Abstract
Introduction
Night shift work could be a modifiable risk factor for prostate cancer. However, the epidemiological evidence is inconsistent. To summarize the existing evidence on this topic, we conducted a two-stage dose-response meta-analysis.
Methods
Medical librarians searched PubMed, EMBASE, and the Cochrane Library on December 30, 2022. Seven criteria were used to determine the inclusion of each study in the present analysis.
Results
Eleven cohort studies (12 cohort reports; total cases: 9366; and total person-years: 88,238,009) and seven case-control studies (seven case-control reports; total cases: 5593; and total controls: 6876) were included. This study estimated that the risk of prostate cancer increased by 1, 12, 24, and 39% after 1, 10, 20, and 30 years of night shift work exposure, respectively, according to four cohort and five case-control studies.
Discussion
Seven inclusion criteria were used to determine which studies were eligible for this analysis. Risk ratios from cohort studies and odds ratios from case-control studies were analyzed separately. However, all odds ratios from the case-control studies were excluded because of a high likelihood of publication bias. Moreover, exposure, measured in years of night shift work, was defined based on the information provided by individual studies. Finally, we utilized a recently reported two-stage dose-response meta-analysis method. This study provides evidence that night shift work contributes to the risk of prostate cancer in a dose-dependent manner.
Keywords: Night shift work, Prostate cancer, Two-stage dose-response meta-analysis, Light exposure at night, Cohort study, Case-control studies
1. Introduction
The relationship between night shift work and prostate cancer has been analyzed in previous meta-analyses. However, these findings were not definitive. In a meta-analysis study, Rivera-Izquierdo et al. reported a pooled risk ratio (RR) of 1.03 (95% confidence interval [CI] 0.96–1.10) from cohort studies and pooled odds ratio (OR) of 1.28 (95% CI 0.98–1.58) from case-control studies. In another meta-analysis study, Mancio et al. reported a pooled RR of 1.04 (95% CI 0.98–1.11) from cohort studies and a pooled OR of 1.18 (95% CI 1.02–1.36) from case-control studies. Xie et al. reported in their meta-analysis study a pooled RR of 1.05 (95% CI 1.00–1.10) from cohort studies and a pooled OR of 1.51 (95% CI 0.99–1.24) from case-control studies. Most meta-analyses reported an increased risk for the point estimate. However, the corresponding CI usually reported a statistically insignificant result.
Prior meta-analyses suggest that night shift workers experience higher rates of prostate cancer than daytime workers; however, these studies have some limitations. First, various definitions of night shift work were applied to the inclusion criteria. To overcome this limitation, we applied strict inclusion criteria. Second, the dose-response relationship was not investigated. A single risk estimate was extracted from each study to calculate a pooled risk estimate. However, the conventional meta-analysis method could not reveal a real-world relationship between hazardous exposure and health outcomes in occupational and environmental health studies. Third, ORs from case-control studies were pooled with RRs from cohort studies without appropriate conversion. We addressed the methodological shortcomings identified in previous meta-analyses by implementing rigorous inclusion criteria and adhering to stringent statistical principles throughout the analysis.
Although previous studies have not provided definitive evidence, the underlying biological rationale linking night shift work (or exposure to light at night) to cancer remains relatively consistent. The International Agency for Research on Cancer (IARC) has classified night shift work as a Group 2A carcinogen, indicating a probable link to cancer development [1]. Based on an extensive body of cancer epidemiology and mechanistic studies in humans, the National Toxicology Program (NTP) has determined that there is abundant evidence supporting the carcinogenicity of exposure to night shift work (or light at night) and its association with cancer [2]. Numerous studies have provided substantial evidence for the biological basis of this association [3]. These include (i) circadian disruption and phase alteration caused by light exposure at night, leading to various internal/cellular environments that favor carcinogenesis; (ii) faulty cell division and DNA repair induced by night shift work; (iii) melatonin suppression caused by night shift work; and (iv) sleep deprivation in night shift workers, which compromises immune surveillance and leads to metabolic disarrangement. Moreover, many studies investigating the association between light exposure at night and prostate cancer have supported a positive link between night shift work and prostate cancer. This is attributed to the significant similarities in the underlying biological mechanisms of these two areas of inquiry [[4], [5], [6]].
The primary objective of this study was to examine the potential link between night shift work exposure and an elevated risk of prostate cancer. To test this association, we conducted a comprehensive two-stage dose-response meta-analysis. Additionally, particular attention was paid to defining the exposure dose for each risk estimate based on the information extracted from the original articles. To estimate the dose-response relationship, a novel two-stage dose-response meta-analysis methodology was employed [7,8]. The findings of this study build on previous literature by addressing the weaknesses of prior meta-analyses.
2. Methods
2.1. Literature search
A literature search was conducted by a medical librarian at the Medical Library of Inha University, Incheon, South Korea. The medical librarian searched PubMed, EMBASE, and the Cochrane Library databases on December 30, 2022.
2.2. Inclusion criteria and selection of articles
The inclusion criteria were: (i) Articles dealing with the relationship between night shift work and prostate cancer. (ⅱ) The exposure of interest, night shift work, should be stated clearly in the text. Articles dealing with work experience in jobs that could be associated with night shift work without a clear statement of night shift work as the exposure of interest were excluded. However, studies that considered night shift work as a categorical or continuous variable were included. Articles in which the exposure of interest was light exposure at night, disturbance of the sleep-wake cycle, or melatonin level were excluded. Night shift work should be considered an occupational exposure. (ⅲ) Only studies that featured quantitative analyses were included, where results were provided as a risk ratio or OR in cohort or case-control studies, respectively. Hazard ratios (HR) from the survival analyses were interpreted as RRs based on previous studies [[9], [10], [11]]. (ⅳ) Only studies published in English were included in this analysis. (ⅴ) Studies involving human (not animal) participants were included. (ⅵ) For the article type, only original articles were included. However, if all other criteria were met, letters to the editor were included after careful examination. Abstracts were excluded because of the possibility of inaccuracy and duplication of data with other official publications. (ⅶ) Several articles were included after screening and reviewing the bibliographies of essential articles.
JM and YM conducted the article selection process separately and compared the results to determine the final set of articles for inclusion. Disagreements between the two authors were resolved through discussions.
2.3. Quality assessment of each included study
The quality of all included studies was assessed based on the NTP Office of Health Assessment and Translation (OHAT) risk of bias (RoB) tool [12]. The biases and corresponding questions in the NTP OHAT RoB tool are provided in Supplementary Material A. Each study was rated separately by each author. To investigate the quality of each study in more detail, selection bias, exposure assessment, outcome classification, and confounding factors were assessed. Based on these results, the authors summarized the stages of prostate cancer, adjusted confounders, and overall reliability for each study.
2.4. Data extraction
Risk estimates from each study were extracted to construct the dose-response meta-analysis dataset. To assess the dose-response relationship, the authors extracted the risk estimates for each category of years of night shift work from each study. Several studies lacked information on the duration of night shift work. They classified exposure as rotating night shift work versus daytime work. In these studies, the authors extracted relevant information from the main texts or directly calculated the duration of night shift work from the numbers (person-years divided by the number of persons) provided in the main texts.
2.5. Examination of publication bias
Publication bias was assessed by examining Begg's funnel plot for asymmetry and using Egger's regression test. Egger's regression test uses the precision and standardized effect size of the effect estimate from a study as independent and dependent variables, respectively [13]. If Egger's regression test showed a statistically significant result, publication bias was suspected. The statistically significant p-value for publication bias was set at 0.05.
For Egger's regression test, only one representative effect estimate was required for each study. Therefore, we separately applied the same two-stage dose-response meta-analysis method to each included study [7,8]. Next, we calculated the RR or OR of prostate cancer for each year of night shift work in each study. These RRs or ORs and the calculated variances were used to conduct Egger's regression test.
2.6. Primarymeta-analysis and dose-response meta-analysis
To investigate the dose-response relationship between years of night shift work (exposure dose) and incidence of prostate cancer (response), we conducted a two-stage dose-response meta-analysis [7,8]. A two-stage dose-response meta-analysis involves obtaining a regression coefficient for each included study in the first stage and calculating a pooled regression coefficient in the second stage using the regression coefficients obtained in the first stage. For the estimation method, the restricted maximum likelihood model was applied. The method proposed by Greenland and Longnecker was used for covariance approximation [14]. The statistically significant p-value for the main meta-analysis was set at 0.05. A two-stage dose-response meta-analysis was conducted for cohort and case-control studies and a part of both studies, which were rated as reliable in the quality assessment of each study. To convert ORs obtained from case-control studies into relative risks, we applied a method suggested in the literature [15]. Equations (1), (2)) provide the conversion equation and calculation method for person-years for each case-control study.
| (1) |
| (2) |
2.7. Statistical software
All statistical analyses were conducted using R software version 4.2.2 (The R Foundation, Vienna, Austria). For the conventional meta-analysis, the R package “meta” was used [16]. The R package “dosresmeta” was used for the dose-response meta-analysis [14].
3. Results
3.1. Literature search and screening
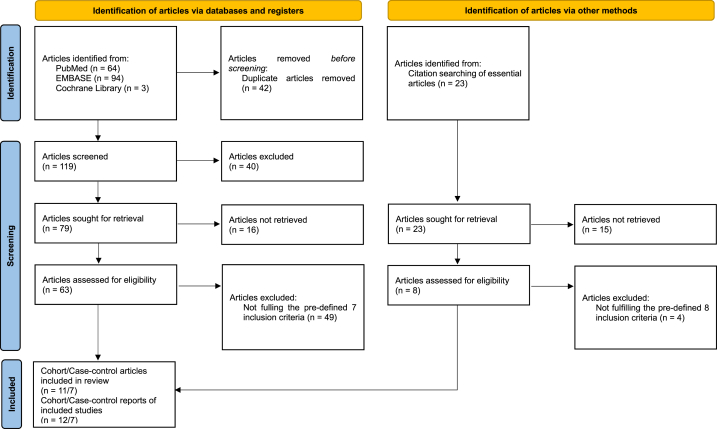
Search terms and syntax used are provided in Supplementary Material B. Search results in each of the three databases are provided in Supplementary Material C. Fig. 1 provides the PRISMA flow diagram with the grey literature. A total of 64 articles were identified from PubMed. In EMBASE, 94 articles were identified. Three articles were retrieved from the Cochrane Library. Of these 161 articles, 42 duplicate articles were excluded, leaving 119. The titles and abstracts of the remaining 119 articles were analyzed. Of these, 40 articles were excluded, leaving 79 articles of which each original text was examined. After this step, 16 articles were excluded, leaving 63 articles. After applying the previously defined inclusion criteria, 14 articles were included in the meta-analysis. The authors also examined the bibliographies of several essential articles. For these 23 articles, each original text was attached and examined. During this process, 15 articles were excluded, and eight articles remained. Among these eight articles, four were excluded based on the inclusion criteria, and four were included in the meta-analysis. After this selection process, 11 cohort study articles and seven case-control study articles remained. In these 18 articles, 12 cohort study reports and seven case-control study reports were included.
Fig. 1.
PRISMA flow diagram with grey literature [17].
3.2. Characteristics of included articles
Table 1 presents the characteristics of the 11 cohort studies (12 reports). The total number of cases and person-years were 9366 and 88,238,009, respectively. The first report was the Screening Across the Lifespan Twin (SALT) study. For 1–5, 6–10, 11–20, and 21–45 years of night shift work exposure, compared with 0 years of shift work, the RRs for prostate cancer were 1.02, 1.97, 0.88, and 1.05, respectively. The second report was the Heinz Nixdorf Recall Cohort Study (HNR) conducted in the Ruhr area of Germany. For 1–10, 10–20, and >20 years of night shift work exposure, compared with 0–1 years of night shift work, the RRs of prostate cancer were 1.72, 1.68, and 3.76, respectively. The third report was the Cancer Prevention Study–II. For the rotating shift work exposure categories, the RR of prostate cancer was 1.13, compared with fixed-day work. The fourth report was the healthcare database of a Japanese corporation manufacturing innovative products based on chemistry and material sciences. The RR of developing prostate cancer in shift workers was 1.79, compared with that in day shift workers. The fifth report was the Japan Collaborative Cohort study. For rotating shift work exposure, compared with daytime work, the RR for prostate cancer was 3. The sixth report was from the Whole Swedish working population study. For shift work exposure, compared with no shift work, the RR for prostate cancer was 1.04. The seventh report was a retrospective cohort study conducted in a German chemical company. For rotating shift workers compared with day workers, the RR for prostate cancer was 0.93. The eighth report was from the Norwegian Offshore Petroleum Workers cohort. For 0–3, 3–9, 9–16, 16–19.5, and 19.5–33.3 years of night shift work exposure, compared with 0 years of night shift work exposure, the RR for prostate cancer was 1.18, 1.19, 1.38, 1.92, and 1.9, respectively. The ninth report was the Alberta's Tomorrow Project cohort. For 0.1–5.9 and ≥ 6 years of night shift work exposure, compared with 0 years of night shift exposure, the RR was 0.86 and 0.88, respectively. The tenth report was the Older Finnish Twin cohort study. This study did not find a difference in the relative risk of prostate cancer based on exposure to rotating shift work. The eleventh report was on the male production worker cohort at BASF SE, Ludwigshafen. For shift workers, compared with day workers, the RR for prostate cancer was 1.37. The twelfth report was the same as the eleventh report. For daytime and shift workers' exposure categories, the RR point estimates were 1 and 1.37, respectively.
Table 1.
Characteristics of cohort studies.
| Authors | Report distinction | Study name | Years of night shift work (range) | Years of night shift work (point dose) | Prostate cancer cases (total cases: 9366) | Person-years (total person-years: 88,238,009) | Risk ratio and 95% confidence interval |
|---|---|---|---|---|---|---|---|
| Akerstedt et al. (2012) [18] | 1 | Screening Across the Lifespan Twin (SALT) study | 0 | 0 | 225 | 1957.5 | 1 |
| 1–5 | 2.5 | 42 | 365.4 | 1.02 (0.48–2.18) | |||
| 6–10 | 7.5 | 19 | 165.3 | 1.97 (0.64–6.02) | |||
| 11–20 | 15 | 22 | 191.4 | 0.88 (0.32–2.43) | |||
| 21–45 | 32.5 | 24 | 208.8 | 1.05 (0.39–2.84) | |||
| Behrens et al. (2017) [19] | 2 | Heinz Nixdorf Recall Cohort Study (HNR) from the Ruhr area in Germany | 0–1 | 0.5 | 44 | 13,511 | 1 |
| 1–10 | 5.5 | 11 | 2089 | 1.72 (0.88–3.35) | |||
| 10–20 | 15 | 5 | 1031 | 1.68 (0.66–4.26) | |||
| >20 | 25 | 16 | 1606 | 3.76 (2.04–6.93) | |||
| Gapstur et al. (2014) [20] | 3 | Cancer Prevention Study–II | Fixed day work | 0 | 4497 | 6,465,182 | 1 |
| Rotating shift work | 23.31 | 268 | 422,487 | 1.13 (1–1.28) | |||
| Kubo et al. (2011) [21] | 4 | Health-care database of a Japanese corporation manufacturing innovative products based on chemistry and material sciences | Day time work | 0 | 13 | 93363.2 | 1 |
| Shift work | 25.3 | 4 | 21998.2 | 1.79 (0.57–5.68) | |||
| Kubo et al. (2006) [22] | 5 | Japan Collaborative Cohort study | Daytime work | 0 | 21 | 89,179 | 1 |
| Rotating shift work | 8.06 | 7 | 14,523 | 3 (1.2–7.7) | |||
| Schwartzbaum et al. (2007) [23] | 6 | Whole Swedish working population study | No shift work | 0 | 1267 | 39,940,394 | 1 |
| Shift work | 19 | 1319 | 39,940,394 | 1.04 (0.99–1.1) | |||
| Yong et al. (2014) [24] | 7 | Retrospective cohort in a German chemical company | Day worker | 0 | 191 | 152,190 | 1 |
| Rotating shift worker | 25 | 146 | 126,090 | 0.93 (0.71–1.21) | |||
| Berge et al. (2022) [25] | 8 | Norwegian Offshore Petroleum Workers (NOPW) cohort | 0 | 0 | 117 | 20410.65 | 1 |
| 0–3 | 1.5 | 41 | 5950.03 | 1.18 (0.83–1.69) | |||
| 3–9 | 6 | 48 | 5958.95 | 1.19 (0.86–1.66) | |||
| 9–16 | 12.5 | 46 | 3397.82 | 1.38 (0.97–1.95) | |||
| 16–19.5 | 17.75 | 15 | 578.6 | 1.92 (1.09–3.37) | |||
| 19.5–33.3 | 26.4 | 9 | 343.46 | 1.9 (0.92–3.95) | |||
| McNeil et al. (2020) [26] | 9 | Alberta's Tomorrow Project cohort | 0 | 0 | 165 | 41,558 | 1 |
| 0.1–5.9 | 3 | 89 | 28324.2 | 0.86 (0.66–1.12) | |||
| ≥6 | 9 | 67 | 20320.6 | 0.88 (0.66–1.17) | |||
| Dickerman et al. (2016) [27] | 10 | Older Finnish Twin cohort | No shift work | 0 | 509 | 237,642 | 1 |
| Rotating shift work | 26.24 | 80 | 46,463 | 1 (0.7–1.2) | |||
| Hammer et al. (2015): stage 4 [28] | 11 | Male production workers cohort at BASF SE, Ludwigshafen | Daytime workers | 0 | 5 | 147,892 | 1 |
| Shift workers | 9.69 | 3 | 122,176 | 1.37 (0.25–6.19) | |||
| Hammer et al. (2015): stage X [28] | 12 | Male production workers cohort at BASF SE, Ludwigshafen | Daytime workers | 0 | 14 | 147,892 | 1 |
| Shift workers | 9.69 | 17 | 122,176 | 1.37 (0.61–3.1) |
Table 2 shows the characteristics of the included case-control studies (seven reports). The total cases, controls, and participants were 5,593, 6,876, and 12,469, respectively. The first report was the Prostate Cancer and Environment Study. For 0–4, 4–11, 11–21, and >21 years of night shift work exposure compared with 0 years of night shift work, the RRs for prostate cancer were 0.9, 1.04, 1.1, and 1.19, respectively. The second report was the 25-page mailed questionnaire study in Ontario, Canada. For 0–7, 7–22, 22–34, and >34 years of night shift work exposure, compared with 0 years of night shift work exposure, the RRs for prostate cancer were 1.44, 1.14, 0.93, and 1.3, respectively. The third report was the MCC-Spain study. For 0–10, 10–28, and >28 years of night shift work exposure, compared with 0 years of night shift work exposure, the RRs were 1.1, 0.94, and 1.38, respectively. The fourth report was the Montreal Multisite Case-Control Cancer Study. For 0–5, 5–10, and >10 years of night shift work exposure, compared with 0 years of night shift work exposure, the RRs were 3.13, 2.11, and 2.68, respectively. The fifth report was the Hong Kong prostate cancer case-control study. Participants who reported ever working night shift work, compared with those who reported never working night shift work, had an RR for prostate cancer of 1.76. The sixth report was the CAPLIFE study. For 0–7, 7–26, and >26 years of night shift work exposure, compared with 0 years of night shift work exposure, the RRs were 1.33, 1.93, and 1.18, respectively. The seventh report was the Epidemiology of Prostate Cancer (EPICAP) study. For 0–10, 10–20, 20–30, and >30 years of night shift work exposure, compared with 0 years of night shift work, the RRs were 1.31, 1.47, 1.07, and 2.49, respectively.
Table 2.
Characteristics of case-control studies.
| Authors | Report distinction | Study name | Years of night shift work (range) | Years of night shift work (point dose) | Cases (total cases: 5593) | Controls (total controls: 6876) | Total participants (total: 12,469) | Odds ratio and 95% confidence interval |
|---|---|---|---|---|---|---|---|---|
| Barul et al. (2019) [29] | 1 | Prostate Cancer and Environment study | 0 | 0 | 1642 | 1718 | 3360 | 1 |
| 0–4 | 2 | 59 | 67 | 126 | 0.9 (0.63–1.27) | |||
| 4–11 | 7.5 | 67 | 63 | 130 | 1.04 (0.72–1.5) | |||
| 11–21 | 16 | 56 | 46 | 102 | 1.1 (0.74–1.64) | |||
| >21 | 26 | 68 | 57 | 125 | 1.19 (0.83–1.72) | |||
| Conlon et al. (2007) [30] | 2 | 25-page mailed questionnaire study in Ontario, Canada | 0 | 0 | 391 | 909 | 1300 | 1 |
| 0–7 | 3.5 | 115 | 185 | 300 | 1.44 (1.1–1.87) | |||
| 7–22 | 14.5 | 87 | 179 | 266 | 1.14 (0.86–1.52) | |||
| 22–34 | 28 | 81 | 205 | 286 | 0.93 (0.7–1.23) | |||
| >34 | 40 | 86 | 154 | 240 | 1.3 (0.97–1.74) | |||
| Papantoniou et al. (2015) [31] | 3 | MCC-Spain study | 0 | 0 | 733 | 948 | 1681 | 1 |
| 0–10 | 5 | 128 | 145 | 273 | 1.1 (0.83–1.45) | |||
| 10–28 | 19 | 92 | 130 | 222 | 0.94 (0.69–1.27) | |||
| >28 | 37 | 138 | 128 | 266 | 1.38 (1.05–1.81) | |||
| Parent et al. (2012) [32] | 4 | Montreal Multisite Case-Control Cancer study | 0 | 0 | 268 | 438 | 706 | 1 |
| 0–5 | 2.5 | 68 | 36 | 104 | 3.13 (1.98–4.95) | |||
| 5–10 | 7.5 | 27 | 19 | 46 | 2.11 (1.11–3.99) | |||
| >10 | 12.5 | 36 | 19 | 55 | 2.68 (1.45–4.95) | |||
| Tse et al. (2017) [33] | 5 | Hong Kong prostate cancer case-control study | Night shift work: never | 0 | 366 | 372 | 738 | 1 |
| Night shift work: ever | 10 | 58 | 30 | 88 | 1.76 (1.07–2.89) | |||
| Lozano-Lorca et al. (2020) [34] | 6 | CAPLIFE study | 0 | 0 | 344 | 368 | 712 | 1 |
| 0–7 | 3.5 | 29 | 23 | 52 | 1.33 (0.75–2.38) | |||
| 7–26 | 16.5 | 40 | 22 | 62 | 1.93 (1.11–3.36) | |||
| >26 | 35.5 | 28 | 21 | 49 | 1.18 (0.65–2.14) | |||
| Wendeu-Foyet et al. (2018): >10 h [35] | 7 | Epidemiology of Prostate Cancer (EPICAP) study | 0 | 0 | 532 | 556 | 1088 | 1 |
| 0–10 | 5 | 13 | 11 | 24 | 1.31 (0.57–3.01) | |||
| 10–20 | 15 | 11 | 8 | 19 | 1.47 (0.58–3.74) | |||
| 20–30 | 25 | 10 | 10 | 20 | 1.07 (0.43–2.66) | |||
| >30 | 35 | 20 | 9 | 29 | 2.49 (1.11–5.61) |
Supplementary Material D provides information sources for the duration of night shift work in studies in which workers were classified as rotating night shift workers versus daytime workers.
3.3. Quality assessment of each included study
The risk of bias, rated separately by each author, is provided in Supplementary Materials E and F. In general, the ratings by the first author (J.M.) were stricter than those by the second author (Y.M.). In other words, the first author rated the risk of bias for questions 1 and 3 (selection bias), 5 (performance bias), 8 (detection bias), and 11 (other biases) higher than the second author.
To investigate the quality of each study in more detail, we assessed the quality based on selection bias, exposure assessment, outcome classification, and confounding factors. The assessment results are provided in Supplementary Material G. Based on these results, the stages of prostate cancer, adjusted confounders, and overall reliability for each study are summarized (Supplementary Material H). Four cohort and five case-control studies were found to be reliable.
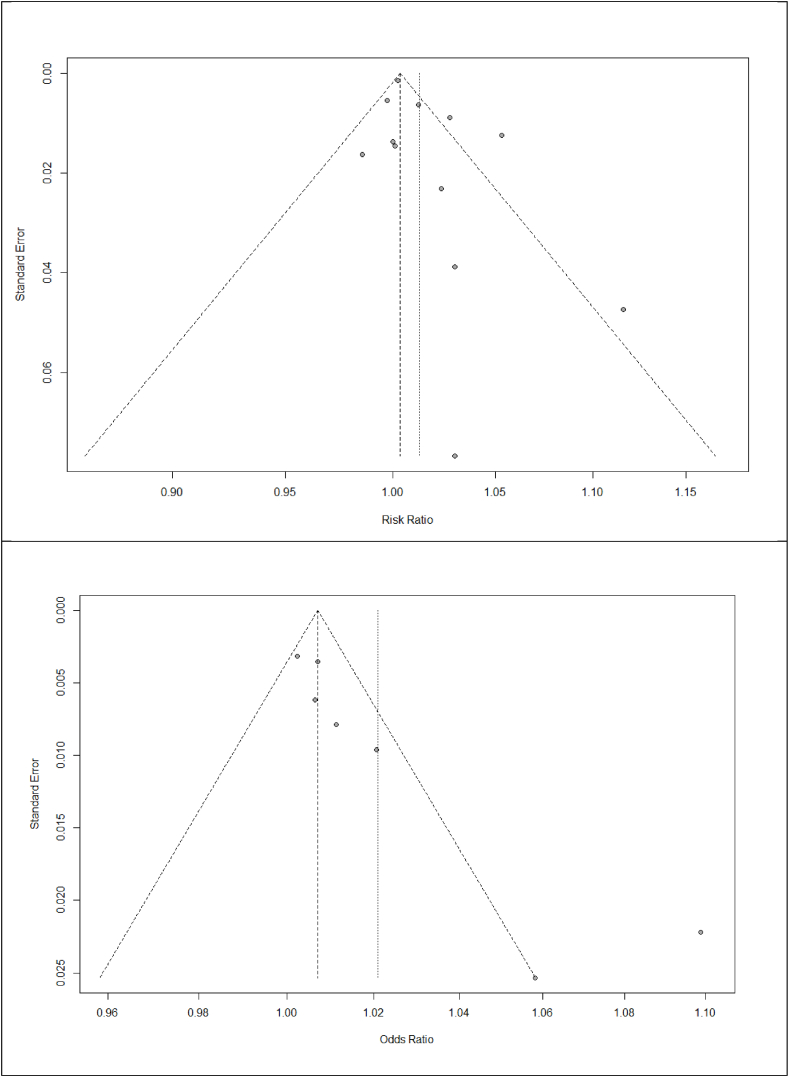
3.4. Publication bias
Fig. 2 shows Begg's funnel plots for the cohort and case-control studies. Supplementary Material I provides the representative RRs and ORs calculated in each study using the same dose-response meta-analysis method used in this study. Egger's regression test results for cohort and case-control studies showed a p-value of 0.08 and 0.01, respectively.
Fig. 2.
Begg's funnel plot for cohort and case-control studies.
Based on the asymmetry observed in Begg's funnel plot and the statistically significant Egger's regression test result (p = 0.01), the estimates from the case-control studies were unreliable owing to publication bias. Supplementary Material J provides the R code and Egger's regression test results for cohort and case-control studies.
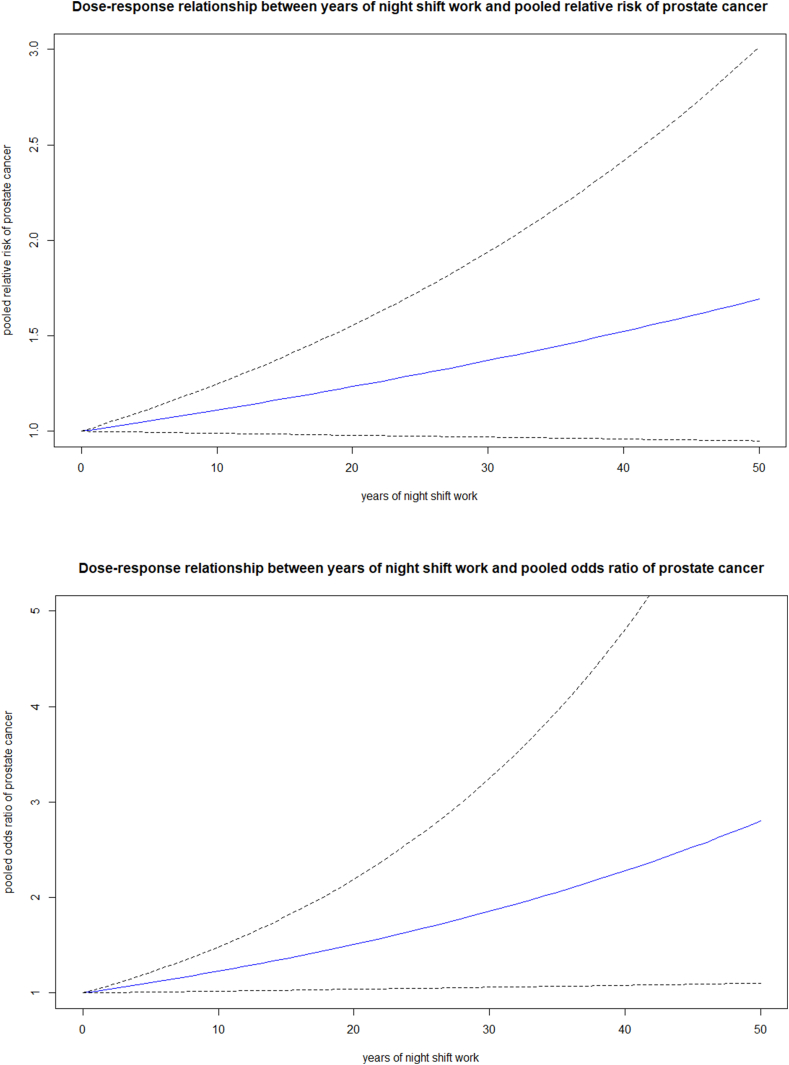
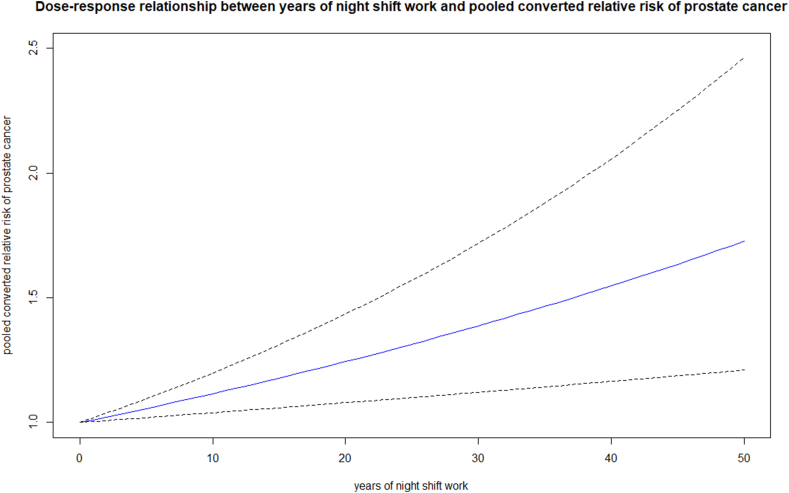
3.5. Dose-response meta-analysis
For the conversion of ORs to relative risks, P0 was calculated as 0.029. The average number of years of follow-up for the non-exposed groups in the cohort studies was calculated to be 14.08. Details of the calculations are provided in Supplementary Material K.
Table 3 shows the results of the dose-response meta-analysis. First, the dose-response meta-analysis model for cohort studies was statistically insignificant, with a p-value of 0.07. The pooled RR of prostate cancer for 1, 10, 20, and 30 years of night shift work exposure, compared with 0 years of exposure, were 1.01 (95% CI 1.00–1.02), 1.11 (95% CI 0.99–1.25), 1.2341 (95% CI 0.98–1.55), and 1.37 (95% CI 0.97–1.94), respectively. Second, the dose-response meta-analysis model for case-control studies was statistically significant, with a p-value of 0.0305. The pooled RR of prostate cancer for 1, 10, 20, and 30 years of night shift work exposure was 1.02 (95% CI 1.00–1.04), 1.23 (95% CI 1.08–1.48), 1.51 (95% CI 1.04–2.19), and 1.86 (95% CI 1.06–3.25), respectively. Third, the dose-response meta-analysis model for only reliable cohort and case-control studies (Supplementary Material H) (each OR converted into a relative risk) was statistically significant, with a p-value of 0.00. The pooled RRs of prostate cancer for 1, 10, 20, and 30 years of night shift work exposure were 1.01 (95% CI 1.00–1.02), 1.12 (95% CI 1.04–1.20), 1.24 (95% CI 1.08–1.43), and 1.39 (95% CI 1.12–1.72), respectively.
Table 3.
Results of a dose-response meta-analysis.
| Years of night shift work |
||||
|---|---|---|---|---|
| 1 year |
10 years |
20 years |
30 years |
|
| Pooled risk ratios and pooled odds ratios for prostate cancer (95% confidence interval) | ||||
| Cohort studies | 1.01 (1.00–1.02) | 1.11 (0.99–1.25) | 1.23 (0.98–1.55) | 1.37 (0.97–1.94) |
| Case-control studies | 1.02 (1.00–1.04) | 1.23 (1.02–1.48) | 1.51 (1.04–2.19) | 1.86 (1.06–3.25) |
| Combined (only reliable studiesa) | 1.01 (1.00–1.02) | 1.12 (1.04–1.20) | 1.24 (1.08–1.43) | 1.39 (1.12–1.72) |
Four cohort and five case-control studies provided in Supplementary material H.
Fig. 3 provides a dose-response meta-analysis plot for cohort studies, case-control studies, and reliable studies (combined).
Fig. 3.
Dose-response relationship between years of night shift work and pooled relative risks/pooled odds ratios of prostate cancer.
4. Discussion
This two-stage dose-response meta-analysis included 11 cohort studies (12 cohort reports) and seven case-control studies. This study estimated the risk of prostate cancer increased by 1, 12, 24, and 39% after 1, 10, 20, and 30 years of night shift work exposure, respectively, according to reliable four cohort and five case-control studies.
4.1. Source of heterogeneity and reliability of each study
We analyzed the source of heterogeneity in each study based on selection bias, exposure assessment, outcome classification, and confounding factors (Supplementary Material G). Specifically, two studies used male twin pairs to study the effects of night shift work (selection bias) [27,36]. Several studies assessed exposure to night shift work in more detail, whereas others classified ever/never night shift work. For outcome classification, most studies used all prostate cancer cases regardless of their stage. However, three cohort reports (from two cohort studies) used only aggressive stages [28,37]. In addition, one cohort study used mortality due to prostate cancer as the outcome instead of the incidence [38]. Four cohort and two case-control studies were adjusted for only a few potential confounders [28,[39], [40], [41], [42], [43]]. This might have caused a bias in estimating the risk of night shift work. Supplementary Material H summarizes the prostate cancer stages, adjusted confounders, and overall reliability of each study.
4.2. Review of previous main studies
Several systematic reviews and meta-analyses have investigated the relationship between night shift work and prostate cancer. Rivera-Izquierdo et al. published a systematic review and meta-analysis of the association between night shift work and prostate cancer in 2020 [44]. In this study, the pooled RR for cohort studies was 1.03 (95% CI 0.96–1.10), and the pooled OR for case-control studies was 1.28 (95% CI 0.98–1.58). The pooled estimates are not statistically significant. In addition, we calculated a pooled effect estimate based on the RRs and ORs from individual studies without using an appropriate conversion method that incorporated prevalence in the non-exposed group (from RRs to ORs or from ORs to RRs). This approach could result in bias because ORs must be converted into RRs using prevalence among non-exposed individuals [15]. Furthermore, this study considered night shift work as a binary exposure and did not consider the dose-response relationship between years of night shift work and the risk of prostate cancer.
Mancio et al. published a systematic review and meta-analysis on the relationship between shift work and prostate cancer in 2018 [45]. In the study, the pooled RR for cohort studies was 1.04 (95% CI 0.98–1.11), and the pooled OR for case-control studies was 1.18 (95% CI 1.02–1.36). This study also calculated a pooled effect estimate based on the RRs and ORs from individual studies without appropriate conversion using the prevalence in the non-exposed group (from RRs to ORs or from ORs to RRs). Furthermore, this study treated night shift work as a binary exposure and did not consider a dose-response relationship between years of night shift work and the risk of prostate cancer.
Xie et al. published a systematic review and meta-analysis of the relationship between shift work and prostate cancer in 2015, including assessing a dose-response relationship [46]. In this study, the pooled RR from cohort studies was 1.05 (95% CI 1.00–1.10), and the pooled OR from case-control studies was 1.51 (95% CI 0.99–1.24). This study also calculated a pooled effect estimate based on the RRs and ORs from individual studies without appropriate conversion using the prevalence in the non-exposed group (from RRs to ORs or from ORs to RRs). In assessing a dose-response relationship based on three case-control studies, an increase of 5 years in night shift work was associated with a 2.8% (95% CI 0.3%–5.4%) increase in pooled OR for prostate cancer. One strength of our study is the application of a more advanced dose-response meta-analysis method to cohort and case-control studies. Furthermore, our study converted the ORs reported in case-control studies into RRs using prevalence in the non-exposed group [15]. Our study also conducted the same dose-response meta-analysis using the RRs reported from cohort studies and converted RRs from the ORs of case-control studies.
4.3. Biological background for the carcinogenicity of night shift work
IARC has categorized night shift work as a Group 2A carcinogen, indicating limited evidence of its carcinogenicity in humans, sufficient evidence in experimental animals, and strong evidence that it exhibits the key characteristics of carcinogens [1]. Several potential mechanistic connections between night shift work and prostate cancer have been identified. In a 2013 review article, Haus and Smolensky summarized four biological mechanisms of carcinogenesis in night shift workers [3]. These include (ⅰ) circadian disruption and phase alteration caused by light exposure at night, leading to various internal/cellular environments that favor carcinogenesis, including epigenetic modifications, (ⅱ) faulty cell division and DNA repair induced by night shift work, which can result in malignant potential, (ⅲ) melatonin suppression caused by night shift work, affecting important functions such as neutralizing free radicals, inhibiting the uptake of free acids in potential tumor cells, and regulating testosterone metabolism, (ⅳ) sleep deprivation in night shift workers, which compromises immune surveillance and leads to metabolic disarrangement. Metabolic disarrangement is associated with obesity, a low-grade inflammatory state, and the generation of reactive oxygen species, all of which increase the risk of carcinogenesis. The NTP has concluded that there is sufficient evidence linking night shift work to the carcinogenicity of prostate cancer based on a comprehensive body of cancer epidemiology and mechanistic studies in humans. Animal studies have demonstrated the biological effects associated with circadian disruption or characteristics of carcinogens, providing a connection between exposure, intermediate biological effects, and cancer [2].
4.4. Association between light-at-night exposure and prostate cancer incidence
Kim et al. published a study on the association between artificial light at night (ALAN) and prostate cancer in Gwangju, South Korea [4]. In the Poisson regression analysis, exposure to ALAN was significantly associated with the incidence of prostate cancer (RR, 1.0231; p = 0.0369). In addition, when the incidence of prostate cancer at the 75% level of ALAN was compared with that at the 25% level of ALAN, the RR was 1.726 (12.6 over 7.3). This indicates a meaningful relationship between ALAN exposure and prostate cancer.
Garcia-Saenz et al. conducted a case-control study on the association between ALAN exposure and prostate cancer [5]. In this study, exposure to outdoor ALAN in the blue light spectrum was associated with increased odds of breast cancer (adjusted OR [aOR] for highest vs. lowest tertile, aOR = 1.47, 95% CI 1.00–2.17) and prostate cancer (aOR = 2.05, 95% CI 1.38–3.03). In addition, compared with those who reported sleeping in total darkness, men who slept in “quite illuminated” bedrooms had a higher risk of prostate cancer (aOR = 2.79, 95% CI 1.55–5.04). These results indicate a statistically significant relationship between ALAN exposure and prostate cancer.
Rybnikova et al. published a study on the association between ALAN exposure and the risk of prostate cancer [6]. Using three separate data sources, this study investigated this association in 180 countries. The linear regression coefficient was marginally statistically significant when the 2012 ASIR prostate cancer data were used (p < 0.1). This coefficient was more statistically significant when only 110 countries with well-maintained cancer registries were analyzed (p < 0.01).
Pukkala et al. reported that the breast cancer risk in women decreased with the degree of visual impairment, and a similar but less consistent trend was observed for prostate cancer in men [47].
In 1998, Feychting et al. reported that people with blindness had a lower incidence of all cancers combined (standardized incidence ratio of 0.69, 95% CI 0.59–0.82) [48]. Risk reduction is prominent in hormone-dependent tumors, including breast and prostate cancers.
However, several studies have suggested no statistically significant association between ALAN exposure and prostate cancer. Chowdhury-Paulino et al. reported no association between the interquartile range increase in cumulative light exposure at night and total and fatal prostate cancer incidence [49].
4.5. Examination of publication bias in a two-stage dose-response meta-analysis
In this study, we performed Egger's regression test utilizing representative RRs or ORs obtained by applying an identical two-stage dose-response meta-analysis method to the effect estimates derived from each study separately. This unique method warrants further in-depth discussion in terms of its methodology. We intend to publish a separate methodology paper with diverse examples, including those utilized in this study, to elaborate on this approach.
4.6. Meaning of this study
To date, literature and meta-analyses have presented conflicting findings regarding the association between exposure to night shift work and the incidence of prostate cancer. This inconsistency can be attributed to various factors: (i) the lack of stringent and transparent application of inclusion criteria in meta-analyses; (ii) misconceptions regarding the distinctions between effect estimates derived from different study designs (e.g., RRs from cohort studies and ORs from case-control studies); (iii) inaccurate assessment of exposure in original studies or the utilization of imprecise exposure doses in meta-analyses; and (iv) the use of rudimentary evidence synthesis methods to explore the dose-response relationship. Conversely, in this study, (ⅰ) a strict application of seven transparent inclusion criteria was implemented, and (ⅱ) a comprehensive separation was made between RRs from cohort studies and ORs from case-control studies, with each type of pooled effect estimate synthesized separately. However, case-control studies were excluded from the present analysis because of the high likelihood of publication bias (as determined by the statistically significant result from Egger's regression test). Additionally, (ⅲ) the exposure dose (years of night shift work) was precisely defined in the evidence synthesis based on the years of night shift work reported in individual studies. Finally, (ⅳ) the authors employed a novel two-stage dose-response meta-analysis method recently reported in the literature [7,8]. Consequently, this study provides the most comprehensive evidence on the relationship between the risk of prostate cancer and years of exposure to night shift work.
4.7. Limitations
This study had several limitations. First, more valid and reliable observational studies are required to calculate reliable pooled risk estimates. We classified each study as reliable based on the selection, exposure, outcome, and confounding factors. Several studies have demonstrated the possibility of design bias. Second, the biological background of the induction of prostate cancer in night shift workers should be elucidated more thoroughly. The biological steps between melatonin suppression and prostate cancer incidence must be investigated in more detail.
5. Conclusion
This dose-response meta-analysis included 11 cohort studies (12 cohort reports) and seven case-control studies. Egger's regression test results indicated no statistically significant evidence of publication bias for the cohort studies, but there was statistically significant evidence of publication bias for the case-control studies. This study estimated that the risk of prostate cancer increased by 1.10, 11.54, 24.41, and 38.76% after 1, 10, 20, and 30 years of night shift work exposure, respectively, according to the reliable four cohort and five case-control studies.
To ensure the reliability of the findings, this study (ⅰ) rigorously applied seven transparent inclusion criteria. Furthermore, (ⅱ) a complete separation was made between the RRs derived from cohort studies and ORs derived from case-control studies, with each type of pooled effect estimate being synthesized independently. However, owing to the substantial likelihood of publication bias, all ORs from case-control studies were excluded. Moreover, (ⅲ) the exposure dose (measured in years of night shift work) was clearly defined based on information provided in individual studies. Finally, (ⅳ) the authors employed a novel two-stage dose-response meta-analysis method recently documented in the literature [7,8]. Therefore, this study provides the most robust evidence available regarding the relationship between the risk of prostate cancer and exposure to night shift work.
Ethics statement
Review and/or approval by an ethics committee was not needed for this study because it is a meta-analysis. All data used in this study were extracted from previously published studies.
Informed consent was not required because of the same reason mentioned above.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Consent for publication
Not applicable.
Registration information for meta-analysis
This dose-response meta-analysis was not registered. However, any information regarding the process of evidence synthesis can be provided by the authors upon request.
Protocol information
The protocol for this dose-response meta-analysis was not prepared. However, any information regarding the process of evidence synthesis can be provided by the authors upon request.
Data availability statement
This study is a meta-analysis. Therefore, anyone who wants to acquire the used data can access the original data through the original articles. The specific data used in this dose-response meta-analysis were included in this article.
CRediT authorship contribution statement
Jinyoung Moon: Writing – review & editing, Writing – original draft, Visualization, Validation, Supervision, Software, Resources, Project administration, Methodology, Investigation, Funding acquisition, Formal analysis, Data curation, Conceptualization. Elizabeth A. Holzhausen: Writing – review & editing. Yongseok Mun: Writing – review & editing, Investigation, Data curation.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
The authors appreciate the efforts of Minji Kim, an information specialist in the medical library of Inha University, Incheon, South Korea.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.heliyon.2024.e29080.
Contributor Information
Jinyoung Moon, Email: pollux@snu.ac.kr.
Elizabeth A. Holzhausen, Email: Elizabeth.Holzhausen@colorado.edu.
Yongseok Mun, Email: yongseokmun@hallym.or.kr.
Appendix A. Supplementary data
The following is/are the supplementary data to this article:
References
- 1.Night shift work, Lyon (FR), IARC_Working_Group. IARC Monographs on the Identification of Carcinogenic Hazards to Humans Int. Agency Res. Cancer. 2020;124:41. [Google Scholar]
- 2.National_Toxicology_Program . National Toxicology Program; Research Triangle Park (NC): 2021. NTP Cancer Hazard Assessment Report on Night Shift Work and Light at Night. [PubMed] [Google Scholar]
- 3.Haus E.L., Smolensky M.H. Shift work and cancer risk: potential mechanistic roles of circadian disruption, light at night, and sleep deprivation. Sleep Med. Rev. 2013;17(4):273–284. doi: 10.1016/j.smrv.2012.08.003. [DOI] [PubMed] [Google Scholar]
- 4.Kim K.Y., Lee E., Kim Y.J., Kim J. The association between artificial light at night and prostate cancer in Gwangju City and South Jeolla Province of South Korea. Chronobiol. Int. 2017;34(2):203–211. doi: 10.1080/07420528.2016.1259241. [DOI] [PubMed] [Google Scholar]
- 5.Garcia-Saenz A., Miguel ASd, Espinosa A., Valentin A., Aragonés N., Llorca J., et al. Evaluating the association between artificial light-at-night exposure and breast and prostate cancer risk in Spain (MCC-Spain study) Environ. Health Perspect. 2018;126(4) doi: 10.1289/EHP1837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rybnikova N.A., Haim A., Portnov B.A. Is prostate cancer incidence worldwide linked to artificial light at night exposures? Review of earlier findings and analysis of current trends. Arch. Environ. Occup. Health. 2017;72(2):111–122. doi: 10.1080/19338244.2016.1169980. [DOI] [PubMed] [Google Scholar]
- 7.Berlin J.A., Longnecker M.P., Greenland S. Meta-analysis of epidemiologic dose-response data. Epidemiology. 1993;4(3):218–228. doi: 10.1097/00001648-199305000-00005. [DOI] [PubMed] [Google Scholar]
- 8.Shim S.R., Lee J. Dose-response meta-analysis: application and practice using the R software. Epidemiol Health. 2019;41 doi: 10.4178/epih.e2019006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Diaz-Quijano F.A. A simple method for estimating relative risk using logistic regression. BMC Med. Res. Methodol. 2012;12(1):14. doi: 10.1186/1471-2288-12-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lee J., Chia K.S. Estimation of prevalence rate ratios for cross sectional data: an example in occupational epidemiology. Occup. Environ. Med. 1993;50(9):861–862. doi: 10.1136/oem.50.9.861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nijem K., Kristensen P., Al-Khatib A., Bjertness E. Application of different statistical methods to estimate relative risk for self-reported health complaints among shoe factory workers exposed to organic solvents and plastic compounds. Norsk Epidemiol. 2009;15(1) [Google Scholar]
- 12.National_Toxicology_Program . United States Department of Health and Human Services; Washington, DC, USA: 2015. OHAT (Office of Health Assessment and Translation) Risk of Bias Rating Tool for Human and Animal Studies. [Google Scholar]
- 13.Sterne J.A.C., Becker B.J., Egger M. 2005. The Funnel Plot. Publication Bias in Meta‐Analysis; pp. 73–98. [Google Scholar]
- 14.Crippa A., Orsini N. Multivariate dose-response meta-analysis: the dosresmeta R package. J. Stat. Software, Code Snippets. 2016;72(1):1–15. [Google Scholar]
- 15.Zhang J., Yu K.F. What's the relative risk? JAMA. 1998;280(19):1690. doi: 10.1001/jama.280.19.1690. [DOI] [PubMed] [Google Scholar]
- 16.Schwarzer G. vol. 9. The R foundation for statistical computing; 2012. p. 27. (Package ‘meta’). [Google Scholar]
- 17.Page M.J., McKenzie J.E., Bossuyt P.M., Boutron I., Hoffmann T.C., Mulrow C.D., et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372 doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ahn Y.S., Jeong K.S., Kim K.S. Cancer morbidity of professional emergency responders in Korea. Am. J. Ind. Med. 2012;55(9):768–778. doi: 10.1002/ajim.22068. [DOI] [PubMed] [Google Scholar]
- 19.Behrens T., Rabstein S., Wichert K., Erbel R., Eisele L., Arendt M., et al. Shift work and the incidence of prostate cancer: a 10-year follow-up of a German population-based cohort study. Scand. J. Work. Environ. Health. 2017;43(6):560–568. doi: 10.5271/sjweh.3666. [DOI] [PubMed] [Google Scholar]
- 20.Gapstur S.M., Diver W.R., Stevens V.L., Carter B.D., Teras L.R., Jacobs E.J. Work schedule, sleep duration, insomnia, and risk of fatal prostate cancer. Am. J. Prev. Med. 2014;46(3 SUPPL. 1):S26–S33. doi: 10.1016/j.amepre.2013.10.033. [DOI] [PubMed] [Google Scholar]
- 21.Kubo T., Oyama I., Nakamura T., Kunimoto M., Kadowaki K., Otomo H., et al. Industry-based retrospective cohort study of the risk of prostate cancer among rotating-shift workers. Int. J. Urol. 2011;18(3):206–211. doi: 10.1111/j.1442-2042.2010.02714.x. [DOI] [PubMed] [Google Scholar]
- 22.Kubo T., Ozasa K., Mikami K., Wakai K., Fujino Y., Watanabe Y., et al. Prospective cohort study of the risk of prostate cancer among rotating-shift workers: findings from the Japan Collaborative Cohort Study. Am. J. Epidemiol. 2006;164(6):549–555. doi: 10.1093/aje/kwj232. [DOI] [PubMed] [Google Scholar]
- 23.Schwartzbaum J., Ahlbom A., Feychting M. Cohort study of cancer risk among male and female shift workers. Scand. J. Work. Environ. Health. 2007;33(5):336–343. doi: 10.5271/sjweh.1150. [DOI] [PubMed] [Google Scholar]
- 24.Yong M., Blettner M., Emrich K., Nasterlack M., Oberlinner C., Hammer G.P. A retrospective cohort study of shift work and risk of incident cancer among German male chemical workers. Scand. J. Work. Environ. Health. 2014;40(5):502–510. doi: 10.5271/sjweh.3438. [DOI] [PubMed] [Google Scholar]
- 25.Berge L.A.M., Liu F.C., Grimsrud T.K., Stoer N.C., Veierod M.B., Stenehjem J.S. Night shift work and risk of aggressive prostate cancer in the Norwegian Offshore Petroleum Workers (NOPW) Cohort. Saf. Health Work. 2022;13(Supplement):S263. [Google Scholar]
- 26.McNeil J., Heer E., Willemsen R.F., Friedenreich C.M., Brenner D.R. The effects of shift work and sleep duration on cancer incidence in Alberta's Tomorrow Project cohort. Cancer Epidemiol. 2020;67 doi: 10.1016/j.canep.2020.101729. (no pagination) [DOI] [PubMed] [Google Scholar]
- 27.Dickerman B.A., Markt S.C., Koskenvuo M., Hublin C., Pukkala E., Mucci L.A., et al. Sleep disruption, chronotype, shift work, and prostate cancer risk and mortality: a 30-year prospective cohort study of Finnish twins. Cancer Causes Control. 2016;27(11):1361–1370. doi: 10.1007/s10552-016-0815-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hammer G.P., Emrich K., Nasterlack M., Blettner M., Yong M. Shift work and prostate cancer incidence in industrial workers. Deutsches Ärzteblatt Int. 2015 doi: 10.3238/arztebl.2015.0463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Barul C., Richard H., Parent M.E. Night-shift work and risk of prostate cancer: results from a Canadian case- control study, the prostate cancer and environment study. Am. J. Epidemiol. 2019;188(10):1801–1811. doi: 10.1093/aje/kwz167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Conlon M., Lightfoot N., Kreiger N. Rotating shift work and risk of prostate cancer. Epidemiology. 2007;18(1):182–183. doi: 10.1097/01.ede.0000249519.33978.31. [DOI] [PubMed] [Google Scholar]
- 31.Papantoniou K., Castano-Vinyals G., Espinosa A., Aragones N., Perez-Gomez B., Burgos J., et al. Night shift work, chronotype and prostate cancer risk in the MCC-Spain case-control study. Int. J. Cancer. 2015;137(5):1147–1157. doi: 10.1002/ijc.29400. [DOI] [PubMed] [Google Scholar]
- 32.Parent M.-É., El-Zein M., Rousseau M.-C., Pintos J., Siemiatycki J. Night work and the risk of cancer among men. Am. J. Epidemiol. 2012;176(9):751–759. doi: 10.1093/aje/kws318. [DOI] [PubMed] [Google Scholar]
- 33.Tse L.A., Lee P.M.Y., Ho W.M., Lam A.T., Lee M.K., Ng S.S.M., et al. Bisphenol A and other environmental risk factors for prostate cancer in Hong Kong. Environ. Int. 2017;107:1–7. doi: 10.1016/j.envint.2017.06.012. [DOI] [PubMed] [Google Scholar]
- 34.Lozano-Lorca M., Olmedo-Requena R., Vega-Galindo M.V., Vazquez-Alonso F., Jimenez-Pacheco A., Salcedo-Bellido I., et al. Night shift work, chronotype, sleep duration, and prostate cancer risk: caplife study. Int. J. Environ. Res. Publ. Health. 2020;17(17):1–17. doi: 10.3390/ijerph17176300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wendeu-Foyet M.G., Bayon V., Cénée S., Trétarre B., Rébillard X., Cancel-Tassin G., et al. Night work and prostate cancer risk: results from the EPICAP Study. Occup. Environ. Med. 2018;75(8):573–581. doi: 10.1136/oemed-2018-105009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Åkerstedt T., Narusyte J., Svedberg P., Kecklund G., Alexanderson K. Night work and prostate cancer in men: a Swedish prospective cohort study. BMJ Open. 2017;7(6) doi: 10.1136/bmjopen-2016-015751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Berge L.A.M., Liu F.-C., Grimsrud T.K., Babigumira R., Støer N.C., Kjærheim K., et al. Night shift work and risk of aggressive prostate cancer in the Norwegian Offshore Petroleum Workers (NOPW) cohort. Int. J. Epidemiol. 2023;52(4):1003–1014. doi: 10.1093/ije/dyac235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gapstur S.M., Diver W.R., Stevens V.L., Carter B.D., Teras L.R., Jacobs E.J., Schedule Work. Sleep duration, insomnia, and risk of fatal prostate cancer. Am. J. Prev. Med. 2014;46(3, Supplement 1):S26–S33. doi: 10.1016/j.amepre.2013.10.033. [DOI] [PubMed] [Google Scholar]
- 39.Barul C., Richard H., Parent M.-E. Night-shift work and risk of prostate cancer: results from a Canadian case-control study, the prostate cancer and environment study. Am. J. Epidemiol. 2019;188(10):1801–1811. doi: 10.1093/aje/kwz167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Conlon M., Lightfoot N., Kreiger N. Rotating shift work and risk of prostate cancer. Epidemiology. 2007;18(1):182–183. doi: 10.1097/01.ede.0000249519.33978.31. [DOI] [PubMed] [Google Scholar]
- 41.Kubo T., Oyama I., Nakamura T., Kunimoto M., Kadowaki K., Otomo H., et al. Industry-based retrospective cohort study of the risk of prostate cancer among rotating-shift workers. Int. J. Urol. 2011;18(3):206–211. doi: 10.1111/j.1442-2042.2010.02714.x. [DOI] [PubMed] [Google Scholar]
- 42.Schwartzbaum J., Ahlbom A., Feychting M. Cohort study of cancer risk among male and female shift workers. Scand. J. Work. Environ. Health. 2007;(5):336–343. doi: 10.5271/sjweh.1150. [DOI] [PubMed] [Google Scholar]
- 43.Yong M., Blettner M., Emrich K., Nasterlack M., Oberlinner C., Hammer G.P. A retrospective cohort study of shift work and risk of incident cancer among German male chemical workers. Scand. J. Work. Environ. Health. 2014;(5):502–510. doi: 10.5271/sjweh.3438. [DOI] [PubMed] [Google Scholar]
- 44.Rivera-Izquierdo M., Martínez-Ruiz V., Castillo-Ruiz E.M., Manzaneda-Navío M., Pérez-Gómez B., Jiménez-Moleón J.J. Shift work and prostate cancer: an updated systematic review and meta-analysis. Int. J. Environ. Res. Publ. Health. 2020;17(4):1345. doi: 10.3390/ijerph17041345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Mancio J., Leal C., Ferreira M., Norton P., Lunet N. Does the association of prostate cancer with night-shift work differ according to rotating vs. fixed schedule? A systematic review and meta-analysis. Prostate Cancer Prostatic Dis. 2018;21(3):337–344. doi: 10.1038/s41391-018-0040-2. [DOI] [PubMed] [Google Scholar]
- 46.Xie L., Rao D., Yu H., Bai Y., Zheng X. Does night-shift work increase the risk of prostate cancer? a systematic review and meta-analysis. OncoTargets Ther. 2015:2817. doi: 10.2147/OTT.S89769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Pukkala E., Ojamo M., Rudanko S.-L., Stevens R.G., Verkasalo P.K. Does incidence of breast cancer and prostate cancer decrease with increasing degree of visual impairment. Cancer Causes Control. 2006;17(4):573–576. doi: 10.1007/s10552-005-9005-6. [DOI] [PubMed] [Google Scholar]
- 48.Feychting M., OsterLund B., Ahlbom A. Reduced cancer incidence among the blind. Epidemiology. 1998;9(5):490–494. [PubMed] [Google Scholar]
- 49.Chowdhury-Paulino I.M., Hart J.E., James P., Iyer H.S., Wilt G.E., Booker B.D., et al. Association between outdoor light at night and prostate cancer in the health professionals follow-up study. Cancer Epidemiol. Biomarkers Prev. 2023;32(10):1444–1450. doi: 10.1158/1055-9965.EPI-23-0208. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
This study is a meta-analysis. Therefore, anyone who wants to acquire the used data can access the original data through the original articles. The specific data used in this dose-response meta-analysis were included in this article.