Abstract
Mental and behavioral disorders are among the leading contributors to disability among US-residing Latinxs. When treated as a homogeneous group, important disparities in the prevalence of such disorders among Latinx subgroups (e.g., by ethnic heritage) are obscured. However, Latinxs may also be characterized by their acculturative experiences while living in the USA, such as discrimination, neighborhood context and family conflict. Latent Profile Analysis with distal outcomes was used to estimate differences in psychiatric disorder prevalence across acculturative subgroups. Data from 2,541 Latinx participants (age 18 +) in the National Latino and Asian American Study (NLAAS) were used to estimate differences in the proportion of three categories of DSM-IV disorder: depressive, anxiety and substance use by four latent subgroups of Latinxs based on their acculturative experiences. Latinxs reporting more positive acculturative experiences had the lowest prevalence of all three disorders (14.8%, 13.6% and 7.1%, respectively). Those whose lives were characterized by high levels of family conflict and discrimination combined with low levels of social cohesion and neighborhood safety had the highest disorder prevalence (34.0%, 26.6% and 22.5%; all p < 0.01 compared to positive experiences subgroup). Latinxs with moderate levels of discrimination and conflict, along with those with high conflict and cohesion, were better off as compared to those with high negative experiences and low cohesion. These latent subgroups of Latinxs according to their acculturative experiences hold important implications for identifying high-risk groups for developing a psychiatric disorder. Findings also point to the protective role of family and neighborhood cohesion when facing high levels of adversity, which may inform prevention and intervention efforts.
Keywords: Acculturation, Immigration, Latinos, Mental health, Latent profile analysis
Introduction
Mental disorders contribute to a high burden of disability worldwide, with depressive, anxiety and substance use disorders being some of the most common contributors (Murray & Lopez, 1996; World Health Organization (WHO), 2008). Although Latinxs in the USA have traditionally been viewed as having lower prevalence of these disorders (see research on the “Hispanic Health Paradox”, Alcántara et al. (2017)), much of the research has treated Latinxs as a homogeneous racial/ethnic group, ignoring important differences by ethnicity and nativity (Alegría et al., 2007a, b, c). Studies that have taken these subgroups into account have found significant differences in prevalence of mental and behavioral symptomatology across Latinx subgroups (Alcántara et al., 2014; Alegría et al., 2007a, b, c; Fortuna et al., 2007; Torres et al., 2012; Wassertheil-Smolle et al., 2014). These findings suggest that there may be important distinctions in other constructs known to be associated with disorder, such as discrimination and family cultural conflict (Cobb et al., 2017; Cook et al., 2009; Mulvaney-Day et al., 2007; Rivera et al., 2008; Torres et al., 2012), by these subgroups. Little attention has been paid to potentially meaningful subgroups within the Latinx population that are more challenging to characterize and impossible to directly observe.
An unobserved subgroup of interest may be Latinxs with distinct types of acculturative experiences while living in the USA. Acculturation is the dynamic process by which immigrants adopt the norms, values, attitudes and behaviors of a new or receiving culture over time (Castro et al., 2010; Lara et al., 2005; Schwartz et al., 2010). As the field has progressed, scholars have moved away from the idea of assimilation, which simply considers adoption of the receiving culture, to a multidimensional conceptualization of acculturation that is influenced by the interactional context in which the migrant is situated (Schwartz et al., 2010). In this vein, Berry’s model of acculturation (2003) incorporates the concept of enculturation, or the process through which immigrants retain the norms of and identification with their culture of origin (Guarnaccia et al., 2007), categorizing individuals into four acculturative groups: assimilated, integrated, marginalized and separated. Further, Berry (1988) posits that while immigrants are exposed to risk factors across all phases of the migration process, primary prevention opportunities are most available during settlement. And although mental health problems often arise during the acculturation process, they are not an inevitable outcome (Berry, 1988). Thus, successful adaptation is possible, but identifying groups at risk of suboptimal adaptation is essential to target preventive interventions appropriately. While the complexity of acculturation, its dynamic nature across the life course, and its measurement warrants extensive discussion, it is beyond the scope of the current analysis. For a thorough discussion of the extant literature, see Schwartz et al. (2010) and Abraído-Lanza et al., (2006, 2016).
One well-replicated epidemiologic finding in acculturation research among nationally representative samples is that, on average, health deteriorates as migrants spend more time in their immigrated country. Thus, as longer time spent living in the USA has been consistently associated with poorer mental health among Latinxs (Alcántara et al., 2014; Alegría et al., 2007a, b, c), acculturation is of interest when investigating health disparities among Latinx immigrants (Thomson & Hoffman-Goetz, 2009). Prior studies have evaluated Berry’s model using latent variable methods (Bulut & Gayman, 2016; Fox et al., 2013; Schwartz & Zamboanga, 2008), but these conceptualizations often ignore other experiences inextricably linked to the acculturation process such as discrimination or family conflict, which can be considered part of the interactional context in which acculturation occurs. Minorities and immigrants navigating a new culture are likely to undergo these other experiences (e.g., discrimination; American Psychological Association, 2012; Kessler et al., 1999). Because they cannot be disentangled from the acculturative process, these experiences may be equally important in the development of disorder and design of interventions to prevent disorder in these populations. To our knowledge, no study has explored the role of acculturation and related acculturative experiences in mental and behavioral disorder among Latinx communities in the USA while allowing for the complexity and multidimensionality of acculturation to be modeled appropriately.
Consistent with a socio-ecological framework (Bronfenbrenner, 1979), acculturative experiences may be conceptualized as not just level of acculturation or enculturation, but also those other experiences or contexts that immigrants or minorities encounter that may be related to acculturation level. These experiences may include discrimination, neighborhood context and family environment. Research has shown that acculturation and these related experiences are associated with negative mental health outcomes (Alcántara et al., 2014; Blanco et al., 2013; Alexander Ortega et al., 2000; Rivera et al., 2008; Valencia-Garcia et al., 2012). Because these acculturative experiences are correlated, it stands to reason that they may cluster in meaningful ways. If so, distinct subgroups of Latinxs that tend to experience and interact with their surroundings in a certain way may be more likely to develop certain disorders. Further, subgroups may be differentially related to different types of disorder, making it important to examine specific mental and behavioral categories rather than any psychiatric disorder as a whole. Identifying high-risk or resilient acculturative subgroups can provide important clues regarding etiologic mechanisms as well as places to intervene.
This study builds off of prior work which identified four latent acculturative experience profiles of Latinxs in the National Latino and Asian American Study (Roth et al., 2019). The primary objective of the present study is to determine whether there are differences in the prevalence of depressive, anxiety and substance use disorders after accounting for sociodemographic characteristics. A secondary objective is to estimate the direct association between Latinx ethnic and generational subgroups and the three disorder categories after accounting for acculturative experiences. Ultimately, the findings have the potential to inform targeted interventions to prevent development of disorder among a diverse and growing population in the USA.
Methods
Participants and Procedure
Data come from the National Latino and Asian American Study (NLAAS), a nationally representative, probability-based survey conducted between 2001 and 2003 as part of the Collaborative Psychiatric Epidemiology Surveys funded by the National Institute of Mental Health (Heeringa et al., 2004; Pennell et al., 2004). The NLAAS target population was civilian, non-institutionalized adults (18 years or older) of Latinx or Asian origin in the contiguous USA. Investigators used a stratified, multiframe probability sampling strategy to oversample these minority groups (Pennell et al., 2004), making it the first nationally representative study powered to examine acculturation and psychiatric disorder by population subgroups. Lay interviewers administered in-person, computer-assisted structured interviews at the respondent’s home. The final response rate for the Latinx sample was 75.5% (Heeringa et al., 2004). These analyses included 2,541 NLAAS participants of Latinx ethnicity after excluding 13 individuals with unknown generational status.
Measures
All non-diagnostic measures are described elsewhere, including reliability results (Alegría et al., 2004). Questionnaires for the Latinx sample were adapted, translated into Spanish, and back-translated to ensure cross-cultural equivalency (Alegría et al., 2004). Respondents could complete the interview in the language of their choice. All scales described below can be reviewed in full in Online Resource 1.
Indicators of Acculturative Experiences
Guided by acculturation literature which encourages using a multidimensional definition of acculturation and the context of reception from a socio-ecological perspective (Bronfenbrenner, 1979; Schwartz et al., 2010), five scales were chosen to represent the latent construct of acculturative experiences. Scales were either measures of acculturation or enculturation, or related acculturative experiences across different ecological levels with known associations with disorder and acculturation in the literature. Prior research (Roth et al., 2020) used exploratory factor analysis in an exploratory structural equation modeling framework to generate factor scores after accounting for measurement invariance by generational status. This work resulted in nine indicators of acculturative experiences, detailed below.
Language
Two correlated latent factors were derived from the Language Proficiency and Language Preference scales (Felix-Ortiz et al., 1994; 6 items): Spanish and English. Higher factor scores indicate greater language use and preference.
Ethnic Identity
Ethnic identity refers to the degree to which individuals feel connected to others with the same country of origin (Phinney, 1990). The Ethnic Identity scale (Guarnaccia et al., 2007; 4 items) resulted in a single factor. Higher scores indicate increased identification with one’s racial/ethnic group.
Neighborhood Context
Two correlated factors underlaid this 7-item scale: Neighborhood Cohesion and Neighborhood Danger, reflecting the two subscales: The Neighborhood Social Cohesion (4 items) and Neighborhood Safety (3 items) scales (Bearman et al., 1997; National Institute of Mental Health, 1994; Sampson et al., 1997). Higher Cohesion and Danger scores indicate the respondent perceived their neighborhood as being more cohesive and dangerous, respectively.
Family Context
This 15-item measure had two underlying factors: Family Cohesion and Family Conflict. Cohesion reflected the 7-item Family Pride and 3-item Family Cohesion subscales (Olson, 1986, 1989), with higher scores indicating greater feelings of familial respect/closeness and shared values/beliefs. The conflict factor reflected the 5-item Family Conflict subscale (Cervantes et al., 1991), which addresses cultural conflict between respondents and their families. Higher scores indicate increased familial cohesion and conflict, respectively.
Discrimination
Two latent discrimination factors were identified: Observed and Perceived. The former was characterized by the 9-item Everyday Discrimination scale (Jackson et al., 1995; Williams et al., 1997), the latter by three items adapted from Vega and colleagues (Vega et al., 1993). Higher scores indicate greater discrimination, whether observed in day-to-day life (e.g., harassment) or perceived as attributable to race/ethnicity.
Latent Profiles of Latinxs’ Acculturative Experiences
Individuals were classified into similar subpopulations or “profiles” using Latent Profile Analysis (LPA) with an expectation-maximum algorithm. This method helps explain covariation between observed indicator variables (Masyn, 2013; Nylund et al., 2007). Prior work identified four latent profiles of Latinxs in the sample based on nine factor scores derived from more than 40 item responses in five scales on acculturation and related experiences described above (language, ethnic identity, neighborhood context, family context, and discrimination; Roth et al., 2019). LPA seeks to identify unobserved groups or “profiles” of individuals who are similar to one another based on a set of observed indicators (Gibson, 1959; Goodman, 1974; Lazarsfeld & Henry, 1968). As a person-centered approach, it helps capture underlying heterogeneity in a given population (Gibson, 1959; Lanza & Rhoades, 2013; Masyn, 2013; Nylund et al., 2007), thus identifying meaningful at-risk or resilient subpopulations. Individuals are given a score indicating the probability of membership for each profile, which helps account for measurement error. Factors within scales (e.g., neighborhood cohesion and danger) were allowed to be correlated. Fit statistics (log likelihood, Akaike’s Information Criteria, Bayesian Information Criteria, Lo-Mendell-Rubin Likelihood Ratio Test), smallest profile size, and substantive interpretation guided profile selection during the profile enumeration process. High entropy (0.966) confirmed that individuals could be classified into their most likely profile with high confidence (Clark & Muthén, 2009). For fit statistics for ah models, see Table 2 in Roth et al. (2019).
As previously reported (Roth et al., 2019), the four profiles were most differentiated by family context, neighborhood context, and discrimination: 1) Positive Experiences (69% of the sample), 2) Cohesive-Conflict (17%), 3) Marginalized-Conflict (9%), and 4) Marginalized (5%). Briefly, the Positive Experiences profile was characterized by the lowest levels of discrimination and family conflict, the highest levels of ethnic identity, and the highest neighborhood cohesion and safety. The Cohesive-Conflict profile had similarly high levels of cohesion but increased neighborhood danger and the highest levels of discrimination and family conflict. It had medium levels of ethnic identity. The Marginalized-Conflict profile had similarly high discrimination and conflict to the Cohesive-Conflict group, but significantly lower levels of family and neighborhood cohesion. Finally, the Marginalized profile had the lowest levels of cohesion and moderate levels of discrimination and conflict. Ethnic identity levels were similarly low in both Marginalized groups. No differences in English language were observed across profiles. See Online Resource 2 for mean factor scores by profile. The methods and sample characteristics by most probable profile membership (the profile an individual is most likely to belong to based on their indicator responses) are described in detail elsewhere (Roth et al., 2019, 2020).
Outcomes
Mental and behavioral disorders were assessed via a modified version of the World Mental Health Composite International Diagnostic Interview (WMH-CIDI; Kessler et al., 2004) to obtain the following Diagnostic and Statistical Manual, Fourth Edition (DSM-IV; American Psychiatric Association 1994) psychiatric diagnoses: any Depressive Disorder (Major Depressive Disorder/Episode or Dysthymia); any Anxiety Disorder (Post Traumatic Stress Disorder, Generalized Anxiety Disorder, Panic Disorder, Agoraphobia or Social Phobia); and any Substance Use Disorder (SUD; Alcohol or Drug Abuse/Dependence). Self-reported age of onset of disorder was created for each category, using the earliest age if criteria for multiple disorders were met.
Covariates
Sociodemographics
Characteristics included age at interview, gender, education (less than high school, high school, some college and college degree) and marital status (married/cohabitating, previously married [i.e., divorced/separated/widowed] and never married).
Ethnic Heritage
Self-reported ancestry was collapsed into four Latinx subgroups: Puerto Ricans (n = 495), Mexicans (n = 868), Cubans (n = 577) and Ah Others (n = 614).
Generational Status
Four categories of generational status were created: first generation (arriving in the USA at age 13 or older, n = 1257), 1.5 generation (arriving when less than age 13, n = 365), second generation (US-born with at least one parent foreign-born, n = 522) and third generation (US-born, both parents US-born, n = 397). The distinction between the first and 1.5 generations is important from a developmental perspective, as it allows for differences based on age of migration to the USA, which has been linked to increased prevalence of psychiatric disorder (Alegría et al., 2007a, b, c; Vega et al., 2004).
Statistical Analysis
Distal outcomes of psychiatric disorder categories were incorporated into the final structural model chosen from prior work (Roth et al., 2019). These categories (any depressive disorder, any anxiety disorder and any substance use disorder) were added as distal outcomes of profile membership using the BCH method (Bolck et al., 2004) laid out by Asparouhov and Muthén (2014b). This approach uses weights to avoid profile shifting after the addition of external variables in the structural component. In addition, these weights reflect the uncertainty or measurement error associated with profile membership as a latent variable. Simulations have shown that the modified BCH method outperforms other 3-step methods when estimating the association between profile membership and a distal outcome, particularly when its variance differs significantly across profiles (Asparouhov & Muthén, 2014a, b; Bakk et al., 2013; Bakk & Vermunt, 2016).
This approach was carried out manually in Mplus Version 8 (Muthén & Muthén, 1998). First, the unconditional latent 4-profile model was estimated without covariates. From that model, BCH weights were created and saved. Finally, the auxiliary structural model including predictors, outcomes and direct effects was estimated as a multiple group model using the BCH weights. Here, the groups or latent profiles are treated as “known” to prevent profile shifting, but using the weights allows for measurement error.
Carrying out the steps manually allows incorporation of direct effects from each predictor (e.g., sex, generational status) on the outcome. We used a Wald test and pairwise comparison z-tests to assess differences in the prevalence of each outcome across the four acculturative experiences profiles. The association between the outcome and each profile is controlled for the influence of all the covariates (sex, age, education category, marital status, Latinx ethnic heritage and generational status) on both latent profile membership and the three disorder categories. Online Resource 3 depicts a path diagram of the final structural model. In addition to statistical analyses being conducted in Mplus Version 8 (Muthén & Muthén, 1998), RStudio (RStudio Team, 2015), in particular the MplusAutomation R package (Hallquist & Wiley, 2018) was utilized for data management and graphics. Statistical significance was at the 0.05 level.
Results
The analytic sample was comprised of 490 (19.3%) Puerto Ricans, 576 (22.7%) Cubans, 862 (33.9%) Mexicans and 613 (24.1%) from other Latinx countries (Table 1). Participants were approximately 40 years of age, mostly female (55.8%), married or cohabitating (62.6%), and about half were first-generation immigrants arriving at age 13 or older (49.5%). A large percentage did not complete high school (38.7%). Eighteen percent (n = 460) of the total sample had ever met criteria for a DSM-IV depressive disorder, with an average first onset at 26.5 years of age (sd = 15.5). Fewer participants ever met criteria for an anxiety disorder (n = 429, 16.9%) or a substance use disorder (n = 241, 9.5%) in their lifetime. Average age of onset was younger for both anxiety and substance use disorders (18.7 years, sd = 13.8; 21.9 years, sd = 7.8, respectively). Almost one third of participants met criteria for any lifetime disorder (n = 779). Among those ever meeting disorder criteria, 471 (18.5%) individuals only met criteria for one disorder, whereas 265 (10.4%) met criteria for two and 43 (1.7%) for all three (data not shown).
Table 1.
Sociodemographic Characteristics and Lifetime DSM-IV Disorder Prevalence in Overall Sample and by Disorder Category
| Overall Sample |
Depressive Disorder |
Anxiety Disorder |
Substance Use Disorder |
|||||
|---|---|---|---|---|---|---|---|---|
| 2541 (100%) | 460 (18.1%) | 429 (16.9%) | 241 (9.5%) | |||||
| Age in years, mean (sd) | 40.61 | 15.63 | 41.62 | 15.76 | 41.82 | 14.53 | 38.74 | 12.94 |
| Gender, N (%) | ||||||||
| Male | 1123 | 44.2 | 148 | 32.2 | 139 | 32.4 | 179 | 74.3 |
| Female | 1418 | 55.8 | 312 | 67.8 | 290 | 67.6 | 62 | 25.7 |
| Education, N (%) | ||||||||
| Less than high school | 984 | 38.7 | 200 | 43.5 | 178 | 41.5 | 85 | 35.3 |
| High school | 632 | 24.9 | 104 | 22.6 | 106 | 24.7 | 70 | 29.0 |
| Any post-secondary | 565 | 22.2 | 101 | 22.0 | 100 | 23.3 | 63 | 26.1 |
| College degree or more | 360 | 14.2 | 55 | 12.0 | 45 | 10.5 | 23 | 9.5 |
| Marital Status, N (%) | ||||||||
| Married | 1591 | 62.6 | 252 | 54.8 | 253 | 59.0 | 146 | 60.6 |
| Previously Married | 477 | 18.8 | 127 | 27.6 | 97 | 22.6 | 41 | 17.0 |
| Never Married | 473 | 18.6 | 81 | 17.6 | 79 | 18.4 | 54 | 22.4 |
| Ethnic Heritage, N (%) | ||||||||
| Puerto Rican | 490 | 19.3 | 113 | 24.6 | 101 | 23.5 | 63 | 26.1 |
| Cuban | 576 | 22.7 | 109 | 23.7 | 97 | 22.6 | 34 | 14.1 |
| Mexican | 862 | 33.9 | 137 | 29.8 | 130 | 30.3 | 95 | 39.4 |
| Other Latinx | 613 | 24.1 | 101 | 22.0 | 101 | 23.5 | 49 | 20.3 |
| Generational Status, N (%) | ||||||||
| 1st Generation | 1257 | 49.5 | 212 | 46.1 | 199 | 46.4 | 60 | 24.9 |
| 1.5 Generation | 365 | 14.4 | 68 | 14.8 | 66 | 15.4 | 26 | 10.8 |
| 2nd Generation | 522 | 20.5 | 92 | 20.0 | 88 | 20.5 | 78 | 32.4 |
| 3rd Generation | 397 | 15.6 | 88 | 19.1 | 76 | 17.7 | 77 | 32.0 |
| Any Depressive Disorder | ||||||||
| No, N (%) | 2081 | 81.9 | – | – | 199 | 46.4 | 155 | 64.3 |
| Yes, N (%) | 460 | 18.1 | – | – | 230 | 53.6 | 86 | 35.7 |
| Age of Onset, mean (sd) | 26.49 | 15.46 | – | – | 25.9 | 14.46 | 21.94 | 12.01 |
| Any Anxiety Disorder | ||||||||
| No, N (%) | 2112 | 83.1 | 230 | 50 | – | – | 163 | 67.6 |
| Yes, N (%) | 429 | 16.9 | 230 | 50 | – | – | 78 | 32.4 |
| Age of Onset, mean (sd) | 18.69 | 13.82 | 19.25 | 14.36 | – | – | 14.09 | 8.73 |
| Any Substance Use Disorder | ||||||||
| No, N (%) | 2300 | 90.5 | 374 | 81.3 | 351 | 81.8 | – | – |
| Yes, N (%) | 241 | 9.5 | 86 | 18.7 | 78 | 18.2 | – | – |
| Age of Onset, mean (sd) | 21.85 | 7.84 | 21.74 | 6.95 | 21.19 | 6.98 | – | – |
| Any Disorder, N (%) | ||||||||
| No | 1762 | 69.3 | – | – | – | – | – | – |
| Yes | 779 | 30.7 | – | – | – | – | – | – |
DSM Diagnostic and Statistical Manual, sd standard deviation
Participants ever meeting criteria for a depressive disorder were more likely to be female and had received less education than the sample as a whole. They were also more likely to be previously married. Fifty percent had ever met criteria for an anxiety disorder, and almost one fifth (18.7%) ever met criteria for a substance use disorder. Those ever meeting criteria for an anxiety disorder were similar in sociodemographics to individuals with a depressive disorder. Over half had ever met criteria for a depressive disorder (53.6%) and 18.2% met criteria for a substance use disorder. Individuals with a substance use disorder tended to be slightly younger, were overwhelmingly male, and more likely to have never married than those with an anxiety or depressive disorder. A larger proportion of these individuals were Mexican and they were much more likely to be born in the USA. Approximately one-third (35.7%) had ever met criteria for a depressive disorder and one third met criteria for an anxiety disorder at some point in time in their life (these categories are not mutually exclusive).
Table 2 displays the direct effects of all model covariates on each disorder category. After adjusting for profile membership, females were almost 80 percent more likely to have a depressive or anxiety disorder and 80 percent less likely to have a substance use disorder. Persons with a college degree or more were approximately 40 percent less likely to have a disorder regardless of type. Previously married individuals were 1.56 times more likely to meet criteria for a depressive disorder at some time in their lives (95% CI: 1.20–2.03).
Table 2.
Direct Effects of Covariates on Lifetime Disorder Categories Adjusted for Latent Profile Membership of Acculturative Experiences (n = 2541)
| Any Depressive Disorder |
Any Anxiety Disorder |
Any Substance Use Disorder |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| 460 (18.1%) | 429 (16.9%) | 241 (9.5%) | |||||||
|
| |||||||||
| OR | 95% CI | p-value | OR | 95% CI | p-value | OR | 95% CI | p-value | |
| Age in years | 1.00 | (0.99–1.01) | 0.665 | 1.01 | (1.00–1.01) | 0.107 | 1.01 | (1.00–1.02) | 0.207 |
| Sex | |||||||||
| Male | REE | – | – | REF | – | – | REF | – | – |
| Female | 1.77 | (1.42–2.21) | <0.001 | 1.78 | (1.42–2.24) | <0.001 | 0.21 | (0.15–0.29) | <0.001 |
| Education | |||||||||
| Less than high school | REE | – | – | REF | – | – | REF | – | – |
| High school | 0.70 | (0.53–0.93) | 0.015 | 0.87 | (0.65–1.15) | 0.315 | 0.97 | (0.67–1.41) | 0.867 |
| Any post-secondary | 0.77 | (0.58–1.02) | 0.067 | 0.90 | (0.67–1.20) | 0.468 | 0.96 | (0.65–1.41) | 0.828 |
| College degree or more | 0.65 | (0.45–0.92) | 0.016 | 0.60 | (0.41–0.87) | 0.007 | 0.58 | (0.34–0.98) | 0.042 |
| Marital Status | |||||||||
| Married | REF | – | – | REF | – | – | REF | – | – |
| Previously Married | 1.56 | (1.20–2.03) | 0.001 | 1.02 | (0.76–1.36) | 0.915 | 1.03 | (0.68–1.58) | 0.880 |
| Never Married | 0.91 | (0.67–1.23) | 0.549 | 0.96 | (0.71–1.31) | 0.816 | 0.92 | (0.62–1.36) | 0.672 |
| Ethnic Heritage | |||||||||
| Puerto Rican | REF | – | – | REF | – | – | REF | – | – |
| Cuban | 0.97 | (0.69–1.35) | 0.856 | 0.92 | (0.66–1.29) | 0.626 | 0.82 | (0.49–1.39) | 0.461 |
| Mexican | 0.66 | (0.49–0.89) | 0.007 | 0.72 | (0.53–0.98) | 0.036 | 1.04 | (0.71–1.52) | 0.85 |
| Other Latinx | 0.71 | (0.52–0.97) | 0.034 | 0.82 | (0.60–1.13) | 0.235 | 0.92 | (0.59–1.45) | 0.72 |
| Generation | |||||||||
| 1st Generation | REF | – | – | REF | – | – | REF | – | – |
| 1.5 Generation | 1.13 | (0.82–1.57) | 0.458 | 1.22 | (0.88–1.70) | 0.236 | 1.58 | (0.97–2.57) | 0.069 |
| 2nd Generation | 1.07 | (0.79–1.45) | 0.654 | 1.17 | (0.86–1.58) | 0.323 | 3.70 | (2.48–5.52) | <0.001 |
| 3rd Generation | 1.47 | (1.08–2.01) | 0.016 | 1.30 | (0.94–1.80) | 0.117 | 4.73 | (3.13–7.15) | <0.001 |
Data are from the National Latino and Asian American Study (n = 2,541)
Estimates in bold are significant at the p<0.05 level
OR Odds Ratio, CI Confidence Interval
Cubans and Puerto Ricans had similar odds of disorder for all categories. Mexicans and other Latinxs were at least one third less likely to have a depressive disorder (OR = 0.66, 95% CI: 0.49–0.89; OR = 0.71, 95% CI: 0.52–0.97, respectively) than other Latinx ethnicities. Mexicans were also less likely to ever meet criteria for an anxiety disorder (OR = 0.72, 95% CI: 0.53–0.98). There were no differences in the odds of lifetime substance use disorder by Latinx heritage after accounting for acculturative experiences and other sociodemographic characteristics. Only third-generation Latinxs had an increased odds of a depressive disorder (OR = 1.47, 95% CI: 1.08–2.01). Latinxs born in the USA had over three or four times the odds of ever meeting substance use disorder criteria, and those arriving as children were approximately 50% more likely to meet SUD criteria than those arriving as adolescents or adults, although the result was marginally significant (OR = 1.58, 95% CI: 0.97–2.57).
Figure 1 graphically displays the estimated proportion of individuals ever meeting criteria for each disorder category by latent profile. The prevalence of all disorder categories differed significantly across acculturative experiences profiles even after adjusting for sociodemographic characteristics (Wald test: depressive χ2 = 40.392, anxiety χ2 = 36.230, substance use χ2 = 34.330; all p < 0.0001; Online Resource 4). Latinxs belonging to the Positive Experiences profile had the lowest proportion with a disorder for all disorder categories: 14.8% ever met criteria for a depressive disorder, 13.6% for an anxiety disorder, and 7.1% for a substance use disorder. Regardless of disorder category, those in the Marginalized Conflict profile had much higher disorder prevalence (34.0% had a depressive disorder, 26.6% an anxiety disorder and 22.5% a substance use disorder). The Cohesive-Conflict and low-conflict Marginalized profiles tended to look similar, having higher disorder prevalence than Latinxs with Positive Experiences but lower than the Marginalized Conflict profile. This pattern was particularly true for depressive and substance use disorders. The two largest differences were seen between the Positive Experiences and the Marginalized Conflict profiles for depressive (difference = −0.192, p < 0.001;) and substance use disorders (difference = −0.155, p < 0.001). Fewer differences between profiles were observed for lifetime prevalence of anxiety disorders, with no differences between the Marginalized and Marginalized Conflict profiles or between the Cohesive-Conflict and Marginalized Conflict profiles.
Fig. 1.
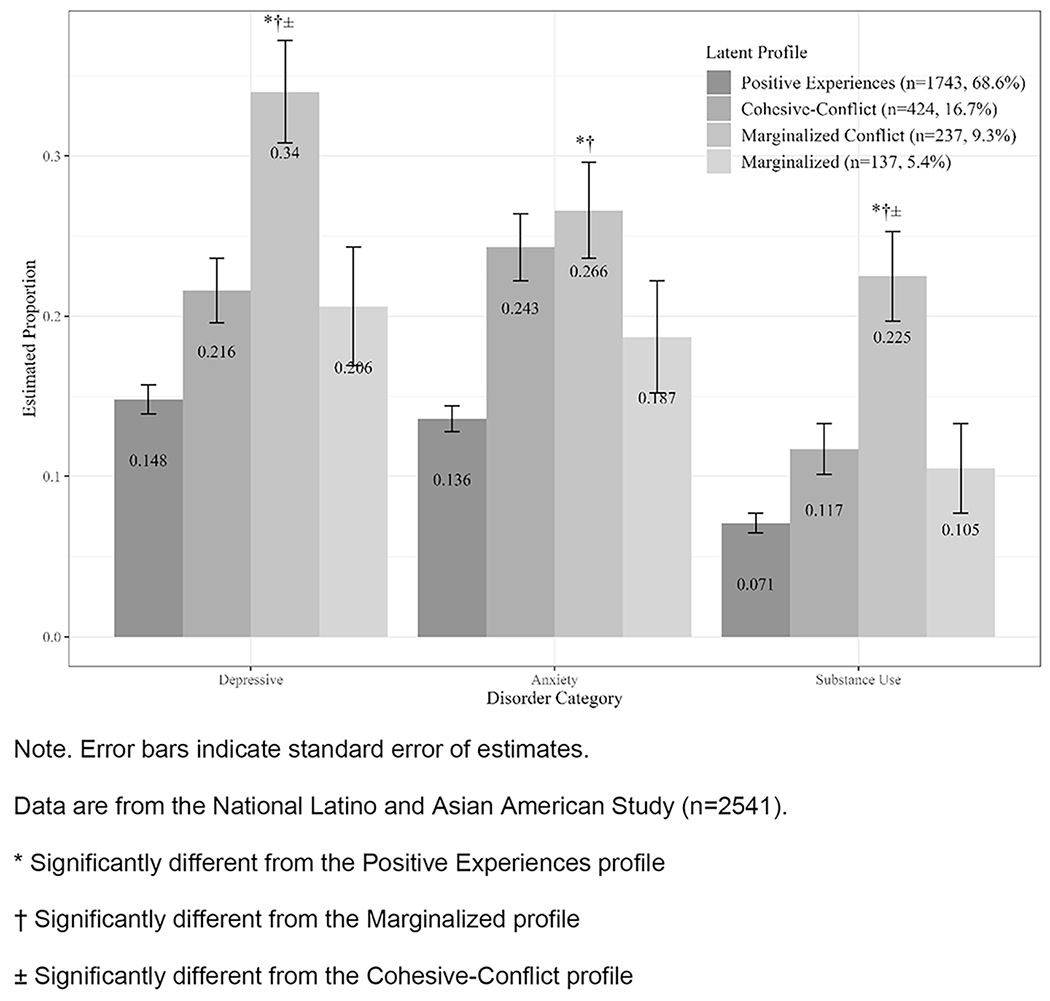
Proportion with Lifetime Depressive, Anxiety, and Substance Use Disorder by Latent Profiles
Discussion
Few studies have reported on lifetime prevalence of categories of DSM diagnoses of Latinxs in the United States. We found that Latinxs in the National Latino and Asian American Study had similar lifetime prevalence estimates of disorder as compared to other nationally representative studies of Latinxs (Karno et al., 1987; Kessler et al., 1994; Vega et al., 1998). Weighted lifetime prevalence of depressive, anxiety and substance use disorders from the NLAAS have been reported elsewhere (Alegría et al., 2007a, b, c), which were similar to our estimates. Our sample also had a high burden of comorbidity, with approximately 12 percent meeting criteria for two or more disorder categories in their lifetime. As expected, depressive and anxiety disorders were highly comorbid. A large proportion of those with a substance use disorder were also likely to have either a depressive or anxiety disorder, reinforcing the notion of a significant health burden among Latinxs affected by a mental disorder.
Latent profiles of acculturative experiences were significantly related to lifetime diagnoses of disorder. This strong association lends credibility to the underlying latent construct of acculturation and other related experiences identified in prior work (Roth et ah, 2019). Of note, the prominence of contextual factors in our acculturative experiences construct highlights the importance of these influences on the mental health of Latinxs and immigrants. It is unsurprising that Latinxs having overwhelmingly positive experiences, whether it be lower levels of discrimination and conflict or higher levels of neighborhood and family cohesion, have significantly lower prevalence of disorder. This finding also underscores that many Latinxs can flourish during the acculturation process. However, there are striking differences among Latinxs whose lives are characterized by less favorable experiences. In particular, the difference in depressive and substance use disorder prevalence between the Marginalized Conflict and Cohesive-Conflict profiles suggests a potential buffering effect of social cohesion in the face of conflict, discrimination and less safe neighborhood environments. Latinxs in both of these profiles reported similarly elevated levels of family conflict, discrimination, and lack of neighborhood safety. The main distinguishing feature was the distinct levels of cohesion, particularly among the family, with the Cohesive-Conflict profile having levels of family cohesion on par with the Positive Experiences profile. It is possible that this difference may contribute to the decreased disorder prevalence among the Cohesive-Conflict group through strengthened family or neighborhood social ties.
In light of the high levels of comorbidity in our sample, those Latinxs experiencing moderate to high levels of discrimination and conflict, coupled with low social cohesion, may be contributing to a large proportion of disorder in the population. Prior research in the NLAAS has shown this comorbidity of depressive and anxiety disorders does not differ by Latinx country of origin (Ortega et ah, 2006), but few psychiatric comorbidity studies have been conducted in this sample. Given the synergistic effects observed between the presence of stressors and availability of supportive resources at various socio-ecological levels for all three disorder categories, both physiological and psychosocial mechanisms could be interacting to produce multiple disorders. Thus, future work should specifically investigate the relationship between comorbidity and profile membership in this framework, paying particular attention to understanding the underlying mechanisms at play.
The absence of a direct relationship between ethnic heritage and having a substance use disorder implies that any crude differences in SUD prevalence by Latinx country of origin may be entirely accounted for by the experiences Latinxs have in the USA and other sociodemographic characteristics. Conversely, the strong dose–response effect of generational status on substance use disorder prevalence supports the well-replicated immigrant health paradox as it pertains to substance use problems (Alegría et al., 2006, 2007a, b, c, 2008; Burnam et al., 1987; Escobar et al., 2000; Grant et al., 2004; Vega et al., 1998). While these results clearly indicate that acculturation and other experiences (whether positive or negative) have important implications with regard to mental health, other factors seem to be at play beyond the constructs assessed in this study. One such possibility is access to alcohol or other substances, which is necessary to develop a SUD. This prerequisite is a key distinction between risk for substance-related problems and anxiety or depression, and may be related to time spent in the USA (e.g., knowing how and where to obtain substances).
Differences in associations by ethnicity were also seen for depressive and anxiety disorders. In particular, after accounting for acculturative experiences, a strong inverse relationship remained between Mexicans and both depression and anxiety as compared to Puerto Ricans. The fact that this association persists for Mexicans suggests that there may be additional factors unique to Mexicans that are not accounted for in this model. This is particularly noteworthy given that Cubans have consistently been shown to have the lowest prevalence of distress and disorder among all Latinx ethnic subgroups (Guarnaccia et al., 2002). It may be that Mexicans have other sources of resilience, such as perceptions of social mobility in society, that can confer extra protection against life’s stressors (Alcántara et al., 2014; American Psychological Association, 2012; Gonzalez-Barrera & Lopez, 2013). Future research should explore these differences.
This study’s findings have important implications for preventive interventions among US Latinxs. First, universal prevention programing could focus on social support for immigrants and strengthening family relationships to reduce conflict and decrease feelings of marginalization. In a multitiered prevention approach, our research has shown that Latinxs should not be treated as a homogenous group. Observable characteristics such as country of origin should not overshadow more meaningful characteristics that are less easily measured. The latent profiles provide clues to modifiable factors strongly associated with disorder, as well as the identification of high-risk and resilient groups. Second, by expanding our acculturative construct to include multiple socio-ecological levels, we uncovered the need to develop, implement, and rigorously test prevention programs targeting processes at these levels, rather than solely focusing on modifying individual-level factors. In particular, family and neighborhood environments may be important contexts that can be targeted to improve mental health outcomes among Latinxs and immigrants. Notably, the large difference in disorder prevalence between the Latinx profiles with similarly high levels of family conflict but significantly different cohesion offers a clear modifiable factor on which preventive interventions can operate. Finally, the field must consider the interactional contexts of US Latinxs when culturally adapting programs, as cultural adaptation and humility are key to promoting positive health outcomes and can improve efficacy of prevention and intervention efforts (Griner & Smith, 2006; Kutob et al., 2013). Given the influence interpersonal relationships exert on Latinxs’ mental health, ensuring cultural humility (Tervalon & Murray-Garcia, 1998) among prevention personnel continues to be a crucial yet too-often overlooked part of prevention programming.
Study Limitations
This study is not without limitations. The NLAAS data are self-report and are therefore vulnerable to recall or social desirability bias. Our analyses did not explore whether the direct effects of heritage and generational status vary by profile. This may be the case and should be investigated in future work. Also, as information on documentation status was not available for this sample, effects of being undocumented on disorder were not accounted for. The prevalence of comorbidity in the sample was high, particularly between depressive and anxiety disorders, but its association with acculturative experiences was not explored. Because a large proportion of our sample met diagnosis for two or more disorders, future work should explore the importance of comorbidity and how this is affected by acculturative experiences. Similarly, although the findings point to possible mechanisms contributing to and buffering against disorder, constructs such as resilience are complex and vary both by context and type of stressor. Guided by conceptual models (e.g., the Transactional Stress-Coping Model (Lazarus & Folkman, 1984)), future work should explore how resilience operates in each acculturative profile, as the processes are likely heterogeneous depending on a person’s acculturative experiences and coping resources. Additionally, these data are approximately 20 years old. In light of current issues regarding immigration, the findings here may not be generalizable to the present day. However, given the more intense and often negative sociopolitical climate, combined with more ubiquitous exposure via social media and the internet, it would not be unexpected for more of the Latinx community to fall into one of the three profiles not characterized by positive experiences.
Finally, no causal statements can be made, as all data are cross-sectional. Further, because this is a cross-sectional study, it is possible that individuals with a mental or behavioral disorder may be more likely to report discrimination, conflict or other acculturative stressors as a result of their mental illness. This may lead to biased results. There is also a possibility that there are reciprocal processes in play, and that the presence of mental illness actually leads to increased levels of acculturative stress and other negative experiences. As acculturation is a dynamic process, future work should look at longitudinal trajectories of these latent acculturative experiences profiles and how they impact mental and behavioral health.
Conclusion
There is a gap in the current literature in how the construct of acculturation is conceptualized and modeled, given its complexity and multidimensionality. Despite the limitations, to our knowledge this study is the first to look at the relationship between acculturative experiences and DSM diagnoses of common mental and behavioral disorders in a nationally representative sample of Latinxs using a latent variable framework and informed by a socio-ecological perspective. The associations between the latent construct of acculturative experiences accounted for both the unobserved nature of the complex constructs of interest (e.g., discrimination and family environment) and the effects of relevant covariates on profile membership and lifetime disorder. These analyses also do not collapse disorders into one broad category, which is important particularly seen here in the adjusted associations between ethnic heritage, generational status, and specific disorders. The NLAAS continues to be the largest nationally representative study of Latinxs with data on acculturation and other experiences and mental and behavioral disorder, allowing exploration of associations by important subgroups of interest. This study’s findings highlight modifiable risk and protective factors for mental and behavioral disorders among Latinxs and immigrants, as well as the identification of high-risk and resilient subgroups. In particular, the finding that supportive resources may lessen the negative effects of exposure to significant acculturative stressors points to how bolstering those resources may be key to lessening the burden of psychiatric disorder in Latinx individuals attempting to navigate two cultures. Finally, in light of the nature of the latent acculturative experiences construct being primarily defined by contextual (rather than individual) factors, family and neighborhood contexts, including their interactive effects, may be key places to locate preventive interventions to improve Latinx and immigrant mental and behavioral health. For example, Familias Unidas (Coatsworth et al., 2002) is an evidenced-based program designed to increase family functioning and decrease adolescent substance use. Future research should test these interventions in the context of established conceptual models to continue to shed light on the underlying mechanisms which produce disorder in these populations.
Acknowledgements
We gratefully acknowledge the contribution of NLAAS participants and the contribution of Dr. M. Claire Green and Dr. Ramin Mojtabai in their comments on the manuscript throughout its development.
Funding
This work was supported by the National Institute of Mental Health [grant numbers 5T32MH014592-39, 2T32MH019960].
Footnotes
Supplementary Information The online version contains supplementary material available at https://doi.org/10.1007/s11121-022-01376-2.
Consent to Participate This study was a secondary data analysis. Informed consent was obtained from all participants included in the original study.
Conflicts of Interest Not applicable.
Ethics Approval This study was performed in line with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. Approval was obtained from the IRB Office at the Johns Hopkins Bloomberg School of Public Health (IRB#00008615).
References
- Abraído-Lanza AF, Armbrister AN, Flórez KR, & Aguirre AN (2006). Toward a theory-driven model of acculturation in public health research. American Journal of Public Health, 96, 1342–1346. 10.2105/AJPH.2005.064980 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abraído-Lanza AF, Echeverría SE, & Flórez KR (2016). Latino immigrants, acculturation, and health: promising new directions in research. Annual Review of Public Health, 37, 219–236. 10.1146/annurev-publhealth-032315-021545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alcántara C, Chen CN, & Alegría M (2014). Do post-migration perceptions of social mobility matter for Latino immigrant health? Social Science and Medicine, 101, 94–106. 10.1016/j.socscimed.2013.11.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alcántara C, Estevez CD, & Alegría M (2017). Latino and Asian Immigrant Adult Health: Paradoxes and Explanations. In Schwartz SJ & Unger JB (Eds.), The Oxford Handbook of Acculturation and Health (pp. 197–220). Oxford University Press. [Google Scholar]
- Alegría M, Canino G, Shrout PE, Woo M, Duan N, Vila D, Torres M, Chen C, & Meng XL (2008). Prevalence of mental illness in immigrant and non-immigrant U.S. Latino groups. American Journal of Psychiatry, 165(3), 359–369. 10.1176/appi.ajp.2007.07040704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alegría M, Canino G, Stinson FS, & Grant BF (2006). Nativity and DSM-IV Psychiatric Disorders Among Puerto Ricans, Cuban Americans, and Non-Latino Whites in the United States: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. The Journal of Clinical Psychiatry, 67, 56–65. 10.4088/JCP.v67n0109 [DOI] [PubMed] [Google Scholar]
- Alegría M, Mulvaney-Day N, Torres M, Polo A, Cao Z, & Canino G (2007a). Prevalence of psychiatric disorders across latino subgroups in the United States. American Journal of Public Health, 97, 68–75. 10.2105/AJPH.2006.087205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alegría M, Shrout PE, Woo M, Guarnaccia P, Sribney W, Vila D, Polo A, Cao Z, Mulvaney-Day N Torres M & Canino G (2007b). Understanding differences in past year psychiatric disorders for Latinos living in the US. Social Science & Medicine, 65, 214–230. 10.1016/j.socscimed.2007.03.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alegría M, Sribney W, Woo M, Torres M, & Guarnaccia P (2007c). Looking beyond nativity: The relation of age of immigration, length of residence, and birth cohorts to the risk of onset of psychiatric disorders for Latinos. Research in Human Development, 4, 19–47. 10.1080/15427600701480980 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alegría M, Vila D, Woo M, Canino G, Takeuchi D, Vera M, Febo V, Guarnaccia P, Aguilar-Gaxiola S, & Shrout P (2004). Cultural relevance and equivalence in the NLAAS instrument: Integrating etic and emic in the development of cross-cultural measures for a psychiatric epidemiology and services study of Latinos. International Journal of Methods in Psychiatric Research, 13, 270–288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. (1994). Diagnostic and Statistical Manual of Mental Disorders (4th ed.). American Psychiatric Association. [Google Scholar]
- American Psychological Association. (2012). Crossroads: The psychology of immigration in the new century [Executive Summary]. APA Presidential Task Force on Immigration, https://www.apa.org/topics/immigration/executive-summary.pdf. Accessed 26 June 2018.
- Asparouhov T, & Muthén B (2014a). Auxiliary variables in mixture modeling: Three-step approaches using Mplus. Structural Equation Modeling: A Multidisciplinary Journal, 21, 329–341. [Google Scholar]
- Asparouhov T, & Muthén B (2014b). Auxiliary variables in mixture modeling: Using the BCH Method in Mplus to Estimate a Distal Outcome Model and an Arbitrary Secondary Model. Mplus Web Notes: No. 21, Version 2, October 7, 2014b. [Google Scholar]
- Bakk Z, Tekle FB, & Vermunt JK (2013). Estimating the association between latent class membership and external variables using bias-adjusted three-step approaches. Sociological Methodology, 43, 272–311. 10.1177/0081175012470644 [DOI] [Google Scholar]
- Bakk Z, & Vermunt JK (2016). Robustness of stepwise latent class modeling with continuous distal outcomes. Structural Equation Modeling: A Multidisciplinary Journal, 23, 20–31. 10.1080/10705511.2014.955104 [DOI] [Google Scholar]
- Bearman J, Jones J, & Udry R (1997). The National Longitudinal Study of Adolescent Health. Carolina Population Center. [Google Scholar]
- Berry JW (1988). Understanding the Process of Acculturation for Primary Prevention. National Institute of Mental Health (DHHS). [Google Scholar]
- Berry JW (2003). Conceptual approaches to acculturation. In Chun KM, Balls Organista P, & Marin G (Eds.), Acculturation: Advances in theory, measurement, and applied research (pp. 17–37). American Psychological Association. 10.1037/10472-004 [DOI] [Google Scholar]
- Blanco C, Morcillo C, Alegría M, Dedios MC, Fernández-Navarro P, Regincos R, & Wang S (2013). Acculturation and Drug Use Disorders among Hispanics in the U.S. Journal of Psychiatric Research, 47(2), 226–232. 10.1016/j.jpsychires.2012.09.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bolck A, Croon M, & Hagenaars J. (2004). Estimating latent structure models with categorical variables: one-step versus three-step estimators. Political Analysis, 12, 3–27. [Google Scholar]
- Bronfenbrenner U. (1979). The Ecology of Human Development. Harvard University Press. [Google Scholar]
- Bulut E, & Gayman MD (2016). Acculturation and self-rated mental health among Latino and Asian immigrants in the United States: A latent class analysis. Journal of Immigrant and Minority Health, 18, 836–849. 10.1007/sl0903-015-0258-l [DOI] [PubMed] [Google Scholar]
- Burnam MA, Hough RL, Karno M, Escobar JI, & Telles CA (1987). Acculturation and lifetime prevalence of psychiatric disorders among Mexican Americans in Los Angeles. Journal of Health & Social Behavior, 28, 89–102. [PubMed] [Google Scholar]
- Castro FG, Marsiglia FF, Kulis S & Kellison JG (2010). Lifetime Segmented Assimilation Trajectories and Health Outcomes in Latino and Other Community Residents. American Journal of Public Health, 100, 669–676. 10.2105/AJPH.2009.167999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cervantes RC, Padilla AM, & Salgado de Snyder N. (1991). The Hispanic Stress Inventory: A culturally relevant approach to psychosocial assessment. Psychological Assessment, 3, 438–447. 10.1037/1040-3590i3.3.438 [DOI] [Google Scholar]
- Clark SL, & Muthén B (2009). Relating Latent Class Analysis Results to Variables not Included in the Analysis. https://www.statmodel.com/download/relatinglca.pdf. Accessed 17 July 2019. [Google Scholar]
- Coatsworth JD, Pantin H, & Szapocznik J (2002). Familias Unidas: a family-centered ecodevelopmental intervention to reduce risk for problem behavior among hispanic adolescents. Clinical Child and Family Psychology Review, 5, 113–132. [DOI] [PubMed] [Google Scholar]
- Cobb CL, Xie D, Meca A, & Schwartz SJ (2017). Acculturation, discrimination, and depression among unauthorized Latinos/as in the United States. Cultural Diversity and Ethnic Minority Psychology, 23, 258–268. 10.1037/cdp0000118 [DOI] [PubMed] [Google Scholar]
- Cook B, Alegría M, Lin JY, & Guo J (2009). Pathways and correlates connecting Latinos’ mental health with exposure to the United States. American Journal of Public Health, 99, 2247–2254. 10.2105/AJPH.2008.137091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Escobar JI, Nervi CH, & Gara MA (2000). Immigration and mental health: Mexican Americans in the United States. Harvard Review of Psychiatry, 8, 64–72. [PubMed] [Google Scholar]
- Felix-Ortiz M, Newcomb MD, & Myers H (1994). A multidimensional measure of cultural identity for latino and latina adolescents. Hispanic Journal of Behavioral Sciences, 16(2), 99–115. 10.1177/07399863940162001 [DOI] [Google Scholar]
- Fortuna LR, Perez DJ, Canino G, Sribney W & Alegría M. (2007). Prevalence and correlates of lifetime suicidal ideation and suicide attempts among Latino subgroups in the United States. The Journal of Clinical Psychiatry, 68, 572–581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fox RS, Merz EL, Solórzano MT, & Roesch SC (2013). Further examining berry’s model: the applicability of latent profile analysis to acculturation. Measurement and Evaluation in Counseling and Development, 46, 270–288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibson WA (1959). Three multivariate models: Factor analysis, latent structure analysis, and latent profile analysis. Psychometrika, 24, 229–252. [Google Scholar]
- Gonzalez-Barrera A, & Lopez MH (2013). A demographic portrait of Mexican-origin Hispanics in the United States. Pew Hispanic Center. [Google Scholar]
- Goodman LA (1974). Exploratory Latent Structure Analysis Using Both Identifiable and Unidentifiable Models. Biometrika, 61, 215–231. 10.2307/2334349 [DOI] [Google Scholar]
- Grant BF, Stinson FS, Hasin DS, Dawson DA, Chou SP, & Anderson K (2004). Immigration and lifetime prevalence of DSM-IV psychiatric disorders among mexican americans and non-hispanic whites in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Archives of General Psychiatry, 61, 1226–1233. 10.1001/archpsyc.61.12.1226 [DOI] [PubMed] [Google Scholar]
- Griner D, & Smith TB (2006). Culturally adapted mental health intervention: A meta-analytic review. Psychotherapy: Theory, Research, Practice, Training, 43(4), 531–548. [DOI] [PubMed] [Google Scholar]
- Guarnaccia PJ, Martinez I, & Acosta H (2002). Comprehensive in-Depth Literature Review and Analysis of Hispanic Mental Health Issues. New Jersey Mental Health Institutes. [Google Scholar]
- Guarnaccia PJ, Pincay IM, Alegría M, Shrout PE, Lewis-Fernández R, & Canino GJ (2007). Assessing diversity among Latinos: Results from the NLAAS. Hispanic Journal of Behavioral Sciences, 29, 510–534. 10.1177/0739986307308110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hallquist MN, & Wiley JF (2018). MplusAutomation: an R Package for facilitating large-scale latent variable analyses in Mplus. Structural Equation Modeling, 25, 621–638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heeringa SG, Wagner J, Torres M, Duan N, Adams T, & Berglund P (2004). Sample designs and sampling methods for the Collaborative Psychiatric Epidemiology Studies (CPES). International Journal of Methods in Psychiatric Research, 13, 221–240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson J, Williams DR, & Torres M (1995). Chapter 8: Perceptions of Discrimination, Health and Mental Health: The Social Stress Process. Institute for Social Research. University of Michigan. [Google Scholar]
- Karno M, Hough RL, Burnam MA, Escobar JI, Timbers DM, Santana F, & Boyd JH (1987). Lifetime prevalence of specific psychiatric disorders among Mexican Americans and non-Hispanic Whites in Los Angeles. Archives of General Psychiatry, 44, 695–701. 10.1001/archpsyc.1987.01800200021004 [DOI] [PubMed] [Google Scholar]
- Kessler RC, Abelson J, Demler O, Escobar JI, Gibbon M, Guyer ME, Howes MJ, Jin R, Vega WA, Walters EE, Wang P, Zaslavsky A, & Zheng H (2004). Clinical calibration of DSM-IV diagnoses in the World Mental Health (WMH) version of the World Health Organization (WHO) Composite International Diagnostic Interview (WMHCIDI). International Journal of Methods in Psychiatric Research, 13, 122–139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, Wittchen HU & Kendler KS (1994). Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States. Results from the National Comorbidity Survey. Archives of General Psychiatry, 51(1), 8–19. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Mickelson KD, & Williams DR (1999). The prevalence, distribution, and mental health correlates of perceived discrimination in the United States. Journal of Health and Social Behavior, 40, 208–230. [PubMed] [Google Scholar]
- Kutob RM, Senf J, & Shisslak CM (2013). Cultural Competence Education for Practicing Physicians: Lessons in Cultural Humility, Nonjudgmental Behaviors, and Health Beliefs Elicitation. Journal of Continuing Education in the Health Professions, 33, 164–173. 10.1002/chp.21181 [DOI] [PubMed] [Google Scholar]
- Lanza ST, & Rhoades BL (2013). Latent Class Analysis: An alternative perspective on subgroup analysis in prevention and treatment. Prevention Science, 14, 157–168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lara M, Gamboa C, Kahramanian MI, Morales LS, & Bautista DEH (2005). Acculturation and Latino health in the United States: A review of the literature and its sociopolitical context. Annual Review of Public Health, 26, 367–397. 10.1146/annurev.publhealth.26.021304.144615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazarsfeld PE, & Henry NW (1968). Latent structure analysis. Houghton. [Google Scholar]
- Lazarus RS, & Folkman S (1984). Stress, Appraisal, and Coping. Springer Publishing Company. [Google Scholar]
- Masyn KE (2013). Latent Class Analysis and Finite Mixture Modeling. In Little TD (Ed.), The Oxford Handbook of Quantitative Methods in Psychology, 2, 551–611). 10.1093/oxfordhb/9780199934898.013.0025 [DOI] [Google Scholar]
- Mulvaney-Day NE, Alegría M, & Sribney W (2007). Social cohesion, social support, and health among Latinos in the United States. Social Science & Medicine, 64, 477–495. 10.1016/j.socscimed.2006.08.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray CJ, & Lopez AD (1996). The Global Burden of Disease: A comprehensive assessment of mortality and disability from diseases, injuries, and risk factors in 1990 and projected to 2020. Harvard University Press. [Google Scholar]
- Muthén LK, & Muthén BO (1998). Mplus User’s Guide (8th ed.). Muthén & Muthén. [Google Scholar]
- National Institute of Mental Health. (1994). Cooperative Agreement for a Multi-Site Study of Mental Health Service Use, Need, Outcomes, and Costs in Child and Adolescent Populations (UNO-CAP). In G.S. Administration (Ed.), Catalog of Federal Domestic Assistance 93.242-Request for Applications. [Google Scholar]
- Nylund KL, Asparouhov T, & Muthén BO (2007). Deciding on the number of classes in latent class analysis and growth mixture modeling: A Monte Carlo simulation study. Structural Equation Modeling: A Multidisciplinary Journal, 14, 535–569. 10.1080/10705510701575396 [DOI] [Google Scholar]
- Olson DH (1986). Circumplex Model VII: Validation studies and FACES III. Family Process, 25. 337–351. [DOI] [PubMed] [Google Scholar]
- Olson DH (1989). Circumplex Model of Family Systems VIII: Family Assessment and Intervention. In Olson DH, Russell CS, & Sprenkle DH (Eds.), Circumplex Model: Systemic Assessment and Treatment of Families. Haworth Press. [Google Scholar]
- Ortega AN, Feldman JM, Canino G, Steinman K, & Alegría M (2006). Co-occurrence of mental and physical illness in US Latinos. Social Psychiatry and Psychiatric Epidemiology, 41. 927–934. 10.1007/s00127-006-0121-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ortega AN, Rosenheck R, Alegría M, & Desai RA (2000). Acculturation and the lifetime risk of psychiatric and substance use disorders among Hispanics. Journal of Nervous and Mental Disease, 188. 728–735. 10.1097/00005053-200011000-00002 [DOI] [PubMed] [Google Scholar]
- Pennell BE, Bowers A, Carr D, Chardoul S, Cheung GQ, Dinkelmann K, Gebler N, Hansen SE, Pennell S, & Torres M (2004). The development and implementation of the National Comorbidity Survey Replication, the National Survey of American Life, and the National Latino and Asian American Survey. International Journal of Methods in Psychiatric Research, 13. 241–269. 10.1002/mpr.180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phinney JS (1990). Ethnic identity in adolescents and adults: Review of research. Psychological Bulletin, 108, 499–514. 10.1037/0033-2909.108.3.499 [DOI] [PubMed] [Google Scholar]
- Rivera FI, Guarnaccia PJ, Mulvaney-Day N, Lin JY, Torres M, & Alegría M (2008). Family Cohesion and Its Relationship to Psychological Distress Among Latino Groups. Hispanic Journal of Behavioral Sciences, 30. 357–378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roth KB, Musci RJ, & Eaton WW (2019). Heterogeneity of Latina/os’ acculturative experiences in the National Latino and Asian American Study: A latent profile analysis. Annals of Epidemiology, 38, 48–56.e2. 10.1016/j.annepidem.2019.07.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roth KB, Musci RJ, & Eaton WW (2020). Refining acculturation measures for health research: Latina/o heterogeneity in the National Latino and Asian American Study. International Journal of Methods in Psychiatric Research, 29. e1844. 10.1002/mpr.1844 [DOI] [PMC free article] [PubMed] [Google Scholar]
- RStudio Team. (2015). RStudio: Integrated Development for R. Computer Program. http://www.rstudio.com/ [Google Scholar]
- Sampson RJ, Raudenbush SW, & Earls F (1997). Neighborhoods and violent crime: A multilevel study of collective efficacy. Science, 277, 918–924. [DOI] [PubMed] [Google Scholar]
- Schwartz SJ, Unger JB, Zamboanga BL, & Szapocznik J (2010). Rethinking the concept of acculturation: Implications for theory and research. The American Psychologist, 65, 237–251. 10.1037/a0019330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz SJ, & Zamboanga BL (2008). Testing Berry’s model of acculturation: A confirmatory latent class approach. Cultural Diversity & Ethnic Minority Psychology, 14, 275–285. 10.1037/a0012818 [DOI] [PubMed] [Google Scholar]
- Tervalon M, & Murray-Garcia J. (1998). Cultural humility versus cultural competence: A critical distinction in defining physician training outcomes in multicultural education. Journal of Health Care for the Poor and Underserved, 9, 117–125. 10.1353/hpu.2010.0233 [DOI] [PubMed] [Google Scholar]
- Thomson MD, & Hoffman-Goetz L (2009). Defining and measuring acculturation: A systematic review of public health studies with Hispanic populations in the United States. Social Science & Medicine, 69, 983–991. 10.1016/j.socscimed.2009.05.011 [DOI] [PubMed] [Google Scholar]
- Torres L, Driscoll MW, & Voell M (2012). Discrimination, acculturation, acculturative stress, and Latino psychological distress: A moderated mediational model. Cultural Diversity and Ethnic Minority Psychology, 18, 17–25. 10.1037/a0026710 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valencia-Garcia D, Simoni JM, Alegría M, & Takeuchi DT. (2012). Social capital, acculturation, mental health, and perceived access to services among Mexican American women. Journal of Consulting and Clinical Psychology, 80, 177–185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vega WA, Gil AG, Warheit GJ, Zimmerman RS, & Apospori E (1993). Acculturation and delinquent behavior among Cuban American adolescents: Toward an empirical model. American Journal of Community Psychology, 21, 113–125. [DOI] [PubMed] [Google Scholar]
- Vega WA, Kolody B, Aguilar-Gaxiola S, Alderete E, Catalano R, & Caraveo-Anduaga J (1998). Lifetime prevalence of DSM-III-R psychiatric disorders among urban and rural Mexican Americans in California. Archives of General Psychiatry, 55, 771–778. [DOI] [PubMed] [Google Scholar]
- Vega WA, Sribney WM, Aguilar-Gaxiola S, & Kolody B (2004). 12-month prevalence of DSM-III-R psychiatric disorders among Mexican Americans: Nativity, social assimilation, and age determinants. Journal of Nervous and Mental Disease, 192, 532–541. [DOI] [PubMed] [Google Scholar]
- Wassertheil-Smolle S, Arredondo EM, Cai J, Castaneda SF, Choca JP, Gallo LC, Jung M, LaVange LM, Lee-Rey E, Mosley T Jr., Penedo FJ, Santistaban DA, & Zee PC. (2014). Depression, anxiety, antidepressant use, and cardiovascular disease among Hispanic men and women of different national backgrounds: Results from the Hispanic Community Health Study/Study of Latinos. Annals of Epidemiology, 24, 822–830. 10.1016/j.annepidem.2014.09.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, Yu Y, Jackson JS, & Anderson NB (1997). Racial Differences in Physical and Mental Health: Socio-economic Status, Stress and Discrimination. Journal of Health Psychology, 2, 335–351. 10.1177/135910539700200305 [DOI] [PubMed] [Google Scholar]
- World Health Organization (WHO). (2008). The global burden of disease: 2004 update. WHO Press. [Google Scholar]


