Abstract
Background and study aims Symptomatic simple hepatic cysts require treatment, with several guidelines recommending laparoscopic deroofing. However, cysts located in the posterosuperior segments are considered poor candidates for this procedure. Gastrointestinal endoscopes are more flexible and able to reach less accessible areas than laparoscopes. This study aimed to evaluate the utility of endoscopic transgastric hepatic cyst deroofing (ETGHCD) for treatment of simple hepatic cysts.
Patients and methods Seven patients with simple hepatic cysts were evaluated between June 2021 and October 2023. The success rate, procedure time, post-procedure length of hospital stays, complications, pathologic diagnosis, and efficacy were recorded.
Results Eleven cysts in seven patients (5 men; mean age 65.5 (standard deviation [SD] 8.5) years) were successfully treated without any complications. The mean procedure time was 65.6 minutes (SD 17.2). Mean post-procedure hospitalization was 4.4 days (SD 1.0). The pathologic diagnosis of 11 cysts showed simple hepatic cysts. The size of the cysts was significantly decreased from 337.0 cm 3 (SD 528.8) to 5.2 cm 3 (SD 6.3) 1 month after ETGHCD. During the median 12.7-month follow-up in seven patients, the cysts showed a 99.6% reduction with no recurrence.
Conclusions ETGHCD provided a feasible, safe, effective, and minimal invasive alternative approach for the treatment of simple hepatic cysts.
Introduction
Simple hepatic cysts are common benign liver lesions, with a prevalence ranging from 3% to 5% on endoscopic ultrasound (EUS) to as high as 18% on computed tomography (CT). Only about 5% of these cysts require treatment 1 . Larger lesions may require treatment if patients present with abdominal pain, epigastric fullness, early satiety, or other related symptoms 2 . However, it should be noted that attributing symptoms to simple cysts should be done with caution after ruling out all other possible causes. To manage simple hepatic cysts, it is important to correctly differentiate them from neoplasms and infections, and then choose a reliable treatment, including percutaneous aspiration, aspiration followed by sclerotherapy, or surgery 3 .
Laparoscopic deroofing has become the preferred method due to its low recurrence rate, less postoperative complications, and exact efficacy 4 5 6 7 8 9 10 . Percutaneous procedures can provide immediate relief but are not generally recommended due to their high rate of recurrence and lack of histological examination 11 . An open approach can handle any conditions of hepatic cysts; however, it is rarely the first choice due to its substantial morbidity and associated adverse events (AEs).
The American Society of Gastroenterology recommends laparoscopic deroofing over aspiration and sclerotherapy for symptomatic simple hepatic cysts, but laparoscopic deroofing has limitations 12 . Cysts located in the peripheral portion of the anterolateral segments of the liver (S2, S3, S5, S6, and the inferior part of S4 in Couinaud’s classification) are suitable for laparoscopy; however, cysts located in the posterosuperior segments (S1, S7, S8, and the superior part of S4) are considered poor candidates for laparoscopic resection because of limited visualization and the difficulty of controlling bleeding 13 . Natural-orifice transluminal endoscopic surgery (NOTES) is a less invasive procedure that avoids skin incisions and related complications 14 . It accesses the second space through a natural orifice, using gastrointestinal endoscopes which can reach areas that are inaccessible to laparoscopes. NOTES is effective for handling cysts in the posterosuperior segments. Some researchers have used NOTES technology for cystic fluid aspiration and sclerotherapy 15 16 17 . However, it has a high rate of recurrence and histological examination is limited, similar to percutaneous procedures.
We developed a new method evolved from NOTES, endoscopic transgastric hepatic cyst deroofing (ETGHCD), which not only can deal with cysts in posterosuperior localizations but also allows histological examination of the cysts. We reported a case using ETGHCD in which we easily achieved deroofing of simple hepatic cysts in 2022 18 . The patient had a short hospital stay, rapid recovery, and optimal short-term and long-term effects with no complications observed after a 20-month follow-up. ETGHCD may also be a feasible treatment method for simple hepatic cysts. This study aimed to further investigate the safety and therapeutic value of ETGHCD for treatment of simple hepatic cysts.
Patients and methods
Study design and protocol
This study was reviewed and approved by the Ethics Committee of Shanghai General Hospital affiliated with Shanghai Jiao Tong University School of Medicine (2022-N-25).
Patients with simple hepatic cysts admitted to Shanghai General Hospital from June 2021 to October 2023 were eligible for inclusion in this study. The inclusion criterion was applied to patients with simple hepatic cysts diagnosed by abdominal CT or magnetic resonance imaging 19 that cause discomfort to the patient, with caution after excluding all other possible causes and located in the peripheral portion of liver.
The exclusion criteria were as follows: 1) hepatic cysts connected with the biliary tract, with infection or suspected malignancy; 2) history of abdominal surgery; and 3) coagulation disorders preoperatively and/or inability to tolerate anesthesia with tracheal intubation.
Description of technique
Video showing the endoscopic transgastric hepatic cyst deroofing (ETGHCD) procedure.
Video 1
Prior to the procedure, patients underwent blood routine examination, blood coagulation function tests, biochemical routine tests, and electrocardiograms. All patients fasted for at least 6 hours. General anesthesia was administered and patients were positioned in a supine position.
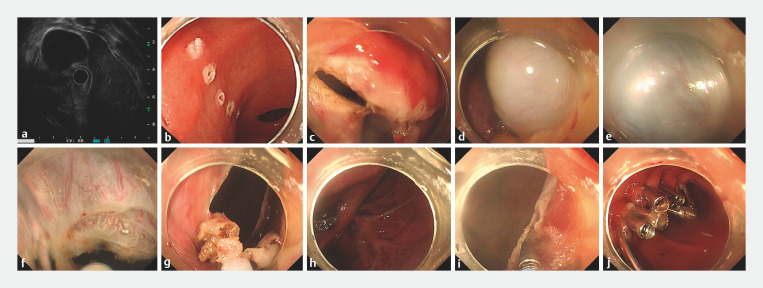
The main procedure was as follows ( Fig. 1 , Video 1 ) 18 :
Fig. 1.
Endoscopic images of the endoscopic transgastric hepatic cyst deroofing (ETGHCD) procedure. a Endoscopic ultrasonography was performed to confirm the location of the cysts. b,c Active perforation of the anterior wall of the gastric antrum. d Entering the abdominal cavity and locating the cyst. e Finding the thinnest part of the cyst wall. f,g,h,i Puncturing cyst and cyst deroofing. j Closure of the gastric wall.
Active perforation of the gastric antrum: A sterile colonoscopy (PCF-Q260JI, 3.2-mm channel diameter; Olympus, Tokyo, Japan) specifically used for upper gastrointestinal surgery in our department with a conical transparent cap (Olympus, Tokyo, Japan) was inserted into the stomach. The anterior wall of the gastric antrum was incised with a flush knife (Fuji, Tokyo, Japan).
Precise localization of the hepatic cyst: The abdominal cavity was explored according to preoperative imaging to locate the cysts. Endoscopic ultrasonography was performed if necessary to confirm the location of the cysts.
Puncture the cyst: A 23-gauge puncture needle (Boston Scientific, United States) was used to extract transparent liquid, which was subjected to routine testing including bilirubin, cytological examination, and bacterial culture. If colorless or light-yellow bile-free fluid was extracted, the case was classified as a simple liver cyst and the puncture opening was expanded for cyst fenestration. If yellow cystic fluid was extracted and suspected to connect with the biliary tract, a contrast agent was injected for contrast examination. If the cyst was found to be connected to the bile duct, we closed the cyst cavity with Titanium clips. Next, we suctioned out the fluid from the abdominal cavity and closed the gastric wall. Then we undertook multidisciplinary discussions to determine the most suitable treatment plan based on a patient's individual condition and had a thorough discussion with the patient and their family.
Cyst deroofing: The thinnest part of the cyst was further cut with an IT knife (Olympus, Tokyo, Japan). After aspirating the cyst fluid with an endoscope, the cyst wall was opened and removed in sections with a snare (Boston Scientific, United States) at the interface with the hepatic parenchyma. The removed cysts were sent for pathologic examination. If a nodule was found on the cyst wall, the cyst wall nodule was taken for biopsy. If necessary, frozen sections were sent for examination to exclude the possibility of cancer. If there was definite malignant change, the patient was immediately transitioned to open surgery for cyst resection or partial hepatectomy.
After removal of the cyst wall, the cyst cavity was flushed, the vessels of the cyst wall were addressed and checked for active bleeding and bile leakage, and the liquid in the abdominal cavity was then suctioned. The gastric wall was then closed.
Postoperative management
Following the procedure, patients were required to fast for 48 hours. Acid inhibitors, antibiotics, and nutritional support therapy were prescribed, and patients’ vital signs and abdominal signs were closely monitored. If patients had no abdominal discomfort and their vital signs remained normal 48 hour after the procedure, a full fluid diet was provided. Blood routine and biochemical tests were conducted 24 hours after the procedure.
Efficacy evaluation
The patients were followed with clinic visits and telephone calls and underwent CT 1 month after the procedure to evaluate the short-term efficacy and then underwent CT or US at 3- to 6-month intervals after the procedure to detect the presence of hepatic cyst recurrence at 6 to 24 months. Cyst volume was calculated on CT or MRI by using an ellipsoid formula that multiplied the product of the three orthogonal diameters by 0.523 (volume = height × width × length × 0.523) 16 .
Safety evaluation
Observation was performed for any AEs or complications after the procedure, such as abdominal distension and pain, fever, diarrhea, vomiting, bleeding, or biliary fistula.
Statistical analysis
Data are expressed as the means and standard deviation (SD) or interquartile range (IQR) or numbers with percentages. All analyses were performed using SPSS software (version 25.0, IBM, Armonk, New York, United States). P < 0.05 was considered statistically significant.
Results
Clinical characteristics of ETGHCD in seven patients with simple hepatic cysts
A total of seven patients (5 males and 2 females) with a mean age of 65.5 years (SD 8.5) were included in the study. Clinical symptoms included epigastric fullness in six patients (85.7%) and early satiety in two patients (28.6%). All seven patients had multiple hepatic cysts with volumes ranging from 5.2 to 1870.2 cm 3 , and four patients also had renal cysts. ETGHCD was only used to treatlarge cysts located on the surface of the liver and it was successful in 11 cysts in seven patients. All hepatic cysts were considered simple hepatic cysts not connected to the bile duct, and no patients required transfer to surgery. The clinical characteristics of ETGHCD for seven patients with 11 large simple hepatic cysts are listed in Table 1 . The mean procedure time, defined as the time from the beginning of endoscopy to the end of treatment, was 65.6 minutes (SD 17.2), with no intraoperative complications. Mean blood loss was < 5 mL. The mean hospital stay after the procedure was 4.4 days (SD 1.0). It is worth mentioning that the hospital stay after the procedure for seven patients was slightly extended for safety reasons. In fact, all seven patients were able to be discharged 48 hours after the procedure based on their condition evaluation.
Table 1 Clinical characteristics of endoscopic transgastric hepatic cyst deroofing in seven patients with simple hepatic cysts.
| No. | Gender | Age (y) | Renal cysts | Reason for intervention | Conditions of treated liver cyst | Procedure time (minutes) | Adverse events | Hospital stays post-procedure (days) | Pathologic diagnosis | Follow-up (months) | Symptom relief rate during follow-up | |||
| Quantity | Location | Initial volume of cyst (cm 3 ) | Final volume of cyst (cm 3 ) | |||||||||||
| S , liver segment in Couinaud’s classification. | ||||||||||||||
| 1 | F | 50 | No | Epigastric fullness | 2 | S3, S4b | 291.4, 39.4 | 1.6, 2.1 | 57 | None | 5 | Simply hepatic cyst | 24 | 100% |
| 2 | M | 73 | Yes | Early satiety | 1 | S4a | 308.8 | 0 | 72 | Transient fever | 4 | Simply hepatic cyst | 20 | 100% |
| 3 | M | 70 | Yes | Epigastric fullness | 2 | S1, S2 | 45.9, 140.4 | 0.9, 3.1 | 64 | None | 6 | Simply hepatic cyst | 12 | 100% |
| 4 | M | 64 | No | Epigastric fullness; early satiety | 3 | S3, S4a, S5 | 109.1, 429.7, 29.2 | 2.1, 3.6, 0.6 | 107 | None | 5 | Simply hepatic cyst | 10.5 | 100% |
| 5 | M | 61 | Yes | Epigastric fullness; | 1 | S7 | 377.2 | 0 | 65 | None | 4 | Simply hepatic cyst | 10 | 100% |
| 6 | F | 66 | No | Epigastric fullness | 1 | S3 | 66.0 | 0.5 | 62 | None | 3 | Simply hepatic cyst | 10 | 100% |
| 7 | M | 75 | No | Epigastric fullness; increased size | 1 | S5 | 1870.2 | 22.7 | 60 | None | 4 | Simply hepatic cyst | 2.5 | 100% |
Safety evaluation of ETGHCD
Almost none of the patients experienced any AEs or complications, except one patient had a transient fever and recovered 24 hours after the procedure. The anal exhaust time was within 24 hours, and a full fluid diet was given to all patients 48 hours after the procedure. There was no significant difference in hepatic function before or after ETGHCD and there was an obvious but not serious inflammatory reaction 24 hours after the procedure, which was considered a normal stress response ( Table 2 ). The incidence rates for fever, abdominal pain, vomiting, post-procedure infection, delayed perforation, bleeding, diffuse peritonitis, biliary fistula and other complications were 16.7%, 0%, 0%, 0%, 0%, 0%, 0%, and 0%, respectively.
Table 2 Comparison of laboratory values before and after ETGHCD.
| Pre-ETGHCD | Post-ETGHCD | P value | |
| ETGHCD, endoscopic transgastric hepatic cyst deroofing; WBC, white blood cell; CRP, C-reactive protein; neu, neutrophils; Tbil, total bilirubin; ALT, alanine transaminase; AST, aspartate transaminase. *Statistically significant. | |||
| WBC (×10 9 /L) | 5.37 ± 1.04 | 9.69 ± 2.99 | 0.002* |
| CRP (mg/L) | 0.99 ± 076 | 81.00 ± 39.69 | 0.000* |
| Neu% | 60.16 ± 7.23 | 70.41 ± 29.00 | 0.000* |
| Tbil (μmol/L) | 15.41 ± 5.76 | 24.54 ± 12.48 | 0.081 |
| ALT (U/L) | 21.81 ± 10.72 | 32.02 ± 21.59 | 0.251 |
| AST (U/L) | 21.69 ± 5.13 | 30.85 ± 15.69 | 0.139 |
| Cyst volume (cm 3 ) | 337.0 ± 528.8 | 5.2 ± 6.3 | < 0.0001* |
Efficacy evaluation and follow-ups of ETGHCD
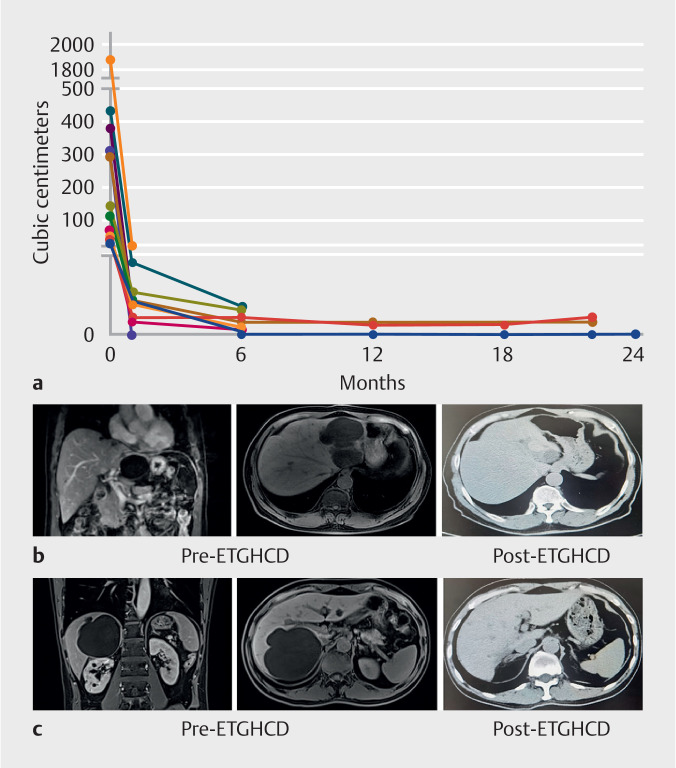
All seven patients treated with ETGHCD were followed up with regular clinic visits or telephone calls. During the follow-up, short-term efficacy was evaluated 1 month after the procedure. The results suggest that the mean volume of treated hepatic cysts was reduced from 337.0 cm 3 (SD 528.8) to 5.2 cm 3 (SD 6.3) ( P < 0.000) ( Table 2 ; Fig. 2 ), which was a 98.5% reduction. During the median 12.7-month follow-up in seven patients, the cysts showed a 99.6% reduction, and all patients experienced symptom relief. At the latest follow-up, the mean cyst volume was 1.45 cm 3 (IQR, 0–3.6 cm 3 ) ( Fig. 2 ). There were no complications during or after the procedure, no recurrences of hepatic cyst, and no AEs were noted over the 12.7 months of follow-up (SD 7.1, IQR 2.5–24).
Fig. 2.
Comparison of pre-procedure and post-procedure efficacy of ETGHCD in the treatment of hepatic cysts. a Volumes of cysts before and after ETGHCD treatment. b Imaging comparison of hepatic cysts in left liver before and after ETGHCD. c Imaging comparison of hepatic cysts in right liver before and after ETGHCD.
Discussion
This study is the first to investigate the feasibility, efficacy, and safety of endoscopic deroofing in treating simple hepatic cysts. After ETGHCD, the cysts showed a 99.6% reduction, and symptom relief was 100% for the median 12.7-month follow-up in seven patients. Except for one patient who had a transient fever after the procedure, no patients had AEs. No short-term or long-term complications occurred, indicating a high level of safety. However, long-term follow-up is needed to assess for potential for recurrence. Follow-up to date results indicates no recurrence of the cysts.
ETGHCD has an advantage over cyst aspiration or sclerotherapy in that it allows for histological examination. The pathologic diagnosis of 11 cysts showed simple hepatic cysts, which further confirmed the diagnosis of simple cysts. Thus, ETGHCD of symptomatic simple liver cysts seems to be a feasible and effective method, comparable to laparoscopy.
Technically, ETGHCD has several advantages over laparoscopic deroofing. First, gastrointestinal endoscopes are more flexible and better able to reach less accessible areas than laparoscopes, so ETGHCD can easily handle cysts in the posterosuperior segments of the liver (S1, S7, S8, and the superior part of S4), which are considered poor candidates for laparoscopy. In this study, we easily and successfully treated cysts located in S1, S7 and S4a through ETGHCD, as well as cysts in S2, S3, S4b and S5, which were also suitable for laparoscopes. Second, ETGHCD was minimally invasive compared with laparoscopic deroofing, with no injuries to the body surface, rapid recovery, and less trauma. Reported AEs associated with laparoscopic fenestration include wound infections, bile leak, chest infections, subphrenic hematomas, and prolonged post-procedure drainage 19 . Our data showed that ETGHCD was less invasive and associated with no AEs.
However, ETGHCD also has several disadvantages. First, visibility is reduced compared with laparoscopy, and it requires an experienced endoscopist to perform the procedure. It is important to note that the endoscopist’s experience level can impact the success of ETGHCD. Therefore, it is recommended that the procedure be performed by an experienced endoscopist. Second, laparoscopic deroofing can prevent injury to Glisson's capsule by utilizing fluorescence guidance with indocyanine green, which is currently not achievable with ETGHCD. Currently, our endoscope cannot achieve 750 to 810 nm near-infrared light irradiation to excite indocyanine green fluorescence. However, we believe that as endoscopic technology continues to advance, it will soon be possible to realize ETGHCD assisted by indocyanine green fluorescence imaging technology. Third, ETGHCD is inadequate for handling deep cysts, as is the same for laparoscopy. Simple cysts in the deep part of the liver are often very small and grow slowly, rarely causing symptoms, so most of them do not need to be treated 20 . For large, symptomatic, deep hepatic cysts, EUS guidance or percutaneous aspiration and sclerotherapy may be an alternative approach. In addition, while ETGHCD does not result in any external wounds, it does result in a 2-cm wound inside the stomach that is closed with clips. After the wound heals, the clips are excreted in feces, leaving a small scar in the stomach. Therefore, we prescribe patients proton pump inhibitors (PPIs) for 1 months after the procedure. During the follow-up period, none of the six patients report any stomach discomfort.
This study has some limitations, including characterization of the new technique, retrospective design, a small cohort, and absence of a control group. Further research is needed to determine the long-term effectiveness of ETGHCD for treating simple hepatic cysts. Although the results of this study are promising, a larger sample size and a control group are necessary to confirm the effectiveness of this new approach. In addition, more studies are needed comparing ETGHCD with other minimally invasive techniques for treating simple hepatic cysts.
Furthermore, while ETGHCD has demonstrated effectiveness in treating simple hepatic cysts, it is important to note that not all hepatic cysts require treatment. Asymptomatic cysts that are small and slow growing may not require intervention, and observation may be a more appropriate approach. In addition, patients with complex hepatic cysts or cysts that are suspected to be malignant may not be good candidates for ETGHCD and may require more invasive procedures. Therefore, an individualized approach is necessary for management of hepatic cysts, taking into account various factors such as cyst size, location, and patient comorbidities.
Conclusions
In conclusion, ETGHCD offers an additional new approach for the management of simple hepatic cysts. It should be noted that this study represents an initial and incomplete exploration of the technique. While further research is needed to confirm its effectiveness and long-term outcomes, ETGHCD has demonstrated a high leel of safety and efficacy in the short term. As this technique continues to be refined and more data become available, it has the potential to become a standard of care for the treatment of symptomatic simple hepatic cysts.
Footnotes
Conflict of Interest The authors declare that they have no conflict of interest.
References
- 1.Reid-Lombardo KM, Khan S, Sclabas G. Hepatic cysts and liver abscess. Surg Clin North Am. 2010;90:679–697. doi: 10.1016/j.suc.2010.04.004. [DOI] [PubMed] [Google Scholar]
- 2.Gomez A, Wisneski AD, Luu HY et al. Contemporary Management of hepatic cyst disease: techniques and outcomes at a tertiary hepatobiliary center. J Gastrointest Surg. 2021;25:77–84. doi: 10.1007/s11605-020-04821-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shimizu T, Yoshioka M, Kaneya Y et al. Management of simple hepatic cyst. J Nippon Med Sch. 2022;89:2–8. doi: 10.1272/jnms.JNMS.2022_89-115. [DOI] [PubMed] [Google Scholar]
- 4.Gloor B, Ly Q, Candinas D. Role of laparoscopy in hepatic cyst surgery. Dig Surg. 2002;19:494–499. doi: 10.1159/000067603. [DOI] [PubMed] [Google Scholar]
- 5.Xu S, Rao M, Pu Y et al. The efficacy of laparoscopic lauromacrogol sclerotherapy in the treatment of simple hepatic cysts located in posterior segments: a refined surgical approach. Ann Palliat Med. 2020;9:3462–3471. doi: 10.21037/apm-20-1723. [DOI] [PubMed] [Google Scholar]
- 6.Gigot JF, Metairie S, Etienne J et al. The surgical management of congenital liver cysts. Surg Endosc. 2001;15:357–363. doi: 10.1007/s004640090027. [DOI] [PubMed] [Google Scholar]
- 7.Zacherl J, Scheuba C, Imhof M et al. Long-term results after laparoscopic unroofing of solitary symptomatic congenital liver cysts. Surg Endosc. 2000;14:59–62. doi: 10.1007/s004649900012. [DOI] [PubMed] [Google Scholar]
- 8.Z'Graggen K, Metzger A, Klaiber C. Symptomatic simple cysts of the liver: treatment by laparoscopic surgery. Surg Endosc. 1991;5:224–225. doi: 10.1007/BF02653270. [DOI] [PubMed] [Google Scholar]
- 9.Loehe F, Globke B, Marnoto R et al. Long-term results after surgical treatment of nonparasitic hepatic cysts. Am J Surg. 2010;200:23–31. doi: 10.1016/j.amjsurg.2009.06.031. [DOI] [PubMed] [Google Scholar]
- 10.Maruyama Y, Okuda K, Ogata T et al. Perioperative challenges and surgical treatment of large simple, and infectious liver cyst - a 12-year experience. PLoS One. 2013;8:e76537. doi: 10.1371/journal.pone.0076537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jang SY, Park SY, Tak WY et al. Long-term follow-up of large symptomatic hepatic cysts treated by percutaneous ethanol sclerotherapy. Acta Radiol. 2016;57:1205–1209. doi: 10.1177/0284185115626476. [DOI] [PubMed] [Google Scholar]
- 12.Marrero JA, Ahn J, Rajender Reddy K et al. ACG clinical guideline: the diagnosis and management of focal liver lesions. Am J Gastroenterol. 2014;109:1328–1347. doi: 10.1038/ajg.2014.213. [DOI] [PubMed] [Google Scholar]
- 13.Stanescu CA, Paduraru DN, Cirimbei C et al. The laparoscopic management of simple hepatic cysts. J Med Life. 2015;8:342–345. [PMC free article] [PubMed] [Google Scholar]
- 14.Ullah S, Ali FS, Liu BR. Advancing flexible endoscopy to natural orifice transluminal endoscopic surgery. Curr Opin Gastroenterol. 2021;37:470–477. doi: 10.1097/MOG.0000000000000753. [DOI] [PubMed] [Google Scholar]
- 15.Lee DS, Lee SK, Seo DW. Long-term safety and efficacy of ethanol retention therapy via percutaneous approach and/or EUS guidance for symptomatic large hepatic cysts (with video) Endosc Ultrasound. 2020;9:31–36. doi: 10.4103/eus.eus_42_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lee S, Seo DW, Paik WH et al. Ethanol lavage of huge hepatic cysts by using EUS guidance and a percutaneous approach. Gastrointest Endosc. 2014;80:1014–1021. doi: 10.1016/j.gie.2014.03.037. [DOI] [PubMed] [Google Scholar]
- 17.Stavropoulos SN, Im GY, Jlayer Z et al. High yield of same-session EUS-guided liver biopsy by 19-gauge FNA needle in patients undergoing EUS to exclude biliary obstruction. Gastrointest Endosc. 2012;75:310–318. doi: 10.1016/j.gie.2011.09.043. [DOI] [PubMed] [Google Scholar]
- 18.Chen C, Zhang R, Wan R. Novel technique for treating simple hepatic cysts: endoscopic transgastric hepatic cyst deroofing. Endoscopy. 2022;54:E1045–E1046. doi: 10.1055/a-1909-1392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Karam AR, Connolly C, Fulwadhva U et al. Alcohol sclerosis of a giant liver cyst following failed deroofings. J Radiol Case Rep. 2011;5:19–22. doi: 10.3941/jrcr.v5i2.634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pompili M, Ardito F, Brunetti E et al. Benign liver lesions 2022: Guideline for clinical practice of Associazione Italiana Studio del Fegato (AISF), Societa Italiana di Radiologia Medica e Interventistica (SIRM), Societa Italiana di Chirurgia (SIC), Societa Italiana di Ultrasonologia in Medicina e Biologia (SIUMB), Associazione Italiana di Chirurgia Epatobilio-Pancreatica (AICEP), Societa Italiana Trapianti d'Organo (SITO), Societa Italiana di Anatomia Patologica e Citologia Diagnostica (SIAPEC-IAP) - Part I - Cystic lesions. Dig Liver Dis. 2022;54:1469–1478. doi: 10.1016/j.dld.2022.08.030. [DOI] [PubMed] [Google Scholar]