Abstract
Dyslipidemias are the most important coronary artery disease (CAD) risk factor. Proper management of dyslipidemia is crucial to control the epidemic of premature CAD in India. Cardiological Society of India strived to develop consensus-based guidelines for better lipid management for CAD prevention and treatment. The executive summary provides a bird's eye-view of the ‘CSI: Clinical Practice Guidelines for Dyslipidemia Management’ published in this issue of the Indian Heart Journal. The summary is focused on the busy clinician and encourages evidence-based management of patients and high-risk individuals. The summary has serialized various aspects of lipid management including epidemiology and categorization of CAD risk. The focus is on management of specific dyslipidemias relevant to India-raised low density lipoprotein (LDL) cholesterol, non-high density lipoprotein cholesterol (non-HDL-C), apolipoproteins, triglycerides and lipoprotein(a). Drug therapies for lipid lowering (statins, non-statin drugs and other pharmaceutical agents) and lifestyle management (dietary interventions, physical activity and yoga) are summarized. Management of dyslipidemias in oft-neglected patient phenotypes-the elderly, young and children, and patients with comorbidities-stroke, peripheral arterial disease, kidney failure, posttransplant, HIV (Human immunodeficiency virus), Covid-19 and familial hypercholesterolemia is also presented. This consensus statement is based on major international guidelines (mainly European) and expert opinion of lipid management leaders from India with focus on the dictum: earlier the better, lower the better, longer the better and together the better. These consensus guidelines cannot replace the individual clinician judgement who remains the sole arbiter in management of the patient.
Keywords: Dyslipidemia, LDL cholesterol, Triglycerides, Statins, India, Lipid management
1. Introduction
India has the dubious distinction of having the highest number of coronary artery disease (CAD) patients in the world. Case-control and prospective studies in India have reported that lipid abnormalities, especially raised total-, low density lipoprotein (LDL)-, and non-high-density lipoprotein-cholesterol (non-HDL-C), triglycerides and apolipoprotein B (ApoB), are the most important risk factors. Lipid management based on LDL-C and non-HDL-C target is crucial to reduce the incidence of CAD in both primary and secondary prevention settings. A number of challenges exist which include premature occurrence of major CAD risk factors; large burden of premature CAD; high prevalence of raised total, LDL and non-HDL cholesterol, familial hypercholesterolemia (FH), hypertriglyceridemia (in association with diabetes and metabolic syndrome) and elevated Lipoprotein(a) [Lp(a)]. Low status of population-level and individual-level awareness and treatment of dyslipidemias and extremely low status of guideline recommended control in the community and the clinic is also a barrier for optimal Lipid Management. There is also lack of large randomized controlled studies of various pharmacological and clinical interventions in India to develop context-specific evidence-based guidelines. The current consensus document for management of various dyslipidemias, especially raised LDL cholesterol and triglycerides, has been developed through a review of major international guidelines on lipid management and local evidence (wherever available), and reflects opinions of the leaders in lipid management in the country. The executive summary highlights specific focus areas in each of the chapters in this special issue of Indian Heart Journal.
2. Epidemiology of dyslipidemias in India
-
•
There is a significant epidemiological, genetic and causal association of raised total cholesterol, non-HDL cholesterol, LDL cholesterol, and triglycerides with ASCVD events and mortality.
-
•
Regional and multisite studies in India and data from emigrant South Asians have reported increasing population-level total- and LDL-cholesterol and triglycerides. This is in contrast to developed countries where they are declining.
-
•
Raised triglycerides are an important and unique feature of dyslipidemias in India.
-
•
HDL cholesterol has recently been relegated as a risk marker and not a risk factor.
-
•
Epidemiological studies have reported variable prevalence rates of important dyslipidemias in India. The prevalence of total cholesterol ≥200 mg/dl ranges from 25 to 30 %, non-HDL cholesterol ≥160 mg/dl 25–30 %, LDL cholesterol ≥130 mg/dl: 25–30 %, non-HDL cholesterol ≥130 mg/dl: 50–55 %, LDL cholesterol >100 mg/dl: 50–55 %, triglycerides >150 mg/dl: 30–40 % and low HDL cholesterol: 60–70 %.
-
•
Most national studies have reported higher prevalence of hypercholesterolemia in most Southern and a few North Indian states, more in urban than rural areas, whereas the prevalence of high triglycerides and low HDL cholesterol is similar throughout the country.
-
•
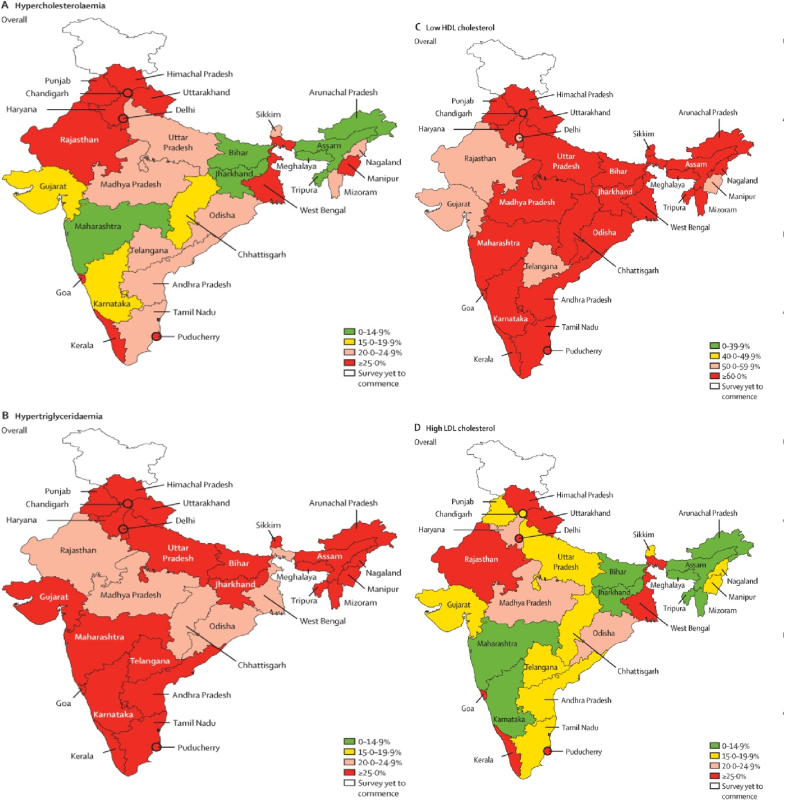
The 2023 ICMR-INDIAB study has also reported the prevalence of various dyslipidemias in all the states of the country (Fig. 1). The prevalence of total cholesterol ≥200 mg/dl ranges from 4.6-7.9 % to 45.6–50.3 %; LDL cholesterol ≥130 mg/dl from 4.6-6.2 % to 46.8–52.1 %; triglycerides ≥150 mg/dl from 21.2-22.7 % to 43.4–47.9 %; and low HDL cholesterol ranges from 51.8 to 83.1 %.
-
•
Studies have also reported low status of population-level and individual-level awareness and treatment of various dyslipidemias.
Fig. 1.
State level prevalence of various dyslipidemias in ICMR-INDIAB Study. All rights and permissions secured (Licence No. 5740641442671). Original figure from Anjana RM, Unnikrishnan R, Deepa M, et al.; ICMR-INDIAB Collaborative Study Group. Metabolic noncommunicable disease health report of India: the ICMR-INDIAB national cross-sectional study (ICMR-INDIAB-17). Lancet Diabetes Endocrinol. 2023 Jul;11(7):474-489. doi: 10.1016/S2213-8587(23)00119-5.
3. Evaluation of lipid parameters
-
•
Accurate measurement of various lipids-total cholesterol, cholesterol lipoproteins and triglycerides-is important for CAD prevention and risk management.
-
•
Measurement of non-fasting levels of total cholesterol, LDL cholesterol, HDL cholesterol, non-HDL cholesterol, and triglycerides for risk estimation and guiding treatment is recommended.
-
•
Measurement of lipid profile in clinics and emergency departments can lead to early estimation of CAD risk and rapid initiation of lipid lowering lipid lowering therapies.
-
•
CAD risk and baseline levels of LDL cholesterol guide intensity of lipid lowering therapies (Table 1).
-
•
There is an urgent need for standardization of lipid estimation in medical laboratories across the country so that every eligible individual can receive evidence-based lipid lowering interventions.
Table 1.
Standard lipid testing panels and targets for various risk groups (all values in mg/dl).
| Lipid parametera | Desirable levels of various lipid fractions |
|||
|---|---|---|---|---|
| Low risk | Moderate risk | High risk | Very High Risk | |
| LDL cholesterolb | <100 | <100 | <70 | <55 |
| Non-HDL cholesterol | <130 | <130 | <100 | <85 |
| HDL cholesterol | >40 M, >50 W | >40 M, >50 W | >40 M, >50 W | >40 M, >50 W |
| Triglycerides | <150 | <150 | <150 | <150 |
| Lipoprotein(a)a | <50 | <50 | <50 | <50 |
The values may vary according to the laboratory-method used.
Direct or calculated according to Friedewald formula; Extremely high-risk group has not been included in this Table. (refer to Fig. 2).
4. Cardiovascular risk classification and suggested targets
-
•
Risk stratification is important to guide lipid lowering therapy and to identify goals (Fig. 2).
-
•
Five categories are recommended: low risk, moderate risk, high risk, very high risk and extremely high-risk groups. Goals for various dyslipidemias are summarized in Table 1.
-
•
General population with no risk factor can be classified as low risk.
-
•
Moderate risk group comprises presence of any one of the standard risk factors: smoking/tobacco use, hypertension, diabetes or family history of premature CAD (men <55 and women <60 years).
-
•
High-risk category includes individuals with 2 or more risk factors with no manifest atherosclerotic cardiovascular disease (ASCVD), chronic kidney disease, long standing diabetes >10 years, or heterozygous familial hypercholesterolemia (HeFH).
-
•
Very high-risk category has individuals with clinical evidence of atherosclerotic CAD, atherosclerotic disease in other vascular beds, diabetes >20 years, HeFH with ASCVD, or coronary imaging showing >50 % lesion in 2 coronary vessels. ASCVD includes coronary artery, cerebrovascular and peripheral vascular disease.
-
•
Extremely high-risk group comprises those with recurrent vascular events and ASCVD with genetic dyslipidemias (FH& High Lp(a)).
Fig. 2.
Cardiovascular risk estimation and lipid management goals.
4.1. Acute coronary syndrome (Fig. 3)
Fig. 3.
Lipid management in the setting of acute coronary syndromes.
-
•
In acute coronary syndrome (ACS) patients, a non fasting lipid profile is acceptable as the goal is to achieve LDL cholesterol below 55 mg/dl as early as possible.
-
•
A proven concept in LDL cholesterol management in ACS hit hard and hit early with combination Lipid-lowering therapy.
-
•
High dose of statins alone may not be able to attain the LDL cholesterol goal in a significant number of patients. Therefore, addition of ezetimibe at initiation of treatment is recommended.
-
•
It is recommended to add another non-statin drug if LDL cholesterol target of <55 mg/dl is not achieved at 4 weeks: choices are bempedoic acid, PCSK9 inhibitors or inclisiran.
4.2. Stable atherosclerotic cardiovascular disease (Fig. 4)
Fig. 4.
Lipid management in chronic coronary syndromes.
-
•
Chronic coronary syndrome (CCS) and other ASCVDs are common in clinical practice.
-
•
In these patients the goal is to achieve LDL cholesterol <55 mg/dl and non HDL cholesterol <85 mg/dl (Table 1).
-
•
A significant proportion of Indian population suffers from atherogenic dyslipidemia (raised small dense LDL cholesterol and triglycerides with low HDL cholesterol). In such patients, it is recommended to initiate high intensity statin therapy (Table 2). A significant proportion shall also require additional ezetemibe.
Table 2.
Commonly available statins in India and daily dose according to intensity of treatment.
| Drug | High Intensity | Moderate intensity | Low intensity |
|---|---|---|---|
| Atorvastatin | 40–80 mg | 10–20 mg | 5 mg |
| Rosuvastatin | 20–40 mg | 5–10 mg | – |
| Pitavastatin | – | 2–4 mg | 1 mg |
5. Drug therapy
5.1. Statins in dyslipidemia management
-
•
Statins are the drugs of choice for management if dyslipidemias.
-
•
Statins have proven protective effects in all clinical situations: primary prevention, secondary prevention, following revascularization, diabetes and patients with HFeH.
-
•
Observational studies have suggested that South Asians and Indians are hyper-responders to statins and may require lower doses to achieve the same effect. This group may also be more susceptible to statin-induced adverse effects.
-
•
Statins are particularly useful in lowering total and LDL cholesterol and triglycerides in high dose.
-
•
Statins effects are dose dependent and the lipid lowering efficacy varies for different statins.
-
•
Rosuvastatin (water soluble) and atorvastatin (fat soluble) are considered the most potent statins and lower doses of these agents are considered as moderate intensity statins.
-
•
All newer lipid lowering agents: ezetimibe, bempedoic acid, PCSK9 (proprotein convertase subtilisin/kexin type 9) inhibitors and Inclisiran can be combined with statins and have multiplicative effect.
-
•
In general, statins are safe and well tolerated, but are associated with (usually reversible) muscle and liver toxicity. This should be promptly detected and treated. Reduction of the dose, temporary withdrawal with careful re-introduction or changing to a lower potency statin may help (Fig. 5).
-
•
Statins are contraindicated during pregnancy and breast feeding and are not recommended in pre-menopausal patients with or without diabetes who are considering pregnancy, or not using adequate contraception.
-
•
An increased incidence of new onset diabetes has been noted with statins. This is dose dependent and is particularly seen in patients with preexisting metabolic syndrome and prediabetes. However, the benefits far outweigh the risk.
-
•
Increase of hepatic transaminases occurs in 0.5–2% of statin users within 3 months of drug initiation and is not significantly different from placebo in randomized clinical trials.
-
•
Routine use of muscle and liver enzyme monitoring either at baseline or subsequently are not recommended.
-
•
Severe liver or muscle injury are uncommon and are usually reversible once the offending statin is withdrawn.
Fig. 5.
Statin associated muscle symptoms (SAMS) management.
5.2. Traditional and novel non-statin lipid lowering drugs
5.2.1. Ezetimibe
-
•
The statin-ezetimibe combination is recommended to achieve LDL cholesterol target early after acute coronary events.
-
•
This combination is also useful in HeFH as an initial therapy.
-
•
Ezetimibe may be used alone (15 % reduction in LDL cholesterol) or in combination with bempedoic acid (40 % reduction in LDL cholesterol) in statin-intolerant patients.
5.2.2. Bempedoic acid
-
•
Bempedoic acid added to maximally tolerated statin therapy is approved to lower LDL cholesterol in adults with primary hypercholesterolemia or mixed dyslipidemias, HeFH, and in patients with ASCVD who require additional lowering of LDL cholesterol despite on maximum tolerated dose of a statin or statin plus ezetimibe.
-
•
It is also indicated either alone or in combination with ezetimibe in patients who are statin-intolerant. Alone, bempedoic acid reduces LDL cholesterol by 25 %. The risk of myopathy is low.
-
•
No increase in new-onset or worsening of diabetes is observed with bempedoic acid. There is a mild but clinically relevant increase in serum uric acid.
5.2.3. Inclisiran
-
•
Inclisiran is a long-acting small interfering RNA (siRNA) that inhibits the transcription of PCSK9. This results in a decrease in PCSK9 generation in hepatocytes and increase in LDL receptor expression in liver cell membrane leading to about 50 % reduction in serum LDL cholesterol levels.
-
•
Inclisiran is administered subcutaneously twice a year and has potential of better compliance.
-
•
Inclisiran therapy is associated with 24 % lower rate of major adverse cardiovascular events with no increase in unwanted side events. Results of major outcome trials are awaited.
-
•
Inclisiran improves compliance (twice a year injection) and causes less LDL-C variability.
5.2.4. Fibrates
-
•
The most definite indication of fenofibrate monotherapy is fasting serum triglyceride >500 mg/dl, primarily to reduce the risk of acute pancreatitis.
-
•
Fibrate monotherapy offers only a modest reduction in cardiovascular events without no reduction in stroke, cardiovascular mortality, or total mortality.
-
•
Combination of fenofibrate and statin in patients with type 2 diabetes may yield better outcomes in management of mixed dyslipidemia.
5.2.5. Fish oils
-
•
Fish oils (eicosapentenoic acid EPA, docosahexanoic acid DHA) reduce serum triglycerides by about 25 %. They may mildly increase LDL cholesterol levels.
-
•
EPA (and not DHA) in large dose may have cardioprotective effects. Randomised trials of high dose EPA are inconclusive.
-
•
A randomized trial of highly purified IPE (icosapent ethyl) showed significant reduction of major cardiovascular events.
-
•
Clinical use of these omega 3 fatty acids from dietary supplements is limited by large number of capsules required to achieve triglyceride reducing doses.
-
•
Alpha linolenic acid (ALA) concentrates have no significant benefits on cardiovascular outcomes.
5.3. Miscellaneous drugs
5.3.1. Bile Acid Sequestrants (BAS)
-
o
Reduce serum LDL cholesterol by about 20 % but may accentuate hypertriglyceridemia.
-
o
Despite cardiovascular outcome benefits, BAS have a limited use due to poor tolerance and better efficacy of statins.
-
o
In practice, BAS find use as second-line lipid-lowering agents in patients who cannot tolerate high-dose statin or in subjects whose target levels are not achieved with statin monotherapy. Triple drug therapy with statin, ezetimibe, and a bile acid sequestrant is effective in many patients with HeFH.
-
o
BAS is the only lipid-lowering class that is safe for women planning pregnancy or during lactation.
5.3.2. Lomatipide
-
o
Lomitapide lowers levels of all ApoB-containing lipoproteins, including very low density (VLDL), LDL and chylomicrons by inhibiting microsomal triglyceride transfer protein (MTP) enzyme. It causes significant reduction in both LDL-C (more so in combination with statins) and triglycerides.
-
o
Lomatipide is approved for the treatment of adult patients with HoFH.
-
o
Close monitoring for hepatotoxicity is required.
5.3.3. Mipomersen
-
o
Mipomersen is a single-stranded synthetic antisense oligonucleotide (ASO) that affects the production and secretion of apoB-containing lipoproteins with demonstrated efficacy in both HeFH and HoFH patients but response is variable.
-
o
Due to the risk for hepatotoxicity, it is approved in the US for restricted use in homozygous FH.
5.4. PCSK9 inhibitors
-
•
PCSK9 inhibitors reduce LDL receptor (LDLR) clearance, increase hepatic LDLR density that results in increased hepatic uptake and lowering of LDL cholesterol.
-
•
PCSK9 inhibitors evolocumab and alirocumab are approved for clinical use. Evolocumab is presently available in India. These drugs reduce LDL cholesterol by 50–60 %.
-
•
Evolocumab is available as subcutaneous injection, to be administered as 140 mg every 2 weeks or 420 mg once a month.
-
•
PCSK9 inhibitors are generally well tolerated with few side effects.
-
•
PCSK9 Inhibitors are indicated in patients with established cardiovascular disease, or high risk of cardiovascular events or and familial hypercholesterolemia.
-
•
Currently they are used to reduce LDL cholesterol below 70 mg/dl in high risk patients on maximally tolerated dose of statins and/or ezetimibe who fail to reach targets.
-
•
They have been proven to reduce risk of major adverse cardiovascular events in patients with cardiovascular disease, especially post-acute coronary syndrome or stroke.
-
•
PCSK9 inhibitors are very efficacious but expensive. They should be used in those who are most likely to benefit: very high ASCVD risk population (Table 3).
Table 3.
Non statin drugs and their effects.
| Drug | Major Mechanism | Lipid Effects |
CV Outcomes | Clinical Indication | Dose, Frequency | Use in Special Situations |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| LDL-C | TG | HDL-C | Apo B | Lp(a) | Hepatic Dysfunction | Renal Dysfunction | Pregnancy Category | Lactation | |||||
| Fenofibrate | PPAR α Activation | −10 %–15 % | −30 %–45 % | +10 %–15 % | −10 %–15 % | Limited data suggest increase in Lp(a) | −11 % in total CV events | Fasting TG > 500 mg/dl | 145 mg OD |
C/I in acute liver disease | C/I in severe renal disease | C | Avoidable |
| Niacin | Decreased production of VLDL-TG | −20 %–40 % | −25 %–30 % | +20 %–35 % | Decrease in dose- dependent manner | −23 % | −28 % in non-fatal MI, no further benefit on background statin | Withdrawn from market | 2–3 g/day | May cause acute liver injury | Well tolerated | C | Avoidable |
| Icosapent Ethyl | Supresses lipogenic gene expression; enhances expression of LPL; β oxidation of FA | +3 % | −25 % | −5% | −7% | Not well studied | −25 % in fatal and non-fatal CV outcomes on background statin | Adjunct to diet to reduce TG levels in adults with severe hypertriglyceridemia; Adjunct to statin therapy to reduce the risk of CV events when TG > 150 mg/dl. | 2 g BD | Believed to be safe and beneficial | Safe | C | Not C/I but safety not well documented |
| Colesevalam | Interruption of enterohepatic circulation of bile acids | −20 % | Trivial increase | +10 % | Modest decrease | – | −20 % in non-fatal MI | Add on therapy for LDL-C reduction | 625 mg tab: 3 tabs BD |
No signals of toxicity | Safe in mild to moderate dysfunction | Not assigned but seems safe | Seems safe |
| Ezetimibe | Inhibition of NPC1L1 | −15 % | −10 % | +5 % | −11 %–17 % | – | 2 % ARR in CV outcomes added to statin after ACS | Inability to achieve LDL-C target on statin, HeFH; β sitosreolemia | 10 mg OD | Not recommended in moderate to severe hepatic insufficiency | No serious safety concerns | No safety signals but not well studied | Risk unknown |
| Bempedoic Acid | Inhibition of ACL | −17 % TO 28 % | – | – | −15 % | – | 1.3 % ARR in 3 point MACE among patients with ASCVD/high risk and statin intolerance | Inability to achieve LDL-C target on statin/statin intolerance | 180 mg OD | Safe in mild to moderate hepatic dysfunction, not studied in severe dysfunction | Safe in mild to moderate renal dysfunction, not studied in severe dysfunction | Not recommended | Not recommended |
| Evolocumab (PSCK9i) |
PCSK9i | −60 % | −10 %–15 % | +6 % | −53 % | −20 %–25 % | −15 % in adverse CV outcomes over background statin therapy | ASCVD, Primary hypercholesterolemia, HeFH, HoFH | ASCVD, HeFH: 140 mg sc every 2 weeks; HoFH: 420 mg once a month | Safe in mild to moderate hepatic dysfunction | Safe | Limited data; benefit: risk assessment desirable | Limited data |
| Inclisiran | A siRNA that Inhibits transcription of PCSK9 | −51 % | −12 % | +5 % | −43 % | −25 % | −24 % MACE | HeFH and ASCVD adjuvant to statin | 284 mg sc on day 1 and 90 then twice a year | Safe in mild to moderate hepatic dysfunction | Safe in mild to moderate renal dysfunction, not studied in severe dysfunction | Not recommended | Not recommended |
Abbreviations: ACL: Adenosine triphosphate-citrate lyase, ACS: Acute coronary syndrome, ApoB: Apolipoprotein B 100, ARR: Absolute risk reduction, ASCVD: Atherosclerotic cardiovascular disease, C/I: Contraindicated, ESRD: End stage renal disease, FA: Fatty acid, HDL C: High density lipoprotein cholesterol, HeFH: Heterozygous familial hypercholesterolemia, HoFH: Homozygous familial hypercholesterolemia; hsCRP: Hight sensitive C reactive protein, LDL-C: Low density lipoprotein cholesterol, Lp(a): Lipoprotein a, LPL: Lipoprotein lipase, PPAR α: Peroxisome proliferator-activated receptor alpha, MACE: Major adverse cardiovascular events, NPC1L1: Niemann-Pick C1-Like 1, PCSK9i: Proprotein convertase subtilisin/kexin type 9; SC: Subcutaneous, siRNA: small interfering RNA, TG: Triglycerides, VLDL: Very low density lipoprotein. Pregnancy Category C: There are no satisfactory studies in pregnant women but animal studies demonstrated a risk to the foetus; potential benefits of the drug may outweigh the risks (Table courtesy: Dr. Bhavna Mastebhakti, DNB (T), Cardiology, Fortis-Escorts Heart Institute, New Delhi, India).
6. Triglycerides, Non-HDL cholesterol and low HDL cholesterol
-
•
Triglyceride level in the plasma is a marker for VLDL, chylomicrons, VLDL remnants and chylomicron remnants which are together called triglyceride-rich lipoproteins (TGRL).
-
•
HDL plays a prominent role in the transportation of cholesterol from the periphery to the liver, a process called reverse cholesterol transport (RCT).
-
•
Non-HDL cholesterol is comprised of all pro-atherogenic lipoproteins containing apolipoprotein B which include VLDL, IDL, LDL, chylomicron remnants and Lp(a).
-
•
Hypertriglyceridemia is closely associated with obesity, metabolic syndrome and diabetes mellitus. Nearly half of all patients with diabetes mellitus have concomitant hypertriglyceridemia.
-
•
Hypertriglyceridemia is managed by treatment of underlying causes and ASCVD risk factors, lifestyle modifications, statins to lower non-HDL-C, control of diabetes and pharmacotherapy (Fig. 6).
-
•
Though omega-3 fatty acids can bring down triglyceride levels, only icosapent ethyl has been shown to reduce cardiovascular events.
-
•
Fibric acid derivatives can lower triglyceride levels by 30–50 %, but have not been shown to reduce cardiovascular events when used without background statin therapy.
-
•
In patients with mild to moderate hypertriglyceridemia (TG 150–499 mg/dl), there is no role for fibric acid derivatives. In those with diabetes (≥40 years) or ASCVD, IPE may be considered if TG remains high after lifestyle measures and control of diabetes.
-
•
Measurement of non-HDL cholesterol is simpler, more convenient and more predictive of ASCVD than LDL-C, but less often used because LDL-C is more widely used in randomised controlled trials and international guidelines but we have included non-HDL-C as co-primary goal in our guidelines.
-
•
Therapeutic strategies directed at increasing HDL cholesterol have not been shown to improve cardiovascular outcomes and are not recommended by guidelines. However, lifestyle changes known to increase HDL cholesterol should be encouraged. These include weight reduction, aerobic physical activity like brisk walking, smoking cessation, and dietary modification (reducing carbohydrate intake).
Fig. 6.
Management of hypertriglyceridemia.
7. Lifestyle management
7.1. Issues in dietary management
-
•
Food patterns, choices, and preparation influence health, rather than rigid counting of calories or proportion of macronutrients.
-
•
Weight management is best achieved using healthy dietary patterns combined with regular exercise.
-
•
Severe restriction on total fats in diet is not supported by evidence. Increased intake of combination unsaturated fats as in Mediterranean diets is recommended. Omega-3 polyunsaturated fats (PUFA) supplementation may be useful in reducing ASCVD events in moderate to high-risk individuals with high triglycerides.
-
•
Plasma saturated fats correlate better with dietary refined carbohydrates. LDL cholesterol slightly increases with higher intake of saturated fats but restriction has no discernible effect on ASCVD incidence or mortality in randomized trials.
-
•
Atherogenic dyslipidemia is best managed by restriction of excess calories, sugars, refined carbohydrates, fried foods, and trans-fats while maintaining ideal body weight.
-
•
Isolated elevation of LDL cholesterol is managed by restriction of trans-fats and saturated fats.
-
•
The healthiest oils appear to be those high in monounsaturated fats (MUFA) and PUFA with a high N-3/N-6 ratio. The combination of MUFA- and PUFA-containing oils is a good option.
-
•
Trans fats should be totally avoided. Trans fats are present in fried foods and are influenced by cooking practices.
-
•
Minimize deep frying in refined oils because refined oils degrade easily. Traditional Indian oils with a high smoking point may be considered for frying, while reinforcing that fried foods are harmful. Palm oils should be avoided.
-
•
Food (dietary) cholesterol has a neutral association with ASCVD and lipoprotein levels. However, blood cholesterol is a major ASCVD risk factor.
-
•
Refined carbohydrates, sugar-sweetened beverages, and processed foods should be strongly restricted and replaced with healthy grains and fiber.
-
•
Dairy fats are controversial; due to recent data suggesting a neutral association with CVD, these may be advocated to replace unhealthy foods like refined carbohydrates or processed foods.
-
•
Healthy diets are plant-based, but an omnivorous diet with eggs, dairy and occasional intake of unprocessed meats is acceptable. In ASCVD patients egg yolk and red meat should be restricted. The emphasis is on intake of fruits, vegetables, whole grains, legumes, poultry, fish, and nuts. More details are in Table 4.
-
•
Modest consumption of nuts reduces cardio metabolic risk.
-
•
A healthy calorie distribution is achieved by reducing carbohydrates to approximately 50 % of total calories (restricting sugars and refined carbohydrates) and adding some healthy fats and proteins.
-
•
Alcohol intake should be restricted as much as possible and is not recommended for preventing heart disease.
-
•
Moderate consumption of tea (3–5 cups of day) and coffee (1–3 cups per day) is acceptable.
Table 4.
Recommended amounts of specific food items.
| Food items | Recommended amount (servings) | Size of 1 serving |
|---|---|---|
| Fresh vegetables, legumes | 3–5 per day | 1 cup raw veg, 1/2 cup cooked or cut veg, veg soup |
| Fresh fruits | 2–3 per day | 1medium size fruit, 1/2 cup fresh or unsweetened canned fruits, one piece about the size of your palm |
| Nuts and seeds | 1 per day | 1 ounce or a small handful of nuts |
| Whole grains | 2–3 per day | 1 medium chapati (multigrain/flour with bran, 1 slice whole grain bread, 1 cup high fibre cereal, 1/2 cup cooked brown rice |
| Dairy | 2–3 per day | 1 cup milk/curd (preferred), 1 ounce (∼28 g) cheese |
| Fish/seafoods | 2–3 per week | 100 g |
| Vegetable oils | 2–5 per day | 1 tsp oil, prefer unrefined virgin/extra virgin oils |
| Unprocessed meats | 1–3 per week | 100 g |
| Refined grains | <1–2 per day | 1 medium chapati (refined flour), 1 slice bread, 1/2 cup rice or cereal, 1 small sweet or dessert |
| Hydrogenated oils | Avoid as much as possible | Foods made with partially hydrogenated oils, fried foods (especially re-frying in same oil) |
| Sugar sweetened beverages | Avoid as much as possible | 300 ml |
| Sodium | <2.3 g recommended, 2–5 g may be acceptable per day | Not relevant |
| Eggs | 1–2 whole eggs per day | 1 egg |
| Alcohol | 1–2 small drinks males; 1 small drink females less than 3–5/week | 10 g of ethyl alcohol |
| Tea | 3-5 cups per day | 2 g loose tea in 200 ml boiled water |
| Coffee | 1–3 cups per day | 1 tablespoon full of coffee in 6 oz (∼170 ml) cup |
7.2. Exercise and lipids
-
•
Sedentary behavior and physical inactivity are associated with many negative health outcomes, including increased incidence of CAD.
-
•
Moderate to vigorous intensity physical activity (40–80 % heart rate reserve) leads to favorable changes in blood lipids and lipoproteins.
-
•
Moderate intensity physical activity should ideally be performed daily or at least 5 days/week to achieve the target of 150 min/week.
-
•
The exercise program should be personalized to each individual.
-
•
Resistance training thrice per week, in addition to moderate aerobic exercise, is recommended to reduce CAD risk.
-
•
In individuals unaccustomed to exercise it is recommended to initiate with short duration mild-to-moderate intensity sessions and gradually increase every 2–4 weeks.
-
•
It is important to consider an interaction between exercise and various lipid-lowering medications. Individuals taking statins may experience muscle pain and soreness that limit the ability to exercise. In such cases, it is recommended to temporarily discontinue the drug before resuming the challenge or introduction of another lipid-lowering agent
-
•
The current guidelines encourage yoga practice among Indians due to its numerous cardioprotective effects, including possible lipid improvement. More trials are needed.
-
•
Though the Indian data depicting the effect of exercise on lipids is scarce, exercise directly improves “Atherogenic Dyslipidemia” which is frequently present among Indians. i.e. HDL-C is increased, TG is reduced and LDL-C particle size is improved.
8. Specific co-morbidities
8.1. Stroke
-
•
Dyslipidemias, especially raised LDL cholesterol, are important risk factors for atherothrombotic ischemic stroke.
-
•
A statin-based lipid lowering strategy is effective both for primary and secondary prevention.
-
•
Treatment targets for LDL cholesterol (<55 mg/dl) in stroke survivors leads to a lower risk for additional CV events.
-
•
If the LDL cholesterol goal is not achieved or in statin-intolerant patients, a combination of ezetimibe and/or bempedoic acid along with the maximum tolerated dose of statin may be considered.
-
•
Evolocumab treatment decreases CVD and ischemic stroke risk.
8.2. Peripheral arterial disease
-
•
Peripheral arterial disease (PAD) affects 12 % of the adult population and is increasing globally.
-
•
Prevalence of CAD in PAD is 65 %. PAD is considered as very high risk and the LDL cholesterol goal is < 55 mg/dl.
-
•
High-Intensity lipid-lowering therapy is the mainstay of treatment.
-
•
Ezetimibe when added to statin leads to significant reduction of major adverse cardiovascular events in PAD.
-
•
PCSK9 inhibitors have been reported to significantly reduce adverse events in PAD vs non-PAD patients.
8.3. Congestive heart failure
-
•
Routine statin administration is not recommended in non-ischemic congestive heart failure (CHF).
-
•
Statins should be continued in CHF with CAD.
-
•
Lipophilic statins (simvastatin, pitavastatin or atorvastatin) may have beneficial effects on cardiovascular outcomes irrespective of the etiology and left ventricular function.
-
•
PCSK 9 inhibition appears to have no benefit in HF without ASCVD.
8.4. Diabetes
-
•
Dyslipidemia is common in diabetes and is characterized by low HDL cholesterol, raised triglycerides, and small dense LDL cholesterol.
-
•
Persons with diabetes are risk-stratified according to the duration of their disease, risk factor burden, and presence or absence of target organ damage.
-
•
LDL cholesterol goal is < 55 mg/dl for diabetes with ASCVD and diabetes >20 years or with multiple risk factors. Diabetes with any risk factor should have LDL cholesterol <70 mg/dl. Diabetes without risk factors or new-onset diabetes could have LDL cholesterol <100 mg/dl.
-
•
Good glycemic control helps in reducing serum triglycerides in a person with poorly controlled diabetes. Non-insulin glucose-lowering drugs may have a beneficial impact on lipid profile.
-
•
The risk-benefit ratio of statin therapy is beneficial in persons with diabetes, and this should be clearly communicated to all stakeholders.
-
•
While statins remain the first choice of therapy, in intensive or moderate dosage, bempedoic acid, ezetimibe, PCSK9 inhibitors or fenofibrate can be used to intensify treatment if targets are not met.
8.5. Other endocrine disorders
-
•
Endocrine diseases are a common cause of secondary dyslipidemia. Common endocrine causes are hypothyroidism, poorly controlled diabetes mellitus, and Cushing's syndrome. Anabolic drug abuse is emerging as an important cause.
-
•
All individuals with endocrine disease and those on long-term endocrinotropic drugs should be screened for dyslipidemia and assessed for cardiovascular risk. Those with dyslipidemia should be screened clinically and biochemically (if indicated) for endocrine disorders.
-
•
Obesity, polycystic ovary syndrome, and type 2 diabetes are associated with hypertriglyceridemia and low HDL cholesterol.
-
•
Both hypo- and hyper-thyroidism can present with hypertriglyceridemia. LDL cholesterol and Lp(a) may be lower in hyperthyroidism, but elevated in hypothyroidism
-
•
Both adult growth hormone (GH) deficiency and acromegaly may exhibit elevated LDL cholesterol and triglycerides.
-
•
Cushing's syndrome and chronic glucocorticoid therapy may be associated with increased LDL cholesterol and hypertriglyceridemia. Chronic glucocorticoid therapy may lead raised HDL cholesterol.
-
•
Menopause and male hypogonadism are associated with raised LDL cholesterol and Lp(a) and lower HDL cholesterol: these abnormalities can be reversed with appropriate hormone therapy.
-
•
Optimal hormonal status, i. e, euthyroidism, and eugonadism must be ensured in hypothyroid and hypogonadal individuals, prior to starting statin therapy
-
•
Persons on chronic lipid-lowering therapy should be screened for possible endocrine and metabolic dysfunction. Vitamin D supplementation may be offered according to individualized standards of care.
8.6. Chronic kidney disease
-
•
Patients with chronic kidney disease (CKD) have an increased risk for cardiovascular events. About 50 % of patients with CKD (Stages 4–5) have CVD.
-
•
A multipronged approach to reduce this risk includes good blood pressure control and lipid management.
-
•
Large clinical studies have reported that statins reduce all-cause mortality and cardiovascular (CV) events in people with CKD.
-
•
Lipid-lowering therapy with a statin with or without ezetimibe is recommended in patients with eGFR <60 ml/min/1.73 m2 and also in those with a preserved GFR but who have an increased urinary albumin-to-creatinine ratio (≥3 mg/mmol) for at least 3 months.
-
•
Statin treatment should not be started for the majority of hemodialysis patients without evidence of ASCVD.
-
•
Patients who were already taking statins, ezetimibe, or a statin/ezetimibe combination at the time of dialysis should consider continuing these medications, especially if they have ASCVD.
-
•
Fibrates should not be used in conjunction with statins in patients with CKD, and ezetimibe monotherapy is not recommended.
-
•
PCSK9 inhibitors are effective in lowering LDL cholesterol in CKD patients without affecting renal outcomes, although more data is awaited.
-
•
Bempedoic acid is safe in patients with mild or moderate renal impairment. No dose adjustments is necessary for patients with mild or moderate renal impairment.
8.7. Solid-organ transplant patients
-
•
Patients of organ transplant are at a significantly higher risk of developing ASCVD, triggered largely by the dyslipidemia associated with immunosuppressants.
-
•
Drug interactions with ongoing immunosuppressant therapy remain a major challenge in managing these patients with dyslipidemia.
-
•
Before initiating drug therapy for dyslipidemia, lifestyle measures such as physical activity, a Mediterranean diet, feasibility of replacing cyclosporin and mTOR inhibitors should be implemented.
-
•
Various lipid-lowering drugs particularly statins may be given, but there are no large studies available in this subset of patients. There is evidence of benefit for statins in patients undergoing transplant.
-
•
Statins intolerance or dyslipidemia despite on maximally tolerated dose, alternative or additional ezetimibe therapy may be considered. Ezetimibe should be avoided in patients who are on cyclosporin.
-
•
Combination of statins with fibrates significantly increases the risk of myotoxicity and is not recommended.
8.8. Pregnancy
-
•
Serum triglycerides and total cholesterol levels are often elevated in pregnancy.
-
•
Dietary interventions are the mainstay of the management in pregnant women.
-
•
Omega 3 fatty acids and bile acid sequestrants are safe but only moderately effective.
-
•
Statins are contraindicated in pregnancy due to the risk of teratogenicity and should also be avoided during lactation.
-
•
Statins are not recommended in pre-menopausal women considering pregnancy and not using adequate contraception.
-
•
Ezetimibe and Bempedoic acid are not recommended in pregnancy.
8.9. Liver disease
-
•
Statins are the first-line treatment for dyslipidemia in metabolic dysfunction-associated steatotic liver disease (MASLD).
-
•
Mild elevation (up to 3 fold) of liver transaminases is not a contraindication for statins.
-
•
Statins are contraindicated in decompensated cirrhosis or acute liver failure.
-
•
Drug interactions must be considered when prescribing statins to these patients particularly when given with antiviral drugs for hepatitis B and C.
-
•
Combination of ezetimibe with rosuvastatin may be more effective in reducing liver fat.
-
•
Both fibrates and omega-3 fatty acids reduce triglyceride levels but not liver fat
-
•
Saroglitazaar is approved to treat NAFLD and being evaluated for benefits in MASLD.
8.10. Inflammatory diseases
-
•
Autoimmunne connective disorders and inflammatory conditions such as rheumatoid arthritis (RA), systemic lupus erythematosus (SLE), etc. increase the risk of CVD.
-
•
The most common derangements are high triglycerides, small dense LDL and Lp(a) and low HDL cholesterol. There is direct correlation of C-reactive protein (CRP) with HDL cholesterol.
-
•
Hydroxychloroquine has been shown to reduce total and LDL cholesterol.
-
•
Cyclophosphamide reduces levels of LDL and VLDL cholesterol.
-
•
Statins are the first-choice drugs to reduce LDL cholesterol and choice depends on magnitude of lowering required and drug interactions.
-
•
Treatment of underlying condition can reduce dyslipidaemia while anti-inflammatory drugs such as steroids and calcineurin inhibitors can aggravate it. Anti-inflammatory drugs have differential effects, depending on the type of inflammatory condition, and individualization is recommended.
8.11. HIV patients
-
•
Dyslipidaemia is common in human immunodeficiency virus (HIV) patients and lead to heightened CVD risk.
-
•
There is lack of randomized trial data and expert opinion suggests statin use only if clearly indicated. Interactions of statins with HIV drugs should be considered before initiation. There is increased risk of myopathy and rhabdomyolysis with statins when prescribed along with protease inhibitors and CYP3A4 inhibitors.
-
•
Pitavastatin is the safest and simvastatin is contraindicated. The use of lower doses is suggested.
-
•
Omega 3 fatty acids are effective, though cholestyramine use is not recommended as they may interfere with the absorption of anti-retroviral drugs.
8.12. COVID-19
-
•
Dyslipidaemia has been linked with increased severity of COVID-19 infection.
-
•
Statins are generally safe for COVID-19 patients and may offer additional benefits owing to pleiotropic effects.
-
•
Statins should be continued during acute COVID-19 infection, particularly in patients with manifest ASCVD or dyslipidemia.
9. Specific phenotypes
9.1. Dyslipidemia in the elderly
-
•
Cardiovascular disease (CVD) is a leading cause of morbidity and mortality in elderly, defined here as age ≥70 years.
-
•
Initiation of drug therapy for dyslipidemia for primary prevention in the elderly should be individualized considering co-morbidities, drug interactions and patient preferences.
-
•
All elderly patients must be counselled for lifestyle measures and medication adherence.
-
•
Statin use as primary prevention for the elderly is supported by meta-analysis and statins are recommended in elderly with high risk of CVD or CAD.
-
•
Statins should be started at a low dose with monitoring for adverse effects. The dose should be titrated to achieve LDL cholesterol goals (Table 1).
-
•
Among very elderly (>80 years) there is inadequate evidence for drug treatment of dyslipidemia for primary prevention and clinical judgment and patient preferences should guide decisions.
-
•
In the elderly, statins have been found to reduce CAD risk and mortality in secondary prevention, the goals for LDL cholesterol are similar to the non-elderly (Table 1).
-
•
In the elderly with high and very high CAD risk, the addition of ezetimibe is likely to be beneficial.
-
•
Evolocumab is safe and effective in the elderly and could be an alternative in high and very high CAD risk.
9.2. Dyslipidemia in the young
-
•
Myocardial infarction (MI), and sudden cardiac deaths in young adults (<40 years) are common in India. Dyslipidaemia and tobacco are one of the primary drivers.
-
•
All individuals should have their lipid profile evaluated by the age of 18. Screening may be of particular benefit in identifying young adults with elevated LDL cholesterol due to unrecognized HeFH. Young adults (18–40 yrs) having ASCVD should be on intensive lipid-lowering therapy to keep LDL-C below 55 mg/dl.
-
•
If a young adult has LDL cholesterol of ≥190 mg/dl on repeated evaluation, statin therapy should be initiated.
-
•
Young adults with hypertension and diabetes should receive mild to moderate-intensity statin therapy to achieve the LDL-C goal (Table 2).
-
•
Additionally, all individuals should be advised to lead a healthy lifestyle, increase physical activity, adhere to dietary restrictions and refrain from smoking and tobacco use.
-
•
Young adults who are carrier of HeFH gene should be on healthy lifestyle and small to moderate dose of statin.
-
•
Managing hypertriglyceridemia in young adults is similar to the middle-aged adults.
9.3. Pediatric hyperlipidemia
-
•
Identifying dyslipidemia in childhood is an opportunity for preventing adult CAD.
-
•
Encouraging a healthy lifestyle with high levels of physical activity, tobacco avoidance, and intake of a healthy diet is necessary.
-
•
Secondary dyslipidemia due to drugs, metabolic, renal, and hepatic causes should be excluded.
-
•
Dyslipidemia due to genetic defects in lipid metabolism should also be considered.
-
•
US National Institutes of Health (NIH) recommends selective screening of children 2–9 years (positive family history, high body mass index or CVD risk factors) and universal screening for children aged 9–11 years.
-
•
In children, drug therapy is indicated only with very high LDL cholesterol levels or in children with risk factors following failure of lifestyle changes.
-
•
Pharmacotherapy is best avoided in children less than 10 years of age except in the presence of severe primary hyperlipidaemia or multiple risk factors.
-
•
Statins and fibrates, respectively, are first-line drugs for hypercholesterolemia and hypertriglyceridemia. Monitoring of liver functions, creatine kinase, and lipid profile should be performed following 1 month of therapy and every 3–6 months thereafter.
-
•
Ezetimibe can be given to children above the age of 10 years.
-
•
A phase-4 study in India, that included children 12–18 years reported that PCSK9 inhibitor-evolocumab was safe and well tolerated.
10. Genetic dyslipidemia
10.1. Familial hypercholesterolemia
-
•
Familial hypercholesterolemia (FH) is caused by genetic defects in LDL cholesterol pathways, common are defects in LDLR, PCSK9, and Apo B genes). It is associated with elevated LDL cholesterol and a risk of premature CAD.
-
•
Studies have reported an FH prevalence of 15–20 % in premature CAD in India. Population prevalence varies from 100 to 300/100,000 in small epidemiological studies. FH is more common in younger patients with higher LDL levels and with lower incidence of other risk factors such as diabetes, hypertension, and smoking.
-
•
Dutch Lipid Clinic Network (DLCN) criteria are simple clinical tools for FH diagnosis. DLCN is based on a scoring system. A score >8 suggests definite HF, a while score 6–8 is probable FH. DLCN criteria could also be used after applying correction factors in patients already on statins. Genetic testing is confirmatory.
-
•
Homozygous FH is very rare with a prevalence of 1/500,000 to 1,000,000, CAD manifests in the first or second decade of life.
-
•
Statins are used to treat adult FHeH with a LDL cholesterol goal of <70 mg/dl for primary prevention and <55 mg/dl for secondary prevention. High-intensity statin with ezetimibe is recommended as initial therapy. If targets are not achieved, other non-statin drugs (bempedoic acid, PCSK9 inhibitors, inclisiran) should be considered (Fig. 7).
-
•
Cascade screening of family members is recommended following diagnosis of FH in an individual. HeFH detected children should be managed with statins to achieve an LDL cholesterol target of <130 mg/dl.
-
•
Patients with HoFH high LDL cholesterol >500 mg/dl and require combination therapy with high-intensity statins, ezetimibe, and PCSK9 inhibitors. Mipomersen, lomitapide, and plasmapheresis are approved for HoFH treatment.
Fig. 7.
Familial hypercholesterolemia diagnosis and management.
10.2. Elevated Lipoprotein (a)
-
•
Lp(a) is inherited, independent and causal risk factor for CAD and other ASCVD. Epidemiological, genome-wide association and mendelian randomization studies have demonstrated an association between increased Lp(a) levels incidence of myocardial Infarction, aortic stenosis, ischemic stroke, heart failure, and cardiovascular and all-cause deaths.
-
•
The Lp(a)-mediated CVD risk is mediated by pro-inflammatory, pro-thrombotic, and pro-atherogenic processes.
-
•
Elevated Lp(a) is not uncommon and 1 in 5 individuals worldwide have elevated Lp(a) (>50 mg/dl or >125 nmol/L). In South Asians, the prevalence is 1 in 4.
-
•
Elevated Lp(a) is genetically determined, not influenced by diet and exercise, and remains stable over time. The levels may increase in thyroid diseases, CKD, inflammation, and sepsis. It also increases in pregnancy and menopause. It should be measured at least once in a lifetime.
-
•
An Indian study reported association of Lp(a) > 50 mg/dl with severe angiographic CAD. Elevated Lp(a) in 43 % of FHeH patients and higher levels in young CAD patients compared to the elderly.
-
•
Cascade testing for Lp(a) is recommended in settings of FH, family history of CAD and high Lp(a) and in premature CAD.
-
•
Presently there are no approved therapies but many are in pipeline. Comprehensive lifestyle and aggressive risk factor control is recommended. PCSK9 inhibitor and Inclisiran reduces Lp(a) by 25 % but are not recommended therapies.
-
•
Novel antisense oligonucleotide and small interfering RNA treatments that target apo(a) in hepatocytes reduce Lp(a). Some drugs being evaluated for outcomes are pelacarsen, olpasiran, and other antisense oligonucleotides.
11. Apolipoprotein B: an ideal biomarker
-
•
Apolipoprotein B (ApoB) is a critical structural component of atherogenic lipoproteins. A single ApoB molecule is present in every particle of VLDL, IDL, LDL, and Lp(a) but not in HDL cholesterol.
-
•
Plasma ApoB concentration is a direct measure of circulating atherogenic lipoproteins and can be measured more accurately than LDL particles.
-
•
Several large epidemiological studies indicate that apolipoproteins (Apo-B and Apo-A1) are better predictors of ASCVD than total cholesterol, LDL cholesterol, and non-HDL cholesterol.
-
•
Genetic studies showed that high levels of Apo-B correspond to high levels of LDL-C and non-HDL-C and are associated with an increased risk of CVD.
-
•
Further, genetic studies suggest that some Apo B (& LDL-C) elevations are caused by mutations in the APOB gene, which causes it to produce Apo B that is not as easily recognised by LDL receptors. These genetic changes impede LDL-C clearance from the blood, resulting in LDL cholesterol accumulation in plasma increasing the risk of heart disease.
-
•
Currently most international and Indian guidelines on dyslipidaemia management recommends Apo B for testing in case of familial hypercholesterolemia and to estimate the ASCVD risk in the younger population reliably.
-
•
The European Society of Cardiology 2019 guidelines emphasized that Apo-B is the preferred measurement to estimate ASCVD risk because Apo-B provides an accurate estimate of the total concentration of atherogenic particles under all circumstances.
-
•
Though, limited data exists comparing Apo B and very low LDL-C in the Indian population, given that we have one Apo B particle per VLDL-C and LDL-C including triglycerides and cholesterol, it is highly atherogenic.
-
•
Hence, Apo B potentially could be a better biomarker in predicting CHD as well as in secondary prevention of ASCVD.
-
•
Replacing the conventional lipid panel with Apo B could simultaneously simplify and improve clinical care for patients at high risk of ASCVD as Apo B is a single atherogenic lipid marker present in all lipids sub-fractions except HDL-C, and thus, Apo B integrates and extends the information from triglycerides and cholesterol.
-
•
However, we need longitudinal data and standardization to boldly replace LDL-C or non-HDL-C with Apo B (See Table 5).
Table 5.
Atherogenic lipoproteins and their targets.
| Atherogenic lipoproteins | Target |
|---|---|
| Apo B | <65 mg/dl: very high risk |
| <80 mg/dl: high risk | |
| <100 mg/dl: moderate CV risk | |
| non-HDL-C | <85 mg/dl: Very high risk |
| <100 mg/dl: High risk | |
| <130 mg/dl: Moderate risk |
12. Non-adherence and strategies to improve adherence
-
•
The significance of lipid-lowering, particularly through statin therapy, in preventing cardiovascular events is well-established, but its use in clinical practice is suboptimal, with poor long-term adherence.
-
•
Common reasons for declining or discontinuing therapy are costs, fear of actual or perceived side effects, and conflicting opinions regarding the risk-benefit ratio.
-
•
Statins can cause muscle pains while non-statins can cause gastrointestinal side effects, injection site reaction, influenza-like symptoms, and nasopharyngitis.
-
•
Adherence rates are particularly low for statin therapy for primary prevention.
-
•
Factors such as polypharmacy, lack of understanding, misconceptions, and media coverage affect adherence. Addressing these factors and better patient education and empowerment are crucial to improve the adherence to lipid-lowering therapies.
-
•
Use of technology and artificial intelligence-guided therapy-adherence prompts, and patient education and empowerment can significantly improve adherence.
13. Conclusions
Lipid management is crucial for ASCVD prevention and management. Dyslipidemias are widely prevalent in the general population and CAD patients. There is humongous evidence that lowering LDL cholesterol using statins and other non-statin drugs can reduce the incidence of primary CAD events, and also prevent recurrent events in established ASCVD patients. The Cardiological Society Clinical Practice Guidelines for dyslipidemia management has focused on common drugs available in India and their evidence-guided and expert-opinion for better management.
This guideline has uniquely discussed lipid management in specific co-morbidities and patient phenotypes.These issues are especially relevant in India. Adherence to lifelong therapy is a challenge and we believe that better health literacy, financial support, and the use of algorithm-based therapies can improve initiation and continuation.
Footnotes
From: Cardiological Society of India Expert Group, Indian Heart House, Kolkata, India.
Contributor Information
Jitendra PS. Sawhney, Email: jpssawhney@yahoo.com.
Sivasubramanian Ramakrishnan, Email: ramaaiims@gmail.com.
Kushal Madan, Email: kushalmadan@gmail.com.
Saumitra Ray, Email: drsaumitra@yahoo.co.in.
P Balagopalan Jayagopal, Email: jaigopallakshmi@gmail.com.
Dorairaj Prabhakaran, Email: dprabhakaran@ccdcindia.org.
Tiny Nair, Email: tinynair@gmail.com.
Geevar Zachariah, Email: geevarzachariah@gmail.com.
Peeyush Jain, Email: dpn2005@gmail.com.
Jamshed Dalal, Email: jjdalal@hotmail.com.
Sitaraman Radhakrishnan, Email: Samurai43@yahoo.com.
Arun Chopra, Email: akchopra1@rediffmail.com.
Sanjay Kalra, Email: brideknl@gmail.com.
Ashwani Mehta, Email: drashwanimehta@gmail.com.
Arvind K. Pancholia, Email: drpancholia@gmail.com.
Nitin K. Kabra, Email: nitink99@yahoo.com.
Dhiman Kahali, Email: dhiman.kahali@gmail.com.
Tapan Ghose, Email: ghosetapan@gmail.com.
Satyavir Yadav, Email: drsatyaviryadav87@gmail.com.
Prafulla Kerkar, Email: prafullakerkar@gmail.com.
Ajay Yadav, Email: Ajay.vascular@gmail.com.
Debabrata Roy, Email: debroy67@ymail.com.
Mrinal Kanti Das, Email: drmkdas2001@yahoo.co.in.
Vijay H. Bang, Email: shivvhb@yahoo.com.
Pratap Chandra Rath, Email: drpcrath@hotmail.com.
Dhurjati Prasad Sinha, Email: drdpsinha@gmail.com.
P.S. Banerjee, Email: drpartha76@gmail.com.
Rakesh Yadav, Email: Rakeshyadav123@yahoo.com.
Rajeev Gupta, Email: rajeevgg@gmail.com.