Abstract
Pancreatic cancer is an aggressive disease with a 5 year survival rate of 13%. This poor survival is attributed, in part, to limited and ineffective treatments for patients with metastatic disease, highlighting a need to identify molecular drivers of pancreatic cancer to target for more effective treatment. CD200 is a glycoprotein that interacts with the receptor CD200R and elicits an immunosuppressive response. Overexpression of CD200 has been associated with differential outcomes, depending on the tumor type. In the context of pancreatic cancer, we have previously reported that CD200 is expressed in the pancreatic tumor microenvironment (TME), and that targeting CD200 in murine tumor models reduces tumor burden. We hypothesized that CD200 is overexpressed on tumor and stromal populations in the pancreatic TME and that circulating levels of soluble CD200 (sCD200) have prognostic value for overall survival. We discovered that CD200 was overexpressed on immune, stromal, and tumor populations in the pancreatic TME. Particularly, single-cell RNA-sequencing indicated that CD200 was upregulated on inflammatory cancer-associated fibroblasts. Cytometry by time of flight analysis of PBMCs indicated that CD200 was overexpressed on innate immune populations, including monocytes, dendritic cells, and monocytic myeloid-derived suppressor cells. High sCD200 levels in plasma correlated with significantly worse overall and progression-free survival. Additionally, sCD200 correlated with the ratio of circulating matrix metalloproteinase (MMP) 3: tissue inhibitor of metalloproteinase (TIMP) 3 and MMP11/TIMP3. This study highlights the importance of CD200 expression in pancreatic cancer and provides the rationale for designing novel therapeutic strategies that target this protein.
Supplementary Information
The online version contains supplementary material available at 10.1007/s00262-024-03678-6.
Keywords: Pancreatic cancer, CD200, Tumor microenvironment, Overall Survival
Introduction
Pancreatic cancer is the 3rd leading cause of cancer deaths in the USA and has a 5 year survival rate of 13% [1]. Pancreatic ductal adenocarcinoma (PDAC) is the most common type of pancreatic cancers, accounting for over 90% of cases [2–4]. The combination of systemic chemotherapy and surgery can be potentially curative; however, most patients (> 80%) have locally advanced or metastatic disease at cancer diagnosis, so this is not feasible [5, 6]. While there have been recent advances in options for systemic chemotherapy, responses are not universal and dose-limiting toxicities are common [7–10]. Moreover, the tumors can become resistant to chemotherapy within weeks after starting treatment, limiting the beneficial effects [11]. As a result, efforts have been focused on identifying genetic and molecular drivers of PDAC progression to target to develop efficacious therapeutics.
The PDAC tumor microenvironment (TME) is characterized by a desmoplastic reaction and heterogeneous stromal and immune populations [12]. One of the major stromal components of the PDAC TME is the presence of cancer-associated fibroblasts (CAFs), which are differentiated from pancreatic stellate cells (PSCs). Two major populations of CAFs have been identified in PDAC: inflammatory and myo-cancer-associated fibroblasts (iCAFs and myCAFs) [13, 14]. The iCAFs are characterized as expressing low levels of αSMA and high levels of the inflammatory cytokines IL-6 and IL-11 that can expand and promote the immunosuppressive function of myeloid populations, such as tumor-associated macrophages (TAMs) and myeloid-derived suppressor cells (MDSCs) [14–16]. These myeloid cells are the most prominent immune populations in the pancreatic TME and can inhibit T cell effector function and proliferation and promote Treg differentiation through the secretion of immunosuppressive factors, such as IDO1 and Arg1 [17, 18]. The myCAFs are characterized as expressing high levels of αSMA and are involved in promoting a stiff extracellular matrix (ECM) comprised of collagen and fibronectin that can contribute to resistance to chemotherapy and limit T cell proliferation and movement [14, 19–21]. Identification and characterization of upregulated genes and proteins on these heterogeneous populations may provide insights for targeting the TME to limit PDAC progression.
CD200 is a glycoprotein that is expressed in the stromal, epithelial, and tumor cells, though CD200 expression has also been reported on small subsets of T cells, B cells, and dendritic cells [22–25]. CD200 expression has been reported to be induced by NF-κB and ERK signaling pathways [26, 27]. It binds to its receptor, CD200R, which is expressed by Tregs and myeloid cells [22, 28]. Overexpression of CD200 has been associated with differential outcomes across cancer types. In some tumors, such as central nervous system tumors and breast cancer, CD200 overexpression has been associated with a pro-tumorigenic effect [29, 30]. However, there have been studies in a melanoma model that have shown that CD200 expression in melanoma has an anti-tumor effect [31, 32]. Our laboratory previously reported that CD200 is overexpressed in patients with PDAC and that blockade of CD200 in a murine subcutaneous and genetically engineered mouse models reduced tumor burden, suggesting a pro-tumor role for CD200 in the context of pancreatic cancer [33]. Previously, we showed that CD200 is expressed by PDAC cell lines and in the stromal compartments of PDAC tissue specimens [33]. However, exactly which stromal and tumor populations in the pancreatic TME express CD200 has yet to be determined.
In addition to existing as a cell-surface protein, the ectodomain of CD200 can be cleaved by matrix metalloproteinases (MMPs) and a disintegrin and metalloproteinase (ADAM) proteins [34, 35]. The resulting soluble CD200 (sCD200) can be readily measured in plasma samples [35, 36]. Importantly, the CD200 ectodomain is still functional and thus can still interact with its receptor and initiate an immunosuppressive response [37]. Furthermore, in chronic lymphocytic leukemia (CLL), patients with higher sCD200 levels have worse overall survival (OS) and progression-free survival (PFS) than patients with lower sCD200 [38]. In PDAC, it is unknown if sCD200 is detectable in the plasma, which MMPs are involved, and if circulating levels of sCD200 correlate with worse OS and PFS in patients.
We hypothesize that CD200 protein and mRNA transcripts are upregulated by the tumor and stroma cells in the PDAC TME. Furthermore, we hypothesize that sCD200 is upregulated in PDAC and correlates to OS and PFS. Here, we investigate where CD200 is spatially expressed in the pancreatic TME and identify CD200 + cell populations. Finally, we investigate the mechanism of CD200 cleavage in PDAC and the correlation between sCD200 and OS and PFS in metastatic PDAC.
Methods
Multiplex immunofluorescence of PDAC specimens
Human tissue microarrays (TissueArray.com, PA961f and PA807) containing pancreatic tumors (n = 127), pancreatic tumor-adjacent tissue (n = 27), and normal pancreatic tissue (n = 18) were stained according to the protocol described previously [39, 40]. In brief, tissues were prepped on a slide warmer at 60 °C for 1 h, followed by three 10 min washes in xylene to remove paraffin. Tissue was rehydrated by 10 min washes in 100%, 90%, and 75% ethanol, followed by a 2 min wash with deionized water. Slides were fixed with 10% neutral buffered formalin for 30 min. Slides were blocked in BLOXALL (Vector, SP-6000) for 10 min. The primary antibodies for αSMA (Abcam, ab5694), CD45 (Abcam, ab10558), and FAP (Abcam, ab53066) were diluted 1:100. Primary antibody for PDGFRβ (Abcam, ab32570) was diluted 1:300, primary antibody for CD200 (Abcam, ab203887) was diluted 1:75, and primary antibody for PanCK (DAKO, M3515) was diluted 1:50. For each round of staining, slides were incubated with primary antibody for 1 h. DAPI (AKOYA Biosciences, FP1490) was diluted by adding 3 drops into 1 mL TBST. Slides were stained with DAPI for 10 min. 3 drops of Mouse/Rabbit (AKOYA Biosciences, ARH1001EA) secondary antibody were used for 10 min. Opals (AKOYA Biosciences, NEL861001KT) 480, 520, 570, 620, 690 were diluted 1:50; TSA-DIG was diluted 1:100; and 780 was diluted 1:25. Slides were stained with opals 480, 520, 570, 620, 690, and TSA-DIG for 10 min. Slides were stained with opal 780 for 1 h. Antigen-Retrieval was accomplished using AR6 (AKOYA, AR600250ML) and AR9 (AKOYA, AR900250ML) buffers followed by microwaving for 45 s at 100% power and 15 min at 20% power. After completing all rounds of staining, slides were mounted using ProLong™ Diamond Antifade Mountant (Invitrogen, P36970). Slides were imaged using Vectra Polaris and analyzed with QuPath.
Pancreatic stellate cell isolation and nanostring analysis
Human PDAC tissues were obtained from ten patients (PSC1-PSC10) undergoing surgical resection at The Ohio State University Wexner Medical Center. The tissue was dissected into 0.5–1 mm3 pieces and plated in six-well 10 cm2 uncoated culture wells in DMEM (10% FBS, 1% AA) for two to three weeks. PSCs grew out of the pancreas and were characterized by morphology and αSMA expression. PSCs were maintained in culture for three passages. Human fetal primary pancreatic fibroblast cell lines were used as a control for normal PSCs and were obtained from Vitro Biopharma and cultured in MSC-GRO media with antibiotics. RNA was collected from patient PSCs (PSC1-PSC10) and control fibroblast cell lines via TRIzol extraction. RNA was analyzed using the nCounter PanCancer Immune Profiling Panel (Nanostring Technologies, Seattle Washington).
Western blot
Harvested PSC1, PSC2, PSC3, PSC4, and PSC5 cells were incubated in lysis buffer (RIPA buffer, 1:100 protease inhibitor, 1:100 phosphatase inhibitor) for 1 h, after which sample buffer/mercaptoethanol (1:100 mercaptoethanol in Laemmli buffer) was added. Samples were then boiled for 10 min. Samples were run on an SDS–polyacrylamide gel (BioRad Mini Protean Tgx gradient gels) followed by transfer to nitrocellulose membranes (BioRad). Proteins were blocked in Tris-buffered saline containing 0.5% BSA. Primary antibodies used: rabbit anti-human CD200 (Abcam, ab203887) and mouse anti-human β-actin loading control (Invitrogen, MA5-15739). IRDye-fluorescent secondary antibodies for goat anti-rabbit (LiCOR, 926-32211) and goat anti-mouse (LiCOR, 926-68070) were used. Images for protein bands were obtained using LiCOR Odyssey CLx and analyzed with ImageStudio.
Single-cell RNA-sequencing dataset analysis
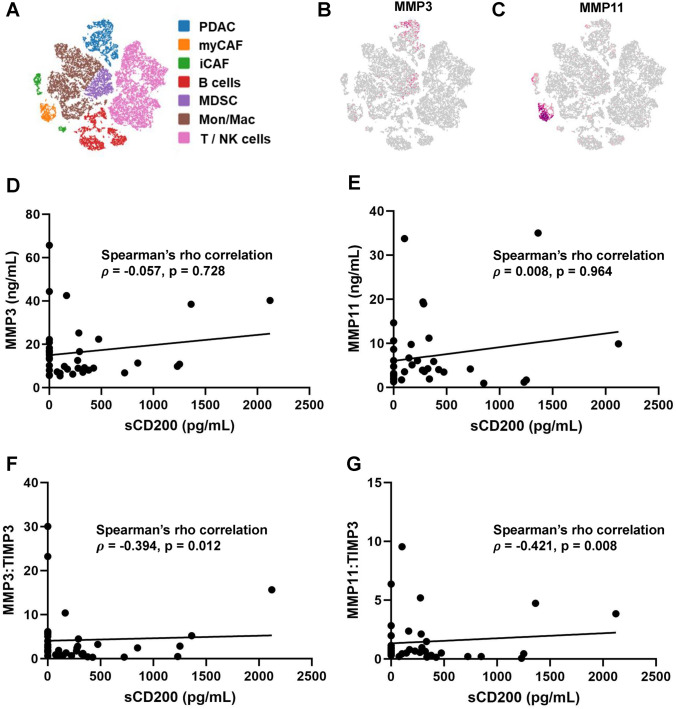
Publicly available single-cell RNA-sequencing data (accession number GSE129455) on PDAC patient tumor samples from NIH dbGaP [41] were used to evaluate CD200 expression on myCAFs and iCAFs, and MMP3 and MMP11 expression in the pancreatic TME. Volcano plots were generated using Molecular and Genomics Informatics Core (MaGIC) Volcano Plot Tool, and pathway analysis was done via the Reactome pathway database.
Cytometry by time of flight (CyTOF)
Peripheral Blood Mononuclear Cells (PBMCs) were obtained from additional research participants with PDAC and healthy donors using a density gradient centrifugation method with Ficoll-Paque (Pharmacia Biotech, 171440-03). Isolated PBMCs were lysed with Red Blood Cells lysis buffer and then washed with Maxpar Cell Staining Buffer (Standard Biotools, 201068). 3 × 106 cells were aliquoted per sample and treated with 5 uL of Human TruStain FcX (BioLegend, 422302) for 10 min. Samples were then surfaced stained with metal-isotope bound antibodies (Supplemental Table 1) from the Maxpar Direct Immune Profiling Assay kit (Standard Biotools, 201334) with the addition of antibodies for CD11b (Standard Biotools, 3209003B), CD33 (BioLegend, 303419), and CD200 (BioLegend, 329219) followed by three washes in Maxpar Cell Staining Buffer. Cells were then stained with intercalation solution (Cell-ID Intercalator-Ir (Standard Biotools, S00093) diluted to 125 nM in Maxpar Fix and Perm (Standard Biotools, S00092)). After staining, samples were washed twice with Maxpar cell staining buffer, followed by two washes with EDTA diluted to 5 uM in deionized H2O. PBMCs were transferred to filter cap flow tubes. Maxpar acquisition solution (Standard Biotools, 201248) and EQ Four Element Calibration beads (Standard Biotools, 201078) were added to the samples prior to being run through the Helios Mass Cytometer. Data were uploaded to and analyzed with OMIQ.
Enzyme-linked immunosorbent assay (ELISA)
Blood samples were obtained from patients with metastatic PDAC who previously participated in a randomized clinical trial (RCT) [NCT01280058]. In this phase 2, RCT participants were randomized to receive pelareorep (a proprietary oncolytic reovirus under investigation as a cancer therapeutic) + carboplatin/paclitaxel or carboplatin/paclitaxel alone [42]. There were no differences in clinical outcomes, including PFS or OS, between the two trial arms. Baseline plasma samples collected prior to receiving therapy were selected for the current analysis. sCD200 in the plasma and pancreatic cell supernatants was measured using a human CD200 ELISA kit (Invitrogen by Thermo Fisher Scientific, EHCD200) which was run according to the manufacturer’s instructions. MMP3, MMP11, and TIMP3 in PDAC participants were measured by human MMP3 (R&D Systems, DMP300), Human MMP11 (LSBio, LS-F21105-1), and human TIMP3 (Thermo Fisher, EH458RB) ELISA kits which were run according to the manufacturer’s instructions. The median sCD200 level was calculated in participants that had detectable sCD200 (defined 40 pg/mL or greater; this value represents the lower detection limit of the kit). Concentrations above the median were defined as “high,” and values below the mean were classified as “low.” Quantified MMP3, MMP11, and TIMP3 were used to calculate patient ratios of circulating MMP3/TIMP3 and MMP11/TIMP3, and the ratios were correlated to sCD200 plasma concentrations.
Statistics
Analysis of variance using Tukey’s test for pairwise comparisons was used to compare CD200 by pathology diagnosis (normal, cancer adjacent, pancreatic cancer), pathology grade (1, 2, 3), and cancer stage (I, II, and III/IV), while independent-samples t tests were used to compare CD200 in relation to median age (i.e., < 53 yrs vs. ≥ 53 yrs) and sex. Independent-samples t tests were also used to compare CD200 MMI between PDAC subjects and healthy controls for myeloid populations and specific T cell populations as well as to compare CD200 expression between PSCs derived from PDAC patients and healthy controls. Kaplan–Meier curves were used to examine the differences in overall survival and progression-free survival between those with detectable sCD200 (> 40 pg/mL) and those with undetectable sCD200 and then between those with sCD200 in the upper 25th percentile and those in the lower 75th percentile. Log-rank tests were used to compare survival between the groups. Scatterplots were constructed to examine the relationship between sCD200 and each of the following: MMP3, MMP11, MMP3/TIMP3, and MMP11/TIMP3, and Spearman’s ρ correlation coefficient was calculated to quantify the strength and direction of the associations. Figures were made using GraphPad Prism 10.
Results
CD200 is overexpressed in the pancreatic TME
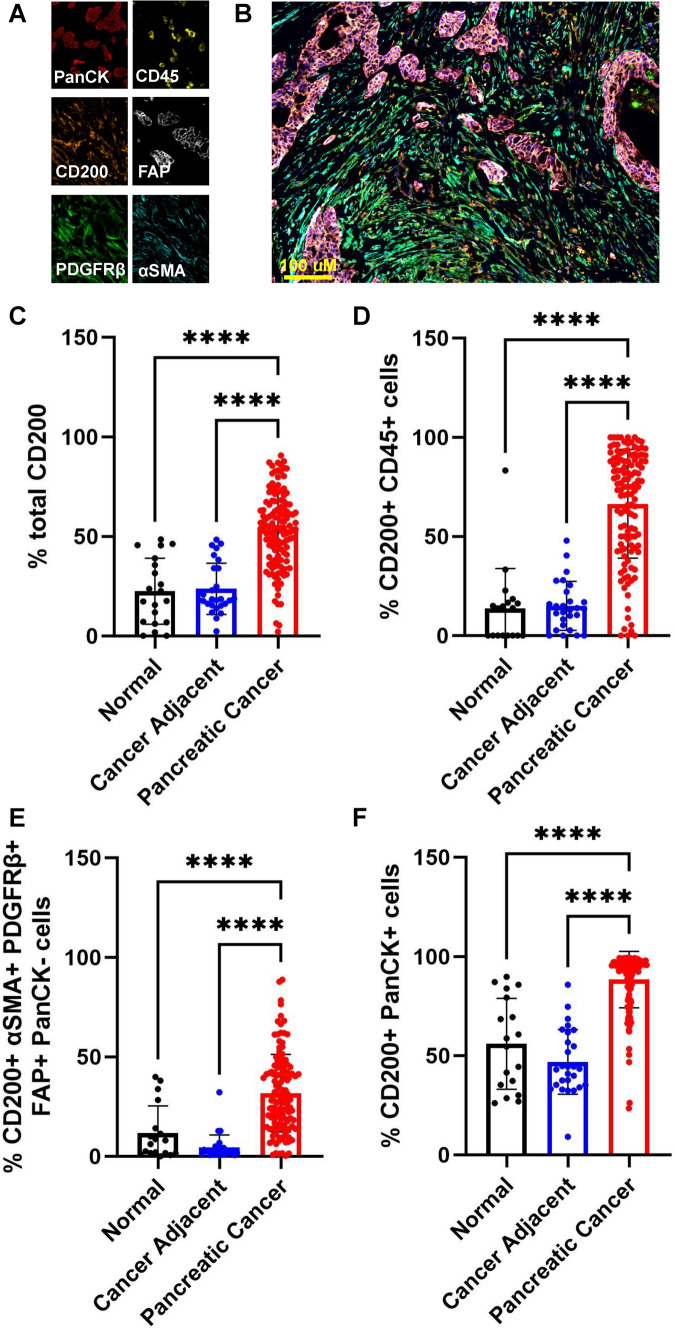
We previously reported that CD200 is elevated in PDAC [33], and we hypothesized that CD200 was overexpressed on both tumor and stromal cells in the pancreatic TME. To further investigate this, we stained pancreatic cancer tissue (n = 127) specimens from different stages of disease progression, sex, and age (Supplemental Table 2) along with cancer-adjacent (n = 27) and normal tissues (n = 18) with a panel for multiplex IF focusing on stromal markers (Fig. 1A & B). Stromal populations were identified as expressing one or a combination of αSMA, PDGFRβ, and FAP and were negative for pan cytokeratin (PanCK). CD45 + only cells were identified as immune cells and PanCK expression was used to identify epithelial cells and tumor cells of epithelial origin. Malignant tissues significantly expressed more CD200 overall than the cancer-adjacent and normal pancreatic tissues (Fig. 1C). When looking at CD200 across different cell populations in the pancreatic TME, we observed that CD200 expression was increased on immune populations (Fig. 1D), stromal populations (Fig. 1E), and epithelial cells (Fig. 1F). We also found that total CD200 expression was not affected by pathology grade (Supplemental Fig. 1A), nor did pathology grade impact CD200 expression on immune (Supplemental Fig. 1B) or stromal (Supplemental Fig. 1C) cells. CD200 expression was significantly decreased on tumor cells in grade 3 tumors (Supplemental Fig. 1D). Similarly, when examining if CD200 expression in the TME was affected by disease stage, we observed an insignificant difference in total CD200 expression (Supplemental Fig. 1E) as well no significant difference in CD200 expression on immune (Supplemental Fig. 1F), stromal (Supplemental Fig. 1G), and tumor cells (Supplemental Fig. 1H). When looking at age, we observed no significant difference in CD200 expression in younger patients compared to older patients (Supplemental Fig. 1I-L). We also compared CD200 expression in the pancreatic TME of females and males. There was an insignificant difference in CD200 expression between female and male patients (Supplemental Fig. 1M-P). Ultimately, these results indicate that CD200 is overexpressed by tumor, stromal cells, and immune populations in the PDAC TME, and that CD200 expression is not dependent on pathology grade or cancer stage.
Fig. 1.
CD200 is upregulated in the pancreatic TME. Tissue microarrays were stained for A tumor (PanCK), immune (CD45), stroma (FAP, PDGFRβ, αSMA), and CD200. B Representative image of full multiplex IF panel. CD200 expression in normal (n = 18), cancer-adjacent (n = 27), and pancreatic cancer (n = 127) tissues were quantified in QuPath as C % total CD200 D % CD200 + CD45 + immune cells, E % CD200 + αSMA + PDGFRβ + FAP + PanCK- stromal cells, and F % CD200 + PanCK + epithelial cells. Means ± STD, **** = p < 0.0001
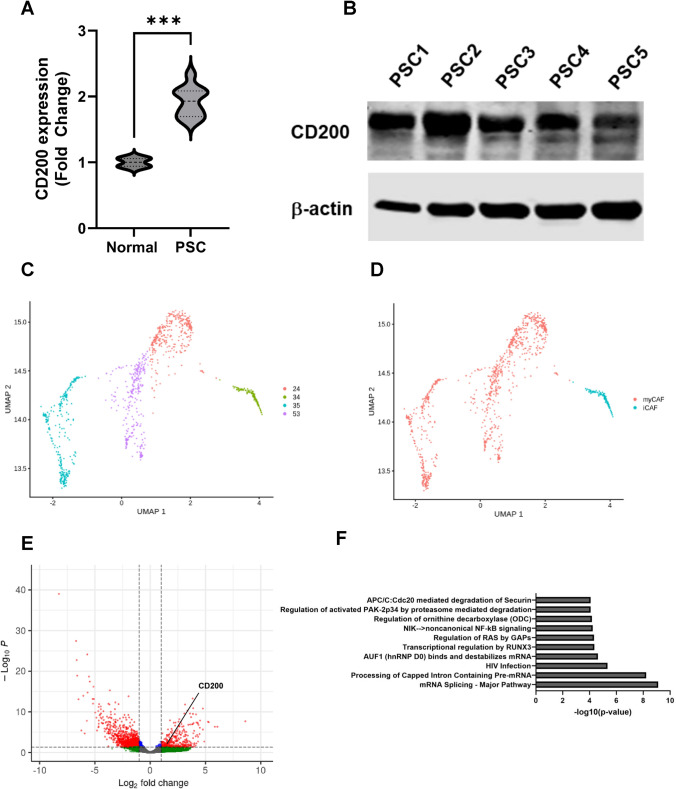
CD200 is upregulated by iCAFs in the pancreatic TME
Our multiplex IF identified that CD200 was expressed by stromal cells in the PDAC TME. We confirmed that PDAC-derived PSCs had upregulated CD200 mRNA (Fig. 2A) and protein (Fig. 2B) expression compared to normal pancreas fibroblast controls. However, the stromal cells of the PDAC TME are heterogeneous, comprising of PSCs, iCAFs, and myCAFs. Thus, we investigated whether CD200 expression was limited to specific subsets of stromal populations. We analyzed publicly available single-cell RNA-seq data [41] of PDAC tissue collected from patients. We identified 4 clusters of CAFs (Fig. 2C). Genetic markers to distinguish iCAFs and myCAFs (Supplemental Table 3) were used to further identify clusters 24, 35, and 53 as myCAFs and cluster 34 as iCAFs (Fig. 2D). Analysis of genes on the iCAFs revealed that CD200 was significantly upregulated on iCAFs (Fig. 2E) and that iCAFs had significant changes in the NFκB and RUNX3 pathways as well as pathways related to mRNA processing (Fig. 2F). These data indicate that CD200 is more highly expressed on iCAFs in PDAC.
Fig. 2.
CD200 expression is upregulated on iCAFs. A CD200 mRNA expression from PDAC patient PSCs compared to normal HPPFC controls via Nanostring analysis. B Western Plot showing CD200 expression in PDAC patient PSCs. C UMAP of CAF clusters from single-cell RNA-sequencing dataset of PDAC patients from NIH dbGaP and D identification of clusters as myCAFs and iCAFs. E Volcano-plot showing significantly upregulated and downregulated genes in iCAFs. F Top 10 pathways significantly affected in iCAFs via Reactome analysis. *** = p < 0.001
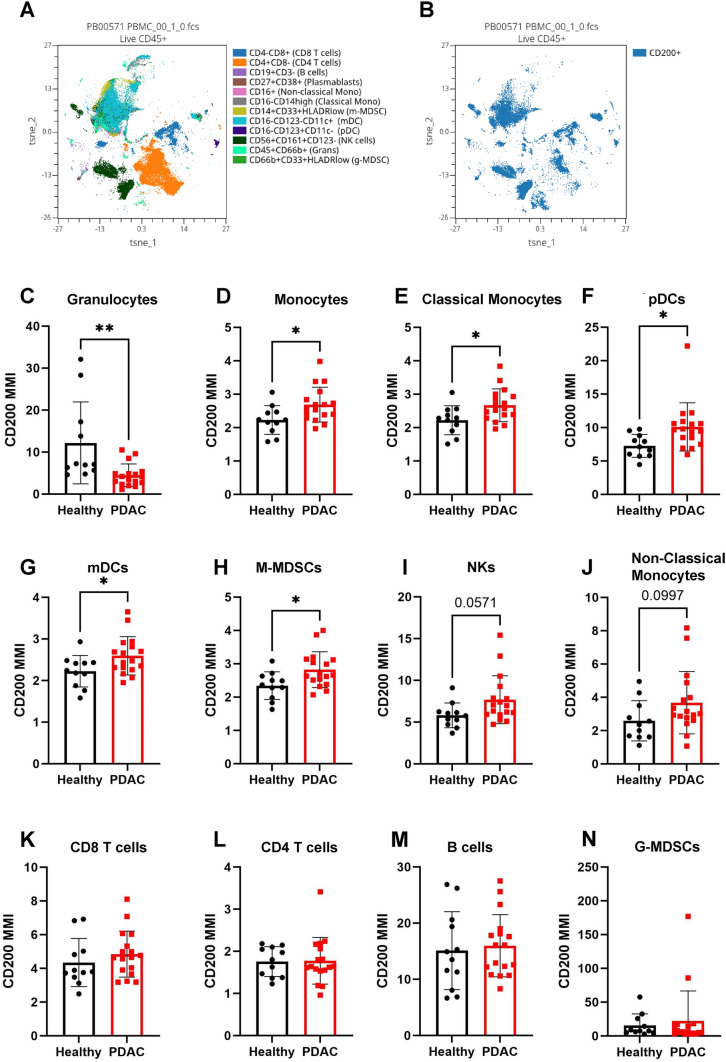
CD200 expression on immune populations
While we have observed CD200 expression on the tumor and stromal cells in the PDAC TME, CD200 has been reported to be expressed on immune populations, such as T cells [23], B cells [24], and DCs [25]. To investigate changes in CD200 expression on immune populations in PDAC, we designed a CyTOF panel to analyze over 37 different immune populations (Supplemental Fig. 2) on PBMCs of PDAC patients (n = 17) undergoing surgical resection and healthy/control individuals (n = 12) as previously described [43]. We identified circulating immune populations (Fig. 3A) and quantified their CD200 expression (Fig. 3B). We observed that PDAC patients had significantly decreased CD200 expression on granulocytes (Fig. 3C). CD200 expression was significantly increased on monocytes (Fig. 3D), classical monocytes (Fig. 3E), plasmacytoid DCs (pDCs) (Fig. 3F), myeloid DCs (mDCs) (Fig. 3G), and monocytic MDSCs (M-MDSCs) (Fig. 3H). We also observed a general increase in NK cells (Fig. 3I) and non-classical monocytes (Fig. 3J). However, we observed no significant difference in CD200 expression on CD8 T cells (Fig. 3K), CD4 T cells (Fig. 3L), B cells (Fig. 3M), and granulocytic MDSCs (G-MDSCs) (Fig. 3N). Our CyTOF panel also allowed for us to compare CD200 expression on specific T cell populations in PDAC patients compared to healthy individuals. PDAC patients did not have a significant change in CD200 expression on naïve (Supplemental Fig. 3A), activated (Supplemental Fig. 3B), CM (Supplemental Fig. 3C), EM (Supplemental Fig. 3D), or TE (Supplemental Fig. 3E) CD8 T cells. However, on CD4 T cells, we observed a significant increase in EM CD4 T cells (Supplemental Fig. 3F), and no significant change in naïve (Supplemental Fig. 3G), activated (Supplemental Fig. 3H), CM (Supplemental Fig. 3I), or TE (Supplemental Fig. 3J) CD4 T cells. We also observed no significant difference in CD200 expression on Tregs (Supplemental Fig. 3K), Th1 (Supplemental Fig. 3L), Th2 (Supplemental Fig. 3M), or Th17 cells (Supplemental Fig. 3N). This indicates that CD200 expression is upregulated on myeloid-derived immune populations in PDAC, and that there is no significant change in CD200 on CD8 T cell populations in PDAC.
Fig. 3.
CD200 is upregulated on myeloid populations in the blood of patients with PDAC. PBMCs were isolated from PDAC patients (n = 17) and healthy donors (n = 12) and stained with a panel of 38 antibodies for CyTOF. A A tSNE showing immune populations and B CD200 expression across immune populations. Mean metal intensity (MMI) of CD200 was quantified on C granulocytes, D monocytes, E classical monocytes, F pDCs, G mDCs, H M-MDSCs, I NK, J Non-classical monocytes, K CD8 T cells, L CD4 T cells, M B cells, and N G-MDSCs. Means ± STD, * = p < 0.05
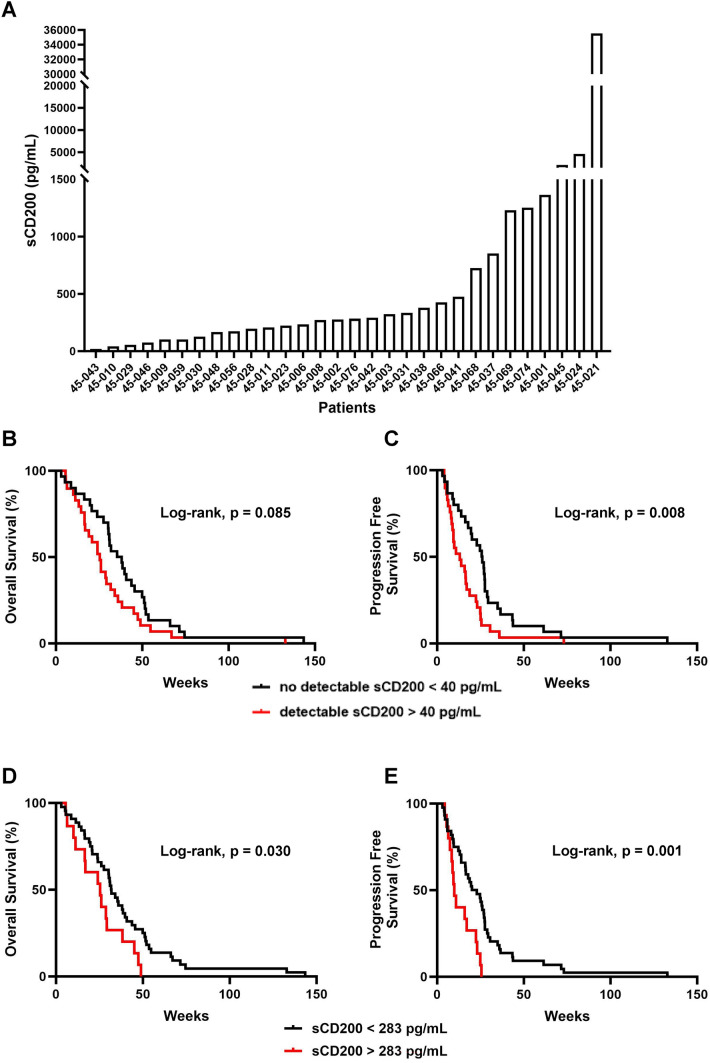
PDAC patients with high sCD200 have worse survival
CD200 can be cleaved and expressed as sCD200 in the plasma in patients with CLL [38]; however, this has not been explored in PDAC. Thus, we investigated whether sCD200 levels were elevated in metastatic PDAC. We confirmed via ELISA that PDAC patients can express sCD200 in their plasma, though there is intersubject variability in concentrations (Fig. 4A). Due to the variance of sCD200 levels, we hypothesized that the amount of sCD200 correlated with OS and PFS in PDAC. We compared OS and PFS of patients that had detectable sCD200 (n = 29) to patients that did not have detectable sCD200 (n = 30) and observed worse OS when sCD200 was detectable (Fig. 4B) and significantly worse PFS (Fig. 4C). We further decided to look at how high sCD200 correlates with survival. We observed that patients that have high sCD200 (n = 15) levels have significantly worse OS (Fig. 4D) and PFS (Fig. 4E) than patients with low or non-detectable sCD200 (n = 44). Ultimately, these data suggest that sCD200 can be predicative of worse survival outcomes in patients with metastatic PDAC.
Fig. 4.
Higher sCD200 is associated with worse survival in PDAC patients. A Waterfall plot of sCD200 expression in plasma from patients with metastatic PDAC measures with ELISA. Survival curves for B OS and C PFS in patients with detectable sCD200 (n = 29) compared to patients with undetectable sCD200 (n = 30). Survival curves for D OS and E PFS in patients with high sCD200 (n = 15) compared to patients with low sCD200 (n = 44)
MMP3 and MMP11 levels in patients with PDAC patients correlate with sCD200 levels
MMP3 and MMP11 have previously been shown to be involved in CD200 ectodomain shedding in basal cell carcinoma [34] and thus may be involved in regulating the cleavage of CD200 in PDAC. Single-cell RNA-sequencing of cell populations from the NIH dbGaP [41] in the PDAC TME (Fig. 5A) indicates that MMP3 is expressed in the tumor (Fig. 5B) and MMP11 is expressed in the stromal populations (Fig. 5C). Since both MMP3 and MMP11 are expressed in the pancreatic TME and can cleave the ectodomain of CD200, we hypothesized that the circulating levels of MMP3 and MMP11 in patients with PDAC correlated with the circulating levels of sCD200. To investigate this, we performed ELISAs to quantify the concentration of MMP3 and MMP11 in the plasma of patients with PDAC, which we then correlated to the sCD200 levels. There was no significant correlation between the circulating levels of MMP3 (Fig. 5D) or MMP11 (Fig. 5E) and sCD200 in PDAC. We then hypothesized that factors that regulate MMP3 and MMP11 enzymatic activity, such as expression of TIMP3 [35, 44], may be contributing to the lack of correlation observed. Since TIMP3 can inhibit MMP3 and MMP11 cleavage activity, we performed an ELISA to quantify TIMP3, then quantified the ratio of MMP3/TIMP3 and MMP11/TIMP3, and ultimately correlated these ratios to sCD200 levels. We observed that patients with a higher MMP3/TIMP3 (Fig. 5F) ratio or MMP11/TIMP3 (Fig. 5G) ratio had a significant correlation with sCD200 levels in PDAC. These results suggest that sCD200 correlates with MMP3 and MMP11 levels.
Fig. 5.
MMP3 and MMP11 correlate with sCD200. A tSNE of populations in pancreatic TME identified by single-cell RNA-sequencing dataset of PDAC patients from NIH dbGaP and expression of B MMP3 and C MMP11 in the PDAC TME. ELISA on plasma from metastatic PDAC patients (n = 40) targeting MMP3, MMP11, and TIMP3 expression. D MMP3 expression and E MMP11 expression correlated with sCD200 levels. F MMP3/TIMP3 and G MMP11/TIMP3 ratios correlated with sCD200 levels
Discussion
We previously reported CD200 is expressed in the pancreatic TME [33], and in this report, we are the first to show that CD200 is overexpressed on stromal, immune, and epithelial cells compared to cancer-adjacent tissues and normal tissues. However, an important limitation to our studies is that we were not able to analyze tissue that contain invasive edges. Future staining of invasive edges for CD200 expression may reveal whether or not CD200 plays a role for pancreatic cancer invasion and progression. Furthermore, staining of the tissue only indicates which cell types express CD200 in the pancreatic TME. Future analyses using newer techniques such as spatial transcriptomics could provide valuable information to the function of these CD200 + cell types and their interactions in the tumor.
Importantly, this is the first demonstration that CD200 is expressed on iCAFs in PDAC. iCAFs have a secretory phenotype and can secrete inflammatory cytokines and chemokines [14, 15]. In particular, iCAFs secrete SDF-1 and MCP-1 [15]. SDF-1 and MCP-1 have previously been shown to be chemoattractants for MDSCs and other myeloid cells through the SDF-1/CXCR4 axis [45] and MCP-1/CCR2 axis [46], respectively. The CD200 + iCAFs would be able to interact directly with the recruited myeloid cells, which express the receptor CD200R [33]. As CD200-CD200R signaling has been previously reported to promote an immunosuppressive phenotype in dendritic cells and macrophages [47, 48], the interaction between CD200 + iCAFs and CD200R + myeloid cells may be a mechanism that promotes an immunosuppressive TME in pancreatic cancer. Thus, further studies analyzing whether CD200 + iCAFs interact with CD200R + myeloid cells and promote their immunosuppressive activity is warranted.
In addition to having upregulated CD200, we have reported that iCAFs in PDAC have significant changes in in the NFκB and RUNX3 pathways as well as pathways related to mRNA processing and splicing. Importantly, the NFκB pathway has previously been shown to be involved in upregulating CD200 expression [26]. We also observed a significant difference in the RUNX3 pathway in iCAFs. Increased RUNX3 expression was previously shown to be increased in CD200 + CTLs and may also be correlative to CD200 expression in iCAFs [23]. RUNX3 has also previously been shown to be expressed in pancreatic cancer and to play a role in promoting immunosuppression [49, 50]. Interestingly, we also observed a significant difference in mRNA splicing pathways. CD200 has previously been shown to be affected by alternative splicing, which can result in a truncated version of CD200 [51]. This truncated CD200 has been shown to be a competitive antagonist to full-length CD200 [52]. Further investigation into the ratio of full-length CD200 expression vs truncated CD200 expression on iCAFs and how this ratio impacts iCAF function is warranted.
MDSCs and monocytes were both observed to be circulating in peripheral blood of PDAC patients and are associated with worse overall survival in PDAC [53, 54]. We are the first to report that CD200 expression increases on circulating monocytes, particularly classical monocytes, pDCs and mDCs, and M-MDSCs in patients with PDAC compared to healthy individuals. We have previously reported that the receptor CD200R is also significantly upregulated on MDSCs and that CD200 stimulation promotes their expansion [33]. Interactions between the circulating CD200 + myeloid cells and CD200R + MDSCs could be promoting the differentiation and expansion of immunosuppressive myeloid populations that could infiltrate into the tumor and promote an immunosuppressive TME. CD200 + CD8 + T cells were previously reported to be crucial for effective PD-1/PDL-1 blockade in murine tumor models [23]. Here, we did not observe any differences in CD200 expression on CD8 + T cells; furthermore, we previously reported that dual blockade of CD200 and PD-1 further reduces tumor burden in a subcutaneous pancreatic tumor model [33]. The discrepancy may be due to the abundance of myeloid populations in PDAC [55] and that CD200 signaling in myeloid cells is associated with the secretion of factors that mediate an immunosuppressive response on T cells [17, 18, 47, 48]. Our observation that CD200 expression increases on myeloid populations coupled with previous observations of myeloid populations (macrophages and MDSCs) being abundant in PDAC [55] may suggest that CD200 is promoting tumor progression through a myeloid-dependent mechanism. Thus, future studies should be conducted to specifically investigate the role of CD200 signaling in myeloid cells in PDAC.
The ectodomain of CD200 has been reported to be shed, and the resulting sCD200 has been reported in the plasma of patients with various types of cancers, including CLL and breast cancer [38, 56]. This is the first report to show that sCD200 is expressed in the plasma of PDAC patients. MMPs are secreted in the pancreatic TME and are involved in ECM remodeling, angiogenesis, metastasis. MMP3 and MMP11 are stromelysins that are involved in degrading ECM components [57] and their overexpression in PDAC is associated with worse survival [58, 59]. Both MMP3 and MMP11 have been shown to be capable of cleaving CD200 [34]. Though we reported no correlation between MMP3 and MMP11 plasma levels with sCD200 plasma levels in PDAC patients, we are the first to show a correlation of MMP3/TIMP3 and MMP11/TIMP3 plasma levels with sCD200 levels. However, our findings do not show causation, and further investigation is necessary to determine if MMP3 and MMP11 directly contribute to the sCD200 levels observed in patients. In addition, this study is not comprehensive of all MMPs and ADAM proteins that may be involved in CD200 ectodomain shedding in PDAC. For example, in CLL, ADAM28 is involved in CD200 ectodomain shedding [35], and other MMPs and ADAM proteins are involved in regulating protein shedding [60, 61], and thus, more comprehensive analyses on how CD200 ectodomain shedding is regulated are warranted. In addition, as there was a wide range of sCD200 expression in patients with metastatic PDAC, it would be worthwhile to expand the population size to further understand sCD200 correlation with MMP3 and MMP11.
Finally, we are the first to report that sCD200 is expressed in the plasma in metastatic PDAC patients and, importantly, that high levels of circulating sCD200 are associated with worse OS and PFS. This study is limited as only the plasma from metastatic patients were used to evaluate sCD200. Future investigations into whether sCD200 levels are impacted by cancer stage and if it is also a prognostic biomarker in earlier stages in PDAC are warranted. sCD200 has been reported to be fully functional and thus is still capable of interacting with the receptor bound on the surface of myeloid cells [37]. The circulating sCD200 in PDAC patients may be another avenue in which CD200R + myeloid cells can be stimulated and skewed towards an immunosuppressive phenotype, though this will need to be investigated in future studies. Ultimately, these results suggest that CD200 may be a biomarker for survival prognosis and may provide support for future investigations on targeting CD200 in PDAC.
Supplementary Information
Below is the link to the electronic supplementary material.
Author contributions
JW and TAM conceived and designed the study. JW, SJ, DM, HL, TP, and MAT performed the experiments. JM and TLF provided methodology and resources for multiplex IF. BWB performed the analyses for the single-cell RNA-sequencing. SC provided statistical analysis on raw data. JW wrote the manuscript, which was reviewed and edited by all co-authors. All authors read and approved the final manuscript.
Funding
The project described was in part funded by OSUCCC Cure for Pancreatic Cancer Development Fund. This project was supported by the OSU Comprehensive Cancer Center (OSUCCC-P30CA016058), Analytical Cytometry, Genomics, Bioinformatics and Clinical and Translational Sciences Shared Resources and University Laboratory Animal Resources. The original clinical trial NCI 8601/NCT01280058 from which pre-treatment samples were used was funded by the Cancer Therapy Evaluation Program (CTEP) through the UM1 grant held by OSUCCC. We also thank K. Das from the Immune Monitoring and Discovery Platform (IMDP) of the Pelotonia Institute for Immuno-Oncology (PIIO) for technical support. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Advancing Translational Sciences or the National Institutes of Health.
Declarations
Conflict of Interest
Authors declare that they have no potential conflict of interest.
Ethics approval and consent to participate
All patients provided voluntary written informed consent (Institutional Review Board protocol: 2010C0051 and 2010C0055) to participate. The protocols and subsequent amendments were approved by The Ohio State University Institutional Review Board. All other experiments were completed under the research protocols (2014R00000086; 2013R00000056) approved by The Ohio State University Institutional Biosafety Committee.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Siegel RL, Giaquinto AN, Jemal A. Cancer statistics. CA Cancer J Clin. 2024;74(1):12–49. doi: 10.3322/caac.21820. [DOI] [PubMed] [Google Scholar]
- 2.Kamisawa T, Wood LD, Itoi T, Takaori K. Pancreatic cancer. Lancet. 2016;388(10039):73–85. doi: 10.1016/S0140-6736(16)00141-0. [DOI] [PubMed] [Google Scholar]
- 3.Mpilla GB, Philip PA, El-Rayes B, Azmi AS. Pancreatic neuroendocrine tumors: therapeutic challenges and research limitations. World J Gastroenterol. 2020;26(28):4036–4054. doi: 10.3748/wjg.v26.i28.4036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Backx E, Coolens K, Van den Bossche JL, Houbracken I, Espinet E, Rooman I. On the origin of pancreatic cancer: molecular tumor subtypes in perspective of exocrine cell plasticity. Cell Mol Gastroenterol Hepatol. 2022;13(4):1243–1253. doi: 10.1016/j.jcmgh.2021.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Moletta L, Serafini S, Valmasoni M, Pierobon ES, Ponzoni A, Sperti C. Surgery for recurrent pancreatic cancer: is it effective? Cancers (Basel) 2019 doi: 10.3390/cancers11070991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wood LD, Canto MI, Jaffee EM, Simeone DM. Pancreatic cancer: pathogenesis, screening, diagnosis, and treatment. Gastroenterology. 2022;163(2):386–402 e1. doi: 10.1053/j.gastro.2022.03.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Karandish F, Mallik S. Biomarkers and targeted therapy in pancreatic cancer. Biomark Cancer. 2016;8(Suppl 1):27–35. doi: 10.4137/BiC.s34414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Adamska A, Elaskalani O, Emmanouilidi A, Kim M, Abdol Razak NB, Metharom P, Falasca M. Molecular and cellular mechanisms of chemoresistance in pancreatic cancer. Adv Biol Regul. 2018;68:77–87. doi: 10.1016/j.jbior.2017.11.007. [DOI] [PubMed] [Google Scholar]
- 9.Conroy T, Desseigne F, Ychou M, Bouche O, Guimbaud R, Becouarn Y, Adenis A, Raoul JL, Gourgou-Bourgade S, de la Fouchardiere C, Bennouna J, Bachet JB, Khemissa-Akouz F, Pere-Verge D, Delbaldo C, Assenat E, Chauffert B, Michel P, Montoto-Grillot C, Ducreux M, Groupe Tumeurs Digestives of U, Intergroup P FOLFIRINOX versus gemcitabine for metastatic pancreatic cancer. N Engl J Med. 2011;364(19):1817–1825. doi: 10.1056/NEJMoa1011923. [DOI] [PubMed] [Google Scholar]
- 10.Von Hoff DD, Ervin T, Arena FP, Chiorean EG, Infante J, Moore M, Seay T, Tjulandin SA, Ma WW, Saleh MN, Harris M, Reni M, Dowden S, Laheru D, Bahary N, Ramanathan RK, Tabernero J, Hidalgo M, Goldstein D, Van Cutsem E, Wei X, Iglesias J, Renschler MF. Increased survival in pancreatic cancer with nab-paclitaxel plus gemcitabine. N Engl J Med. 2013;369(18):1691–1703. doi: 10.1056/NEJMoa1304369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Amrutkar M, Gladhaug IP. Pancreatic cancer chemoresistance to gemcitabine. Cancers (Basel) 2017 doi: 10.3390/cancers9110157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ho WJ, Jaffee EM, Zheng L. The tumour microenvironment in pancreatic cancer - clinical challenges and opportunities. Nat Rev Clin Oncol. 2020;17(9):527–540. doi: 10.1038/s41571-020-0363-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Geng X, Chen H, Zhao L, Hu J, Yang W, Li G, Cheng C, Zhao Z, Zhang T, Li L, Sun B. Cancer-associated fibroblast (CAF) heterogeneity and targeting therapy of CAFs in pancreatic cancer. Front Cell Dev Biol. 2021;9:655152. doi: 10.3389/fcell.2021.655152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ohlund D, Handly-Santana A, Biffi G, Elyada E, Almeida AS, Ponz-Sarvise M, Corbo V, Oni TE, Hearn SA, Lee EJ, Chio II, Hwang CI, Tiriac H, Baker LA, Engle DD, Feig C, Kultti A, Egeblad M, Fearon DT, Crawford JM, Clevers H, Park Y, Tuveson DA. Distinct populations of inflammatory fibroblasts and myofibroblasts in pancreatic cancer. J Exp Med. 2017;214(3):579–596. doi: 10.1084/jem.20162024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mace TA, Ameen Z, Collins A, Wojcik S, Mair M, Young GS, Fuchs JR, Eubank TD, Frankel WL, Bekaii-Saab T, Bloomston M, Lesinski GB. Pancreatic cancer-associated stellate cells promote differentiation of myeloid-derived suppressor cells in a STAT3-dependent manner. Cancer Res. 2013;73(10):3007–3018. doi: 10.1158/0008-5472.CAN-12-4601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Weber R, Groth C, Lasser S, Arkhypov I, Petrova V, Altevogt P, Utikal J, Umansky V. IL-6 as a major regulator of MDSC activity and possible target for cancer immunotherapy. Cell Immunol. 2021;359:104254. doi: 10.1016/j.cellimm.2020.104254. [DOI] [PubMed] [Google Scholar]
- 17.Yu J, Du W, Yan F, Wang Y, Li H, Cao S, Yu W, Shen C, Liu J, Ren X. Myeloid-derived suppressor cells suppress antitumor immune responses through IDO expression and correlate with lymph node metastasis in patients with breast cancer. J Immunol. 2013;190(7):3783–3797. doi: 10.4049/jimmunol.1201449. [DOI] [PubMed] [Google Scholar]
- 18.Miret JJ, Kirschmeier P, Koyama S, Zhu M, Li YY, Naito Y, Wu M, Malladi VS, Huang W, Walker W, Palakurthi S, Dranoff G, Hammerman PS, Pecot CV, Wong KK, Akbay EA. Suppression of myeloid cell arginase activity leads to therapeutic response in a NSCLC mouse model by activating anti-tumor immunity. J Immunother Cancer. 2019;7(1):32. doi: 10.1186/s40425-019-0504-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Amrutkar M, Aasrum M, Verbeke CS, Gladhaug IP. Secretion of fibronectin by human pancreatic stellate cells promotes chemoresistance to gemcitabine in pancreatic cancer cells. BMC Cancer. 2019;19(1):596. doi: 10.1186/s12885-019-5803-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nicolas-Boluda A, Vaquero J, Vimeux L, Guilbert T, Barrin S, Kantari-Mimoun C, Ponzo M, Renault G, Deptula P, Pogoda K, Bucki R, Cascone I, Courty J, Fouassier L, Gazeau F, Donnadieu E. Tumor stiffening reversion through collagen crosslinking inhibition improves T cell migration and anti-PD-1 treatment. Elife. 2021 doi: 10.7554/eLife.58688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kuczek DE, Larsen AMH, Thorseth ML, Carretta M, Kalvisa A, Siersbaek MS, Simoes AMC, Roslind A, Engelholm LH, Noessner E, Donia M, Svane IM, Straten PT, Grontved L, Madsen DH. Collagen density regulates the activity of tumor-infiltrating T cells. J Immunother Cancer. 2019;7(1):68. doi: 10.1186/s40425-019-0556-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Liu JQ, Hu A, Zhu J, Yu J, Talebian F, Bai XF. CD200-CD200R Pathway in the regulation of tumor immune microenvironment and immunotherapy. Adv Exp Med Biol. 2020;1223:155–165. doi: 10.1007/978-3-030-35582-1_8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wang X, Zha H, Wu W, Yuan T, Xie S, Jin Z, Long H, Yang F, Wang Z, Zhang A, Gao J, Jiang Y, Wang L, Hu C, Wan YY, Li QJ, Symonds ALJ, Jia Q, Zhu B. CD200(+) cytotoxic T lymphocytes in the tumor microenvironment are crucial for efficacious anti-PD-1/PD-L1 therapy. Sci Transl Med. 2023;15(679):eabn5029. doi: 10.1126/scitranslmed.abn5029. [DOI] [PubMed] [Google Scholar]
- 24.Diskin B, Adam S, Soto GS, Liria M, Aykut B, Sundberg B, Li E, Leinwand J, Chen R, Kim M, Salas RD, Cassini MF, Buttar C, Wang W, Farooq MS, Shadaloey SAA, Werba G, Fnu A, Yang F, Hirsch C, Glinski J, Panjwani A, Weitzner Y, Cohen D, Asghar U, Miller G. BTLA(+)CD200(+) B cells dictate the divergent immune landscape and immunotherapeutic resistance in metastatic vs. primary pancreatic cancer. Oncogene. 2022;41(38):4349–4360. doi: 10.1038/s41388-022-02425-4. [DOI] [PubMed] [Google Scholar]
- 25.Izumi G, Nakano H, Nakano K, Whitehead GS, Grimm SA, Fessler MB, Karmaus PW, Cook DN. CD11b(+) lung dendritic cells at different stages of maturation induce Th17 or Th2 differentiation. Nat Commun. 2021;12(1):5029. doi: 10.1038/s41467-021-25307-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pontikoglou C, Langonne A, Ba MA, Varin A, Rosset P, Charbord P, Sensebe L, Deschaseaux F. CD200 expression in human cultured bone marrow mesenchymal stem cells is induced by pro-osteogenic and pro-inflammatory cues. J Cell Mol Med. 2016;20(4):655–665. doi: 10.1111/jcmm.12752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Petermann KB, Rozenberg GI, Zedek D, Groben P, McKinnon K, Buehler C, Kim WY, Shields JM, Penland S, Bear JE, Thomas NE, Serody JS, Sharpless NE. CD200 is induced by ERK and is a potential therapeutic target in melanoma. J Clin Invest. 2007;117(12):3922–3929. doi: 10.1172/JCI32163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gorczynski R, Chen Z, Kai Y, Lee L, Wong S, Marsden PA. CD200 is a ligand for all members of the CD200R family of immunoregulatory molecules. J Immunol. 2004;172(12):7744–7749. doi: 10.4049/jimmunol.172.12.7744. [DOI] [PubMed] [Google Scholar]
- 29.Moertel CL, Xia J, LaRue R, Waldron NN, Andersen BM, Prins RM, Okada H, Donson AM, Foreman NK, Hunt MA, Pennell CA, Olin MR. CD200 in CNS tumor-induced immunosuppression: the role for CD200 pathway blockade in targeted immunotherapy. J Immunother Cancer. 2014;2(1):46. doi: 10.1186/s40425-014-0046-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Curry A, Khatri I, Kos O, Zhu F, Gorczynski R. Importance of CD200 expression by tumor or host cells to regulation of immunotherapy in a mouse breast cancer model. PLoS ONE. 2017;12(2):e0171586. doi: 10.1371/journal.pone.0171586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Liu JQ, Talebian F, Wu L, Liu Z, Li MS, Wu L, Zhu J, Markowitz J, Carson WE, 3rd, Basu S, Bai XF. A critical role for CD200R signaling in limiting the growth and metastasis of CD200+ melanoma. J Immunol. 2016;197(4):1489–1497. doi: 10.4049/jimmunol.1600052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Talebian F, Liu JQ, Liu Z, Khattabi M, He Y, Ganju R, Bai XF. Melanoma cell expression of CD200 inhibits tumor formation and lung metastasis via inhibition of myeloid cell functions. PLoS ONE. 2012;7(2):e31442. doi: 10.1371/journal.pone.0031442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Choueiry F, Torok M, Shakya R, Agrawal K, Deems A, Benner B, Hinton A, Shaffer J, Blaser BW, Noonan AM, Williams TM, Dillhoff M, Conwell DL, Hart PA, Cruz-Monserrate Z, Bai XF, Carson WE, 3rd, Mace TA. CD200 promotes immunosuppression in the pancreatic tumor microenvironment. J Immunother Cancer. 2020 doi: 10.1136/jitc-2019-000189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Morgan HJ, Rees E, Lanfredini S, Powell KA, Gore J, Gibbs A, Lovatt C, Davies GE, Olivero C, Shorning BY, Tornillo G, Tonks A, Darley R, Wang EC, Patel GK. CD200 ectodomain shedding into the tumor microenvironment leads to NK cell dysfunction and apoptosis. J Clin Invest. 2022 doi: 10.1172/JCI150750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Twito T, Chen Z, Khatri I, Wong K, Spaner D, Gorczynski R. Ectodomain shedding of CD200 from the B-CLL cell surface is regulated by ADAM28 expression. Leuk Res. 2013;37(7):816–821. doi: 10.1016/j.leukres.2013.04.014. [DOI] [PubMed] [Google Scholar]
- 36.Wong KK, Brenneman F, Chesney A, Spaner DE, Gorczynski RM. Soluble CD200 is critical to engraft chronic lymphocytic leukemia cells in immunocompromised mice. Cancer Res. 2012;72(19):4931–4943. doi: 10.1158/0008-5472.CAN-12-1390. [DOI] [PubMed] [Google Scholar]
- 37.Wong KK, Zhu F, Khatri I, Huo Q, Spaner DE, Gorczynski RM. Characterization of CD200 ectodomain shedding. PLoS ONE. 2016;11(4):e0152073. doi: 10.1371/journal.pone.0152073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.D'Arena G, Vitale C, Coscia M, Lamorte D, Pietrantuono G, Perutelli F, D'Auria F, Statuto T, Valvano L, Tomasso A, Griggio V, Jones R, Mansueto G, Villani O, D'Agostino S, Viglioglia V, De Feo V, Calapai F, Mannucci C, Sgambato A, Efremov DG, Laurenti L. CD200 Baseline serum levels predict prognosis of chronic lymphocytic leukemia. Cancers (Basel) 2021 doi: 10.3390/cancers13164239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lazarus J, Akiska Y, Perusina Lanfranca M, Delrosario L, Sun L, Long D, Shi J, Crawford H, Di Magliano MP, Zou W, Frankel T. Optimization, design and avoiding pitfalls in manual multiplex fluorescent immunohistochemistry. J Vis Exp. 2019 doi: 10.3791/59915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mukherjee D, Chakraborty S, Bercz L, D'Alesio L, Wedig J, Torok MA, Pfau T, Lathrop H, Jasani S, Guenther A, McGue J, Adu-Ampratwum D, Fuchs JR, Frankel TL, Pietrzak M, Culp S, Strohecker AM, Skardal A, Mace TA. Tomatidine targets ATF4-dependent signaling and induces ferroptosis to limit pancreatic cancer progression. iScience. 2023;26(8):107408. doi: 10.1016/j.isci.2023.107408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Elyada E, Bolisetty M, Laise P, Flynn WF, Courtois ET, Burkhart RA, Teinor JA, Belleau P, Biffi G, Lucito MS, Sivajothi S, Armstrong TD, Engle DD, Yu KH, Hao Y, Wolfgang CL, Park Y, Preall J, Jaffee EM, Califano A, Robson P, Tuveson DA. Cross-species single-cell analysis of pancreatic ductal adenocarcinoma reveals antigen-presenting cancer-associated fibroblasts. Cancer Discov. 2019;9(8):1102–1123. doi: 10.1158/2159-8290.CD-19-0094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Noonan AM, Farren MR, Geyer SM, Huang Y, Tahiri S, Ahn D, Mikhail S, Ciombor KK, Pant S, Aparo S, Sexton J, Marshall JL, Mace TA, Wu CS, El-Rayes B, Timmers CD, Zwiebel J, Lesinski GB, Villalona-Calero MA, Bekaii-Saab TS. Randomized phase 2 trial of the oncolytic virus pelareorep (reolysin) in upfront treatment of metastatic pancreatic adenocarcinoma. Mol Ther. 2016;24(6):1150–1158. doi: 10.1038/mt.2016.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Thomas J, Torok MA, Agrawal K, Pfau T, Vu TT, Lyberger J, Chang H, Castillo AMM, Chen M, Remaily B, Kim K, Xie Z, Dillhoff ME, Kulp SK, Behbehani GK, Cruz-Monserrate Z, Ganesan LP, Owen DH, Phelps MA, Coss CC, Mace TA. The neonatal Fc receptor is elevated in monocyte-derived immune cells in pancreatic cancer. Int J Mol Sci. 2022 doi: 10.3390/ijms23137066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Su CW, Lin CW, Yang WE, Yang SF. TIMP-3 as a therapeutic target for cancer. Ther Adv Med Oncol. 2019 doi: 10.1177/1758835919864247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Jiang K, Li J, Zhang J, Wang L, Zhang Q, Ge J, Guo Y, Wang B, Huang Y, Yang T, Hao D, Shan L. SDF-1/CXCR4 axis facilitates myeloid-derived suppressor cells accumulation in osteosarcoma microenvironment and blunts the response to anti-PD-1 therapy. Int Immunopharmacol. 2019;75:105818. doi: 10.1016/j.intimp.2019.105818. [DOI] [PubMed] [Google Scholar]
- 46.Mittal P, Wang L, Akimova T, Leach CA, Clemente JC, Sender MR, Chen Y, Turunen BJ, Hancock WW. The CCR2/MCP-1 chemokine pathway and lung adenocarcinoma. Cancers (Basel) 2020 doi: 10.3390/cancers12123723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Fallarino F, Asselin-Paturel C, Vacca C, Bianchi R, Gizzi S, Fioretti MC, Trinchieri G, Grohmann U, Puccetti P. Murine plasmacytoid dendritic cells initiate the immunosuppressive pathway of tryptophan catabolism in response to CD200 receptor engagement. J Immunol. 2004;173(6):3748–3754. doi: 10.4049/jimmunol.173.6.3748. [DOI] [PubMed] [Google Scholar]
- 48.Hayakawa K, Wang X, Lo EH. CD200 increases alternatively activated macrophages through cAMP-response element binding protein - C/EBP-beta signaling. J Neurochem. 2016;136(5):900–906. doi: 10.1111/jnc.13492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Li J, Kleeff J, Guweidhi A, Esposito I, Berberat PO, Giese T, Buchler MW, Friess H. RUNX3 expression in primary and metastatic pancreatic cancer. J Clin Pathol. 2004;57(3):294–299. doi: 10.1136/jcp.2003.013011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Wang L, Tang W, Yang S, He P, Wang J, Gaedcke J, Strobel P, Azizian A, Ried T, Gaida MM, Yfantis HG, Lee DH, Lal A, Van den Eynde BJ, Alexander HR, Ghadimi BM, Hanna N, Hussain SP. NO(*) /RUNX3/kynurenine metabolic signaling enhances disease aggressiveness in pancreatic cancer. Int J Cancer. 2020;146(11):3160–3169. doi: 10.1002/ijc.32733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Chen Z, Ma X, Zhang J, Hu J, Gorczynski RM. Alternative splicing of CD200 is regulated by an exonic splicing enhancer and SF2/ASF. Nucleic Acids Res. 2010;38(19):6684–6696. doi: 10.1093/nar/gkq554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Chen Z, Chen DX, Kai Y, Khatri I, Lamptey B, Gorczynski RM. Identification of an expressed truncated form of CD200, CD200tr, which is a physiologic antagonist of CD200-induced suppression. Transplantation. 2008;86(8):1116–1124. doi: 10.1097/TP.0b013e318186fec2. [DOI] [PubMed] [Google Scholar]
- 53.Trovato R, Fiore A, Sartori S, Cane S, Giugno R, Cascione L, Paiella S, Salvia R, De Sanctis F, Poffe O, Anselmi C, Hofer F, Sartoris S, Piro G, Carbone C, Corbo V, Lawlor R, Solito S, Pinton L, Mandruzzato S, Bassi C, Scarpa A, Bronte V, Ugel S. Immunosuppression by monocytic myeloid-derived suppressor cells in patients with pancreatic ductal carcinoma is orchestrated by STAT3. J Immunother Cancer. 2019;7(1):255. doi: 10.1186/s40425-019-0734-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hansen FJ, David P, Akram M, Knoedler S, Mittelstadt A, Merkel S, Podolska MJ, Swierzy I, Rossdeutsch L, Klosch B, Kouhestani D, Anthuber A, Benard A, Brunner M, Krautz C, Grutzmann R, Weber GF. Circulating monocytes serve as novel prognostic biomarker in pancreatic ductal adenocarcinoma patients. Cancers (Basel). 2023 doi: 10.3390/cancers15020363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Clark CE, Hingorani SR, Mick R, Combs C, Tuveson DA, Vonderheide RH. Dynamics of the immune reaction to pancreatic cancer from inception to invasion. Cancer Res. 2007;67(19):9518–9527. doi: 10.1158/0008-5472.CAN-07-0175. [DOI] [PubMed] [Google Scholar]
- 56.Celik B, Yalcin AD, Genc GE, Bulut T, Kuloglu Genc S, Gumuslu S. CXCL8, IL-1beta and sCD200 are pro-inflammatory cytokines and their levels increase in the circulation of breast carcinoma patients. Biomed Rep. 2016;5(2):259–263. doi: 10.3892/br.2016.709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Cabral-Pacheco GA, Garza-Veloz I, Castruita-De la Rosa C, Ramirez-Acuna JM, Perez-Romero BA, Guerrero-Rodriguez JF, Martinez-Avila N, Martinez-Fierro ML. The roles of matrix metalloproteinases and their inhibitors in human diseases. Int J Mol Sci. 2020 doi: 10.3390/ijms21249739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Mehner C, Miller E, Nassar A, Bamlet WR, Radisky ES, Radisky DC. Tumor cell expression of MMP3 as a prognostic factor for poor survival in pancreatic, pulmonary, and mammary carcinoma. Genes Cancer. 2015;6(11–12):480–489. doi: 10.18632/genesandcancer.90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Zhang X, Lu J, Zhou L, You L, Liang Z, Guo J, Zhao Y. Matrix Metalloproteinase 11 as a novel tumor promoter and diagnostic and prognostic biomarker for pancreatic ductal adenocarcinoma. Pancreas. 2020;49(6):812–821. doi: 10.1097/MPA.0000000000001583. [DOI] [PubMed] [Google Scholar]
- 60.Loffek S, Schilling O, Franzke CW. Series "matrix metalloproteinases in lung health and disease": Biological role of matrix metalloproteinases: a critical balance. Eur Respir J. 2011;38(1):191–208. doi: 10.1183/09031936.00146510. [DOI] [PubMed] [Google Scholar]
- 61.Huovila AP, Turner AJ, Pelto-Huikko M, Karkkainen I, Ortiz RM. Shedding light on ADAM metalloproteinases. Trends Biochem Sci. 2005;30(7):413–422. doi: 10.1016/j.tibs.2005.05.006. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.