TO THE EDITOR:
Chimeric antigen receptor (CAR) T-cell therapy has transformed the landscape of relapsed/refractory B-cell acute lymphoblastic leukemia (ALL) in children and young adults,1,2 with a 3-year relapse-free survival of 52% for tisagenlecleucel in the pivotal ELIANA trial.3 B-cell aplasia (BCA) is an indirect measure of anti-CD19 CAR T-cell presence. Early (≤6 months from infusion) loss of BCA (LBCA) was associated with high relapse risk in studies with tisagenlecleucel or other 41BBz anti-CD19 CAR T-cell products.4, 5, 6, 7, 8, 9 However, with different anti-CD19 CAR T cells (eg, CD28-containing brexucabtagene), the long-term persistence of CAR T cells seems not required for durable remission.10
The optimal therapeutic strategy for patients with early LBCA after tisagenlecleucel is unclear; good outcomes have been achieved with consolidative hematopoietic stem cell transplant (SCT).3,9 However, SCT is associated with significant mortality, especially for patients with prior SCT within 12 months,11 and with long-term side effects.12 Indeed, a benefit of consolidative SCT after CAR T-cell therapy has not been demonstrated for patients who have received prior transplant.13 Moreover, not all patients have a suitable donor, and some are precluded from SCT because of comorbidities. At our center, children who received tisagenlecleucel and presented with early LBCA with a contraindication to SCT were treated with a maintenance chemotherapy regimen for 2 years, with promising early outcomes.14 Here, we report on the longer follow-up of a larger cohort of children and young adults from across the United Kingdom receiving maintenance chemotherapy or SCT after early LBCA.
We retrospectively collected data of patients treated either with tisagenlecleucel or experimental 41BBz anti-CD19 and anti-CD19/anti-CD22 CAR T cells (NCT02443831) in the United Kingdom from June 2017 to June 2022. The data cut-off date was 20 March 2023. Data were collected on a health service evaluation basis, on the basis of outcome assessment after CAR T-cell therapy. Consent for data collection was obtained from patients, parents, or legal guardians. Inclusion criteria were early LBCA (≤6 months from infusion) without evidence of disease, defined as morphological complete remission (CR) and negative measurable residual disease (MRD) by polymerase chain reaction analysis. LBCA was defined as peripheral B-cell count ≥ 0.10 × 109/L and/or bone marrow CD19+ events ≥ 0.1%, measured on >1 occasion, at least 2 weeks apart. Peripheral lymphocyte subsets were monitored monthly, whereas marrow aspirate was checked at 1, 3, 6, 9, and 12 months after CAR T-cell infusion. MRD negativity was defined at a lower limit of at least 1 × 10−4 by polymerase chain reaction for leukemia-specific immunoreceptor gene rearrangements. Maintenance was administered as per the United Kingdom National Randomised Trial For Children and Young Adults with Acute Lymphoblastic Leukaemia and Lymphoma 2011 (UKALL2011) protocol (European Union Drug Regulating Authorities Clinical Trials Database, number 2010-020924-22): oral mercaptopurine (75 mg/m2 daily) with weekly oral methotrexate (20 mg/m2) and 3-monthly intrathecal methotrexate (age-adjusted doses) for 2 years. Patients were also treated with or without monthly pulses (vincristine 1.5 mg/m2 IV, day 1; dexamethasone 6 mg/m2 per day, days 1-5), depending on prior toxicity to these agents. Allogeneic SCT was performed according to institutional guidelines and donor availability.
Categorical variables were compared using 2-tailed Fisher test, and continuous variables using the Wilcoxon test for unpaired data. Survival was calculated by Kaplan-Meier analysis and group comparison by log-rank test. Overall survival (OS) was defined as the time from LBCA to death, and patients were censored at the last follow-up. Event-free survival (EFS) was defined as the time from LBCA to death or relapse, whichever occurred first. Significance was set at a P value < .05 (2-sided).
We retrospectively collected data of pediatric and young adult patients (aged ≤25 years) treated in the United Kingdom for ALL with tisagenlecleucel, AUTO1, or AUTO1/22 (experimental 41BBz anti-CD19 or anti-CD19-CD22 CAR T-cell product, respectively, NCT02443831). Of 151 patients who received CAR T-cell infusion (125 with tisagenlecleucel, 14 with AUTO1, and 12 with AUTO1/22), 137 (90.7%; 115 receiving tisagenlecleucel, 12 receiving AUTO1, and 10 receiving AUTO1/22) achieved CR with the onset of BCA and were evaluable for longer term outcomes. Of these patients, 32 patients (21.2%; 27 receiving tisagenlecleucel, 3 receiving AUTO1, and 2 receiving AUTO1/22) developed early LBCA with no evidence of detectable disease. For 11 of 32 patients (34.3%), allogeneic SCT was undertaken, 8 patients (25%) were started on maintenance therapy, 6 (18.7%) had no further therapy, 4 (12.5%) received a second tisagenlecleucel infusion, 2 (6.2%) had other treatment, and 1 (3%) had missing data. Of the 6 patients who received no immediate treatment for early LBCA, 5 had a frank relapse: 2 are alive in CR, 2 died of disease, and 1 died after achieving another remission (supplemental Table).
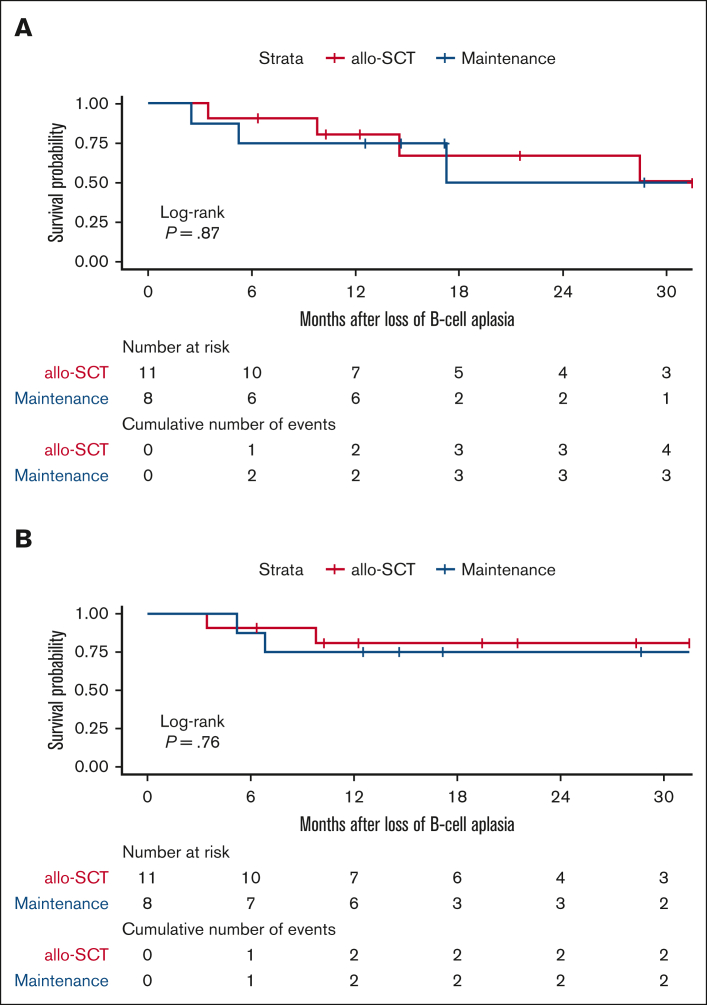
For the purposes of this report, the study population comprised the 11 patients who received SCT and the 8 patients who received maintenance. This cohort included 17 patients receiving tisagenlecleucel and 2 receiving experimental CAR T-cell products (1 receiving AUTO1 and 1 receiving AUTO1/22). Reasons for being treated with maintenance rather than SCT were prior total body irradiation–based SCT (3 patients), absence of a well-matched SCT donor (2 patients), patient comorbidities (2 patients), and family preference (1 patient). The baseline characteristics of patients in each treatment cohort were well matched (Table 1). All patients achieved complete remission with incomplete hematologic recovery (CR/CRi) on day 30 after CAR T-cell infusion, and the median time to LBCA was similar in the 2 cohorts. Median follow-up time from LBCA was 21.5 months (95% confidence interval [CI], 12.3 to not reached) for the SCT and 23 months (95% CI, 14.7 to not reached) for the maintenance group. There was no significant difference between the survival of patients receiving either SCT or maintenance: the 1-year OS rate was 80.8% (95% CI, 60-100) and 75% (95% CI, 50.3-100), respectively; the 1-year EFS rate was 80.8% (95% CI, 60-100) and 75% (95% CI, 50.3-100), respectively (P > .05; Figure 1). In the SCT group, 2 patients relapsed with CD19− disease, 1 and 2 years after SCT, respectively, and both patients are alive, receiving further treatment. Two patients died of transplant-related mortality (TRM). Seven patients (63.6%) remain alive in molecular remission without further treatment. In the maintenance group, 3 of 8 patients (37.5%) relapsed with CD19+ disease at a median 76 days (95% CI, 60 to not reached) after LBCA: 1 patient received transplantation, had a further relapse, and is currently alive with disease; 2 patients died of disease; and no patient died of treatment-related toxicity. Five patients (62.5%) remain alive in molecular remission: 2 have completed 2 years of maintenance, and 3 remain on maintenance therapy. Of these patients, 4 had favorable cytogenetics (ETV6-RUNX1, n = 1 and high hyperdiploidy, n = 3), 1 patient had KMT2A rearrangement, and 1 patient had complex cytogenetics.
Table 1.
Characteristic of patients, disease, and treatment
| Variable | Total treated cohort, N = 19 |
Allogeneic SCT cohort, n = 11 |
Maintenance therapy cohort, n = 8 |
P | |||
|---|---|---|---|---|---|---|---|
| N or median | % or IQR | n or median | % or IQR | n or median | % or IQR | ||
| Male | 6 | 31.60% | 3 | 27.30% | 3 | 37.5% | 1 |
| Age at CAR T-cell infusion, y | 7.9 | 6.1-12.6 | 7.9 | 6.3-12.8 | 8.75 | 4.9-12.2 | .8043 |
| Characteristics of initial diagnosis | |||||||
| Infant ALL, n | 3 | 15.80% | 1 | 9.10% | 2 | 25% | .5459 |
| Median WCC (x 109/L) | 10 | 9.4-99.8 | 10 | 9.9-44 | 40 | 8.5-128.5 | .8729 |
| NCI risk | |||||||
| High | 7 | 36.80% | 2 | 27.30% | 4 | 50% | .37 |
| Standard | 9 | 47.40% | 7 | 54.50% | 3 | 37.50% | |
| Not known | 3 | 15.80% | 2 | 18.20% | 1 | 12.50% | |
| Cytogenetic risk | |||||||
| Good risk (total) | 9 | 47.40% | 5 | 45.50% | 4 | 50% | 1 |
| G ood risk (ETV6-RUNX1) | 3 | 15.80% | 2 | 18.20% | 1 | 12.50% | |
| Good risk (high hyperdiploid) | 6 | 31.60% | 3 | 27.30% | 3 | 37.50% | |
| Intermediate risk (total) | 1 | 5.30% | 1 | 9.10% | 0 | ||
| Intermediate risk (IKZF1 deletion) | 1 | 5.30% | 1 | 9.10% | 0 | ||
| High risk (total) | 5 | 26.30% | 3 | 27.30% | 2 | 25% | |
| High risk (KMT2Ar) | 3 | 15.80% | 1 | 9.10% | 2 | 25% | |
| High risk (BCR-ABL) | 1 | 5.30% | 1 | 9.10% | 0 | ||
| High risk (t(17;19)/TCF3-HLF) | 1 | 5.30% | 1 | 9.10% | 0 | ||
| Uninformative cytogenetics | 4 | 21.10% | 2 | 18.20% | 2 | 25% | |
| Unknown | 1 | 5.30% | 1 | 9.10% | 0 | ||
| Other | 3 | 15.80% | 1 | 9.10% | 2 | 25% | |
| Characteristics of relapsed/refractory disease | |||||||
| Indication for CAR T-cell therapy | |||||||
| Primary refractory | 1 | 5.30% | 1 | 9.10% | 0 | 1 | |
| Relapse | 18 | 94.70% | 10 | 90.90% | 8 | 100% | |
| Refractory status at any time point | 11 | 57.90% | 7 | 63.60% | 4 | 50% | .6577 |
| Prior therapy | |||||||
| Median number of relapses | 1 | 1.0-2.0 | 1 | 1.0-1.5 | 1.5 | 1.0-2.0 | .2754 |
| CNS and extramedullary disease | |||||||
| CNS at any point | 11 | 57.90% | 5 | 45.50% | 6 | 75% | .3521 |
| EM non-CNS relapses (both isolated and combined) | 2 | 10.50% | 1 | 9.10% | 1 | 12.50% | 1 |
| Median number of previous therapy lines (excluding SCT) | 2 | 2.0-2.0 | 2 | 2.0-2.0 | 2 | 2.0-2.2 | .7737 |
| Prior SCT | 5 | 26.30% | 2 | 18.20% | 3 | 37.50% | .6027 |
| Blinatumomab exposure | 4 | 21.10% | 1 | 9.10% | 3 | 37.50% | .2621 |
| Inotuzumab exposure | 1 | 5.30% | 0 | 1 | 12.50% | .4211 | |
| CAR T-cell therapy | |||||||
| Status before lymphodepletion | |||||||
| High disease burden (≥5%) | 3 | 15.80% | 2 | 18.20% | 1 | 12.50% | 1 |
| Low disease burden (<5%) | 11 | 57.90% | 6 | 54.60% | 5 | 62.50% | |
| Undetectable by MRD | 5 | 26.30% | 3 | 27.30% | 2 | 25% | |
| CAR T-cell product | |||||||
| Tisagenlecleucel | 17 | 89.50% | 10 | 90.90% | 7 | 87.50% | 1 |
| Experimental | 2 | 10.50% | 1 | 9.10% | 1 | 12.50% | |
| Median CAR T-cell dose, cells per kg, (n = 17) | 2.7 × 106 | 1.8-3.7 x 106 | 3.4 × 106 | 2.5-4.3 x 106 | 2.4 × 106 | 1.5-2.8 x 106 | .2069 |
| Time to LBCA | |||||||
| Median (months) | 2.66 | 95% CI : 2.3-3.6 | 2.66 | 95% CI : 2.07 to NR | 2.64 | 95% CI : 2.3 to NR | .9 |
| 0-3 months | 13 | 68.4% | 7 | 63.60% | 6 | 75% | 1 |
| 3-6 months | 6 | 31.60% | 4 | 34.4% | 2 | 25% | |
| Post–CAR T-cell treatment | |||||||
| Median time from LBCA to SCT (mo) | 2.4 | 1.7-4.5 | 1 | ||||
| SCT conditioning | |||||||
| TBI-based | 8 | 72.7% | |||||
| Non-TBI | 3 | 27.30% | |||||
| SCT donor | |||||||
| MUD | 7 | 72.70% | |||||
| MMUD (UCB) | 1 | 9.00% | |||||
| MSD | 2 | 18.20% | |||||
| Haplo | 1 | 9.00% | |||||
| Maintenance with VCR/Dexa pulses | |||||||
| Yes | 4 | 50% | |||||
| No | 4 | 50% | |||||
CNS, central nervous system; Dexa, dexamethasone; EM, extramedullary; Haplo, haploidentical; IQR, interquartile range; MMUD, mismatched unrelated donor; MRD minimal residual disease; MSD, matched sibling donor; MUD, matched unrelated donor; NCI, National Cancer Institute; NR, not reached; TBI, total body irradiation; UCB umbilical cord blood; VCR, vincristine; WCC, white blood cell count.
Figure 1.
Oucomes for children with early loss of B-cell aplasia following CAR T according to further therapy (maintenance vs stem cell transplantation). EFS (A) and OS (B) for patients treated with allogeneic SCT (red line) or maintenance therapy (blue line) for early LBCA after CAR T-cell treatment.
Early LBCA after tisagenlecleucel is associated with a high risk of relapse: cumulative incidence of CD19+ relapse approached 65% at 2 years in a French cohort,7 whereas the 2-year EFS rate was 15% for patients with LBCA of <6 months in a recent study.5 Treatment strategies for this group remain limited. Infusion of a further dose of the same CAR T-cell product reinduced BCA in approximately half of patients without detectable disease, but the 3-year disease-free survival rate was only 33%.15 Most patients have been treated with SCT in this context. A study from the National Institute of Health reported a 5-year EFS rate of 61.9% in 21 patients who received consolidative SCT after nonpersisting CD28z anti–CD19 CAR T cells.9 However, whether SCT confers a definitive survival advantage in this setting remains unclear. A Seattle group reported that SCT led to improved disease-free survival among 23 patients, with short persistence of experimental 41BBz anti-CD19 CAR T cells; however, this did not translate into a better OS, and the benefit of consolidative SCT was only seen for patients without a prior history of SCT.13
In a single-center setting, we noted preliminary good outcomes from maintenance therapy for patients with a contraindication to SCT.14 As a UK pediatric ALL CAR T-cell consortium, we therefore collected data on patients with early LBCA to compare the impact of maintenance vs SCT. Our analysis shows that maintenance was a safe alternative for these patients. Despite a slightly higher number of relapses in the maintenance group, there were no TRM events in this group, compared with 2 TRM deaths after SCT. As a result, both groups had similar OS and EFS. This highlights the toxicity of SCT in patients who are heavily pretreated.
Maintenance was well tolerated, low cost, easy to deliver, and with a good quality of life reported informally by patients and their families. Because of the small size of the cohort, it was not possible to identify predictive factors for patients with a good outcome from maintenance, for example, characteristics suggesting particularly chemotherapy-sensitive disease; however, 4 of 6 patients had good risk cytogenetics at diagnosis.
Our preliminary study is limited by the retrospective design and, despite being population-based, by the small cohort size; moreover, we recognize that longer term follow-up will be needed to capture late relapses seen in some genetic subtypes, for example, ETV6-RUNX1 and high hyperdiploid ALL.
Our data show that maintenance chemotherapy could have a potential benefit in patients with LBCA who cannot proceed to SCT or second CAR T-cell infusion, either because of contraindications or because of limited resources. A prospective clinical trial comparing SCT vs maintenance therapy is needed to clearly define outcomes of these therapies in this setting.
Conflict-of-interest disclosure: P.J.A. declares patents with and royalties from University College London Business and Autolus; received research funding from Autolus; and declares consultancy with Beam Therapeutics. S.G. received honoraria and speaker’s fees from Novartis and declares patents with and royalties from University College London Business. The remaining authors declare no competing financial interests.
Acknowledgments
Contribution: M.G., M.O.-E., P.A., and S.G. designed the research study and wrote the manuscript; M.G. and M.O.-E. collected and analyzed the data; and all authors looked after patients, provided essential data, and reviewed and approved the final manuscript.
Footnotes
M.G. and M.O.-E. are joint first authors.
P.J.A. and S.G. are joint last authors.
The data sets are available on reasonable request from the corresponding author, Sara Ghorashian (s.ghorashian@ucl.ac.uk).
The full-text version of this article contains a data supplement.
Supplementary Material
References
- 1.Maude SL, Laetsch TW, Buechner J, et al. Tisagenlecleucel in children and young adults with B-cell lymphoblastic leukemia. N Engl J Med. 2018;378(5):439–448. doi: 10.1056/NEJMoa1709866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pasquini MC, Hu Z-H, Curran K, et al. Real-world evidence of tisagenlecleucel for pediatric acute lymphoblastic leukemia and non-Hodgkin lymphoma. Blood Adv. 2020;4(21):5414–5424. doi: 10.1182/bloodadvances.2020003092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Laetsch TW, Maude SL, Rives S, et al. Three-year update of tisagenlecleucel in pediatric and young adult patients with relapsed/refractory acute lymphoblastic leukemia in the ELIANA Trial. J Clin Oncol. 2023;41(9):1664–1669. doi: 10.1200/JCO.22.00642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pillai V, Muralidharan K, Meng W, et al. CAR T-cell therapy is effective for CD19-dim B-lymphoblastic leukemia but is impacted by prior blinatumomab therapy. Blood Adv. 2019;3(22):3539–3549. doi: 10.1182/bloodadvances.2019000692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pulsipher MA, Han X, Maude SL, et al. Next-generation sequencing of minimal residual disease for predicting relapse after tisagenlecleucel in children and young adults with acute lymphoblastic leukemia. Blood Cancer Discov. 2022;3(1):66–81. doi: 10.1158/2643-3230.BCD-21-0095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Turtle CJ, Hanafi L-A, Berger C, et al. CD19 CAR-T cells of defined CD4+:CD8+ composition in adult B cell ALL patients. J Clin Invest. 2016;126(6):2123–2138. doi: 10.1172/JCI85309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dourthe M-E, Rabian F, Yakouben K, et al. Determinants of CD19-positive vs CD19-negative relapse after tisagenlecleucel for B-cell acute lymphoblastic leukemia. Leukemia. 2021;35(12):3383–3393. doi: 10.1038/s41375-021-01281-7. [DOI] [PubMed] [Google Scholar]
- 8.Mueller KT, Maude SL, Porter DL, et al. Cellular kinetics of CTL019 in relapsed/refractory B-cell acute lymphoblastic leukemia and chronic lymphocytic leukemia. Blood. 2017;130(21):2317–2325. doi: 10.1182/blood-2017-06-786129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shah NN, Lee DW, Yates B, et al. Long-term follow-up of CD19-CAR T-cell therapy in children and young adults with B-ALL. J Clin Oncol. 2021;39(15):1650–1659. doi: 10.1200/JCO.20.02262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shah BD, Ghobadi A, Oluwole OO, et al. Two-year follow-up of KTE-X19 in patients with relapsed or refractory adult B-cell acute lymphoblastic leukemia in ZUMA-3 and its contextualization with SCHOLAR-3, an external historical control study. J Hematol Oncol. 2022;15(1):170. doi: 10.1186/s13045-022-01379-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yaniv I, Krauss AC, Beohou E, et al. Second hematopoietic stem cell transplantation for post-transplantation relapsed acute leukemia in children: a retrospective EBMT-PDWP study. Biol Blood Marrow Transplant. 2018;24(8):1629–1642. doi: 10.1016/j.bbmt.2018.03.002. [DOI] [PubMed] [Google Scholar]
- 12.Holmqvist AS, Chen Y, Hageman L, et al. Severe, life-threatening, and fatal chronic health conditions after allogeneic blood or marrow transplantation in childhood. Cancer. 2023;129(4):624–633. doi: 10.1002/cncr.34575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Summers C, Wu QV, Annesley C, et al. Hematopoietic cell transplantation after CD19 chimeric antigen receptor T cell-induced acute lymphoblastic lymphoma remission confers a leukemia-free survival advantage. Transplant Cell Ther. 2022;28(1):21–29. doi: 10.1016/j.jtct.2021.10.003. [DOI] [PubMed] [Google Scholar]
- 14.Gabelli M, Oporto Espuelas M, Bonney D, et al. ALL maintenance treatment for early loss of B-cell aplasia after tisagenlecleucel therapy. Blood. 2021;138(suppl 1):3859. [Google Scholar]
- 15.Myers RM, Devine K, Li Y, et al. Outcomes after reinfusion of CD19-specific chimeric antigen receptor (CAR)-modified T cells in children and young adults with relapsed/refractory B-cell acute lymphoblastic leukemia [abstract] Blood. 2021;138(suppl 1):474. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.