Highlights
-
•
Social determinants of health are fundamental causes of poor cardiovascular health.
-
•
Low income and educational attainment are associated with cardiovascular risk.
-
•
CVD risk was lower among Hispanic adults of low income compared with other groups.
-
•
Socioeconomic status considerations are lacking in CVD prediction and prevention.
Keywords: Atherosclerotic Cardiovascular Disease (ASCVD) risk, Social Determinants of Health (SDOH), Socioeconomic status (SES), Health disparities, Cardiovascular Disease (CVD)
Abstract
Introduction
Social determinants of health (SDOH) are fundamental causes of poor cardiovascular health, yet cardiovascular disease (CVD) risk assessment tools exclude SDOH. Our objective was to determine whether SDOH are independently associated with CVD risk in US adults.
Methods
Utilizing the National Health and Nutrition Examination Survey (NHANES), we combined years 1999–2018 and included participants aged 40–79 without history of CVD and with information to calculate CVD risk (n = 21,694). Ten-year risk of atherosclerotic CVD (ASCVD) was calculated using the American Heart Association/American College of Cardiology (AHA/ACC) pooled cohort equations. We used linear regression models to estimate the association between SDOH and ASCVD risk, after adjusting for demographic factors. All analyses accounted for the complex survey design.
Results
Mean age was 54.7 years, with 52.7 % female, 73.8 % non-Hispanic White, 9.4 % non-Hispanic Black, and 10.7 % Hispanic. From adjusted models, compared with an income of ≥ $75 K, ASCVD risk was greater by 3.06 (95 % CI: 2.65, 3.47) among those with income < $25 K, by 1.55 (95 % CI: 1.21, 1.89) among those with income $25 K–<$55 K, and by 1.20 (95 % CI: 0.84, 1.56) among those with income $55 K–<$75 K. Compared to college graduates, ASCVD risk was greater by 3.09 (95 % CI: 2.56, 3.62) among those with less than a high school education, by 1.65 (95 % CI: 1.31, 200) among those who were high school graduates, and by 1.41 (95 % CI: 1.11, 1.72) among those with some college education.
Conclusion
We found strong graded associations between lower income and lower educational attainment with greater CVD risk.
1. Introduction
Cardiovascular disease (CVD) is the leading cause of death in the US (Tsao et al., 2022), and about 10 % of the US population is actively affected by CVD (Tsao et al., 2022). To help identify those at increased risk of CVD, risk assessment tools are frequently utilized (Goff et al., 2014). For example, the American College of Cardiology/American Heart Association (ACC/AHA) atherosclerotic cardiovascular disease (ASCVD) risk calculator is used to predict the likelihood of a first CVD event within the next ten years (Goff et al., 2014). Beyond its utility as a risk assessment tool, the ASCVD risk score is also used clinically to guide treatment decisions, demonstrating its wide range of importance (Whelton et al., 2018). While CVD is common among men, women, and across all race/ethnic groups, individuals of lower socio-economic status (SES) are disproportionately burdened (Schultz et al., 2018, Abdalla et al., 2020).
In fact, social determinants of health (SDOH) are recognized as a major driver of health inequities and health disparities (Abdalla et al., 2020, Lloyd-Jones et al., 2022). At the individual level, income and education remain the most common measures of SES (Braveman and Gottlieb, 2014). The strong inverse gradient between education and income with CVD has been frequently described in high income countries (Schultz et al., 2018, Kaplan and Keil, 1993, Stringhini et al., 2017), with socioeconomically disadvantaged populations having greater risk of CVD related morbidity and mortality (Framke et al., 2020, Hamad et al., 2019, Schultz et al., 2018). Women and historically marginalized groups, such as Black and Hispanic persons, are overrepresented among those living in poverty and thus, disproportionately affected by health disparities in CVD (Wenger et al., 2022, Woodward, 2019, Mosca et al., 2011, Humphries et al., 2017). In fact, numerous studies have highlighted stronger associations between SDOH with cardiovascular health among women compared with men (Lindley Kathryn et al., 2021, Kathryn et al., 2017, Gebreab et al., 2015). Likewise, compared to non-Hispanic White adults, racial/ethnic minority populations are more likely to have lower educational attainment, which is widely considered one of the most reliable social risk factors for the development of CVD (Kelli et al., 2019, De Brey et al., 2018). As a consequence, lower SES results in substantial health disparities and health inequities, manifesting as higher rates of CVD for racial/ethnic minorities and women.
While the relationship between SES and cardiovascular health (CVH) outcomes has been well studied in various racial/ethnic groups (Lloyd-Jones et al., 2009, Brewer et al., 2018, Gasevic et al., 2015, Wenger et al., 2022, Bello et al., 2022), fewer studies have evaluated the relationship between SDOH and ASCVD risk among ethnic/racial minorities within the US (Shen et al., 2022). Therefore, the goal of our study was to assess the relationship between SES and ASCVD risk and determine whether these associations were modified by sex and race/ethnicity. We leveraged data from the National Health and Nutrition Examination Survey (NHANES), a representative survey of the US general adult population.
2. Methods
All data have been made publicly available by the National Center for Health Statistics, and thus, the study is exempt from ethical compliance.
2.1. Study sample
The National Health and Nutrition Examination Survey (NHANES) is a cross-sectional survey conducted annually since 1999 and representative of the US non-institutionalized population. NHANES is designed to evaluate the health and nutritional status of the US population using the standardized household interview questionnaires and physical examinations. Since 1999, NHANES participants have been drawn from a multi-year, stratified, clustered four-stage sample design (Curtin et al., 2012, Mirel et al., 2013, Chen et al., 2018, Chen et al., 2020). NHANES data collection occurs in three steps: a household screener determines eligible individuals for the home interview and examination, the interviewer administers questionnaires and collects demographic, health, and nutritional information, and the participant then schedules and attends an examination at the mobile examination center where physical measurements, and blood and urine specimens are collected for laboratory testing (Curtin et al., 2012, Mirel et al., 2013, Chen et al., 2018, Chen et al., 2020). An appointment can be made to administer the household interview at a later date. Each participant provided information that was current at the time of their respective NHANES data cycle. The current study utilizes NHANES data from all nationally representative and available survey cycles, years 1999 to 2018, and restricted to 21,694 participants between the ages of 40 and 79, without a history of CVD, and with complete data on SES and CVD risk factors necessary to calculate the ASCVD risk score (all described and defined below) (NCHS, xxxx). A study flow chart is shown in Supplemental Fig. 1. The National Center for Health Statistics approved all NHANES protocols and obtained written informed consent from all participants prior to survey commencement.
2.2. Socio-economic Status (SES)
SES was conceptualized with three measures. Annual family income was self-reported in the following categories: <$25 K, $25 K-<$55 K, $55 K-<75 K, or ≥ $75 K. Income criteria were selected to ensure consistency across data cycles with the lowest top-coded income criteria from 4 cycles from 1999 to 2006. Further, the lowest income level (<25 k) was selected to reflect living below the poverty level for a family of four in 2018 (Services USDoHaH, 2018). Finally, the threshold of 55 k reflects the unadjusted median household income in the U.S. in 2016. Annual family income to poverty ratio (FIPR) was calculated as a ratio between annual family income to the federal poverty threshold based on household size (NCHS, xxxx). FIPR was treated as both a continuous variable and a categorical variable with the following groups: FIPR < 1.00; 1.00 to <1.39; 1.39 to <2.00; 2.00 to <3.00; or ≥3.00. The category boundary of 1.39 was chosen to acknowledge medical benefits that were expanded to individuals in certain states with a FIPR between 1.00–1.38 as a result of passage of the Affordable Care Act (ACA) (Lin et al., 2021). Education: was self-reported as the highest education grade level achieved at the time of interview and categorized as: less than high school (HS), HS graduate, some college, or college graduate and above.
2.3. Atherosclerotic Cardiovascular Disease Risk (ASCVD)
Described in detail elsewhere, ASCVD risk was calculated using the sex and race specific ACC/AHA ASCVD pooled cohort equation (Goff et al., 2014). Given that the pooled cohort equation only provides black and white specific parameters, white equation parameters were applied to all non-black race groups, per ACC/AHA recommendations (Goff et al., 2014). Briefly, ASCVD risk was calculated based on previously published parameter estimates (Goff et al., 2014), in combination with individual specific factors such as: age, sex, race, total cholesterol (mg/dL), HDL cholesterol (mg/dL) (HDL-C), systolic blood pressure (mmHg) (SBP), use of blood pressure medication, current smoking status, and diabetes status (all defined below). These variables were incorporated into a series of equations used to quantify 10-year risk of having an ASCVD event. The first step was to calculate the natural log of age, total cholesterol, HDL-C, and SBP (untreated and treated), in addition to all appropriate interaction terms. Next, these individual values were multiplied by respective race and sex-specific coefficients provided within the ACC/AHA guideline and totaled as the sum for each individual. The estimated ASCVD risk is then calculated as 1 minus the provided baseline survival rate at 10 years based on each sex/race group, raised to the power of the exponent of the individual sum minus the overall average sum for each race/sex group.
The ASCVD risk component variables (detailed above) were determined through utilization of both questionnaire responses and physical examination measurements. Sex, race/ethnicity, age, smoking status, use of BP medication, and use of diabetes medication were all self-reported. SBP was measured three consecutive times, 30 s apart, and using the same arm, while seated, after an appropriate five-minute rest period, with the average recorded as the final measurement (Lamprea-Montealegre et al., 2021). HDL-C was measured by the heparin-manganese precipitation method technique (NCHS, xxxx, CDC, 2010), while total cholesterol was measured in a series of enzymatic reactions (Gao et al., 2023). Diabetes was defined by a self-reported history of diabetes, fasting glucose ≥126 mg/dL, or hemoglobin A1c ≥ 6.5 %. Once risk estimates were calculated, ASCVD risk was classified into the following categories: low risk (<5%); borderline risk (5 % to <7.5 %); intermediate risk (7.5 % to <20 %); or high risk (≥20 %), based on previously published thresholds (Grundy et al., 2019).
2.4. Other variables
Participants also self-reported their current marital status (married or unmarried), and current health insurance status (yes/no).
2.5. Statistical analysis
Demographic and socio-economic characteristics were assessed overall and according to ASCVD risk groups. Differences across categories of ASCVD risk were assessed using chi-square tests for proportions or ANOVAs for continuous variables. Next, we estimated the age-standardized prevalence of ASCVD risk levels overall and according to important demographic (sex and race/ethnicity) and SES factors of interest. To determine whether SES was associated with ASCVD risk, we utilized a series of multivariable adjusted linear regressions with ASCVD risk conceptualized continuously and modeled as a percentage multiplied by 100. Model 1 was adjusted for age only. Model 2 was adjusted for age, sex, and race/ethnicity. Model 3 was adjusted for age, sex, race/ethnicity, marital status, and health insurance. Given the strong correlation between our SES factors of interest, we considered Model 3 to be our final model. As a supplementary analysis, we also included an additional model which adjusted for age, sex, race/ethnicity, marital status, health insurance status, education (in income and FIPR models), and income (in education models). Finally, we used multiplicative interaction terms (in Model 3) to determine whether the association between SES and ASCVD risk was modified by sex or race/ethnicity. Significant interactions (α < 0.10) resulted in stratified models. All analyses accounted for the NHANES complex survey design, and data were weighted to correspond to individuals who attended the mobile examination clinic and ensure representativeness of the US population (i.e. including 20-year mobile examination center weights to reflect the ten 2-year data cycles). Analyses were conducted using SUDAAN V11.0.4.
3. Results
Among US adults aged 40–79 without a history of CVD, approximately half (52.7 %) were women, 73.8 % were white, 9.4 % were black, and 10.7 % were Hispanic (Table 1). Most were US born (84.7 %), married (65.9 %), and insured (87.4 %). Approximately one third (31.1 %) had a college education or greater, 38.4 % had an annual income ≥$75,000 and 59 % had a FIPR ≥ 3.00. Participants at greater risk of an ASCVD event were more likely to be older, male, unmarried, insured, have lower education attainment, and lower incomes (all p-values < 0.05).
Table 1.
Characteristics of the study sample, overall and stratified by CVD risk, NHANES 1999–2018.
|
10-year ASCVD risk |
|||||
|---|---|---|---|---|---|
|
Overall N = 21,694 |
< 5 % (n = 9,512) |
5 % – < 7.5 % (n = 2,479) |
7.5 % – < 20 % (n = 5,861) |
≥ 20 % (n = 3,842) |
|
| Characteristics |
% or mean (95 % CI) |
% or mean (95 % CI) |
% or mean (95 % CI) |
% or mean (95 % CI) |
% or mean (95 % CI) |
| Age* | |||||
| 40–49 | 37.1 (36.0, 38.2) | 60.0 (58.6, 61.4) | 22.8 (20.8, 24.9) | 10.6 (9.5, 11.7) | 2.3 (1.7, 3.1) |
| 50–59 | 31.8 (30.8, 32.7) | 33.6 (32.3, 35.0) | 47.9 (45.5, 50.2) | 31.4 (29.6, 33.3) | 8.2 (6.8, 9.8) |
| 60–69 | 20.3 (19.5, 21.1) | 6.4 (5.7, 7.1) | 28.3 (26.0, 30.9) | 43.7 (42.0, 45.4) | 28.1 (26.3, 30.0) |
| 70–79 | 10.9 (10.3, 11.5) | 0.0 (0.0, 0.0) | 1.0 (0.7, 1.6) | 14.4 (13.3, 15.5) | 61.4 (59.2, 63.7) |
| Female* | 52.7 (51.9, 53.4) | 65.8 (64.7, 66.9) | 41.6 (39.2, 44.1) | 37.3 (35.8, 38.8) | 36.1 (34.4, 38.0) |
| Race/ethnicity* | |||||
| White | 73.8 (71.8, 75.8) | 73.7 (71.6, 75.7) | 74.4 (72.0, 76.7) | 73.4 (70.9, 75.8) | 74.5 (71.6, 77.1) |
| Black | 9.4 (8.5, 10.5) | 7.6 (6.8, 8.6) | 11.0 (9.6, 12.6) | 12.1 (10.7, 13.6) | 10.7 (9.2, 12.5) |
| Hispanic | 10.7 (9.4, 12.2) | 11.9 (10.6, 13.4) | 9.9 (8.4, 11.5) | 9.1 (7.8, 10.6) | 9.5 (7.8, 11.5) |
| Other | 6.0 (5.4, 6.7) | 6.7 (5.9, 7.6) | 4.7 (3.8, 5.8) | 5.5 (4.6, 6.5) | 5.3 (4.4, 6.5) |
| US born | 84.7 (83.3, 86.0) | 83.0 (81.5, 84.5) | 86.2 (84.5, 87.8) | 87.0 (85.4, 88.4) | 86.2 (84.1, 88.1) |
| Married* | 65.9 (64.7, 67.1) | 67.7 (66.3, 69.0) | 64.5 (62.1, 66.9) | 64.2 (62.2, 66.2) | 62.8 (60.3, 65.3) |
| Insured* | 87.4 (86.5, 88.2) | 86.2 (85.0, 87.3) | 84.4 (82.4, 86.2) | 88.0 (86.7, 89.1) | 94.6 (93.5, 95.5) |
| Education* | |||||
| < HS | 15.3 (14.3, 16.4) | 11.8 (10.8, 12.8) | 15.9 (14.2, 17.8) | 18.1 (16.6, 19.7) | 24.6 (22.7, 26.7) |
| HS Graduate | 23.7 (22.7, 24.7) | 21.1 (20.0, 22.4) | 23.8 (21.6, 26.3) | 27.7 (25.8, 29.6) | 26.9 (24.9, 29.1) |
| Some College | 29.9 (28.9, 30.9) | 31.0 (29.6, 32.3) | 30.1 (27.8, 32.5) | 29.4 (27.7, 31.2) | 26.3 (24.3, 28.5) |
| College+ | 31.1 (29.4, 32.8) | 36.1 (34.0, 38.2) | 30.1 (27.3, 33.1) | 24.8 (22.8, 26.9) | 22.1 (20.1, 24.2) |
| Annual Income* | |||||
| < $25 K | 20.4 (19.1, 21.7) | 15.6 (14.4, 16.8) | 20.6 (18.5, 22.9) | 24.6 (22.8, 26.4) | 32.9 (30.5, 35.4) |
| $25 K – < $55 K | 27.6 (26.4, 28.7) | 24.8 (23.5, 26.2) | 25.5 (23.2, 28.0) | 30.9 (29.1, 32.8) | 35.1 (32.5, 37.8) |
| $55 K – < $75 K | 13.7 (12.9, 14.5) | 13.9 (12.8, 15.0) | 16.0 (14.2, 18.0) | 12.8 (11.7, 14.0) | 12.5 (10.9, 14.4) |
| ≥$75 K | 38.4 (36.5, 40.2) | 45.7 (43.6, 47.8) | 37.8 (34.6, 41.2) | 31.8 (29.4, 34.2) | 19.5 (17.3, 21.9) |
| FIPR, (mean)* | 3.3 (3.3, 3.4) | 3.5 (3.4, 3.6) | 3.4 (3.3, 3.5) | 3.2 (3.1, 3.2) | 2.8 (2.7, 2.9) |
| FIPR* | |||||
| < 1.00 | 10.0 (9.3, 10.8) | 9.0 (8.2, 9.8) | 10.4 (9.0, 12.1) | 11.2 (10.0, 12.4) | 11.7 (10.4, 13.1) |
| 1.00 – <1.39 | 7.3 (6.8, 7.9) | 6.1 (5.5, 6.7) | 6.4 (5.4, 7.6) | 8.8 (8.0, 9.7) | 10.9 (9.7, 12.2) |
| 1.39 – <2.00 | 9.5 (8.8, 10.2) | 8.1 (7.3, 8.9) | 9.1 (7.7, 10.7) | 10.3 (9.2, 11.5) | 14.6 (13.0, 16.3) |
| 2.00 – <3.00 | 14.2 (13.5, 15.0) | 12.7 (11.7, 13.7) | 12.2 (10.6, 14.0) | 16.3 (14.9, 17.7) | 19.1 (17.2, 21.2) |
| ≥$3.00 | 59.0 (57.2, 60.7) | 64.2 (62.4, 66.0) | 61.9 (58.9, 64.9) | 53.4 (51.1, 55.8) | 43.7 (41.0, 46.4) |
| Smoker* | 18.9 (18.0, 19.8) | 12.5 (11.5, 13.4) | 24.8 (22.7, 27.0) | 28.5 (27.0, 30.1) | 22.4 (20.6, 24.3) |
| SBP, mean (mmHg)* | 125.6 (125.2, 126.0) |
119.0 (118.6,119.4) |
126.4 (125.7, 127.2) |
131.3 (130.6, 132.0) |
142.6 (141.7, 143.4) |
| BP Medication* | 27.4 (26.5, 28.3) | 14.6 (13.6, 15.6) | 29.6 (27.4, 31.9) | 39.6 (37.9, 41.3) | 57.4 (55.2, 59.6) |
| Diabetes* | 12.8 (12.2, 13.4) | 5.1 (4.6, 5.7) | 12.2 (10.5, 14.1) | 18.3 (16.9, 19.7) | 36.2 (34.3, 38.1) |
| Cholesterol, mean (mg/dL)* | 205.4 (204.4, 206.4) |
202.8 (201.7, 203.9) |
209.6 (207.2, 212.0) |
208.7 (207.0, 210.4) |
206.2 (203.2, 209.3) |
| HDL, mean (mg/dL)* | 54.4 (54.0, 54.9) |
57.4 (56.9, 57.9) |
52.2 (51.0, 53.5) |
51.0 (50.4, 51.6) |
50.2 (49.6, 50.8) |
Abbreviations: NHANES: National Health and Nutrition Examination; HS: High school; FIPR: Family income to poverty ratio; SBP: Systolic blood pressure; BP: Blood pressure; HDL: High-Density Lipoprotein.
Missing Data: Nativity 0.4 %, Marital status 1.0 %.
Indicates estimates differ across categories of ASCVD risk, p < 0.05 using chi-square tests for proportions or ANOVAs for means.
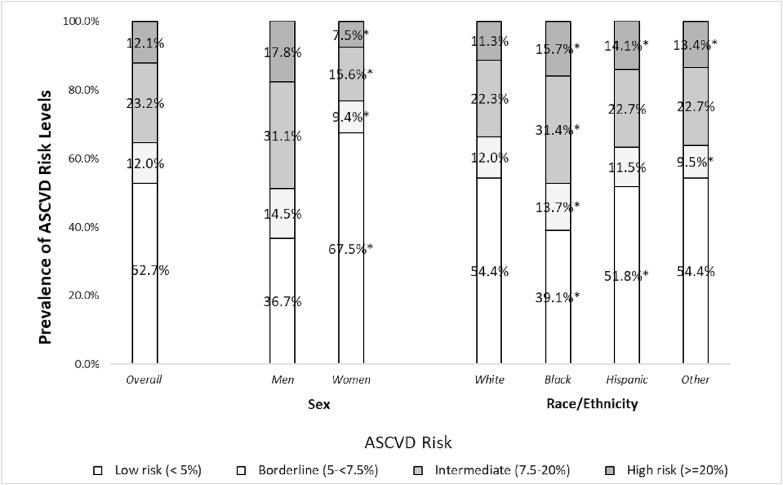
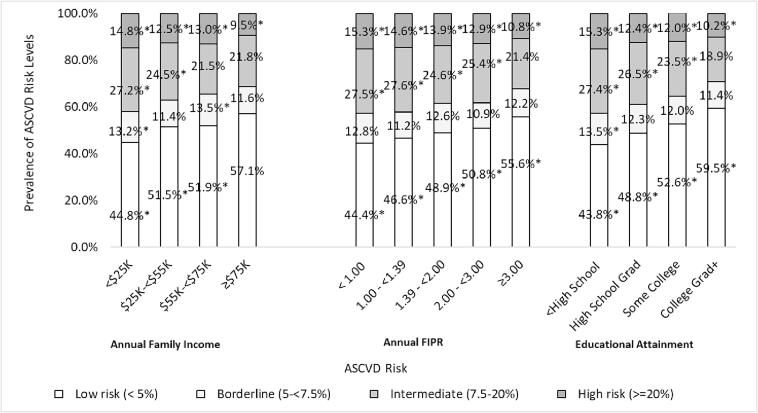
Risk of ASCVD was low in 52.7 % (95 % CI: 51.9, 53.4), borderline in 12.0 % (95 % CI: 11.5, 12.6), intermediate in 23.2 % (95 % CI: 22.6, 23.8), and high in 12.1 % (95 % CI: 11.6, 12.5) of the US population (Fig. 1). The distribution of ASCVD risk differed by sex and race/ethnicity, men compared with women, and non-Hispanic Black and Hispanic adults compared with non-Hispanic White adults, who were at a significantly greater risk of an ASCVD event over 10 years (p-values < 0.05). The distribution of ASCVD risk also differed significantly according to SES (Fig. 2). The 10-year risk of an ASCVD event was significantly higher among those with lower income, lower FIPR, and with less education in a graded manner.
Fig. 1.
Age standardized prevalence of ASCVD Risk, Overall and Stratified by Race and Gender *Statistically significant differences between ASCVD risk level and reference group (sex reference group: male; race/ethnicity reference group: white).
Fig. 2.
Age standardized prevalence of ASCVD Risk, Stratified by Family Income, FIPR, and Education *Statistically significant differences between ASCVD risk level and reference group (annual family income: $≥75 K, FIPR: ≥3.00, educational attainment: college grad+).
From fully adjusted linear regression models (Table 2), compared to those with the highest income (≥$75 K), ASCVD risk was significantly greater by: 1.20 % (95 %CI: 0.84, 1.56) with an income $55 K to <$75 K, 1.55 % (95 % CI: 1.21, 1.89) with an income $25 K to <$55 K, and 3.06 % with an income <$25 K (95 % CI: 2.65, 3.47). Each one-unit decrement in FIPR was associated with a 0.67 % greater ASCVD risk (95 % CI: 0.57, 0.77). Compared to those with the highest FIPR (≥3.00), ASCVD risk was significantly greater by: 1.17 % (95 %CI: 0.70, 1.64) with an FIPR of 2.00 to <3.00, 1.48 % (95 % CI: 1.01, 1.95) with an FIPR 1.39 to <2.00, 2.45 % (95 % CI: 1.98, 2.91) with an FIPR of 1.00 to <1.39, and 2.66 % (95 % CI: 2.16, 3.16) with an FIPR of < 1.00. Compared to US adults with a college degree, ASCVD risk was greater by 1.41 % (95 % CI: 1.11, 1.72) among those with some college, 1.65 % (95 % CI: 1.31, 2.00) among those who were high school graduates, and by 3.09 % (95 % CI: 2.56, 3.62) among those with less than high school education. Model 4 results (additionally adjusted for SES) were similar to model 3 results, though attenuated.
Table 2.
Associations of SES factors with CVD Risk, NHANES 1999–2018.
|
Model 1 |
Model 2 |
Model 3 |
|
|---|---|---|---|
| β (95 % CI) | β (95 % CI) | β (95 % CI) | |
| Annual Income | |||
| ≥$75 K (ref) | − | − | − |
| $55 K – < $75 K | 1.10* (0.72, 1.47) | 1.17* (0.81, 1.53) | 1.20* (0.84, 1.56) |
| $25 K – < $55 K | 1.34* (1.02, 1.66) | 1.45* (1.13, 1.78) | 1.55* (1.21, 1.89) |
| < $25 K | 2.71* (2.34, 3.09) | 2.89* (2.51, 3.26) | 3.06* (2.65, 3.47) |
| FIPR (one-unit decrement) | 0.63* (0.55, 0.72) | 0.65* (0.57, 0.74) | 0.67* (0.57, 0.77) |
| FIPR | |||
| ≥3.00 (ref) | − | − | − |
| 2.00 – < 3.00 | 1.13* (0.66, 1.61) | 1.15* (0.69, 1.62) | 1.17* (0.70, 1.64) |
| 1.39 – < 2.00 | 1.38* (0.90, 1.86) | 1.45* (1.00, 1.89) | 1.48* (1.01, 1.95) |
| 1.00 – < 1.39 | 2.27* (1.81, 2.74) | 2.41* (1.96, 2.86) | 2.45* (1.98, 2.91) |
| < 1.00 | 2.65* (2.22, 3.08) | 2.64* (2.17, 3.10) | 2.66* (2.16, 3.16) |
| Education | |||
| College Graduate+ (ref) | − | − | − |
| Some College | 1.28* (0.96, 1.60) | 1.45* (1.15, 1.74) | 1.41* (1.11, 1.72) |
| High School Graduate | 1.70* (1.36, 2.04) | 1.69* (1.35, 2.03) | 1.65* (1.31, 2.00) |
| < High School | 3.36* (2.89, 3.83) | 3.13* (2.64, 3.63) | 3.09* (2.56, 3.62) |
a. Model 1 is adjusted for age.
b. Model 2 is additionally adjusted for sex and race/ethnicity.
c. Model 3 is additionally adjusted for marital status and health insurance.
Statistically significant (p-value < 0.05).
3.1. Differences by sex
The association between annual income and FIPR with ASCVD risk differed by sex (interaction p-values < 0.1) (Table 3). From fully adjusted models, the associations between both annual income and FIPR with ASCVD risk were stronger among men. For example, each one-unit increment in FIPR was associated with greater ASCVD risk among men by: 0.74 % (95 % CI: 0.57, 0.90) or 0.63 % (95 % CI: 0.53, 0.72) among women.
Table 3.
Associations of SES factors with CVD Risk by Sex and Race/Ethnicity, NHANES 1999–2018.
|
Sex |
Race/ethnicity |
|||||
|---|---|---|---|---|---|---|
| Men | Women | White | Black | Hispanic | Other | |
| β (95 % CI) | β (95 % CI) | β (95 % CI) | β (95 % CI) | β (95 % CI) | β (95 % CI) | |
| Annual Income | ||||||
| ≥$75 K (ref) | − | − | − | − | − | − |
| $55 K – < $75 K | 1.68* (1.07, 2.29) | 0.74* (0.34, 1.14) | 1.26* (0.81, 1.72) | 0.96* (0.22, 1.71) | 0.27 (−0.45, 1.00) | 1.95* (0.88, 3.02) |
| $25 K – < $55 K | 1.98* (1.41, 2.55) | 1.18* (0.85, 1.51) | 1.68* (1.26, 2.10) | 1.49* (0.75, 2.22) | 0.49 (−0.31, 1.29) | 1.70* (0.68, 2.71) |
| <$25 K | 3.41* (2.71, 4.10) | 2.74* (2.28, 3.20) | 3.38* (2.84, 3.91) | 2.95* (2.13, 3.78) | 1.26* (0.35, 2.18) | 3.04* (1.84, 4.24) |
| FIPR (one-unit decrement) | 0.74* (0.57, 0.90) | 0.63* (0.53, 0.72) | 0.72* (0.60, 0.84) | 0.66* (0.48, 0.85) | 0.31* (0.10, 0.53) | 0.58* (0.33, 0.83) |
| FIPR | ||||||
| ≥3.00 (ref) | − | − | − | − | − | − |
| 2.00 – < 3.00 | 1.43* (0.70, 2.15) | 1.02* (0.47, 1.56) | 1.22* (0.64, 1.81) | 0.98* (0.19, 1.76) | 0.31 (−0.54, 1.16) | 1.68* (0.23, 3.14) |
| 1.39 – < 2.00 | 1.83* (1.14, 2.52) | 1.39* (0.92, 1.87) | 1.70* (1.03, 2.36) | 1.16* (0.31, 2.00) | 0.69 (−0.28, 1.66) | 0.47 (−0.79, 1.72) |
| 1.00 – < 1.39 | 2.56* (1.84, 3.29) | 2.34* (1.78, 2.90) | 2.92* (2.23, 3.60) | 2.29* (1.25, 3.33) | 0.66 (−0.19, 1.50) | 1.63* (0.31, 2.94) |
| < 1.00 | 2.66* (1.87, 3.46) | 2.58* (2.01, 3.14) | 2.80* (2.06, 3.54) | 2.78* (1.85, 3.71) | 1.18* (0.21, 2.15) | 2.96* (1.55, 4.36) |
| Education | ||||||
| College Graduate+ (ref) | − | − | − | − | − | − |
| Some College | 2.13* (1.62, 2.64) | 1.03* (0.75, 1.31) | 1.35* (0.98, 1.73) | 1.97* (1.35, 2.59) | 0.85* (0.03, 1.66) | 1.72* (0.92, 2.52) |
| High School Graduate | 2.17* (1.52, 2.81) | 1.65* (1.32, 1.98) | 1.70* (1.29, 2.12) | 1.70* (0.88, 2.52) | 0.92* (0.25, 1.60) | 1.56* (0.44, 2.69) |
| < High School | 3.37* (2.59, 4.14) | 3.13* (2.60, 3.66) | 3.41* (2.60, 4.22) | 3.21* (2.40, 4.02) | 1.71* (0.91, 2.50) | 3.46* (2.14, 4.78) |
a. Model 3: Adjusted for age, sex (in race/ethnicity models), race/ethnicity (in sex models), marital status, and insurance status.
Statistically significant (p-value < 0.05).
3.2. Differences by race/ethnicity
The association between annual income, FIPR, and education with ASCVD risk also differed by race/ethnicity (interaction p-value < 0.1). For example, from fully adjusted models, each one-unit increment in FIPR was associated with greater ASCVD risk score by: 0.72 % (95 % CI: 0.60, 0.84) among White adults; 0.66 % (95 % CI: 0.48, 0.85) among Black adults; and 0.31 % (95 % CI: 0.10, 0.53) among Hispanic adults. Compared to college graduates, less than a high school education was associated with greater ASCVD risk score by: 3.41 % (95 % CI: 2.60, 4.22) among White adults; 3.21 % (95 % CI: 2.40, 4.02) among Black adults; and 1.71 % (95 % CI: 0.91, 2.50) among Hispanic adults.
4. Discussion
In a nationally representative study of US adults without a history of CVD, SES, specifically less educational attainment and lower income, were strongly associated with greater ASCVD risk, with differential associations by sex and race/ethnicity. While there were strong graded associations between SES and ASCVD risk in all groups, associations were more pronounced among men compared to women and less pronounced among Hispanic adults compared with other race/ethnic groups. Taken together, these findings emphasize that SDOH are strong predictors of ASCVD risk but the association between SES and ASCVD risk varies by demographic factors. In conjunction with the ACC’s recent study highlighting that pooled cohort equations for ASCVD underpredict risk in low SES populations (Lloyd-Jones et al., 2019), our findings emphasize the importance of SDOH as a major risk factor for CVD. Furthermore, the AHA’s novel Predicting Risk of cardiovascular disease EVENTs (PREVENT) score contains an optional variable for the prediction of social deprivation but emphasizes the need for more individual-level information related to SDOH, as described within this work (Khan et al., 2023).
We found that high school attainment compared with college graduation and an income of $75 K or higher compared to less than $25 K were both associated with a 3 % greater 10-year risk of an ASCVD event. These findings of strong graded associations between lower educational attainment/income with increasing ASCVD risk are consistent with other studies (Woodward et al., 2015). A recent meta-analysis by Wang et al. (2023) found that the risk of CVD incidence in low-income groups was 22 % higher than that in high-income groups across 21 included studies. Further, across 10 studies, CVD incidence was 44 % higher in the low education groups when compared to high education groups (Wang et al., 2023). However, Zhang et al. found in a study of both NHANES and the UK Biobank that lifestyle factors only mediated a small proportion of socioeconomic inequity in cardiovascular health (Zhang et al., 2021). These studies emphasize that SDOH are indeed fundamental drivers of poor health. For example, adjustment for lifestyle factors assessed by life’s simple 7 score, now life’s essential 8, only slightly attenuated the association between SES and ASCVD risk in another study of NHANES participants (Shen et al., 2022). In fact, some studies have suggested that even at best, traditional CVD risk factors can account for only 15–30 percent of the relationship between SES with CVD mortality (Marmot et al., 1984, Bhatnagar, 2017, Henderson et al., 2022).
Associations between SDOH and ASCVD risk differed by sex. We found that the associations between both annual income and FIPR with ASCVD risk were stronger among men compared with women. This is in direct contrast to prior studies which have shown stronger associations between lower income and adverse health outcomes among women. For example, Backholer et al. found in a meta-analysis conducted in 2017 that the association between CVD and SES was significantly stronger amongst women in comparison with men even when controlling for conventional CVD risk factors (Backholer et al., 2017). Guma et al. hypothesized that gender inequalities across western society mean that SDOH differentially affect health in men and women, with low SES women faring worse on average in comparison with low SES men (Gumà et al., 2019). Consequently, a better understanding sex differences in CVD risk across the spectrum of socioeconomic groups must be elucidated.
In addition to sex differences, we found that the association between SDOH and ASCVD risk was less pronounced among Hispanic adults compared with other race/ethnic groups. For example, each one-unit decrement in FIPR was associated with increased ASCVD risk by 0.72 % among non-Hispanic White adults, 0.66 % among non-Hispanic Black adults, and 0.31 % among Hispanic adults. These findings are in line with recent studies evaluating the relationship between SES with cardiovascular risk factors in Hispanic/Latino communities (Sorlie et al., 2014). For example, Lopez-Cevallos et al. found no change in the prevalence of hypertension or diabetes with increasing SES in the Hispanic Community Health Study/Study of Latinos in fully adjusted models (López-Cevallos et al., 2018). Likewise, as has been highlighted and termed the “Hispanic Paradox” (Ruiz et al., 2013), Hispanic adults have lower all-cause mortality rates than non-Hispanic White adults despite being disproportionately burdened by low SES (Khambaty et al., 2020, Morales et al., 2002) and with higher rates of unhealthy behaviors (Lloyd-Jones et al., 2022, Lloyd-Jones et al., 2022). Indeed, in our study, Hispanic adults had higher ASCVD risk than their White counterparts as shown in Fig. 1. These counterintuitive observations may be explained by several potential factors. First, and importantly, the Framingham risk factors from which ASCVD risk is derived came from a cohort that underrepresented Hispanics and “normal” values of cholesterol and BMI may vary between groups. Further, the well-described concept of Hispanic resilience suggests that cultural values engender larger and stronger social networks which can buffer health challenges (Gallo et al., 2009, Ruiz et al., 2016). Previous reviews by Cortes-Bergoderi et al. and Ruiz et al. have supported this concept by showing lower all-cause and CVD mortality in Hispanics despite having worse risk factor profiles (Ruiz et al., 2013, Balfour et al., 2016, Cortes-Bergoderi et al., 2013). Our findings are consistent with such studies showing a less pronounced association between SES and ASCVD risk compared with other racial/ethnic groups.
There are many potential pathways by which SDOH exert influence on health. SDOH confer resources such as: improved health literacy, positive social relationships, healthier foods, guaranteed transportation, lower chronic stress levels, safe communities, and improved local environmental factors (Bhatnagar, 2017, Hicken et al., 2014, Schilbach et al., 2016). These factors also contribute to the well-studied phenomena of biological weathering. Weathering refers to the effects of chronic stress and other SDOH on biological aging (Das, 2013). Forrester et al., in a longitudinal study of young adults, found that after multivariable adjustment, lower SES was associated with increased biological aging, especially in black adults (Forrester et al., 2019). Thus, groups of low SES are not only more likely to have higher ASCVD risk, but are also more likely to progress to a worse disease state. Given these findings, early and accurate risk prediction are ever more important.
4.1. Limitations
This study is not without limitations. First, due the cross-sectional nature of NHANES, we were not able to establish temporality or assess the associations between life-course income changes with ASCVD risk. Further, we could not calculate incident CVD, so we were unable to assess accuracy of ASCVD risk prediction across SES strata. However, the mitigating fact remains that specific measures of SES such as education are usually established in early adulthood, prior to the development of ASCVD risk. Other limitations inherent to large cross sectional studies (Idler et al., 2000) include self-report of SES and medication use (for the calculation of ASCVD risk). Moreover, we could not assess the association between ASCVD risk and SES in other minority populations such as Asians because of lack of data. Further, the ASCVD risk calculator is built using parameters applicable to white and black adults; therefore, the absence of additional race or ethnic-specific risk algorithms limits our understanding of ASCVD risk in these populations. While our study follows ACC/AHA guidelines in application of non-Hispanic white equations for these participants, there is still potential for risk overestimation (Goff et al., 2014). Regardless of these potential gaps, our study maintains notable strengths, including a diverse and representative sample of US adults, utilization of standardized measurements of ASCVD risk, and focus on multiple SES factors. While previous studies have commented on the association between SES and ASCVD in the US population, our study is the largest and most up to date.
5. Conclusions
In conclusion, in an analysis representative of the broader US population, we found significant associations between lower annual family income and educational attainment with higher ten-year risk of ASCVD. As presented, these associations were found in both overall and stratified models with differential associations by sex and race/ethnicity. These findings confirm socioeconomic levels – represented by annual family income and education – allow detection of individuals at higher risk of CVD and provide a basis for additional targeted research and management.
Credit authorship contribution statement
Julien O. Tremblay: Writing – review & editing, Writing – original draft, Visualization, Methodology, Formal analysis, Conceptualization. Lauren Nahodyl: Writing – review & editing, Formal analysis, Conceptualization. Robert A. Mesa: Writing – review & editing, Methodology, Formal analysis. Lilliana Vilchez: Writing – review & editing. Tali Elfassy: Writing – review & editing, Supervision, Methodology, Formal analysis, Conceptualization.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
None.
Disclosure of Funding and Conflicts of Interests
Tali Elfassy, PhD is funded by NIH/NIMHD (K01MD014158). Robert A Mesa is funded by NIH/NHLBI (5T32HL007426-45) and the American Heart Association (24DECCADG1285241). All authors confirm they have no conflict of interest.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.pmedr.2024.102720.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
Data availability
Data will be made available on request.
References
- Abdalla S.M., Yu S., Galea S. Trends in cardiovascular disease prevalence by income level in the United States. JAMA Netw. Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.18150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Backholer K., Peters S.A.E., Bots S.H., Peeters A., Huxley R.R., Woodward M. Sex differences in the relationship between socioeconomic status and cardiovascular disease: A systematic review and meta-analysis. J. Epidemiol. Community Health. 2017;71:550–557. doi: 10.1136/jech-2016-207890. [DOI] [PubMed] [Google Scholar]
- Balfour P.C., Jr., Ruiz J.M., Talavera G.A., Allison M.A., Rodriguez C.J. Cardiovascular disease in Hispanics/Latinos in the United States. J. Lat. Psychol. 2016;4:98–113. doi: 10.1037/lat0000056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bello N.A., Merz C.N.B., Cheng S. A scientific imperative as seen through a sharpened lens: Sex, gender, and the cardiovascular condition. Circ. Res. 2022;130:433–435. doi: 10.1161/CIRCRESAHA.122.320825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhatnagar A. Environmental determinants of cardiovascular disease. Circ. Res. 2017;121:162–180. doi: 10.1161/CIRCRESAHA.117.306458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braveman P., Gottlieb L. The social determinants of health: It's time to consider the causes of the causes. Public Health Rep. 2014;129(Suppl 2):19–31. doi: 10.1177/00333549141291S206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewer L.C., Redmond N., Slusser J.P., Scott C.G., Chamberlain A.M., Djousse L., Patten C.A., Roger V.L., Sims M. Stress and achievement of cardiovascular health metrics: The American Heart Association life's simple 7 in Blacks of the Jackson Heart Study. J. Am. Heart Assoc. 2018;7 doi: 10.1161/JAHA.118.008855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CDC. National Health and Nutrition Examination Survey. 2001–2002 Data Documentation, Codebook, and Frequencies (Cholesterol). 2010; 2023.
- Chen T.C., Parker J.D., Clark J., Shin H.C., Rammon J.R., Burt V.L. National health and nutrition examination survey: Estimation procedures, 2011–2014. Vital Health Stat. 2018;2:1–26. [PubMed] [Google Scholar]
- Chen T.C., Clark J., Riddles M.K., Mohadjer L.K., Fakhouri T.H.I. National health and nutrition examination survey, 2015–2018: Sample design and estimation procedures. Vital Health Stat. 2020;2:1–35. [PubMed] [Google Scholar]
- Cortes-Bergoderi M., Goel K., Murad M.H., Allison T., Somers V.K., Erwin P.J., Sochor O., Lopez-Jimenez F. Cardiovascular mortality in Hispanics compared to non-Hispanic whites: A systematic review and meta-analysis of the Hispanic paradox. Eur. J. Intern. Med. 2013;24:791–799. doi: 10.1016/j.ejim.2013.09.003. [DOI] [PubMed] [Google Scholar]
- Curtin L.R., Mohadjer L.K., Dohrmann S.M., Montaquila J.M., Kruszan-Moran D., Mirel L.B., Carroll M.D., Hirsch R., Schober S., Johnson C.L. The national health and nutrition examination survey: Sample design, 1999–2006. Vital Health Stat. 2012;2:1–39. [PubMed] [Google Scholar]
- Das A. How does race get “under the skin”?: Inflammation, weathering, and metabolic problems in late life. Soc. Sci. Med. 2013;77:75–83. doi: 10.1016/j.socscimed.2012.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Brey, C., Musu, L., McFarland, .J, Wilkinson-Flicker, S., Diliberti, M., Zhang, A., Branstetter, C., Wang, X. 2019. Status and trends in the education of racial and ethnic groups 2018. Nces 2019-038. National Center for Education Statistics.
- Forrester S., Jacobs D., Zmora R., Schreiner P., Roger V., Kiefe C.I. Racial differences in weathering and its associations with psychosocial stress: The cardia study. SSM Popul. Health. 2019;7:3. doi: 10.1016/j.ssmph.2018.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Framke E., Sørensen J.K., Andersen P.K., Svane-Petersen A.C., Alexanderson K., Bonde J.P., Farrants K., Flachs E.M., Hanson L.L.M., Nyberg S.T., et al. Contribution of income and job strain to the association between education and cardiovascular disease in 1.6 million Danish employees. Eur. Heart J. 2020;41:1164–1178. doi: 10.1093/eurheartj/ehz870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallo L.C., Penedo F.J., Espinosa de los Monteros K., Arguelles W. Resiliency in the face of disadvantage: Do Hispanic cultural characteristics protect health outcomes? J. Pers. 2009;77:1707–1746. doi: 10.1111/j.1467-6494.2009.00598.x. [DOI] [PubMed] [Google Scholar]
- Gao Y., Shah L.M., Ding J., Martin S.S. Us trends in cholesterol screening, lipid levels, and lipid-lowering medication use in us adults, 1999 to 2018. J. Am. Heart Assoc. 2023;12 doi: 10.1161/JAHA.122.028205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gasevic D., Ross E.S., Lear S.A. Ethnic differences in cardiovascular disease risk factors: A systematic review of North American evidence. Can. J. Cardiol. 2015;31:1169–1179. doi: 10.1016/j.cjca.2015.06.017. [DOI] [PubMed] [Google Scholar]
- Gebreab S.Y., Diez Roux A.V., Brenner A.B., Hickson D.A., Sims M., Subramanyam M., Griswold M.E., Wyatt S.B., James S.A. The impact of life course socioeconomic position on cardiovascular disease events in African Americans: The Jackson Heart Study. J. Am. Heart Assoc. 2015;4 doi: 10.1161/JAHA.114.001553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goff D.C., Jr., Lloyd-Jones D.M., Bennett G., Coady S., D'Agostino R.B., Gibbons R., Greenland P., Lackland D.T., Levy D., O'Donnell C.J., et al. 2013 acc/aha guideline on the assessment of cardiovascular risk: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129:S49–S73. doi: 10.1161/01.cir.0000437741.48606.98. [DOI] [PubMed] [Google Scholar]
- Goff D.C., Lloyd-Jones D.M., Bennett G., Coady S., D’Agostino R.B., Gibbons R., Greenland P., Lackland D.T., Levy D., O’Donnell C.J., et al. 2013 acc/aha guideline on the assessment of cardiovascular risk. J. Am. Coll. Cardiol. 2014;63:2935–2959. doi: 10.1016/j.jacc.2013.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grundy S.M., Stone N.J., Bailey A.L., Beam C., Birtcher K.K., Blumenthal R.S., Braun L.T., de Ferranti S., Faiella-Tommasino J., Forman D.E., et al. 2018 aha/acc/aacvpr/aapa/abc/acpm/ada/ags/apha/aspc/nla/pcna guideline on the management of blood cholesterol: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;139:e1082–e1143. doi: 10.1161/CIR.0000000000000625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gumà J., Solé-Auró A., Arpino B. Examining social determinants of health: The role of education, household arrangements and country groups by gender. BMC Public Health. 2019;19 doi: 10.1186/s12889-019-7054-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamad R., Nguyen T.T., Bhattacharya J., Glymour M.M., Rehkopf D.H. Educational attainment and cardiovascular disease in the United States: A quasi-experimental instrumental variables analysis. PLoS Med. 2019;16 doi: 10.1371/journal.pmed.1002834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henderson K., Kaufman B., Rotter J.S., Stearns S., Sueta C.A.A., Foraker R., Ho P.M., Chang P.P. Socioeconomic status and modification of atherosclerotic cardiovascular disease risk prediction: Epidemiological analysis using data from the atherosclerosis risk in communities study. BMJ Open. 2022;12 doi: 10.1136/bmjopen-2021-058777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hicken M.T., Lee H., Morenoff J., House J.S., Williams D.R. Racial/ethnic disparities in hypertension prevalence: Reconsidering the role of chronic stress. Am. J. Public Health. 2014;104:117–123. doi: 10.2105/AJPH.2013.301395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Humphries K.H., Izadnegahdar M., Sedlak T., Saw J., Johnston N., Schenck-Gustafsson K., Shah R.U., Regitz-Zagrosek V., Grewal J., Vaccarino V., et al. Sex differences in cardiovascular disease - Impact on care and outcomes. Front. Neuroendocrinol. 2017;46:46–70. doi: 10.1016/j.yfrne.2017.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Idler E.L., Russell L.B., Davis D. Survival, functional limitations, and self-rated health in the nhanes i epidemiologic follow-up study, 1992. Am. J. Epidemiol. 2000;152:874–883. doi: 10.1093/aje/152.9.874. [DOI] [PubMed] [Google Scholar]
- Kaplan G.A., Keil J.E. Socioeconomic factors and cardiovascular disease: A review of the literature. Circulation. 1993;88:1973–1998. doi: 10.1161/01.cir.88.4.1973. [DOI] [PubMed] [Google Scholar]
- Kathryn B., Sanne A.E.P., Sophie H.B., Anna P., Rachel R.H., Mark W. Sex differences in the relationship between socioeconomic status and cardiovascular disease: A systematic review and meta-analysis. J. Epidemiol. Commun. Health. 2017;71 doi: 10.1136/jech-2016-207890. [DOI] [PubMed] [Google Scholar]
- Kelli H.M., Mehta A., Tahhan A.S., Liu C., Kim J.H., Dong T.A., Dhindsa D.S., Ghazzal B., Choudhary M.K., Sandesara P.B., et al. Low educational attainment is a predictor of adverse outcomes in patients with coronary artery disease. J. Am. Heart Assoc. 2019;8 doi: 10.1161/JAHA.119.013165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khambaty T., Schneiderman N., Llabre M.M., Elfassy T., Moncrieft A.E., Daviglus M., Talavera G.A., Isasi C.R., Gallo L.C., Reina S.A., et al. Elucidating the multidimensionality of socioeconomic status in relation to metabolic syndrome in the Hispanic community health study/study of Latinos (hchs/sol) Int. J. Behav. Med. 2020;27:188–199. doi: 10.1007/s12529-020-09847-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khan S.S., Coresh J., Pencina M.J., Ndumele C.E., Rangaswami J., Chow S.L., Palaniappan L.P., Sperling L.S., Virani S.S., Ho J.E., et al. Novel prediction equations for absolute risk assessment of total cardiovascular disease incorporating cardiovascular-kidney-metabolic health: A scientific statement from the American Heart Association. Circulation. 2023;148:1982–2004. doi: 10.1161/CIR.0000000000001191. [DOI] [PubMed] [Google Scholar]
- Lamprea-Montealegre J.A., Shlipak M.G., Estrella M.M. Chronic kidney disease detection, staging and treatment in cardiovascular disease prevention. Heart. 2021;107 doi: 10.1136/heartjnl-2020-318004. [DOI] [PubMed] [Google Scholar]
- Lin Y., Monnette A., Shi L. Effects of medicaid expansion on poverty disparities in health insurance coverage. Int. J. Equity Health. 2021;20:171. doi: 10.1186/s12939-021-01486-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindley Kathryn J., Aggarwal Niti R., Briller Joan E., Davis Melinda B., Douglass P., Epps Kelly C., Fleg Jerome L., Hayes S., Itchhaporia D., Mahmoud Z., et al. Socioeconomic determinants of health and cardiovascular outcomes in women. J. Am. Coll. Cardiol. 2021;78:1919–1929. doi: 10.1016/j.jacc.2021.09.011. [DOI] [PubMed] [Google Scholar]
- Lloyd-Jones D., Adams R., Carnethon M., De Simone G., Ferguson T.B., Flegal K., Ford E., Furie K., Go A., Greenlund K., et al. Heart disease and stroke statistics–2009 update: A report from the American Heart Association statistics committee and stroke statistics subcommittee. Circulation. 2009;119:480–486. doi: 10.1161/CIRCULATIONAHA.108.191259. [DOI] [PubMed] [Google Scholar]
- Lloyd-Jones D.M., Braun L.T., Ndumele C.E., Smith S.C., Sperling L.S., Virani S.S., Blumenthal R.S. Use of risk assessment tools to guide decision-making in the primary prevention of atherosclerotic cardiovascular disease: A special report from the American Heart Association and American College of Cardiology. Circulation. 2019;139:e1162–e1177. doi: 10.1161/CIR.0000000000000638. [DOI] [PubMed] [Google Scholar]
- Lloyd-Jones D.M., Ning H., Labarthe D., Brewer L., Sharma G., Rosamond W., Foraker R.E., Black T., Grandner M.A., Allen N.B., et al. Status of cardiovascular health in us adults and children using the American Heart Association’s new “life’s essential 8” metrics: Prevalence estimates from the National Health and Nutrition Examination Survey (nhanes), 2013 through 2018. Circulation. 2022;146:822–835. doi: 10.1161/CIRCULATIONAHA.122.060911. [DOI] [PubMed] [Google Scholar]
- Lloyd-Jones D.M., Allen N.B., Anderson C.A.M., Black T., Brewer L.C., Foraker R.E., Grandner M.A., Lavretsky H., Perak A.M., Sharma G., et al. Life’s essential 8: Updating and enhancing the American Heart Association’s construct of cardiovascular health: A presidential advisory from the American Heart Association. Circulation. 2022;146:e18–e43. doi: 10.1161/CIR.0000000000001078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- López-Cevallos D.F., Gonzalez P., Bethel J.W., Castañeda S.F., Isasi C.R., Penedo F.J., Ojeda L., Davis S.M., Chirinos D.A., Molina K.M., et al. Is there a link between wealth and cardiovascular disease risk factors among Hispanic/Latinos? Results from the hchs/sol sociocultural ancillary study. Ethn. Health. 2018;23:902–913. doi: 10.1080/13557858.2017.1315370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marmot M.G., Shipley M.J., Rose G. Inequalities in death–specific explanations of a general pattern? Lancet. 1984;1:1003–1006. doi: 10.1016/s0140-6736(84)92337-7. [DOI] [PubMed] [Google Scholar]
- Mirel L.B., Mohadjer L.K., Dohrmann S.M., Clark J., Burt V.L., Johnson C.L., Curtin L.R. National health and nutrition examination survey: Estimation procedures, 2007–2010. Vital Health Stat. 2013;2:1–17. [PubMed] [Google Scholar]
- Morales L.S., Lara M., Kington R.S., Valdez R.O., Escarce J.J. Socioeconomic, cultural, and behavioral factors affecting Hispanic health outcomes. J. Health Care Poor Underserved. 2002;13:477–503. doi: 10.1177/104920802237532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mosca L., Barrett-Connor E., Wenger N.K. Sex/gender differences in cardiovascular disease prevention: What a difference a decade makes. Circulation. 2011;124:2145–2154. doi: 10.1161/CIRCULATIONAHA.110.968792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCHS. Nhanes Questionnaires, Datasets, and Related Documentation.
- Ruiz J.M., Steffen P., Smith T.B. Hispanic mortality paradox: A systematic review and meta-analysis of the longitudinal literature. Am. J. Public Health. 2013;103:e52–e60. doi: 10.2105/AJPH.2012.301103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruiz J.M., Campos B., Garcia J.J. Special issue on Latino physical health: Disparities, paradoxes, and future directions. J. Latina/o Psychol. 2016;4:61–66. [Google Scholar]
- Schilbach F., Schofield H., Mullainathan S. The psychological lives of the poor. Am. Econ. Rev. 2016;106:435–440. doi: 10.1257/aer.p20161101. [DOI] [PubMed] [Google Scholar]
- Schultz W.M., Kelli H.M., Lisko J.C., Varghese T., Shen J., Sandesara P., Quyyumi A.A., Taylor H.A., Gulati M., Harold J.G., et al. Socioeconomic status and cardiovascular outcomes: Challenges and interventions. Circulation. 2018;137:2166–2178. doi: 10.1161/CIRCULATIONAHA.117.029652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schultz W.M., Kelli H.M., Lisko J.C., Varghese T., Shen J., Sandesara P., Quyyumi A.A., Taylor H.A., Gulati M., Harold J.G., et al. Socioeconomic status and cardiovascular outcomes. Circulation. 2018;137:2166–2178. doi: 10.1161/CIRCULATIONAHA.117.029652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Services USDoHaH. Prior hhs Poverty Guidelines and Federal Register References. 2018; 2024.
- Shen R., Zhao N., Wang J., Guo P., Shen S., Liu D., Liu D., Zou T. Association between socioeconomic status and arteriosclerotic cardiovascular disease risk and cause-specific and all-cause mortality: Data from the 2005–2018 National Health and Nutrition Examination Survey. Front. Public Health. 2022;10 doi: 10.3389/fpubh.2022.1017271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sorlie P.D., Allison M.A., Avilés-Santa M.L., Cai J., Daviglus M.L., Howard A.G., Kaplan R., Lavange L.M., Raij L., Schneiderman N., et al. Prevalence of hypertension, awareness, treatment, and control in the Hispanic community health study/study of Latinos. Am. J. Hypertens. 2014;27:793–800. doi: 10.1093/ajh/hpu003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stringhini S., Carmeli C., Jokela M., Avendaño M., Muennig P., Guida F., Ricceri F., d'Errico A., Barros H., Bochud M., et al. Socioeconomic status and the 25 × 25 risk factors as determinants of premature mortality: A multicohort study and meta-analysis of 1·7 million men and women. Lancet. 2017;389:1229–1237. doi: 10.1016/S0140-6736(16)32380-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsao C.W., Aday A.W., Almarzooq Z.I., Alonso A., Beaton A.Z., Bittencourt M.S., Boehme A.K., Buxton A.E., Carson A.P., Commodore-Mensah Y., et al. Heart disease and stroke statistics-2022 update: A report from the American Heart Association. Circulation. 2022;145:e153–e639. doi: 10.1161/CIR.0000000000001052. [DOI] [PubMed] [Google Scholar]
- Wang T., Li Y., Zheng X. Association of socioeconomic status with cardiovascular disease and cardiovascular risk factors: A systematic review and meta-analysis. J. Public Health. 2023 doi: 10.1007/s10389-023-01825-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wenger N.K., Lloyd-Jones D.M., Elkind M.S.V., Fonarow G.C., Warner J.J., Alger H.M., Cheng S., Kinzy C., Hall J.L., Roger V.L., et al. Call to action for cardiovascular disease in women: Epidemiology, awareness, access, and delivery of equitable health care: A presidential advisory from the American Heart Association. Circulation. 2022;145:e1059–e1071. doi: 10.1161/CIR.0000000000001071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whelton P.K., Carey R.M., Aronow W.S., Casey D.E., Collins K.J., Himmelfarb C.D., DePalma S.M., Gidding S., Jamerson K.A., Jones D.W., et al. 2017 acc/aha/aapa/abc/acpm/ags/apha/ash/aspc/nma/pcna guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: A report of the American College Of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71:e13–e115. doi: 10.1161/HYP.0000000000000065. [DOI] [PubMed] [Google Scholar]
- Woodward M. Cardiovascular disease and the female disadvantage. Int. J. Environ. Res. Public Health. 2019;16 doi: 10.3390/ijerph16071165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woodward M., Peters S.A.E., Batty G.D., Ueshima H., Woo J., Giles G.G., Barzi F., Ho S.C., Huxley R.R., Arima H., et al. Socioeconomic status in relation to cardiovascular disease and cause-specific mortality: A comparison of Asian and Australasian populations in a pooled analysis. BMJ Open. 2015;5 doi: 10.1136/bmjopen-2014-006408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y.-B., Chen C., Pan X.-F., Guo J., Li Y., Franco O.H., Liu G., Pan A. Associations of healthy lifestyle and socioeconomic status with mortality and incident cardiovascular disease: Two prospective cohort studies. BMJ. 2021;373 doi: 10.1136/bmj.n604. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data will be made available on request.