newsletter (i2) 3x/week over 4 months, after 4 month decision: continue at facility, at home or combined (i3) i1 and i2 combined (c) months 1–3: monthly meeting months 4–5: monthly phone contact months 5+: bimonthly contact |
(i1) – (i2) yes (i3) i1 and i2 combined (c) – |
(i1) 1 initial visit at home, months 1–4: NA months 5–6: NA months 7+: NA (i2) 60 min over 4 months (i3) i1 and i2 combined (c) months 1–3: 1 h months 4–5: NA months 5+: NA |
(i1) diet: group and individual (i2)* group and individual exercise therapy (i3)* i1 and i2 combined (c) healthy lifestyle control |
| Stan et al. 2015 [85] |
Knee osteoarthritis Inpatient, therapy/operation |
(i) exercises and following PT session, 2x/day over 5 days before discharging c1) – c2) – |
(i) NA c1) – c2) – |
(i) 30 min (exercises) c1) – c2) – |
(i)* individual rehabilitation program c1) total knee arthroplasty c2) total knee arthroplasty following high tibial osteotomy # |
| Tan et al. 2010 [89] |
Patellofemoral pain syndrome Outpatient, therapy |
(i) 9 sessions over 6 weeks (c) NA |
(i) NA (c) NA |
(i) NA (c) NA |
(i)* individual exercise therapy and home exercises and c-intervention (c) education by a physician |
| Van de Graaf et al. 2020 [90] |
Meniscal tear Outpatient, therapy |
(i) 16 sessions over 8 weeks, 2x/week home exercises (c) – |
(i) yes (c) – |
(i) 30 min (individual PT) (c) – |
(i)* individual physiotherapy and home exercises (c) arthroscopic partial meniscectomy and same home exercises as i # |
| Van der Graaff et al. 2023 [92] |
Meniscal tear (traumatic) Outpatient, rehabilitation |
(i) NA (c) NA |
(i) partly |
(i) NA (c) – |
(i)* exercise programme, home exercises (c) arthroscopic partial meniscectomy |
| Others/mixed | |||||
|
A Abbott et al. 2019 [13] B Pinto et al. 2013 [74] |
Hip osteoarthritis, knee osteoarthritis Outpatient, therapy |
(i1), (i2) and (i3) 7 sessions over 9 weeks, 2 booster sessions at week 16 and 54 (c) – |
A (i1) NA (i2) NA (i3) NA (c) – B (i1) partly (i2) partly (i3) partly (c) – |
(i1) approx. 50 min (i2) approx. 50 min (i3) approx. 50 min (c) – |
(i1)* individual exercise therapy (i2)* manual therapy (i3)* individual exercise and manual therapy (c) usual care in GP |
| Bulthuis et al. 2008 [25] |
Hip osteoarthritis, knee osteoarthritis Inpatient, rehabilitation |
(i) 2x/day over 3 weeks (exercise therapy), 2x/week over 3 weeks (education) (c) NA |
(i) partly (c) NA |
(i) 75 min (exercise therapy) (c) NA |
(i)* individual and group exercise therapy and education by PT (c)* usual PT-care |
| Coupé et al.‚ 2007 [31] |
Hip osteoarthritis, knee osteoarthritis Outpatient, therapy |
(i) max. 18 session over 12 weeks and max. 7 booster sessions (c) max. 18 sessions within 12 weeks |
(i) partly (c) NA |
(i) NA (c) NA |
(i)* individual exercise therapy and booster session (c)* usual physiotherapeutic care |
| Fernandes et al. 2017 [97] |
Total hip replacement, total knee replacement Outpatient, prehabilitation |
(i) 2x/week over 8 weeks (c) – |
(i) partly (c) – |
(i) 1 h (c) – |
(i)* group neuromuscular exercise program and education by PT before surgery (c) standard preoperative information by leaflet |
| Lin et al. 2008 [66] |
Ankle fracture Outpatient, therapy |
(i) mean no. of treatment: 10 sessions, 2x/week over 4 weeks (c) first week: 2 sessions, after that 1x/week, mean number of sessions: 6 |
(i) yes (c) partly |
(i) NA (c) NA |
(i)* individual physiotherapy and manual therapy (c)* individual physiotherapy |
| Other conditions | |||||
| Barnhoorn et al. 2018 [19] |
Complex regional pain syndrome type 1 Outpatient, therapy |
(i) max. 5 sessions (c) – |
(i) NA (c) – |
(i) 40 min (c) – |
(i)* individual pain exposure physical therapy (c)* usual physiotherapeutic care+ |
| Daker-White et al. 1999 [33] |
Musculoskeletal problems Outpatient, therapy |
(i) – (c) – |
(i) – (c) – |
(i) NA (c) NA |
(i)* treatment by PT (orthopedic specialist) (c) treatment by orthopedic surgeons # |
| Heij et al. 2022 [44] |
Mobility problems Outpatient, therapy |
(i) mean: 15 sessions (c) mean: 22 sessions |
(i) partly+ | (i) 30 min+ |
(i)* physical therapy (Coach2move) (c)* usual physiotherapeutic care |
| Lilje et al. 2014 [65] |
Mixed (on a waiting list for surgery regarding neck, shoulder/arm, back, pelvis/hip, knee or leg/foot condition)+ Outpatient, therapy |
(i) up to 5 sessions over 5 weeks (c) as many appointments as required |
(i) NA (c) – |
(i) 30–45 min (c) NA |
(i)* manual therapy (c) standard care of orthopedic surgeons |
| Sevick et al. 2000 (life) [79] |
Sedentary adults Outpatient, therapy |
(i) 1x/week (1–16 week), biweekly (17–24 week), 1x/month group meeting (7–12 months), every other month group meeting (13–18 months), quarterly group meeting (19–24 months) (c) exercise (1–6 months), receiving a calendar—monthly, invitation to activities, newsletter: quarterly (7–18 months) |
(i) partly (c) yes |
(i) NA (c) 20 min—1 h (exercise) |
(i)* group education and lifestyle exercise therapy (for 6 months), individual/group—education, life exercise therapy (7–18 months) (c) 1–6 months: individual exercises at a fitness facility 7–18 months: patients had the choice if they want to continue exercising at a fitness facility, calendar of activities, invitation to activities and newsletter # |
| Van den Hout et al. 2005 [91] |
Rheumatoid arthritis Outpatient, therapy |
(i) 2x/week over 2 years, in total: 60 sessions (c) mean sessions of individual PT: 8.4 over 2 years |
(i) partly (c) – |
(i) 75 min (c) NA |
(i)* group exercise therapy ('Rheumatoid Arthritis Patients in Training'-program: weight bearing) (c) usual care in GP (individual physiotherapy if necessary) |
# control group defined by authors, +information found in an additional paper, ~assumption of the authors, […] inclusion criteria, —not applicable, *physiotherapeutic treatment, NA not available, (i) intervention, (c) control intervention, A, B publications based on the same conducted study, bold printed description of one (control-) intervention the authors’ treatment of interest
ACL anterior cruciate ligament, GP general practice, LBP low back pain, PT physiotherapist(s), prehabilitation physiotherapeutic treatment before a scheduled surgery, rehabilitation physiotherapeutic treatment after a surgery or traumatic injury, therapy physiotherapeutic treatment of a degenerative disease or an inflammatory disease
Fig. 4.
Cost-effectiveness plane of any physiotherapeutic intervention versus another non-physiotherapeutic intervention. BH, behavior; ED, education; EX, exercises; H, home; IN, injection; MD, medical doctor; MT, manual therapy; MX, mixed; OT, others; PT, physiotherapy; SU, surgery; b, booster session; eb, evidence-based; g, group; i, individual; p, placebo; s, stratified care; u, usual; w, written; 2×, twice, *physiotherapeutic intervention, #no significant differences in the health outcome, ‘no significant differences in the costs
Fig. 5.
Cost-effectiveness plane of a primary physiotherapeutic intervention vs another physiotherapeutic intervention. BH, behavior; ED, education; EX, exercises; H, home; IN, injection; MD, medical doctor; MT, manual therapy; MX, mixed; OT, others; PT, physiotherapy; SU, surgery; b, booster session; eb, evidence-based; g, group; i, individual; p, placebo; s, stratified care; u, usual; w, written; 2×, twice; *physiotherapeutic intervention, #no significant differences in the health outcome, ‘no significant differences in the costs
Critical Appraisal of the Included Articles
More than two-thirds of the included 83 trials-based economic evaluations were of high quality with sum-yes-scores of 17 (n = 13), 18 (n = 16), or 19 (n = 31) on the Consensus on Health Economic Criteria checklist (Additional file 3: Table S3). The lowest score was 11 which was observed in two articles. Scores of 12, 13, and 14 were observed in two articles each. The scores 15, and 16 were reached by five and ten articles, respectively. The three items “Is a well-defined research question posed in answerable form?”, “Is the actual perspective chosen appropriate?”, and “Are all outcomes measured appropriately?” were evaluated with a ‘Yes’ for all the articles. The lowest sum of positive evaluation was observed for the item “Does the article indicate that there was no potential conflict of interest of study researchers and funders?” (n = 58). Limitations were also observed in 23 articles when it comes to the performance of incremental analyses of the costs and outcomes of alternatives. Fifty-nine publications met the criteria regarding sensitivity analyses to account for uncertain variable values. Nonetheless, the overall article quality was high.
Results of Syntheses Grouped by Body Parts
Spine
Of our 39 articles dealing with spine-related conditions four address the back in general [17, 18, 71, 84], 25 deal with the low back [14–16, 21, 26–29, 32, 38, 39, 43, 45, 46, 50, 55, 57, 59, 72, 73, 77, 83, 87, 93, 95], six with the neck [24, 62–64, 68, 94] and four include mixed patients [34, 67, 81, 82] (Tables 1, 2).
The four articles on general back conditions [17, 18, 71, 84] built on three clinical trials. The sessions varied between 1 and 36 over a time horizon of 1 to 24 weeks. Most interventions were conducted 1–2 times per week. The duration if indicated varied between 60 and 90 min. The intervention and control groups contained individual and group-based exercise therapy, manual therapy, and education as well as usual care (Table 2). Group exercise therapy was deemed cost-effective over usual care [71] and interpatient exchange group meetings were cost-effective over increasing the frequency of traditional therapy according to the authors [84]. The articles from Barker et al. considered three interventions provided by physiotherapists [17, 18]. The findings of all cost-effectiveness comparisons can be found in Figs. 4 and 5.
The 25 articles on low back pain were built on 24 clinical trials [14–16, 21, 26–29, 32, 38, 39, 43, 45, 46, 50, 55, 57, 59, 72, 73, 77, 83, 87, 93, 95]. Niemistö et al. published two articles based on the same clinical trial [72, 73]. Patients received between 1 and 46 sessions lasting between 20 and 120 min, spread out over a maximum of 30 weeks. Sessions were most often offered 1 to 3 times a week. The treatments in the intervention and control groups included mostly group and individual exercise therapy, individual physiotherapeutic treatments, and education. Additional manual therapy, McKenzie-based treatments, behavioral graded activity, behavior change techniques, a walking program, visits at the workplace, yoga, usual care, chiropractic treatment, and a massage chair were provided (Table 2). Fritz et al. compared individual physical therapy following evidence-based guidelines to physical therapy not following those guidelines and found that following evidence-based guidelines is cost-effective [38]. The articles on low back pain included a total of 67 comparisons of interventions of which 34 were between a physiotherapeutic intervention and another treatment (Figs. 4, 5).
Of the 6 articles on neck conditions all addressed neck pain [24, 62–64, 68, 94]. One to 24 sessions were offered. They lasted between 20 and 60 min and were spread over up to 12 weeks. Most treatments were offered 1–2 times per week. The intervention contained exercises, cognitive behavioral treatment, behavior-graded activity, manual therapy, individual therapy, and advice. The control group received exercises, usual care involving physiotherapeutic treatments, and written information (Table 2). The articles involve 12 treatment comparisons. Five highlighted better outcomes at higher costs for the physiotherapeutic intervention, and three were dominant. In the four dominated investigations three of the comparison interventions were offered by physiotherapists (Figs. 4, 5).
Two of the four articles with a mixed spine population originated from the same study. These studies did not differentiate between neck and back pain [34, 67, 81, 82]. Participants received up to 8 sessions. One article focused on physiotherapeutic care in comparison to traditional medical referral care, another compared the McKenzie treatment concept to the individual solution-finding approach, and the remaining two, from the same study, compared physiotherapeutic to chiropractic care (Table 2). Considering only the effectiveness, all articles favored the intervention offered by physiotherapists, although not significantly in the articles by Skargren et al. [81,82]. In the article of Manca et al. the psychotherapeutic treatments involved higher costs [67]; dominance of the physiotherapeutic treatment was found in the remaining articles [34, 81, 82] (Figs. 4, 5).
Upper Limb
The seven papers addressing the upper limb dealt with carpal tunnel syndrome [37], epicondylitis lateralis [61, 86], and shoulder complaints [23, 41, 53] involving a rotator cuff disorder [48]. The number of intervention and control group sessions varied between 3 and 18. Patients were treated 1–2 times a week for 20 to 60 min. All but three articles involved one intervention and one control group. The exceptions involved three different intervention groups. The provided interventions contained manual therapy, education, exercises, and physiotherapeutic treatments such as friction, ultrasound, and massage. The control groups received surgery, injections, braces, and usual care. One study also included a wait-and-see approach (Table 2). The articles involve 14 treatment comparisons. The physiotherapeutic treatment for carpal tunnel syndrome was dominant [37]. The remaining comparison of physiotherapeutic interventions, but one, may as well be cost-effective, depending on the willingness to pay (Figs. 4, 5).
Lower Limb
The included 30 articles built on 28 clinical trials dealing with the lower limb. Of these trials, four addressed the hip [40, 42, 56, 88], nineteen the knee [20, 22, 35, 47, 49, 51, 52, 54, 58, 60, 69, 70, 75, 78, 80, 85, 88, 92], and five a mixed population [13, 25, 31, 36, 66, 74]. Nineteen of the clinical trials dealt with osteoarthritis including the last therapy option of a joint replacement [13, 22, 25, 31, 36, 40, 47, 49, 56, 58, 60, 69, 70, 75, 76, 78, 80, 85, 88].
Among the hip-related clinical trials, three dealt with osteoarthritis and one addressed the femoroacetabular impingement syndrome [42]. Patients participated in 1 to 12 sessions. The duration of a session ranged from 30 to 60 min. The frequency varied between twice a day in the inpatient setting and one time in 2 weeks. The treatments offered contained individual as well as group exercises and education. The control groups received the usual care or an arthroscopy. Besides that, Fusco et al. compared the cost-effectiveness of a treatment with or without limiting hip motion [40] (Table 2). They conclude that not limiting hip motions after a hip replacement is dominant. Similarly, Griffin et al. and Juhakoski et al. highlight dominance of the physiotherapeutic treatment [42, 56]. However, Tan et al. found, that the physiotherapeutic intervention involved cost savings but was also less effective [89] (Figs. 4, 5).
The 19 knee complaint clinical trials bear 20 included articles. Two articles built on one clinical trial dealing with chronic knee pain [64, 65]. One article deals with patellofemoral pain [89], one with ACL tears [35], two with meniscal tears [90, 92], and two with knee pain [20, 54]. The remaining twelve articles investigated treatments for knee osteoarthritis. Patients participated in 1 to 18 sessions spread out mostly over 12 weeks (minimum 6 weeks, maximum 12 months). Inpatients were treated up to twice a day and all patients were treated at least once a month. The intervention for knee pain patients lasted the longest—24 months. Interventions contained mainly individual as well as group-based exercise therapy and education, but manual therapy was also offered in some clinical trials. The control groups received usual care, injections, surgery, education, and physiotherapeutic treatments (Table 2). In total the articles include 40 treatment comparisons (Figs. 4, 5).
Of the five trials on mixed lower limb conditions, we included five articles dealing with hip and knee osteoarthritis [13, 25, 31, 36, 74], and one article on ankle fractures [66]. The patients participated in 6 to 18 sessions spread out over 3 to 12 weeks. Inpatients again received treatments up to twice a day, but most interventions were offered 1–2 times a week. The sessions lasted between 50 and 75 min and contained individual physiotherapeutic treatments, manual therapy, and individual and group-based exercises. The control groups received information, usual care, and individual physiotherapeutic treatments (Table 2). Three articles favored a physiotherapeutic treatment. The remaining articles compared different physiotherapeutic treatments with each other. It was highlighted by the authors, that exercise therapy (individual and group) and education were more cost-effective than usual physiotherapeutic care [25], and that individual physiotherapy alone is cost-effective compared to individual physiotherapy combined with manual therapy [66] (Figs. 4, 5).
Other Conditions
Other conditions evaluated in cost-effectiveness studies included the complex regional pain syndrome [19], musculoskeletal problems [33], rheumatoid arthritis [91], and mixed patients [44, 65, 79] consisting of older adults, sedentary adults, and orthopedic outpatients. Patients participated in 5 to 60 sessions over a maximum of 24 months. The interventions contained individual pain exposure therapy, physiotherapeutic care, education, manual therapy, and group exercises. The control groups received usual care and exercises (Table 2). In each of the six articles only one cost-effectiveness comparison was performed (Figs. 4, 5).
Summary
The provided details on the delivered treatments varied widely between articles. A type of treatment was mentioned in all, however three articles only named “physiotherapy” as treatment without further explanations. Information on the frequency of the treatment was given in 67 articles; 16 provided no information. Similarly, the intensity was mentioned in 53 articles and missing in 30 articles. However, 28 of the 53 articles providing information on the intensity only mention that it was increased during the intervention or tailored to the patient without further explanation. Finally, the dose was mentioned in 55 and lacking in 28 articles (Table 2).
Due to the limited description of the interventions and the heterogeneity of treatment combinations in the intervention and control groups, summarizing comparisons based on interventions was largely restricted.
Nonetheless, in the 81 comparisons between a physiotherapeutic intervention and any other intervention we found the following insights [13, 14, 19, 20, 23, 26, 29, 30, 33–35, 37, 39, 41, 42, 45–49, 51–53, 55–57, 59, 61–63, 65, 67, 68, 72, 74, 76, 79–82, 84–92, 95–97]: 27 comparisons were performed between a physiotherapeutic intervention (without care provided by a medical doctor) and an intervention involving care from a medical doctor (Fig. 4) [13, 23, 26, 33, 34, 41, 46, 47, 49, 51, 52, 56, 62, 65, 72–74, 88, 91]. Of those about 50% (n = 13) were dominant [13, 34, 46, 47, 49, 51, 56, 62, 72, 74], two were dominated [52, 91], one involved lower costs and lower effects [88], and 11 had better outcomes but involved higher costs [13, 23, 26, 33, 41, 52, 74, 96]. Seven comparisons involved surgery in the control group [35, 37, 42, 85, 92], most of these (n = 6) were more expensive than the physiotherapeutic intervention [35, 37, 42, 85, 92]. The clinical outcome of the physiotherapeutic interventions was better in three of the comparisons [37, 42, 92]. Additionally, we found three comparisons between an intervention provided by a physiotherapist with one provided by a chiropractor [29, 81, 82]. Two originate from the same study and found physiotherapeutic care to be dominant, however, in the third comparison physiotherapeutic care was dominated. Injections were compared to solely other treatments in five comparisons stemming from three studies [30, 48, 53]. In three of these comparisons, physiotherapeutic care was more expensive but led also to better effects [30, 53]. In the remaining two comparisons (from the same study) physiotherapeutic care was cheaper but also less effective (Fig. 4).
Among the 69 comparisons between two physiotherapeutic interventions [13–18, 21, 22, 24–28, 31, 32, 38, 40, 43, 44, 48, 50, 52, 54, 57, 58, 60, 62–64, 66, 69–71, 74, 75, 77, 78, 80, 83, 86, 93, 94], we found 57 mentioning exercises as a treatment modality [13–18, 21, 22, 25–28, 31, 32, 48, 54, 57, 58, 60, 63, 64, 69–71, 74, 75, 78, 80, 83, 94, 93], however, it should be noted that if usual physiotherapy was provided this could also include exercises. Nonetheless, since it was not explicitly mentioned we do not consider “usual physiotherapy” as any intervention involving exercises. Of those comparisons 22 mentioned exercises for both comparators. Twenty-four of the comparisons involved manual therapy as part of an intervention, four in both groups [13, 16–18, 24, 26, 62–64, 66, 74, 75, 94]. Again, it should be noted that individual physiotherapy could have included manual therapies as well but this was not mentioned. Overall, there was no clear trend regarding the cost and the clinical outcomes observed. Having a closer look at comparisons between group-based and individual physiotherapeutic interventions, we found no clear trend regarding cost-effectiveness. This can partly be explained by the mixed treatments that were involved in these interventions as well, hindering clear comparisons.
Discussion
Key Results
Several good quality cost-effectiveness evaluations of physiotherapeutic interventions for patients with musculoskeletal conditions exist. Low back and knee conditions are frequently evaluated, however, for conditions addressing other joints none to few studies are available, here further research is needed. Unfortunately, the description of investigated interventions is often limited in detail and the combination of treatments varies widely. This restricted the ability to fairly compare different treatments.
In the comparisons between a physiotherapeutic intervention and those provided by other health professionals, a minor indication of physiotherapy was found to be cost-effective. Of the 42 comparisons between physiotherapeutic care and care provided by a chiropractor or a medical doctor involving surgeries and injections, we found that 18 were dominant and only four were dominated. For the 14 comparisons with higher costs and better effects, as well as for the 6 with a lower effect and lower costs the willingness to pay is crucial for deciding if the treatment should be considered cost-effective or not. The identification of which physiotherapeutic interventions are cost-effective was hindered by clear descriptions of the provided interventions and similar comparisons of treatment combinations.
To the best of our knowledge, this is the first review summarizing the findings of cost-effectiveness evaluations of physiotherapeutic interventions for musculoskeletal conditions. The earliest full-economic evaluation of a physiotherapeutic intervention for a musculoskeletal condition was published in 1994. However, since 2003 at least one new trial-based economic evaluation article has been released each year. This long inclusion period should be noticed when evaluating the relevance of a specific recommended treatment. The physiotherapeutic care and also the comparison treatments could have been enhanced during this time, meaning careful consideration of the (albeit often limited) intervention details is necessary before implementation.
Similarly, when utilizing and comparing the individual study findings of this review the underlying context of the study, the clinical outcome measures, and the findings of the Health Economic Criteria checklist should be considered. Different healthcare systems, as well as the culture of clinicians and patients could influence the cost-effectiveness. As an example, while in some countries like the Netherlands, Great Britain, and Sweden the patients may proceed directly to the physiotherapist, in other countries like Germany they have to consult a medical doctor first—this of course affects the overall cost-effectiveness and should be considered when studies from different countries are compared. Similarly, summarizing and comparing studies that utilized different health outcome measures is challenging. Of course, it is most important that the clinical outcomes are relevant to the patient, however, if different health outcome measures are utilized the comparison of the studies is limited, as the cost-effectiveness might change with a different health outcome. Finally, attention should be given to the evaluation of the Health Economic Criteria checklist of the individual studies/comparisons, which we do not indicate in the cost-effectiveness plane.
The availability of economic evaluation studies in our work mirrors the prevalence of the conditions, which is in line with previous reviews [9, 98]. We found that osteoarthritis was frequently studied. Similarly, a review of orthopedic surgery interventions found that joint arthroplasty, which is the last treatment option for patients with hip and knee osteoarthritis, was commonly investigated in related cost-effectiveness analyses [98]. Additionally, like our work, a review on physical exercise found most cost-effectiveness studies involved back conditions, osteoarthritis, and knee pain [10]. Single studies were also found for the musculoskeletal disorders of the shoulder and the neck [10].
That review [10] on physical exercise in the treatment of various diseases overlaps partly with our study. It includes 28 studies on musculoskeletal conditions of which we included 12 as well. However, the investigators focused on exercises as an intervention while we focused on treatments delivered by physiotherapists.
Interestingly, exercise was the most studied physiotherapeutic treatment in our work. Unfortunately, the treatments like exercise considered in our review were often combined with other treatments such as education, which often leaves the effectiveness of one specific treatment modality open. Furthermore, the treatments were rarely described sufficiently. For exercises e.g. they often lacked at least one dimension of frequency, intensity, time, and type of exercises e.g. aerobic vs. anaerobic or group vs individual therapy. Some articles even mentioned physiotherapy as provided treatment only. However, physiotherapy is not a treatment but a profession [99]. Consequently, several of the described interventions lack details, which leaves practitioners with the intention to implement cost-effective treatments with uncertainty and limits the ability to compare between different physiotherapeutic treatments.
The lack of provided details of the provided physiotherapeutic intervention is present in several studies and in clinical practice. Some initiatives aim to improve the documentation of provided treatments [100, 101]. However, they often apply to one specific treatment only such as exercises or the McKenzie treatment method [102]. Therefore, their applicability to other physiotherapeutic treatments is limited and therapists without special training sometimes do not understand the documentation. Hence, a specific but detailed documentation system for the provision of physiotherapeutic treatments is yet to the best of our knowledge missing.
Interestingly the provided treatments were similar across different body parts. This might suggest that the ideal treatment for a painful joint does not depend on the location. However, studies with more detailed treatment descriptions and with mixed population groups need to prove this hypothesis.
Future Research
The findings of our study indicate that there is a lack of economic evaluations for musculoskeletal conditions affecting joints other than the back and knee. Furthermore, conditions other than osteoarthritis such as fractures were rarely investigated and need further attention. Finally, systematic reviews of economic evaluations for physiotherapeutic treatments of back and knee complaints may be indicated, if not already covered by available reviews [103–106]. Additionally, a systematic review of the cost-effectiveness of preventive interventions could be interesting, since our focus was on studies dealing with patients with musculoskeletal conditions, thus excluding primary preventions.
Strength and Limitations
The major limitation of our study relates to the investigated interventions. First, defining the inclusion and exclusion criteria for an intervention was challenging. We aimed to include physiotherapeutic interventions, however, there is a large body of treatments such as tai chi, yoga, behavior change techniques, etc. which can be offered by physiotherapists but require further training. This training is open to non-health professionals as well. Some treatments e.g. behavior change techniques can also be offered by other health professionals who may be better qualified and thus more likely to provide a specific treatment. Furthermore, we decided to take a rather narrow approach regarding the inclusion criteria to ensure that the intervention was offered by physiotherapists. Second, we excluded conference abstracts, reviews, and model-based studies, which might involve the exclusion of relevant publications. Finally, our systematic search could have been broadened by additional search terms and the involvement of an additional database. This could have identified additional relevant publications since two of the included publications were only identified through the recommendation of experts in the field. The major strength of this overview is its transparency. Besides publishing a protocol and providing details on the conduct of our study and using the PRISMA statement, we also provide a list of the excluded full-text publications. The qualitative completeness of this review is underpinned by the quality evaluation of the individual articles and the provision of a cost-effectiveness plane. Consequently, we provide insights on the availability and quality of available articles and in this way highlight knowledge gaps in the literature.
Conclusions
Several high-quality trial-based economic evaluations of physiotherapeutic interventions for patients with musculoskeletal disorders exist and demonstrate cost-effectiveness. However, most articles address low back and knee conditions, and evaluations concerning other joints are limited. Finally, the documentation of provided interventions needs improvement to enable clinicians and stakeholders to fairly compare and finally to implement cost-effective treatments.
Supplementary Information
Additional file 1. Details on the PubMed search.
Additional file 2. Overview of excluded full text articles.
Additional file 3. Evaluation of the study quality with the Consensus on Health Economic Criteria checklist.
Acknowledgements
Not applicable.
Abbreviations
- QALY
Quality-adjusted life-year
- RCT
Randomized controlled trial
Author’s contribution
LB: conceptualization, methodology, formal analysis, writing—original draft, writing—review and editing. WF: methodology, formal analysis, writing—original draft, writing—review and editing. BK: conceptualization, methodology, formal analysis, writing—review and editing. AH: conceptualization, methodology, writing—review and editing. HHK: conceptualization, methodology, formal analysis, writing—review and editing. All authors read and approved the final version.
Funding
Open Access funding enabled and organized by Projekt DEAL. No sources of funding were used to assist in the preparation of this article.
Availability of Data and Materials
All data involved data in this article are available online through the original articles. Where there is uncertainty, the authors are happy to provide details on the analyses on request.
Declarations
Ethics Approval and Consent to Participate
No ethic approval was required for this review article. This review was registered at Prospero with the ID “CRD42021276050”.
Consent for Publication
Not applicable.
Competing interests
The authors declare no conflicts of interest with the content of this review.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.World Health Organization. Musculoskeletal health. 2022, 2023. https://www.who.int/news-room/fact-sheets/detail/musculoskeletal-conditions#:~:text=A%20recent%20analysis%20of%20Global,and%20rheumatoid%20arthritis%20(1). Accessed 7 Mar 2023.
- 2.Kapitel 5.3.2 Inanspruchnahme [Gesundheit in Deutschland, 2015], 2024. https://www.gbe-bund.de/gbe/abrechnung.prc_abr_test_logon?p_uid=gast&p_aid=0&p_knoten=FID&p_sprache=D&p_suchstring=25752. Accessed 10 Feb 2024.
- 3.Williams A, Kamper SJ, Wiggers JH, et al. Musculoskeletal conditions may increase the risk of chronic disease: a systematic review and meta-analysis of cohort studies. BMC Med. 2018;16:1–9. doi: 10.1186/s12916-018-1151-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Björnsdóttir S, Jónsson S, Valdimarsdóttir U. Mental health indicators and quality of life among individuals with musculoskeletal chronic pain: a nationwide study in Iceland. Scand J Rheumatol. 2014;43(5):419–423. doi: 10.3109/03009742.2014.881549. [DOI] [PubMed] [Google Scholar]
- 5.Gesundheitsausgaben nach Leistungsarten. 2021; https://www.destatis.de/DE/Themen/Gesellschaft-Umwelt/Gesundheit/Gesundheitsausgaben/Tabellen/leistungsarten.html.
- 6.Turner HC, Archer RA, Downey LE, et al. An introduction to the main types of economic evaluations used for informing priority setting and resource allocation in healthcare: key features, uses, and limitations. Front Public Health. 2021;9:722927. doi: 10.3389/fpubh.2021.722927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Grønne DT, Roos EM, Ibsen R, Kjellberg J, Skou ST. Cost-effectiveness of an 8-week supervised education and exercise therapy programme for knee and hip osteoarthritis: a pre–post analysis of 16 255 patients participating in good life with osteoArthritis in Denmark (GLA: D) BMJ Open. 2021;11(12):e049541. doi: 10.1136/bmjopen-2021-049541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mazzei D, Ademola A, Abbott J, Sajobi T, Hildebrand K, Marshall D. Are education, exercise and diet interventions a cost-effective treatment to manage hip and knee osteoarthritis? A systematic review. Osteoarthr Cartil. 2021;29(4):456–470. doi: 10.1016/j.joca.2020.10.002. [DOI] [PubMed] [Google Scholar]
- 9.García-Álvarez D, Sempere-Rubio N, Faubel R. Economic evaluation in neurological physiotherapy: a systematic review. Brain Sci. 2021;11(2):265. doi: 10.3390/brainsci11020265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Roine E, Roine RP, Räsänen P, Vuori I, Sintonen H, Saarto T. Cost-effectiveness of interventions based on physical exercise in the treatment of various diseases: a systematic literature review. Int J Technol Assess Health Care. 2009;25(4):427–454. doi: 10.1017/S0266462309990353. [DOI] [PubMed] [Google Scholar]
- 11.Baumbach L, König H-H, Kretzler B, Hajek A. Economic evaluations of musculoskeletal physiotherapy: protocol of a systematic review. BMJ Open. 2022;12(2):e058143. doi: 10.1136/bmjopen-2021-058143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Evers S, Goossens M, De Vet H, Van Tulder M, Ament A. Criteria list for assessment of methodological quality of economic evaluations: consensus on health economic criteria. Int J Technol Assess Health Care. 2005;21(2):240–245. doi: 10.1017/S0266462305050324. [DOI] [PubMed] [Google Scholar]
- 13.Abbott JH, Wilson R, Pinto D, Chapple CM, Wright AA. Incremental clinical effectiveness and cost effectiveness of providing supervised physiotherapy in addition to usual medical care in patients with osteoarthritis of the hip or knee: 2-year results of the MOA randomised controlled trial. Osteoarthr Cartil. 2019;27(3):424–434. doi: 10.1016/j.joca.2018.12.004. [DOI] [PubMed] [Google Scholar]
- 14.Aboagye E, Karlsson ML, Hagberg J, Jensen I. Cost-effectiveness of early interventions for non-specific low back pain: a randomized controlled study investigating medical yoga, exercise therapy and self-care advice. J Rehabil Med. 2015;47(2):167–173. doi: 10.2340/16501977-1910. [DOI] [PubMed] [Google Scholar]
- 15.Ankjaer-Jensen A, Manniche C, Nielsen H. [Postoperative rehabilitation of patients operated for lumbar disk prolapse. An analysis of the socioeconomic consequences] Ugeskr Laeger. 1994;156(5):647–652. [PubMed] [Google Scholar]
- 16.Apeldoorn AT, Bosmans JE, Ostelo RW, de Vet HC, van Tulder MW. Cost-effectiveness of a classification-based system for sub-acute and chronic low back pain. Eur Spine J. 2012;21(7):1290–1300. doi: 10.1007/s00586-011-2144-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Barker KL, Newman M, Stallard N, et al. Exercise or manual physiotherapy compared with a single session of physiotherapy for osteoporotic vertebral fracture: three-arm PROVE RCT. Health Technol Assess. 2019;23(44):1–318. doi: 10.3310/hta23440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Barker KL, Room J, Knight R, et al. Outpatient physiotherapy versus home-based rehabilitation for patients at risk of poor outcomes after knee arthroplasty: CORKA RCT. Health Technol Assess. 2020;24(65):1–116. doi: 10.3310/hta24650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Barnhoorn K, Staal JB, van Dongen RT, et al. Pain exposure physical therapy versus conventional treatment in complex regional pain syndrome type 1-a cost-effectiveness analysis alongside a randomized controlled trial. Clin Rehabil. 2018;32(6):790–798. doi: 10.1177/0269215518757050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Barton GR, Sach TH, Jenkinson C, Doherty M, Avery AJ, Muir KR. Lifestyle interventions for knee pain in overweight and obese adults aged >=45: economic evaluation of randomised controlled trial. BMJ. 2009;339:b2273. doi: 10.1136/bmj.b2273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bello AI, Quartey J, Lartey M. Efficacy of behavioural graded activity compared with conventional exercise therapy in chronic non-specific low back pain: implication for direct health care cost. Ghana Med J. 2015;49(3):173–180. doi: 10.4314/gmj.v49i3.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bennell KL, Ahamed Y, Jull G, et al. Physical therapist-delivered pain coping skills training and exercise for knee osteoarthritis: randomized controlled trial. Arthritis Care Res (Hoboken) 2016;68(5):590–602. doi: 10.1002/acr.22744. [DOI] [PubMed] [Google Scholar]
- 23.Bergman GJD, Winter JC, van Tulder MW, Meyboom-de Jong B, Postema K, van der Heijden GJMG. Manipulative therapy in addition to usual medical care accelerates recovery of shoulder complaints at higher costs: economic outcomes of a randomized trial. BMC Musculoskelet Disord. 2010;11:200. doi: 10.1186/1471-2474-11-200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bosmans JE, Pool JJM, Vet HCWd, van Tulder MW, Ostelo RWJG. Is behavioral graded activity cost-effective in comparison with manual therapy for patients with subacute neck pain? An economic evaluation alongside a randomized clinical trial. Spine. 2011;36(18):E1179–E1186. doi: 10.1097/BRS.0b013e31820644ed. [DOI] [PubMed] [Google Scholar]
- 25.Bulthuis Y, Mohammad S, Braakman-Jansen LM, Drossaers-Bakker KW, van de Laar MA. Cost-effectiveness of intensive exercise therapy directly following hospital discharge in patients with arthritis: results of a randomized controlled clinical trial. Arthritis Rheum. 2008;59(2):247–254. doi: 10.1002/art.23332. [DOI] [PubMed] [Google Scholar]
- 26.Burton United Kingdom back pain exercise and manipulation (UK BEAM) randomised trial: cost effectiveness of physical treatments for back pain in primary care. BMJ. 2004;329(7479):1381. doi: 10.1136/bmj.38282.607859.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Canaway A, Pincus T, Underwood M, Shapiro Y, Chodick G, Ben-Ami N. Is an enhanced behaviour change intervention cost-effective compared with physiotherapy for patients with chronic low back pain? Results from a multicentre trial in Israel. BMJ Open. 2018;8(4):e019928. doi: 10.1136/bmjopen-2017-019928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Carr JL, Klaber Moffett JA, Howarth E, et al. A randomized trial comparing a group exercise programme for back pain patients with individual physiotherapy in a severely deprived area. Disabil Rehabil. 2005;27(16):929–937. doi: 10.1080/09638280500030639. [DOI] [PubMed] [Google Scholar]
- 29.Cherkin DC, Deyo RA, Battié M, Street J, Barlow W. A comparison of physical therapy, chiropractic manipulation, and provision of an educational booklet for the treatment of patients with low back pain. N Engl J Med. 1998;339(15):1021–1029. doi: 10.1056/NEJM199810083391502. [DOI] [PubMed] [Google Scholar]
- 30.Coombes BK, Connelly L, Bisset L, Vicenzino B. Economic evaluation favours physiotherapy but not corticosteroid injection as a first-line intervention for chronic lateral epicondylalgia: evidence from a randomised clinical trial. Br J Sports Med. 2015;50:1400–1405. doi: 10.1136/bjsports-2015-094729. [DOI] [PubMed] [Google Scholar]
- 31.Coupé VM, Veenhof C, van Tulder MW, Dekker J, Bijlsma JW, Van den Ende CH. The cost effectiveness of behavioural graded activity in patients with osteoarthritis of hip and/or knee. Ann Rheum Dis. 2007;66(2):215–221. doi: 10.1136/ard.2006.054478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Critchley DJ, Ratcliffe J, Noonan S, Jones RH, Hurley MV. Effectiveness and cost-effectiveness of three types of physiotherapy used to reduce chronic low back pain disability: a pragmatic randomized trial with economic evaluation. Spine (Phila Pa 1976) 2007;32(14):1474–1481. doi: 10.1097/BRS.0b013e318067dc26. [DOI] [PubMed] [Google Scholar]
- 33.Daker-White G, Carr AJ, Harvey I, et al. A randomised controlled trial. Shifting boundaries of doctors and physiotherapists in orthopaedic outpatient departments. J Epidemiol Community Health. 1999;53(10):643–650. doi: 10.1136/jech.53.10.643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Denninger TR, Cook CE, Chapman CG, McHenry T, Thigpen CA. The influence of patient choice of first provider on costs and outcomes: analysis from a physical therapy patient registry. J Orthop Sports Phys Ther. 2018;48(2):63–71. doi: 10.2519/jospt.2018.7423. [DOI] [PubMed] [Google Scholar]
- 35.Eggerding V, Reijman M, Meuffels DE, et al. ACL reconstruction for all is not cost-effective after acute ACL rupture. Br J Sports Med. 2021;56:24–28. doi: 10.1136/bjsports-2020-102564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fernandes L, Roos EM, Overgaard S, Villadsen A, Søgaard R. Supervised neuromuscular exercise prior to hip and knee replacement: 12-month clinical effect and cost-utility analysis alongside a randomised controlled trial. BMC Musculoskelet Disord. 2017;18(1):1–11. doi: 10.1186/s12891-016-1369-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Fernández-de-Las-Peñas C, Ortega-Santiago R, Díaz HF, et al. Cost-effectiveness evaluation of manual physical therapy versus surgery for carpal tunnel syndrome: evidence from a randomized clinical trial. J Orthop Sports Phys Ther. 2019;49(2):55–63. doi: 10.2519/jospt.2019.8483. [DOI] [PubMed] [Google Scholar]
- 38.Fritz JM, Cleland JA, Speckman M, Brennan GP, Hunter SJ. Physical therapy for acute low back pain: associations with subsequent healthcare costs. Spine (Phila Pa 1976) 2008;33(16):1800–1805. doi: 10.1097/BRS.0b013e31817bd853. [DOI] [PubMed] [Google Scholar]
- 39.Fritz JM, Kim M, Magel JS, Asche CV. Cost-effectiveness of primary care management with or without early physical therapy for acute low back pain: economic evaluation of a randomized clinical trial. Spine (Phila Pa 1976) 2017;42(5):285–290. doi: 10.1097/BRS.0000000000001729. [DOI] [PubMed] [Google Scholar]
- 40.Fusco F, Campbell H, Barker K. Rehabilitation after resurfacing hip arthroplasty: cost-utility analysis alongside a randomized controlled trial. Clin Rehabil. 2019;33(6):1003–1014. doi: 10.1177/0269215519827628. [DOI] [PubMed] [Google Scholar]
- 41.Geraets JJXR, Goossens MEJB, Bruijn CPCd, et al. Cost-effectiveness of a graded exercise therapy program for patients with chronic shoulder complaints. Int J Technol Assess Health Care. 2006;22(1):76–83. doi: 10.1017/S0266462306050860. [DOI] [PubMed] [Google Scholar]
- 42.Griffin DR, Dickenson EJ, Achana F, et al. Arthroscopic hip surgery compared with personalised hip therapy in people over 16 years old with femoroacetabular impingement syndrome: UK FASHIoN RCT. Health Technol Assess (Winchester, England) 2022;26(16):1–236. doi: 10.3310/FXII0508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hahne AJ, Ford JJ, Surkitt LD, et al. Individualized physical therapy is cost-effective compared with guideline-based advice for people with low back disorders. Spine (Phila Pa 1976) 2017;42(3):E169–E176. doi: 10.1097/BRS.0000000000001734. [DOI] [PubMed] [Google Scholar]
- 44.Heij W, Sweerts L, Staal JB, et al. Implementing a personalized physical therapy approach (Coach2Move) is effective in increasing physical activity and improving functional mobility in older adults: a cluster-randomized, stepped wedge trial. Phys Ther. 2022;102:138. doi: 10.1093/ptj/pzac138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Herman PM, Szczurko O, Cooley K, Mills EJ. Cost-effectiveness of naturopathic care for chronic low back pain. Altern Ther Health Med. 2008;14(2):32–39. [PubMed] [Google Scholar]
- 46.Hlobil H, Uegaki K, Staal JB, de Bruyne MC, Smid T, van Mechelen W. Substantial sick-leave costs savings due to a graded activity intervention for workers with non-specific sub-acute low back pain. Eur Spine J. 2007;16(7):919–924. doi: 10.1007/s00586-006-0283-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ho-Henriksson C-M, Svensson M, Thorstensson CA, Nordeman L. Physiotherapist or physician as primary assessor for patients with suspected knee osteoarthritis in primary care - a cost-effectiveness analysis of a pragmatic trial. BMC Musculoskelet Disord. 2022;23(1):260. doi: 10.1186/s12891-022-05201-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hopewell S, Keene DJ, Heine P, et al. Progressive exercise compared with best-practice advice, with or without corticosteroid injection, for rotator cuff disorders: the GRASP factorial RCT. Health Technol Assess. 2021;25(48):1–158. doi: 10.3310/hta25480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Huang SW, Chen PH, Chou YH. Effects of a preoperative simplified home rehabilitation education program on length of stay of total knee arthroplasty patients. Orthop Traumatol Surg Res. 2012;98(3):259–264. doi: 10.1016/j.otsr.2011.12.004. [DOI] [PubMed] [Google Scholar]
- 50.Hurley DA, Tully MA, Lonsdale C, et al. Supervised walking in comparison with fitness training for chronic back pain in physiotherapy: results of the SWIFT single-blinded randomized controlled trial (ISRCTN17592092) Pain. 2015;156(1):131–147. doi: 10.1016/j.pain.0000000000000013. [DOI] [PubMed] [Google Scholar]
- 51.Hurley MV, Walsh NE, Mitchell H, Nicholas J, Patel A. Long-term outcomes and costs of an integrated rehabilitation program for chronic knee pain: a pragmatic, cluster randomized, controlled trial. Arthritis Care Res (Hoboken) 2012;64(2):238–247. doi: 10.1002/acr.20642. [DOI] [PubMed] [Google Scholar]
- 52.Hurley MV, Walsh NE, Mitchell HL, et al. Economic evaluation of a rehabilitation program integrating exercise, self-management, and active coping strategies for chronic knee pain. Arthritis Rheum. 2007;57(7):1220–1229. doi: 10.1002/art.23011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.James M, Stokes EA, Thomas E, Dziedzic K, Hay EM. A cost consequences analysis of local corticosteroid injection and physiotherapy for the treatment of new episodes of unilateral shoulder pain in primary care. Rheumatology. 2005;44(11):1447–1451. doi: 10.1093/rheumatology/kei043. [DOI] [PubMed] [Google Scholar]
- 54.Jessep SA, Walsh NE, Ratcliffe J, Hurley MV. Long-term clinical benefits and costs of an integrated rehabilitation programme compared with outpatient physiotherapy for chronic knee pain. Physiotherapy. 2009;95(2):94–102. doi: 10.1016/j.physio.2009.01.005. [DOI] [PubMed] [Google Scholar]
- 55.Johnson RE, Jones GT, Wiles NJ, et al. Active exercise, education, and cognitive behavioral therapy for persistent disabling low back pain: a randomized controlled trial. Spine (Phila Pa 1976) 2007;32(15):1578–1585. doi: 10.1097/BRS.0b013e318074f890. [DOI] [PubMed] [Google Scholar]
- 56.Juhakoski R, Tenhonen S, Malmivaara A, Kiviniemi V, Anttonen T, Arokoski JP. A pragmatic randomized controlled study of the effectiveness and cost consequences of exercise therapy in hip osteoarthritis. Clin Rehabil. 2011;25(4):370–383. doi: 10.1177/0269215510388313. [DOI] [PubMed] [Google Scholar]
- 57.Karjalainen K, Malmivaara A, Pohjolainen T, et al. Mini-intervention for subacute low back pain: a randomized controlled trial: LWW. Spine. 2003;28(6):533–540. doi: 10.1097/01.BRS.0000049928.52520.69. [DOI] [PubMed] [Google Scholar]
- 58.Kigozi J, Jowett S, Nicholls E, Tooth S, Hay EM, Foster NE. Cost-utility analysis of interventions to improve effectiveness of exercise therapy for adults with knee osteoarthritis: the BEEP trial. Rheumatol Adv Pract. 2018;2(2):rky1018. doi: 10.1093/rap/rky018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kim G, Kim WS, Kim TW, Lee YS, Lee H, Paik NJ. Home-based rehabilitation using smart wearable knee exercise device with electrical stimulation after anterior cruciate ligament reconstruction: a study protocol for a randomized controlled trial. Medicine (Baltimore) 2020;99(20):e20256. doi: 10.1097/MD.0000000000020256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Knoop J, Esser J, Dekker J, de Joode JW, Ostelo RW, van Dongen JM. No evidence for stratified exercise therapy being cost-effective compared to usual exercise therapy in patients with knee osteoarthritis: economic evaluation alongside cluster randomized controlled trial. Braz J Phys Ther. 2023;27(1):100469. doi: 10.1016/j.bjpt.2022.100469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Korthals-de Bos IB, Smidt N, van Tulder MW, et al. Cost effectiveness of interventions for lateral epicondylitis: results from a randomised controlled trial in primary care. Pharmacoeconomics. 2004;22:185–195. doi: 10.2165/00019053-200422030-00004. [DOI] [PubMed] [Google Scholar]
- 62.Korthals-de Bos IBC, Hoving JL, van Tulder MW, et al. Cost effectiveness of physiotherapy, manual therapy, and general practitioner care for neck pain: economic evaluation alongside a randomised controlled trial. BMJ (Clin Res Ed) 2003;326(7395):911. doi: 10.1136/bmj.326.7395.911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Leininger B, McDonough C, Evans R, Tosteson T, Tosteson AN, Bronfort G. Cost-effectiveness of spinal manipulative therapy, supervised exercise, and home exercise for older adults with chronic neck pain. Spine J. 2016;16(11):1292–1304. doi: 10.1016/j.spinee.2016.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Lewis M, James M, Stokes E, et al. An economic evaluation of three physiotherapy treatments for non-specific neck disorders alongside a randomized trial. Rheumatology (Oxford) 2007;46(11):1701–1708. doi: 10.1093/rheumatology/kem245. [DOI] [PubMed] [Google Scholar]
- 65.Lilje SC, Persson UB, Tangen ST, Kåsamoen S, Skillgate E. Costs and utilities of manual therapy and orthopedic standard care for low-prioritized orthopedic outpatients of working age: a cost consequence analysis. Clin J Pain. 2014;30(8):730–736. doi: 10.1097/AJP.0000000000000000. [DOI] [PubMed] [Google Scholar]
- 66.Lin C-WC, Moseley AM, Haas M, Refshauge KM, Herbert RD. Manual therapy in addition to physiotherapy does not improve clinical or economic outcomes after ankle fracture. J Rehabil Med. 2008;40(6):433–439. doi: 10.2340/16501977-0187. [DOI] [PubMed] [Google Scholar]
- 67.Manca A, Dumville JC, Torgerson DJ, et al. Randomized trial of two physiotherapy interventions for primary care back and neck pain patients: cost effectiveness analysis. Rheumatology (Oxford) 2007;46(9):1495–1501. doi: 10.1093/rheumatology/kem183. [DOI] [PubMed] [Google Scholar]
- 68.Manca A, Epstein DM, Torgerson DJ, et al. Randomized trial of a brief physiotherapy intervention compared with usual physiotherapy for neck pain patients: cost-effectiveness analysis. Int J Technol Assess Health Care. 2006;22(1):67–75. doi: 10.1017/S0266462306050859. [DOI] [PubMed] [Google Scholar]
- 69.McCarthy CJ, Mills PM, Pullen R, et al. Supplementation of a home-based exercise programme with a class-based programme for people with osteoarthritis of the knees: a randomised controlled trial and health economic analysis. Health Technol Assess. 2004;8(46):iii–iv, 1–61. doi: 10.3310/hta8460. [DOI] [PubMed] [Google Scholar]
- 70.Mitchell C, Walker J, Walters S, Morgan AB, Binns T, Mathers N. Costs and effectiveness of pre- and post-operative home physiotherapy for total knee replacement: randomized controlled trial. J Eval Clin Pract. 2005;11(3):283–292. doi: 10.1111/j.1365-2753.2005.00535.x. [DOI] [PubMed] [Google Scholar]
- 71.Müller G, Pfinder M, Clement M, et al. Therapeutic and economic effects of multimodal back exercise: a controlled multicentre study. J Rehabil Med. 2019;51(1):61–70. doi: 10.2340/16501977-2497. [DOI] [PubMed] [Google Scholar]
- 72.Niemistö L, Lahtinen-Suopanki T, Rissanen P, Lindgren K-A, Sarna S, Hurri H. A randomized trial of combined manipulation, stabilizing exercises, and physician consultation compared to physician consultation alone for chronic low back pain. Spine. 2003;28(19):2185–2191. doi: 10.1097/01.BRS.0000085096.62603.61. [DOI] [PubMed] [Google Scholar]
- 73.Niemistö L, Rissanen P, Sarna S, Lahtinen-Suopanki T, Lindgren K-A, Hurri H. Cost-effectiveness of combined manipulation, stabilizing exercises, and physician consultation compared to physician consultation alone for chronic low back pain: a prospective randomized trial with 2-year follow-up: LWW. Spine (Phila Pa 1976) 2005;28(19):2185–2191. doi: 10.1097/01.BRS.0000085096.62603.61. [DOI] [PubMed] [Google Scholar]
- 74.Pinto D, Robertson MC, Abbott JH, Hansen P, Campbell AJ. Manual therapy, exercise therapy, or both, in addition to usual care, for osteoarthritis of the hip or knee. 2: economic evaluation alongside a randomized controlled trial. Osteoarthr Cartil. 2013;21(10):1504–1513. doi: 10.1016/j.joca.2013.06.014. [DOI] [PubMed] [Google Scholar]
- 75.Pryymachenko Y, Wilson R, Sharma S, Pathak A, Abbott JH. Are manual therapy or booster sessions worthwhile in addition to exercise therapy for knee osteoarthritis: Economic evaluation and 2-year follow-up of a randomized controlled trial. Musculoskelet Sci Pract. 2021;56:102439. doi: 10.1016/j.msksp.2021.102439. [DOI] [PubMed] [Google Scholar]
- 76.Rhon DI, Kim M, Asche CV, Allison SC, Allen CS, Deyle GD. Cost-effectiveness of physical therapy vs intra-articular glucocorticoid injection for knee osteoarthritis: a secondary analysis from a randomized clinical trial. JAMA Netw Open. 2022;5(1):e2142709. doi: 10.1001/jamanetworkopen.2021.42709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Rivero-Arias O, Gray A, Frost H, Lamb SE, Stewart-Brown S. Cost-utility analysis of physiotherapy treatment compared with physiotherapy advice in low back pain. Spine (Phila Pa 1976) 2006;31(12):1381–1387. doi: 10.1097/01.brs.0000218486.13659.d5. [DOI] [PubMed] [Google Scholar]
- 78.Sevick MA, Bradham DD, Muender M, et al. Cost-effectiveness of aerobic and resistance exercise in seniors with knee osteoarthritis. Med Sci Sports Exerc. 2000;32(9):1534–1540. doi: 10.1097/00005768-200009000-00002. [DOI] [PubMed] [Google Scholar]
- 79.Sevick MA, Dunn AL, Morrow MS, Marcus BH, Chen GJ, Blair SN. Cost-effectiveness of lifestyle and structured exercise interventions in sedentary adults: results of project ACTIVE. Am J Prev Med. 2000;19(1):1–8. doi: 10.1016/S0749-3797(00)00154-9. [DOI] [PubMed] [Google Scholar]
- 80.Sevick MA, Miller GD, Loeser RF, Williamson JD, Messier SP. Cost-effectiveness of exercise and diet in overweight and obese adults with knee osteoarthritis. Med Sci Sports Exerc. 2009;41(6):1167–1174. doi: 10.1249/MSS.0b013e318197ece7. [DOI] [PubMed] [Google Scholar]
- 81.Skargren EI, Carlsson PG, Öberg BE. One-year follow-up comparison of the cost and effectiveness of chiropractic and physiotherapy as primary management for back pain: subgroup analysis, recurrence, and additional health care utilization. Spine. 1998;23(17):1875–1883. doi: 10.1097/00007632-199809010-00016. [DOI] [PubMed] [Google Scholar]
- 82.Skargren EI, Öberg BE, Carlsson PG, Gade M. Cost and effectiveness analysis of chiropractic and physiotherapy treatment for low back and neck pain: six-month follow-up. Spine. 1997;22(18):2167–2177. doi: 10.1097/00007632-199709150-00015. [DOI] [PubMed] [Google Scholar]
- 83.Smeets RJ, Severens JL, Beelen S, Vlaeyen JW, Knottnerus JA. More is not always better: cost-effectiveness analysis of combined, single behavioral and single physical rehabilitation programs for chronic low back pain. Eur J Pain. 2009;13(1):71–81. doi: 10.1016/j.ejpain.2008.02.008. [DOI] [PubMed] [Google Scholar]
- 84.Søgaard R, Bünger CE, Laurberg I, Christensen FB. Cost-effectiveness evaluation of an RCT in rehabilitation after lumbar spinal fusion: a low-cost, behavioural approach is cost-effective over individual exercise therapy. Eur Spine J. 2008;17(2):262–271. doi: 10.1007/s00586-007-0479-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Stan G, Orban H, Orban C. Cost effectiveness analysis of knee osteoarthritis treatment. Chirurgia (Bucur) 2015;110(4):368–374. [PubMed] [Google Scholar]
- 86.Struijs PA, Korthals-de Bos IB, van Tulder MW, van Dijk CN, Bouter LM, Assendelft WJ. Cost effectiveness of brace, physiotherapy, or both for treatment of tennis elbow. Br J Sports Med. 2006;40(7):637–643. doi: 10.1136/bjsm.2006.026187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Suni JH, Kolu P, Tokola K, et al. Effectiveness and cost-effectiveness of neuromuscular exercise and back care counseling in female healthcare workers with recurrent non-specific low back pain: a blinded four-arm randomized controlled trial. BMC Public Health. 2018;18(1):1376. doi: 10.1186/s12889-018-6293-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Tan SS, Teirlinck CH, Dekker J, et al. Cost-utility of exercise therapy in patients with hip osteoarthritis in primary care. Osteoarthr Cartil. 2016;24(4):581–588. doi: 10.1016/j.joca.2015.11.010. [DOI] [PubMed] [Google Scholar]
- 89.Tan SS, van Linschoten RL, van Middelkoop M, Koes BW, Bierma-Zeinstra SM, Koopmanschap MA. Cost-utility of exercise therapy in adolescents and young adults suffering from the patellofemoral pain syndrome. Scand J Med Sci Sports. 2010;20(4):568–579. doi: 10.1111/j.1600-0838.2009.00980.x. [DOI] [PubMed] [Google Scholar]
- 90.van de Graaf VA, van Dongen JM, Willigenburg NW, et al. How do the costs of physical therapy and arthroscopic partial meniscectomy compare? A trial-based economic evaluation of two treatments in patients with meniscal tears alongside the ESCAPE study. Br J Sports Med. 2020;54(9):538–545. doi: 10.1136/bjsports-2018-100065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.van den Hout WB, Jong Zd, Munneke M, Hazes JMW, Breedveld FC, Vliet Vlieland TPM. Cost-utility and cost-effectiveness analyses of a long-term, high-intensity exercise program compared with conventional physical therapy in patients with rheumatoid arthritis. Arthritis Rheum. 2005;53(1):39–47. doi: 10.1002/art.20903. [DOI] [PubMed] [Google Scholar]
- 92.van der Graaff SJ, Reijman M, Meuffels DE, Koopmanschap MA. Cost-effectiveness of arthroscopic partial meniscectomy versus physical therapy for traumatic meniscal tears in patients aged under 45 years. Bone Joint J. 2023;105(11):1177–1183. doi: 10.1302/0301-620X.105B11.BJJ-2023-0107.R1. [DOI] [PubMed] [Google Scholar]
- 93.van der Roer N, van Tulder M, van Mechelen W, de Vet H. Economic evaluation of an intensive group training protocol compared with usual care physiotherapy in patients with chronic low back pain. Spine. 2008;33(4):445–451. doi: 10.1097/BRS.0b013e318163fa59. [DOI] [PubMed] [Google Scholar]
- 94.van Dongen JM, Groeneweg R, Rubinstein SM, et al. Cost-effectiveness of manual therapy versus physiotherapy in patients with sub-acute and chronic neck pain: a randomised controlled trial. Eur Spine J. 2016;25(7):2087–2096. doi: 10.1007/s00586-016-4526-0. [DOI] [PubMed] [Google Scholar]
- 95.Whitehurst DG, Lewis M, Yao GL, et al. A brief pain management program compared with physical therapy for low back pain: results from an economic analysis alongside a randomized clinical trial. Arthritis Rheum. 2007;57(3):466–473. doi: 10.1002/art.22606. [DOI] [PubMed] [Google Scholar]
- 96.Niemistö L, Rissanen P, Sarna S, Lahtinen-Suopanki T, Lindgren KA, Hurri H. Cost-effectiveness of combined manipulation, stabilizing exercises, and physician consultation compared to physician consultation alone for chronic low back pain: a prospective randomized trial with 2-year follow-up. Spine (Phila Pa 1976) 2005;30(10):1109–1115. doi: 10.1097/01.brs.0000162569.00685.7b. [DOI] [PubMed] [Google Scholar]
- 97.Fernandes L, Roos EM, Overgaard S, Villadsen A, Søgaard R. Supervised neuromuscular exercise prior to hip and knee replacement: 12-month clinical effect and cost-utility analysis alongside a randomised controlled trial. BMC Musculoskelet Disord. 2017;18(1):5. doi: 10.1186/s12891-016-1369-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Brauer CA, Neumann PJ, Rosen AB. Trends in cost effectiveness analyses in orthopaedic surgery. Clin Orthop Relat Res®. 2007;457:42–48. doi: 10.1097/BLO.0b013e31803372c9. [DOI] [PubMed] [Google Scholar]
- 99.Jull G, Moore AP. Physiotherapy is not a treatment technique. Musculoskelet Sci Pract. 2021;56:102480. doi: 10.1016/j.msksp.2021.102480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Slade SC, Dionne CE, Underwood M, Buchbinder R. Consensus on exercise reporting template (CERT): explanation and elaboration statement. Br J Sports Med. 2016;50(23):1428–1437. doi: 10.1136/bjsports-2016-096651. [DOI] [PubMed] [Google Scholar]
- 101.Vreeman DJ, Taggard SL, Rhine MD, Worrell TW. Evidence for electronic health record systems in physical therapy. Phys Ther. 2006;86(3):434–446. doi: 10.1093/ptj/86.3.434. [DOI] [PubMed] [Google Scholar]
- 102.May S. Classification by McKenzie mechanical syndromes: a survey of McKenzie-trained faculty. J Manip Physiol Ther. 2006;29(8):637–642. doi: 10.1016/j.jmpt.2006.08.003. [DOI] [PubMed] [Google Scholar]
- 103.Andronis L, Kinghorn P, Qiao S, Whitehurst DG, Durrell S, McLeod H. Cost-effectiveness of non-invasive and non-pharmacological interventions for low back pain: a systematic literature review. Appl Health Econ Health Policy. 2017;15:173–201. doi: 10.1007/s40258-016-0268-8. [DOI] [PubMed] [Google Scholar]
- 104.Miyamoto GC, Lin C-WC, Cabral CMN, van Dongen JM, van Tulder MW. Cost-effectiveness of exercise therapy in the treatment of non-specific neck pain and low back pain: a systematic review with meta-analysis. Br J Sports Med. 2019;53(3):172–181. doi: 10.1136/bjsports-2017-098765. [DOI] [PubMed] [Google Scholar]
- 105.Pinto D, Robertson MC, Hansen P, Abbott JH. Cost-effectiveness of nonpharmacologic, nonsurgical interventions for hip and/or knee osteoarthritis: systematic review. Value Health. 2012;15(1):1–12. doi: 10.1016/j.jval.2011.09.003. [DOI] [PubMed] [Google Scholar]
- 106.Woods B, Manca A, Weatherly H, et al. Cost-effectiveness of adjunct non-pharmacological interventions for osteoarthritis of the knee. PLoS ONE. 2017;12(3):e0172749. doi: 10.1371/journal.pone.0172749. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. Details on the PubMed search.
Additional file 2. Overview of excluded full text articles.
Additional file 3. Evaluation of the study quality with the Consensus on Health Economic Criteria checklist.
Data Availability Statement
All data involved data in this article are available online through the original articles. Where there is uncertainty, the authors are happy to provide details on the analyses on request.