Abstract
Background:
Social determinants of health (SDoH) have significant implications for health outcomes in the United States. Emergency departments (EDs) function as the safety nets of the American health care system, caring for many vulnerable populations. ED-based interventions to assess social risk and mitigate social needs have been reported in the literature. However, the breadth and scope of these interventions have not been evaluated. As the field of social emergency medicine (SEM) expands, a mapping and categorization of previous interventions may help shape future research. We sought to identify, summarize, and characterize ED-based interventions aimed at mitigating negative SDoH.
Methods:
We conducted a scoping review to identify and characterize peer-reviewed research articles that report ED-based interventions to address or impact SDoH in the United States. We designed and conducted a search in Medline, CINAHL, and Cochrane CENTRAL databases. Abstracts and, subsequently, full articles were reviewed independently by two reviewers to identify potentially relevant articles. Included articles were categorized by type of intervention and primary SDoH domain. Reported outcomes were also categorized by type and efficacy.
Results:
A total of 10,856 abstracts were identified and reviewed, and 596 potentially relevant studies were identified. Full article review identified 135 articles for inclusion. These articles were further subdivided into three intervention types: a) provider educational intervention (18%), b) disease modification with SDoH focus (26%), and c) direct SDoH intervention (60%), with 4% including two "types." Articles were subsequently further grouped into seven SDoH domains: 1) access to care (33%), 2) discrimination/group disparities (7%), 3) exposure to violence/crime (34%), 4) food insecurity (2%), 5) housing issues/homelessness (3%), 6) language/literacy/health literacy (12%), 7) socioeconomic disparities/poverty (10%). The majority of articles reported that the intervention studied was effective for the primary outcome identified (78%).
Conclusion:
Emergency department-based interventions that address seven different SDoH domains have been reported in the peer-reviewed literature over the past 30 years, utilizing a variety of approaches including provider education and direct and indirect focus on social risk and need. Characterization and understanding of previous interventions may help identify opportunities for future interventions as well as guide a SEM research agenda.
INTRODUCTION
The emergency department (ED) provides evaluation and treatment regardless of patients’ social or financial background.1, 2 To this end, millions of Americans impacted by social risks and social needs rely on the ED for both routine and urgent medical care.3, 4 As a result, the ED has been described as a “window into the community” through which emergency medicine (EM) providers regularly witness the healthcare disparities associated with adverse social determinants of health (SDoH).5 Defined by the Centers for Disease Control and Prevention (CDC) as the “conditions in the environments in which people are born, live, learn, work, play, worship, and age that affect a wide range of health, functioning, and quality of life outcomes and risks,” SDoH have effects on individuals’ quality of life, morbidity, and life expectancy.6, 7 SDoH encompass social risks, conditions that put an individual at higher risk for poor health, such as poverty, as well as social needs, the actual needs recognized by an individual at a given time, such as lack of housing.8, 9
Social emergency medicine (SEM) has been described as a concerted effort to counter the impact of negative SDoH by expanding the role of EM to also “diagnose and treat … social determinants of health,” rather than focusing solely on a biologic model of health.4, 10 Even prior to the recent coining of “SEM,” however, ED-based educational curricula, screening programs, outreach programs, and collaborations have been developed and evaluated in attempts to mitigate the impact of adverse SDoH on patients. As testament to its contemporary relevance in EM, SEM was selected as the topic of the 2021 Society for Academic Emergency Medicine (SAEM) Consensus Conference “From Bedside to Policy: Advancing Social Emergency Medicine and Population Health through Research, Collaboration, and Education.”11 Although a 2018 systematic review confirmed high rates of material needs and social risk in ED patients, no summation of previous ED-based SEM interventions has been collated or characterized.4 As we build a roadmap for future SEM projects and priorities, knowledge of what has already been done, including successes and failures, as well as opportunities for future growth, will be crucial.
Due to the anticipated breadth and diversity of research evaluating ED interventions focused on SDoH, we felt that a scoping review, which “aims to map the existing literature in a field,” was most appropriate.12 A scoping review is conducted for the purpose of summarizing and disseminating research findings, to provide insight into knowledge gaps (and opportunities), and to explore and describe the general scope of a body of literature. We asked the question: “What interventions to mitigate the effects of negative SDoH (social risk) on ED patients in the US have been published in the peer-reviewed literature?” Our objective was to identify and categorize the different types of SEM interventions implemented in the ED setting.
METHODS
We adhered to the five-step framework provided by Arksey and O’Malley for conducting a scoping review.12 In step 1, a lead research taskforce was assembled to compose the research question and consider definitions. We elected to use the CDC’s definition for SDoH, which focuses on economic stability, neighborhood and physical environment, education, food, community and social context, and the health care system.6 To be included, articles had to involve an intervention (in the ED or with participants identified via an ED visit), defined as an action or process of intervening, with or without a control group, with the intent to mitigate the negative effect of a SDoH on patient outcomes. Given its unique health care model, we elected to focus this review on U.S.-based projects.
In step 2, with the assistance of a medical librarian, we designed and conducted searches in PubMed (MEDLINE), CINAHL, and Cochrane CENTRAL to identify relevant articles. Search strategies were designed and searches were conducted in January 2020, inclusive of all published articles to that date, incorporating controlled vocabulary subject headings and keywords based on the following concepts: 1) emergency medicine, 2) SDoH (including numerous specific topics such as employment or housing), and 3) United States location (including specific states; see Data Supplement S1, Appendix S1, available as supporting information in the online version of this paper, which is available at http://onlinelibrary.wiley.com/doi/10.1111/acem.14201/full). To augment this initial search, we also conducted and included a “pearl-growing” search in PubMed.13, 14 A pearl-growing search incorporates the citation lists of previously identified representative articles that meet the inclusion criteria. Seven highly relevant articles, one from each of the SDoH domain focus categories (see below), were identified by the review team and subjected to this “citation-mining” process to find any additional potentially relevant articles.
In step 3 our research team identified relevant articles. Specific inclusion and exclusion criteria utilized are listed in Table 1. The Covidence systematic review support tool was used to review abstracts.15 All abstracts were reviewed independently and in duplicate by two authors and continued to full review if one or both reviewers indicated possible inclusion. All full articles were reviewed by two authors for final inclusion. Disagreements were resolved by a third author.
TABLE 1.
Scoping review inclusion and exclusion criteria
| Inclusion and exclusion criteria |
Inclusion | Exclusion |
|---|---|---|
| Population |
|
|
| Intervention |
|
|
| Study type |
|
|
Abbreviation: SDoH, social determinants of health.
In step 4, the included articles were sorted and organized by the research team. The categorization scheme was determined by consensus after full review of the included articles. We categorized articles by 1) intervention type, 2) SDoH domain, and 3) outcome.
Categorization of intervention type
Based on iterative evaluation, we determined that interventions fell into one or more of three intervention types: a) educational interventions for EM providers or staff, b) “disease modification” interventions aimed at a subset of patients directly affected by a social risk, or c) interventions (non–disease specific) that aimed to affect a social risk or social need itself (“direct social need” focus).
Categorization of SDoH domain
Social determinants of health domain groupings were likewise determined by research team consensus after summative review of included articles. The choice of these particular domains was based on recurrent article themes and guided by the CDC’s definition of SDoH. This resulted in seven SDoH domains: 1) access to care, 2) discrimination/group disparities, 3) exposure to violence/crime, 4) food insecurity, 5) housing insecurity/homelessness, 6) language/literacy/health literacy, and 7) socioeconomic disparities/poverty. All articles in the review were collated by intervention type and SDoH domain (Table 2). Of note, while our search criteria were guided by CDC SDoH-defined variables, the seven SDoH focus domains identified by the research team were felt to offer a more formative categorization of the available articles from a subspecialty perspective.
TABLE 2.
SDoH categories and outcome reporting
|
Access to care (44 articles) Medical:
|
Reported Outcomes (57)a
|
Discrimination/group disparities (10 articles)
|
Reported outcomes (13)a
|
Exposure to violence/crime (46 articles)
|
Reported outcomes (64)a
|
Food insecurity (2 articles)
|
Reported outcomes (3)a
|
Housing insecurity/homelessness (4 articles)
|
Reported outcomes results (6):
|
Language/literacy/healthcare literacy (16 articles)
|
Reported Outcomes (23)*:
|
Socioeconomic disparities/poverty (13 articles)
|
Reported outcomes (19)a
|
Abbreviation: SDoH, social determinants of health.
Several articles reported more than one outcome.
Categorization of outcomes
After initial review of the articles, a descriptive outcome categorization scheme was created by the research team. We categorized outcomes and collected reported outcome efficacy (as reported by the articles); disagreements were resolved by consensus. Outcome categories included 1) operational outcomes (e.g., number of ED visits, number of primary care provider visits, length of time to subspecialty consult); 2) health outcomes (objective measures of health such as hemoglobin A1C level or rehospitalizations, as well as subjective measures including self-reported wellness on follow- up survey); 3) feasibility and/or acceptability (e.g., patient satisfaction with the intervention or provider assessment of intervention reproducibility); 4) linkage to resources (e.g., direct connection to medical and/or social support, including insurance referral); 5) provider knowledge (e.g., pre–/post–educational intervention test results); 6) case identification (e.g., specific social need or risk detection); and 7) patient comprehension. Several articles included multiple outcome categories and occasionally several outcome measures from within one outcome category. However, efficacy was determined by the articles’ summative reporting of these outcomes (for instance, if one article reported on three health outcomes, two “positive” and one “ineffective,” the health outcome assigned to this article was considered “mixed”; Table 2).
In step 5, we collated and summarized the data from the included articles. Data extraction was performed by the research team using a standardized data collection form developed by the study team. Collected variables included intervention type, SDoH domain focus, number of patients enrolled, and article summary. Because our goal was to provide an overview and characterization of existing literature, we did not evaluate the quality of the individual studies, which is consistent with scoping review methodology.12
RESULTS
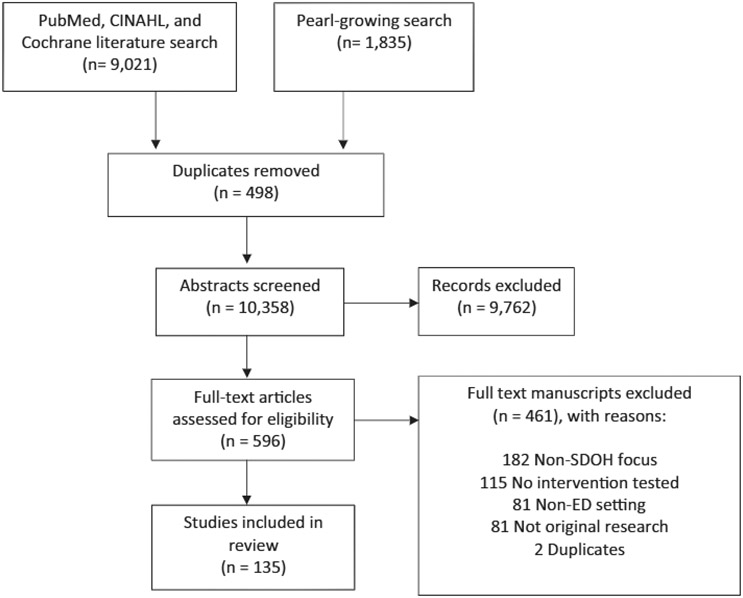
The database searches yielded a total of 9,021 records (Figure 1). The pearl-growing search yielded 1,835 additional records. When duplicate references were removed, there were 10,358 abstracts screened for inclusion. Of these, 596 were classified as potentially relevant by at least one reviewer and advanced to the full article review phase. A total of 135 articles describing 123 unique interventions were selected for final inclusion (Data Supplement S1, Table S1). The most common reasons for article exclusion included non-ED setting, lack of intervention, and/or non-SDoH article focus (Figure 1).
FIGURE 1.
Scoping review inclusion/exclusion flowchart
Included article publication dates ranged from 1989 to 2020. Over half (75, 56%) were published within the past decade, and over one-third (53, 39%) were published between 2015 and 2020. Nearly half (66, 49%) appeared in EM-specific journals; the other half (69, 51%) were published in journals with a variety of foci including public health, technology, health care management, and preventive medicine. Roughly one-third (48, 35%) were randomized controlled trials.
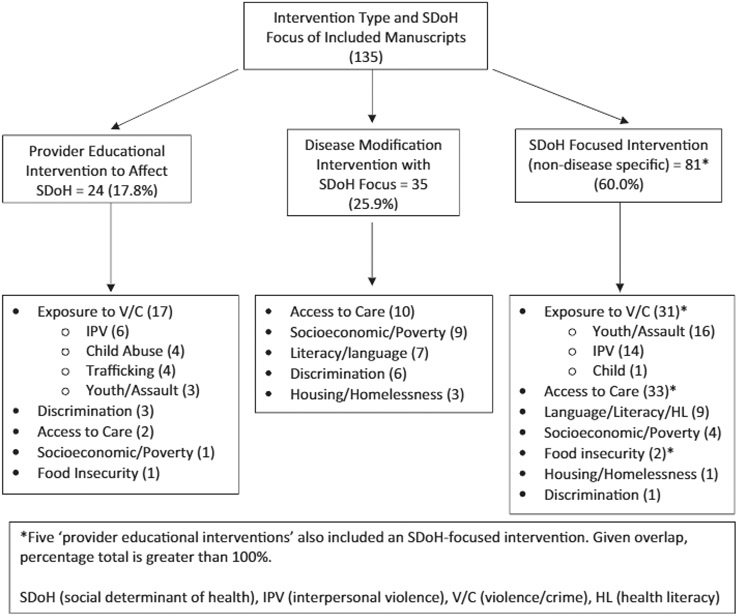
Intervention types (Figure 2)
FIGURE 2.
Manuscript types and domain focus
Twenty-four articles (18%) described an educational intervention implemented to improve EM providers’ awareness of, or approach to, ED patients’ SDoH. A representative example would be a study that used a training module to increase providers’ ability to recognize and appropriately treat human trafficking patients in the ED.16
Thirty-five articles (26%) evaluated a disease-specific modification (e.g., asthma, diabetes) with a focus on a vulnerable population. For instance, one study of this type utilized trained paraprofessionals, both in the ED and subsequently as a community link, to screen and counsel African American men regarding cardiovascular risk factors.17
The remaining 81 articles (60%), including five that also included a component of provider education, evaluated interventions to directly affect a social risk or social need without consideration or requirement of a specific disease process. Studies in this category are exemplified by the implementation of screening and referral programs where the intervention aims to screen for “at-risk” patients and provide referrals. For example, several studies reported integrative ED-based case management programs to identify un- or underinsured patients and provide referral to public insurance and/or charity care programs.18-21
SDoH domains
Forty-four articles (33%) focused on interventions to improve access to care, primarily linkage to post-ED follow-up, including referral to a “medical home” or facilitation of enrollment in a charity care or managed care system. These studies targeted patients in disadvantaged cohorts, including the un- or underinsured. This subgroup also included interventions which addressed transportation issues (two studies) as well as medical care access in rural communities (six studies). The majority (34, 77%) were non–disease specific.
Ten articles (7%) focused exclusively on discrimination/group disparities. For the purpose of this review's categorization, discrimination/group disparities refers to interventions implemented to specifically mitigate the negative effects of SDoH in demographic groups delineated by race, ethnicity, and/or sexual orientation and gender identity. All intervention types were represented in these 10 articles, including three provider educational articles, six disease-specific, and one non–disease-specific intervention.
Forty-six articles (34%) focused on exposure to violence/crime. This category included articles addressing human trafficking (four studies), domestic or interpersonal violence (17 studies), violent assault (including firearms and other weapons; most frequently youth focused; 19 studies), and child abuse (six studies). Intervention types included provider educational interventions (37%) and interventions aimed directly at decreasing subsequent violence exposure and recidivism (63%).
Two articles (2%) assessed interventions addressing food insecurity, defined by interventions designed to increase the availability of food or an individuals’ ability to access it. One of these articles also included a provider educational intervention component.
Four articles (3%) directly addressed housing insecurity/homelessness, where housing insecurity is defined as lack of sufficient domicile or shelter. Three of these articles addressed this SDoH issue in the context of a disease-specific intervention while one article addressed this SDoH directly in a non–disease-specific context.
Sixteen articles (12%) focused on language/literacy/health care literacy. This category included all interventions that considered SDoH from a communication perspective. It included all article that considered primary literacy, health care literacy, and non–English-speaking populations in its intervention aim. Typical interventions included increasing access to interpreters, improving or creating alternative discharge instructions, and other interventions to improve communication or patients’ understanding. Seven articles (44%) had a disease-specific focus and nine (56%) did not. There were no educational-type interventions that focused on communication.
Thirteen socioeconomic disparities/poverty articles (10%) included those interventions which aimed to intervene specifically on patients impacted by lower socioeconomic status. All intervention types were represented. The majority (69%) targeted a disease-specific modification intervention with a SDoH focus.
Outcomes
The included articles reported 185 primary or major secondary outcomes by category. The majority, 144 (78%), were reported as positive or effective while 18 (10%) were mixed or equivocal and 23 (12%) were deemed ineffective. Of the 144 outcomes reported as positive or effective, operational outcomes accounted for the majority (24%), followed by linkage to resources (20%), feasibility and acceptability (20%), health outcomes (14%), provider knowledge (12%), patient comprehension (7%), and case identification (3%). Of the 23 outcomes reported as ineffective, health outcomes accounted for the majority (30%), followed by case identification (17%), operational metrics (16%), feasibility and acceptability (13%), linkage to resources (9%), and patient comprehension (4%).
DISCUSSION
Principal findings
This review highlights ED-initiated interventions that have been designed, implemented, and assessed over the past three decades with the goal of mitigating the harmful effects of negative SDoH as they relate to social risk and need. Included studies represent a variety of approaches with regard to type of intervention as well as intervention focus. Our analysis demonstrates that these interventions and evaluations are becoming increasingly frequent, as suspected based on increasing interest in SEM.
With regard to SDoH domain, it is notable that cumulatively, two-thirds (90, 67%) of the interventions focused on either access to care or exposure to violence/crime. The reason for this majority may have a financial explanation. Access to care, specifically provision of insurance, is tied tightly to reimbursement. A prioritization of this specific social need may result in better care for patients and, concomitantly, improve health care reimbursement and reduce health care costs for the medical system, a financial “win–win.”22, 23 As a result, it is conceivable that financial support for studies aiming to decrease unreimbursed care may be more prevalent and accessible than that which is available for other SDoH domains. Similarly, from a funding perspective, grants for programs addressing exposure to violence/crime have become increasingly available, including from the U.S. Department of Justice, since the 1994 Violence Against Women Act and the Victims of Trafficking and Violence Protection Act of 2000.24-27 Therefore, projects that fall into these SDoH domains, access to care and exposure to violence/crime, may be more prevalent due to the availability of funding and support. Conversely, however, interventions which do not generate direct health care reimbursement or are not otherwise socially prioritized may have fewer funding opportunities. Although we did not set out to evaluate this hypothesis, this was reflected in our search results.
Two of our SDoH domains, while unique enough in primary focus to warrant unique SDoH grouping by research team consensus, accounted for fewer than 5% of our final articles—housing/homelessness and food insecurity. It is worth noting, however, that some access to care and/or socioeconomic disparities/poverty interventions may have overlapped into these two domains, resulting in a somewhat exaggerated underrepresentation. For instance, some access to care and/or socioeconomic disparities/poverty interventions engaged a case manager or social work services, a component of which might have dealt with food or housing access, however, not as an explicit focus of the initial intervention.28, 29 Both categories, particularly housing/homelessness, represent often chronic, complex issues that are both challenging and resource consuming when attempting to address in the acute care setting.30 The six articles included in these categories, however, offer helpful insights into overcoming these barriers and suggest that these SDoH foci do lie within EM’s domain to assess and intervene.
The domain of discrimination/group disparities was also underrepresented in the articles (7.4% of total). However, again, some overlap with access to care and/or socioeconomic-designated articles was noted during the categorization process by investigators. Many access to care and/or socioeconomic disparities/poverty–focused articles included a disproportionate number of underrepresented groups or minorities. However, the primary intent of the intervention in these instances was not to reduce disparities for minorities or otherwise underrepresented groups.31, 32 This highlights and reflects the intersectionality in the United States of race/ethnicity with insurance status, socioeconomic status, and access to medical care.33-35 As such, while the focus of any particular access to care or socioeconomic disparities/poverty article might not have been a particular racial or ethnic minority group, racial and ethnic minorities were often overrepresented in the intervention group compared to the national average due to eligibility requirements for enrollment, such as lack of insurance. This overlap implies that interventions aimed at affecting social risk and need will very likely have additional impact and reach beyond the primary SDoH focus. Despite this overlap, however, the disproportionate burden of disease borne by minority populations should be addressed directly by future interventions, not only indirectly via attempts to rectify disparities in access to care.
While several interventions relied on technology-based interventions, including text-capable smartphones or home computer access, no interventions directly addressed access to technology or education or career opportunities, domains of SDoH by the CDC’s framework.36, 37 This may simply be due to lack of funding, because studies providing phones, computers, Internet access, or career training would likely be expensive. However, as COVID-19 social distancing precautions remain, and we continue to rely heavily on virtual and teleoptions for all facets of life, including health care, access to technology and education may have an increasing impact on both SDoH and health outcomes.38 In response, the EM community might consider previously unconventional funding partnerships, including technology-based corporations, to prevent the inevitable worsening of disparities based on the growing digital divide.39
Finally, while we did not assess study quality nor validity, the preponderance of articles reported that their interventions were effective. In fact, within all outcome categories except case identification, more studies reported positive outcomes than ineffective or equivocal outcomes. This may be due, in part, to publication bias resulting in the disproportionate publication of statistically significant and effective interventions.40 Of note, the three most commonly reported effective outcome categories were not health outcomes. Outcomes such as operational metrics, linkage to resources, and feasibility/acceptability are often easier to affect and measure, from a research perspective, than the long-term health-related outcomes typically associated with SDoH. In addition, while not specifically a health outcome, many of the more commonly measured outcomes may be considered steps to improve health outcomes—linkage to a primary care provider or provision of social resources, for instance, are actions with potential indirect positive effects on health outcomes.41, 42 The number and distribution of outcome categories also reflects the heterogeneity of health issues affected by SDoH as well as the diversity of interventions implemented to address them.
Finally, it is important to acknowledge that while EDs are frequently called upon to be the social safety nets for our society, many are not adequately equipped to handle these interventions. By summarizing and categorizing previous projects and successes, this review may provide a guide to assist with future upstream social advocacy and health care policy direction as it pertains to SEM.
Future directions
This review aims to improve our appreciation of the extant literature on ED interventions addressing SDoH and to summarize what has been published on this topic to date to provide insight into the development of a future research agenda. Our review highlights several areas that have substantial research and other areas that have gaps. As SEM continues to develop and evolve, these results will provide launching points for researchers, advocates, and policy-makers considering EM-based interventions to address SDoH in the United States.
In addition, based on this review, we hypothesize that funding sources may play a considerable role in the existence of this body of literature. Those wishing to advance research in any particular domain should consider efforts to affect funding priorities, to include provision of feedback and direct outreach to national and specialty specific funding organizations.
LIMITATIONS
We limited our database search to PubMed, CINAHL, and Cochrane and, as such, it is possible that unique peer-reviewed literature that met our inclusion criteria might have been missed if it did not appear in these databases. Because these databases include the vast majority of medical and allied health professional literature, we believe the likelihood of missing a pertinent article using our search strategy is low. As noted, because of the breadth and variety of studies included, quality assessment was not performed.12
As an additional note, we recognize that definitions of SDoH can vary, depending on the source. In utilizing the CDC-recognized definition of SDoH to help design our search criteria, we used a well-recognized, nationally accepted definition. However, our search terms may not have included categories that many view as part of SEM, such as access to substance abuse treatment or immigration or legal issues. Finally, no standards or guidelines exist for categorization of SEM interventions to date; the intervention types and domains created were done by research team consensus with the primary goal to assist with overall assessment and analysis. Many included articles may have components of several SDoH domains; however, the authors chose to categorize based on predominant focus and consensus agreement. It is conceivable that, under different scrutiny, categorization results would differ.
We also recognize that many interventions aimed at mitigating negative SDoH have originated in locations outside of the ED—such as in community health centers—yet very much address the needs and risks of ED patients. These interventions would not have been captured by our review, but may be part of an important foundation for future work within the above-mentioned domains. In addition, while there appears to be a growing literature base of intervention studies, many of these studies address downstream social needs, addressing an individual patients’ needs, rather than broadly affecting negative SDoH for a population. This review did not aim to include policy and advocacy interventions that aim to address SDoH at a more upstream point.
CONCLUSION
This scoping review reveals that researchers have been assessing, engaging, and intervening with vulnerable ED populations for decades and are doing so with increasing frequency. As emergency medicine continues to embrace a public health–oriented role within the U.S. health care system, this review helps us consider ED-based interventions that have already been developed, implemented, and evaluated. An understanding of previous work and research in this area will serve as a foundation for future ED-based interventions addressing social risk and social need and, ultimately, may help address persistent disparities in health outcomes across the United States.
Supplementary Material
Footnotes
CONFLICT OF INTEREST
The authors have no potential conflicts to disclose.
REFERENCES
- 1.Bitterman RA. EMTALA and the ethical delivery of hospital emergency services. Emerg Med Clin North Am. 2006;24(3):557–577. [DOI] [PubMed] [Google Scholar]
- 2.Terp S, Seabury SA, Arora S, Eads A, Lam CN, Menchine M. Enforcement of the Emergency Medical Treatment and Labor Act, 2005 to 2014. Ann Emerg Med. 2017;69(2):155–162.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cone DC, Richardson LD, Todd KH, Betancourt JR, Lowe RA. Health care disparities in emergency medicine. Acad Emerg Med. 2003;10(11):1176–1183. [DOI] [PubMed] [Google Scholar]
- 4.Malecha PW, Williams JH, Kunzler NM, Goldfrank LR, Alter HJ, Doran KM. Material needs of emergency department patients: a systematic review. Acad Emerg Med. 2018;25(3):330–359. [DOI] [PubMed] [Google Scholar]
- 5.Anderson ES, Lippert S, Newberry J, Bernstein E, Alter HJ, Wang NE. Addressing social determinants of health from the emergency department through social emergency medicine. West J Emerg Med. 2016;17(4):487–489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention. Social Determinants of Health. https://www.cdc.gov/socialdeterminants/index.htm. Accessed August 28, 2020.
- 7.Braveman P, Gottlieb L. The social determinants of health: it's time to consider the causes of the causes. Public Health Rep. 2014;129(1 suppl 2):19–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Samuels-Kalow ME, Ciccolo GE, Lin MP, Schoenfeld EM, Camargo CA Jr. The terminology of social emergency medicine: Measuring social determinants of health, social risk, and social need. JACEP Open. 2020;22(6):18–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Alderwick H, Gottlieb LM. Meanings and misunderstandings: a social determinants of health lexicon for health care systems. Milbank Q. 2019;97(2):407–419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Alter HJ. Foreword to conference proceedings, Inventing Social Emergency Medicine. Ann Emerg Med. 2019;74(5S):S1–S2. [DOI] [PubMed] [Google Scholar]
- 11.Society for Academic Emergency Medicine. Consensus Conference 2021. https://www.saem.org/annual-meeting/future-and-past-meetings/future-meet.… Accessed August 28, 2020. [Google Scholar]
- 12.Daudt HM, van Mossel C, Scott SJ. Enhancing the scoping study methodology: a large, inter-professional team's experience with Arksey and O'Malley's framework. BMC Med Res Methodol. 2013;13:48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cochrane Training, Technical Supplement to Chapter 4: Searching for and Selecting Studies. https://training.cochrane.org/handbook/current/chapter-04-technical-supp.… Accessed August 28, 2020.
- 14.Schlosser RW, Wendt O, Bhavnani S, Nail-Chiwetalu B. Use of information-seeking strategies for developing systematic reviews and engaging in evidence-based practice: the application of traditional and comprehensive Pearl Growing. A review. Int J Lang Commun Disord. 2006;41(5):567–582. [DOI] [PubMed] [Google Scholar]
- 15.Van der Mierden S, Tsaioun K, Bleich A, Leenaars CH. Software tools for literature screening in systematic reviews in biomedical research. Altex. 2019;36(3):508–517. [DOI] [PubMed] [Google Scholar]
- 16.Chisolm-Straker M, Richardson LD, Cossio T. Combating slavery in the 21st century: the role of emergency medicine. J Health Care Poor Underserved. 2012;23(3):980–987. [DOI] [PubMed] [Google Scholar]
- 17.Bone LR, Mamon J, Levine DM, et al. Emergency department detection and follow-up of high blood pressure: use and effectiveness of community health workers. Am J Emerg Med. 1989;7(1):16–20. [DOI] [PubMed] [Google Scholar]
- 18.Schrader CD, Robinson RD, Blair S, et al. Common step-wise interventions improved primary care clinic visits and reduced emergency department discharge failures: a large-scale retrospective observational study. BMC Health Serv Res. 2019;19(1):451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Acosta C, Dibble C, Giammona M, Wang NE. A model for improving uninsured children's access to health insurance via the emergency department. J Healthc Manag. 2009;54(2):105–116. [PubMed] [Google Scholar]
- 20.Gordon JA, Dupuie TA. Child health insurance outreach through the emergency department: a pilot study. Acad Emerg Med. 2001;8(11):1088–1090. [DOI] [PubMed] [Google Scholar]
- 21.Kanak M, Rutman L, Pirrotta EA, Giammona M, Bermudez M, Wang NE. Emergency department-based health insurance enrollment for children: does linkage lead to insurance retention and utilization? Pediatr Emerg Care. 2015;31(3):169–172. [DOI] [PubMed] [Google Scholar]
- 22.Gaudette É, Pauley GC, Zissimopoulos JM. Lifetime consequences of early-life and midlife access to health insurance: a review. Med Care Res Rev. 2018;75(6):655–720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Obama B. United States health care reform: progress to date and next steps. JAMA. 2016;316(5):525–532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Library of Congress. Violence Against Women Act. https://www.congress.gov/bill/103rd-congress/senate-bill/11. Accessed August 28, 2020.
- 25.U.S. Department of Health &Human Services, Office on Women’s Health, Federal Funding to Address Violence Against Women. https://www.womenshealth.gov/30-achievements/12. Accessed August 28, 2020.
- 26.Library of Congress. Victims of Trafficking and Violence Protection Act of 2000. https://www.congress.gov/bill/106th-congress/house-bill/3244. Accessed August 28, 2020.
- 27.U.S. Department of Health and Human Services, Office on Trafficking in Persons. Grants. https://www.acf.hhs.gov/otip/grants. Accessed August 28, 2020. [Google Scholar]
- 28.Bernstein J, Dorfman D, Lunstead J, et al. Reaching adolescents for prevention: the role of pediatric emergency department health promotion advocates. Pediatr Emerg Care. 2017;33(4):223–229. [DOI] [PubMed] [Google Scholar]
- 29.Losonczy LI, Hsieh D, Wang M, et al. The Highland Health Advocates: a preliminary evaluation of a novel programme addressing the social needs of emergency department patients. Emerg Med J. 2017;34(9):599–605. [DOI] [PubMed] [Google Scholar]
- 30.Mabhala MA, Yohannes A, Griffith M. Social conditions of becoming homelessness: qualitative analysis of life stories of homeless peoples. Int J Equity Health. 2017;16(1):150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gielen AC, McKenzie LB, McDonald EM, et al. Using a computer kiosk to promote child safety: results of a randomized, controlled trial in an urban pediatric emergency department. Pediatrics. 2007;120(2):330–339. [DOI] [PubMed] [Google Scholar]
- 32.Zorc JJ, Scarfone RJ, Li Y, et al. Scheduled follow-up after a pediatric emergency department visit for asthma: a randomized trial. Pediatrics. 2003;111(3):495–502. [DOI] [PubMed] [Google Scholar]
- 33.Kirby JB, Kaneda T. Unhealthy and uninsured: exploring racial differences in health and health insurance coverage using a life table approach. Demography. 2010;47(4):1035–1051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Manuel JI. Racial/ethnic and gender disparities in health care use and access. Health Serv Res. 2018;53(3):1407–1429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Williams DR, Priest N, Anderson NB. Understanding associations among race, socioeconomic status, and health: patterns and prospects. Health Psychol. 2016;35(4):407–411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Joseph CL, Mahajan P, Stokes-Buzzelli S, et al. Pilot study of a randomized trial to evaluate a Web-based intervention targeting adolescents presenting to the emergency department with acute asthma [published correction appears in Pilot Feasibility Stud. 2017;3:48]. Pilot Feasibility Stud. 2017;4:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Burner ER, Menchine MD, Kubicek K, Robles M, Arora S. Perceptions of successful cues to action and opportunities to augment behavioral triggers in diabetes self-management: qualitative analysis of a mobile intervention for low-income Latinos with diabetes. J Med Internet Res. 2014;16(1):e25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Smith B, Magnani JW. New technologies, new disparities: the intersection of electronic health and digital health literacy. Int J Cardiol. 2019;292:280–282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ramsetty A, Adams C. Impact of the digital divide in the age of COVID-19. J Am Med Inform Assoc. 2020;27(7):1147–1148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Murad MH, Chu H, Lin L, Wang Z. The effect of publication bias magnitude and direction on the certainty in evidence. BMJ Evid Based Med. 2018;23(3):84–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Freidberg MW, Hussey PS, Schneider EC. Primary care: a critical review of the evidence on quality and costs of health care. Health Aff (Millwood). 2010;29(5):766–772. [DOI] [PubMed] [Google Scholar]
- 42.Solomon LS, Kanter MH. Health care steps up to social determinants of health: current context. Perm J. 2018;22(22):18–139. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.