Abstract
Objective:
Sacral neuromodulation (SNM) has emerged as an effective therapy for refractory lower urinary tract dysfunction (LUTD). Remote programming holds promise in addressing the time and economic burdens associated with outpatient programming, especially for patients in the observation period following Stage I implant surgery (where the lead is implanted first without the pulse generator). The study aimed to explore the effectiveness and patient satisfaction of remote programming for Stage I SNM patients, and analyze the benefits patients gain from remote programming.
Methods:
This prospective study was conducted at multiple high-level clinical SNM centres in China. Patients requiring SNM implantation were enroled and divided into two groups based on patient preference: remote programming (RP) group and outpatient control (OC) group. Patient attitudes toward RP were assessed through questionnaires, and the degree of symptom improvement was compared between the two groups to explore the usability of RP.
Results:
A total of 63 participants from 6 centres were included in the study, with 32 belonging to the RP group. The remote programming system presents a high level of usability (98%) and willingness (satisfaction rate: 96.83%) in result of questionnaire. RP showed a significant advantage in improving patients’ score of ICSI/ICPI (medianΔICSI/ICPI RP vs. OC= −13.50 vs −2, P=0.015). And slightly ameliorate urinary symptoms such as pain (medianΔVAS RP vs. OC= −1 vs 0, P= 0.164) and urgency (medianΔOBASS −2.5 vs. −1, P= 0.,229), but the difference was not statistically significant. RP did not significantly impact the quality of life of patients (P=0.113), so do the rate of phase-two conversion (P= 0.926) or programming parameters.
Conclusion:
To the best of our knowledge, the presented study is the first multicenter research focusing on the remote programming of Stage I SNM patients. Through the clinical implementation and patient feedback, we demonstrate that remote programming is not inferior to in-person programming in terms of success rate, effectiveness, safety, and patient satisfaction.
Keywords: lower urinary tract dysfunction, remote programming, sacral neuromodulation, stage I surgery
Introduction
Highlights
The presented research is the first multicenter clinical study of remote programming for patients post-stage I sacral neuromodulation surgery around the world.
This study employed a prospective multicenter research approach to investigate patients’ willingness, user experience, and the effectiveness of remote control for sacral nerve modulation, as reflected by multiple objective indicators. It represents the outcomes of remote programming therapy in the Chinese population.
Refractory lower urinary tract dysfunction (LUTD) refers to non-obstructive functional abnormalities in the bladder and urethra during the storage and/or voiding phases, resulting from various neurogenic or non-neurogenic factors1,2. LUTD encompasses a wide spectrum of disorders, presenting with a range of symptoms, from continuous urinary leakage to urinary retention, recurrent urolithiasis, bladder pain, and recurrent urinary tract infections (UTIs). These conditions can ultimately lead to a significant decline in the quality of life and have a detrimental impact on the upper urinary tract, causing substantial patient distress and imposing a significant economic burden3,4.
Sacral neuromodulation (SNM) has a history of over thirty years in the treatment of refractory LUTD and was approved for clinical use by the U.S. Food and Drug Administration in 19975,6 In China, SNM has been applied for nearly a decade, with recent developments and expansions7,8. While SNM can effectively improve the clinical symptoms of patients with refractory LUTD, patients often need to visit the hospital regularly for programming adjustments to maintain satisfactory efficacy.
The term “Stage I surgery” is commonly utilized in staged sacral nerve modulation therapy. In this procedure, a lead wire is initially implanted into the sacral foramen without the inclusion of a pulse generator. Subsequently, during the postoperative Stage I, patients often necessitate more frequent programming to ensure they attain the best therapeutic results.
Due to the fact that most qualified SNM centres in China are located in first-tier cities, and given the vast geographical expanse and uneven regional healthcare development in our country, many patients find it challenging to obtain timely and appropriate adjustments and planning after seeking medical treatment. In their pursuit of suitable programming, these patients often incur substantial time and economic costs travelling to hospitals with the implanted devices. Undoubtedly, it not only increases the time and economic burden on patients but also adversely affects their willingness to seek medical care and their medical compliance, ultimately leading to suboptimal long-term postoperative outcomes9.
Tsinghua University’s PINS Corporation has developed a novel SNM product, utilizing their unique remote programming technology. In simple terms, this technology allows patients to contact their physicians via the internet or mobile 4G/5G networks, from the comfort of their homes or any location with internet access, to adjust parameters and improve their symptoms. This technology undoubtedly alleviates many of the aforementioned challenges, and prior research by our team suggests that patients have benefited from it10. However, whether Stage I patients can benefit from remote control and whether it is beneficial for the conversion to Stage II remains a subject for further investigation.
To the best of our knowledge, the presented study is the first multicenter research focusing on the remote programming of Stage I SNM patients, aims to explore the benefits of remote programing for patients after Stage I SNM surgery, with the goal of guiding the refinement of remote programing technology.
Method
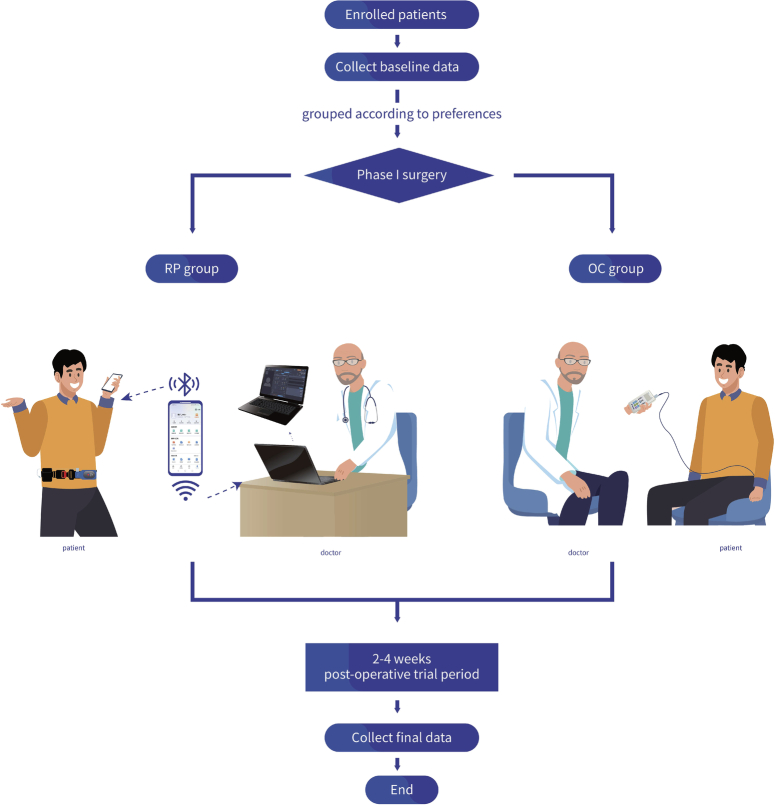
The presented study is a prospective multicenter case-control research and has been reported in line with the STROCSS criteria11, Supplemental Digital Content 1, http://links.lww.com/JS9/B825. Enroled patients are categorized into either the Remote Programing Group (RP group) or the Outpatient Control Group (OC group) based on their preferences. Initially, baseline research data is collected from the patients, followed by the surgical procedure. After the completion of the patients’ Stage I trial period (typically spanning 2–4 weeks), a second set of research data is collected. Subsequently, statistical analysis is conducted to explore the therapeutic effects, economic benefits, and analyze potential risk factors among the patients (Fig. 1).
Figure 1.
Study design. OC, outpatient control; RP, remote programming.
Patient information
This study was conducted across six accredited clinical centres specializing in SNM. The participants were patients who met the diagnostic criteria for refractory LUTD and willingly participated in the study after providing informed consent.
Inclusion criteria were as follows
Age older than or equal to 18 years;
Patients implanted with sacral nerve stimulation systems due to refractory lower urinary tract dysfunction between August 2022 and June 2023, such as overactive bladder, neurogenic bladder, interstitial cystitis/chronic pelvic pain syndrome, non-obstructive urinary retention, etc.;
Agreement to refrain from arbitrarily altering medications that may affect lower urinary tract symptoms and pelvic function during the trial period;
Voluntary participation in the research study and signing of informed consent;
Possess the needed ability to communicate effectively with the investigators and willingness to adhere to the requirements of the entire trial.
Exclusion criteria included:
Pregnant or lactating women;
Concurrent uncontrolled urinary tract infections, urinary tract obstruction, urological tumours;
Mental health conditions hindering collaboration with medical professionals;
Presence of severe concomitant diseases, such as non-urological malignant tumours, significantly impacting health;
Other circumstances deemed unsuitable for participation in the study by the investigators.
Clinical data
Data collection primarily comprises two components: a self-designed questionnaire and symptom questionnaires. The self-designed questionnaire was developed by the researchers to supplement remote control information in alignment with the practical aspects of the study. The questionnaire includes information about the time and economic costs (including costs incurred by accompanying family members) associated with each routine hospital visit for programming, reasons for requesting remote programming, the anticipated frequency of remote control, the extent to which remote control has been beneficial for the patients, the ease of operating remote control, patient satisfaction with remote control, and their likelihood of recommending it, among other aspects.
The symptom questionnaire focuses on specific aspects of the patients’ Lower Urinary Tract Dysfunction (LUTD) and primarily includes the following: Standard voiding diary; Visual analogue scale (VAS); Overactive Bladder Symptom Score (OABSS); Voiding Symptom Quality of Life Questionnaire (QoL); Interstitial Cystitis O’Leary-Sant Symptom and Problem Index (ICPI&ICSI); The scales used in the research are available in Supplement 1 for reference.
Remote programming system
The remote programming system, refers to a programming method distinct from traditional face-to-face programming. Specifically, it involves utilizing specialized remote devices to communicate and conduct programming and debugging with physicians or device engineers through wireless or wired network connections.
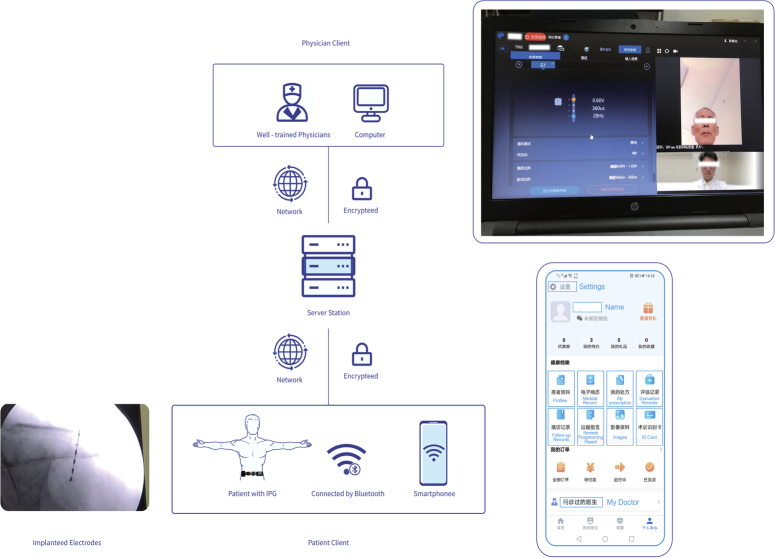
The remote programming system adopted by the presented was developed and launched by Tsinghua Pins Medical Technology Co., Ltd. in 2019, is currently applicable in several neuromodulation system10,12,13. The system comprises three main components: the Doctor’s Console, the Patient’s Interface, and the Central Server terminal. The patient’s interface and the doctor’s console are connected to the central server through two different versions of applications (Fig. 2).
Figure 2.
Schematic diagram of how remote programming system works.
In our remote programming system, patients at home use their mobile devices (tablets or smartphones) to access the patient version of the application. They can schedule appointments with their doctors and pair their devices with the implanted pulse generator (IPG) via Bluetooth for remote programming. Video, audio, and stimulation signals are transmitted to the central server.
Meanwhile, in the physician’s interface doctors are able to adjust the patient’s stimulation program based on their condition. The principle involves doctors sending programming commands to the central server through the interface, and the server converts these commands into operational instructions recognizable by the stimulator, pushing them to the patient’s interface. This facilitates functions such as audio-visual communication, telemetry, parameter adjustments, electrode impedance detection, and more. Research by Chinese scholars has confirmed that this technology is just as effective as in-person programming in outpatient settings14.
Furthermore, to ensure data security, we have three levels of protection: secure Hyper Text Transfer Protocol over Secure Socket Layer (HTTPS) with asymmetric encryption, secure Low Energy Bluetooth (BLE), and Near Field Communication (NFC) mode for device communication. The patient’s app includes a “one-click restore/shutdown” function for network issues.
Figure 2 illustrates the remote programming system, which consists of three parts: the patient’s interface, the physician’s interface, and the central server. The physician’s interface is depicted in the lower right corner, and the patient’s interface is shown in the upper right corner.
Ethics
This study has undergone ethical review at Beijing Hospital and the various research unit subcenters, with an ethics approval number of 2020BJYYEC07802. This approval ensures the ethical compliance of the study and underscores the ethical standards that researchers are obligated to adhere to. Furthermore, this study is registered with the China Clinical Trial Center, with registration number ChiCTR2000036677. (https://www.chictr.org.cn/index.html).
Prior to the commencement of this study, each participant undergoes a comprehensive informed consent procedure. The study will maintain transparency at all times, and the research plan and results will be publicly disclosed. We employ institutional-level review oversight to prevent potential conflicts of interest, ensuring the fairness and reliability of the study.
Statistical analysis
Initially, data cleaning was conducted to ensure data quality and consistency. Descriptive statistical methods were used to analyze baseline data to understand the characteristics of the two patient groups. For continuous variables that followed a normal distribution, mean and standard deviation were presented, and t-tests were used for comparisons. For variables that did not follow a normal distribution, median and interquartile range were presented, and the Mann–Whitney U test was used for group comparisons. Categorical variables were presented as counts (percentages), and χ2 tests were used for between-group comparisons.
Subgroup analyses, if required, would be conducted to delve deeper into the differences in treatment outcomes and economic benefits among different subgroups of patients. All statistical analyses would be performed using IBM SPSS Statistics 19.0.0.329, and visualizing by GraphPad Prism 8.3.0, Python to ensure the accuracy and reliability of the results.
Result
General information
A total of 63 participants were included in the study across 6 centres. Among them, 32 belonged to the RP group. The patients were primarily from North China, East China, and Central China. The vast majority of patients decided on surgery due to difficulties in urination caused by neurogenic lower urinary tract dysfunction. Other symptoms include overflow urinary incontinence, pain or dysuria (painful urination), frequent urination, and urinary retention. In most cases, the modulating electrodes were implanted in the left S3 sacral foramen (about 56%). There were no significant differences between the two groups in terms of general data such as age and sex. However, it’s noteworthy that there were statistically significant differences in diagnoses and some symptoms between the two groups. Specifically, 7 patients with interstitial cystitis (IC) were included in the RP group. Measures will be taken to avoid the deviation of statistical analysis from reality in subsequent analysis. (Table 1, Fig. 3A).
Table 1.
General Information of enroled patients.
| RP group (n=32) | OC group (n=31) | t/χ2 | p | |
|---|---|---|---|---|
| Age, mean (SD) | 44.75 (20.28) | 51.10 (17.08) | 1.341 | 0.185 |
| Sex | 2.045 | 0.153 | ||
| Male | 16 | 21 | ||
| Female | 16 | 10 | ||
| Implant side | 3.625 | 0.161 | ||
| Left | 18 | 18 | ||
| Right | 14 | 10 | ||
| Double | 0 | 3 | ||
| Implanted sacral hiatus | 2.506a | 0.113 | ||
| S3 | 32 | 27 | ||
| S4 | 0 | 4 | ||
| Residence type | 0.762 | 0.383 | ||
| Countryside | 12 | 16 | ||
| City | 20 | 20 | ||
| Diagnose | 7.653 | 0.022 | ||
| NLUTD | 24 | 30 | ||
| IC | 7 | 0 | ||
| UUI/OAB | 1 | 1 | ||
| Difficulty urinating | 5.028 | 0.025 | ||
| Do not have | 12 | 4 | ||
| Have | 20 | 27 | ||
| Overflow urinary incontinence | 0.169 | 0.681 | ||
| Do not have | 28 | 26 | ||
| Have | 4 | 5 | ||
| Pain or dysuria | 3.059 | 0.08 | ||
| Do not have | 25 | 29 | ||
| Have | 7 | 2 | ||
| Frequent urination | 3.65 | 0.056 | ||
| Do not have | 20 | 26 | ||
| Have | 12 | 5 | ||
| Urgency with incontinence | 7.497 | 0.006 | ||
| Do not have | 21 | 29 | ||
| Have | 11 | 2 | ||
| Urinary retention | 5.341 | 0.021 | ||
| Do not have | 27 | 18 | ||
| Have | 5 | 13 |
IC, interstitial cystitis; NLUTD, neurogenic lower urinary tract dysfunction; OAB, overactive bladder; OC, outpatient control; RP, remote programming; UUI, Urge Urinary Incontinence.
Using χ2 test with continuity correction.
Figure 3.
Statistical graphs of self-designed questionnaire and symptom questionnaire results. A: Pie chart of self-designed questionnaire survey results; B: Violin plot comparing quality of life scores (QOL), visual analog scale for pain scores (VAS), overactive bladder symptom scores (OBASS), and International O'Leary-Sant Symptom and Problem Index (OLS) between the RP group and OC group. OBASS, Overactive Bladder Awareness and Symptom Score; OC, outpatient control; QoL, Voiding Symptom Quality of Life Questionnaire; P, remote programming; VAS, visual analogue scale.
Survey results
Through the survey, the study found that although the cost of a single session of remote programming is relatively low for most patients (~60% of patients have a single-session cost <500 yuan), the time cost is quite high, with the majority needing to spend more than a working day. Therefore, upon group comparison, it becomes evident that the economic cost associated with outpatient control (OC) group is notably lower (P=0.02), possibly explaining their preference for choosing this group when enroling. It’s also noteworthy that the two groups differ in their motivations for seeking remote programming. The Remote Programming (RP) group tends to opt for it more due to considerations of time and economic costs, while OC patients primarily lean towards remote programming because of the frequent recurrence of symptoms (P=0.02). No substantial differences were observed between the two groups in response to other questionnaire items. In fact, although over 80% of patients stated that their desired frequency of programming is not fixed and occurs only when needed, the majority had a frequency greater than once a week during the observation period. This was even more true for the RP (remote programming) group, indicating that the actual demand for programming is greater than what patients themselves think. In summary, the remote programming system presents a high level of usability (98%) and willingness (satisfaction rate: 96.83%) in result of questionnaire. (Table 2)
Table 2.
The result of self-made survey.
| RP group (n=32) | OC group (n=31) | ||||||
|---|---|---|---|---|---|---|---|
| Item | Category | n | % | n | % | χ2 | p |
| Cost of outpatient programming at the hospital (in RMB yuan) | about 0 | 9 | 28.13 | 12 | 38.71 | 13.35 | 0.02 |
| <500 | 5 | 15.63 | 12 | 38.71 | |||
| 500–2000 | 17 | 53.13 | 4 | 12.90 | |||
| 2000–5000 | 0 | 0.00 | 1 | 3.23 | |||
| 5000–10 000 | 1 | 3.13 | 1 | 3.23 | |||
| >10 000 | 0 | 0.00 | 1 | 3.23 | |||
| Duration of outpatient programming at the hospital | 0–30 min | 7 | 21.88 | 3 | 9.68 | 3.40 | 0.49 |
| 30 min–12 h | 19 | 59.38 | 25 | 80.65 | |||
| 12–24 h | 2 | 6.25 | 1 | 3.23 | |||
| 24–48 h | 2 | 6.25 | 1 | 3.23 | |||
| ≥48 h | 2 | 6.25 | 1 | 3.23 | |||
| Reasons for requesting remote programming (multiple choices) | Regular follow-up | 6 | 18.75 | 6 | 19.35 | 10.40 | 0.02 |
| Symptoms recurring/no improvement | 12 | 37.50 | 17 | 54.84 | |||
| Seeking further improvement | 14 | 43.75 | 4 | 12.90 | |||
| Discomfort or side effects | 0 | 0.00 | 4 | 12.90 | |||
| Frequency of programming | Less than once a week | 1 | 3.13 | 1 | 3.23 | 8.95 | 0.06 |
| Once a week | 6 | 18.75 | 0 | 0.00 | |||
| Once per 1–3 week | 1 | 3.13 | 1 | 3.23 | |||
| A month or more | 2 | 6.25 | 0 | 0.00 | |||
| Not fixed, as needed | 22 | 68.75 | 29 | 93.55 | |||
| Reasons for choosing remote programming (multiple choices) | Professional, expert-level service | 14 | 43.75 | 10 | 32.26 | 0.61 | 0.43 |
| Convenient for adjustments | 18 | 56.25 | 23 | 74.19 | 1.51 | 0.22 | |
| Time and cost-saving | 23 | 71.88 | 23 | 74.19 | 0.00 | 1.00 | |
| Improved effectiveness | 11 | 34.38 | 9 | 29.03 | 0.03 | 0.85 | |
| Reduced travel due to pandemic reasons | 10 | 31.25 | 8 | 25.81 | 0.04 | 0.84 | |
| Can you understand the operation process and use the remote | I cannot understand or use it | 1 | 3.13 | 0 | 0.00 | 2.64 | 0.27 |
| I can understand and use it according to the instructions | 27 | 84.38 | 23 | 74.19 | |||
| I am very familiar with it | 4 | 12.50 | 8 | 25.81 | |||
| Level of satisfaction with the remote programming platform | Not satisfied | 2 | 6.25 | 0 | 0.00 | 6.32 | 0.10 |
| Basically satisfied | 9 | 28.13 | 3 | 9.68 | |||
| Satisfied | 8 | 25.00 | 13 | 41.94 | |||
| Very satisfied | 13 | 40.63 | 15 | 48.39 | |||
| Would you recommend the remote programming platform to other | Might not | 3 | 9.38 | 0 | 0.00 | 7.35 | 0.06 |
| Not sure | 5 | 15.63 | 2 | 6.45 | |||
| Might do | 0 | 0.00 | 3 | 9.68 | |||
| Definitely will | 24 | 75.00 | 26 | 83.87 | |||
OC, outpatient control; RP, remote programming.
Baseline symptoms
Through the standard urination diary, researchers have recorded the basic urination conditions of patients before surgery. The results showed that the median daily urination frequency is around seven times per day, and the median volume per urination is 170 ml. The median OBASS is 4–5 points, while the median QoL remains at around 2–3 points. During the baseline period, there was no statistically significant difference between the two groups in the above data. Interestingly, the baseline ICSI/ICPI scores for the RP group seemed higher than the OC group (median values 21.5 vs. 11 P=0.001). (supplement Table 1, Supplemental Digital Content 1, http://links.lww.com/JS9/B826).
Symptom improvement
Symptom score scales were collected again from each patient at the end of the observation period (Supplementary Table 1, Supplemental Digital Content 1, http://links.lww.com/JS9/B826). Due to the difference in ICSI/ICPI between the two groups at baseline, the researchers decided to investigate the relationship between programmed mode and patient symptom improvement by examining the changes in the score scales before and after the observation period. The findings indicated a marginal enhancement in urinary symptoms, particularly in pain (median ΔVAS RP vs. OC=−1 vs. 0, P=0.164) and urgency (median ΔOBASS −2.5 vs. −1, P=0.229). Despite this, it’s essential to note that these disparities did not attain statistical significance. And RP did not significantly impact the quality of life of patients (P=0.113) (Table 3). On the other hand, there was a more notable improvement in ICSI/ICPI in the RP group (median −2 vs. −13.5, P=0.015). We wondered if this was because the RP group included 7 IC patients. To this end, we conducted a subgroup analysis. The results showed that after excluding IC patients, there was no significant difference between the two groups at baseline(median ICSI/ICPI RP vs. OC=5 vs. 3, P=0.07) and in the change values(median ΔICSI/ICPI RP vs. OC=5 vs. 6, P=0.70) (Supplementary Table 2, Supplemental Digital Content 1, http://links.lww.com/JS9/B826, 4, Supplemental Digital Content 1, http://links.lww.com/JS9/B8, 5, Supplemental Digital Content 1, http://links.lww.com/JS9/B826), which confirmed our assumption.
Table 3.
The change value of certain urinary indices before and after the observational period.
| OC group (n=31) | RP group (n=32) | |||||||
|---|---|---|---|---|---|---|---|---|
| Median | q1 | q3 | Median | q1 | q3 | Z | p | |
| Average urination frequency per day | 0.000 | −4.000 | 2.000 | −2.500 | −9.500 | 0.000 | −1.862 | 0.063 |
| Average urine volume per void | 63.000 | 10.000 | 90.000 | 34.000 | 11.500 | 83.750 | −0.674 | 0.500 |
| Urgency score | 0.000 | −2.000 | 0.000 | −1.000 | −2.000 | 0.000 | −0.678 | 0.498 |
| Average incontinence episodes | 0.000 | −1.000 | 0.000 | 0.000 | −0.875 | 0.000 | −0.408 | 0.683 |
| Average incontinence volume | 0.000 | −3.000 | 0.000 | 0.000 | 0.000 | 0.000 | −0.664 | 0.507 |
| VAS | 0.000 | 0.000 | 0.000 | −1.000 | −5.000 | 0.000 | −1.391 | 0.164 |
| QoL | 2.000 | 1.000 | 3.000 | 1.500 | 1.000 | 2.000 | −1.010 | 0.313 |
| OBASS | −1.000 | −4.000 | 0.000 | −2.500 | −6.500 | 0.000 | −1.204 | 0.229 |
| ICSI/ICPI | −2.000 | −5.000 | 0.000 | −13.50 | −23.75 | −0.250 | −2.428 | 0.015 |
ICSI/ICPI, Interstitial Cystitis O’Leary-Sant Symptom and Problem Index; OBASS, Overactive Bladder Awareness and Symptom Score; OC, outpatient control; QoL, Voiding Symptom Quality of Life Questionnaire; RP, remote programming; VAS, visual analogue scale.
Final
Upon completion of the observation period, we collected pertinent patient-controlled data. The median observation period for both groups of patients is 28 days, with no significant differences(P=0.861). The data indicate that the voltage utilized in the OC group was slightly higher (P=0.04), whereas there were no significant differences in terms of pulse interval and frequency. Furthermore, there were no noticeable differences between the two groups in terms of phase-two conversion rate (P= 0.926), suggesting that remote patient-controlled interventions possess conversion capabilities akin to those in outpatient settings. (Supplementary Table 3, Supplemental Digital Content 1, http://links.lww.com/JS9/B826)
Discussion
Sacral nerve modulation therapy, as a first-line treatment for refractory neurogenic lower urinary tract dysfunction, has gained widespread promotion and application worldwide over the past decade, bringing significant clinical benefits to a large number of patients15–17. However, conventional sacral nerve modulation therapy is primarily conducted through in-person programming, requiring patients to visit a healthcare facility for each adjustment. In China, most centres with authoritative qualifications for sacral nerve modulation therapy are located in major eastern cities, which imposes a significant financial burden on many patients suffering from the condition. This, to some extent, reduces their willingness to undergo in-person programming.
Currently, there have been global efforts to implement remote programming for sacral neuromodulation therapy. However, these studies predominantly focus on patients after permanent implant and are often retrospective in nature14,18,19. Concerning SNM patients after Stage I surgery, while foundational research has explored remote programming techniques, there’s a significant absence of clinical studies reporting on the remote programming for this specific patient cohort. To the best of our knowledge, the presented study is the first multicenter research focusing on the remote programming of Stage I SNM patients. In our team’s previous research, we found that remote programming might help address the aforementioned problem10. However, most of these studies were retrospective, and as far as we know, patients receiving sacral nerve modulation therapy are predominantly those with refractory lower urinary tract dysfunction, often accompanied by intense subjective symptoms such as voiding difficulty, urinary frequency, and pain. Prior research has shown significant discrepancies between retrospective subjective data and real-time semi-objective data, likely due to patients’ tendency to embellish or exaggerate their recollections20,21. Additionally, previous studies mainly focused on patients with permanent implants who require fewer programming adjustments, making remote programming less beneficial10. Therefore, we designed a prospective case-control study, focusing on patients in the observation period following stage I implantation surgery, who frequently require programming adjustments to find suitable parameters. This study explores whether they can benefit from remote programming, and to our knowledge, it represents the first prospective multicenter clinical study in this regard.
Based on preliminary research, the study included 63 participants and six participating centres, which are primarily distributed in eastern, central, and northern China, representing the highest level of sacral nerve modulation therapy in the country. This ensures that patients get the right level of treatment and accurately reflects the diversity of the patient population. Our results indicate that the included patients are primarily those with neurogenic lower urinary tract dysfunction (NLUTD), IC, and overactive bladder (OAB), with NLUTD being the most prevalent. This contrasts with what was observed in our previous studies9. We speculate that this difference may be attributed to the fact that patients willing to participate in the study may generally have more severe symptoms compared to other populations, thereby altering the distribution of the diseases. It could also be a result of the relatively small sample size. We will endeavour to explore this issue further in future research studies.
From a results perspective, remote programming achieved similar efficacy and user experience as in-person programming. Both important subjective symptom assessment scales and semi-objective voiding diaries showed similar changes between the two groups. Notably, patients in the remote programming group exhibited a more pronounced decrease in ICSI/ICPI scores. Further analysis revealed that this was mainly due to the presence of seven patients with IC in the RP group. Unfortunately, IC patients were not included in the OC group to explore the effects of RP on this specific population. However, upon analyzing the indicators in the RP group specifically among patients with IC, we observed that despite IC patients showing a greater degree of improvement in indicators compared to patients with other diagnoses in the same group, the comparison of efficacy indicators between the RP and OC groups, after excluding IC patients, still leads to similar conclusions. However, through a comparison with retrospective data from IC patients receiving conventional programming, we found that IC patients using remote programming may experience greater symptom improvement, suggesting that IC patients may have a higher programming demand.
In other results, our questionnaire survey showed that a significant proportion came from rural areas. And the survey also indicated that most patients chose to undergo sacral nerve modulation therapy due to refractory NLUTD, aligning with previous research10. The economic cost of programming for most patients was not as high as initially imagined, but the time cost was substantial, underscoring the significant practical value of remote programming. Based on the experience of the remote programming system, the majority of participants reported that the remote system was a safe and satisfactory solution, worthy of wider adoption.
Additionally, technology is also one of the crucial factors influencing patients’ choice of remote programming. The remote programming system used in this study is derived from the classical face-to-face programming technology. Therefore, the two programming technologies show no significant differences in daily portability and usage. (Supplement Table 6, Supplemental Digital Content 1, Supplemental Digital Content 1, http://links.lww.com/JS9/B826) However, compared to clinic-based programming, remote programming requires a wired or wireless network technically, and patients have additional tasks: (1) using the patient-side programming app and (2) precisely describing their sensations regarding programming. Our survey results indicate that the majority of patients can use this system with guidance.
Nevertheless, it’s important to note that there is still a very small percentage of patients facing accessibility issues with remote programming due to technical reasons. We look forward to further improvements in the future. Nevertheless, our study still has room for improvement. Firstly, IC patients were not included in the OC group, and while we supplemented retrospective data for comparison, there may still be some bias. Secondly, despite addressing issues such as the lack of comparison with traditional programming and the absence of before-and-after symptom improvement comparisons compared to our previous study, the current research only collected subjective data such as symptom questionnaires. Since this study is mainly observational, we did not conduct invasive examinations like urodynamic studies before and after patient treatment. However, the study has demonstrated that remote programming is not inferior to in-person programming. In future research, if patients require urodynamic studies, we will conduct more in-depth exploration of the objective effects of remote programming.
Furthermore, it is important to note that this study primarily focused on the effectiveness of remote teleoperation, assessed through user satisfaction. Detailed comparative research on the technical aspects of remote teleoperation was not conducted, potentially limiting the broader application and further exploration of this technology. We acknowledge this limitation and plan to undertake more in-depth investigations in the future.
For similar reasons, real-time recording of all remote teleoperation parameters, such as feeling points and voltage, during the entire patient trial period was not implemented in this study. Only the final parameters were collected. While this may have limitations, the outcomes could prove beneficial for the clinical application of remote teleoperation.
In an upcoming study, soon to be published, we have summarized the parameter characteristics used by all patients transitioning to the second phase. We hope that this compilation will contribute to the wider adoption of this technology. Our commitment to advancing this research remains unwavering, and we plan to continually progress in this field.
Conclusion
Through clinical implementation and patient feedback, this study formally demonstrates that remote programming is not inferior to in-person programming in terms of success rate, effectiveness, safety, and patient satisfaction. It supports the significant potential for the development and application of remote programming services for patients after Stage I surgery, which can provide efficient, cost-effective, and convenient programming services for a broader range of sacral nerve modulation patients.
Ethical considerations
This study has undergone ethical review at Beijing Hospital and the various research unit subcenters, with an ethics approval number of 2020BJYYEC07802. Informed consent will be obtained from all study participants.
Consent
Written informed consent has been obtained from the patient for the publication of this research and accompanying images. A copy of this written consent is available for review upon request by the Editor-in-Chief of the journal.
Sources of funding
This research is supported by the National High-Level Hospital Clinical Research Funding (BJ-2021- 184 and BJ-2023-099).
Author contribution
J.J. contributed to the project by performing writing, formal analysis, investigation, and data curation. M.L. played a role in conceptualization, project administration, and securing funding for the research. Z.Y. contributed to the project by providing supervision and expertise in methodology. W.X. was involved in investigation and validation of the research. Z.W. participated in the investigation and provided necessary resources. W.Q. contributed to the project by providing supervision and guidance. L.L. played a role in the investigation and contributed to the allocation of resources. S.W. was involved in the investigation and provided necessary resources. Z.Y. contributed to the investigation and provided resources for the project. L.Y. participated in the investigation and allocation of resources. N.J. was involved in the investigation phase of the project. W.H. participated in the investigation phase of the project. All authors declare that this manuscript is original, has not been published before and is not currently being considered for publication elsewhere. We confirm that the manuscript has been read and approved by all named authors and that there are no other persons who satisfied the criteria for authorship but are not listed. We further confirm that the order of authors listed in the manuscript has been approved by all of us. We understand that the Corresponding Author is the sole contact for the Editorial process. He/she is responsible for communicating with the other authors about progress, submissions of revisions and final approval of proofs.
Conflicts of interest disclosure
The authors declare that there is no conflict of interest to disclose.
Research registration unique identifying number (UIN)
This study is registered with the China Clinical Trial Center, with registration number ChiCTR2000036677.
Guarantor
Zhang Yaoguang.
Data collection
Data were collected from [patients, medical records, surveys] between 2022.08.01] and [2023.06.30]. Data will include information on [demographics, medical history, exposure variables, Lower Urinary Tract Dysfunction (LUTD) and primarily includes the following: Standard voiding diary; Visual analogue scale (VAS); Overactive Bladder Symptom Score (OABSS); Voiding Symptom Quality of Life Questionnaire (QoL); Interstitial Cystitis O’Leary-Sant Symptom and Problem Index (ICPI&ICSI)].
Data sources: study population
The study population were patients who met the diagnostic criteria for refractory Lower Urinary Tract Dysfunction (LUTD) and willingly participated in the study after providing informed consent.
Data handling and management
Data will be collected and managed using [Excel]. All data will be stored securely to maintain confidentiality and privacy.
Data analysis
Data analysis will be performed using IBM SPSS Statistics 19.0.0.329. Statistical tests and methods will include [Descriptive statistical methods were used to analyze baseline data to understand the characteristics of the two patient groups. For continuous variables that followed a normal distribution, mean and standard deviation were presented, and t-tests were used for comparisons. For variables that did not follow a normal distribution, median and interquartile range were presented, and the Mann–Whitney U test was used for group comparisons. Categorical variables were presented as counts (percentages), and χ2 tests were used for between-group comparisons.
Data sharing
The data used to support the findings of this study are available upon request from the corresponding author. The data are not publicly available due to privacy and ethical considerations. Requests for access to the data should be directed to corresponding author.
Data statement last updated:
This data statement was last updated on [2023.08.31].
Data availability statement
The data used to support the findings of this study are available upon request from the corresponding author. The data are not publicly available due to privacy and ethical considerations. Requests for access to the data should be directed to corresponding author.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Supplementary Material
Footnotes
Sponsorships or competing interests that may be relevant to content are disclosed at the end of this article.
Supplemental Digital Content is available for this article. Direct URL citations are provided in the HTML and PDF versions of this article on the journal’s website, www.lww.com/international-journal-of-surgery.
Published online 7 February 2024
Contributor Information
Jibo Jing, Email: jibojing@outlook.com.
Lingfeng Meng, Email: menglfdzs@163.com.
Yaoguang Zhang, Email: zhang003887@sina.com;172097006@qq.com.
Xinhao Wang, Email: 2111210550@stu.pku.edu.cn.
Wen Zhu, Email: 13700860013@163.com.
Qingwei Wang, Email: wangwang4677@126.com.
Li Lu, Email: luli8@mail.sysu.edu.cn.
Wei Song, Email: sdslyysw@163.com.
Yifei Zhang, Email: zhangyifei05214@163.com.
Yan Li, Email: yanli@sdu.edu.cn.
Jiaxing Ning, Email: 1084409183@qq.com.
Haoran Wang, Email: whr950716@163.com.
References
- 1.Hamid R, Averbeck MA, Chiang H, et al. Epidemiology and pathophysiology of neurogenic bladder after spinal cord injury. World J Urol 2018;36:1517–1527. [DOI] [PubMed] [Google Scholar]
- 2.Nambiar AK, Arlandis S, Bo K, et al. European Association of Urology Guidelines on the Diagnosis and Management of Female Non-neurogenic Lower Urinary Tract Symptoms. Part 1: Diagnostics, Overactive Bladder, Stress Urinary Incontinence, and Mixed Urinary Incontinence. Eur Urol 2022;82:49–59. [DOI] [PubMed] [Google Scholar]
- 3.Romo PGB, Smith CP, Cox A, et al. Non-surgical urologic management of neurogenic bladder after spinal cord injury. World J Urol 2018;36:1555–1568. [DOI] [PubMed] [Google Scholar]
- 4.Schiavina R, Brunocilla E, Martorana G. Editorial Comment from Dr Schiavina et al. to Cystectomy and urinary diversion as management of treatment-refractory benign disease: the impact of preoperative urological conditions on perioperative outcomes. Int J Urol 2014;21:387–388. [DOI] [PubMed] [Google Scholar]
- 5.Bemelmans BL, Mundy AR, Craggs MD. Neuromodulation by implant for treating lower urinary tract symptoms and dysfunction. Eur Urol 1999;36:81–91. [DOI] [PubMed] [Google Scholar]
- 6.Kessler TM, La Framboise D, Trelle S, et al. Sacral neuromodulation for neurogenic lower urinary tract dysfunction: systematic review and meta-analysis. Eur Urol 2010;58:865–874. [DOI] [PubMed] [Google Scholar]
- 7.Meng L, Tian Z, Zhang W, et al. Influence of patient sex on the effectiveness of sacral neuromodulation: a cohort study from China. Int J Surg 2020;84:13–17. [DOI] [PubMed] [Google Scholar]
- 8.Meng L, Zhang W, Zhang Y, et al. Analysis of the correlation between the clinical effect of sacral neuromodulation and patient age: a retrospective multicenter study in China. Neuromodulation 2020;23:1189–1195. [DOI] [PubMed] [Google Scholar]
- 9.Zhang P, Wang JY, Zhang Y, et al. Results of sacral neuromodulation therapy for urinary voiding dysfunction: five-year experience of a retrospective, multicenter study in China. Neuromodulation 2019;22:730–737. [DOI] [PubMed] [Google Scholar]
- 10.Meng L, Hou H, Zhang P, et al. Sacral neuromodulation remote programming in patients with refractory lower urinary tract dysfunction: China’s experience during the COVID-19 pandemic. Front Med (Lausanne) 2023;10:977433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mathew G, Agha R, Albrecht J, et al. STROCSS 2021: Strengthening the reporting of cohort, cross-sectional and case-control studies in surgery. Int J Surg 2021;96:106165. [DOI] [PubMed] [Google Scholar]
- 12.Dario A, Frigerio G. Commentary: Management of intractable pain in patients with implanted spinal cord stimulation devices during the COVID-19 pandemic using a remote and wireless programming system. Front Neurosci 2021;15:696830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Xu J, Wang J, Keith S, et al. Management of Parkinson’s disease patients after DBS by remote programming: preliminary application of single center during quarantine of 2019-nCoV. J Neurol 2021;268:1295–1303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhang Y, Zhang P, Tian X, et al. Remotely programmed sacral neuromodulation for the treatment of patients with refractory overactive bladder: a prospective randomized controlled trial evaluating the safety and efficacy of a novel sacral neuromodulation device. World J Urol 2019;37:2481–2492. [DOI] [PubMed] [Google Scholar]
- 15.Chartier-Kastler E, Normand LL, Ruffion A, et al. Sacral neuromodulation with the interstim system for overactive bladder: 3-year results from the french prospective, multicenter, observational SOUNDS Study. Eur Urol Focus 2022;8:1399–1407. [DOI] [PubMed] [Google Scholar]
- 16.Harvie HS, Amundsen CL, Neuwahl SJ, et al. Cost-effectiveness of sacral neuromodulation versus onabotulinumtoxina for refractory urgency urinary incontinence: results of the ROSETTA Randomized Trial. J Urol 2020;203:969–977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Thomas T. Sacral neuromodulation for LUTS has promising long-term outcomes. Nat Rev Urol 2021;18:72. [DOI] [PubMed] [Google Scholar]
- 18.Banakhar MA, Al-Qahtani W, Al-Shaiji TF, et al. Multicenter study for the effect of COVID-19 lockdown on patients with sacral neuromodulation implants. Neuromodulation 2022;25:1160–1164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhang Y, Meng L, Zhang P, et al. Intermediate-term results of a prospective, multicenter study on remote programming sacral neuromodulation for refractory overactive bladder. Transl Androl Urol 2021;10:1966–1975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chartier-Kastler E, Le Normand L, Ruffion A, et al. Sacral Neuromodulation with the InterStim System for Intractable Lower Urinary Tract Dysfunctions (SOUNDS): Results of Clinical Effectiveness, Quality of Life, Patient-Reported Outcomes and Safety in a French Multicenter Observational Study. Eur Urol Focus 2021;7:1430–1437. [DOI] [PubMed] [Google Scholar]
- 21.De Wachter S, Vaganee D, Kessler TM. Sacral neuromodulation: mechanism of action. Eur Urol Focus 2020;6:823–825. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data used to support the findings of this study are available upon request from the corresponding author. The data are not publicly available due to privacy and ethical considerations. Requests for access to the data should be directed to corresponding author.