Abstract
Background:
Persistent weakness of the quadriceps muscles and extension deficit after knee injuries are due to specific alterations in neural excitability - a process known as arthrogenic muscle inhibition (AMI). The effects of a novel neuromotor reprogramming (NR) treatment based on the use of proprioceptive sensations associated with motor imagery and low frequency sounds have not been studied in AMI after knee injuries.
Hypothesis:
This study aimed to assess quadriceps electromyographic (EMG) activity and the effects on extension deficits in persons with AMI who completed 1 session of NR treatment. We hypothesized that the NR session would activate the quadriceps and improve extension deficits.
Study Design:
Case series.
Level of Evidence:
Level 4.
Methods:
Between May 1, 2021 and February 28, 2022, patients who underwent knee ligament surgery or sustained a knee sprain with a deficit of >30% of the vastus medialis oblique (VMO) on EMG testing in comparison with the contralateral limb after their initial rehabilitation were included in the study. The maximal voluntary isometric contraction of the VMO measured on EMG, the knee extension deficit (distance between the heel and the table during contraction), and the simple knee value (SKV) were assessed before and immediately after completion of 1 session of NR treatment.
Results:
A total of 30 patients with a mean age of 34.6 ± 10.1 years (range, 14-50 years) were included in the study. After the NR session, VMO activation increased significantly, with a mean increase of 45% (P < 0.01). Similarly, the knee extension deficit significantly improved from 4.03 ± 0.69 cm before the treatment to 1.93 ± 0.68 after the treatment (P < 0.01). The SKV was 50 ± 5.43% before the treatment, and this increased to 67.5 ± 4.09% after the treatment (P < 0.01).
Conclusion:
Our study indicates that this innovative NR method can improve VMO activation and extension deficits in patients with AMI. Therefore, this method could be considered a safe and reliable treatment modality in patients with AMI after knee injury or surgery.
Clinical Relevance:
This multidisciplinary treatment modality for AMI can enhance outcomes through the restoration of quadriceps neuromuscular function and subsequent reduction of extension deficits after knee trauma.
Keywords: arthrogenic muscle inhibition, knee, neuromotor reprogramming
The knee is the joint most commonly injured in young sports participants. 4 After an injury to the knee, it is common to observe a deficit in the muscle strength of the quadriceps, in particular the vastus medialis obliquus (VMO) muscle. This deficit is often aggravated by reflex hypertonia of the hamstrings, leading to an extension deficit. These effects have been attributed to a natural phenomenon known as arthrogenic muscle inhibition (AMI), defined as the inability of the patient to maximally contract a muscle.35,36 Persistence of a deficit in quadriceps strength after initial rehabilitation can increase the risk of reinjury to the knee.29,39,42 Furthermore, early operative intervention after a knee injury is associated with complications such as arthrofibrosis, which is most likely due to the lack of recognition of AMI in the period after injury.2,6,40
AMI is a sequential and cumulative neurological process that inhibits surrounding musculature after joint trauma, hypothesized to be a protective mechanism to avoid further joint damage.13,20 The primary influences of these neural alterations in the short term are pain, swelling, inflammation, and damage to mechanoreceptors that alters afferent signalling from the joint to the central nervous system. In the longer term, there is strong evidence that AMI is attributable to a degenerative cycle of muscle wasting and weakness that subsequently limits the effectiveness of rehabilitation protocols.
Most therapeutic exercises are designed to strengthen the musculature but are often ineffective in AMI. Recently, several intervention strategies have been suggested to alter motor excitability using disinhibitory mechanisms. Among them, cryotherapy, transcutaneous electrical nerve stimulation, electromyographic (EMG) biofeedback, transcranial magnetic stimulation, and neuromuscular electrical stimulation may be beneficial to counteract the negative effects of AMI during a short rehabilitation session (30-90 min).3,16,21,31,32,34 Despite improvements in quadriceps function (knee extension strength, quadriceps activation, and EMG activity), persistent deficits have been found, hence possible failures in current treatment strategies.3,11,22,36,38 Indeed, recent reviews by Sonnery-Cottet et al 37 and Tayfur et al 38 concluded that there was low-to-moderate quality evidence for the efficacy of therapeutic interventions and a lack of activation deficit resolution in the long term.
Over the last 2 decades, studies of interventions to treat AMI with motor imagery practice have emerged with the aim of targeting neural mechanisms, 27 recently described in theoretical AMI paradigm. 20 Known without any adverse effect, this practice may be combined with sensory modalities or used in conjunction with other disinhibitory interventions targeting different neural pathways to achieve the ideal therapeutic goal for AMI treatment.15,28
Interestingly, the effect of a novel neuromotor reprogramming (NR) treatment based on the use of proprioceptive sensations associated with motor imagery and low frequency sounds (LFS) has not been studied in AMI after knee injuries. Fundamentally, motor imagery and movement execution share substantial overlap of active brain regions that may minimize AMI and quadriceps dysfunction. 20 This tripod-based method (proprioception, motor imagery, and LFS) uses the triggering of a previously learned and stored central nervous system neural program (motor memory) as support. However, the effects of this intervention style on AMI reduction among patients with a history of knee pathologies have not yet been studied.
Therefore, the aim of this study was to assess the quadriceps surface EMG activity during maximal voluntary contraction in persons with AMI after knee injuries who completed 1 session of NR treatment in addition to their standard rehabilitation. We hypothesized that the NR session would activate the quadriceps and improve extension deficits.
Methods
Study Design and Participants
Patients who underwent knee ligament surgery or sustained a knee sprain between May 1, 2021 and February 28, 2022 were considered for study inclusion. Inclusion criteria were all patients with a deficit of >30% of the VMO on EMG testing after their initial rehabilitation in comparison with the contralateral limb. Exclusion criteria were patients with severe cognitive impairment and patients with hearing impairment. Institutional review board approval (COS-RGDS-2021-09-008-SONNERYCOTTET-B) was granted for this retrospective study.
NR Technique and Clinical Outcomes
Before the NR session, walking backward and submaximal voluntary isometric VMO contractions of all patients were recorded on video, allowing the patient to be conscious of their movement before intervention. The patient was placed supine on a table with the involved knee in maximum comfortable extension. The maximal voluntary isometric contractions of the VMO was measured before and immediately after the NR session with a NeuroTrac Simplex Plus (Verity Medical Ltd) EMG device using pairs of surface electrodes (30 mm in diameter, self-adhesive, 0.2-2000 mV with a sensitivity of 0.1 mV root mean square [RMS]). Electrodes were placed on the most prominent bulge of the muscle at a point 80% from a line between the anterior superior iliac spine and the joint space in front of the anterior border of the medial ligament as per the European recommendations for surface EMG. 12 Participants were then asked to perform 3 maximal voluntary isometric contractions for 6 s, separated from each other by a 10-s period for recovery. These were performed in the right limb and the left limb successively before the intervention. To provide a more reliable recording, dual-channel EMG monitoring was used. As a result, the contractions were recorded at the same time without having to change the connections from one knee to the other. After each maximal voluntary contraction, the EMG device screen automatically displayed the mean EMG amplitude of the muscle activity of the VMO surface, which was calculated for a 6-s contraction. The device displayed the RMS signal received for EMG recording with 3 bandpass filters applied (wide: 18 ± 4 Hz, narrow: 100 ± 5 Hz, and notch filter: 50 Hz). The measurement was read and recorded to the nearest millivolt. An identical procedure was performed immediately after the NR session.
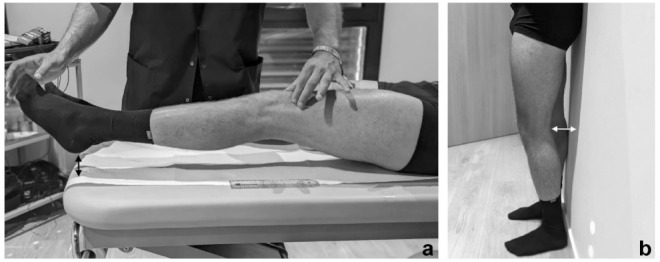
Knee extension deficit was estimated with measurements during static muscle contraction and active movement. During static muscle contraction, subjects were instructed to maintain an upright standing posture with their scapula and their heel against the wall. Bilateral measurements were then taken to determine the distance between their popliteal fossa and the wall (DPW) while they were at rest (Figure 1b). During active movement, the practitioner lifted the heel of the patient by holding the big toe. 5 The patient was asked to hold this phase, focusing on isometric quadriceps contractions for a few seconds. During the contraction, the practitioner checked the correct contraction of the muscle by looking for patella migration and absence of quadriceps and hamstrings cocontraction (Figure 1a). The distance between the heel and the table (DHT) was measured during the contraction (0 cm, patient is not able to maintain the isometric quadriceps contraction; 4 cm, patient is able to lift and hold the heel 4 cm above the table). To evaluate knee function before and after the intervention, the simple knee value (SKV) was used, which asks the participant “How would you rate your knee’s function today as a percentage of normal (0-100% scale with 100% being normal)?”. 24
Figure 1.
Technique for measuring knee extension deficit. (a) Distance between the heel and the table (DHT) during VMO contraction and holding the heel up (black arrow). (b) Distance between the popliteal fossa and the wall (DPW) during stand-up position (white arrow).
Indeed, there is evidence of a link between auditory and motor systems in the brain that could justify utilization of LFS, and it has long been established that proprioceptive training and motor imagery can yield meaningful improvements in motor function. 1
The Alphabox (Allyane) provides 2 types of LFS through headphones. The first type of sound, known as “pulsed sounds,” ranged from 200 to 400 Hz. The second type of sound, known as “associated sounds” (from 50 to 150 Hz) was chosen by the patient during the NR session to ensure listening comfort.
The NR technique (or Allyane method) is composed of 4 different periods involving motor imagery practice, proprioception, and listening to LFS (Figure 2). Participants were instructed to mentally simulate maximal voluntary isometric VMO contraction without overt execution, corresponding to motor imagery practice. With as much visual detail as possible, patients were requested to imagine contracting their VMO and the perceived force and effort associated with the movement. Maximal voluntary isometric VMO contraction mental representation was repeated until significant feeling and sensations of muscle contractions were perceived. Some periods during the session were associated with LFS such as relating a stimulus with a particular dynamic mental state, which may allow better associative learning. The time dedicated for each period included mental practice and listening to LFS depending on the period. Patients received practitioner instructions for the next period during the interval between periods. The detailed instruction for each period is presented in the online Appendix (available in the online version of this article).
Figure 2.
Description of neuromotor reprogramming.
Statistical Analysis
Descriptive statistics were calculated to summarize the demographics and clinical characteristics and described using means and standard deviations. After passing the Shapiro-Wilk test for normality, paired t tests on the differences of all scores obtained before and after session were used to compare the pre- and post-NR results. If the condition of normality is not met, the Wilcoxon sign rank test was used for paired samples. The level of significance was set at P < 0.05 for all statistical tests. All analyses were performed using R Statistical Software (Version 3.6.3; R Foundation for Statistical Computing). Cohen’s d was used to study effect size.
Results
Patient Demographics
A total of 30 patients were included in the study; 13 patients were male (43%) and 14 injuries were to the right knee (47%). The mean age of the patients was 34.6 ± 10.1 years (range, 14-50 years). Based on distance tests (DHT, DPW), 4 patients did not have an extension deficit (13%). A total of 26 patients presented postoperatively after anterior cruciate ligament (ACL) reconstruction (ACLR) (87%) and 4 patients after a knee sprain (13%). The average time to assessment was 1.6 ± 0.43 months (range, 1-2 months) from injury and 11.18 ± 10.3 months (range, 0.5-36.5 months) from surgery.
Clinical Outcomes
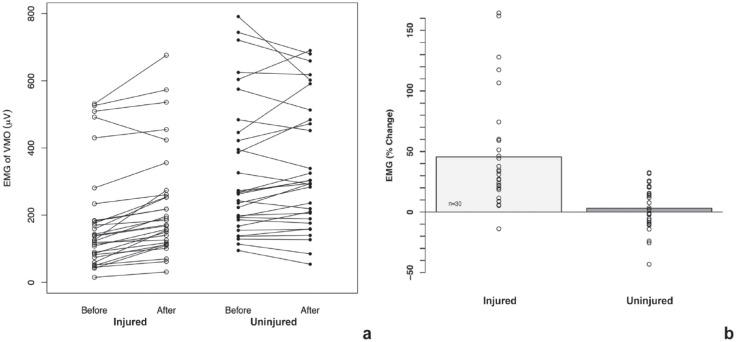
While there was no significant difference when comparing the healthy limb VMO activity at baseline and after the NR session (P = 0.66, d = 0.08), the VMO activation for the injured limb was significantly higher after the NR (P < 0.01, d = 1.10, Figure 3a). Except for 1 participant (-13.8%), the mean difference in the VMO EMG for the injured limb increased from 5.3% to 164.4%. The mean change after 1 session of NR was 45% (range, -13.8 to -164.4%) for the injured limb compared with 3% (range, -43.16 to -32.51%) for the uninjured limb (Figure 3b).
Figure 3.
Mean EMG change for the injured and uninjured limbs during maximum voluntary isometric contraction. (a) Mean EMG changes across individual patients. (b) Mean EMG increase at the group level. Positive values indicate an increase of VMO activity after intervention compared with baseline. EMG, electromyographic; VMO, vastus medialis oblique.
Knee extension deficit was estimated by 2 measurements. First, the distance in centimeters between the heel and the table while holding the foot above the table in a supine position (DHT) assessing active movement. Second, the distance in centimeters between the popliteal fossa and the wall in standing posture, shoulder blades and buttocks touching the wall (DPW) assessing static muscle contraction. Based on DHT and DPW measurements between limbs, 87% of patients had an extension deficit before the intervention. After the session, the DHT of the injured limb improved significantly (P < 0.01; +2.1 cm; d = 1.21; Figure 4a). In addition, the DPW for the injured limb was significantly lower (P < 0.01; d = 1.21) in a straight upright position indicating an improvement in knee extension (+2.21 cm; Figure 4b).
Figure 4.
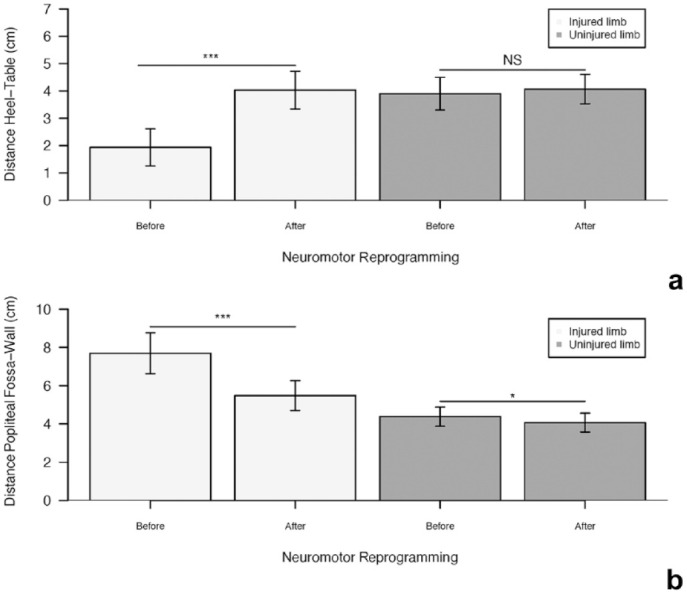
Barplots with 95% CIs (error bars) of extension deficit measurements before and after NR. (a) DHT during VMO contraction and holding the heel up. (b) DPW during stand-up position. *P < 0.05, ***P < 0.01. DHT, distance between the heel and the table; DPW, distance between the popliteal fossa and the wall; NR, neuromotor reprogramming; NS, not statistically significant; VMO, vastus medialis oblique.
Uninjured limb deficit extension measurements revealed a significant difference from baseline after the NR session for DPW (P = 0.05; -0.31 cm; d = 0.44; Figure 4b) but no significant difference for DHT (P = 0.40, d = 0.13; Figure 4a).
Pre- and post-SKV scores demonstrated significant improvements concerning the injured limb knee function after an NR session (P < 0.01, d = 1.71; Figure 5). Patients graded their knee functionality as 50% compared with a healthy knee before the session and 67.5% after the session (+17.5%).
Figure 5.
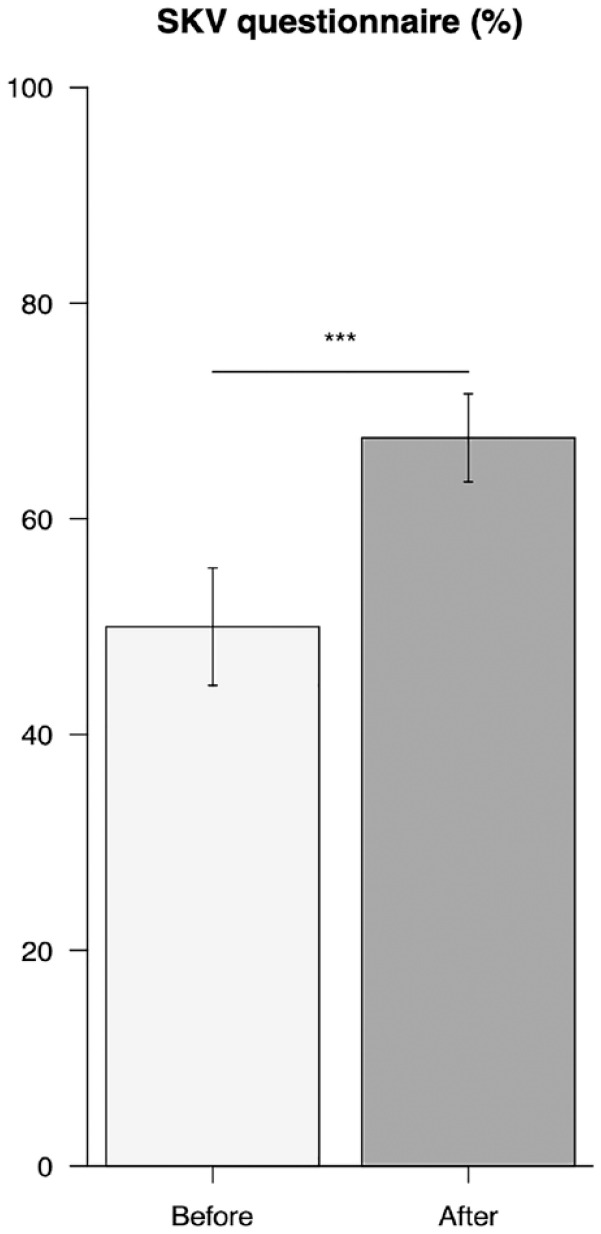
Scores of self-reports on knee function (SKV) before and after NR session. Error bars, 95% CI; P < 0.01. NR, neuromotor reprogramming.
Discussion
The main finding of this study was that 1 session of NR is effective in activation of the VMO and in improving extension deficits. These findings suggest that this therapeutic approach to treat AMI with noninvasive and no-contact treatment as a complement of normal rehabilitation is advantageous.
Our findings agree with those of previous researchers who reported VMO activation patterns altered, as identified by EMG, after ACL injury and its surgical management.7,10,18,25 We observed that the EMG amplitude of the injured limb at different timescales after injury remained significantly reduced in comparison with the uninjured limb with respect to VMO contraction. This is not surprising given that knee muscle weakness after ACL injury can be persistent from 3 months to 20 years.32,39 In accordance with our results, previous studies have suggested that decreased voluntary activation might be explained, at least partly, by alterations in corticospinal excitability, also termed AMI. 20
Quadriceps AMI has been shown to contribute to posttraumatic knee injury deficits including muscle size and extension deficit, which limits the ability to progress during rehabilitation.8,19 In the management of AMI, most clinicians base their programs on atrophy minimization and full muscle strength recovery. Specifically, hamstring fatigue exercises may improve quadriceps activation but do not overcome muscle inhibition. 16 Recently, studies have demonstrated both neural excitability differences and cortical reorganization occurrence in injured persons, in particular patients with ACL injuries when compared with uninjured subjects.20,27 These studies highlighted both the requirement of special training programs other than regular physical activities and the need to identify interventions aimed to impact the neurological aspect of quadriceps weakness. Whereas our study investigated the short-term clinical effects of NR, which combined the use of motor imagery, proprioception, and LFS listening, there is evidence to suggest that motor imagery techniques could be effective to reduce postinjury consequences.27,30 Indeed, motor imagery may influence neural modulation, providing better biofeedback of joints and muscles, as well as facilitating motor excitability.17,33 Interestingly, some studies have demonstrated that corticospinal facilitation during motor imagery is associated with proprioception, suggesting that afferent feedback affects the central motor imagery processes.26,41 In addition, it is important to note that applied music listening interventions in postoperative rehabilitation settings improve the rehabilitation effectiveness in patients with total knee replacement, demonstrating the potential to explore the link between auditory and motor systems in the brain. 14
Our study reported that the NR session resulted in an estimated 45% VMO activity improvement of the injured limb, whereas the uninjured limb had a 3% increase on average after a 1-h intervention (Figure 3). To the best of the authors’ knowledge, studies investigating EMG amplitude changes after a single session for the injured limb undergoing reconstruction of the ACL or suffering from a knee sprain, did not report both superior improvement and effect size for the intervention (ie, medium effect sizes for the cryotherapy treatment on vastus medialis activation deficits indexed from EMG measures).22,34 Nevertheless, even if these findings suggest that NR session could increase the availability of inhibited motor neurons (responsible for VMO weakness) for the injured knee joint in the short term, these results and the absence of a control group do not provide enough evidence to consider this technique efficient alone.
Indeed, the goal of using NR is to allow better motor unit recruitment to optimize physical exercise effects during knee rehabilitation. Whereas the majority of studies investigating AMI management relate to its biomechanical effects, these findings illustrate the importance of multidisciplinary management, as in the case of NR, to act on neurological influences.
Surprisingly, although the NR session is a mental unilateral practice, VMO EMG amplitude change relative to the uninjured limb after intervention can be estimated at 3%. As already reported in crosseducation investigations,1,9,23 the very small amounts of EMG activation (range, 1%-6%) after unilateral training are too small to be considered as significant. Nevertheless, our findings demonstrate the same rate of EMG change for an uninjured limb after mental unilateral practice, suggesting further investigation into the effects of a crosseducation event during mental practice.
There are some limitations to this study that should be considered. First, measurements of VMO activation could differ from the time of injury, limiting the conclusions that can be drawn from our results. Second, our results are based on EMG data providing indirect muscle activation measurements, supporting the necessity of direct techniques in future randomized controlled studies. In addition, further studies are needed both to examine the long-term effects of this NR session to confirm these results and to compare this intervention against a control group.
Conclusion
This study has demonstrated that this novel multidisciplinary treatment modality for AMI can enhance outcomes, especially the restoration of quadriceps neuromuscular function and reduction of extension deficits after knee injury or surgery. Although these results need confirmation in a randomized clinical trial, our study provides a rationale for the use of this noninvasive NR technique using motor imagery, proprioception, and LFS in patients with knee injuries.
Supplemental Material
Supplemental material, sj-docx-1-sph-10.1177_19417381231169285 for Neuromotor Treatment of Arthrogenic Muscle Inhibition After Knee Injury or Surgery by Typhanie Dos Anjos, François Gabriel, Thais Dutra Vieira, Graeme Philip Hopper and Bertrand Sonnery-Cottet in Sports Health
Footnotes
The following authors declared potential conflicts of interest: T.D.V. received collaborative research funding from Allyane. B.S-C. is a paid consultant for Arthrex and has received royalties from Arthrex.
ORCID iDs: Thais Dutra Vieira  https://orcid.org/0000-0002-1624-1824
https://orcid.org/0000-0002-1624-1824
Bertrand Sonnery-Cottet  https://orcid.org/0000-0002-6837-0425
https://orcid.org/0000-0002-6837-0425
References
- 1. Andrushko JW, Gould LA, Farthing JP. Contralateral effects of unilateral training: sparing of muscle strength and size after immobilization. Appl Physiol Nutr Metab. 2018;43(11):1131-1139. [DOI] [PubMed] [Google Scholar]
- 2. Bierke S, Abdelativ Y, Hees T, et al. Risk of arthrofibrosis in anatomical anterior cruciate ligament reconstruction: the role of timing and meniscus suture. Arch Orthop Trauma Surg. 2021;141(5):743-750 [DOI] [PubMed] [Google Scholar]
- 3. Bremner CB, Holcomb WR, Brown CD, Perreault ME. The effectiveness of neuromuscular electrical stimulation in improving voluntary activation of the quadriceps: a critically appraised topic. J Sport Rehab. 2017;26(4):316-323. [DOI] [PubMed] [Google Scholar]
- 4. Clayton RAE, Court-Brown CM. The epidemiology of musculoskeletal tendinous and ligamentous injuries. Injury. 2008;39(12):1338-1344. [DOI] [PubMed] [Google Scholar]
- 5. Delaloye JR, Murar J, Sánchez MG, et al. How to rapidly abolish knee extension deficit after injury or surgery: a practice-changing video pearl from the Scientific Anterior Cruciate Ligament Network International (SANTI) Study Group. Arthrosc Tech. 2018;7(6):e601-e605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Deroche E, Batailler C, Swan J, Lustig S, Servien E. Significant risk of arthrolysis after simultaneous anterior cruciate ligament reconstruction and treatment of dislocated bucket-handle meniscal tear. Orthop Traumatol Surg Res. 2022;108(3):103252. [DOI] [PubMed] [Google Scholar]
- 7. Drechsler WI, Cramp MC, Scott OM. Changes in muscle strength and EMG median frequency after anterior cruciate ligament reconstruction. Eur J Appl Physiol. 2006;98(6):613-623. [DOI] [PubMed] [Google Scholar]
- 8. Dutaillis B, Maniar N, Opar DA, Hickey JT, Timmins RG. Lower limb muscle size after anterior cruciate ligament injury: a systematic review and meta-analysis. Sports Med. 2021;51(6):1209-1226. [DOI] [PubMed] [Google Scholar]
- 9. Farthing JP, Chilibeck PD, Binsted G. Cross-education of arm muscular strength is unidirectional in right-handed individuals. Med Sci Sports Exerc. 2005;37(9):1594-1600. [DOI] [PubMed] [Google Scholar]
- 10. Gabler C, Kitzman PH, Mattacola CG. Targeting quadriceps inhibition with electromyographic biofeedback: a neuroplastic approach. Crit Rev Biomed Eng. 2013;41(2):125-135. [DOI] [PubMed] [Google Scholar]
- 11. Hart JM, Kuenze CM, Diduch DR, Ingersoll CD. Quadriceps muscle function after rehabilitation with cryotherapy in patients with anterior cruciate ligament reconstruction. J Athl Train. 2014;49(6):733-739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hermens HJ, Freriks B, Disselhorst-Klug C, Rau G. Development of recommendations for SEMG sensors and sensor placement procedures. J Electromyogr Kinesiol. 2000;10(5):361-374. [DOI] [PubMed] [Google Scholar]
- 13. Hopkins JT, Ingersoll CD. Arthrogenic muscle inhibition: a limiting factor in joint rehabilitation. J Sport Rehab. 2000;9(2):135-159. [Google Scholar]
- 14. Hsu CC, Chen WM, Chen SR, Tseng YT, Lin PC. Effectiveness of music listening in patients with total knee replacement during CPM rehabilitation. Biol Res Nurs. 2016;18(1):68-75. [DOI] [PubMed] [Google Scholar]
- 15. Konishi Y, Yoshii R, Ingersoll CD. Gamma loop dysfunction as a possible neurophysiological mechanism of arthrogenic muscle inhibition: a narrative review of the literature. J Sport Rehabil. 2022;31(6):736-741. [DOI] [PubMed] [Google Scholar]
- 16. Kuenze CM, Kelly AR, Jun HP, Eltoukhy M. Unilateral quadriceps strengthening with disinhibitory cryotherapy and quadriceps symmetry after anterior cruciate ligament reconstruction. J Athl Train. 2017;52(11):1010-1018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Lebon F, Guillot A, Collet C. Increased muscle activation following motor imagery during the rehabilitation of the anterior cruciate ligament. Appl Psychophysiol Biofeedback. 2012;37(1):45-51. [DOI] [PubMed] [Google Scholar]
- 18. Lent M, Drost M, Wildenberg FAJM van den. EMG profiles of ACL-deficient patients during walking: the influence of mild fatigue. Int J Sports Med. 1994;15(8):508-514. [DOI] [PubMed] [Google Scholar]
- 19. Lepley AS, Grooms DR, Burland JP, Davi SM, Kinsella-Shaw JM, Lepley LK. Quadriceps muscle function following anterior cruciate ligament reconstruction: systemic differences in neural and morphological characteristics. Exp Brain Res. 2019;237(5):1267-1278. [DOI] [PubMed] [Google Scholar]
- 20. Lepley AS, Lepley LK. Mechanisms of arthrogenic muscle inhibition. J Sport Rehabil. 2021;31(6):707-716. [DOI] [PubMed] [Google Scholar]
- 21. Lepley LK, Wojtys EM, Palmieri-Smith RM. Combination of eccentric exercise and neuromuscular electrical stimulation to improve biomechanical limb symmetry after anterior cruciate ligament reconstruction. Clin Biomech (Bristol, Avon). 2015;30(7):738-747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Loro WA, Thelen MD, Rosenthal MD, Stoneman PD, Ross MD. The effects of cryotherapy on quadriceps electromyographic activity and isometric strength in patient in the early phases following knee surgery. J Orthop Surg (Hong Kong). 2019;27(1):230949901983145. [DOI] [PubMed] [Google Scholar]
- 23. Magnus CRA, Barss TS, Lanovaz JL, Farthing JP. Effects of cross-education on the muscle after a period of unilateral limb immobilization using a shoulder sling and swathe. J Appl Physiol. 2010;109(6):1887-1894. [DOI] [PubMed] [Google Scholar]
- 24. Marot V, Justo A, Alshanquiti A, et al. Simple knee value: a simple evaluation correlated to existing knee PROMs. Knee Surg Sports Traumatol Arthrosc. 2021;29(6):1952-1959. [DOI] [PubMed] [Google Scholar]
- 25. McNair PJ, Wood GA. Frequency analysis of the EMG from the quadriceps of anterior cruciate ligament deficient individuals. Electromyogr Clin Neurophysiol. 1993;33(1):43-48. [PubMed] [Google Scholar]
- 26. Mercier C, Aballea A, Vargas CD, Paillard J, Sirigu A. Vision without proprioception modulates cortico-spinal excitability during hand motor imagery. Cerebral Cortex. 2008;18(2):272-277. [DOI] [PubMed] [Google Scholar]
- 27. Norte G, Rush J, Sherman D. Arthrogenic muscle inhibition: best evidence, mechanisms, and theory for treating the unseen in clinical rehabilitation. J Sport Rehabil. 2021;31(6):717-735. [DOI] [PubMed] [Google Scholar]
- 28. Oda S, Izumi M, Takaya S, et al. Promising effect of visually-assisted motor imagery against arthrogenic muscle inhibition - a human experimental pain study. J Pain Res. 2021;14:285-295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Palmieri-Smith RM, Lepley LK. Quadriceps strength asymmetry after anterior cruciate ligament reconstruction alters knee joint biomechanics and functional performance at time of return to activity. Am J Sports Med. 2015;43(7):1662-1669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Pastora-Bernal JM, Estebanez-Pérez MJ, Lucena-Anton D, García-López FJ, Bort-Carballo A, Martín-Valero R. The effectiveness and recommendation of motor imagery techniques for rehabilitation after anterior cruciate ligament reconstruction: a systematic review. JCM. 2021;10(3):428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Pietrosimone BG, McLeod MM, Lepley AS. A theoretical framework for understanding neuromuscular response to lower extremity joint injury. Sports Health. 2012;4(1):31-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Pietrosimone BG, Saliba SA, Hart JM, Hertel J, Ingersoll CD. Contralateral effects of disinhibitory tens on quadriceps function in people with knee osteoarthritis following unilateral treatment. N Am J Sports Phys Ther. 2010;5(3):111-121. [PMC free article] [PubMed] [Google Scholar]
- 33. Ranganathan VK, Siemionow V, Liu JZ, Sahgal V, Yue GH. From mental power to muscle power - gaining strength by using the mind. Neuropsychologia. 2004;42(7):944-956. [DOI] [PubMed] [Google Scholar]
- 34. Rice D, McNair PJ, Dalbeth N. Effects of cryotherapy on arthrogenic muscle inhibition using an experimental model of knee swelling. Arthritis Rheum. 2009;61(1):78-83. [DOI] [PubMed] [Google Scholar]
- 35. Rice DA, McNair PJ. Quadriceps arthrogenic muscle inhibition: neural mechanisms and treatment perspectives. Semin Arthritis Rheum. 2010;40(3):250-266. [DOI] [PubMed] [Google Scholar]
- 36. Sonnery-Cottet B, Hopper GP, Gousopoulos L, et al. Arthrogenic muscle inhibition following knee injury or surgery: pathophysiology, classification, and treatment. Video J Sports Med. 2022;2(3):263502542210862. [Google Scholar]
- 37. Sonnery-Cottet B, Saithna A, Quelard B, et al. Arthrogenic muscle inhibition after ACL reconstruction: a scoping review of the efficacy of interventions. Br J Sports Med. 2019;53(5):289-298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Tayfur B, Charuphongsa C, Morrissey D, Miller SC. Neuromuscular function of the knee joint following knee injuries: does it ever get back to normal? A systematic review with meta-analyses. Sports Med. 2021;51(2):321-338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Tengman E, Brax Olofsson L, Stensdotter AK, Nilsson KG, Häger CK. Anterior cruciate ligament injury after more than 20 years. II. Concentric and eccentric knee muscle strength. Scand J Med Sci Sports. 2014;24(6):e501-509. [DOI] [PubMed] [Google Scholar]
- 40. Thaunat M, Barbosa NC, Gardon R, et al. Prevalence of knee stiffness after arthroscopic bone suture fixation of tibial spine avulsion fractures in adults. Orthop Traumatol Surg Res. 2016;102(5):625-629. [DOI] [PubMed] [Google Scholar]
- 41. Vargas CD. The influence of hand posture on corticospinal excitability during motor imagery: a transcranial magnetic stimulation study. Cerebral Cortex. 2004;14(11):1200-1206. [DOI] [PubMed] [Google Scholar]
- 42. Yoshida Y, Mizner RL, Ramsey DK, Snyder-Mackler L. Examining outcomes from total knee arthroplasty and the relationship between quadriceps strength and knee function over time. Clin Biomech (Bristol, Avon). 2008;23(3):320-328. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-sph-10.1177_19417381231169285 for Neuromotor Treatment of Arthrogenic Muscle Inhibition After Knee Injury or Surgery by Typhanie Dos Anjos, François Gabriel, Thais Dutra Vieira, Graeme Philip Hopper and Bertrand Sonnery-Cottet in Sports Health