Abstract
OBJECTIVE:
To examine contraceptive use among women with selected medical conditions.
METHODS:
We used a nationwide health care claims database to identify women aged 15–44 years continuously enrolled in private insurance during 2004–2011 with and without selected medical conditions. We assessed current permanent and reversible prescription contraceptive use during October 1, 2010, to September 30, 2011, with diagnosis, procedure, and pharmacy codes and calculated prevalence by age and condition. We used polytomous logistic regression to calculate odds of female sterilization or reversible prescription methods compared with neither. Among users of reversible methods, we used logistic regression to calculate odds of using long-acting reversible contraceptives compared with shorter acting methods.
RESULTS:
A low proportion of women with medical conditions were using sterilization or reversible prescription methods (45% and 30% of women aged 15–34 and 35–44 years, respectively), and this proportion was consistently lower among the older age group across all medical conditions. Across both age groups, sterilization and long-acting reversible contraceptives were used less frequently than shorter acting methods (injectable, pill, patch, or ring). The odds of sterilization were higher among women with any compared with no condition for women aged 15–34 years (odds ratio [OR] 4.9, 95% confidence interval [CI], 4.5–5.3) and 35–44 years (OR 1.2, 95% CI, 1.1–1.2). Among women using reversible prescription methods, the odds of using long-acting reversible contraceptives were increased among those with any compared with no condition for women aged 15–34 years (OR 2.2, 95% CI, 2.1–2.5) and 35–44 years (OR 1.1, 95% CI, 1.1–1.2).
CONCLUSION:
Despite the potential for serious maternal and fetal pregnancy-associated risks, contraceptive use was not optimal among women with medical conditions.
Several recent trends in the United States affect the health of reproductive-aged women. Pregnancy later in reproductive life is becoming more common,1 and such pregnancies are at higher risk for complications.2–4 Additionally, rates of certain conditions such as hypertension and diabetes are increasing among U.S. women of reproductive age and can increase the risk for pregnancy complications.3,5 Furthermore, the proportion of pregnancies that are unintended, often having negative consequences for mothers and infants, remains persistently high in the United States and is higher among adult women with medical conditions compared with women not having medical conditions.6–8 Together, these trends indicate the importance of preventing unintended pregnancy among women with medical conditions.
According to the U.S. Medical Eligibility Criteria for Contraceptive Use, 2010, highly effective contraceptive methods may be the best choice for women with conditions that place them at increased risk for adverse events if they experience an unintended pregnancy.9 Long-acting reversible contraceptive methods (LARCs), which include intrauterine devices (IUDs) and implants, may be particularly good choices because they are highly effective, require little action on the part of the user, and are generally safe for most women, including those with medical conditions.9 Nonetheless, little is known about the prevalence of contraceptive methods used among women with medical conditions.
The purpose of this analysis was to assess the contraceptive methods used among women with selected medical conditions compared with women not having those conditions, stratified by age.
MATERIALS AND METHODS
We used data from the Truven Health MarketScan Commercial Claims and Encounters databases, which contain individual-level health care claims information from employers, health plans, and hospitals.10 The databases provide information on both outpatient and inpatient health care services and linked information on filled outpatient prescription drug claims. Rigorous quality assessments, including validity and reasonableness checks, are conducted on these databases.10 Because the data are deidentified, an institutional review board of the Centers for Disease Control and Prevention determined that this was not human subjects research.
We identified current permanent or reversible prescription contraceptive use among women, with and without selected medical conditions, during the index year of interest (October 1, 2010–September 30, 2011). To account for previously initiated LARC methods or permanent methods, we included women aged 15–44 years who had been continuously enrolled in private insurance during January 2004 to September 2011. These women also were required to have health plans with available pharmaceutical data. We excluded women who had a diagnosis or procedure code for hysterectomy during 2004–2011. International Classification of Diseases, 9th Revision, Clinical Modification and Current Procedural Terminology codes were used to identify selected medical conditions from the inpatient or outpatient services databases. Medical conditions were those identified by the U.S. Medical Eligibility Criteria for Contraceptive Use9 to be associated with increased health risks from an unintended pregnancy: bariatric surgery within 2 years of the index date (October 1, 2010), breast cancer, cirrhosis, diabetes, endometrial cancer, epilepsy, human immunodeficiency virus, hypertension, ischemic heart disease, liver cancer, lupus, ovarian cancer, peripartum cardiomyopathy, schistosomiasis, sickle cell disease, stroke, thrombophilia, transplant within 2 years of the index date, trophoblastic disease, tuberculosis, and valvular heart disease. We considered women as having a medical condition during the index year if related codes were present during 2004–2011, with the exception of bariatric surgery and transplant; for these, we only considered codes within 2 years of the index year. We considered an outpatient diagnosis valid only if there were two outpatient codes present at least 30 days apart. Such an approach can increase the specificity of outpatient diagnoses by avoiding overdiagnosis of individuals evaluated for a particular condition but later deemed not to have it.11 Inpatient diagnoses were considered valid regardless of the number of times the codes were present because these diagnosis codes are assigned at the time of hospital discharge and therefore likely to represent confirmed diagnoses. For all analyses, we defined women as having any medical condition if at least one of the 21 conditions in the U.S. Medical Eligibility Criteria for Contraceptive Use was identified. We defined women as having no medical condition if none of the 21 conditions in the U.S. Medical Eligibility Criteria for Contraceptive Use was identified.
Current permanent or reversible prescription contraceptive use during the index year was identified from inpatient, outpatient, and pharmaceutical databases using International Classification of Diseases, 9th Revision, Clinical Modification diagnosis and procedure codes, Healthcare Common Procedure Coding System supply codes, Current Procedural Terminology codes, and the U.S. Food and Drug Administration’s National Drug Codes. We considered prescriptions to be a proxy measure for actual use. Contraceptive methods examined included female sterilization and reversible prescription methods such as IUDs, implants, injectables, pills, patches, and rings (Fig. 1). A woman was considered to be sterilized if a sterilization code was present in the inpatient or outpatient databases during 2004–2011. A woman was considered to be an IUD or implant user if an insertion or supply code from the inpatient or outpatient databases was present before the index year (2004–2011 for copper IUD, 2005–2011 for levonorgestrel IUD, and 2007–2011 for implant) and no removal code was found. If no sterilization, IUD, or implant codes were found, we searched for codes indicating injectable, pill, patch, or ring use and, if present, assigned classification based on the most recent code used during the index year. Injectable use was identified from inpatient and outpatient claims if there was a depot medroxyprogesterone acetate supply code or a family planning encounter diagnosis code coupled with a generic injection procedure code. Use of oral contraceptive pills (including combined and progestin-only pill), a combined hormonal patch, or a combined vaginal ring was identified by National Drug Codes in the pharmaceutical databases. If a woman’s record did not contain codes indicating female sterilization, or use of an IUD, implant, injectable, pill, patch, or ring, she was classified as using neither female sterilization nor a reversible prescription method of contraception. For reversible contraceptive methods, we classified methods into two categories based on typical effectiveness of the methods: LARC methods (IUD and implant; typical use failure rate less than 1%) and shorter acting prescription methods (injectable, pill, patch, or ring; typical use failure rate 6–9%). Both of these are more effective than nonprescription methods, which have typical use failure rates 18% or greater.12,13 We analyzed IUDs and implants together because the proportion of women using implants was low. We examined permanent and reversible contraceptive use for women without medical conditions, for women with medical conditions, and for women with nine specific conditions having sufficient sample sizes to evaluate separately (bariatric surgery, breast cancer, diabetes, epilepsy, hypertension, ischemic heart disease, lupus, stroke, and thrombophilia). For these nine conditions, we only reported cell counts that had 30 or more individuals. We excluded medical conditions for which no cell counts were 30 or greater. All analyses were stratified by age (15–34 and 35–44 years).
Fig. 1.
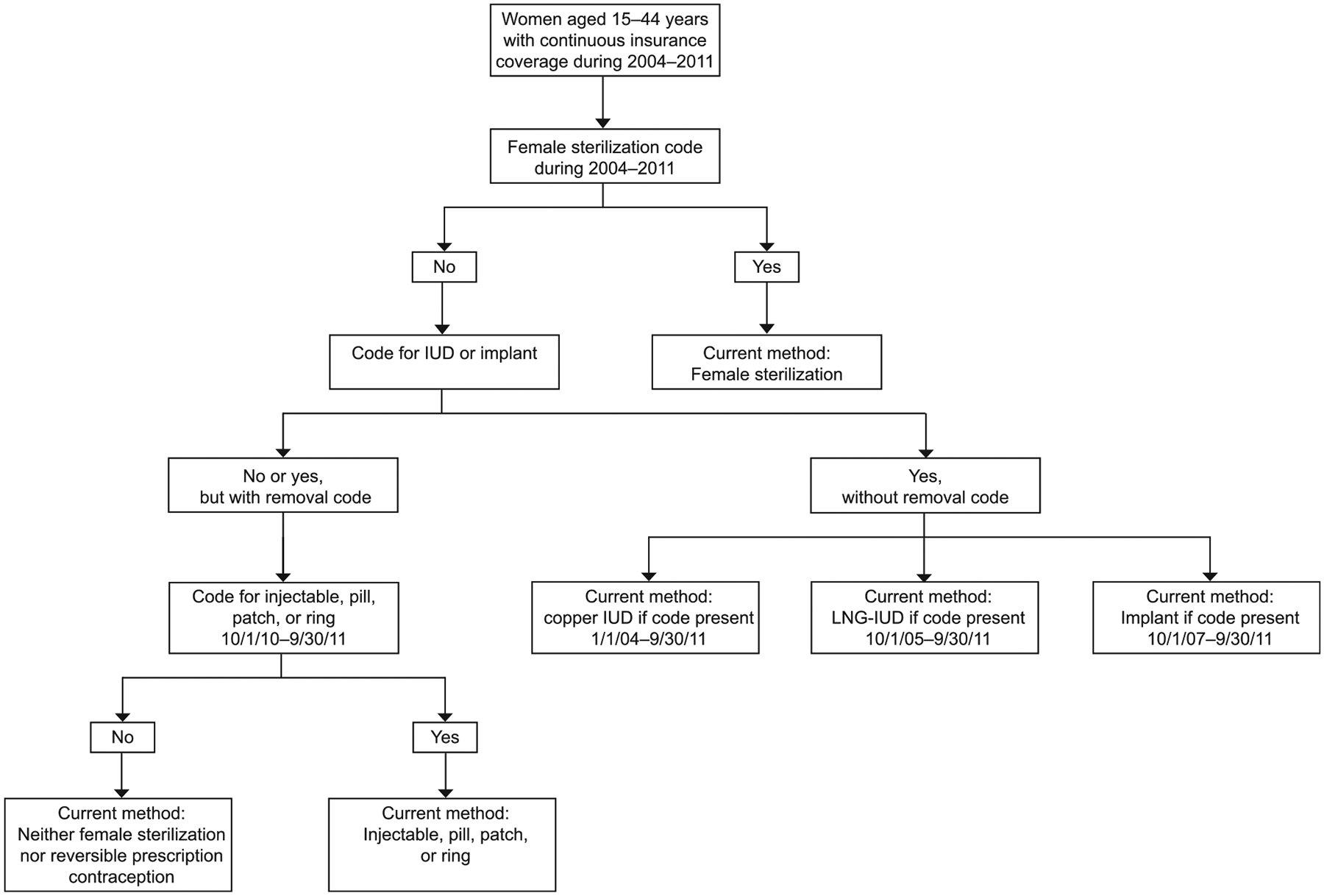
Classification of current contraceptive method. IUD, intrauterine device; LNG, levonorgestrel. Champaloux. Contraception in Women With Medical Conditions. Obstet Gynecol 2015.
We sought to examine the use of any method compared with no method as well as use of longer acting compared with shorter acting methods. We used polytomous logistic regression to calculate unadjusted odds ratios (ORs) and 95% confidence intervals (CIs) to compare use of female sterilization or reversible prescription methods (IUDs, implants, injectable, pill, patch, or ring) compared with neither female sterilization nor reversible prescription methods among women with medical conditions compared with women without medical conditions. This model included a three-level outcome: sterilization, reversible prescription methods, or neither. Among women using reversible prescription contraception, we used logistic regression to calculate unadjusted ORs and 95% CIs for use of LARCs (IUD or implant) compared with shorter acting methods (injectable, pill, patch, or ring) among women with medical conditions compared with women without medical conditions. This model included a two-level outcome: LARCs or shorter acting methods. For each regression, first we compared women with any of the selected medical conditions compared with none of the medical conditions. Then we created separate models for each medical condition compared with none of the medical conditions. SAS 9.3 was used for all analyses.
| % Using Contraceptive Methods | ||||
|---|---|---|---|---|
| Aged 35–44 Years | ||||
| n | Female Sterilization | LARC (IUD or Implant) | Injectable, Pill, Patch, or Ring | Neither Female Sterilization Nor Prescription Method |
| 163,426 | 8.2 | 5.6 | 18.1 | 68.1 |
| 129,264 | 7.9 | 5.6 | 18.7 | 67.8 |
| 34,162 | 9.4 | 5.4 | 15.6 | 69.6 |
| 25,467 | 9.4 | 5.3 | 16.6 | 68.7 |
| 8,282 | 8.9 | 4.7 | 13.9 | 72.5 |
| 1,000 | 8.7 | 4.6 | 11.5 | 75.2 |
| 1,479 | 7.2 | 6.0 | 6.8 | 79.9 |
| 1,132 | 9.7 | 6.0 | 10.0 | 74.3 |
| 1,156 | 10.1 | 7.4 | 15.8 | 66.6 |
| 1,126 | 8.0 | 4.4 | 10.2 | 77.4 |
| 869 | 6.8 | 6.6 | 12.5 | 74.1 |
| 473 | 13.3 | 8.9 | 6.8 | 71.0 |
RESULTS
Among 368,448 women aged 15–44 years with continuous enrollment in private health insurance during 2004–2011, 12% had any of the selected medical conditions; hypertension (8%) and diabetes (3%) were the most prevalent (Table 1). Among women aged 15–34 years, 3% had hypertension and 1% had diabetes. Among women aged 35–44 years, 16% had hypertension and 5% had diabetes. For all of the medical conditions examined, the prevalence was higher among women aged 35–44 years than among women aged 15–34 years with the exception of epilepsy.
Table 1.
Prevalence of Selected Medical Conditions Among Privately Insured Women Aged 15–44 Years, 2004–2011
| Medical Condition | Total (N=368,448) | Age (y) | Codes | ||
|---|---|---|---|---|---|
| 15–34 (n=205,022) | 35–44 (n = 163,426) | ICD-9-CM | CPT | ||
| Any medical condition* | 44,523 (12.1) | 10,361 (5.1) | 34,162 (20.9) | ||
| Hypertension | 30,515 (8.3) | 5,048 (2.5) | 25,467 (15.6) | 401.X-405.X | |
| Diabetes | 10,903 (3.0) | 2,621 (1.3) | 8,282 (5.1) | 250.X | |
| Epilepsy | 2,842 (0.8) | 1,842 (0.9) | 1,000 (0.6) | 345.0–345.5, 345.7–345.9 | |
| Breast cancer | 1,587 (0.4) | 108 (0.1) | 1,479 (0.9) | 233.0, 174.X, 198.81, 238.3, 239.3 | |
| Stroke | 1,612 (0.4) | 480 (0.2) | 1,132 (0.7) | 430.X-437.X | |
| Bariatric surgery within 2 y | 1,480 (0.4) | 324 (0.2) | 1,156 (0.7) | V45.86 | 43644, 43645, 43370, 43771, 43773, 43842–43843, 43845–43848, 43886–43888 |
| Ischemic heart disease | 1,298 (0.4) | 172 (0.1) | 1,126 (0.7) | 410.X-414.X | |
| Lupus | 1,270 (0.3) | 401 (0.2) | 869 (0.5) | 710.0 | |
| Thrombophilia | 735 (0.2) | 262 (0.1) | 473 (0.3) | 289.81 | |
ICD-9-CM, International Classification of Diseases, 9th Revision, Clinical Modification; CPT, Current Procedural Terminology.
Data are n (%).
Any of the 21 medical conditions identified by the U.S. Medical Eligibility Criteria for Contraceptive Use9 as placing women at increased risk for adverse events if they experience an unintended pregnancy (bariatric surgery within 2 years, breast cancer, diabetes, epilepsy, hypertension, ischemic heart disease, lupus, stroke, thrombophilia, endometrial cancer, ovarian cancer, human immunodeficiency virus, trophoblastic disease, liver cancer, peripartum cardiomyopathy, schistosomiasis, cirrhosis, sickle cell disease, transplant within 2 years, tuberculosis, and valvular heart disease).
During October 2010 to September 2011, a low proportion of younger women aged 15–34 years (40%) and older women aged 35–44 years (32%) were using female sterilization or reversible prescription methods (Table 2). These proportions were similarly low across all of the specific medical conditions examined. Among younger women, the proportion of women using female sterilization or reversible prescription contraceptive methods was higher among those with any medical condition (45%) compared with those with no medical condition (39%); the highest proportion was among women who had had bariatric surgery within the past 2 years (53%) and the lowest was among women with epilepsy (37%). Among older women, the proportion was similar among those with any (30%) compared with no (32%) medical condition; the highest proportion was among women with bariatric surgery within the past 2 years (33%), and the lowest was among women with breast cancer (20%).
Table 2.
Current Permanent or Reversible Contraceptive Use Among Women Aged 15–44 Years With and Without Selected Medical Conditions, Stratified by Age, October 2010 to September 2011
| Medical Condition | % Using Contraceptive Methods | ||||
|---|---|---|---|---|---|
| Aged 15–34 Years | |||||
| n | Female Sterilization | LARC (IUD or Implant) | Injectable, Pill, Patch, or Ring | Neither Female Sterilization Nor Prescription Method | |
| Total | 205,022 | 1.7 | 3.4 | 34.6 | 60.3 |
| No medical condition* | 194,661 | 1.5 | 3.2 | 34.7 | 60.6 |
| Any medical condition† | 10,361 | 6.5 | 6.7 | 32.1 | 54.8 |
| Hypertension | 5,048 | 9.0 | 7.6 | 32.0 | 51.3 |
| Diabetes | 2,621 | 5.5 | 4.9 | 33.6 | 56.0 |
| Epilepsy | 1,842 | 2.2 | 4.1 | 30.7 | 63.0 |
| Breast cancer | 108 | NR‡ | NR‡ | NR‡ | 60.2 |
| Stroke | 480 | 6.7 | 7.7 | 25.2 | 60.4 |
| Bariatric surgery within 2 y | 324 | NR‡ | 15.1 | 29.3 | 47.2 |
| Ischemic heart disease | 172 | NR‡ | NR‡ | 30.2 | 55.2 |
| Lupus | 401 | NR‡ | NR‡ | 29.4 | 59.4 |
| Thrombophilia | 262 | 12.2 | 14.9 | 14.9 | 58.0 |
LARC, long-acting reversible contraception; IUD, intrauterine device; NR, not reported.
None of the 21 medical conditions identified by the U.S. Medical Eligibility Criteria for Contraceptive Use9 as placing women at increased risk for adverse events if they experience an unintended pregnancy (bariatric surgery within 2 years, breast cancer, diabetes, epilepsy, hypertension, ischemic heart disease, lupus, stroke, thrombophilia, endometrial cancer, ovarian cancer, human immunodeficiency virus, trophoblastic disease, liver cancer, peripartum cardiomyopathy, schistosomiasis, cirrhosis, sickle cell disease, transplant within 2 years, tuberculosis, and valvular heart disease).
Any of the 21 medical conditions.
Not reported because of small numbers (less than 30).
Overall, shorter acting methods (injectable, pill, patch, or ring) were used more frequently than female sterilization or LARCs, except by women with thrombophilia (Table 2). Among younger women, female sterilization and LARCs were used by a higher proportion of women with any medical condition (7% for each) than those with no medical condition (2% and 3%, respectively). Among older women, the proportion using female sterilization or LARCs was similar between those with any medical condition (9% and 5%, respectively) and those with no medical condition (8% and 6%, respectively).
Among younger women, the odds of using female sterilization was 4.88 times higher (95% CI, 4.46–5.33) among those with any medical condition compared with no medical condition (Table 3). An association was also seen among women with each of the specific conditions examined with odds of using female sterilization highest among women with hypertension, diabetes, stroke, and thrombophilia. Younger women with any medical condition compared with no medical condition also had increased odds of using reversible prescription methods (OR 1.13, 95% CI, 1.08–1.18). Similar associations were found among younger women with hypertension, diabetes, and bariatric surgery within 2 years. Conversely, younger women with epilepsy compared with no medical condition had reduced odds of using reversible prescription contraception (OR 0.88, 95% CI, 0.80–0.97).
Table 3.
Odds of Using Female Sterilization or Reversible Prescription Contraception Compared With Using Neither
| Medical Condition | Aged 15–34 Years* | Aged 35–44 Years* | ||
|---|---|---|---|---|
| Female Sterilization vs Neither | Reversible Prescription Contraceptive† vs Neither | Female Sterilization vs Neither | Reversible Prescription Contraceptive† vs Neither | |
| Any medical condition‡ | 4.88 (4.46–5.33) | 1.13 (1.08–1.18) | 1.16 (1.11–1.21) | 0.84 (0.82–0.87) |
| Hypertension | 7.29 (6.55–8.10) | 1.23 (1.16–1.31) | 1.17 (1.11–1.22) | 0.89 (0.86–0.92) |
| Diabetes | 4.09 (3.43–4.87) | 1.10 (1.01–1.19) | 1.05 (0.97–1.14) | 0.72 (0.68–0.76) |
| Epilepsy | 1.43 (1.04–1.97) | 0.88 (0.80–0.97) | 0.99 (0.79–1.24) | 0.60 (0.50–0.71) |
| Breast cancer | NR§ | 0.88 (0.59–1.33) | 0.77 (0.63–0.94) | 0.45 (0.38–0.52) |
| Stroke | 4.57 (3.17–6.60) | 0.87 (0.72–1.06) | 1.12 (0.91–1.36) | 0.60 (0.51–0.71) |
| Bariatric surgery within 2 y | NR§ | 1.50 (1.20–1.89) | 1.30 (1.07–1.58) | 0.97 (0.85–1.12) |
| Ischemic heart disease | NR§ | 1.06 (0.77–1.46) | 0.88 (0.71–1.10) | 0.52 (0.44–0.62) |
| Lupus | NR§ | 0.96 (0.78–1.18) | 0.78 (0.60–1.02) | 0.72 (0.61–0.85) |
| Thrombophilia | 8.75 (5.97–12.82) | 0.82 (0.62–1.08) | 1.60 (1.22–2.10) | 0.61 (0.48–0.79) |
Data are odds ratio (95% confidence interval).
Bold indicates significant results (P<.01).
Odds ratio represents the odds of using female sterilization or a reversible prescription method (intrauterine device [IUD], implant, injectable, pill, patch, or ring) compared with neither among those with the selected medical condition compared with those without any of the 21 medical conditions.
Includes IUD, implant, injectable, pill, patch, or ring.
Any of the 21 medical conditions identified by the U.S. Medical Eligibility Criteria for Contraceptive Use9 as placing women at increased risk for adverse events if they experience an unintended pregnancy (bariatric surgery within 2 years, breast cancer, diabetes, epilepsy, hypertension, ischemic heart disease, lupus, stroke, thrombophilia, endometrial cancer, ovarian cancer, human immunodeficiency virus, trophoblastic disease, liver cancer, peripartum cardiomyopathy, schistosomiasis, cirrhosis, sickle cell disease, transplant within 2 years, tuberculosis, and valvular heart disease).
Not reported because of small numbers (less than 30).
Among older women, those with any medical condition compared with no medical condition also had increased odds of using female sterilization (OR 1.16, 95% CI, 1.11–1.21), but the magnitude of the association was smaller than for younger women (Table 3). Similar associations were found among older women with hypertension, bariatric surgery within 2 years, and thrombophilia. A reverse association was observed for women with breast cancer who had reduced odds of using female sterilization compared with women having no medical condition (OR 0.77, 95% CI, 0.63–0.94). Unlike younger women, older women with any medical condition had reduced odds of using a reversible contraceptive method compared with those having no medical condition (OR 0.84, 95% CI, 0.82–0.87). Reduced odds of using a reversible contraceptive method were also observed for each of the specific conditions examined except bariatric surgery within 2 years with odds ranging from 0.45 (95% CI, 0.38–0.52) for breast cancer to 0.89 (95% CI, 0.86–0.92) for hypertension.
Among women using reversible prescription methods, the odds of using LARCs compared with shorter acting prescription methods (injectable, pill, patch, or ring) were higher among women having any medical condition compared with women having no medical condition among those aged 15–34 years (OR 2.24, 95% CI, 2.06–2.45) and those aged 35–44 years (OR 1.14, 95% CI, 1.08–1.21) (Table 4). Among women aged 15–34 years, increased odds of using LARCs compared with shorter acting prescription methods (injectable, pill, patch, or ring) were observed for each of the specific conditions with sufficient sample sizes with the highest odds among women with hypertension, stroke, and thrombophilia. Among women aged 35–44 years, increased odds of using LARCs were observed for each of the specific conditions with the highest odds among women with breast cancer and thrombophilia.
Table 4.
Among Women Using Reversible Prescription Contraception, Odds of Using Long-Acting Reversible Contraceptives (Intrauterine Device or Implant) Compared With Other Reversible Prescription Methods
| Medical Condition | LARC Use vs Other Reversible Prescription Methods* | |
|---|---|---|
| Aged 15–34 Years | Aged 35–44 Years | |
| Any medical condition† | 2.24 (2.06–2.45) | 1.14 (1.08–1.21) |
| Hypertension | 2.56 (2.29–2.87) | 1.07 (1.00–1.14) |
| Diabetes | 1.55 (1.29–1.88) | 1.13 (1.00–1.27) |
| Epilepsy | 1.43 (1.12–1.82) | 1.33 (0.95–1.88) |
| Breast cancer | NR‡ | 2.94 (2.21–3.91) |
| Stroke | 3.30 (2.28–4.78) | 2.01 (1.49–2.72) |
| Bariatric surgery within 2 y | NR‡ | 1.57 (1.21–2.03) |
| Ischemic heart disease | NR‡ | 1.42 (1.02–1.99) |
| Lupus | NR‡ | 1.75 (1.27–2.41) |
| Thrombophilia | 10.78 (6.91–16.82) | 4.38 (2.76–6.93) |
LARC, long-acting reversible contraceptive.
Data are odds ratio (95% confidence interval).
Bold indicates significant results (P<.01).
Odds ratio represents the odds of use of LARCs compared with use of injectable, pill, patch, or ring among those with the selected medical condition compared with those without any of the 21 medical conditions.
Any of the 21 medical conditions identified by the U.S. Medical Eligibility Criteria for Contraceptive Use9 as placing women at increased risk for adverse events if they experience an unintended pregnancy (bariatric surgery within 2 years, breast cancer, diabetes, epilepsy, hypertension, ischemic heart disease, lupus, stroke, thrombophilia, endometrial cancer, ovarian cancer, human immunodeficiency virus, trophoblastic disease, liver cancer, peripartum cardiomyopathy, schistosomiasis, cirrhosis, sickle cell disease, transplant within 2 years, tuberculosis, and valvular heart disease).
Not reported because of small numbers (less than 30).
DISCUSSION
Despite potential elevated risks during pregnancy for women with certain medical conditions, our analysis demonstrated that their contraceptive method use is not optimal, because the prevalence of female sterilization and reversible prescription methods was low among both younger and older women with medical conditions. In addition, similar to the proportion among all women, the most frequently used methods among women with medical conditions were shorter acting prescription methods, which are not as effective as LARCs or female sterilization. These results are consistent with previous studies examining specific populations or conditions that also found high proportions of nonuse of prescription methods among women with medical conditions.14–18
Although there was an overall low prevalence of sterilization, our study demonstrated increased odds of sterilization for women with medical conditions compared with women without medical conditions; this association was strongest among younger women with hypertension, diabetes, stroke, and thrombophilia. The magnitude of the associations suggests that health care providers may be more aware of the need for highly effective contraception among women with these conditions. Our findings are consistent with another study that found women with diabetes were more likely to undergo sterilization compared with women without any medical conditions and also found that women with diabetes received less contraceptive counseling than women without any medical conditions17; therefore, these women may not be receiving enough information on alternative, highly effective reversible contraceptive methods. Women with medical conditions may prefer sterilization because follow-up would not be needed in addition to their other medical needs. However, the possibility of later regret, particularly among younger women who undergo sterilization, should be considered.19
The overall proportion of women using LARC methods in our cohort was low, consistent with national estimates of LARC use (eg, IUD use was 3.5% in the United States during 2006–2010).18 However, among women who used reversible prescription contraception, women with medical conditions were more likely to use LARCs than other shorter acting reversible methods compared with women not having medical conditions. Among younger women, odds were highest among those with hypertension, stroke, and thrombophilia, and among older women, odds were highest among those with breast cancer and thrombophilia. These findings may be influenced by recommendations that women with certain medical conditions not use combined hormonal methods because of safety concerns.9
A major strength of our study was the use of nationwide data that included millions of health claims and the ability to capture inpatient, outpatient, and pharmaceutical services for individual women. The size of the databases allowed us to examine medical conditions that are rare among women of reproductive age.
The use of administrative data based on insurance claims has several limitations. The prevalence of medical conditions may have been underestimated if the medical conditions were not coded during women’s health encounters. However, we attempted to increase detection of medical conditions by examining several years of data, which would increase the chance that a woman with significant disease would require an encounter for her condition. Use of pharmaceutical codes for pills, patch, and ring is a proxy measure and may not reflect actual use. In addition, women classified as nonusers may have included those with IUD insertion, sterilizations, or hysterectomy before 2004; women relying on male sterilization or using nonprescription methods (barrier methods or fertility awareness-based methods); or women who were pregnant, trying to become pregnant, not sexually active, or otherwise not at risk for unintended pregnancy. We examined only those women with commercial insurance, and our results may not be generalizable to women on Medicaid or without insurance. Finally, we were unable to examine whether contraceptive choice was affected by insurers, although we expect that access will improve with implementation of the Affordable Care Act.
The increasing rate of medical conditions among women of reproductive age, coupled with the persistently high rates of unintended pregnancy in the United States, is a significant public health concern. Women with certain medical conditions face significant risks if they become pregnant. Therefore, decreasing unintended pregnancy through increasing access to and use of highly effective contraception is critically important for these women. Women with medical conditions may face additional barriers to using highly effective contraception, including LARCs, because of misperceptions among patients and health care providers about the safety of these methods and of logistics and cost issues. Health care providers may be more focused on a woman’s medical condition and overlook a possible need for contraception, and women with medical conditions may receive care from specialists who are less experienced in providing family planning. Most women, even those with medical conditions, can safely use most contraceptive methods.9 Our analysis shows that there is a large unmet need for contraceptive use among women with medical conditions. All health care providers who care for women with medical conditions should be aware of the critical importance of highly effective contraception to prevent unintended pregnancy and associated complications.
Footnotes
LEVEL OF EVIDENCE: III
Presented as a poster at the Society for Epidemiologic Research Annual Meeting, June 24–27, 2014, Seattle, WA.
The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Financial Disclosure
The authors did not report any potential conflicts of interest.
REFERENCES
- 1.Mathews TJ, Hamilton BE. First births to older women continue to rise. NCHS Data Brief. No. 152; 2014. Available at: http://www.cdc.gov/nchs/data/databriefs/db152.pdf. Retrieved March 34, 2015. [PubMed] [Google Scholar]
- 2.Berg CJ, Mackay AP, Qin C, Callaghan WM. Overview of maternal morbidity during hospitalization for labor and delivery in the United States: 1993–1997 and 2001–2005. Obstet Gynecol 2009;113:1075–81. [DOI] [PubMed] [Google Scholar]
- 3.Creanga AA, Berg CJ, Ko JY, Farr SL, Tong VT, Bruce FC, et al. Maternal mortality and morbidity in the United States: where are we now? J Womens Health (Larchmt) 2014;23:3–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Luke B, Brown MB. Contemporary risks of maternal morbidity and adverse outcomes with increasing maternal age and plurality. Fertil Steril 2007;88:283–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hayes DK, Fan AZ, Smith RA, Bombard JM. Trends in selected chronic conditions and behavioral risk factors among women of reproductive age, behavioral risk factor surveillance system, 2001–2009. Prev Chronic Dis 2011;8:A120. [PMC free article] [PubMed] [Google Scholar]
- 6.Finer LB, Zolna MR. Shifts in intended and unintended pregnancies in the United States, 2001–2008. Am J Public Health 2014;104(suppl 1):S43–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gipson JD, Koenig MA, Hindin MJ. The effects of unintended pregnancy on infant, child, and parental health: a review of the literature. Stud Fam Plann 2008;39:18–38. [DOI] [PubMed] [Google Scholar]
- 8.Chor J, Rankin K, Harwood B, Handler A. Unintended pregnancy and postpartum contraceptive use in women with and without chronic medical disease who experienced a live birth. Contraception 2011;84:57–63. [DOI] [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention (CDC). U.S. Medical Eligibility Criteria for Contraceptive Use, 2010. MMWR Recomm Rep 2010;59:1–86. [PubMed] [Google Scholar]
- 10.Hansen LG, Chan S. Health research data for the real world: the Marketscan databases. Bethesda (MD): Truven Health Analytics; 2012. [Google Scholar]
- 11.Hebert PL, Geiss LS, Tierney EF, Engelgau MM, Yawn BP, McBean AM. Identifying persons with diabetes using Medicare claims data. Am J Med Qual 1999;14:270–7. [DOI] [PubMed] [Google Scholar]
- 12.Centers for Disease Control and Prevention. Effectiveness of family planning methods. Adapted from World Health Organization (WHO) Department of Reproductive Health and Research, Johns Hopkins Bloomberg School of Public Health/-Center for Communication Programs (CCP). Geneva (Switzerland): CCP and WHO; 2011. [Google Scholar]
- 13.Trussell J Contraceptive failure in the United States. Contraception 2011;83:397–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chuang CH, Chase GA, Bensyl DM, Weisman CS. Contraceptive use by diabetic and obese women. Womens Health Issues 2005;15:167–73. [DOI] [PubMed] [Google Scholar]
- 15.DeNoble AE, Hall KS, Xu X, Zochowski MK, Piehl K, Dalton VK. Receipt of prescription contraception by commercially insured women with chronic medical conditions. Obstet Gynecol 2014;123:1213–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.O’Brien SH, Klima J, Reed S, Chisolm D, Schwarz EB, Kelleher KJ. Hormonal contraception use and pregnancy in adolescents with sickle cell disease: analysis of Michigan Medicaid claims. Contraception 2011;83:134–7. [DOI] [PubMed] [Google Scholar]
- 17.Schwarz EB, Postlethwaite D, Hung YY, Lantzman E, Armstrong MA, Horberg MA. Provision of contraceptive services to women with diabetes mellitus. J Gen Intern Med 2012; 27:196–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jones J, Mosher WD, Daniels K. Current contraceptive use in the United States, 2006–2010, and changes in patterns of use since 1995. National health statistics reports; No. 60. Hyattsville (MD): National Center for Health Statistics. 2012. Available at: http://www.cdc.gov/nchs/data/nhsr/nhsr060.pdf. Retrieved January 7, 2014. [PubMed] [Google Scholar]
- 19.Curtis KM, Mohllajee AP, Peterson HB. Regret following female sterilization at a young age: a systematic review. Contraception 2006;73:205–10. [DOI] [PubMed] [Google Scholar]


