Abstract
Background:
Opioid overdose deaths have continued to rise in Tennessee (TN) with fentanyl emerging as a major contributor. Current data are needed to identify at-risk populations to guide prevention strategies. We conducted a large statewide observational study among TN adult decedents (2013–2016) to evaluate the association of sociodemographic factors and prescribing patterns with opioid overdose deaths.
Methods:
Among drug overdose decedents identified using death certificate data (n=5,483), we used logistic regression to estimate adjusted odds ratios and 95% confidence intervals for characteristics associated with prescription opioid (PO) (excluding fentanyl), fentanyl, and heroin alone overdoses. Among decedents linked to TN’s Prescription Drug Monitoring Database using deterministic algorithms, we obtained prescription history in the year before death (n=3,971), which was evaluated by type of overdose using descriptive statistics.
Results:
Younger, non-White decedents had lower odds of PO overdose, while females and benzodiazepines as a contributing cause were associated with increased odds of PO overdose. Younger age, Non-Hispanic Black race/ethnicity, greater than high school education, and cocaine/other stimulants as a contributing cause were associated with increased odds of fentanyl or heroin overdoses. Over 55% of PO, 39.2% of fentanyl, and 20.7% of heroin overdoses had an active opioid prescription at death. For PO, fentanyl, and heroin decedents, respectively, 46.0%, 30.5%, and 26.2% had an active prescription for benzodiazepines at death.
Conclusions:
Prescription opioid overdose deaths were associated with different sociodemographic profiles and prescribing history compared to fentanyl and heroin overdose deaths in TN. Data can guide prevention strategies to reduce opioid overdose mortality.
Keywords: Drug Overdose, Drug Mortality, Prescription Drugs, Fentanyl, Heroin, Benzodiazepines
1. Introduction
Drug overdose deaths in the US have been increasing since 1999, with an age-adjusted rate of 6.1 per 100,000 in 1999 and 16.3 per 100,000 in 2015 (Hedegaard et al., 2017; Rudd et al., 2016). Increases in all drug overdose deaths have occurred across all age groups, with the highest rates among ages 45–54 years (Hedegaard et al., 2017). Opioid overdose deaths have also increased, with substantial elevations since 2013 for heroin and synthetic opioids (excluding methadone) regardless of sex, age, and race/ethnicity (Rudd et al., 2016).
In Tennessee (TN), the age-adjusted rate of overdose deaths increased from 18.2 per 100,000 in 2010 to 24.6 per 100,000 in 2016. Fentanyl, a synthetic opioid known to be manufactured illegally (illicitly manufactured fentanyl (IMF)) (Peterson et al., 2016), has emerged as a major contributor to opioid overdose deaths in TN, with 7.0% and 24.8% of opioid deaths involving fentanyl in 2013 and 2016, respectively. Similarly, heroin deaths rose from 8.4% to 21.9% of opioid deaths in 2012 and 2016, respectively. The age-adjusted rate of opioid and benzodiazepine deaths has continued to rise (3.1 per 100,000 in 2010; 8.1 per 100,000 in 2016), which is particularly concerning given the known harmful interaction of combined opioid and benzodiazepines on respiration (Garg et al., 2017; Volkow and McLellan, 2016),
Prescription Drug Monitoring Programs (PDMPs), now implemented in all 50 states, collect data on controlled substance prescriptions, prescribers, and dispensers. Some studies have shown the implementation of PDMPs has resulted in reduced opioid mortality and prescribing, although data are not consistent with comparisons hampered by differences in state-specific policies (Pardo 2017; Patrick et al., 2016; Suffoletto et al., 2018). Several decedent-only/crosssectional studies have linked PDMP and mortality data to understand characteristics of opioid deaths (Austin et al., 2017; Hall et al., 2008; Lev et al., 2015; Lev et al., 2016; Mercado et al., 2018; Paulozzi et al., 2009; Slavova et al., 2017a; Weimer et al., 2011). Further, many ecological and descriptive studies have evaluated the role of prescribing practices/behaviors and sociodemographic factors in overdose deaths (Cerda et al., 2013; Green et al., 2011; King et al., 2014). However, studies included data from earlier years, which may not reflect current trends as the drug epidemic in the US has shifted (Kolodny et al., 2015; Rudd et al., 2016), or were limited by small sample size and/or did not consider sociodemographic factors and prescribing history by contributing drugs. Data on sociodemographic factors and prescribing patterns by type of drug overdose death (e.g., prescription opioids, fentanyl, and heroin) are needed to guide development and implementation of education and intervention efforts. These include improved awareness of risk factors for prescription and illicit opioid overdoses to inform timely state policies and harm reduction strategies for clinical practice, and identification of high risk populations to target for community-based prevention programs that include overdose prevention training and take-home naloxone kits (Coffin et al., 2016; Fairbairn et al., 2017; Raffel et al., 2018; Starrels et al., 2011).
We conducted a statewide observational study among all drug overdose decedents aged ≥18 years during 2013–2016 in TN. Our specific objectives were: (1) to evaluate the associations of sociodemographic factors and multiple drug use with opioid overdose deaths and (2) to evaluate opioid and benzodiazepine prescription history by type of opioid overdose death.
2. Materials and Methods
2.1. Data Sources
2.1.1. TN Death Certificates (2013–2016).
TN’s death certificates provide data on cause of death (COD) and decedent characteristics for the TN death statistical files at the TN Department of Health (TDH). Deaths are coded according to the ICD-10 guidelines by the National Center for Health Statistics with an underlying COD (UCD) code and up to 20 additional multiple COD (MCOD) codes. Additional data collected on the death certificate includes name, address, date of birth (DOB), date of death, and sociodemographic information (e.g., sex, race, ethnicity, education, and marital status). The percent of deaths with unknown underlying COD (R99) was <1.0% during the study years.
2.1.2. TN’s Controlled Substance Monitoring Database (CSMD) (2012–2016).
In accordance with the Controlled Substance Monitoring Act of 2002, TDH established the CSMD in 2006 to monitor the dispensing of Schedule II, III, IV & V controlled substances with required reporting within seven days of dispensing effective January 1st, 2013 based on the TN Prescription Safety Act of 2012. This was changed to required reporting within 1 business day in the TN Prescription Safety Act of 2016 (Tennesee Department of Health, 2017). Controlled substances administered directly to a patient, as part of a narcotic treatment program registered by the U.S. Drug Enforcement Administration (DEA), or samples of a schedule IV (for treatment ≤ 3 days) or schedule V controlled substances (for treatment ≤ 14 days) do not have to be reported. Selected data items collected include patient name, address, and DOB, and prescriptions characteristics (e.g., national drug code, quality, days’ supply, date filled, payment type, prescriber DEA number, dispenser DEA number). Prescription data collected follow the American Society for Automation in Pharmacy standards for PDMPs, which are used by all states.
2.2. Study Design and Study Population
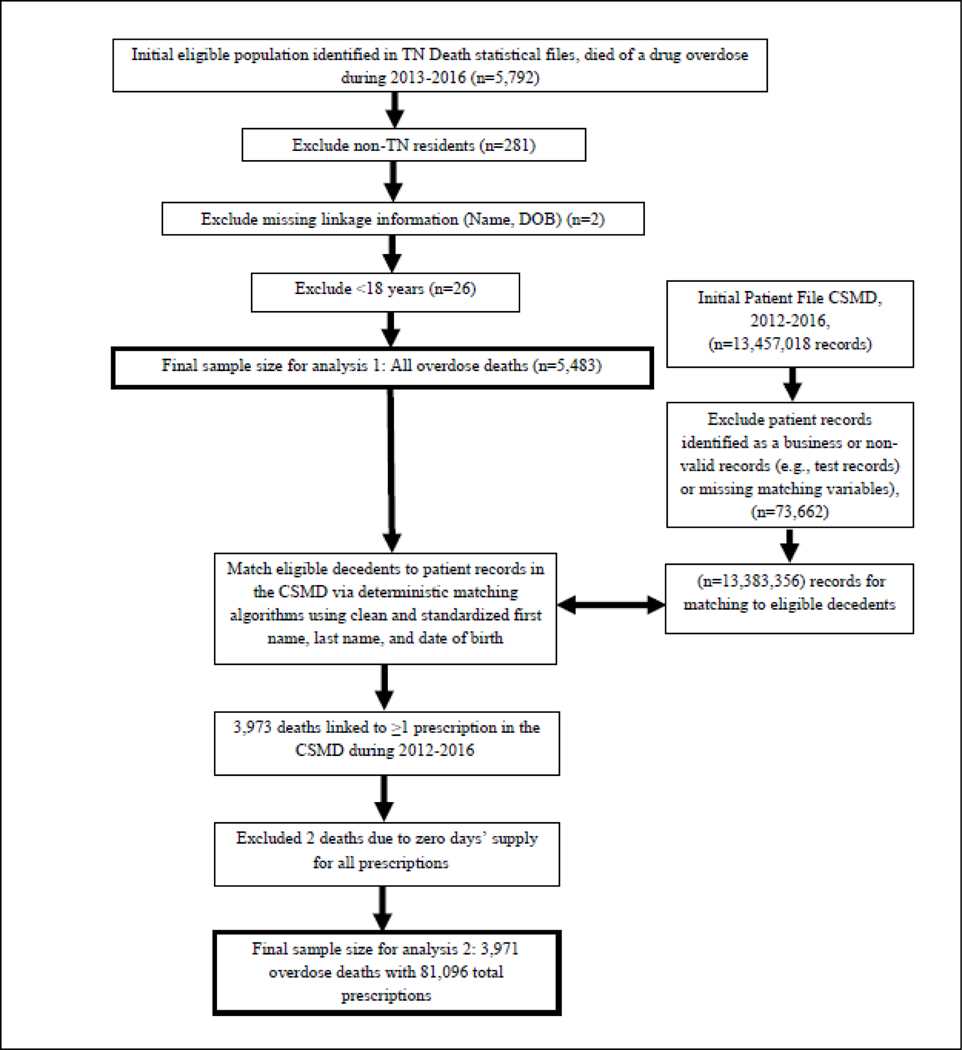
We conducted an observational population-based study among TN adult residents aged ≥18 years who died of a drug overdose between 2013 and 2016 (n=5,483). Eligible decedents had drug poisoning as their underlying COD (ICD-10 codes X40–X44; X60-X64; X85; Y10-Y14) (Rudd et al., 2016). To obtain prescription history in the year before death (Hall et al., 2008; Lev et al., 2015), decedents with ≥ one prescription record and at least one days’ supply were identified in the CSMD (n=3,971). Figure 1 provides information on the study population and exclusions. The study was approved by the TDH IRB.
Figure 1.
Study Design and Population: Data Linkage Methods, Exclusions, and Sample Size.
2.3. Drug Overdose Death Definitions
ICD-10 MCOD codes T40.0 to 40.6 were used for contributing CODs related to opioids, including any opioids (T40.1-T40.4, T40.6), prescription opioids excluding fentanyl (T40.2-T40.4), heroin (T40.1), fentanyl (identified via literal text searches in the MCOD text fields for the term “FENTAN” (Trinidad et al., 2016)), methadone (T40.3) and benzodiazepines (T42.4) (Rudd et al., 2016; Trinidad et al., 2016; Warner et al., 2016). Cocaine (T40.5), stimulants (T43.6), and alcohol (T51.0, T51.9) were included as contributing causes (Hedegaard et al., 2017; Kandel et al., 2017). Supplementary Table S1 describes the ICD-10 codes1. Drug overdose deaths may involve multiple contributing drugs and categories are not mutually exclusive unless indicated.
2.4. Sociodemographic Characteristics
Characteristics available in TN death certificate data included the following, categorized based on standard definitions and sample size considerations: age in years (18–24, 25–34, 35–44, 45–54, 55–64, 65–74, ≥75), race/ethnicity (Non-Hispanic White, Non-Hispanic Black, other Non-Hispanic, Hispanic), gender (male, female), marital status (married, divorced/separated, never married, widowed), education (<high school, high school, some college, ≥college), and place of death (TN hospital, TN jail, non-medical facility, private residence, out-of-state hospital, hospice, other residence, and nursing home) (Green et al., 2011; Siegler et al., 2014).
2.5. Data Linkage Strategy
Identifiers available for linkage in the CSMD included patient name and DOB. Data cleaning and standardization methods were applied to names in the CSMD (e.g., removing extra spaces, special characters, identifying and extracting prefixes and suffixes, and identifying names/text to be parsed into separate columns to enable linkage (e.g., “Samantha (Sam)”), described in detail here: (Golladay and Nechuta, 2018). Names in the death certificate file were similarly cleaned and standardized. A multi-step deterministic approach was used to link eligible overdose deaths to the CSMD patient file using multiple variations of first and last names (a patient may have >one record in the CSMD with a name variation), and DOB (see Figure 1).
We developed an approach to identify potential false positives (i.e., incorrect matches) by patient in the CSMD using manual review for a subset of cases with more than one name, including multiple first or last names or middle initial across patient records in the CSMD (n=2,598 records, 26.1%). The address was used to identify potential false positives among matched patient recordsets. The address was geocoded and standardized for both death and CSMD files using ArcGIS (ESRI, Redlands, CA). Among the 2,598 records, 76.3% matched on address across all available records for a patient, and of the remaining, 20.9% matched on full name via manual review, leaving 71 records with differing address information or non-match on full name (<1% of records), as potential false positives. As patients may move and address changes across a patient’s record in the CSMD are common over time, without additional identifying information (e.g., social security number), the possibility that these matches are incorrect cannot be excluded.
2.6. Prescription History in the CSMD
Prescription history in the year before death was collected for decedents linked to the CSMD. Information on class of drugs (opioids, benzodiazepines) was obtained from the CDC Conversion Reference Table, based on national drug code number (National Center for Injury Prevention and Control, 2016). Dichotomous variables were created for specific drug types in the CSMD for three-time frames (active at death, within 30 days of death, and within 90 days of death). Specific drug types included any opioid, fentanyl, hydrocodone, oxycodone, buprenorphine for medication-assisted treatment (MAT), and benzodiazepines. Active prescriptions at death were defined as having overlapping days’ supply with date of death (Slavova et al., 2017a). Total morphine milligram equivalents (MME) were calculated using strength × oral MME conversion factor × quantity. Number of prescribers and dispensers were calculated using prescriber and dispenser DEA number (Lev et al., 2016; Paulozzi et al., 2012). Payment type was collapsed into categories of cash, Medicare, and Medicaid to evaluate number of payments for an opioid prescription by these payment types.
2.7. Statistical Analysis
First, we calculated descriptive statistics for sociodemographic factors and contributing drugs among all drug overdose decedents (n=5,483, Figure 1). Based on literature review, we selected age, race/ethnicity, gender, place of death, marital status, and education level as characteristics potentially associated with drug overdose deaths (Green et al., 2011; Hall et al., 2008; King et al., 2014; Siegler et al., 2014). We estimated unadjusted and adjusted ORs and corresponding 95% CIs using binary logistic regression. We created three separate models for each of the primary outcomes: 1. deaths due to prescription drugs excluding fentanyl; 2. deaths due to fentanyl; and 3. deaths due to heroin). We also evaluated deaths due to a combination of opioids and benzodiazepines. The reference for all models was all other types of opioid deaths. Covariates, selected a priori and using statistical considerations (sample size, multicollinearity), included year of death, age, race/ethnicity, sex, and education (when not main effects of interest). Missing data for covariates (frequencies shown in Table 1) were excluded in adjusted models, results from a sensitivity analyses to include missing data via indicator variables were similar (Smith-Warner et al., 2006).
Table 1.
Sociodemographic characteristics among TN adult drug overdose decedents by contributing drugs, 2013–2016 (n=5,483)a
| All Overdoseb (n=5,483) | Opioid Overdosec (n=3,818) | Prescription Opioid Overdose (excluding fentanyl)d (n=2,594) | Fentanyl Overdosee (n=583) | Heroin Overdosef (n=674) | Methadone Overdoseg (n=303) | Opioid and Benzodiazepines Overdoseh (n=1,656) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | n | % | n | % | n | % | |
| Age at death | ||||||||||||||
| 18–24 | 322 | 5.9 | 242 | 6.3 | 118 | 4.6 | 66 | 11.3 | 68 | 10.1 | 10 | 3.3 | 99 | 6.0 |
| 25–34 | 1,030 | 18.8 | 833 | 21.8 | 477 | 18.4 | 182 | 31.2 | 224 | 33.2 | 66 | 21.8 | 373 | 22.5 |
| 35–44 | 1,271 | 23.2 | 948 | 24.8 | 654 | 25.2 | 140 | 24.0 | 172 | 25.5 | 99 | 32.7 | 428 | 25.9 |
| 45–54 | 1,610 | 29.4 | 1063 | 27.8 | 793 | 30.6 | 119 | 20.4 | 132 | 19.6 | 76 | 25.1 | 465 | 28.1 |
| 55–64 | 944 | 17.2 | 603 | 15.8 | 461 | 17.8 | 60 | 10.3 | 71 | 10.5 | 45 | 14.9 | 250 | 15.1 |
| 65–74 | 204 | 3.7 | 106 | 2.8 | 75 | 2.9 | 15 | 2.6 | 6 | 0.9 | 7 | 2.3 | 36 | 2.2 |
| ≥75 | 102 | 1.9 | 23 | 0.6 | 16 | 0.6 | 1 | 0.2 | 1 | 0.2 | 0 | 5 | 0.3 | |
| Race/ethnicity | ||||||||||||||
| Non-Hispanic White | 4,804 | 89.1 | 3425 | 91.2 | 2398 | 94.0 | 495 | 85.1 | 536 | 82.7 | 295 | 98.3 | 1504 | 91.6 |
| Non-Hispanic Black | 493 | 9.2 | 264 | 7.0 | 124 | 4.9 | 72 | 12.4 | 89 | 13.7 | 5 | 1.7 | 109 | 6.6 |
| Other Non-Hispanic | 24 | 0.5 | 18 | 0.5 | 8 | 0.3 | 4 | 0.7 | 6 | 0.9 | 0 | 6 | 0.4 | |
| Hispanic | 68 | 1.3 | 49 | 1.3 | 21 | 0.8 | 11 | 1.9 | 17 | 2.6 | 0 | 23 | 1.4 | |
| Missing | 94 | 62 | 43 | 1 | 26 | 3 | 14 | |||||||
| Gender | ||||||||||||||
| Male | 3,090 | 56.4 | 2195 | 57.5 | 1381 | 53.2 | 378 | 64.8 | 490 | 72.7 | 170 | 56.1 | 896 | 54.1 |
| Female | 2,393 | 43.6 | 1623 | 42.5 | 1213 | 46.8 | 205 | 35.2 | 184 | 27.3 | 133 | 43.9 | 760 | 45.9 |
| Place of death | ||||||||||||||
| Hospital | 2,186 | 40.0 | 1356 | 35.6 | 931 | 35.9 | 185 | 31.8 | 191 | 28.4 | 96 | 31.8 | 560 | 33.9 |
| Jail | 4 | 0.1 | 3 | 0.1 | 3 | 0.1 | 0 | 0 | 0 | 1 | 0.1 | |||
| Non-medical facility | 466 | 8.5 | 337 | 8.8 | 206 | 8.0 | 46 | 7.9 | 127 | 18.9 | 20 | 6.6 | 131 | 7.9 |
| Private residence | 2,360 | 43.1 | 1775 | 46.6 | 1246 | 48.1 | 290 | 49.9 | 263 | 39.1 | 166 | 55.0 | 822 | 49.7 |
| Out-of-state hospital | 60 | 1.1 | 33 | 0.9 | 20 | 0.8 | NA | 10 | 1.5 | 1 | 0.3 | 6 | 0.4 | |
| Hospice | 12 | 0.2 | 6 | 0.2 | 2 | 0.1 | 0 | 2 | 0.3 | 0 | 1 | 0.1 | ||
| Other residence | 363 | 6.6 | 288 | 7.6 | 176 | 6.8 | 56 | 9.6 | 78 | 11.6 | 19 | 6.3 | 126 | 7.6 |
| Nursing home | 21 | 0.4 | 13 | 0.3 | 7 | 0.3 | 4 | 0.7 | 1 | 0.2 | 7 | 0.4 | ||
| Missing | 11 | 7 | 3 | 2 | 2 | 1 | 2 | |||||||
| Marital status | ||||||||||||||
| Married | 1476 | 27.7 | 999 | 27.0 | 748 | 29.8 | 134 | 23.7 | 103 | 16.1 | 77 | 26.1 | 462 | 28.8 |
| Divorced/separated | 1,878 | 35.3 | 1290 | 34.9 | 935 | 37.2 | 150 | 26.6 | 187 | 29.2 | 118 | 40.0 | 535 | 33.4 |
| Never married | 1,618 | 30.4 | 1205 | 32.6 | 673 | 26.8 | 261 | 46.2 | 330 | 51.6 | 77 | 26.1 | 521 | 32.5 |
| Widowed | 348 | 6.5 | 200 | 5.4 | 158 | 6.3 | 20 | 3.5 | 20 | 3.1 | 23 | 7.8 | 86 | 5.4 |
| Missing | 163 | 124 | 80 | 18 | 34 | 8 | 52 | |||||||
| Education | ||||||||||||||
| <High school diploma | 1,339 | 24.8 | 936 | 24.9 | 686 | 26.8 | 108 | 18.8 | 135 | 20.5 | 92 | 30.7 | 422 | 25.8 |
| High school | 2,516 | 46.6 | 1754 | 46.6 | 1177 | 45.9 | 264 | 45.9 | 314 | 47.7 | 143 | 47.7 | 776 | 47.4 |
| Some college | 1,127 | 20.9 | 810 | 21.5 | 513 | 20.0 | 160 | 27.8 | 167 | 25.4 | 49 | 16.3 | 329 | 20.1 |
| ≥College graduate | 418 | 7.7 | 265 | 7.0 | 186 | 7.3 | 43 | 7.5 | 42 | 6.4 | 16 | 5.3 | 111 | 6.8 |
| Missing | 83 | 53 | 32 | 8 | 16 | 3 | 18 | |||||||
| Cocaine i | ||||||||||||||
| No | 4,768 | 87.0 | 3388 | 88.7 | 2395 | 92.3 | 486 | 83.4 | 501 | 74.3 | 288 | 95.1 | 1469 | 88.7 |
| Yes | 715 | 13.0 | 430 | 11.3 | 199 | 7.7 | 97 | 16.6 | 173 | 25.7 | 15 | 5.0 | 187 | 11.3 |
| Other stimulants i | ||||||||||||||
| No | 5,034 | 91.8 | 3538 | 92.7 | 2436 | 93.9 | 516 | 88.5 | 611 | 90.7 | 287 | 94.7 | 1536 | 92.8 |
| Yes | 449 | 8.2 | 280 | 7.3 | 158 | 6.1 | 67 | 11.5 | 63 | 9.4 | 16 | 5.3 | 120 | 7.3 |
| Alcohol i | ||||||||||||||
| No | 4,781 | 87.2 | 3276 | 85.8 | 2260 | 87.1 | 506 | 86.8 | 512 | 76.0 | 279 | 92.1 | 1443 | 87.1 |
| Yes | 702 | 12.8 | 542 | 14.2 | 334 | 12.9 | 77 | 13.2 | 162 | 24.0 | 24 | 7.9 | 213 | 12.9 |
| Benzodiazepines i | ||||||||||||||
| No | 3,664 | 66.8 | 2162 | 56.6 | 1359 | 52.4 | 347 | 59.5 | 435 | 64.5 | 169 | 55.8 | ||
| Yes | 1819 | 33.2 | 1656 | 43.4 | 1235 | 47.6 | 236 | 40.5 | 239 | 35.5 | 134 | 44.2 | 1656 | 100.0 |
| Intentionality | ||||||||||||||
| Unintentional | 4,789 | 87.3 | 3516 | 92.1 | 2351 | 90.6 | 559 | 95.9 | 656 | 97.3 | 284 | 93.7 | 1508 | 91.1 |
| Suicide | 452 | 8.2 | 179 | 4.7 | 153 | 5.9 | 9 | 1.5 | 6 | 0.9 | 8 | 2.6 | 86 | 5.2 |
| Homicide | 5 | 0.1 | 5 | 0.1 | 4 | 0.2 | 0 | 1 | 0.2 | 1 | 0.3 | 3 | 0.2 | |
| Undetermined | 237 | 4.3 | 118 | 3.1 | 86 | 3.3 | 15 | 2.6 | 11 | 1.6 | 10 | 3.3 | 59 | 3.6 |
Frequencies and percents exclude missing.
ICD-10 codes X40–X44; X60-X64; X85; Y10-Y14
ICD-10 codes X40–X44; X60-X64; X85; Y10-Y14 and T40.0-T40.4, T40.6.
ICD-10 codes X40–X44; X60-X64; X85; Y10-Y14 and T40.2-T40.4, excluding fentanyl deaths (2 fentanyl deaths were identified via literal text searches, but were not classified via ICD-10 T codes for synthetic opioids).
ICD-10 codes X40–X44; X60-X64; X85; Y10-Y14 and literal text searches for fentanyl.
ICD-10 codes X40–X44; X60-X64; X85; Y10-Y14 and T40.1.
ICD-10 codes X40–X44; X60-X64; X85; Y10-Y14 and T40.3.
ICD-10 codes X40–X44; X60-X64; X85; Y10-Y14 and T40.0-T40.4, T40.6 and T42.4.
Other contributing drug besides opioids identified with ICD-10 MCD T codes (cocaine, T40.5, other stimulants T43.6, alcohol T51.0 and T51.9, benzodiazepines T42.4).
In the second analysis, we evaluated associations between prescription history characteristics and type of opioid death (prescription opioids, fentanyl, heroin) using mutually exclusive outcome categories. Frequencies and proportions were calculated for categorical variables and medians with ranges were calculated for continuous variables. Bivariable statistical tests of association were calculated for categorical (general chi-square tests) and continuous (Kruskal-Wallis tests) variables. This analysis was limited to decedents linked to the CSMD with days’ supply ≥ 1 (n=3,971, Figure 1). All analyses were conducted in SAS (SAS Institute Inc., Cary, North Carolina). P-values <0.05 were considered statistically significant.
3. Results
A total of 5,483 TN residents aged ≥18 years died between 2013 and 2016 of a drug overdose. The majority of overdose deaths involved an opioid (n=3,818, 69.6%) and 47.3% were opioids typically obtained through a prescription. Fentanyl was involved in 10.6% (n=583) of deaths, heroin in 12.3% (n=674), buprenorphine in 3.4% (n=186), and methadone in 5.5% (n=303). Additional major drugs involved included benzodiazepines (33.2%, n=1,819), cocaine (13.0%, n=715), other stimulants (8.2%, n=449), and alcohol (12.8%, n=702).
3.1. Sociodemographic Factors and Multiple Drug Use among Overdose Decedents (Table 1)
Heroin and fentanyl decedents were younger, while prescription opioid decedents were older, with the highest number of overdose deaths in the age group of 45–54 years. Most prescription opioid and methadone deaths occurred among Non-Hispanic Whites. The highest proportion of Non-Hispanic black decedents and males was observed in heroin and fentanyl deaths. Heroin deaths had the highest proportion of cocaine and alcohol as contributing substances. The contribution of benzodiazepines was high across all types of deaths.
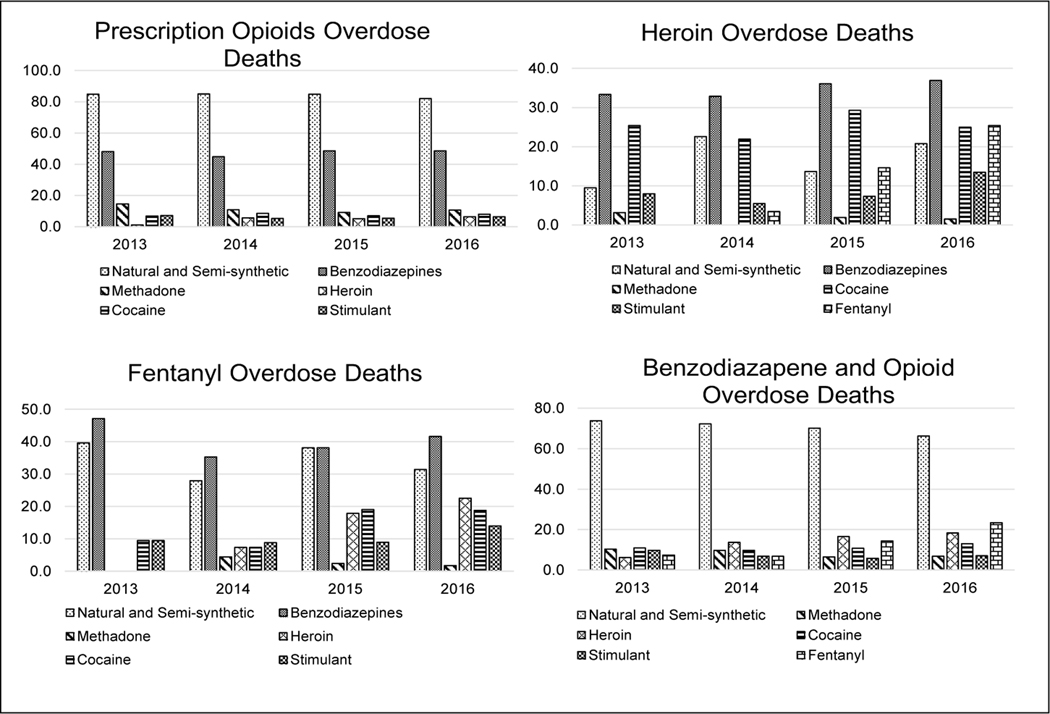
3.2. Polysubstance Use by Year and Type of Opioid-Related Overdose Death (Figure 1)
A high proportion of opioid deaths involved multiple contributing substances, with changing patterns in specific drugs over time by type of death. The contribution of heroin to prescription opioid deaths and fentanyl deaths increased from 1.2% and 0% in 2013 to 6.5% and 22.5% in 2016, respectively. The proportion of heroin deaths also involving fentanyl increased from 0% in 2013 to 25.4% in 2016. Benzodiazepines were involved in about 50% of prescription opioid deaths.
3.3. Factors Associated with Type of Opioid Death in Multivariable Analyses (Table 2)
Table 2.
ORs for the associations of sociodemographic factors by type of opioid overdose death among TN adult opioid overdose decedents 2013–2016 (n=3,818)a
| Prescription Opioid Overdose (excluding fentanyl) (n=2,594) | Fentanyl Overdose (n=582) | Heroin Overdose (n=674) | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Unadjusted Modelb | Adjusted Modelc | Unadjusted Modelb | Adjusted Modelc | Unadjusted Modelb | Adjusted Modelc | ||||||||||||
| n | OR | (95% CI) | OR | (95% CI) | n | OR | (95% CI) | OR | (95% CI) | n | OR | (95% CI) | OR | (95% CI) | |||
| Age at death | |||||||||||||||||
| <25 | 118 | 0.37 | (0.28– 0.49) | 0.44 | (0.34–0.59) | 66 | 2.54 | (1.86–3.46) | 2.18 | (1.57–3.04) | 68 | 2.19 | (1.62–2.98) | 1.68 | (1.21–2.32) | ||
| 25–34 | 477 | 0.52 | (0.44–0.62) | 0.57 | (0.48–0.68) | 181 | 1.88 | (1.52–2.32) | 1.72 | (1.38–2.15) | 224 | 2.07 | (1.70–2.51) | 1.83 | (1.49–2.26) | ||
| 35–54 | 1447 | 1.00 | (reference) | 1.00 | (reference) | 259 | 1.00 | (reference) | 1.00 | (reference) | 304 | 1.00 | (reference) | 1.00 | (reference) | ||
| 55–64 | 461 | 1.27 | (1.02–1.56) | 1.27 | (1.02–1.58) | 60 | 0.75 | (0.56–1.01) | 0.72 | (0.53–0.98) | 71 | 0.75 | (0.57–0.99) | 0.75 | (0.56–1.01) | ||
| ≥65 | 91 | 0.93 | (0.63–1.38) | 0.97 | (0.64–1.46) | 16 | 0.96 | (0.56–1.64) | 0.91 | (0.52–1.58) | 7 | 0.32 | (0.15–0.70) | 0.23 | (0.09–0.57) | ||
| Race/ethnicity | |||||||||||||||||
| Non-Hispanic White | 2398 | 1.00 | (reference) | 1.00 | (reference) | 494 | 1.00 | (reference) | 1.00 | (reference) | 536 | 1.00 | (reference) | 1.00 | (reference) | ||
| Non-Hispanic Black | 124 | 0.38 | (0.30–0.49) | 0.41 | (0.31–0.53) | 72 | 2.23 | (1.67–2.97) | 1.94 | (1.43–2.63) | 89 | 2.74 | (2.09–3.60) | 2.57 | (1.93–3.43) | ||
| Other | 29 | 0.33 | (0.20–0.53) | 0.44 | (0.26–0.74) | 15 | 1.71 | (0.96–3.06) | 1.27 | (0.68–2.37) | 23 | 2.82 | (1.69–4.70) | 2.06 | (1.18–3.62) | ||
| Gender | |||||||||||||||||
| Male | 1381 | 1.00 | (reference) | 1.00 | (reference) | 377 | 1.00 | (reference) | 1.00 | (reference) | 490 | 1.00 | (reference) | 1.00 | (reference) | ||
| Female | 1213 | 1.74 | (1.51–2.01) | 1.60 | (1.38–1.85) | 205 | 0.70 | (0.58–0.84) | 0.77 | (0.64–0.94) | 184 | 0.45 | (0.37–0.53) | 0.47 | (0.38–0.57) | ||
| Never Married | 673 | 1.00 | (reference) | 1.00 | (reference) | 260 | 1.00 | (reference) | 1.00 | (reference) | 330 | 1.00 | (reference) | 1.00 | (reference) | ||
| Not Married | 1093 | 2.18 | (1.85–2.56) | 1.36 | (1.12–1.66) | 170 | 0.47 | (0.38–0.58) | 0.77 | (0.59–1.00) | 207 | 0.43 | (0.35–0.52) | 0.74 | (0.58–0.93) | ||
| Married | 748 | 2.36 | (1.96–2.83) | 1.55 | (1.26–1.90) | 134 | 0.56 | (0.45–0.71) | 0.89 | (0.68–1.16) | 103 | 0.31 | (0.24–0.39) | 0.47 | (0.36–0.61) | ||
| Education | |||||||||||||||||
| <High school | 686 | 1.00 | (reference) | 1.00 | (reference) | 108 | 1.00 | (reference) | 1.00 | (reference) | 135 | 1.00 | (reference) | 1.00 | (reference) | ||
| High school | 1177 | 0.74 | (0.62–0.89) | 0.78 | (0.65–0.94) | 264 | 1.36 | (1.07–1.73) | 1.27 | (0.99–1.63) | 314 | 1.29 | (1.04–1.61) | 1.25 | (0.99–1.58) | ||
| >High School | 699 | 0.68 | (0.56–0.82) | 0.67 | (0.55–0.83) | 202 | 1.77 | (1.38–2.28) | 1.76 | (1.35–2.29) | 209 | 1.43 | (1.13–1.81) | 1.53 | (1.19–1.97) | ||
| Cocaine d | |||||||||||||||||
| No | 2395 | 1.00 | (reference) | 1.00 | (reference) | 485 | 1.00 | (reference) | 1.00 | (reference) | 501 | 1.00 | (reference) | 1.00 | (reference) | ||
| Yes | 199 | 0.36 | (0.29–0.44) | 0.45 | (0.36–0.56) | 97 | 1.74 | (1.36–2.23) | 1.34 | (1.02–1.75) | 173 | 3.88 | (3.13–4.81) | 2.86 | (2.26–3.63) | ||
| Other stimulants d | |||||||||||||||||
| No | 2436 | 1.00 | (reference) | 1.00 | (reference) | 515 | 1.00 | (reference) | 1.00 | (reference) | 611 | 1.00 | (reference) | 1.00 | (reference) | ||
| Yes | 158 | 0.59 | (0.46–0.75) | 0.65 | (0.50–0.84) | 67 | 1.85 | (1.38–2.47) | 1.65 | (1.22–2.25) | 63 | 1.39 | (1.04–1.87) | 1.16 | (0.85–1.59) | ||
| Alcohol d | |||||||||||||||||
| No | 2260 | 1.00 | (reference) | 1.00 | (reference) | 505 | 1.00 | (reference) | 1.00 | (reference) | 512 | 1.00 | (reference) | 1.00 | (reference) | ||
| Yes | 334 | 0.72 | (0.60–0.87) | 0.80 | (0.66–0.98) | 77 | 0.91 | (0.70–1.18) | 0.80 | (0.61–1.06) | 162 | 2.30 | (1.87–2.83) | 2.02 | (1.61–2.52) | ||
| Benzodiazepines d | |||||||||||||||||
| No | 1359 | 1.00 | (reference) | 1.00 | (reference) | 347 | 1.00 | (reference) | 1.00 | (reference) | 435 | 1.00 | (reference) | 1.00 | (reference) | ||
| Yes | 1235 | 1.73 | (1.51–2.00) | 1.76 | (1.51–2.04) | 235 | 0.87 | (0.72–1.04) | 0.85 | (0.70–1.03) | 239 | 0.67 | (0.56–0.80) | 0.71 | (0.59–0.86) | ||
Analysis is among TN adults who died due to an opioid overdose death (T40.1, T40.2, T40.3, T40.4, and T40.6). One fentanyl death that was not classified as an opioid death based on ICD-10 T codes is excluded. The outcome reference group for each model is other type of opioid deaths (e.g., heroin overdose deaths vs. other types of opioid deaths).
Missing data are excluded for race/ethnicity (n=62), marital status (n=124), and education (n=53).
Adjusted for year of death, age, race/ethnicity, gender, and education (when not main effects of interest). Adjusted analysis excludes 101 decedents missing data on age, race/ethnicity, or education (models for marital status exclude an additional 93 decedents).
Other contributing drugs besides opioids identified with ICD-10 MCD T codes (cocaine (T40.5), other stimulants (T43.6), alcohol (T51.0, T51.9), benzodiazepines T42.4). Reference group is absence of the drug
We evaluated sociodemographic factors and multiple drug use among opioid overdose decedents (study population 1 in Figure 1). In adjusted models, younger age (<25 and 25–34 years) was inversely associated with prescription opioid overdose deaths, compared to decedents aged 35–54 years, while decedents aged 55–64 years had increased odds of prescription opioid overdose deaths (ref, other opioid deaths). Female gender, having ever been married, and presence of benzodiazepines as a contributing cause were also associated with increased odds of prescription opioid overdoses. Non-White race/ethnicity, ≥high school education, and involvement of cocaine, stimulants, or alcohol at death were associated with reduced odds of prescription opioid overdoses.
In adjusted models, younger age, Non-Hispanic Black race/ethnicity, >high school education, and presence of cocaine or other stimulants were associated with increased odds of a fentanyl death (ref, other opioid deaths), while female gender was inversely associated with fentanyl. A similar risk factor profile was observed for heroin deaths (ref, other opioid deaths), with the exception of an association between alcohol and increased odds of heroin overdose deaths.
Decedents aged ≥65 years, compared to 35–54 years, had reduced odds of an opioid and benzodiazepine combined overdose death (Table S22), while females had increased odds of death. Race/ethnicity, marital status, and other contributing causes were not significantly associated with a combined opioid and benzodiazepine overdose (Table S22).
3.4. Opioid Prescription History by Type of Opioid Death (Table 3)
Table 3.
Opioid prescription history by type of opioid-related overdose death among individuals who died in TN of a prescription opioid overdose, fentanyl overdose, or heroin overdose and filled ≥1 prescription within 365 days before death (n=2,686)
| Prescription Opioid Overdosea (n=1,965) | Fentanyl Overdoseb (n=393) | Heroin Overdosec (n=328) | P-valued | |
|---|---|---|---|---|
| Number of opioid prescriptions within 365 days before death, n (%) | ||||
| 0 | 126 (6.4) | 43 (10.9) | 54 (16.5) | |
| 1–2 | 306 (15.6) | 94 (23.9) | 83 (25.3) | |
| ≥3 | 1,533 (78.0) | 256 (65.1) | 191 (58.2) | <0.0001 |
| Median (range) | 12 (0–88) | 7 (0–83) | 4 (0–102) | <0.0001 |
| Opioid prescription 90 days before death, n (%) | ||||
| No | 507 (25.8) | 154 (39.2) | 155 (47.3) | |
| Yes | 1,458 (74.2) | 239 (60.8) | 173 (52.7) | <0.0001 |
| Opioid prescription 30 days before death, n (%) | ||||
| No | 746 (38.0) | 211 (53.7) | 222 (67.7) | |
| Yes | 1,219 (62.0) | 182 (46.3) | 106 (32.3) | <0.0001 |
| Active opioid prescription at death, n (%) | ||||
| No | 882 (44.9) | 239 (60.8) | 260 (79.3) | |
| Yes | 1,083 (55.1) | 154 (39.2) | 68 (20.7) | <0.0001 |
| Active hydrocodone prescription at death, n (%) | ||||
| No | 1681 (85.6) | 349 (88.8) | 305 (93.0) | |
| Yes | 284 (14.5) | 44 (11.2) | 23 (7.0) | 0.0005 |
| Active oxycodone prescription at death, n (%) | ||||
| No | 1300 (66.2) | 322 (81.9) | 301 (91.8) | |
| Yes | 665 (33.8) | 71 (18.1) | 27 (8.2) | <0.0001 |
| Active buprenorphine for MAT prescription at death, n (%) | ||||
| No | 1,922 (97.8) | 375 (95.4) | 319 (97.3) | |
| Yes | 43 (2.2) | 18 (4.6) | 9 (2.7) | 0.0246 |
| Active fentanyl prescription at death, n (%) | ||||
| No | 1,955 (99.5) | 335 (85.2) | 0 | |
| Yes | 10 (0.5) | 58 (14.8) | NA | |
| Total MME for opioid analgesics in 90 days before death e , n (%) | ||||
| ≤2395.0 | 264 (18.6) | 74 (32.7) | 92 (57.5) | |
| 2395.0-<12787.5 | 356 (25.1) | 46 (20.4) | 31 (19.4) | |
| 12787.5-<39352.5 | 400 (28.2) | 33 (14.6) | 25 (15.6) | |
| ≥39352.5 | 399 (28.1) | 73 (32.3) | 12 (7.5) | <0.0001 |
| Total MME for opioid analgesics in 30 days before death e , n (%) | ||||
| ≤4992 | 237 (19.9) | 58 (33.5) | 59 (60.2) | |
| 4992-<16350 | 297 (25.0) | 26 (15.0) | 19 (19.4) | |
| 16350-<46800 | 331 (27.8) | 33 (19.1) | 12 (12.2) | |
| ≥46800 | 325 (27.3) | 56 (32.4) | 8 (8.2) | <0.0001 |
| Number of prescribers for opioids f , n (%) | ||||
| 1 | 424 (23.1) | 118 (33.7) | 78 (28.5) | |
| 2 | 360 (19.6) | 65 (18.6) | 66 (24.1) | |
| 3–4 | 527 (28.7) | 76 (21.7) | 70 (25.6) | |
| ≥5 | 528 (28.7) | 91 (26.0) | 60 (21.9) | 0.0001 |
| Median (range) | 3 (1–34) | 2 (1–21) | 2 (1–15) | 0.0002 |
| Number of dispensers for opioids f , n (%) | ||||
| 1 | 688 (37.4) | 143 (40.9) | 106 (38.7) | |
| 2 | 476 (25.9) | 86 (24.6) | 75 (27.4) | |
| 3–4 | 471 (25.6) | 78 (22.3) | 60 (21.9) | |
| ≥5 | 204 (11.1) | 43 (12.3) | 33 (12.0) | 0.6465 |
| Median (range) | 2 (1–13) | 2 (1–12) | 2 (1–10) | 0.6098 |
| Cash payment for an opioid prescription f , n (%) | ||||
| 0 | 218 (62.3) | 147 (53.7) | ||
| 1–2 | 78 (22.3) | 82 (29.9) | ||
| 3–4 | 129 (7.1) | 18 (5.1) | 22 (8.0) | |
| ≥5 | 272 (15.0) | 36 (10.3) | 23 (8.4) | 0.0011 |
| Medicare used for an opioid prescriptions f , n (%) | ||||
| 0 | 1,320 (72.6) | 288 (82.3) | 249 (90.9) | |
| 1–2 | 100 (5.5) | 11 (3.1) | 4 (1.5) | |
| ≥3 | 398 (21.9) | 51 (14.6) | 21 (7.7) | <0.0001 |
| Medicaid used for an opioid prescriptions f , n (%) | ||||
| 0 | 1,411 (77.6) | 265 (75.7) | 212 (77.4) | |
| 1–2 | 119 (6.6) | 38 (10.9) | 21 (7.7) | |
| ≥3 | 288 (15.8) | 47 (13.4) | 41 (15.0) | 0.0655 |
Defined as prescription opioid overdoses excluding fentanyl and heroin overdoses.
All fentanyl overdose deaths based on literal text searches.
Defined as heroin overdoses excluding fentanyl.
Chi-square test for categorical variables and Kruskal-Wallis test for continuous variables.
Limited to decedents with analgesics opioid use in the last 30 days (n=1465) or 90 days (n=1811), cutpoints based on quartiles in each group.
Excludes deaths with no opioid prescription (n=223); payment variables additional exclude missing (n=21).
Overall, prescription opioid use was highest among prescription opioid overdoses, followed by fentanyl and heroin deaths. Within each overdose category, the proportion of decedents without a prescription was higher the closer to date of death the measurement. For example, 60.8% of fentanyl decedents had filled a prescription 90-days before death, 46.3% 30 days before death, and 39.2% had an active prescription at death. Oxycodone was the most frequently filled prescription opioid, in particular among prescription overdose and fentanyl deaths. Only 14.8% of fentanyl decedents had an active prescription for fentanyl at death.
Most decedents filled opioid prescriptions from more than one prescriber in the year before death, and close to 60% of prescription opioid decedents filled prescriptions from more than two prescribers. Across type of death, about 60% of decedents received an opioid from more than one pharmacy. Use of cash payment for at least one opioid prescription was most common among heroin deaths (46.3%), followed by prescription opioid (43.9%) and fentanyl (37.7%) deaths. Use of Medicare for more than one opioid prescription was highest among prescription opioid deaths; use of Medicaid did not vary by type of death.
3.5. Benzodiazepine Prescription History by Type of Opioid Death (Table 3)
Prescription opioid decedents had the highest benzodiazepine use in the 90 days before death (55.7%), followed by fentanyl (40.2%) and heroin (35.7%). About 46% of prescription opioid overdoses had an active benzodiazepine prescription, compared to ~1/3 of fentanyl and heroin overdoses. About half of decedents filled their prescriptions for benzodiazepines from only one provider or one dispenser, with limited variation by type of death.
4. Discussion
Data on sociodemographic and prescribing patterns by contributing substances for overdose deaths are needed to guide targeted and appropriate prevention strategies to reduce opioid mortality. In this large population-based analysis of TN drug overdose decedents, sociodemographic profiles, non-opioid contributing substances, and opioid and benzodiazepine prescribing patterns differed by type of opioid overdose death (i.e., prescription opioid, fentanyl, and heroin deaths). For prescription opioid overdose deaths (compared to other opioid overdose deaths), younger age (<25 and 25–34 years), Non-Hispanic black race/ethnicity, and higher education were associated with reduced odds of overdose, while decedents who were female, married or previously married, or had benzodiazepines as a contributing cause were at increased odds of prescription drug overdose. For fentanyl overdose deaths (compared to other opioid overdose deaths), female gender was associated with reduced odds of overdose, while younger ages (< 25 and 25–34 years), Non-Hispanic Black race/ethnicity, higher education, and cocaine or stimulants as a contributing cause were associated with increased odds of overdose. A similar risk factor pattern was observed among heroin deaths, with the exception of increased odds of overdose death for alcohol use.
Two previous studies reported associations between female gender and presence of benzodiazepines at death with prescription overdose deaths, including a study of 2,231 decedents in Connecticut (1997–2007) (Green et al., 2011) and 2,888 decedents in New York (1990–2006) (Cerda et al., 2013). The authors of the Connecticut study also evaluated characteristics of heroin deaths and reported associations for younger age groups and male gender, similar to our findings. In contrast to our findings, heroin deaths were more likely to occur among white decedents and not involve multiple non-opioid substances. The first study of linked PDMP and mortality data, conducted in West Virginia in 2006 among 295 unintentional prescription overdose deaths, reported decedents who were never married/divorced, of lower education or income, or male had higher death rates, and few decedents had filled a prescription in the year before death (Hall et al., 2008). Mercado et al. evaluated factors associated with illicit fentanyl deaths compared to all overdose deaths in a study of 536 decedents in Rhode Island (2013–2014), and similar to our study, younger age was associated with illicit fentanyl overdose. However other sociodemographic factors were not associated with deaths (Mercado et al., 2017). A study using data from Kentucky found that the highest rates of fentanyl and heroin overdoses were among 25–34-year old’s (Slavova et al., 2017b).
We found that regardless of the type of opioid-related death, a large number involved polysubstance, as observed previously (Hall et al., 2008; King et al., 2014; Mercado et al., 2017; Warner et al., 2016). From 2013–2016, fentanyl involvement increased from 0% to 25.4% among heroin deaths, and cocaine increased 9.4% to 18.8% among fentanyl deaths. Benzodiazepines were involved in nearly half of prescription opioid and ~30–40% of fentanyl and heroin deaths across years, similar to findings from a study of national trends in polysubstance use among overdose deaths (Kandel et al., 2017). This study also reported that heroin increased (1.2% to 24.5%) among deaths due to synthetic opioids other than methadone (a category that includes fentanyl overdoses).
In our study, opioid prescription use was highest for prescription opioid overdose deaths, followed by fentanyl and then heroin only overdose deaths, regardless of opioid use timing or type. Few fentanyl decedents had an active prescription at death (<15%), very similar to the proportion reported in a study of overdose deaths during 2013–2014 in Kentucky (Slavova et al., 2017a), and suggests that the majority of fentanyl deaths in TN are due to illicit use. Potentially risky prescription-related behaviors, including visiting multiple doctors and pharmacies and cash payments for prescriptions, were highly prevalent in the year before death. Of particular concern was the high amount of benzodiazepine use regardless of the type of death, known to have high-risk when co-prescribed with opioids (Dasgupta et al., 2016; Dilokthornsakul et al., 2016; Jones and McAninch, 2015; Park et al., 2015; Volkow and McLellan, 2016).
Our findings support the need to consider multiple susceptible populations and targeted education and intervention efforts to reduce prescription opioid, heroin, and fentanyl overdose deaths. Community-based programs that provide naloxone take-home kits and overdose prevention training are key public health interventions that can be modified and directed to high-risk populations (Straus et al., 2013). To be successful, these strategies should consider younger age groups, males, Non-Hispanic Blacks, and individuals with alcohol and other illicit drug use history, addressing barriers to receiving and using educational and intervention programs. Targeted programs can benefit from the fact that high risk individuals may be more likely to utilize the programs and should consider both community and clinical-based naloxone distribution to maximize effectiveness (Barocas et al., 2015; Coffin et al., 2016; Raffel et al., 2018; Siegler et al., 2014). Our data show that over half of fentanyl and heroin overdoses had a filled opioid prescription in the 90-days before death, suggesting a missed opportunity for prevention. Continued efforts to educate healthcare professionals on evidence-based practices and policies including the Tennessee Chronic Pain Guidelines and resources for implementation, increased availability of medication-assisted treatment as part of an individually-tailored comprehensive treatment program based on best practices, and increased awareness of risky behaviors and adverse outcomes is needed (Cochran et al., 2016; Tennessee Department of Health, 2017; Kolodny et al., 2015; Kresina and Lubran, 2011; Starrels et al., 2011; Volkow and McLellan, 2016). The role of benzodiazepines in the opioid public health crisis needs to be integrated into community and health-care based educational and intervention efforts, and for multiple susceptible populations including illicit users, prescription opioid users, and individuals with opioid use disorder.
4.1. Limitations
The CSMD, similar to other PDMPs (Hartung et al., 2017; Mercado et al., 2017), has limited identifiers available for data linkage. We evaluated the potential for false positives based on our deterministic approach in a subset of patients with multiple names across records and found a very low number of potential false positives (<1% of patient records), consistent with the assumption that matching on full name and DOB accurately identifies an individual if identifiers are reasonably accurate (McCoy et al., 2013). While our approach resulted in few potentially incorrect matches, we may have missed both decedents and prescription records, which would lead to underestimation of the role of prescription history in overdose deaths in the present analysis. Another limitation is the use of DEA number to identify prescribers and dispensers, which may result in misclassification in these variables.
Additional limitations inherent in using PDMP data include: 1) lack of information on drug indication, 2) incomplete opioid prescription history as not all controlled substances are captured by the CSMD (e.g., out of state prescriptions, drugs dispensed directly to the patient, some short-term supply samples, opioids for MAT in federal treatment centers, and drugs obtained illegally), and 4) lack of medical history, including psychiatric or substance abuse history, known predictors of overdose death (Brady et al., 2017; King et al., 2014). The time frame of our study (one year before death) may miss the full trajectory from the first prescription to overdose, for example, as many heroin users may have started with prescription opioids (Muhuri PK et al., 2013).
Using death certificate data to classify overdose deaths has several known limitations including lack of specific drug types, toxicology results, and reporting variations across time and jurisdictions (Moyer et al., 1989; Slavova et al., 2015; Stone et al., 2017; Warner et al., 2016). In particular, heroin deaths may be underestimated as the death certificate may list morphine without providing the source (e.g., metabolized heroin or prescription morphine), which can be difficult to determine without the presence of 6-acetylmophine, a metabolite of heroin (Ellis et al., 2016; Mertz et al., 2014). Further, it is not possible to distinguish fentanyl from fentanyl analogs (e.g., carfentanil) using only death certificate data. Combining toxicology and death certificate data could help address these limitations in the future (Slavova et al., 2017a). It is encouraging that reporting on specific drugs involved in overdose deaths is improving in TN (Rudd et al., 2016). Finally, we did not exclude intentional overdoses or overdoses of undermined intent as misclassification is a known concern (Rockett et al., 2015; Stone et al., 2017).
4.2. Conclusions
Our findings provide a comprehensive description of opioid and benzodiazepine prescribing history in the year before death. These data help to identify the most susceptible populations at risk for opioid mortality. Results regarding benzodiazepine involvement in opioid-related deaths, regardless of type, as well as the high proportions of patients on opioid analgesics receiving prescriptions for benzodiazepines highlight that more work is needed to address risky prescribing practices contributing to opioid deaths. TN has invested substantial effort in legislation, law enforcement, surveillance, population-based analytics, professional education, and community outreach to reduce opioid-related morbidity and mortality. Our findings can support targeted education and intervention efforts, building on existing infrastructure, and help improve utilization of TN’s PDMP.
Supplementary Material
Figure 2.
Major Contributing Causes of Death by Type of Opioid Overdose Death in TN, 2013-2016.
Table 4.
Benzodiazepine prescription history by type of opioid-related overdose death among individuals who died in TN of a prescription opioid overdose, fentanyl overdose, or heroin overdose and filled ≥1 prescription within 365 days before death (n=2,686)
| Prescription Opioid Overdosea (n=1,965) | Fentanyl Overdoseb (n=393) | Heroin Overdosec (n=328) | P-valued | |
|---|---|---|---|---|
| Number of benzodiazepine prescriptions, n (%) | ||||
| 0 | 662 (33.7) | 197 (50.1) | 168 (51.2) | |
| 1–2 | 176 (9.0) | 36 (9.2) | 43 (13.1) | |
| ≥3 | 1,127 (57.4) | 160 (40.7) | 117 (35.7) | <0.0001 |
| Benzodiazepine prescription 90 days before death, n (%) | ||||
| No | 870 (44.3) | 235 (59.8) | 211 (64.3) | |
| Yes | 1,095 (55.7) | 158 (40.2) | 117 (35.7) | <0.0001 |
| Benzodiazepine prescription 30 days before death, n (%) | ||||
| No | 1,026 (52.2) | 270 (68.7) | 238 (72.6) | |
| Yes | 939 (47.8) | 123 (31.3) | 90 (27.4) | <0.0001 |
| Prescription for both opioid and benzodiazepines 30 days before death, n (%) | ||||
| No | 1,225 (62.3) | 305 (77.6) | 283 (86.3) | |
| Yes | 740 (37.7) | 88 (22.4) | 45 (13.7) | <0.0001 |
| Active benzodiazepine prescription at death, n (%) | ||||
| No | 1,062 (54.1) | 273 (69.5) | 242 (73.8) | |
| Yes | 903 (46.0) | 120 (30.5) | 86 (26.2) | <0.0001 |
| Number of prescribers for benzodiazepinese, n (%) | ||||
| 1 | 608 (46.7) | 98 (50.0) | 87 (54.4) | |
| 2 | 371 (28.5) | 51 (26.0) | 37 (23.1) | |
| 3–4 | 265 (20.3) | 34 (17.4) | 29 (18.1) | |
| ≥5 | 59 (4.5) | 13 (6.6) | 7 (4.4) | 0.3858 |
| Median (range) | 2 (1–13) | 1.5 (1–8) | 1 (1–6) | 0.2834 |
| Number of dispensers for benzodiazepinese, n (%) | ||||
| 1 | 654 (50.2) | 110 (56.1) | 84 (52.5) | |
| 2 | 362 (27.8) | 51 (26.0) | 42 (26.3) | |
| 3–4 | 242 (18.6) | 26 (13.3) | 22 (13.8) | |
| ≥5 | 45 (3.5) | 9 (4.6) | 12 (7.5) | 0.0678 |
| Median (range) | 1 (1–10) | 1 (1–7) | 1 (1–9) | 0.3259 |
Defined as prescription opioid overdoses excluding fentanyl.
All fentanyl overdose deaths based on literal text searches.
Defined as heroin overdoses excluding fentanyl.
Chi-square test for categorical variables and Kruskal-Wallis Test for continuous variables.
Excludes deaths with no benzodiazepine prescription (n=1,503).
Highlights.
Large study of prescription history before overdose death by contributing drugs.
Sociodemographic risk factor profiles differed by type of opioid death.
>50% of heroin and fentanyl deaths had an opioid prescription 90 days before death.
>1/3 of opioid decedents had an active prescription for a benzodiazepine at death.
Risky prescription-related behaviors were common in the year before death.
Acknowledgements
This work was supported by a grant from the Centers for Disease Control and Prevention, Prescription Drug Overdose Prevention for States Program (5 NU17CE002731-02-00). The authors thank Molly Golladay for assistance in data cleaning for the CSMD patient information.
Role of Funding Source
The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Abbreviations:
- COD
Cause of Death
- CSMD
Controlled Substance Monitoring Database
- DOB
Date of birth
- DEA
Drug enforcement administration
- IMF
Illicitly manufactured fentanyl
- MAT
Medication-assisted treatment
- MME
Morphine milligram equivalents
- MCOD
Multiple causes of death
- NCHS
National Center for Health Statistics
- PDMPs
Prescription Drug Monitoring Programs
- TN
Tennessee
- TDH
Tennessee Department of Health
- UCD
Underlying cause of death
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Authors Disclosures
Conflict of Interest No conflict declared.
Supplementary material can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi:…
Supplementary material can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi:…
Supplementary material can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi:…
References
- Austin AE, Proescholdbell SK, Creppage KE, Asbun A, 2017. Characteristics of self-inflicted drug overdose deaths in North Carolina. Drug Alcohol Depend. 181, 44–49. [DOI] [PubMed] [Google Scholar]
- Barocas JA, Baker L, Hull SJ, Stokes S, Westergaard RP, 2015. High uptake of naloxone-based overdose prevention training among previously incarcerated syringe-exchange program participants. Drug Alcohol Depend. 154, 283–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brady JE, Giglio R, Keyes KM, DiMaggio C, Li G, 2017. Risk markers for fatal and non-fatal prescription drug overdose: A meta-analysis. Inj. Epidemiol 4, 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention, National Center for Health Statistics, Multiple Cause of Death 1999–2015 on CDC Wonder Online Database, released December 2016. http://wonder.cdc.gov/mcd-icd10.html (Accessed 01-15-18).
- Cerda M, Ransome Y, Keyes KM, Koenen KC, Tracy M, Tardiff KJ, Vlahov D, Galea S, 2013. Prescription opioid mortality trends in New York City, 1990–2006: Examining the emergence of an epidemic. Drug Alcohol Depend. 132, 53–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cochran G, Hruschak V, DeFosse B, Hohmeier KC, 2016. Prescription opioid abuse: Pharmacists’ perspective and response. Integr. Pharm. Res. Pract 5, 65–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coffin PO, Behar E, Rowe C, Santos GM, Coffa D, Bald M, Vittinghoff E, 2016. Nonrandomized intervention study of naloxone coprescription for primary care patients receiving long-term opioid therapy for pain. Ann. Intern. Med 165, 245–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dasgupta N, Funk MJ, Proescholdbell S, Hirsch A, Ribisl KM, Marshall S, 2016. Cohort study of the impact of high-dose opioid analgesics on overdose mortality. Pain Med. 17, 85–98. [DOI] [PubMed] [Google Scholar]
- Dilokthornsakul P, Moore G, Campbell JD, Lodge R, Traugott C, Zerzan J, Allen R, Page RL 2nd, 2016. Risk Factors of Prescription Opioid Overdose Among Colorado Medicaid Beneficiaries. J. Pain 17, 436–43. [DOI] [PubMed] [Google Scholar]
- Ellis AD, McGwin G, Davis GG, Dye DW, 2016. Identifying cases of heroin toxicity where 6-acetylmorphine (6-AM) is not detected by. Forensic Sci. Med. Pathol 12, 243–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairbairn N, Coffin PO, Walley AY, 2017. Naloxone for heroin, prescription opioid, and illicitly made fentanyl overdoses: Challenges and innovations responding to a dynamic epidemic. Int. J. Drug Policy 46, 172–179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garg RK, Fulton-Kehoe D, Franklin GM, 2017. Patterns of opioid use and risk of opioid overdose death among Medicaid patients. Med. Care 55, 661–668. [DOI] [PubMed] [Google Scholar]
- Golladay M, Nechuta S, 2018. Lessons learned: Deep cleaning procedure design for name variables in the Tennessee CSMD. Available at: https://www.tn.gov/content/dam/tn/health/documents/opioid_response/CSMDNameCleaningReport.pdf (Last Accessed: 04-29-18).
- Green TC, Grau LE, Carver HW, Kinzly M, Heimer R, 2011. Epidemiologic trends and geographic patterns of fatal opioid intoxications in Connecticut, USA: 1997–2007. Drug Alcohol Depend. 115, 221–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall AJ, Logan JE, Toblin RL, Kaplan JA, Kraner JC, Bixler D, Crosby AE, Paulozzi LJ, 2008. Patterns of abuse among unintentional pharmaceutical overdose fatalities. JAMA 300, 2613–20. [DOI] [PubMed] [Google Scholar]
- Hartung DM, Ahmed SM, Middleton L, Van Otterloo J, Zhang K, Keast S, Kim H, Johnston K, Deyo RA, 2017. Using prescription monitoring program data to characterize out-of-pocket payments for opioid prescriptions in a state Medicaid program. Pharmacoepidemiol. Drug Saf 26, 1053–1060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hedegaard H, Warner M, Minino A, 2017. Drug overdose deaths in the United States, 1999–2015. NCHS Data Brief, no 273. Hyattsville MD: National Center For Health Statistics. [Google Scholar]
- Jones CM, McAninch JK, 2015. Emergency department visits and overdose deaths from combined use of opioids and benzodiazepines. Am. J. Prev. Med 49, 493–501. [DOI] [PubMed] [Google Scholar]
- Kandel DB, Hu MC, Griesler P, Wall M, 2017. Increases from 2002 to 2015 in prescription opioid overdose deaths in combination with other substances. Drug Alcohol Depend. 178, 501–511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King NB, Fraser V, Boikos C, Richardson R, Harper S, 2014. Determinants of increased opioid-related mortality in the United States and Canada, 1990–2013: A systematic review. Am. J. Public Health 104, e32–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kolodny A, Courtwright DT, Hwang CS, Kreiner P, Eadie JL, Clark TW, Alexander GC, 2015. The prescription opioid and heroin crisis: a public health approach to an epidemic of addiction. Annu. Rev. Public Health 36, 559–74. [DOI] [PubMed] [Google Scholar]
- Kresina TF, Lubran R, 2011. Improving public health through access to and utilization of medication assisted treatment. Int. J. Environ. Res. Public Health 8, 4102–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lev R, Petro S, Lee A, Lee O, Lucas J, Castillo EM, Egnatios J, Vilke GM, 2015. Methadone related deaths compared to all prescription related deaths. Forensic Sci. Int 257, 347–52. [DOI] [PubMed] [Google Scholar]
- Lev R, Petro S, Lee O, Lucas J, Stuck A, Vilke GM, Castillo EM, 2016. A description of Medical Examiner prescription-related deaths and prescription drug monitoring program data. Am. J. Emerg. Med 34, 510–4. [DOI] [PubMed] [Google Scholar]
- McCoy AB, Wright A, Kahn MG, Shapiro JS, Bernstam EV, Sittig DF, 2013. Matching identifiers in electronic health records: implications for duplicate records and patient safety. BMJ Qual. Saf 22, 219–24. [DOI] [PubMed] [Google Scholar]
- Mercado MC, Sumner SA, Spelke MB, Bohm MK, Sugerman DE, Stanley C, 2018. Increase in drug overdose deaths involving fentanyl-Rhode Island, January 2012-March 2014. Pain Med. 19, 511–523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mertz KJ, Janssen JK, Williams KE, 2014. Underrepresentation of heroin involvement in unintentional drug overdose deaths in Allegheny County, PA. J. Forensic Sci 59, 1583–5. [DOI] [PubMed] [Google Scholar]
- Moyer LA, Boyle CA, Pollock DA, 1989. Validity of death certificates for injury-related causes of death. Am. J. Epidemiol 130, 1024–32. [DOI] [PubMed] [Google Scholar]
- Muhuri PK, Gfroerer JC, Davies MC, 2013. Associations of nonmedical pain reliever use and initiation of heroin use in the United States. CBHSQ Data Rev. https://www.samhsa.gov/data/sites/default/files/DR006/DR006/nonmedical-pain-reliever-use-2013.htm (Accessed 11-09-17). [Google Scholar]
- National Center for Injury Prevention and Control. Centers for Disease Control and Prevention compilation of benzodiazepines, muscle relaxants, stimulants, zolpidem, and opioid analgesics with oral morphine milligram equivalent conversion factors, 2016. version. Atlanta, GA: Centers for Disease Control and Prevention. Published September 2017. http://www.pdmpassist.org/pdf/BJA_performance_measure_aid_MME_conversion.pdf (Accessed 12-20-17). [Google Scholar]
- Pardo B, 2017. Do more robust prescription drug monitoring programs reduce prescription opioid overdose? Addiction 112, 1773–1783. [DOI] [PubMed] [Google Scholar]
- Park TW, Saitz R, Ganoczy D, Ilgen MA, Bohnert AS, 2015. Benzodiazepine prescribing patterns and deaths from drug overdose among US veterans receiving opioid analgesics: Case-cohort study. BMJ. 350, h2698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick SW, Fry CE, Jones TF, Buntin MB, 2016. Implementation of prescription drug monitoring programs associated with reductions in opioid-related death rates. Health Aff. (Millwood) 35, 1324–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paulozzi LJ, Logan JE, Hall AJ, McKinstry E, Kaplan JA, Crosby AE, 2009. A comparison of drug overdose deaths involving methadone and other opioid analgesics in West Virginia. Addiction 104, 1541–8. [DOI] [PubMed] [Google Scholar]
- Paulozzi LJ, Kilbourne EM, Shah NG, Nolte KB, Desai HA, Landen MG, Harvey W, Loring LD, 2012. A history of being prescribed controlled substances and risk of drug overdose death. Pain Med. 13, 87–95. [DOI] [PubMed] [Google Scholar]
- Peterson AB, Gladden RM, Delcher C, Spies E, Garcia-Williams A, Wang Y, Halpin J, Zibbell J, McCarty CL, DeFiore-Hyrmer J, DiOrio M, Goldberger BA, 2016. Increases in fentanyl-related overdose deaths - Florida and Ohio, 2013–2015. MMWR Morb. Mortal. Wkly. Rep 65, 844–9. [DOI] [PubMed] [Google Scholar]
- Raffel KE, Beach LY, Lin J, Berchuck JE, Abram S, Markle E, Patel S, 2018. Naloxone distribution and training for patients with high-risk opioid use in a Veterans Affairs community-based primary care clinic. Perm. J 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rockett IR, Hobbs GR, Wu D, Jia H, Nolte KB, Smith GS, Putnam SL, Caine ED, 2015. Variable classification of drug-intoxication suicides across US States: A partial artifact of forensics? PLoS One 10, e0135296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rudd RA, Seth P, David F, Scholl L, 2016. Increases in drug and opioid-involved overdose deaths - United States, 2010–2015. MMWR Morb. Mortal. Wkly. Rep 65, 1445–1452. [DOI] [PubMed] [Google Scholar]
- Siegler A, Tuazon E, Bradley O’Brien D, Paone D, 2014. Unintentional opioid overdose deaths in New York City, 2005–2010: a place-based approach to reduce risk. Int. J. Drug Policy 25, 569–74. [DOI] [PubMed] [Google Scholar]
- Slavova S, O’Brien DB, Creppage K, Dao D, Fondario A, Haile E, Hume B, Largo TW, Nguyen C, Sabel JC, Wright D, Council of State and Territorial Epidemiologists Overdose Subcommittee, 2015. Drug overdose deaths: Let’s get specific. Public Health Rep. 130, 339–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slavova S, Bunn TL, Hargrove SL, Corey T, 2017a. Linking death certificates, postmortem toxicology, and prescription history data for better identification of populations at increased risk for drug intoxication deaths. Pharmaceut. Med 31, 155–165. [Google Scholar]
- Slavova S, Costich JF, Bunn TL, Luu H, Singleton M, Hargrove SL, Triplett JS, Quesinberry D, Ralston W, Ingram V, 2017b. Heroin and fentanyl overdoses in Kentucky: Epidemiology and surveillance. Int. J. Drug Policy 46, 120–129. [DOI] [PubMed] [Google Scholar]
- Smith-Warner SA, Spiegelman D, Ritz J, Albanes D, Beeson WL, Bernstein L, Berrino F, van den Brandt PA, Buring JE, Cho E, Colditz GA, Folsom AR, Freudenheim JL, Giovannucci E, Goldbohm RA, Graham S, Harnack L, Horn-Ross PL, Krogh V, Leitzmann MF, McCullough ML, Miller AB, Rodriguez C, Rohan TE, Schatzkin A, Shore R, Virtanen M, Willett WC, Wolk A, Zeleniuch-Jacquotte A, Zhang SM, Hunter DJ, 2006. Methods for pooling results of epidemiologic studies: the Pooling Project of Prospective Studies of Diet and Cancer. Am. J. Epidemiol 163, 1053–64. [DOI] [PubMed] [Google Scholar]
- Starrels JL, Becker WC, Weiner MG, Li X, Heo M, Turner BJ, 2011. Low use of opioid risk reduction strategies in primary care even for high risk patients with chronic pain. J. Gen. Intern. Med 26, 958–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stone DM, Holland KM, Bartholow B, Logan JE, LiKamWa McIntosh W, Trudeau A, Rockett IRH, 2017. Deciphering suicide and other manners of death associated with drug intoxication: A Centers for Disease Control and Prevention consultation meeting summary. Am. J. Public Health 107, 1233–1239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Straus MM, Ghitza UE, Tai B, 2013. Preventing deaths from rising opioid overdose in the US - the promise of naloxone antidote in community-based naloxone take-home programs. Subst. Abuse. Rehabil 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suffoletto B, Lynch M, Pacella CB, Yealy DM, Callaway CW, 2018. The effect of a statewide mandatory prescription drug monitoring program on opioid prescribing by emergency medicine providers across 15 hospitals in a single health system. J. Pain 19, 430–438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tennessee Department of Health, 2017. Tennessee chronic pain guidelines for 2017. https://www.tn.gov/content/dam/tn/health/healthprofboards/ChronicPainGuidelines.pdf (Accessed 05-01-18).
- Trinidad JP, Warner M, Bastian BA, Minino AM, Hedegaard H, 2016. Using literal text from the death certificate to enhance mortality statistics: Characterizing drug involvement in deaths. Natl.Vital. Stat. Rep 65, 1–15. [PubMed] [Google Scholar]
- Volkow ND, McLellan AT, 2016. Opioid Abuse in Chronic Pain--Misconceptions and Mitigation Strategies. N. Engl. J. Med 374, 1253–63. [DOI] [PubMed] [Google Scholar]
- Warner M, Trinidad JP, Bastian BA, Minino AM, Hedegaard H, 2016. Drugs most frequently involved in drug overdose deaths: United States, 2010–2014. Natl. Vital Stat. Rep 65, 1–15. [PubMed] [Google Scholar]
- Weimer MB, Korthuis PT, Behonick GS, Wunsch MJ, 2011. The source of methadone in overdose deaths in Western Virginia in 2004. J. Addict. Med 5, 188–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.