Abstract
Introduction
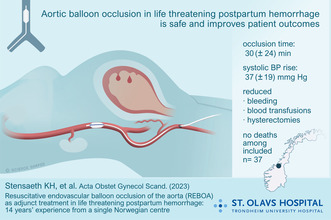
Postpartum hemorrhage (PPH) remains a global health problem. The introduction of resuscitative endovascular balloon occlusion of the aorta (REBOA) in 2008 sought to enhance the management of hemorrhagic shock during PPH. In this study, we present a single Norwegian center's experience with REBOA as a supportive treatment in combating life threatening PPH.
Material and methods
This is a historical cohort study from St Olav's University Hospital, with data from period 2008–2021. It includes all patients who underwent REBOA as an adjunct treatment due to life threatening PPH, analyzing the outcomes and trends over a 14‐year period.
Results
A total of 37 patients received REBOA as an adjunct treatment. All procedures were technically successful, achieving hemodynamic stability with an immediate average increase in systolic blood pressure of 36 ± 22 mmHg upon initial balloon inflation. Additionally, a downward trend was noted in the frequency of hysterectomies and the volume of blood transfusions required over time. No thromboembolic complications were observed.
Conclusions
Our 14 years of experience at St Olav's Hospital suggests that REBOA serves as a safe and effective adjunct interventional technique for managing life‐threatening PPH. Furthermore, the findings indicate that incorporating a multidisciplinary approach to enable rapid aortic occlusion can potentially reduce the necessity for blood transfusions and hysterectomies.
Keywords: balloon catheter, blood transfusions, hysterectomies, mortality, postpartum hemorrhage
A total of 14 years of experience at St Olav's Hospital suggests that REBOA serves as a safe and effective adjunct interventional technique for managing life‐threatening postpartum hemorrhage. Furthermore, the findings indicate that incorporating a multidisciplinary approach to enable rapid aortic occlusion can potentially reduce the necessity for blood transfusions and hysterectomies.
Abbreviations
- PPH
postpartum hemorrhage
- REBOA
resuscitative endovascular balloon occlusion of the aorta
- SBP
systolic blood pressure
Key message.
Resuscitative endovascular balloon occlusion of the aorta is a safe adjunct interventional technique for managing life‐threatening postpartum hemorrhage and may preserve the reproductive function of the patient.
1. INTRODUCTION
Postpartum hemorrhage (PPH) remains a significant global health issue, accounting for up to 27% of maternal deaths worldwide, 1 , 2 and with increasing prevalence in high‐income countries. 3 , 4 Traditional medical approaches, including uterotonic medications and blood product transfusions, combined with surgical interventions, may be insufficient as hemorrhage control or preventing the necessity of a hysterectomy. Notably, early recognition and prompt treatment could potentially prevent about two‐thirds of all maternal deaths resulting from hemorrhage. 5 , 6
Resuscitative endovascular balloon occlusion of the aorta (REBOA) is currently utilized as an auxiliary treatment in cases of noncompressible traumatic hemorrhage. 7 In several case series, REBOA has demonstrated a substantial reduction in blood loss and enhancement of hemodynamic stability in PPH patients. 8 , 9 The inception of REBOA in the management of life threatening PPH, normally defined as a loss of 40% of the blood volume, took place at St Olav's Hospital in 2008, envisioned as a minimally invasive adjunct treatment that may preserve the uterus. Our initial experience with REBOA in managing life threatening PPH in 2012, 8 demonstrated promising outcomes. This was followed by a case series of 36 patients in 2017; 9 however, these initial data were part of a multicenter study. In addition, REBOA is increasingly used for placenta accreta spectrum disorders, 10 which also includes our institution. Recently a large observational study from Japan was published, 11 in addition to several previous case reports. 12 , 13 In 2017, Nyfløt et al. observed that the frequency of severe PPH (defined as blood loss ≥1500 mL) was 2.5% in three Norwegian University Hospitals, 14 the most common etiologies were uterine atony (60%) and placental complications (36%). Also, the women with a history of severe PPH were at highest risk of PPH.
Given the advancements in endovascular techniques, we posit that REBOA could play a pivotal role in addressing life‐threatening PPH. Therefore, this study seeks to delineate our 14‐year experience with utilizing REBOA in managing these patients, and potentially paving the way for more widespread adoption in clinical settings.
2. MATERIAL AND METHODS
The study entails an analysis of a historical cohort using data from St Olav's University Hospital in Trondheim, Norway. The research aligns with the STROBE (Strengthening the reporting of observational studies in epidemiology) guidelines for observational cohort studies. 15 St Olav's Hospital have had an annual rate of deliveries between 3500 and 3900 deliveries in the recent 5 years.
2.1. Patients and study design
We included patients who were administered REBOA as an adjunctive treatment during life‐threatening PPH at St. Olav's University Hospital, spanning from 2008 to 2021. The data set includes cases of PPH succeeding both vaginal and cesarean deliveries without categorizing them based on the delivery mode. Patient demographics and clinical data were obtained from the electronic patient medical records, PICIS Anin©. Invasive systolic blood pressure (SBP) was measured in the patients' radial artery, recording the lowest SBP within a 5‐min interval before aortic occlusion and the highest SBP within 5 min post‐occlusion. Thromboembolic complications were identified based on clinical significance and documented in the patients' medical journals, necessitating therapeutic interventions.
2.2. Endovascular equipment
From 2008 to 2015, various semi‐compliant balloons (NuMED Canada Inc) ranging from 15 to 25 mm were utilized, paired with 23 cm long 6 or 8 Fr introducers (Cordis Corporation). Out of these, an 8 Fr introducer and a 20‐ or 25‐mm balloon were used in 10 patients. Subsequently, from 2016, the standard procedure involved the usage of 6 Fr introducers and 15 mm balloons (Reboa Medical).
2.3. Intervention
PPH is an obstetric emergency that can be managed by a variety of potentially effective medical and surgical interventions. The REBOA procedure was sanctioned for patients clinically assessed as hemodynamically unstable due to life threatening PPH. The decision was jointly made by the gynecologist and the anesthesiologist, primarily following failed attempts to stabilize the patient using a multimodal approach including uterotonics (oxytocin, Methyl‐Ergometrine, Carboprost), uterine balloons, and curettage. The REBOA procedure was performed by the on‐call interventional radiologist, which had a physical response time of less than 30 min. All procedures were executed in the operating room, acquiring common femoral arterial access using standard Seldinger technique without fluoroscopy, but guided by ultrasound. The introducer and side port were flushed with saline as standard procedure. Then the balloon catheter was inserted via the introducer over the guidewire approximately 30 cm into the abdominal aorta. This results in aortic zone III occlusion for most patients. 16 The balloon was inflated using 8 mL of isotonic saline for a 15 mm balloon. The standard operating procedure at our hospital is intermittent balloon occlusion, hence the balloon was deflated every 10–15 min for 1 min, and then reinflated if the bleeding or hemodynamic instability reappeared. However, final deflation of the balloon was not performed before hemostasis was complete.
2.4. Statistical analyses
Data from all the included patients were analyzed using descriptive statistics. The variables are shown as number, percentages, mean values (accompanied by standard deviations), and median values (with interquartile range). The study refrained from performing comparative statistical analyses.
3. RESULTS
Throughout the span of this study, a total of 37 patients were incorporated, distributed over two separate periods: 13 patients from 2008 to 2015 and 24 patients from 2016 to 2021. Multicenter data from the initial period (2008–2015) has been documented in a prior publication. 9 All the REBOA procedures were successfully executed within the operating room environment, with no instances of unsuccessful procedures reported. The demographic details of the patients and other pertinent clinical data are systematically documented in Table 1.
TABLE 1.
Patient demographics and interventions.
| 2008–2021 (N = 37) | 2008–2015 (N = 13) | 2016–2021 (N = 24) | |
|---|---|---|---|
| Age (years; mean ± SD) | 31.4 ± 6.0 | 32.4 ± 7.1 | 30.8 ± 5.3 |
| SBP before inflation (mmHg; mean ± SD) | 76 ± 20 | 71 ± 9 | 78 ± 23 |
| SBP after inflation (mmHg; mean ± SD) | 113 ± 23 | 108 ± 13 | 115 ± 27 |
| SBP increase (mmHg; mean ± SD) | 37 ± 19 | 38 ± 16 | 37 ± 20 |
| Total bleeding (mL; mean ± SD) | 4399 ± 2836 | 6390 ± 3681 | 3447 ± 1725 |
| Balloon deflations (median [IQR]) | 1 (1–2) | 2 (1–2) | 1 (1–2) |
| Aortic occlusion duration (minutes; mean ± SD) | 30 ± 24 | 38 ± 27 | 23 ± 19 |
| Interventions (n [%]) | |||
| Hysterectomy | 9 (24.3) | 6 (46.2) | 3 (12.5) |
| Curettage | 22 (59.5) | 10 (76.9) | 12 (50.0) |
| Uterine balloon | 22 (59.5) | 6 (46.2) | 16 (66.7) |
| Uterine artery embolization | 3 (8.1) | 2 (15.4) | 1 (4.2) |
| Transfusions (mean ± SD) | |||
| PRBC (mL) | 2125 ± 1778 | 3523 ± 2463 | 1457 ± 733 |
| Plasma (mL) | 1194 ± 1014 | 1956 ± 1396 | 896 ± 641 |
| Thrombocytes (mL) | 664 ± 1606 | 1805 ± 2795 | 217 ± 230 |
Abbreviations: IQR, interquartile range; PRBC, packed red blood cells; SBP, systolic blood pressure; SD, standard deviation.
3.1. Clinical outcomes and observations
During the 14‐year study period, 59.5% of the patients underwent treatment with a uterine balloon as well as received curettage prior to aortic occlusion. All patients experienced an immediate mean rise in SBP (37 ± 19 mmHg) following the initial aortic occlusion. One patient suffered hemodynamic collapse in the operating room prior to aortic occlusion but was successfully resuscitated through cardiopulmonary resuscitation. Three patients were treated with uterine artery embolization (8.1%) and nine hysterectomies were performed (24.3%) through the 14‐year period. In the earlier period, one patient experienced an aortic rupture, as documented in a previous publication. 8
Thromboembolic complications were of special concern and assessed on the basis of clinical status and outcome. In our previous publication, 9 iliac artery thrombus formation was associated with a short (11 cm) introducer length; however, in the current study, only long (23 cm) introducers were used, and no instances of thrombus formation were noted in the iliac or femoral artery that necessitated anticoagulant or surgical treatment. Neither was any additional procedures required for limb salvage. The introducer was in situ for a mean of 10 ± 6 h. The common femoral artery was sealed with a 6 or 8 Fr Angio‐Seal closure device (Terumo) and no large hematoma was noted. The survival rate until discharge stood at 100% for all included patients, and follow‐up was based on clinical status.
Over the 14‐year timeframe, we documented a decline in total blood loss, volumes of transfused packed red blood cells, plasma, and thrombocytes. Furthermore, a diminishing trend was also observed in the percentage of hysterectomy procedures undertaken amongst the participating patients (as detailed in Table 1).
4. DISCUSSION
This study delineates a 14‐year experience at a single Norwegian center in utilizing REBOA in treating life‐threatening PPH. A major observation is the noticeable decrease in transfusion rates, overall bleeding, and the number of hysterectomies over time, without observing a surge in REBOA‐associated complications. These findings, therefore, reinforce existing literature suggesting the safety of REBOA when administered by competent healthcare providers.
It is surmised that the earlier intervention with REBOA during hemorrhagic episodes is a critical factor underpinning the observed declines in blood transfusions and hysterectomy procedures, albeit the precise causes weren't the central focus of this study. Moreover, the team's increasing familiarity and expertise with the procedure over the years, as well as calling in the interventional radiologist earlier over time, likely played a role in shortening the time to aortic occlusion, consequently impacting the rate reductions positively. The intricacies of the procedure necessitate execution by clinicians known to arterial access. While interventional radiologists (IR) are typically familiar with this technique, facilities lacking IR services can engage other specialists trained in the Seldinger technique to form an adept team for REBOA administration. This also points to the importance of meticulous documentation of every phase of the procedure is a necessary step to enhance institutional quality. It is also interesting to note a rise in the application of uterine balloon across the two study periods, which in conjunction with uterotonics and a greater focus on the administration of hemostatic agents, might have established a significant synergistic hemostatic effect.
PPH is one of the leading causes of maternal mortality and morbidity worldwide. 1 Therefore, any intervention that can potentially mitigate the adverse outcomes associated with PPH is of utmost importance. Some studies suggest that deaths associated with PPH could be prevented with prompt recognition and adequate treatment. 17 , 18 However, in settings where surgical services and blood products are readily available, a difference in survival may be difficult to demonstrate. 19 The incidence of emergency peripartum hysterectomy is increasing, 20 and even if hysterectomy is an effective treatment, it may be considered catastrophic for fertile women. REBOA has been overlooked as a treatment option in both a Cochrane database review, 21 and a recent review in the New England Journal of Medicine. 22 This study, therefore, fills an important gap by highlighting the possible benefits of REBOA in lowering the usage of blood products and reducing hysterectomy rates, outcomes that are critically important, especially in resource‐limited settings.
Kamijo et al. reported a mortality rate of 7% in their severe PPH cohort, 11 but the time from delivery to aortic occlusion was quite long (24 h). Nevertheless, the authors argue that REBOA, and the uterine artery embolization procedures, may have avoided unnecessary hysterectomies. However, the embolization procedures are mainly performed in hemodynamic stable patients, which emphasizes the life‐threatening condition of our patients, where only a few uterine artery embolization procedures were carried out.
Despite the promising results, it is pertinent to be cautious, as REBOA is not devoid of complications, necessitating a judicious approach to its implementation. It is reassuring to note the low complication rates in our study, potentially attributed to both appropriate training and development of new devices with an enhanced safety profile. 23 Previous studies in trauma patients report complications such as lower limb ischemia; however, large introducers (10 Fr or more) were used, 24 , 25 in contrast to our study with mainly 6 Fr introducers. In addition, an immediate balloon retraction was performed after hemorrhage control. It is also reasonable to believe that a combination of a short aortic occlusion time, which was further reduced over time, and repetitive short balloon deflations, probably will facilitate a minimum of thromboembolic and ischemic complications in nonheparinized patients. Also, a recently released 4 Fr balloon catheter (Frontline Medical Technologies Inc) might further increase the safety profile.
Our study had several limitations, chiefly the constrained generalizability due to its single‐center design and the relatively low patient number, being a nascent procedure. Furthermore, the historical nature of the study establishes potential limitations, especially when it comes to the establishment of causality. The inconsistent recording of time to balloon inflation further adds to these limitations. Coagulation assessments such as thromboelastography (TEG) and rotational thromboelastometry (ROTEM) are lacking, also data from a number of postoperative complications, including postoperative ileus and length of stay in the intensive care unit. These data were not registered in this historical cohort study; however, we admit that these are important data to collect in a future prospective study. Lastly, the decision on when to apply this method was based on a joint clinical decision by the treatment team and not by definite trigger criteria. Development of such criteria and future endeavors might aim to address these limitations, perhaps with multicenter collaborations and prospective study designs. Strengths of the study includes a well‐regarded Norwegian maternity care, and a healthcare system that offers equal care to all.
5. CONCLUSION
Our 14 years of experience at St Olav's Hospital indicate that REBOA in life threatening PPH can be performed safely with a high degree of technical success and contribute to hemodynamic stability. The outcomes seem to strongly advocate for the role of a well‐coordinated multidisciplinary approach in achieving rapid aortic occlusion, potentially leading to reduced blood transfusions and hysterectomy numbers.
AUTHOR CONTRIBUTIONS
Knut Haakon Stensæth: Conceived and designed the analysis, collected the data, contributed data or analysis tools, performed the analysis, wrote the manuscript. Edmund Søvik: Conceived and designed the analysis, collected the data, contributed data or analysis tools, wrote the manuscript. Marte Irene Skille Carlsen: Collected the data, contributed data or analysis tools, performed the analysis, wrote the manuscript. Tone Shetelig Løvvik, Oddvar Uleberg, Jostein Rødseth Brede: Contributed data or analysis tools, performed the analysis, wrote the manuscript.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflicts of interest.
ETHICS STATEMENT
The study was approved by the Regional Ethics Committee (reference no. 351477, South‐East C, Norway) on November 22, 2021. The Ethics Committee granted exemption from the requirement for active consent, hence written information about the study was provided to all patients, and passive informed consent obtained. One patient opted not to participate in the study.
Stensæth KH, Carlsen MIS, Løvvik TS, Uleberg O, Brede JR, Søvik E. Resuscitative endovascular balloon occlusion of the aorta (REBOA) as adjunct treatment in life threatening postpartum hemorrhage: Fourteen years' experience from a single Norwegian center. Acta Obstet Gynecol Scand. 2024;103:965‐969. doi: 10.1111/aogs.14767
REFERENCES
- 1. Gallos I, Devall A, Martin J, et al. Randomized trial of early detection and treatment of postpartum hemorrhage. N Engl J Med. 2023;389:11‐21. [DOI] [PubMed] [Google Scholar]
- 2. Say L, Chou D, Gemmill A, et al. Global causes of maternal death: a WHO systematic analysis. Lancet Glob Health. 2014;2:e323‐e333. [DOI] [PubMed] [Google Scholar]
- 3. Knight M, Callaghan WM, Berg C, et al. Trends in postpartum hemorrhage in high resource countries: a review and recommendations from the International Postpartum Hemorrhage Collaborative Group. BMC Pregnancy Childbirth. 2009;9:55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Rossen J, Okland I, Nilsen OB, Eggebø TM. Is there an increase of postpartum hemorrhage, and is severe hemorrhage associated with more frequent use of obstetric interventions? Acta Obstet Gynecol Scand. 2010;89:1248‐1255. [DOI] [PubMed] [Google Scholar]
- 5. Sakse A, Weber T, Nickelsen C, Secher NJ. Peripartum hysterectomy in Denmark 1995–2004. Acta Obstet Gynecol Scand. 2007;86:1472‐1475. [DOI] [PubMed] [Google Scholar]
- 6. Pettersen S, Falk RS, Vangen S, Nyfløt LT. Peripartum hysterectomy due to severe postpartum hemorrhage: a hospital‐based study. Acta Obstet Gynecol Scand. 2022;101:819‐826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Brenner M, Bulger EM, Perina DG, et al. Joint statement from the American College of Surgeons Committee on Trauma (ACS COT) and the American College of Emergency Physicians (ACEP) regarding the clinical use of Resuscitative Endovascular Balloon Occlusion of the Aorta (REBOA). Trauma Surg Acute Care Open. 2018;3:e000154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Søvik E, Stokkeland P, Storm BS, Åsheim P, Bolås O. The use of aortic occlusion balloon catheter without fluoroscopy for life‐threatening post‐partum haemorrhage. Acta Anaesthesiol Scand. 2012;56:388‐393. [DOI] [PubMed] [Google Scholar]
- 9. Stensaeth KH, Sovik E, Haig INY, Skomedal E, Jorgensen A. Fluoroscopy‐free resuscitative endovascular balloon occlusion of the aorta (REBOA) for controlling life threatening postpartum hemorrhage. PLoS One. 2017;12:e0174520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Peng W, Shen L, Wang S, Wang H. Retrospective analysis of 586 cases of placenta previa and accreta. J Obstet Gynaecol J Inst Obstet Gynaecol. 2020;40:609‐613. [DOI] [PubMed] [Google Scholar]
- 11. Kamijo K, Nakajima M, Shigemi D, et al. Resuscitative endovascular balloon occlusion of the aorta for life‐threatening postpartum hemorrhage: a nationwide observational study in Japan. J Trauma Acute Care Surg. 2022;93:418‐423. [DOI] [PubMed] [Google Scholar]
- 12. Masamoto H, Uehara H, Gibo M, Okubo E, Sakumoto K, Aoki Y. Elective use of aortic balloon occlusion in cesarean hysterectomy for placenta previa percreta. Gynecol Obstet Invest. 2009;67:92‐95. [DOI] [PubMed] [Google Scholar]
- 13. Ji SM, Cho C, Choi G, et al. Successful management of uncontrolled postpartum hemorrhage due to morbidly adherent placenta with Resuscitative endovascular balloon occlusion of the aorta during emergency cesarean section—a case report. Anesth Pain Med. 2020;15:314‐318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Nyfløt LT, Sandven I, Stray‐Pedersen B, et al. Risk factors for severe postpartum hemorrhage: a case‐control study. BMC Pregnancy Childbirth 2017;17:17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. von Elm E, Altman DG, Egger M, Pocock SJ, Gøtszsche PC, Vandenbroucke JP. The strengthening of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Bull World Health Organ. 2007;85:867‐872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Stannard A, Eliason JL, Rasmussen TE. Resuscitative endovascular balloon occlusion of the aorta (REBOA) as an adjunct for hemorrhagic shock. J Trauma. 2011;71:1869‐1872. [DOI] [PubMed] [Google Scholar]
- 17. Berg CJ, Harper MA, Atkinson SM, et al. Preventability of pregnancy‐related deaths: results of a state‐wide review. Obstet Gynecol. 2005;106:1228‐1234. [DOI] [PubMed] [Google Scholar]
- 18. Della Torre M, Kilpatrick SJ, Hibbard JU, et al. Assessing preventability for obstetric hemorrhage. Am J Perinatol. 2011;28:753‐760. [DOI] [PubMed] [Google Scholar]
- 19. Brede JR, Søvik E, Rehn M. Resuscitative endovascular balloon occlusion of the aorta: the postpartum haemorrhage perspective. Crit Care. 2022;26:57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. de la Cruz CZ, Thompson EL, O'Rourke K, Nembhard WN. Cesarean section and the risk of emergency peripartum hysterectomy in high‐income countries: a systematic review. Arch Gynecol Obstet. 2015;292:1201‐1215. [DOI] [PubMed] [Google Scholar]
- 21. Kellie FJ, Wandabwa JN, Mousa HA, Weeks AD. Mechanical and surgical interventions for treating primary postpartum haemorrhage. Cochrane Database Syst Rev. 2020;7:CD013663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Bienstock JL, Eke AC, Hueppchen NA. Postpartum hemorrhage. N Engl J Med. 2021;384:1635‐1645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Teeter WA, Matsumoto J, Idoguchi K, et al. Smaller introducer sheaths for REBOA may be associated with fewer complications. J Trauma Acute Care Surg. 2016;81:1039‐1045. [DOI] [PubMed] [Google Scholar]
- 24. Brenner ML, Moore LJ, DuBose JJ, et al. A clinical series of resuscitative endovascular balloon occlusion of the aorta for hemorrhage control and resuscitation. J Trauma Acute Care Surg. 2013;75:506‐511. [DOI] [PubMed] [Google Scholar]
- 25. Saito N, Matsumoto H, Yagi T, et al. Evaluation of the safety and feasibility of resuscitative endovascular balloon occlusion of the aorta. J Trauma Acute Care Surg. 2015;78:897‐904. [DOI] [PubMed] [Google Scholar]


