Abstract
Background
Factors that predict attempts to discontinue drug use are clinically relevant and may inform treatment. This study investigated drug use-related consequences as a predictor of drug quit attempts and treatment seeking among two cohorts of persons who use drugs.
Methods
Drug use and clinical characteristics were assessed among persons who use cocaine (N=176; urine-verified; ‘Cocaine Cohort’) and among those who use heroin (N=166; urine-verified; ‘Heroin Cohort’). Mediation analyses assessed relationships among age at initial drug use, adverse drug-specific use-related consequences, and drug-specific quit attempts, separately for each cohort. Forward conditional logistic regression models evaluated drug use and clinical symptom scores as predictors of drug-specific treatment seeking.
Results
Controlling for age, mediation models showed that drug use consequences fully mediated the relationship between age at initial drug use and number of drug-specific quit attempts for the ‘Cocaine Cohort’ and ‘Heroin Cohort’ (R2=0.30, p<.001; R2=0.17, p<.001; respectively). Reporting more consequences predicted more quit attempts in each cohort, accounting for duration of use (ps<.001). Reporting more consequences also predicted greater likelihood of seeking drug use treatment (ps<.001) and was associated with more severe clinical symptoms in each cohort (ps<.05).
Conclusions
Using a parallel analysis design, we showed that reporting more drug-specific use-related consequences predicted more drug-specific quit attempts and greater likelihood to seek treatment in two cohorts: persons who use cocaine and those who use heroin. Our findings suggest that experiencing more drug use consequences predicts more attempts to seek drug abstinence and that assessment of consequences may be informative for treatment.
Keywords: Heroin, Cocaine, Drug use consequences, Quit attempts, Drug abstinence
Highlights
-
•
Experiencing adverse drug use consequences may motivate drug use quit attempts.
-
•
Consequences mediated the relationship between initial drug use and quit attempts.
-
•
Reporting more consequences predicted more quits among cocaine and heroin users.
-
•
Reporting more consequences was related to seeking treatment in both groups.
-
•
Reporting more consequences predicted worse clinical symptoms in both groups.
1. Introduction
In 2021, approximately 4.8 million Americans (aged 12 and older) reported past-year cocaine use, and 1.1 million reported past-year heroin use (Center for Behavioral Health Statistics and Quality, 2023). In 2022 alone, nearly 110,000 Americans died from drug-overdose deaths; more than any year prior (Ahmad et al., 2023). Despite significant health risks associated with use, including overdose death, prior research suggests that 20% or fewer individuals experiencing opioid or cocaine use disorder receive treatment for their respective use disorder (Ronsley et al., 2020, Wu et al., 2016). Given the limited utilization of (finite) treatment resources in the United States, maximizing the likelihood of success is paramount for improving public health. Here, we investigated relationships between adverse drug use-related consequences, drug quit attempts, and history of seeking drug treatment among persons who use cocaine and among those who use heroin.
1.1. Theories of behavior change
Motivation to quit using drugs is a well-established factor for treatment success in substance use disorders (SUDs; Prochaska and DiClemente, 1983; Harrell et al., 2013). Three prominent models characterize factors that influence motivation for behavior change: the transtheoretical model (Prochaska and DiClemente, 1983), social-cognitive theory (Bandura, 1986), and McBride et al.’s (2003) “teachable moments” model. The transtheoretical model (TTM) or ‘stages of change’ model postulates six temporal stages – precontemplation, contemplation, preparation, action, maintenance, and termination – through which individuals progress as a function of their ‘decisional balance.’ If the ‘cons’ of drug use (e.g., health concerns) outweigh the ‘pros’ (e.g., psychoactive effects), an individual’s ‘decisional balance’ may tip toward behavior change, i.e., an attempt to discontinue use or a ‘quit attempt’ (Prochaska and DiClemente, 1983). In the social-cognitive theory, behavior change is theorized to result from the interaction between an individual’s self-efficacy, personal beliefs, and past-to-current behaviors, and the socio-environmental consequences of those behaviors (Bandura, 1986). In the third model, McBride et al. (2003) describe “teachable moments” and posit that motivation for behavioral change manifests from events that impact an individual’s perception of risk of negative outcome, elicit a strong emotional response, and/or affect an individual’s social role (McBride et al., 2003).
Common among of these models are two central tenets of behavior change: 1) perception of self-efficacy and 2) importance of adverse consequences. To change a behavior (i.e., quit using a drug), an individual must both believe themselves capable of making change (self-efficacy) (Bandura, 1986) and have potent reasons to make the change (i.e., avoid negative consequences of drug use) which tilt one’s ‘decisional balance’ toward action (Prochaska and DiClemente, 1983). This study focused on the latter factor: adverse drug use consequences. In drug addiction, experiencing adverse consequences related to one’s drug use may be a powerful motivator to discontinue use (i.e., negative reinforcement; McBride et al., 2003). Further, understanding the social, behavioral, environmental, or health factors that drive an individual’s decision to attempt to stop using a drug (i.e., a quit attempt) may provide important contextual information related to a patient’s ‘readiness to change’ and highlight specific elements to address during treatment (e.g., comorbid health problems, legal issues, or dysfunctional interpersonal relationships) which may interfere with therapeutic success (Prochaska and DiClemente, 1983). The overall goal of this study was to investigate relationships between adverse drug use-related consequences and attempts to achieve drug abstinence, which we quantified as number of prior drug quit attempts and having ever sought drug use treatment.
1.2. Drug use consequences
In daily life, heroin and/or cocaine use are often associated with adverse consequences that span social, legal, financial, and health domains (Lister et al., 2015, Moses et al., 2018). Prior research in our laboratory has shown that drug use consequences are related to impulsivity, depression, and treatment outcomes (Lister et al., 2022, Lister et al., 2015, Moses et al., 2018, Woodcock et al., 2015, Reid et al., 2018). For instance, participants reporting more opioid use consequences and greater opioid-related ‘readiness to change’ at entry to methadone maintenance treatment provided more opioid- and drug-negative urine screens during their first month of therapy (Lister et al., 2022). Interestingly, opioid use consequences and opioid-related ‘readiness to change’ were not correlated (p = 0.49; Supplemental Fig. 1), which suggests consequences (1) predict opioid abstinence during treatment, and (2) account for unique variance unrelated to ‘readiness to change’. This important observation highlights the clinical utility for assessing drug use-related consequences and suggests consequences may contribute to motivational processes or other latent factors that are not reflected in self-reported ‘readiness to change’. Building on this finding, we investigated the relationship between drug use consequences and attempts to discontinue drug use among two subject cohorts – persons who use cocaine and those who use heroin – using a parallel analysis design. Specifically, we evaluated whether drug use consequences mediated the relationship between age at initial drug use and number of prior quit attempts, controlling for chronological age (i.e., accounting for duration of use), and predicted likelihood for seeking drug treatment in each subject cohort.
2. Methods
2.1. Participant selection
The Wayne State University Institutional Review Board approved all study procedures which were conducted in accordance with the Declaration of Helsinki (1964) and Belmont Report (1978). Two groups of individuals were recruited via media advertisements and word-of-mouth referrals in the Detroit metropolitan area for ‘parent’ studies: out-of-treatment persons who currently use cocaine (‘Cocaine Cohort’; registered clinical trials: NCT00946660 and NCT01392092; Greenwald et al., 2014; Woodcock et al., 2020) and out-of-treatment persons who currently use heroin (‘Heroin Cohort’; registered clinical trials: NCT00684840 and NCT01536925; Greenwald et al., 2013; Greenwald et al., in preparation). Following a brief telephone-based screening interview, participants were invited to complete in-person screening procedures, including urine drug screen (CLIA Waived, Inc., San Diego, CA), expired breath alcohol screen (Alco-Sensor III Breathalyzer, Intoximeter Inc., St. Louis, MO), and self-report measures of drug use frequency and history, affect, and mood state (see below). Participants were included in analyses if they: 1) presented expired breath alcohol <0.02% (Alco Sensor III Breathalyzer) and cognitively intact (score ≥80 on the Shipley Institute of Living Scale; Zachary, 1991); 2) provided complete data for variables included in each mediation model (see below); and 3) tested positive for recent opioid (≥300 ng/ml morphine; ‘Heroin Cohort’) and/or cocaine use (>300 ng/ml benzoylecgonine [cocaine metabolite]; ‘Cocaine Cohort’). A subset of individuals tested positive for both cocaine and heroin (n=76), and thus, were included in both sets of analyses of drug-specific variables.
2.2. Measures
2.2.1. Demographics
Normative demographic information, including biological sex, race, age, and years of formal education, were collected during the screening visit.
2.2.2. Substance use characteristics
Substance use characteristics were assessed via self-report using the comprehensive Drug History and Use Questionnaire (DHUQ) routinely used in our laboratory studies (Moses et al., 2018). Characteristics assessed included past-month drug use frequency, age at initial use, and treatment seeking (‘ever’ vs. ’never’ sought treatment for drug use). Quit attempts were measured as a count of total lifetime attempts to quit using either cocaine or heroin (depending on cohort) for any reason or length of time (self-directed or in-treatment; range: 0–100). Drug use consequences were operationalized as the total number of lifetime drug-specific use-related consequences endorsed (‘ever’ vs. ‘never’) on an item-level checklist. The heroin-specific consequences checklist consisted of 20 items and the cocaine-specific consequences checklist consisted of 16 items (see Table 3). Higher scores indicate that drug use has more adversely affected the respondent’s health, economic, social, legal, and interpersonal function (Moses et al., 2018, Woodcock et al., 2015).
Table 3.
Drug use consequences by cohort.
| Cocaine Cohort (N=176) | Heroin Cohort (N=166) | ||||
|---|---|---|---|---|---|
| Consequence Item | n | % | n | % | |
| Financial | Financial Problems | 89 | 50.6% | 146 | 88.0% |
| High at Work | 38 | 21.6% | 99 | 59.6% | |
| Missed Work | 54 | 30.7% | 86 | 51.8% | |
| Lost Job | 46 | 26.1% | 72 | 43.4% | |
| Warning at Work | - | - | 53 | 31.9% | |
| Social & Legal | Family Problems | 73 | 41.5% | 124 | 74.7% |
| Drove Under Influence | 65 | 36.9% | 122 | 73.5% | |
| Arrested or Legal Problems | 38 | 21.6% | 62 | 37.3% | |
| Fight or Quarrel | 33 | 18.8% | 45 | 27.1% | |
| Missed School | 16 | 9.0% | 24 | 14.5% | |
| Medical & Health | Suspended or Expelled | - | - | 7 | 4.2% |
| Couldn't Stop Using | 85 | 48.3% | 135 | 81.3% | |
| Unexpected Reaction | - | - | 51 | 30.7% | |
| Overdose | 8 | 4.5% | 44 | 26.5% | |
| Shakes and Tremors | 24 | 13.6% | 40 | 24.1% | |
| Visited Emergency Room | 10 | 5.7% | 38 | 22.9% | |
| Memory Lapse/Blackout | - | - | 36 | 21.7% | |
| Health Problem | 10 | 5.7% | 27 | 16.3% | |
| Accident or Injury | 10 | 5.7% | 15 | 9.0% | |
| Seizure or Fits | 5 | 2.8% | 12 | 7.2% | |
2.2.3. Clinical variables
Current depression symptoms were assessed using the Beck Depression Inventory II (BDI-II), a 21-item self-report measure of past 14-day neurovegetative depression symptom severity (Beck et al., 1988). Scores ranged from 0 to 63, with scores of 14–19 indicative of ‘mild’ depression, 20–28 indicative of ‘moderate’ depression, and 29+ indicative of ‘severe’ depression (Beck et al., 1996). Current depression, anxiety, and stress levels were assessed via the Depression Anxiety Stress Scales (DASS-21; short form), a past-week 21-item self-report measure with three 7-item scales: Depression (dysphoric mood), Anxiety (physiological arousal, fear), and Stress (tension, difficulty relaxing, irritability) (Lovibond and Lovibond, 1995).
2.3. Data analyses
2.3.1. Bivariate analyses
Statistical analyses were conducted using SPSS v27 (IBM Corporation, Armonk, NY). Raw data were screened for statistical outliers (z score ≥ |3|) and non-normal distributions (skewness, kurtosis, and Shapiro-Wilk tests) were corrected with statistical transformations (e.g., log10) prior to outcome analyses. Descriptive data are presented as group Mean (M; ± one standard deviation [SD]) or percentage endorsed (%; see Table 1). The ‘Heroin Cohort’ and ‘Cocaine Cohort’ were analyzed separately for heroin- vs. cocaine-specific drug use characteristics, bivariate correlations, logistic regressions, and mediational models. Bivariate correlations (Pearson’s r) were used to assess statistical relationships between continuous and ordinal variables.
Table 1.
Participant characteristics.
| Cocaine Cohort (N=176) | Heroin Cohort (N=166) | |
|---|---|---|
| Participant Characteristics | ||
| Gender (% male) | 73.3% | 74.7% |
| Race (% Black/African American) | 69.3% | 44.6% |
| Age (years) | 44.3 (8.7) | 41.6 (11.1) |
| Education (years) | 12.8 (1.6) | 12.2 (1.5) |
| Drug-Specific Use Characteristics | ||
| Age at initial use (years) | 24.8 (7.1) | 25.6 (8.6) |
| Age at regular use (years) | 27.3 (7.4) | 27.1 (8.6) |
| Duration since initial use (years) | 19.6 (9.0) | 15.9 (11.9) |
| Past-month uses (#) | 40.8 (48.8) | 104.2 (76.2) |
| Lifetime quit attempts (#) | 12.0 (23.4) | 9.5 (19.2) |
| Lifetime use consequences (#) | 4.1 (4.1) | 7.7 (4.5) |
| Ever sought treatment (%) | 65.7% | 63.3% |
| Clinical Symptom Scores | ||
| BDI-II Total Score | 13.7 (10.6) | 4.5 (4.2) |
| DASS Anxiety | 2.4 (2.8) | 2.3 (2.7) |
| DASS Stress | 4.9 (4.1) | 5.0 (4.0) |
| DASS Depression | 4.2 (4.2) | 4.5 (4.2) |
Note: Values are Means (±1 Standard Deviation) or percentage endorsed (%).
2.3.2. Mediational analyses
Using PROCESS (Preacher and Hayes, 2004) in SPSS v27, mediation analyses assessed the mechanistic influence of lifetime drug use consequences (mediator variable: M) on the relationship between age at initial drug use (independent variable: X) and drug-specific quit attempts (dependent variable: Y), controlling for chronological age. Separate mediation models were conducted for the ‘Heroin Cohort’ evaluating heroin-specific variables and for the ‘Cocaine Cohort’ evaluating cocaine-specific variables. Mediational analyses have been widely used in retrospective cross-sectional data to investigate pathways among substance use characteristics and mental health outcomes (e.g. Asberg and Renk, 2012; Klanecky et al., 2012; Lister et al., 2015). Importantly, we followed guidelines for mediation analyses in observational data (MacKinnon and Luecken, 2008, Preacher and Hayes, 2004, Baron and Kenny, 1986, Shrout and Bolger, 2002). First, it is recommended that independent variable (X) temporally precede both the mediator variable (M) and dependent variable (Y): a recommendation we followed (Baron and Kenny, 1986). Age at initial drug use (X) necessarily occurs prior to both drug use consequences (M) and quit attempts (Y). Second, it is recommended that the dependent variable (Y) should not cause or temporally precede the mediator variable (M): a recommendation we followed (Baron and Kenny, 1986). In theory, a 'quit attempt' (Y), i.e., the absence of drug use, cannot cause a 'drug use-related consequence' (M), but this study is limited to data on the lifetime aggregation of consequences and quit attempts, and thus, we cannot infer ‘causal’ or ‘mechanistic’ relationships (e.g., see recommendations: Maxwell and Cole, 2007; Stuart et al. 2021). Finally, to estimate the indirect effect, we applied a robust bias-corrected bootstrapping technique (5000 iterations) in PROCESS; this technique is less susceptible to Type II errors than the Sobel test (Preacher and Hayes, 2004). Effect sizes (R2) were estimated for each mediation model (Preacher and Hayes, 2004).
2.3.3. Logistic regression models
Predictors of seeking treatment for cocaine or heroin use (coded: ‘ever’ vs. ‘never’) were investigated using a forward conditional logistical regression (stepwise inclusion and exclusion thresholds: p <.05 and p >.10, respectively), controlling for duration of drug use. Predictors included drug use variables (use consequences, age at initial use, and past-month use frequency), demographic variables (age, sex, years of education), and current depression symptoms (BDI-II).
3. Results
3.1. Participant characteristics
The ‘Cocaine Cohort’ (N = 176) was mostly Black/African American (69.3%) and male (73.3%; Table 1). Mean age was 44.3 ± 8.7 years old and about half reported at least a high school education (52.0%). Mean age at initial cocaine use was 24.8 ± 7.1 years and mean duration of cocaine use was 19.6 ± 9.0 years. Participants reported 12.0 ± 23.4 cocaine quit attempts and 4.1 ± 4.1 cocaine use consequences (of 16 possible consequences; 25.6%), on average. Mean past-month cocaine-use frequency was 40.8 ± 48.8 uses (or ~1.4 uses/day).
The ‘Heroin Cohort’ (N = 166) was about half Black/African American (44.6%) and mostly male (74.7%; Table 1). Mean age was 41.6 ± 11.1 years old and the majority reported at least a high school education (70.9%). Mean age at initial heroin use was 25.6 ± 8.6 years and mean duration of heroin use was 15.9 ± 11.9 years. Participants reported 9.5 ± 19.2 heroin quit attempts and 7.7 ± 4.5 heroin use consequences (of 20 possible consequences; 38.5%). Mean past-month heroin-use frequency was 104.2 ± 76.2 times (or ~3.5 times/day).
3.2. Mediation models
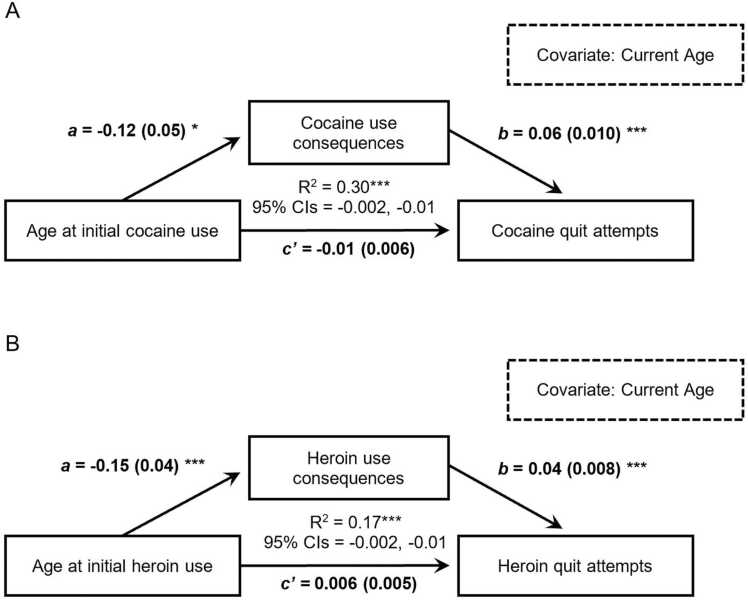
Mediation analyses, conducted separately for the ‘Cocaine Cohort’ and ‘Heroin Cohort’, investigated relationships between age at initial drug use (independent variable), drug use consequences (mediator), and drug quit attempts (dependent variable), controlling for current age (Fig. 1). Direct effect paths for each relationship (X->M [“a” path], M->Y [“b” path]), and X->Y [“c” path], and the indirect effect path (mediation model: X->M->Y [c-prime {c’} path]), as well as the bootstrap-estimated 95% confidence interval to test the significance of the indirect effect, are presented for each model.
Fig. 1.
a) Mediation model with age at initial cocaine use (X), cocaine use consequences (M), and cocaine quit attempts (Y), controlling for current chronological age (covariate). b) Mediation model with age at initial heroin use (X), heroin use consequences (M), and heroin quit attempts (Y), controlling for current chronological age (covariate). For each model, data were bootstrapped 5000 times to estimate bias-corrected 95% confidence intervals (95% CIs) to test the significance of the indirect effect. The unstandardized coefficients and standard errors shown account for the mediator in the equation. We list direct effect paths for predictor to mediator (a path; X-M), mediator to dependent variable (b path; M-Y), and predictor to dependent variable (c’ path; X-Y). Finally, the effect size (or variance explained) for each mediation model is presented (R2). Note. *p<.05; **p<.01; ***p<.001.
In the first mediation analysis, the direct effect of age at initial cocaine use to cocaine quit attempts was not significant (“c” path; p = 0.1; Fig. 1A). Both “a” and “b” paths were significant (p <.05 and p <.001; respectively). The indirect effect (c’ path) was significant (p <.001) with an effect size: R2 = 0.30. Results indicate that cocaine use consequences fully mediated the relationship between age at initial cocaine use and number of cocaine quit attempts, controlling for current age, and accounted for 30% of the variance in cocaine quit attempts.
In the second mediation analysis, the direct effect of age at initial heroin use to heroin quit attempts was not significant (“c” path; p = 0.2; Fig. 1B). Both “a” and “b” paths were significant (p <.001 and p <.001; respectively). The indirect effect (c’ path) was significant (p <.001) with an effect size: R2 = 0.17. Results show that heroin use consequences fully mediated the relationship between age at initial heroin use and number of heroin quit attempts, controlling for current age, and accounted for 17% of the variance in heroin quit attempts.
For completeness, supplemental mediation analyses were conducted which replicated the above models but excluded individuals who tested positive for both cocaine and heroin (n=76). Findings from these sub-group analyses generally replicated findings from the full sample and showed that use-related consequences mediated the relationship between age at initial use and drug-specific quit attempts, controlling for current age, for each drug cohort (Supplemental Fig. 2).
3.3. Logistic regression models
Using a forward conditional logistical regression, predictors of having sought treatment for drug use were investigated. Controlling for duration of cocaine use, cocaine use consequences were the only significant predictor of having sought cocaine treatment among the ‘Cocaine Cohort’ (β = 2.8, SE = 0.7, OR= 16.4, p <.001), whereas age at initial use, past-month use frequency, current depression symptoms, age, sex, and years of education were unrelated (ps >.05). Individuals who had sought treatment for cocaine use reported ~2.5x more cocaine use consequences than individuals who had not sought treatment (6.2 ± 4.0 vs. 2.5 ± 3.2; p <.001).
Controlling for duration of heroin use, a forward conditional logistical regression showed that more heroin use consequences, greater past-month heroin use frequency, and being female predicted greater likelihood for having sought treatment for heroin use among the ‘Heroin Cohort’ (β = 0.20, SE = 0.05, OR= 1.22, p <.001; β = −1.62, SE = 0.67, OR= 0.20, p <.05; β = 1.01, SE = 0.48, OR= 2.75, p <.05, respectively), whereas age at initial use, current depression symptoms, age, and years of education were unrelated (ps >.25). Individuals who had sought treatment for heroin use reported nearly twice more heroin use consequences than individuals who had not sought treatment (8.9 ± 4.3 vs. 5.5 ± 4.0; p <.001).
3.4. Clinical symptom scores
Among the ‘Cocaine Cohort’, reporting more cocaine use consequences was correlated with more current depression symptoms (BDI-II: r = 0.30, p <.01; DASS depression: r = 0.42, p <.001) and higher current stress levels (DASS stress: r = 0.40, p <.001), but was unrelated to current anxiety levels (DASS anxiety: r = 0.17, p >.05; Table 2). Conversely, age at initial cocaine use, cocaine use duration, and past-month cocaine use frequency were not significantly correlated with any current clinical symptom scores (ps >.05).
Table 2.
Bivariate Pearson correlations among drug use variables and clinical symptom scores.
| 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cocaine Cohort | Mediation Variables | 1. Age at initial cocaine use | -0.16* | -0.07 | 0.37** | -0.12 | -0.21 | -0.16 | -0.15 | -0.03 | -0.43** | |
| 2. Cocaine use consequences | 0.48** | 0.06 | 0.30** | 0.42** | 0.17 | 0.40** | 0.24** | 0.18* | ||||
| 3. Cocaine quit attempts | 0.28** | 0.18* | 0.28* | 0.36** | 0.46** | 0.22** | 0.33** | |||||
| 4. Current age | -0.08 | -0.31* | -0.09 | -0.16 | 0.21** | 0.68** | ||||||
| Clinical Symptom Scores | 5. BDI-II | 0.68** | 0.50** | 0.57** | 0.01 | 0.01 | ||||||
| 6. DASS depression | 0.48** | 0.64** | 0.13 | -0.17 | ||||||||
| 7. DASS anxiety | 0.67** | 0.03 | 0.02 | |||||||||
| 8. DASS stress | 0.09 | -0.06 | ||||||||||
| 9. Past-month use frequency | 0.22** | |||||||||||
| 10. Cocaine use duration | ||||||||||||
| Heroin Cohort | Mediation Variables | 1. Age at initial heroin use | -0.30** | 0.05 | 0.27** | -0.05 | -0.13 | -0.15 | -0.07 | -0.03 | -0.45** | |
| 2. Heroin use consequences | 0.32** | -0.16* | 0.25** | 0.37** | 0.26** | 0.38** | -0.04 | 0.07 | ||||
| 3. Heroin quit attempts | 0.20* | 0.06 | 0.17* | 0.05 | 0.14 | -0.07 | 0.15 | |||||
| 4. Current age | -0.24** | -0.24** | -0.12 | -0.14 | -0.06 | 0.74** | ||||||
| Clinical Symptom Scores | 5. BDI-II | 0.70** | 0.45** | 0.58** | -0.05 | -0.19* | ||||||
| 6. DASS depression | 0.48** | 0.72** | -0.07 | -0.13 | ||||||||
| 7. DASS anxiety | 0.60** | -0.03 | -0.01 | |||||||||
| 8. DASS stress | -0.04 | -0.08 | ||||||||||
| 9. Past-month use frequency | -0.04 | |||||||||||
| 10. Heroin use duration | ||||||||||||
Note: Bold values = statistically significant Pearson correlation: *p<.05, **p<.01, ***p<.001.
Among the ‘Heroin Cohort’, reporting more heroin use consequences was correlated with more current depression symptoms (BDI-II: r = 0.25, p <.01; DASS depression: r = 0.37, p <.001) and higher current anxiety and stress levels (DASS anxiety: r = 0.26, p <.01 and DASS stress: r = 0.38, p <.001; Table 2). Conversely, age at initial heroin use, heroin use duration, and past-month heroin use frequency were not significantly correlated with any current clinical symptoms (ps >.05).
4. Discussion
Using a parallel analysis design, the present study examined mediational pathways of age at initial drug use, lifetime drug use consequences, and lifetime drug quit attempts among two currently out-of-treatment cohorts: persons who use cocaine and those who use heroin. Findings indicated that drug use consequences fully mediated the relationship between age at initial drug use and quit attempts, controlling for current age, in both cohorts, yielding an internal statistical replication. Moreover, sub-group analyses, excluding concurrent cocaine- and heroin-using individuals, replicated findings from the full sample indicating these relationships are robust. Further, reporting more lifetime drug use consequences predicted greater likelihood of having ever sought drug treatment. Finally, reporting more lifetime drug use consequences was associated with worse current clinical symptom scores, whereas age at initial use, use duration, and past month use frequency were not related. Our findings support a strong relationship between drug use consequences and drug quit attempts/treatment seeking and suggest that assessment of drug use consequences during clinical intake may be informative for treatment planning.
Drug use consequences can occur across all domains of one’s life, from adverse health effects due to drug self-administration to the legal consequences related to drug purchasing and possession. In this study, we used a ‘checklist’ measure of drug use consequences in which subject’s indicated whether they had experienced an adverse effect on their legal, financial, health, or interpersonal functioning specifically due to their drug use (either cocaine or heroin). Thus, reporting more drug use consequences in this study reflects greater biopsychosocial dysfunction across multiple domains in one’s life rather than numerous instances of the same (repetitive) drug use consequences (e.g., multiple ‘jobs lost’ due to drug use). Among two drug cohorts, 176 persons who use cocaine and 166 persons who use heroin, we showed that self-reporting more drug use consequences mediated the relationship between age at initial drug use and number of quit attempts (controlling for chronological age). Thus, accounting for the duration of use, reporting more consequences predicted more quit attempts, accounting for 30% of the variance in the ‘Cocaine Cohort’ and 17% in the ‘Heroin Cohort.’ Further, we showed that reporting more drug use consequences predicted greater likelihood of having ever sought drug treatment in both cohorts. Individuals who sought drug use treatment reported roughly twice as many drug use consequences than those who had not sought treatment (6.2 vs. 2.5 among the ‘Cocaine Cohort’ and 8.9 vs. 5.5 among the ‘Heroin Cohort’). Notably, more than 60% of this sample had sought drug use treatment in their lifetime, suggesting this may be an especially ‘severe’ sample. Taken together, our findings suggest that drug use consequences may be related to attempts to reduce drug use and/or achieve drug abstinence. An alternate explanation for our findings is that individuals who are engaged in heavier substance use may experience more consequences from their use and thus, have a greater need for treatment. Our findings build on prior research that showed reporting more opioid use consequences and greater opioid-related ‘readiness to change’ predicted greater opioid- and drug-abstinence during the first month of outpatient methadone maintenance therapy (Lister et al., 2022). Importantly, Lister et al., found that opioid use consequences and opioid-related ‘readiness to change’ were not correlated with each other, suggesting that each metric accounts for unique variance related to drug abstinence (Supplemental Fig. 1) and thus, may reflect different underlying processes or factors that regulate drug use behavior. At this time, it is unclear how, or through which processes, experiencing drug use consequences contributes to the regulation of drug use behavior and abstinence. We speculate that experiencing more adverse (especially, emotionally-salient) drug use consequences may: 1) heighten awareness of problematic behavior (“consciousness raising”; Lister et al., 2022); 2) crystalize the discrepancy between one’s self-concept/identity and their substance use behavior (Downey et al., 2000); 3) amplify urgency for behavior change which may not be reflected in ‘readiness to change’ scores; or other factors not discussed here. Future studies are needed to disambiguate those relationships. We contend that assessment of drug use consequences via a simple checklist questionnaire during routine clinical intake may be a useful metric to supplement ‘readiness to change’ (Lister et al., 2022, Norcross et al., 2011, Prochaska and DiClemente, 1983). Further, assessment of drug use consequences during clinical intake may be useful to tailor behavioral interventions to address particularly dysfunctional behavior or biopsychosocial domains, e.g., financial instability or legal problems, which may hinder treatment engagement and effectiveness.
Our findings also show that reporting more drug use consequences was associated with worse clinical symptom scores (Lister et al., 2015, Reid et al., 2018). In both drug cohorts, consequences were associated with more current depression symptoms and higher stress levels, and among the heroin cohort, consequences were also correlated with higher anxiety levels. Interestingly, our results show no significant associations between age at initial use, use duration, and past-month use frequency and any clinical symptom scores in either drug cohort. Further, reporting more cocaine consequences was the only significant predictor for likelihood of having sought treatment for cocaine use, whereas reporting more heroin use consequences, greater past-month heroin use frequency, and being female each predicted greater likelihood for seeking treatment seeking for heroin use. Reporting more depression symptoms and higher stress levels, along with experiencing more consequences, may be indicative of a more severe use disorder and/or problematic behavior patterns, may impede treatment progress and increase the likelihood of individuals discontinuing treatment, thereby underscoring the clinical importance of assessing these relationships.
These results should be interpreted in the context of study limitations. First, this study used retrospective, cross-sectional data to assess relationships, therefore we cannot infer causal relationships: especially with regard to prediction of an individual quit attempt. To achieve that level of event-by-event granularity, one would need longitudinal ecological momentary (or similar) assessments rather than an aggregation of data across years of drug use (as presented herein). Second, this study did not directly assess participants' motivation to quit or ‘readiness to change’. Thus, relationships between consequences, abstinence motivation, and ‘readiness to change’ could not be evaluated. Third, this study relied on self-reported drug use characteristics, affect, and mood symptoms rather than clinician- or independent rater-assessed variables. However, prior research has established the validity of self-reported histories of drug use, affect, and mood symptoms (Darke, 1998, Hjorthøj et al., 2012, Spitzer et al., 1999, Zaldívar Basurto et al., 2009). Fourth, this study did not measure indices of drug use ‘severity’ to evaluate possible relationships with use-related consequences and quit attempts.
5. Conclusion
In this study, we investigated relationships between drug-specific use-related consequences and drug quit attempts/treatment seeking among two cohorts: persons who use cocaine and those who use heroin. Our findings indicate that drug use consequences mediated the relationship between age at initial drug use and drug quit attempts, controlling for current age, and that reporting more consequences predicted greater likelihood of seeking drug treatment in both cohorts. The robust relationship between drug use consequences and quit attempts/treatment-seeking suggests that consequences may be a useful clinical metric related to attempts to reduce or discontinue drug use and may supplement ‘readiness to change’ scores. Further, study findings highlight the importance of social determinants of health, which can be characterized by the legal, financial, and social drug use consequences assessed herein. Implementing an item-checklist of drug use consequences may inform targeted interventions to address dysfunctional behaviors or biopsychosocial domains. Future research should evaluate whether assessment of consequences and targeted interventions impact treatment engagement and/or clinical outcomes.
Funding
R01 DA015462 (MKG), NIH R01 DA026861 (MKG), F31 DA040369 (EAW), and R00 DA048125 (EAW), the Gertrude Levin Endowed Chair in Addiction and Pain Biology (MKG), Joe Young Sr./Helene Lycaki Funds from the State of Michigan, and funds from the Detroit Wayne Mental Health Authority supported this research. Funding sources had no role in the design, conduct, or analysis of these data, nor the decision to submit this manuscript.
CRediT authorship contribution statement
Mark K. Greenwald: Writing – review & editing, Supervision, Project administration, Funding acquisition, Data curation. Jamey J. Lister: Writing – review & editing, Methodology, Conceptualization. Leslie H. Lundahl: Writing – review & editing, Supervision, Methodology. Adura Sogbesan: Writing – original draft, Investigation, Formal analysis, Visualization. Danielle Lenz: Writing – original draft, Visualization, Investigation, Formal analysis, Data curation. Eric A. Woodcock: Writing – review & editing, Writing – original draft, Visualization, Supervision, Methodology, Formal analysis, Data curation, Conceptualization.
Declaration of Competing Interest
All authors declare no conflict of interest with respect to the conduct or content of this work.
Acknowledgments
The authors thank Ken Bates for participant recruitment, and Elorie Eggleston, Debra Kish, Katherine Mattison, Lisa Sulkowski, and Melissa Williams for assistance with data collection and management.
Footnotes
Supplementary data associated with this article can be found in the online version at doi:10.1016/j.dadr.2024.100229.
Appendix A. Supplementary material
Supplementary material
References
- Ahmad F.B., Sutton P., Rossen L.M., Cisewski J.A. Products - vital statistics rapid release - provisional drug overdose data. Cent. Dis. Control Prev. 2023 〈https://www.cdc.gov/nchs/nvss/vsrr/drug-overdose-data.htm〉 [Google Scholar]
- Asberg K., Renk K. Substance use coping as a mediator of the relationship between trauma symptoms and substance use consequences among incarcerated females with childhood sexual abuse histories. Subst. Use Misuse. 2012;47(7):799–808. doi: 10.3109/10826084.2012.669446. [DOI] [PubMed] [Google Scholar]
- Bandura A. Prentice Hall; Englewood Cliffs, NJ: 1986. Social Foundations of Thought and Action: A Social Cognitive theory. [Google Scholar]
- Baron R.M., Kenny D.A. The moderator–mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J. Personal. Soc. Psychol. 1986;51:1173–1182. doi: 10.1037/0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Beck A.T., Epstein N., Brown G., Steer R.A. An inventory for measuring clinical anxiety: psychometric properties. J. Consult. Clin. Psychol. 1988;56(6):893–897. doi: 10.1037/0022-006X.56.6.893. [DOI] [PubMed] [Google Scholar]
- Beck A.T., Steer R.A., Ball R., Ranieri W.F. Comparison of beck depression inventories-IA and-II in psychiatric outpatients. J. Personal. Assess. 1996;67(3):588–597. doi: 10.1207/s15327752jpa6703_13. [DOI] [PubMed] [Google Scholar]
- Center for Behavioral Health Statistics and Quality, 2023. 2021 National Survey of Drug Use and Health (NSDUH) Releases. Substance Abuse and Mental Health Services Administration. 〈https://www.samhsa.gov/data/release/2021-national-survey-drug-use-and-health-nsduh-releases〉..
- Darke S. Self-report among injecting drug users: a review. Drug Alcohol Depend. 1998;51(3):253–263. doi: 10.1016/S0376-8716(98)00028-3. [DOI] [PubMed] [Google Scholar]
- Downey L., Rosengren D.B., Donovan D.M. To thine own self be true: self-concept and motivation for abstinence among substance abusers. Addict. Behav. 2000;25(5):743–757. doi: 10.1016/S0306-4603(00)00091-5. [DOI] [PubMed] [Google Scholar]
- Greenwald M.K., Ledgerwood D.M., Lundahl L.H., Steinmiller C.L. Effect of experimental analogs of contingency management on cocaine seeking behavior. Drug Alcohol Depend. 2014;139:164–168. doi: 10.1016/j.drugalcdep.2014.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenwald M.K., Lundahl L.H., Steinmiller C.L. Yohimbine increases opioid-seeking behavior in heroin-dependent, buprenorphine-maintained individuals. Psychopharmacology. 2013;225(4):811–824. doi: 10.1007/s00213-012-2868-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenwald, M.K., Woodcock, E.A., Moses, T.E.H., Lundahl, L.H., 2024 The “dark side of addiction" in opioid use disorder: affective dysregulation modulates stress-induced opioid-seeking behavior in the absence of withdrawal (in preparation).
- Harrell P., Trenz R., Scherer M., Martins S., Latimer W. A latent class approach to treatment readiness corresponds to transtheoretical (“stages of change”) model. J. Subst. Abus. Treat. 2013;45(3):249–256. doi: 10.1016/j.jsat.2013.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hjorthøj C.R., Hjorthøj A.R., Nordentoft M. Validity of timeline follow-back for self-reported use of cannabis and other illicit substances—systematic review and meta-analysis. Addict. Behav. 2012;37(3):225–233. doi: 10.1016/j.addbeh.2011.11.025. [DOI] [PubMed] [Google Scholar]
- Klanecky A., McChargue D.E., Bruggeman L. Desire to dissociate: implications for problematic drinking in college students with childhood or adolescent sexual abuse exposure. Am. J. Addict. 2012;21(3):250–256. doi: 10.1111/j.1521-0391.2012.00228.x. [DOI] [PubMed] [Google Scholar]
- Lister J.J., Ellis J.D., Struble C.A., Ledgerwood D.M., Greenwald M.K. Protective factor predictors of abstinence and retention in patients receiving methadone treatment for opioid use disorder. Int. J. Ment. Health Addict. 2022:1–19. doi: 10.1007/s11469-022-00893-z. [DOI] [Google Scholar]
- Lister J.J., Ledgerwood D.M., Lundahl L.H., Greenwald M.K. Causal pathways between impulsiveness, cocaine use consequences, and depression. Addict. Behav. 2015;41:1–6. doi: 10.1016/j.addbeh.2014.09.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovibond S.H., Lovibond P.F. Manual for the Depression Anxiety Stress Scales. second ed. Psychology Foundation; Sydney: 1995. [Google Scholar]
- MacKinnon D.P., Luecken L.J. How and for whom? Mediation and moderation in health psychology. Health Psychol. Off. J. Div. Health Psychol. Am. Psychol. Assoc. 2008;27(2 Suppl):S99. doi: 10.1037/0278-6133.27.2(Suppl.).S99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maxwell S.E., Cole D.A. Bias in cross-sectional analyses of longitudinal mediation. Psychol. Methods. 2007;12(1):23. doi: 10.1037/1082-989X.12.1.23. [DOI] [PubMed] [Google Scholar]
- McBride C.M., Emmons K.M., Lipkus I.M. Understanding the potential of teachable moments: the case of smoking cessation. Health Educ. Res. 2003;18(2):156–170. doi: 10.1093/her/18.2.156. [DOI] [PubMed] [Google Scholar]
- Moses T.E.H., Woodcock E.A., Lister J.J., Lundahl L.H., Greenwald M.K. Developing a scale of domains of negative consequences of chronic heroin use. Addict. Behav. 2018;77:260–266. doi: 10.1016/j.addbeh.2017.07.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norcross J.C., Krebs P.M., Prochaska J.O. Stages of change. J. Clin. Psychol. 2011;67(2):143–154. doi: 10.1002/jclp.20758. [DOI] [PubMed] [Google Scholar]
- Preacher K.J., Hayes A.F. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behav. Res. Methods Instrum. Comput. 2004;36(4):717–731. doi: 10.3758/BF03206553. [DOI] [PubMed] [Google Scholar]
- Prochaska J.O., DiClemente C.C. Stages and processes of self-change of smoking: toward an integrative model of change. J. Consult. Clin. Psychol. 1983;51(3):390–395. doi: 10.1037//0022-006x.51.3.390. 〈https://doi-org.proxy.lib.wayne.edu/10.1037//0022-006x.51.3.390〉 [DOI] [PubMed] [Google Scholar]
- Reid H.H., Lundahl L.H., Lister J.J., Woodcock E.A., Greenwald M.K. Mediational pathways among trait impulsivity, heroin-use consequences, and current mood state. Addict. Res. Theory. 2018;26(5):421–429. doi: 10.1080/16066359.2018.1434513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ronsley C., Nolan S., Knight R., Hayashi K., Klimas J., Walley A., Wood E., Fairbairn N. Treatment of stimulant use disorder: a systematic review of reviews. PLoS ONE. 2020;15(6) doi: 10.1371/journal.pone.0234809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shrout P.E., Bolger N. Mediation in experimental and nonexperimental studies: new procedures and recommendations. Psychol. Methods. 2002;7:422–445. doi: 10.1037/1082-989X.7.4.422. [DOI] [PubMed] [Google Scholar]
- Spitzer R.L., Kroenke K., Williams J.B.W., the Patient Health Questionnaire Primary Care Study Group Validation and utility of a self-report version of PRIME-MD. The PHQ Primary Care Study. JAMA. 1999;282(18):1737–1744. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- Stuart E.A., Schmid I., Nguyen T., Sarker E., Pittman A., Benke K., Rudolph K., Badillo-Goicoechea E., Leoutsakos J.M. Assumptions not often assessed or satisfied in published mediation analyses in psychology and psychiatry. Epidemiol. Rev. 2021;43(1):48–52. doi: 10.1093/epirev/mxab007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woodcock E.A., Lundahl L.H., Khatib D., Stanley J.A., Greenwald M.K. N-acetylcysteine reduces cocaine-seeking behavior and anterior cingulate glutamate/glutamine levels among cocaine-dependent individuals. Addict. Biol. 2020;26 doi: 10.1111/adb.12900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woodcock E.A., Lundahl L.H., Stoltman J.J.K., Greenwald M.K. Progression to regular heroin use: examination of patterns, predictors, and consequences. Addict. Behav. 2015;45:287–293. doi: 10.1016/j.addbeh.2015.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu L.-T., Zhu H., Swartz M.S. Treatment utilization among persons with opioid use disorder in the United States. Drug Alcohol Depend. 2016;169:117–127. doi: 10.1016/j.drugalcdep.2016.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zachary R.A. Western Psychological Services; Los Angeles, CA: 1991. The Manual of the Shipley Institute of Living Scale. [Google Scholar]
- Zaldívar Basurto F., García Montes J.M., Flores Cubos P., Sánchez Santed F., López Ríos F., Molina Moreno A. Validity of the self-report on drug use by university students: correspondence between self-reported use and use detected in urine. Psicothema. 2009;21(2):213–219. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material