Abstract
Background
Torture is widespread, with potentially broad and long‐lasting impact across physical, psychological, social and other areas of life. Its complex and diverse effects interact with ethnicity, gender, and refugee experience. Health and welfare agencies offer varied rehabilitation services, from conventional mental health treatment to eclectic or needs‐based interventions. This review is needed because relatively little outcome research has been done in this field, and no previous systematic review has been conducted. Resources are scarce, and the challenges of providing services can be considerable.
Objectives
To assess beneficial and adverse effects of psychological, social and welfare interventions for torture survivors, and to compare these effects with those reported by active and inactive controls.
Search methods
Randomised controlled trials (RCTs) were identified through a search of PsycINFO, MEDLINE, EMBASE, Web of Science, the Cumulative Index to Nursing and Allied Health Literature (CINAHL), the Cochrane Central Register of Controlled Trials (CENTRAL) and the Cochrane Depression, Anxiety and Neurosis Specialised Register (CCDANCTR), the Latin American and Caribbean Health Science Information Database (LILACS), the Open System for Information on Grey Literature in Europe (OpenSIGLE), the World Health Organization International Clinical Trials Registry Platform (WHO ICTRP) and Published International Literature On Traumatic Stress (PILOTS) all years to 11 April 2013; searches of Cochrane resources, international trial registries and the main biomedical databases were updated on 20 June 2014. We also searched the Online Library of Dignity (Danish Institute against Torture), reference lists of reviews and included studies and the most frequently cited journals, up to April 2013 but not repeated for 2014. Investigators were contacted to provide updates or details as necessary.
Selection criteria
Full publications of RCTs or quasi‐RCTs of psychological, social or welfare interventions for survivors of torture against any active or inactive comparison condition.
Data collection and analysis
We included all major sources of grey literature in our search and used standard methodological procedures as expected by The Cochrane Collaboration for collecting data, evaluating risk of bias and using GRADE (Grades of Recommendation, Assessment, Development and Evaluation) methods to assess the quality of evidence.
Main results
Nine RCTs were included in this review. All were of psychological interventions; none provided social or welfare interventions. The nine trials provided data for 507 adults; none involved children or adolescents. Eight of the nine studies described individual treatment, and one discussed group treatment. Six trials were conducted in Europe, and three in different African countries. Most people were refugees in their thirties and forties; most met the criteria for post‐traumatic stress disorder (PTSD) at the outset. Four trials used narrative exposure therapy (NET), one cognitive‐behavioural therapy (CBT) and the other four used mixed methods for trauma symptoms, one of which included reconciliation methods. Five interventions were compared with active controls, such as psychoeducation; four used treatment as usual or waiting list/no treatment; we analysed all control conditions together. Duration of therapy varied from one hour to longer than 20 hours with a median of around 12 to 15 hours. All trials reported effects on distress and on PTSD, and two reported on quality of life. Five studies followed up participants for at least six months.
No immediate benefits of psychological therapy were noted in comparison with controls in terms of our primary outcome of distress (usually depression), nor for PTSD symptoms, PTSD caseness, or quality of life. At six‐month follow‐up, three NET and one CBT study (86 participants) showed moderate effect sizes for intervention over control in reduction of distress (standardised mean difference (SMD) ‐0.63, 95% confidence interval (CI) ‐1.07 to ‐0.19) and of PTSD symptoms (SMD ‐0.52, 95% CI ‐0.97 to ‐0.07). However, the quality of evidence was very low, and risk of bias resulted from researcher/therapist allegiance to treatment methods, effects of uncertain asylum status of some people and real‐time non‐standardised translation of assessment measures. No measures of adverse events were described, nor of participation, social functioning, quantity of social or family relationships, proxy measures by third parties or satisfaction with treatment. Too few studies were identified for review authors to attempt sensitivity analyses.
Authors' conclusions
Very low‐quality evidence suggests no differences between psychological therapies and controls in terms of immediate effects on post‐traumatic symptoms, distress or quality of life; however, NET and CBT were found to confer moderate benefits in reducing distress and PTSD symptoms over the medium term (six months after treatment). Evidence was of very low quality, mainly because non‐standardised assessment methods using interpreters were applied, and sample sizes were very small. Most eligible trials also revealed medium to high risk of bias. Further, attention to the cultural appropriateness of interventions or to their psychometric qualities was inadequate, and assessment measures used were unsuitable. As such, these findings should be interpreted with caution.
No data were available on whether symptom reduction enabled improvements in quality of life, participation in community life, or in social and family relationships in the medium term. Details of adverse events and treatment satisfaction were not available immediately after treatment nor in the medium term. Future research should aim to address these gaps in the evidence and should include larger sample sizes when possible. Problems of torture survivors need to be defined far more broadly than by PTSD symptoms, and recognition given to the contextual influences of being a torture survivor, including as an asylum seeker or refugee, on psychological and social health.
Keywords: Adult; Humans; Mental Health; Cognitive Behavioral Therapy; Cognitive Behavioral Therapy/methods; Human Rights; Human Rights/education; Narrative Therapy; Narrative Therapy/methods; Psychotherapy; Psychotherapy/methods; Psychotherapy, Group; Quality of Life; Quality of Life/psychology; Randomized Controlled Trials as Topic; Refugees; Refugees/psychology; Resilience, Psychological; Stress Disorders, Post‐Traumatic; Stress Disorders, Post‐Traumatic/psychology; Stress Disorders, Post‐Traumatic/therapy; Stress, Psychological; Stress, Psychological/psychology; Stress, Psychological/therapy; Torture; Torture/psychology
Plain language summary
Psychological, social and welfare interventions for the psychological health and well‐being of torture survivors
Why is this review important?
Torture is a widespread problem that can cause lasting and severe physical, psychological, social and welfare problems for survivors. Treatment is offered by various agencies: some provide support in diverse settings from refugee camps to high‐income countries; others support survivors in countries where current or recent repression or armed conflict is known. Resources for these services are scarce, so it is important that they are used to greatest effect to improve the well‐being of torture survivors.
Who will be interested in this review?
Agencies providing health and welfare services for torture survivors; organisations that fund these agencies; torture survivors and those close to them.
What questions does this review aim to answer?
What intervention improves well‐being among torture survivors with psychological, social and welfare problems?
Which studies were included in the review?
We searched the academic literature and the non‐academic literature such as reports of non‐governmental agencies providing services to April 2013, and again to June 2014. Studies had to describe a randomised controlled trial of intervention for psychological, social or welfare problems among torture survivors—adults or children. We found nine trials with 507 adults that examined varied psychological interventions compared with no treatment or a credible alternative treatment. Six trials were conducted at treatment centres in Europe, and three in African refugee settings; all focused on post‐traumatic stress and were of low to moderate quality.
What does the evidence from the review tell us?
Very low‐quality evidence suggests no differences between psychological therapies and controls in terms of an immediate effect on post‐traumatic symptoms, distress or quality of life. However, at six‐month follow‐up, four studies (86 people) showed moderate benefit in terms of post‐traumatic stress and distress. Three trials were of narrative exposure therapy, and one of cognitive‐behavioural therapy, but we have little confidence in these results because the evidence was of very low quality and the trials included very small numbers of people. No studies assessed worsening of problems, nor changes in family and social relationships or community participation, with or without improvement in symptoms.
What should happen next?
Studies need to identify broader aims for intervention and should continue to test a range of interventions consistent with the breadth of problems of torture survivors. Investigators also need to assess changes with validity across cultures and languages.
Summary of findings
Summary of findings for the main comparison. Psychological intervention versus control for psychological health and well‐being of torture survivors.
| Psychological intervention versus control for psychological health and well‐being of torture survivors | ||||||
| Patient or population: people of any age who have survived any type of torture Settings: treatment clinics (Europe) and refugee camps (Africa) Intervention: psychological intervention vs control | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Psychological intervention versus control | |||||
| Reduction on a scale of psychological distress—follow‐up DSM‐based scales: Hamilton Depression Scale, Hopkins Symptom Checklist 25, Beck Depression Inventory Follow‐up: median 6 months | Across studies, mean reduction on a scale of psychological distress at follow‐up in the intervention groups was 0.63 standard deviations lower (1.07 to 0.19 lower) | ‐1.07 to ‐0.19 | 86 (4) | ⊕⊝⊝⊝ very lowa,b,c,d | Corresponds to a mean improvement of 6.4 on the Hamilton Depression Scale, but the score at follow‐up remains at the borderline of severe to very severe depression | |
| Adverse events | No data available | No data available | ||||
| Reduction in post‐traumatic stress symptoms—follow‐up DSM‐based PTSD symptom scales: Clinician Administered PTSD Scale (CAPS), Post‐traumatic Depression Scale, Composite International Diagnostic Interview (CIDI), PTSD scale Follow‐up: median 6 months | Across studies, mean reduction in post‐traumatic stress symptoms at follow‐up in the intervention groups was 0.52 standard deviations lower (0.97 to 0.07 lower) | ‐0.97 to ‐0.07 | 86 (4) | ⊕⊝⊝⊝ very lowa,b,c,d | Mean change of 13.6 points on the CAPS corresponds to a clinically significant change (10‐20 points, depending on population), but follow‐up score still represents substantial symptomatology | |
| Improvement in quality of life—follow‐up | No data available | Data available only immediately post treatment | ||||
| Improvement in participation | No data available | No data available | ||||
| Improvement in family or social relationships | No data available | No data available | ||||
| Satisfaction with treatment | No data available | No data available | ||||
| *The basis for the assumed risk (e.g. median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval. | ||||||
| GRADE Working Group grades of evidence. High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
aThree of the four studies used interpreters for assessment or translation and oral interview. bSubstantial unblinding; transparency of content of measures as focus of treatment; neither conceptual nor linguistic validation of measures. cSubstantial differences among populations. dVery small sample sizes.
Background
Description of the condition
Torture is a gross human rights violation and continues to be practised worldwide (AI 2013). The International Rehabilitation Council for Victims of Torture (IRCT 2010) estimates that around 400,000 torture survivors live in the European Union alone, as well as similar numbers in the USA (Jaranson 1995). These estimates do not include torture survivors who remain in prisons or other detention facilities or refugee camps or in countries where torture continues and those who have not disclosed torture.
Torture is a deliberate assault upon the body, the psyche, the identity and the integrity of the person; it aims to dehumanise, degrade, destroy or debilitate and render the individual helpless. Physical and psychological methods of torture are usually used in combination, and their impact can vary according to the methods used and the context and setting in which torture is inflicted. Torture may impact not only the physical, psychological and interpersonal and social aspects of well‐being, but other aspects as well, such as spiritual. These effects of torture may interact and manifest in complex and diverse ways, mediated by culture, gender and other aspects of the context of the torture survivor, the context of torture and the context of the recovery environment. The impact of torture on a person’s functioning can lead to adverse effects on many areas of the person’s life, including employment. For some, this may result in economic hardship, which can lead to other consequences for the torture survivor, in terms of self‐esteem, sense of agency and quality of life, and for the family of the torture survivor.
The impact of torture on health and well‐being can be immediate and, for some, long‐lasting. Physical health problems related to torture have been widely documented (Jacobs 2001; Moreno 2002; Norredam 2005; for reviews see Jaranson 2011, Montgomery 2011 and Quiroga 2005). Psychological problems related to torture include anxiety, phobias, depression and post‐traumatic stress (Basoglu 2001;Johnson 2008; Patel 2010). Physical health problems not only cause disability or restricted functioning but can impact psychologically, resulting in a significant effect on overall social functioning and well‐being of torture survivors. Torture may affect the individual's interpersonal and familial relationships and may have an impact on the community and on wider society, often by perpetuating fear, uncertainty, mistrust and suspicion and by threatening social cohesion.
In societies undergoing transitional justice processes, continued impunity and lack of access to justice may contribute to fear, mistrust of others and isolation. Stigma related to torture and mental health problems may be experienced as marginalising and silencing. In the case of rape or other sexual violence amounting to torture, the consequences can be health related (e.g. sexual health problems, pregnancy, difficulty forming or maintaining relationships, withdrawal, fear). Consequences may be far‐reaching, particularly when sexual torture leads to other social sanctions such as ineligibility for marriage or ostracism by community and family, or to the perpetration of ‘honour killings’ and other retribution towards survivors, perpetrators and their families. When torture survivors live in countries with continued armed conflict and human rights violations, including torture, and in a context of impunity for perpetrators, the sense of ongoing injustice and threat can further impact their well‐being and their recovery from torture. In countries of exile where torture survivors seek asylum, they may experience many additional difficulties influencing their well‐being (e.g. legal proceedings related to applications for asylum, racism, poverty, inadequate housing and homelessness (Gorst‐Unsworth 1998; Laban 2004)).
Description of the intervention
Documentation of the types of interventions provided to torture survivors is limited. The available literature (Jaranson 2011; McIvor 1995; Quiroga 2005) describes a range of interventions, often offered in combination, specific to the needs of the individual, family and community. Resources include psychological, medical, social welfare, legal, resettlement and reintegration and vocational help, as well as interventions aimed at community support or ‘healing’ and development. We do not address medical interventions here. Interventions to address torture survivors' needs are described in the field mostly as rehabilitation or sometimes as psychosocial interventions, which may be psychological, social, welfare or legal.
Psychological interventions are delivered to the individual, family, group or community with the aim of changing cognitive, emotional or behavioural outcomes. These interventions draw on a variety of theoretical and therapeutic schools but can be grouped into broad models, including behavioural, cognitive‐behavioural, systemic, humanistic, psychodynamic and integrative psychological interventions.
Social interventions may be delivered at individual, group and community levels with the aim of improving interpersonal relationships, social involvement and participation, social integration of individual survivors and their families, and social cohesion. Social interventions may include building communication skills, facilitating the formation and maintenance of relationships, facilitating empowerment and agency and building educational and vocational skills to support reintegration into society. Social interventions can also include community development and resources that can provide a supportive and trusting context for torture survivors and their families.
Welfare interventions are delivered at the level of the individual, family and community with the aim of benefiting survivors’ health and well‐being by improving social conditions, addressing basic needs for food, clothing and adequate housing and meeting educational, employment or vocational needs. Among welfare interventions, legal interventions may be delivered to ensure legal protection (e.g. refugee status), to facilitate access to redress and justice (which can include access to appropriate healthcare) and to provide emotional support for torture survivors.
How the intervention might work
Psychological interventions may or may not be adapted or developed to be relevant to the context of torture survivors and their families (e.g. considering culture, gender and particular belief systems). They may target a specific problem such as flashbacks to the trauma(s) or a broad spectrum of psychological problems such as anxiety and depression and interpersonal relationships. Interventions can effect change via a number of mechanisms, including exposure and/or emotional processing with/or without cognitive restructuring, cognitive processing and/or interpretation and meaning‐making. Psychological interventions may additionally draw on legal principles (as in formally documenting the torture inflicted and its health effects, raising awareness of and supporting the use of mechanisms for redress and accessing justice) as a means of improving survivors’ health and well‐being. Psychological interventions may draw on educational principles (such as raising awareness and understanding of problems related to torture at individual, family and community levels).
Social interventions can effect change by reframing and reinterpreting experience, facilitating social and language skills and communication and strengthening the relationships of survivors with their family or community. Social interventions may improve social functioning, social participation and social and vocational integration, and may restore trust. Social interventions may also draw on legal principles (as in facilitating public recognition of a human rights violation) and educational principles (by raising awareness of torture, its illegality and its effects on communities) to minimise stigmata and marginalisation of torture survivors and their families. Social interventions may facilitate the development of a supportive social context for recovery from torture.
Welfare interventions aim to improve material and environmental conditions and to facilitate access to education or employment or other purposeful activity associated with psychological and physical health and well‐being. Legal interventions, delivered alongside any of the above interventions, can facilitate access to appropriate and timely health care and attainment of justice and legal protection from further harm, thereby contributing to a context of safety associated with psychological and physical health and well‐being.
Why it is important to do this review
In the era of evidence‐based health care, considerable emphasis is placed on services providing interventions demonstrated to be effective. However, evidence for psychological interventions used with torture survivors comes predominantly from studies that involve neither torture survivor populations nor populations diverse in cultural, ethnic, religious and political backgrounds, and whose first language is not English. Both psychological interventions provided to torture survivors and the methods and measures used to evaluate their relevance, effectiveness and impact are based on Western concepts of health and well‐being, which have not been developed or validated with torture survivors from diverse backgrounds. A previous review found that very few studies had been conducted, all with significant limitations, including lack of control groups, variable use of diagnostic criteria, lack of validation of the measures used and very small sample sizes (Jaranson 2011; Quiroga 2005).
Most of the literature on psychological and physical health difficulties experienced by torture survivors (before or without treatment) is based on professional or academic accounts, much in the form of clinical opinions and case studies (for reviews, see Jaranson 2011, Lund 2008 and Quiroga 2005). Relatively little literature is available on outcomes of specific healthcare interventions or on outcomes of a group of psychological, social and welfare interventions delivered simultaneously to torture survivors. What exists is dominated by case studies and clinical narratives, few cohort studies and fewer trials. Some studies have aimed to raise awareness (and funding) for specific initiatives and to inform the wider field, so academic integrity sometimes takes second place to political expediency. In the literature examining psychological outcomes for torture survivors, use of assessment or evaluation tools or measures, which are frequently diagnosis‐based (e.g. focusing on diagnoses of PTSD, depression), is widespread; they have been developed in the West for Western, English‐speaking populations and have been standardised on the same populations. Few of the tools translated for the study of torture survivors have demonstrated validity (Bracken 1995; Johnson 2008; Patel 2003a; Thakker 1999), and many traditional assessment and outcome measures have been criticised for failing to demonstrate linguistic or semantic equivalence, thereby lacking construct validity for culturally diverse populations (e.g. Elsass 2009; Gurr 2001; Hollifield 2002a; Mahtani 2003; Newlands 2004; Patel 2000; Van Ommeren 2001). Such populations include torture survivors amongst refugees and asylum seekers, communities undergoing transitional justice processes and those living under ongoing armed conflict.
A vast body of research describes psychological interventions addressing PTSD in various populations; rarely are such studies based on torture survivor samples (Bisson 2009; Nicholl 2004). As such, they may neglect the range of difficulties (e.g. grief, social isolation), the range of contextual conditions (e.g. racism, destitution, ongoing threat of torture or other harm) and the range of needs experienced by torture survivors. Numerous methodological problems are associated with applying psychiatric diagnostic criteria to this client group (Quiroga 2005), and questions remain about the validity of psychiatric diagnoses in general (Boyle 1999; Boyle 2002; Kutchins 1997; Pilgrim 1999; Rapley 2011). In particular, the validity of a diagnosis of PTSD among torture survivors has been challenged as medicalising the sociopolitical problem of torture (Bracken 1995; Bracken 1998; Patel 2003a; Summerfield 2001) and as psychologising a human rights violation narrowly within a trauma paradigm (Patel 2011).
No systematic reviews have explored which interventions are effective with torture survivors experiencing a range of psychological, social, welfare and interpersonal problems, hence the need for this systematic review. In view of the wide range of evidence that might be relevant to the care and treatment of this population, this review is intended to be as inclusive as possible.
Objectives
To assess beneficial and adverse effects of psychological, social and welfare interventions for torture survivors, and to compare these effects with those reported by active and inactive controls.
Methods
Criteria for considering studies for this review
Types of studies
Randomised controlled trials (RCTs), cluster RCTs and quasi‐randomised controlled trials (QRCTs) were included. QRCTs were included because, given the difficulties of conducting RCTs in this population, a very small number of RCTs were expected to be found.
No restrictions were placed on publication type, status, language or date. If full details were available from the study authors, conference abstracts were included, as relevant material is often published by torture survivor centres themselves. When there was an indication of data in conference publications and attempts to contact study authors were unsuccessful, studies were assigned to Studies awaiting classification.
Types of participants
Participant characteristics
Male and female participants of all ages and of any ethnicity were included. Torture survivors are found among refugees, asylum seekers, war survivors and survivors of organised violence.
Diagnosis
Formal diagnoses in these populations are frequently unavailable, so the review included people who have survived any type of torture, as defined by the study authors.
Co‐morbidities
We included studies that involved people with any physical or psychiatric co‐morbidities.
Setting
Any setting, including healthcare facilities, refugee camps, prison and detention facilities, survivors' homes and communities, was included.
Subset data
When torture survivors constituted some but not all of the study population and were not described separately in trial results, the decision on inclusion or exclusion of the study was made by referring to details of traumatic events sustained by the population as provided in the paper; subset data also consisted of other details of the study concerning prevailing conditions at the time that would have affected those participants not identified as torture survivors and information on prevailing conditions obtained from sources other than the study authors.
Types of interventions
Experimental intervention
Interventions provided in this field tend to be pragmatic and rarely follow treatment manuals/protocols or meet the strict criteria expected in other settings. For this reason, our inclusion criteria were broad. In Appendix 1, we set out a full list of the psychological therapies provided, as defined by the Depression, Anxiety and Neurosis Group of The Cochrane Collaboration, so that readers can understand how these therapies relate to one another.
We included any psychological, social or welfare intervention that aimed to improve the health and well‐being of torture survivors.
Psychological interventions. These included psychodynamic and psychoanalytical therapies, behavioural and cognitive psychotherapies (including cognitive‐behavioural therapy (CBT) and exposure therapy), interpersonal psychotherapy, narrative therapy, cognitive analytic therapy, anxiety/stress management approaches, systemic psychotherapies, counselling, supportive and experiential psychotherapies, art therapy, drama therapy, dance therapy, eye movement desensitisation reprocessing (EMDR) and hypnotherapy. These interventions are undertaken with individuals or with families or groups.
Social interventions. These consist of involvement in community activities, reparation and judicial activities, educational initiatives (such as learning the host country language) and others.
Welfare interventions. These are exemplified by information about legal and welfare rights and entitlements, nursery and school places available for children, productive and creative activities including work initiatives and others.
Comparators
Control comparisons could include waiting list, no treatment, standard care/access to standard care, attention control or alternative treatment that was likely to engender expectations of improvement in people allocated to that condition, such as education, or facilitated group support. We included trials in which the intervention was added to non‐psychosocial standard care given to both groups. Rehabilitation services for torture survivors have arisen largely from psychological interventions. Medical interventions, including pharmacotherapy, when offered, are usually given in combination with other psychosocial interventions and were excluded from the review.
Types of outcome measures
One of the objectives of this review is to describe the outcomes evaluated in these studies. We included any measures of psychological health benefit and well‐being, continuous or categorical. However, studies of populations that include torture survivors address a very wide range of outcomes, including many non‐standardised measures specifically developed for that study (Jaranson 2011). Rarely do measures undergo the conceptual scrutiny that should precede translation and testing (Johnson 2006), and many measures are not translated into the first or fluent language of research participants and tested before use (only a few trauma instruments have been translated and have undergone validity testing in some languages). Furthermore, it is not uncommon to use interpreters to assist in research (see Vara 2012 for additional details), potentially compromising reliability (e.g. by introducing variation in the use of terms and response options).
Primary outcomes
Reduction on a scale of psychological distress, such as a measure of depression (e.g. Beck Depression Inventory) or a broader mental health scale (e.g. Short Form Health Survey (SF‐12) Mental Health subscale).
Any adverse event such as suicide or self‐harm, or reported increase in post‐traumatic stress disorder (PTSD) symptoms.
Secondary outcomes
Change (positive or negative) in psychological status or target behaviour. This is variously measured as change in psychological and emotional symptoms (such as depression, PTSD, anxiety), suitable to be pooled; or as change in diagnostic category (such as depression or PTSD); or as individual or group level change in a target behaviour.
Change (positive or negative) in quality of life or well‐being for which multiple scales are available to assess quality of life or global satisfaction with life and extent of disability.
Increased participation and functioning, as measured by engagement in education, training, work or community activity.
Change in quality and/or quantity of family or social relationships.
Ratings of psychological function made by others, including clinicians; and for children by parents or teachers (ratings by parents or teachers of children's status are widely used in psychological interventions).
Ratings of the intervention itself, such as satisfaction with the intervention, or of the therapeutic alliance.
Timing of outcome assessment
Immediately post treatment.
Medium‐term to long‐term: at least 3 months after the end of treatment. When more than one follow‐up assessment is performed, the longest up to one year will be used.
Hierarchy of outcome measures
When more than one outcome measure is included in the domain of interest, as defined in outcomes, and both describe the domain adequately, preference will be given to a measure that is also used by other trials in the analysis, and secondarily to any measure that authors state was tested for suitability in the population included in the trial.
Search methods for identification of studies
Searches of Cochrane resources and of the main biomedical databases were conducted by The Cochrane Collaboration Depression, Anxiety and Neurosis Review Group (CCDAN) Trials Search Co‐ordinator (TSC) to 20 June 2014; other electronic resources were searched (11 April 2013) by one review author (BK), and searching of websites and handsearching of reviews and reference lists were conducted by two review authors (BK, AW).
Electronic searches
Bibliographic databases and trial registers were searched from the start of database coverage to 20 June 2014.
OVID PsycINFO (online database of psychological literature) (Appendix 2).
OVID MEDLINE (online database of health and medical journals and other news sources) (Appendix 3).
OVID EMBASE (online database of health and medical journals) (Appendix 4).
Cochrane Central Register of Controlled Trials (CENTRAL) (Appendix 5).
Cochrane Depression, Anxiety and Neurosis Group Specialised Register (CCDANCTR) (Appendix 6).
ClinicalTrials.gov and WHO: International Clinical Trials Registry Platform (ICTRP) (Appendix 7).
Bibliographic databases were searched from the start of database coverage to 11 April 2013.
EBSCO Cumulative Index to Nursing and Allied Health Literature (CINAHL) (online database of nursing and allied health literature) (Appendix 8).
Web of Science (online multi‐disciplinary database covering all sciences) (Appendix 9).
Latin American and Caribbean Health Science Information Database (LILACS) (online database on health sciences, published in Latin America and the Caribbean) (Appendix 10).
Open System for Information on Grey Literature in Europe (OpenSIGLE) (online database of reports and other grey literature produced in Europe until 2005) (Appendix 11).
ProQuest Published International Literature On Traumatic Stress (PILOTS) (online database) (Appendix 12).
Searching other resources
Online Library of the Rehabilitation and Research Centre for Torture Victims (RCT) (Appendix 13); this is now called Dignity (Danish Institute against Torture).
Reference lists of reviews emerging from the searches.
Reference lists from the final set of included studies.
Tables of contents from the top 10 most frequently cited sources emerging from the search (expected to be journal issues), using the search terms outlined in Appendix 14.
Contact with authors of studies for which a reference was found (e.g. conference abstracts) but that was not yet published.
Search terms
Search terms were deliberately broad, as many studies are conducted in non‐Western, non‐academic settings, with diverse reporting structures. The following strategy was employed for the main bibliographic databases: (Population + RCT filter) OR (Population + Intervention).
Grey literature
To identify relevant grey literature, the RCT library and OpenSIGLE were included in the list of databases to be searched. In addition, a range of publication types such as reports, conference papers, posters, monographs and anthologies were included in the search.
Reference manager software
References were managed using the bibliographic software EndNote.
Data collection and analysis
Selection of studies
Study selection occurred in two stages.
An initial screening of titles and abstracts was conducted using the inclusion criteria, with the aim of identifying studies that may be eligible and for which the full paper was obtained. This was done independently by two review authors (BK, AW). When abstracts were not available electronically, full papers were sought.
Full papers were read and selected against the inclusion criteria by two of the review authors (BK, AW) independently. The final list was achieved after comparison, and disagreements were resolved by discussion; when doubt or difference could not be resolved, the third review author (NP) was consulted to achieve consensus.
When full details could be obtained from the study authors, conference abstracts were included, as relevant material is often published by torture survivor rehabilitation centres themselves. When there was an indication of data in conference publications and contact with study authors was unsuccessful, such studies were assigned by review authors to Studies awaiting classification.
Data extraction and management
A data extraction form was designed to document the following study details by using as a model data extraction protocols from similar reviews.
Study design.
Setting of intervention.
Types of interventions.
Intervention protocol.
Sample size at baseline and outcome assessments.
Baseline characteristics of the sample (age, gender, nationality, ethnicity, type of torture experienced, legal status if refugees and asylum seekers, living situation, separation from close family members).
Baseline measures.
Types of practitioners/therapists.
Language/s of assessment; translation, interpretation.
Properties of baseline measures (language, translation, validity).
Outcome measures at end of intervention(s) and at follow‐up assessment.
Completion rates.
Adherence to, participation in treatment.
Risk of bias of included studies.
Data were extracted by two of the review authors (BK, AW) independently, and disagreements were resolved by discussion. When doubt or difference could not be resolved, the third review author (NP) was consulted to achieve consensus.
Main comparisons
Psychological intervention, treatment versus any control.
Social intervention, treatment versus any control.
Welfare intervention, treatment versus any control.
We combined all control arms because they represent a continuum of extent of intervention from waiting list (when other treatment may or not be proscribed, and may or may not be declared by the participant) through treatment as usual (which may be minimal or waiting for treatment) to an active intervention much shorter than the treatment arm (such as a single session of education) up to an active intervention that is matched as far as possible with treatment for non‐specific aspects of therapy such as hours of contact, nature (individual or group) of contact, setting and so forth. Further, information on the content and process of control arms is often missing from published papers, making it impossible, for instance, to classify 'no treatment' as a different condition from 'treatment as usual.'
Assessment of risk of bias in included studies
Risk of bias was assessed for each included study using the 'Risk of bias' tool of The Cochrane Collaboration (Higgins 2008a) and issues raised around studies of psychological interventions included in systematic reviews (Yates 2005). The following domains were considered.
Sequence generation: Was the allocation sequence adequately generated by a method unrelated to recruitment decision?
Allocation concealment: Was allocation adequately concealed?
Blinding of participants and personnel (performance bias): Was knowledge of the allocated treatment adequately prevented during the study? Or were expectations of benefit from treatment equivalent across treatment and control arms at the start of treatment?
Blinding of outcome assessment for each main outcome (detection bias): As most outcome assessment is done by self‐report, were assessments performed by third parties who were blind to treatment allocation?
Incomplete outcome data for each main outcome or class of outcomes: Were incomplete outcome data adequately addressed?
Selective outcome reporting: Do the results presented match the assessments described?
Other sources of bias: Was the study apparently free of other problems that could put it at high risk of bias? Items included here are therapist allegiance/conflict of interest, treatment fidelity, therapist qualifications (see Yates 2005) and translation procedures followed for assessment.
Therapist allegiance refers to therapists' beliefs and investment in benefit for the active arm of intervention over control arm/s. Treatment fidelity refers to manualisation of treatment, as this should lead to greater consistency among therapists and clearer distinction from control conditions when they involve intervention, as well as adherence to the manual. Therapist qualifications and training enhance adherence to prescribed and avoidance of proscribed methods. All of these are discussed further in Yates 2005.
Assessment of risk of bias used three categories: low risk, unclear risk (information not provided or effect not clear) and high risk. A risk of bias table was constructed for each study. Risk of bias was assessed independently by two review authors (BK, AW), and remaining disagreements were referred to the third review author (NP). When necessary, further information was sought from study authors.
Measures of treatment effect
Continuous data were analysed using standardised mean differences (SMDs, or effect sizes) with pooled standard deviations and weighting for sample size and with calculation of the 95% confidence interval. Self‐rating or other rating scales may risk reporting of severely skewed data, that is, when they produce a value between ‐1 and +1 when the difference between the scale maximum or minimum and the mean is divided by the standard deviation. We planned to normalise data that were severely skewed by using transforms or, if this did not produce a satisfactory distribution, by dichotomising. Standardised mean differences would then be interpreted individually with reference to the quality and reliability of the measure when available. However, it remained likely that some severely skewed data would have to be excluded from analyses.
Dichotomous outcomes (improved/not improved) were analysed using odds ratios with 95% confidence intervals. We planned to recategorise into two groups any categorical outcomes with more than two categories (such as improved, same, worse). We did not plan to calculate numbers needed to treat for an additional beneficial outcome (NNTBs).
Dichotomous and continuous data analyses were displayed using forest plots.
Unit of analysis issues
Studies with multiple treatment groups
For two or more treatment groups, we combined treatment groups if they were sufficiently similar; for dissimilar treatment groups, we planned to split the control group equally between treatment groups (Higgins 2008b).
Cluster‐randomised trials
In the case of cluster randomisation, we planned to adjust for the effects of clustering using an intraclass correlation coefficient (ICC).
Dealing with missing data
Study authors were contacted for missing data, such as standard deviations. Loss and exclusion of data were examined to try to understand the reasons and implications. When standard deviations were missing and could not be obtained from study authors, we planned to calculate them when possible from F, t or P values, or from standard error. Otherwise the trial was treated as having no usable data.
We identified performing intention‐to‐treat (ITT) analysis as an important marker of effort to reduce bias (see Assessment of risk of bias in included studies).
Assessment of heterogeneity
High levels of heterogeneity are likely when sufficient trials are identified for meta‐analysis. When this was suggested by an I2 statistic greater than 40% and by the forest plot (as poor overlap of confidence intervals and presence of outliers), it was interpreted using Higgins 2003, with reference to in/consistency in the direction of effects, and with particular reference to variation between studies in treatment aims and methods, which might suggest that the set should be split.
Assessment of reporting biases
The following steps were undertaken to address reporting biases, particularly in relation to studies performed in underresourced settings and reported in the grey literature: searches of a range of databases, including those published in languages other than English and those listing non‐peer‐reviewed journals; systematic searches of reference lists of reviews in the field and final included studies; manual searches of contents pages of the top 10 sources of publications yielded by the search; searches of databases for registered trials, which yielded published and unpublished studies; and inclusion in the review of all eligible unpublished and published studies. For eligible studies, a search was made specifically for published protocols or trial register entries for comparison with published studies. Funnel plots were planned when data were sufficient.
Data synthesis
RevMan 5 software was used to conduct meta‐analysis when feasible and appropriate. A random‐effects model was applied, given the various sources of diversity described above.
Subgroup analysis and investigation of heterogeneity
We planned to analyse child and adult studies separately because methods and outcomes differ very substantially, as does, usually, the type of torture experienced.
We planned separate summaries of studies involving direct psychological interventions according to whether they were delivered to individuals, couples, families or groups.
We planned, if sufficient trials were identified, to separate studies conducted on populations whose members still reside in their own homes from those in which people remain in their country of origin but are internally displaced and from those in which people are refugees. The difficulties and dangers of flight and of settling into a refugee camp or a country where asylum has been sought compound and augment existing problems for the torture survivor. Although these are difficult to separate on an individual level, it makes sense when possible to recognise them on a trial level.
Sensitivity analysis
When possible, sensitivity analyses were planned to assess the effects of different methodological decisions made throughout the review process by successively removing the following.
Quasi‐RCTs, to leave only RCTs.
Cluster‐randomised trials, to leave individually randomised trials.
Trials using non‐ITT methods, to leave only those analysed using ITT (to be considered an ITT analysis, the analysis must include all participants who entered treatment, whether or not they provided data at the end of treatment). Nuesch 2009 has found that trials with ITT analyses produce smaller treatment effects in meta‐analyses, and this difference is greater in meta‐analyses in the presence of heterogeneity.
Unpublished trials. Some treatment studies in this literature are published in non‐peer‐reviewed sources, such as chapters and internal reports of non‐governmental organisations, raising concerns about differences in quality.
Summary of findings table
A summary of findings table (Table 1) was prepared for all findings, and a GRADE (Grades of Recommendation, Assessment, Development and Evaluation) summary was prepared using GRADEpro software for positive findings only: distress and post‐traumatic stress symptoms at follow‐up, as any intervention should be expected to have a lasting effect, and effects may reach a maximum some time after cessation of treatment. Additional sources were used to identify the meaning of score ranges on relevant depression and PTSD symptom scales for calculation of clinical interpretation (shown in Effects of interventions).
Results
Description of studies
Results of the search
An initial search of the electronic databases PsycINFO, MEDLINE, EMBASE, CENTRAL, CINAHL, Web of Science (WoS) and the CCDANCTR on 11 April 2013, and of LILACS, OpenSIGLE/OpenGREY, WHO, PILOTS and RCTs on 30 April 2013, yielded 1730 references. A search of reference lists from reviews, tables of contents (of Social Science and Medicine, Journal of Nervous and Mental Disease, Journal of Traumatic Stress, Torture, Nursing Times, JAMA, Prehospital Disaster and Medicine, Nursing Research, American Journal of Public Health, Nursing Standard) and contact with authors of studies that were not yet available yielded 861 references. After deduplication, these 2591 references provided 1919 references (Figure 1). This process was carried out by one review author (BK).
1.
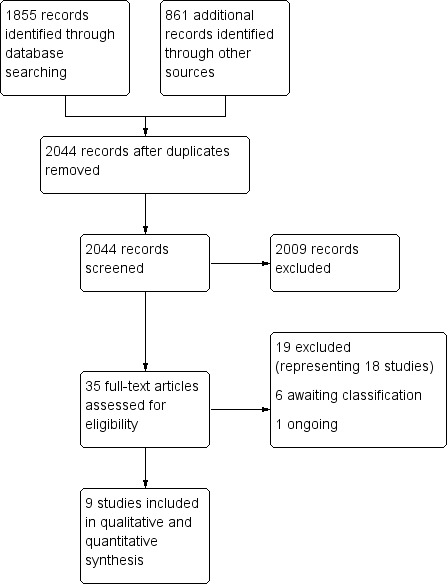
Study flow diagram.
A further search was carried out on CCDANCTR, CENTRAL, EMBASE, MEDLINE, MEDLINE In‐Process, PsycINFO, ICTRP and ClinicalTrials.gov on 20 June 2014. Studies awaiting classification and ongoing studies were followed up at this time. After deduplication, 125 references were identified. As no additional studies were identified by the other resources searched in April 2013 (CINAHL, WoS, PILOTS and the grey literature), these searches were not updated.
Selection against criteria of the 1919 titles and abstracts or summaries from 2013 performed independently by two review authors (BK, AW) revealed 25 possible studies for which the full paper was sought. Many of the excluded titles were news items that were not in any way scientific studies; narrative accounts of torture survivors with no data; and a smaller number of studies that were trials but were not randomised; did not provide psychological, social or welfare interventions; or did not include torture survivors. A total of 18 full papers was obtained; contact with the authors of six unpublished trials established that they were incomplete; three papers could not be found, and no response was obtained from study authors. Only nine studies fulfilled the inclusion criteria: Bichescu 2007; Hensel‐Dittmann 2011; Igreja 2004; Neuner 2010; Paunovic 2001; Pokhariyal 2012; Schauer 2006; ter Heide 2011; Yeomans 2010. See Figure 1 for reasons for exclusion. Involvement of the third review author was required at this stage to inform the decision when less than 100% of study participants reported torture.
As a result of the 2014 search, 10 possible studies were identified from the 125 references and full papers obtained. None fulfilled the inclusion criteria, and they were added to studies excluded or awaiting classification. Three studies resolved the status of earlier studies that were ongoing or awaiting classification. Two studies (Bolton 2011; Weiss 2012) previously identified as ongoing were now recorded as completed, as was another newly identified study from the same research group (Robinson 2014), but trial authors confirmed that they were not yet published, and data were not available.
Included studies
See Characteristics of included studies.
Design
All nine studies that met criteria provided data (Bichescu 2007; Hensel‐Dittmann 2011; Igreja 2004; Neuner 2010; Paunovic 2001; Pokhariyal 2012; Schauer 2006 (obtained from author); ter Heide 2011; Yeomans 2010). Seven had two arms, and two (Igreja 2004; Yeomans 2010) had three arms: One arm in Igreja 2004 did not meet criteria; in Yeomans 2010, the two treatment arms, which differed relatively little, were combined. All participants were randomly assigned.
Sample sizes
The number of participants entering trials varied between 18 and 137, with a total of 507 and a mean of 53 people included across all trials. For the seven studies that provided details on attrition during treatment, the rate varied between 0% and 50%, with a mean of 18%.
Setting
The context of treatment varied across studies. Six studies took place at specialist trauma clinics in Europe: three in Germany (Hensel‐Dittmann 2011; Neuner 2010; Schauer 2006), one in the Netherlands (ter Heide 2011), one in Romania (Bichescu 2007) and one in Sweden (Paunovic 2001). Of these, five (Hensel‐Dittmann 2011; Neuner 2010; Paunovic 2001; Schauer 2006; ter Heide 2011) included mixed refugee populations from Europe, the Middle East and Africa, and the sixth (Bichescu 2007) treated Romanians who had been tortured under a previous regime and were still living in Romania. Three studies were conducted in Africa: one in Mozambique (Igreja 2004), one in Burundi (Yeomans 2010)—both at refugee camps in the country in which they were tortured—and one in Kenya (Pokhariyal 2012), in which participants were a mixture of refugees and nationals tortured in Kenya (Pokhariyal 2012).
Participants
The mixed refugee groups treated in studies in Europe had varying status. Those in Sweden (Paunovic 2001) had refugee status and were not at risk of return, as were some of the populations of two other European studies (Hensel‐Dittmann 2011; ter Heide 2011), but the remainder in those two studies and in Schauer 2006 were awaiting decisions on their claim of asylum status, and in a further study, they had only temporary leave to remain in Germany (Neuner 2010). The studies in Africa were of internally displaced people who retained their citizenship.
In two studies (Bichescu 2007; Pokhariyal 2012), it was stated that all participants had been tortured, and in another (Yeomans 2010), almost all. For three others, it was a clear majority (Hensel‐Dittmann 2011 76%; Neuner 2010 87.5%; ter Heide 2011 70%), and for two (Igreja 2004 56%; Schauer 2006 56%), a slender majority. For the last study, it was 30% (Paunovic 2001). These studies were distinguished from those we rejected on the basis that participants were not all torture survivors as seen by the following: (1) The remainder of the population was subjected to organised violence and experiences that could amount to torture, such as (all from Paunovic 2001) witnessing a massacre and receiving death threats against the family; (2) those in Europe were recognised as refugees because they had been subjected not only to random acts of violence but also to personally directed acts; and (3) checklist summaries of relevant experiences tend to underestimate torture experience (Boynton 2004; Hollifield 2002b), as does reluctance to disclose it. Quantification of torture is extremely difficult, despite widely used checklists such as the Harvard Trauma Questionnaire (Mollica 2004), used by ter Heide 2011 and Yeomans 2010, which count types of torture but not severity, duration, repetition or recency. Nor are other distressing experiences such as multiple losses and separations, violence and sexual exploitation in the country of origin, in refugee camps and during flight to exile quantified other than by the same checklists. Of the eight studies providing information, six required a diagnosis of PTSD for eligibility (Bichescu 2007; Hensel‐Dittmann 2011; Igreja 2004; Paunovic 2001; Schauer 2006; ter Heide 2011); for the other two, most were diagnosed with PTSD (Neuner 2010 85%; Pokhariyal 2012 66%).
Men predominated over women in all studies, with mean age mostly between 30 and 45 years; the exception was Bichescu 2007, whose participants were considerably older. Educational status, marital status and family situation varied considerably across studies. Details on country and cultural and language backgrounds of participants were lacking in most studies or were so broad as to convey little information, such as by describing participants as from the Middle East or Africa. These details are necessary when the appropriateness of interventions and of outcome measures is considered.
Interventions
All trials but one were of individual treatment, some of fixed length and others variable; in the trial of reconciliation and education by Yeomans 2010, participants were treated in groups. Therapy duration varied from one hour (Igreja 2004) to longer than 20 hours (Paunovic 2001), with a mean of around 12 to 15 hours. Four studies (Bichescu 2007; Hensel‐Dittmann 2011; Neuner 2010; Schauer 2006), all from the same group of researchers, used narrative exposure therapy (NET). Two others used related therapies, as far as can be identified from the descriptions: testimony therapy (Igreja 2004) and trauma healing (Yeomans 2010). One study used eye movement desensitisation therapy (EMDR: ter Heide 2011), and another (Pokhariyal 2012) a mixture of therapies under the name of 'trauma processing,' for which EMDR was one of the two major components. One study used cognitive‐behavioural therapy (CBT; Paunovic 2001). Three studies (Hensel‐Dittmann 2011; Schauer 2006; ter Heide 2011) made specific reference to a manual for therapy, and it is likely that Neuner 2010 used a similar if not identical one; two other studies (Bichescu 2007; Igreja 2004) referred to standard sources for treatment methods; the remaining trials provided no details of any protocols or standardisation of what was transacted in therapy. Most trials used an active control such as psychoeducation, although it was much shorter than the treatment sessions (Bichescu 2007); stress inoculation while avoiding any element of exposure (Hensel‐Dittmann 2011); exposure alone (in comparison with exposure plus CBT) (Paunovic 2001); stabilisation (ter Heide 2011); and "conventional psychotherapy," in fact an assortment of therapeutic techniques with varied or no evidence of efficacy (Pokhariyal 2012). The remaining four used treatment as usual (Neuner 2010; Schauer 2006), waiting list control (Yeomans 2010) and no treatment (Igreja 2004).
All of these treatment methods require skills acquired through training. In two studies, the trial authors themselves delivered treatment with the help of interpreters: for Igreja 2004, this entailed an interview to generate the testimony; for Pokhariyal 2012, who give little detail of the eclectic treatment provided, therapists are described as qualified in counselling psychology, but it is not clear to what extent this was relevant to treatment methods provided. Narrative exposure therapy in the study by Bichescu 2007 was delivered by a doctoral student without mention of clinical qualifications or supervision; CBT in Paunovic 2001 was delivered by doctoral clinical psychology trainees, supervised by a more experienced psychologist. Hensel‐Dittmann 2011 and Neuner 2010 used experienced clinicians in NET, and ter Heide 2011 in EMDR; Schauer 2006 provided no details on NET therapists. Yeomans 2010, in Burundi, used local facilitators, who were given brief training in reconciliation and education methods.
One study (Igreja 2004) matched the gender of therapists with that of participants, although interaction with participants was relatively brief compared with other interventions, and in two studies (Bichescu 2007; Igreja 2004), therapists were native speakers of participants' language. Information on those who conducted the studies, who interpreted for therapists or who assessed participants was otherwise lacking.
Outcomes
Outcome data for interventions were as follows: inventories of post‐traumatic stress symptoms for all studies immediately after treatment (Hensel‐Dittmann 2011; Igreja 2004; Paunovic 2001; Pokhariyal 2012; Schauer 2006; ter Heide 2011; Yeomans 2010) and/or at follow‐up (Bichescu 2007; Hensel‐Dittmann 2011; Neuner 2010; Paunovic 2001); PTSD caseness for three studies, all of which required a PTSD diagnosis for entry to the trial, assessed immediately after treatment (Bichescu 2007; Hensel‐Dittmann 2011; ter Heide 2011); distress, usually a depression score, immediately after treatment for five studies (Hensel‐Dittmann 2011; Igreja 2004; Paunovic 2001; ter Heide 2011; Yeomans 2010) and/or at follow‐up for four (Bichescu 2007; Hensel‐Dittmann 2011; Neuner 2010; Paunovic 2001); and quality of life immediately after treatment for two studies (Paunovic 2001; ter Heide 2011). However, Paunovic 2001 predicted no differences between intervention and comparator for quality of life, leaving only ter Heide 2011 providing data.
No outcomes of participation or social function, social relationships, satisfaction with treatment or adverse events were reported. Although a few other relevant measures were used infrequently, such as pain by Neuner 2010, the range fell short of the needs and health problems of torture survivors commonly reported in the literature (Bracken 1995; Burnett 2001; Jaranson 2011; Rasmussen 1990): health problems such as impairment and disability; inadequate social support, interpersonal and family relationships; psychological problems including shame, guilt, low self‐esteem and feeling disempowered; and those related to lacking agency and control in one’s life, having lost a sense of meaning, purpose and worth as a human being and having no sense of justice (Patel 2007; Silove 1999).
Studies used a mixture of clinician‐administered and self‐report measures, but self‐report measures in no case were completed by participants alone in their first language. In Paunovic 2001, all participants and, in Hensel‐Dittmann 2011 and ter Heide 2011, some participants completed assessment instruments in a non‐native language in which they were sufficiently fluent. All but Paunovic 2001 used interpreters and/or interviewers who used translated material. In Bichescu 2007, Igreja 2004, Neuner 2010, Pokhariyal 2012, Schauer 2006, ter Heide 2011 and Yeomans 2010, assessment was largely or entirely conducted by interview, and in two studies (Igreja 2004; Yeomans 2010) because of illiteracy of most or all participants. ter Heide 2011 notes that three participants required "extensive help" from interviewers to complete the assessment. All measures originated in Western clinical and research literature, and all assessments required translation and/or interpretation, but only one study gave details of how this was done: Yeomans 2010 describes a careful process of translation, back‐translation and linguistic scrutiny. Two further studies (Igreja 2004; ter Heide 2011) refer to use and testing of some assessment measures in non‐European languages, although not necessarily the languages used in the studies.
Three studies had no follow‐up (Pokhariyal 2012; Schauer 2006; Yeomans 2010), although in one case (Yeomans 2010), this occurred because the control condition was a waiting list of participants, who subsequently entered treatment. One study (ter Heide 2011) had a three‐month follow‐up, which did not meet our criteria; the remainder had six‐month follow‐up (Bichescu 2007; Neuner 2010; Paunovic 2001), 11‐month follow‐up (Igreja 2004) or six‐ and 12‐month follow‐up (Hensel‐Dittmann 2011).
Excluded studies
Nineteen papers, representing 18 studies, were excluded. Eight included a minority of torture survivors within the population (Adenauer 2011; Akhtar 1994; Carr 2011; Dybdhal 2001; Mills 2012; Morath 2014; Neuner 2004; Stenmark 2013 and its secondary study Halvorsen 2014), usually sampling a population that included people otherwise traumatised, as in road traffic accidents (e.g. Neuner 2004); five further studies were not identified at all as including survivors of torture (Bass 2013; Hijazi 2014; Kalantari 2012; Meffert 2011; Schaal 2009). Two were not RCTs (Talbot 2013; Walstrom 2013); one had randomisation broken at baseline (Rees 2013); and one was a protocol for an RCT (Sonne 2013). One intervention was physical rather than psychological or social (Liedl 2011) (see Characteristics of excluded studies).
Ongoing studies
We identified one ongoing study (Knaevelsrud 2011), marked 'status unknown' in the register of trials, for which we could find no published results. Its eligibility is uncertain. See Characteristics of ongoing studies.
Studies awaiting classification
Six studies are awaiting classification (Bolton 2011; Cavka 2005; Kolassa 2012; Robinson 2014; Stenmark 2008; Weiss 2012). Three (Bolton 2011; Robinson 2014; Weiss 2012) are likely to be eligible for the next update of this review if published; some results for Robinson 2014 are already posted in the Clinical Trials Register. See Characteristics of studies awaiting classification.
Risk of bias in included studies
We used 10 risk of bias categories. Six were standard: random sequence generation (selection bias), allocation concealment (selection bias), blinding of participants and practitioners (performance bias), blinding of outcome assessment (detection bias), incomplete outcome data (attrition bias) and selective reporting of outcome (reporting bias). We added three to the 'other' category: therapist allegiance, treatment fidelity and therapist qualifications. The 'other' category was further populated by concerns about interpretation and translation of assessment questions and responses.
Random sequence generation
Only one of the nine studies used recognised procedures for randomisation (ter Heide 2011). Of the other studies, seven were assessed as having unclear risk of bias, and one (Bichescu 2007) high risk.
Allocation concealment
Eight of the studies gave no information about allocation concealment, and so the risk of bias was assessed as unclear; one study (Igreja 2004) used a method of randomisation and allocation that produced a high risk of unblinding: odd or even numbers were assigned at baseline and subsequently determined the treatment arm.
Blinding of participants and personnel
It was not possible in any study to blind participants or personnel to allocation, nor were expectations of treatment benefit asked of participants at baseline, so all nine were at high risk.
Blinding of outcome assessment
Outcome data were largely self‐report (often assisted by interviewers and/or interpreters) and so were less open to bias by those who assisted assessment than were observer or clinician ratings but were possibly influenced by interpreter expectations or beliefs. Despite the use of blind assessors in four studies (Bichescu 2007; Hensel‐Dittmann 2011; Neuner 2010; Yeomans 2010), all but Yeomans 2010 (rated low bias) remarked on unwitting unblinding by participants' comments, leaving the risk of bias unclear. In two studies, all outcome assessment was self‐report in the host country language in which participants were sufficiently fluent: in one, a clear difference was noted between treatment and control arms (Schauer 2006), and so it was rated as having high risk, but in the other, treatment and control arms were equivalent in many details (Paunovic 2001), and so it was rated as having uncertain risk.
Incomplete outcome data
Only two studies (Hensel‐Dittmann 2011; Neuner 2010) used ITT methods; two others (Bichescu 2007; Schauer 2006) had no dropouts, so all four of these were rated as low risk. All other studies reported results only for those who completed treatment (Paunovic 2001; Pokhariyal 2012; ter Heide 2011; Yeomans 2010), and for one, this information was not clear (Igreja 2004).
Selective reporting
All studies reported the outcomes listed in their methods, but we were unable to find protocols for any of the nine studies against which to compare the published trials; thus all are rated as being at unclear risk of bias for this domain.
Other sources of bias
Therapist allegiance
Four studies declared allegiance to NET (Bichescu 2007; Hensel‐Dittmann 2011; Neuner 2010; Schauer 2006); all were rated as high risk. Two of these (Bichescu 2007; Hensel‐Dittmann 2011) used the same therapists for the active control as for treatment; the other two used a treatment as usual control in which therapists were not involved in the trial. Except possibly in Hensel‐Dittmann 2011, therapists or supervisors were also researchers and authors. One study expressed allegiance, although weakly, to eye movement desensitisation therapy (EMDR) (ter Heide 2011), and different therapists delivered the active control intervention. No study mentioned the use of therapists who had trained in a model other than the preferred one.
Treatment fidelity
Two studies used the same manual (Hensel‐Dittmann 2011; Schauer 2006), a third (Neuner 2010) used an unspecified manual, which was possibly the same as these, and a fourth used a manual produced for the trial (ter Heide 2011) for both treatment and active control arms. These studies were rated as low risk. The other studies provided no information, and none described any method used to assess adherence to the manual or treatment method.
Therapist qualifications
Five studies used trained therapists (Hensel‐Dittmann 2011; Neuner 2010; Pokhariyal 2012; ter Heide 2011; Yeomans 2010), with or without supervision, and were rated as low risk. Two used therapists in training and supervised (Bichescu 2007; Paunovic 2001) and were classified as having uncertain risk when compared with those that provided no information.
Assessment issues
Given the methods of assessment and the use of interpreters, interviewers and formal and informal translation, the risk of interviewers and interpreters influencing responses during assessment was much greater, as was the chance that their expectations might affect the transfer of responses in participants' own language to options on the assessment instrument. No participants completed self‐report measures in their native language. Two additional problems affect assumptions of reliability and validity as cited in the literature. First, the language, metaphors and analogies for expression of depression and trauma symptoms, particularly those referring to somatic experiences (such as 'a heavy heart'; Lee 2007), originate in Western culture. Second, even when the assessment items are understood as intended, the impropriety of disclosing problems, particularly psychological problems, to those outside the family risks serious underestimation of symptoms. By contrast, some of the participants in Neuner 2010 were granted temporary leave to remain in Germany on the basis of their psychological problems—a context that could act against actual or assessed improvement. Further, quality of life measures include items related to performance of activities and satisfaction with aspects of life, such as money and safety, which can be seriously affected by unresolved asylum status and the restrictions associated with it, as in ter Heide 2011.
Effects of interventions
See: Table 1
We combined all treatment methods, although as described under Included studies, trials predominantly used testimony and exposure methods. We had planned to combine treatment arms when more than one was included, but one of the two trials with three arms (Igreja 2004) had a non‐case arm for which results were not relevant to our overall aims. We combined the two fairly similar treatments in Yeomans 2010 as planned and compared them with the inactive control group.
Quality of studies assessed using GRADE methods was very low for all comparisons (Table 1).
Comparison 1. Psychological therapies versus any control
All nine studies contributed data for comparison of psychological therapy versus control.
Primary outcomes
1.1 Psychological distress
This consists of outcomes of psychological distress (such as depression and anxiety). All nine studies contributed to analysis of the outcome of psychological distress, although not all to any single time point.
1.1.1 Psychological distress post treatment
Five studies contributed to this comparison, with 290 people altogether. Distress was measured as depression in four studies (Hensel‐Dittmann 2011; Paunovic 2001; ter Heide 2011; Yeomans 2010) with 255 participants, using two similar symptom scales, and by a broader symptom scale in a fifth (Igreja 2004), so results were combined as standard mean differences (SMDs). Results showed no significant differences in distress (SMD ‐0.15, 95% confidence interval (CI) ‐0.39 to – 0.09; z = 1.25, P value 0.21) (Analysis 1.1). Good consistency was noted for this comparison (I2 = 0%), but multiple sources of bias in methodology were observed.
1.1. Analysis.
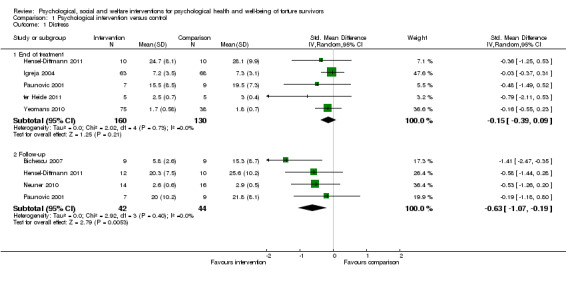
Comparison 1 Psychological intervention versus control, Outcome 1 Distress.
1.1.2 Psychological distress at follow‐up
At follow‐up, four studies with 86 participants—three NET (Bichescu 2007; Hensel‐Dittmann 2011; Neuner 2010) and one CBT (Paunovic 2001)—used three depression scales, which were analysed using SMDs. Results showed statistically significant differences (SMD ‐0.63, 95% CI ‐1.07 to ‐0.19; z = 2.79, P value 0.005) (Analysis 1.1). Heterogeneity was 0%, but multiple sources of bias were identified; this and the small size of the comparison make confidence in findings low. Evidence was assessed as of very low quality because of real‐time interpretation of measures that were therefore inadequately standardised for content or delivery; measures themselves without conceptual or linguistic validation; and very small sample sizes.
One study with low bias (Hensel‐Dittmann 2011), which used the Hamilton Depression Scale (Hamilton 1960), was chosen to calculate mean differences: pooled pretreatment score was 28.1 on the 0 to 50 scale on which a score of 19 to 22 is taken to indicate severe depression, and greater than 22 very severe depression. Mean improvement was seen as 6.4 in the treatment group, but this is still on the borderline of very severe depression.
1.2 Adverse events
No study provided data on adverse events. One comment (ter Heide 2011) was made concerning dropout because of symptom worsening in EMDR treatment. We considered examining dropout, but in studies that provided adequate data, reasons given included external factors such as asylum refusal and deportation, so we did not consider dropout to be an adequate proxy measure.
Secondary outcomes
1.3 Psychological status or target behaviour
No studies were found of behaviour, only of psychological status, assessed as post‐traumatic symptom score by seven studies—all post treatment and four at follow‐up. PTSD caseness was also assessed by three studies, post treatment only.
1.3.1 Post‐traumatic stress symptoms post treatment
Seven studies, including 388 people (Hensel‐Dittmann 2011; Igreja 2004; Paunovic 2001; Pokhariyal 2012; Schauer 2006; ter Heide 2011; Yeomans 2010), used several different PTSD symptom frequency and intensity scales, all based on the DSM (Diagnostic and Statistical Manual of Mental Disorders) formulation of PTSD and broadly similar in content. SMDs were therefore used for analysis. Symptoms post treatment did not show significant differences (SMD ‐0.30, 95% CI ‐0.66 to 0.06; z = 1.65, P value 0.10) (Analysis 1.2). Heterogeneity (I2) was 57%; removing Schauer 2006 improved this considerably (I2 = 0%), but results still fell well below clinical significance for change.
1.2. Analysis.
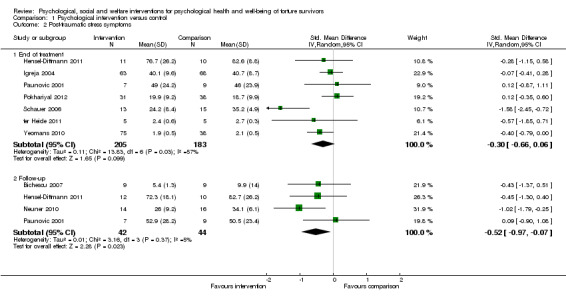
Comparison 1 Psychological intervention versus control, Outcome 2 Post‐traumatic stress symptoms.
1.3.2 Post‐traumatic stress at follow‐up
Four studies contributed with 86 people: three used NET for treatment (Bichescu 2007; Hensel‐Dittmann 2011; Neuner 2010), and one used CBT (Paunovic 2001). Statistically significant differences in symptom score were noted (SMD ‐0.52, 95% CI ‐0.97 to ‐0.07; z = 2.28, P value 0.02) (Analysis 1.2).
Heterogeneity (I2) was 5%, but the studies are the same as those in 1.1.2, and the same concerns about bias applied to this comparison, making confidence in these findings also low. Evidence was of very low quality, with the same problems as in 1.1.2 of real‐time interpretation of measures that therefore were inadequately standardised for content or delivery; measures themselves without conceptual or linguistic validation—a particular issue with PTSD (see Background); diverse populations; and very small sample sizes.
Of these PTSD follow‐up studies, one with low bias (Hensel‐Dittmann 2011) was used to calculate mean differences using the Clinician Administered PTSD Scale (CAPS). The pooled pretreatment score was 91.2 on a 0 to 120 scale with 30 items, each scored 0 to 4 for frequency and 0 to 4 for severity. Scoring at least 1 (at least once a week) for frequency and at least 2 (moderate) for severity is taken to indicate clinical significance, and a change of 10 to 20 points (depending on the population) is taken to indicate clinically significant change; the mean difference of 13.6 fell within this, but follow‐up scores still indicated substantial symptoms in treatment and control groups.
1.3.3 PTSD caseness post treatment
Three studies (Bichescu 2007; Hensel‐Dittmann 2011; ter Heide 2011) with 52 participants classified participants using 'caseness': meeting criteria for the diagnosis of PTSD. Diagnosis did not change significantly, with an odds ratio (OR) of 0.28 (95% CI 0.06 to 1.36: z = 1.58; P value 0.11) (Analysis 1.3). Heterogeneity was 1%.
1.3. Analysis.
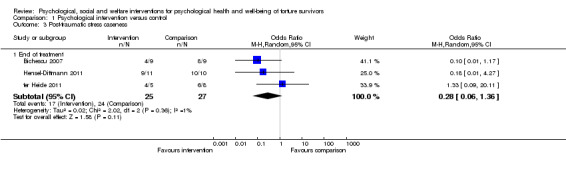
Comparison 1 Psychological intervention versus control, Outcome 3 Post‐traumatic stress caseness.
1.3.4 PTSD caseness at follow‐up
No study assessed PTSD caseness at follow‐up.
1.4 Quality of life or well‐being
Only two studies assessed quality of life, immediately post treatment but not at follow‐up.
1.4.1 Quality of life or well‐being post treatment
The only study that compared intervention and control in terms of quality of life (ter Heide 2011), with 10 participants, did not show statistically significant changes for treatment over control (SMD 0.99, 95% CI ‐0.37 to 2.35; z = 1.43; P value 0.15).
1.4.2 Quality of life or well‐being at follow‐up
No study assessed quality of life at follow‐up.
1.5 Participation and functioning
No studies assessed participation or functioning.
1.6 Quality and/or quantity of family or social relationships
No studies used any measures of family or social relationships.
1.7 Ratings of psychological function made by others
No studies used any third party ratings of psychological function.
1.8 Satisfaction with the intervention
No studies assessed satisfaction with the intervention.
Comparison 2. Social interventions versus any control
No social intervention studies were found.
Comparison 3. Welfare interventions versus any control
No welfare intervention studies were found.
Subgroup analyses
Because of lack of identified studies, no subgroup analyses were undertaken.
Sensitivity analyses
Because of lack of identified studies, no sensitivity analyses were undertaken.
Reporting biases
Data were insufficient for funnel plots or statistical testing. We noted that none of the nine studies showed superiority of comparator over intervention, and no protocols or or trial register entries were found against which published reviews could be compared.
Discussion
Summary of main results
Results showed no differences between psychological therapies and controls in terms of an immediate effect on post‐traumatic symptoms, distress or quality of life, but they revealed a medium‐term effect of moderate size on post‐traumatic stress symptoms and on distress (see Table 1). These medium‐term results were derived from four of the nine studies, and evidence is of very low quality. Interventions in three of the four trials were briefer than recommended even for less complex problems—for trauma (NICE 2005) and for depression (NICE 2010)—and were drawn predominantly from treatment for trauma, not depression. In two of the four studies in the meta‐analysis, participants were permanent residents of their native or host country; in the other two, some participants had only temporary status. In no study can it be assumed that participants had good social support or adequate financial means or accommodation. Clinical practice and guidelines (NICE 2005; Wenk‐Ansohn 2007) suggest that establishing stability and safety is a crucial first stage in therapeutic interventions with asylum seekers and refugees, including torture survivors (NICE 2005). No data on adverse effects were provided, so possible harm is unknown.
Overall completeness and applicability of evidence
The interventions included were of a relatively narrow range among those specified in the protocol, with no social or welfare interventions found, such as are reviewed in Williams 2011. A wider range of interventions was represented by non‐randomised studies found during searching, but many of the excluded studies provided similar interventions to those included. Within the psychological interventions, most expected outcomes were not found, including adverse events (a primary outcome, and a significant risk for PTSD in terms of worsening symptoms) and measures of social participation (a secondary outcome that assesses reintegration into the immediate or wider community). None of the subgroups that we hoped to find, particularly child and adolescent survivors of torture, survived selection of trials, leaving a substantial gap in the evidence.
Torture does not give rise only to psychological needs (Porter 2005). The aim of torture is to attack, debilitate or destroy the individual in ways that also disable the family (causing fear and mutual mistrust, destroying social relationships and economic capability) and the wider community (such as by spreading terror, for example, by publicly displaying mutilated bodies subjected to torture, and generating distrust, which mitigates against disclosure in social relationships). We were disappointed therefore to find only psychological interventions and those to a greater or lesser extent replicating treatments for single‐event trauma (such as a road traffic accident) for individuals in stable societies, with none addressing reintegration or rehabilitation in a broader context.
In effect, the six studies conducted at European treatment centres used orthodox psychological approaches to treatment of participants with post‐traumatic stress disorder: NET, CBT and EMDR—all adequately described in the trauma treatment literature—albeit mainly with participants who had experienced single traumatic events within an otherwise secure environment. Two of the three studies conducted in different African countries took a less orthodox approach of testimony writing (Igreja 2004) and group reconciliation (Yeomans 2010), and the third (Pokhariyal 2012) conducted an eclectic mixture of trauma processing methods that were possibly closer to orthodox treatments. However, these eclectic and non‐manualised interventions are difficult to reproduce and therefore have low generalisability. This resembles a distinction in the wider literature on treatment of survivors of torture and organised violence between studies usually of refugees in developed countries who receive evidence‐based individual treatment and studies of survivors who remain in their own or neighbouring developing countries, many as internal or external refugees, and that use multiple methods designed to address needs identified in that particular population. Because the latter are rarely conducted as RCTs, they are poorly represented in this review. This is regrettable because they usually integrate a variety of approaches with an appreciation of contextual factors, including conditions such as safety, adequate shelter and food; legal issues such as justice or impunity for perpetrators and therefore feelings of validation and acknowledgement of torture as deliberate harm, a crime and a human rights violation; and participation issues such as opportunities for education, work and beneficial community activities. Although changes in these areas may have occurred for some individuals in the studies included, they were not assessed, despite their likely impact on mood and quality of life (Gurr 2001; Nickerson 2011).
Deciding on appropriate treatment requires attention to the specific problems of potential participants and their social and material context; cultural norms about expression and management of psychological problems; and cultural norms about health care and recovery. This might make cognitive and behavioural methods a low‐risk choice for Western‐acculturated refugees with secure status and a stable lifestyle, whose persistent difficulties stand in the way of fuller integration and realisation of their potential in the host country, but a doubtful choice in other circumstances. We have much to learn from consultation with torture survivors, both treated and untreated.
Control conditions were also varied, from no intervention through a single session to specified psychological intervention or unspecified and unquantified treatment as usual. Although no intervention probably represents clinical reality for most torture survivors, discussion is needed about what minimal interventions, appropriate to the needs of torture survivors, would make more meaningful comparators. Here the diversity most likely adds to the heterogeneity in results, without providing helpful pointers for low‐resource interventions. It is a suitable basis for exploration (e.g. using subanalyses) in an update of this review.
A further concern about narrowness arises because four of the nine studies (Bichescu 2007; Hensel‐Dittmann 2011; Neuner 2010; Schauer 2006) were conducted by one research group with an explicit commitment to NET. Beyond the issue of bias of research/therapist allegiance, the use of exposure for torture survivors requires ethical scrutiny. Narrative exposure therapy is not unique in this: all therapeutic interventions that require or result in the person accessing memories of torture and reliving the emotions associated with it involve an element of exposure. The review by Nickerson 2011 raises related concerns about retraumatisation, and about the extent to which refugees can genuinely feel safe, such that extinction procedures are likely to work. None of the studies discussed ethical issues or investigated the practice and impact of exposure (despite one noticing dropout caused by symptom worsening), nor the complexity of obtaining informed consent to exposure methods across cultural and language barriers, and the degree of control that the participant has over the nature, duration, detail and timing of exposure sessions.
Separate issues about applicability of evidence arise from the dominance of PTSD diagnostic concepts and measurement instruments used in defining populations eligible for treatment. Nicholl 2004 described the definition of the field in terms of PTSD as losing the important meaning of experiences that constitute symptoms of PTSD, and McFarlane 2012 criticised it as overmedicalising psychological problems and excluding many torture survivors with other difficulties. PTSD diagnosis as an entry criterion to treatment studies also excludes torture survivors who do not meet caseness because, however severe, their symptoms do not fall into the required number of categories for diagnosis (Gorst‐Unsworth 1998; Summerfield 2001). This may change with the more inclusive DSM‐5 superseding DSM‐IV.
Although the results of this review may be taken to apply to mainstream psychological interventions for trauma and distress, whether treatment occurs in the country of origin or for a refugee in a neighbouring or distant country, for torture survivors who are significantly distressed months or years after the end of torture, the effects themselves are not particularly encouraging, even within the relatively narrow domains of outcome. Further, no effects emerged immediately after treatment, with the only benefits apparent at least six months later, at follow‐up. However, lack of attention to cultural and language issues in the methodology remains a concern: these problems undermine interpretation, in either direction, of outcomes and raise questions about the design of studies, which are discussed briefly in Implications for practice and Implications for research.
Quality of the evidence
Bias is shown in Figure 2 and Figure 3, including several items added to try to capture elements of therapist non‐blinding. The range of scores was relatively small, with extremes of bias among smaller studies with less weight, so the planned sensitivity analysis by bias was abandoned. Additional possible sources of bias are noted in the results section: use of non‐blind interviewers and interpreters, even for some self‐report scales; assessment instruments not in participants' native language; cultural preference and stigma against disclosing psychological difficulties to non‐kin; and possible association between asylum determination and mental health status (Jaranson 2011 in an extensive review of treatment of torture survivors describe obtaining asylum as probably the most important intervention to improve mental health). Sample size was generally very small, with a mean of 53 participants in treatment and control groups combined, and attrition in some trials was substantial.
2.
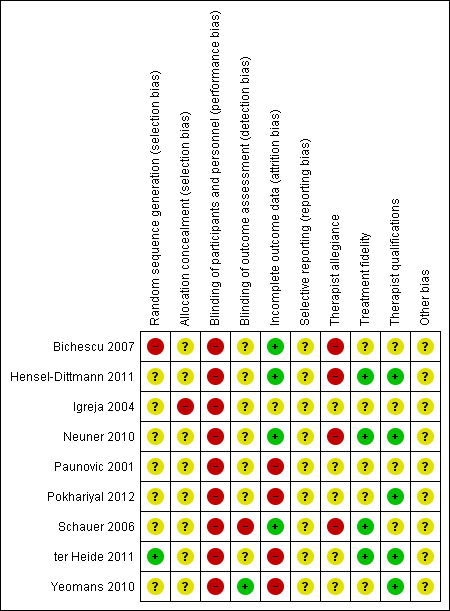
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
3.
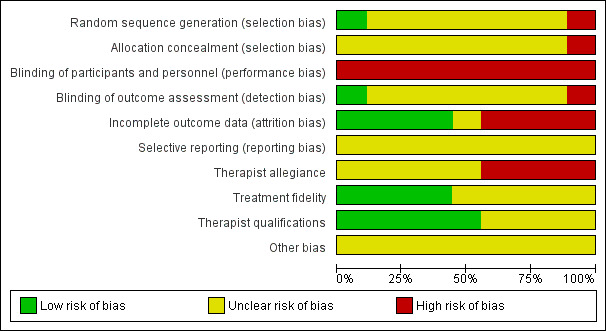
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
Although study effects were combined across different treatments, additional diversity arises from variations in the length of active treatment, the nature of the control and the usually longer treatment duration even than was seen with active controls. For example, in Bichescu 2007, the active treatment intervention (NET) consisted of five interactive sessions of two hours each, compared with one didactic session of the active control (psychoeducation). Establishing a trusting relationship is particularly important among torture survivors, strengthening the potential benefits of non‐specific effects of treatments that allow such a relationship when compared with controls, which do not. Some of these problems are captured in the GRADE summary of findings table (Table 1), which identifies problems of bias, inconsistency and imprecision in all analyses.
Two of the four issues that made the quality of evidence very low concerned assessment processes: use of measures without adequate conceptual and/or linguistic validation, despite the literature on methodology (e.g. Sousa 2011); and real‐time interpretation of measures that therefore were inadequately standardised for content or delivery through variation between assessments, even with the same interpreter.
This is a very difficult area in which to conduct RCTs, so study investigators should be commended, particularly for studies conducted in underresourced settings such as refugee camps. However, in most studies, there was relatively little apparent recognition of the questions raised by transposition of mental health concepts and treatment methods from Western to non‐Western cultures, with very different understandings and ways of dealing with psychological distress, including norms of discussing distress with strangers (therapists and interpreters). Nor did studies (with the partial exception of Yeomans 2010) address intercultural communication during assessment and intervention; cultural diversity of participants; and cultural differences or similarities between participants and therapists, or between participants and interpreters. For instance, even when therapists and participants share their language and nationality (as in Igreja 2004 and Yeomans 2010), differences in class, education, geography, age and background characteristics can constitute significantly different subcultures, potentially impacting outcome. Information on therapists, interpreters and assessors was minimal in the papers reviewed, yet these characteristics interact with the gender, age, ethnicity and cultural background of participants to influence outcome. In particular, gender differences may affect disclosure of the nature of torture experienced and its impact (Bogner 2010; Patel 2004), and stigmata related to describing mental health problems can hinder the establishment of rapport and trust, leading to underassessment of these problems (Hollifield 2002b). All of this makes for substantial heterogeneity within and between trials—a particular problem when trials are difficult to run and generally recruit small samples.
Even translation was addressed relatively superficially by most studies. Culture and language shape the meaning given to, and communication about, experiences of torture and health problems (Mahtani 2003); they shape understandings and expressions of health, health problems, coping and well‐being (Fernando 2003; Laungani 2004) and have a bearing on therapeutic work (Burck 2004). Culture (of participants and therapists) may also determine the extent to which participants are receptive to interventions (e.g. Miranda 2005), and whether participants are able to access and use interventions offered (e.g. Mahtani 2003), influencing participant motivation and the establishment of rapport—all potentially relevant to an understanding of treatment outcomes. The limited number of studies and the lack of detail on participant and practitioner/therapist characteristics precluded meaningful comparisons between cultural backgrounds of participants and treatment outcomes.
Further, use of a language that is not the mother tongue of participants, as was reported in most studies, may influence treatment outcomes. Translators and interpreters may use language for formal assessments that is not semantically equivalent to the language and dialects spoken by participants. No detail is provided in the studies regarding estimation of language competency, choice of language or checks on possible compromises to reliability and validity. Nor (apart from Yeomans 2010) is detail consistently provided on characteristics of interpreters such as gender and nationality—contextual factors that may affect trust and rapport with participants (Patel 2003b; Raval 2003a; Raval 2003b; Temple 2002); their linguistic proficiency and training, if any; and how they were recruited, trained or briefed for the study. All of these influence the effectiveness of communication and the strength of the therapeutic alliance between participant, interpreter and researcher/therapist (Patel 2003b; Temple 1997; Vara 2012), potentially altering treatment outcomes. These issues around the language of assessment and intervention raise ethical problems about the extent to which the voices of participants, already relatively disempowered and vulnerable as asylum‐seeking or refugee torture survivors, could be heard.
Potential biases in the review process
Although participants in the search attempted to access studies from the extensive grey literature in this field, we found none that were not identified in other databases and so did not repeat the grey literature search in the update. Therefore we cannot have total confidence that we did not miss one or more eligible studies. Although it is unlikely that randomised controlled studies are conducted and not published accessibly, not all those conducting research necessarily value academic publication, so work may be disseminated through other channels.
A significant limitation of all studies is lack of relevant information about participants, such as the nature of torture experienced (including recency, type of torture, frequency, severity and duration) and the range of health and well‐being needs. Further, although we tried to make consistent and transparent decisions about selection of studies by using study authors' responses to our questions or their other writings, at times we had to use information about conditions in the country of origin of the survivors to decide whether they were likely to have been subjected to cruel and inhuman treatment. This is the area in which we would expect others to differ most in terms of inclusion of studies. In the future, it would be judicious to specify in inclusion and exclusion criteria the grounds for these decisions. We have greater confidence in our selection processes when we are able to ascertain from study authors or from their other writings the information needed to classify studies. When we were unable to ascertain participant details in mixed populations, study exclusion is open to criticism. Risk of bias scores were not used for sensitivity analyses, so these could not introduce reviewer bias into the results.
A further limitation arises from decisions about acceptable comparators. In aiming for maximum inclusiveness, we retained four trials (Hensel‐Dittmann 2011; Paunovic 2001; Pokhariyal 2012; ter Heide 2011) in which comparator arms contained elements of treatment and were approximately matched for non‐specific effects such as number of sessions with the intervention under trial. Hensel‐Dittmann 2011, Pokhariyal 2012 and ter Heide 2011 compared an enriched or trauma‐focused treatment versus a comparator that did not contain elements aimed at trauma symptoms (Hensel‐Dittmann 2011 stress inoculation with vs without exposure; Pokhariyal 2012 multiple therapies including EMDR with non‐specific conventional psychotherapy; ter Heide 2011 EMDR vs stabilisation). Paunovic 2001 made specific predictions about the superiority of CBT with exposure over exposure alone for trauma symptoms; they predicted equivalence for quality of life as an outcome, so we excluded the trial from the quality of life analysis.
Agreements and disagreements with other studies or reviews
Most RCTs have been published within the past 10 years, so one early review (Nicholl 2004) found only one (Paunovic 2001), and another (Quiroga 2005) reviewed entirely non‐randomised treatment trials, with a preference for community‐based interventions. Since that time, reviews of RCTs (Crumlish 2010; Nickerson 2011) and of both RCTs and non‐randomised trials (Campbell 2007; McFarlane 2012) have reported benefits for torture survivors of CBT and of exposure‐based treatment including NET over control conditions, although in the Nickerson 2011 review with much larger effect sizes than were found in this review. Two studies (McFarlane 2012; Nicholl 2004) are strongly critical of the predominance of the PTSD construct, and all raise methodological concerns. A summary of these reviews can be found in Williams 2013. With Jaranson 2011, which also reviewed randomised and non‐randomised trials, no review reported superior efficacy of either of the most common treatment methods—CBT or exposure.
None of the reviews described above was systematic in terms of search and selection, and few attempted any synthesis of findings; this renders this review an advance on the field, as it stood, despite the numerous reservations described.
Authors' conclusions
Implications for practice.
Very low‐quality evidence suggests no differences between psychological therapies and controls in terms of an immediate effect on post‐traumatic symptoms, distress or quality of life, but shows that NET and CBT have moderate‐sized benefits in reducing distress and symptoms of PTSD in the medium term. However, the very low quality of the evidence means that these findings should be interpreted with caution. In addition to the need for better quality studies, it is essential that adverse effects are assessed. More attention must be paid to establishing culturally and linguistically appropriate outcome measures across a wide range of outcomes that represent the problems, goals and hopes and expectations of torture survivors.
The small number of trials, their diversity and the incompleteness of information provided, suggest that it is not possible to conclude anything about the effects of time from index torture events to the start of treatment; about the setting of treatment; about group versus individual treatment formats; or about training of therapists.
The torture survivor population with problems in psychological and social domains is much wider than that scoring high on PTSD instruments, as characterised entrants to these studies. This review cannot be generalised to those without this level of PTSD symptoms.
Implications for research.
Many methodological issues here cannot be easily resolved and require extended examination elsewhere. However, we would not consider the current studies to exemplify the best design and methodology possible. Much remains to be determined, and Campbell 2007 is highly critical of the lack of research on treatment for torture survivors—a population that he estimates to be of the same magnitude in the USA as that of military veterans, for whom a large body of treatment research literature and substantial resources have been dedicated.
-
Both clinical and legal concerns should guide intervention trials. Most interventions seem rather poorly informed by the legal imperative to provide rehabilitation for torture survivors, as enshrined in the UN 1984 Convention Against Torture. The needs of the target population rather than the allegiances of trialists should guide selection of treatment. It is not clear to what extent different types or conditions of torture and ill treatment result in specific psychological problems (such as guilt, shame or hopelessness), but it is likely that some cognitive and behavioural methods may be better suited to particular problems.
Our review found that use of exposure currently dominates intervention trials. The assumption that it is possible to extinguish multiple and prolonged trauma needs to be questioned carefully. Animal models may be helpful here, and animal work suggests that it is characteristic of fearful responses following trauma that they fail to extinguish spontaneously. Extinction is not, as has sometimes been represented, replacing the cue‐fear association with a cue–no fear association, but it constitutes learning an exception to the cue‐trauma association that continues to compete with it (Goswami 2013). If that competition is influenced by context, then treatment effects (assuming that the participant feels safe in the treatment setting) may not generalise to the world outside treatment. This leads to overly optimistic estimates of treatment effectiveness.
Contextual information about the population should be as full as possible, including details of group identity such as ethnicity and nationality, language and current civil status and living conditions. The situation in the host country is particularly important, as conditions in which refugees live can significantly worsen their psychological and physical health, and can affect outcomes of treatment (Mahtani 2003; Steel 2009).
Descriptions of the psychological and social situation of participants need to be much broader than scores on a narrow range of instruments measuring mental health status, but considerable demands can be placed on participants and on assessment personnel, as well as on interpreters or translation resources, when these are required. Physical health should also be taken into account, including chronic pain (which is common and is associated with depressed mood and reduced activity), head injury and other problems that can affect mood, activity, performance on assessment measures and capacity to adhere to treatment. Torture survivors can identify the areas of well‐being of greatest meaning and relevance for them. At the least, when populations are heterogeneous, the sample needs to be substantially larger than the sample included in most or all of the studies reviewed here.
Productive collaborations between research teams and service providers for torture survivors could overcome some of the shortcomings in design and methods described here. Beyond willingness on both sides, this requires that funders and donors to services are realistic about the resources required for adequate evaluation and for research activities.
Details of those conducting treatment, including their training and familiarity with participants’ culture, are important to record. Cultural norms may dictate that certain types of torture are not disclosed, let alone discussed with or presented for therapeutic intervention by a stranger, as when interventions require detailed description for testimony‐taking or exposure offered to men or women who have been subjected to rape or other sexual violence as torture (Patel 2004).
Closer attention to attrition and collection of adverse effects is essential for a better understanding of what might be contraindications for particular types of treatment. It would also be advisable to evaluate outcomes not only by symptom counts but also by exploring participants’ views on the cultural meaningfulness and appropriateness of the intervention, and on their overall satisfaction with therapy.
-
No ideal solution has been proposed to the problems of measures developed in one culture and available in its language but required for a study in a very different culture and language. However, guides are available for attempts to test or demonstrate authenticity across cultures, and to attend both to broader concepts and to detail in translation and testing of assessment instruments (McHorney 2006; Sousa 2011). Simple translation and back‐translation can only identify linguistic equivalence, not meanings, use or expression—all of which are in part contextual, and which affect the validity of the instrument.
An important step in choosing and adjusting outcome measures is conceptual scrutiny. In this field, conceptual scrutiny would require collecting from potential participants information about health difficulties, how they are defined and understood and which among them are held to indicate well‐being. This leads to exploration of the meanings of items on existing instruments; equivalent expressions or constructs in a given culture and language, if they exist; and alternative indicators meaningful to the population under study that are not captured by the proposed instruments. Such research can also examine the cultural appropriateness of certain items or questions (Elsass 2009; Heine 2002), while taking into account gender and other norms within a cultural group. However, few measures undergo the conceptual scrutiny that should precede translation and testing (Johnson 2006). Working in partnership with interpreters and, when possible, with fully bilingual or multi‐lingual researchers and clinicians who are conversant with or part of the same cultural backgrounds as study participants, makes these tasks easier and better integrated.
Conceptual scrutiny and cultural validation before translation and testing may result in measures differing in structure, such that apparently equivalent scores do not appear to map on to apparently equivalent emotional states (McHorney 2006). Further, dialects and regional and cultural biases in language use can define the meanings of terms differently. For example, Arabic, spoken across many countries, may involve differing use of words and expressions with subtle but important variations in meaning. Even professional interpreters vary in their use of language, their own understanding of psychological health terms and their potential preferences for one or another language for particular purposes. Use of interpreters in conducting therapeutic interventions with torture survivors has been widely addressed (Haenel 1997; Patel 2003b).
Use of PTSD to define need, even with the broader criteria available in DSM‐5, is unsatisfactory for the many reasons outlined above. Difficulties in functioning are associated with post‐traumatic symptoms and with depression, and should be assessed (NICE 2005; NICE 2010). However, the focus needs to stay on disruption by psychological problems of daily functioning, as for some torture survivors (particularly those who are seeking asylum), external barriers impose significant limitations, such as legal sanctions against employment or restricted opportunities for educational or vocational activities. Quality of life measures need to be adjusted for what is culturally appropriate, such as gender‐defined duties; what is restricted by the individual’s refugee status (such as paid employment or disposable income); and what is unsafe (taking a walk in a setting of widespread violence); otherwise these restrictions are represented as individual choices. Beyond wider assessment of the psychological state of the individual is a context of variables, change in which may bring about significant improvement or worsening: granting or refusing asylum status; hearing good or bad news about family members with whom all contact had been lost; reunifying with friends or family; or encountering new persecution.
There is a risk that the requirements for RCTs, many of which are described above, will override participants’ best interests. The research field in this area will be enriched by rigorous case studies, qualitative methods and other designs, which can answer questions that cannot, for ethical, practical or scientific reasons, be resolved by RCTs. The impact of interventions at the level of the family and community, as well as for the individual, is an important area of focus.
Acknowledgements
Thanks to Les Hearn, Amschel de Rothschild, Katrina Scior and Olivia Stocker for help with translation.
Appendices
Appendix 1. CCDAN TOPICS LIST—PSYCHOLOGICAL INTERVENTIONS
-
BEHAVIOR THERAPY / BEHAVIOR MODIFICATION
ACTIVITY SCHEDULING
ASSERTIVENESS TRAINING
-
AVERSION THERAPY
COVERT SENSITIZATION
BEHAVIOR CONTRACTING
BEHAVIOR MODIFICATION
-
BIOFEEDBACK, PSYCHOLOGY
FEEDBACK, SENSORY
CONTINGENCY MANAGEMENT
CONVERSION THERAPY
DISTRACTION THERAPY
-
EXPOSURE THERAPY
Abreaction Therapy
Sensitivity Training
-
Systematic Desensitization Therapy
Eye Movement Desensitization Reprocessing
Implosive Therapy
PLEASANT EVENTS
PSYCHOEDUCATION
PROBLEM‐FOCUSED
RECIPROCAL INHIBITION THERAPY
-
RELAXATION TECHNIQUES
Autogenic Training
Distraction
Guided Imagery
RESPONSE COST
SLEEP PHASE CHRONOTHERAPY
-
SOCIAL SKILLS TRAINING
Social Effectiveness
-
COGNITIVE BEHAVIORAL THERAPY
PROBLEM SOLVING
RATIONAL EMOTIVE THERAPY
REALITY THERAPY
RESTRUCTURING
ROLE PLAY
SCHEMAS
SELF‐CONTROL
STRESS MANAGEMENT
-
THIRD WAVE COGNITIVE BEHAVIORAL THERAPIES
Acceptance and Commitment Therapy (ACT)
BEHAVIORAL ACTIVATION
Cognitive Behavioral Analysis System of Psychotherapy (CBASP)
Compassion‐focused
DIALECTICAL BEHAVIOR THERAPY
DIFFUSION
FUNCTIONAL ANALYTIC PSYCHOTHERAPY (FAP)
METACOGNITIVE THERAPY
Mind Training
Mindfulness
-
PSYCHODYNAMIC THERAPIES
BRIEF PSYCHOTHERAPY
COUNTERTRANSFERENCE
FREUDIAN
-
GROUP THERAPY
Balint Group Therapy
INSIGHT ORIENTED THERAPY
JUNGIAN
KLEINIAN
-
OBJECT RELATIONS
Person Centred Therapy, Client‐Centred Therapy
-
PSYCHOANALYTIC THERAPY
Alderian Therapy
Dream Analysis
Free Association
Self Analysis
SHORT‐TERM PSYCHOTHERAPY
TRANSFERENCE
-
HUMANISTIC THERAPIES
EXISTENTIAL THERAPY
-
EXPERIENTIAL THERAPY
PROCESS‐EXPERIENTIAL
GESTALT THERAPY
EXPRESSIVE THERAPY
GRIEFWORK
ROGERIAN
Non‐directive Therapy
SUPPORTIVE THERAPY
Transactional Analysis
-
INTEGRATIVE THERAPIES
COGNITIVE ANALYTICAL THERAPY
COUNSELLING
ECLECTIC THERAPY
-
INTERPERSONAL THERAPY
Psychodynamic Interpersonal Therapy
MULTIMODAL
TRANSTHEORETICAL
-
SYSTEMIC THERAPIES
-
CONJOINT THERAPY
-
COUPLES, MARITAL OR RELATIONSHIP THERAPY
EMOTION FOCUSSED THERAPY
FAMILY THERAPY
-
Integrative Behavioral Couple Therapy (IBCT)
NARRATIVE THERAPY
Personal Construct
-
Socioenvironmental Therapy
Milieu Therapy
Therapeutic Community
SOLUTION FOCUSED BRIEF THERAPY
-
-
OTHER PSYCHOLOGICALLY‐ORIENTED INTERVENTIONS
ACTING OUT
AGE REGRESSION THERAPY
ART THERAPY
BIBLIOTHERAPY
CATHARSIS
COLOUR THERAPY
CRISIS INTERVENTION
DANCE THERAPY
DRAMA THERAPY
EMOTIONAL FREEDOM TECHNIQUES
-
HYPNOTHERAPY
Autosuggestion
Neuro‐Linguistic Programming (NLP)
Persuasion
Meditation [CINAHL]
MORITA THERAPY
MUSIC THERAPY
PLAY THERAPY
PRIMAL THERAPY
PSYCHODRAMA
REMINISCENCE THERAPY
SEX THERAPY
Appendix 2. OVID PsycINFO (1806 to June 2014)
A sensitive search was conducted using terms for population (only) plus an RCT filter:
1. torture/ 2. torture$.mp. 3. "prisoners of war"/ 4. ((trauma* or psychotrauma* or violence) and (asylum$ or refugee$ or hostage$)).mp. 5. ((organi#ed or mass) adj3 violence).mp. 6. exp survivors/ and War/ 7. ((surviv$ or victim*) adj7 war).mp. 8. (polit$ adj7 persecut$).mp. 9. exp genocide/ 10. genocide.mp. 11. or/1‐10 12. clinical trials.sh. 13. mental health program evaluation.sh. 14. treatment effectiveness evaluation.sh. 15. placebo.sh. 16. placebo$.ti,ab. 17. (wait* and list* and (control* or group)).ab. 18. ("treatment as usual" or TAU).ab. 19. randomly.ab. 20. randomi#ed.ti,ab. 21. trial.ti,ab. 22. ((singl$ or doubl$ or trebl$ or tripl$) adj3 (blind$ or mask$ or dummy)).mp. 23. (control$ adj3 (trial$ or study or studies or group$)).ti,ab. 24. factorial$.ti,ab. 25. allocat$.ti,ab. 26. assign$.ti,ab. 27. (crossover$ or cross over$).ti,ab. 28. (quasi adj (experimental or random$)).mp. 29. "2000".md. 30. or/12‐29 31. 11 and 30
Appendix 3. OVID MEDLINE (1950 to June 2014)
1. torture/ 2. torture$.tw. 3. ((trauma* or psychotrauma* or violence) and (asylum$ or refugee$ or hostage$)).mp. 4. ((organi#ed or mass) adj3 violence).tw. 5. exp survivors/ and war/ 6. ((surviv$ or victim*) adj7 war).tw. 7. (polit$ adj7 persecut$).tw. 8. genocide.tw. 9. or/1‐8 10. randomized controlled trial.pt. 11. controlled clinical trial.pt. 12. randomi#ed.ti,ab. 13. randomly.ab. 14. placebo.ab. 15. (wait* and list* and (control* or group)).ab. 16. (treatment as usual or TAU).ab. 17. trial.ab. 18. groups.ab. 19. (control$ adj3 (trial or study)).ab,ti. 20. ((singl$ or doubl$ or tripl$ or trebl$) adj3 (blind$ or mask$ or dummy)).mp. 21. or/10‐20 22. 9 and 21
Appendix 4. OVID EMBASE (1980 to June 2014)
1. torture/ 2. torture$.tw. 3. torture survivor/ 4. ((trauma* or psychotrauma* or violence) and (asylum$ or refugee$ or hostage$)).mp. 5. ((organi#ed or mass) adj3 violence).tw. 6. survivor/ and war/ 7. ((surviv$ or victim*) adj7 war).tw. 8. (polit$ adj7 persecut$).tw. 9. genocide.mp. 10. or/1‐9 11. randomized controlled trial.de. 12. randomization.de. 13. randomi#ed.ti,ab. 14. randomly.ab. 15. placebo.de. 16. placebo$.ti,ab. 17. (wait* and list* and (control* or group)).ab. 18. (treatment as usual or TAU).ab. 19. ((singl$ or doubl$ or trebl$ or tripl$) adj3 (blind$ or mask$ or dummy)).mp. 20. factorial$.ti,ab. 21. allocat$.ti,ab. 22. assign$.ti,ab. 23. volunteer$.ti,ab. 24. crossover procedure.de. 25. (crossover$ or cross over$).ti,ab. 26. (quasi adj (experimental or random$)).mp. 27. (control$ adj3 (trial$ or study or studies or group$)).ti,ab. 28. or/1‐17 29. 10 and 28
Appendix 5. CENTRAL (all years to June 2014)
#1 MeSH descriptor Torture explode all trees #2 torture* #3 (trauma* or psychotrauma* or violence) and (asylum* or refugee* or hostage*) #4 (organized or organised or mass) and violence #5 MeSH descriptor War this term only #6 MeSH descriptor Survivors explode all trees #7 (#5 AND #6) #8 (surviv* or victim*) and war #9 (polit* and persecut*) #10 genocide #11 (#1 OR #2 OR #3 OR #4 OR #7 OR #8 OR #9 OR #10)
Appendix 6. CCDANCTR (all years to June 2014)
CCDAN Specialised Register (CCDANCTR) The Cochrane Depression, Anxiety and Neurosis Group (CCDAN) maintains two clinical trials registers at its editorial base in Bristol, UK, a references register and a studies‐based register. The CCDANCTR‐References Register contains more than 35,000 reports of randomised controlled trials on depression, anxiety and neurosis. Approximately 60% of these references have been tagged to individual, coded trials. The coded trials are held in the CCDANCTR‐Studies Register, and records are linked between the two registers through the use of unique study ID tags. Coding of trials is based on the EU‐Psi coding manual. Please contact the CCDAN Trials Search Co‐ordinator for further details. Reports of trials for inclusion in the Group's registers are collated from routine (weekly), generic searches of MEDLINE (1950‐), EMBASE (1974‐) and PsycINFO (1967‐); quarterly searches of the Cochrane Central Register of Controlled Trials (CENTRAL) and review‐specific searches of additional databases. Reports of trials are also sourced from international trials registers c/o the trials portal of the World Health Organization (ICTRP), drug companies and handsearching of key journals, conference proceedings and other (non‐Cochrane) systematic reviews and meta‐analyses. Details of CCDAN's generic search strategies can be found on the Group‘s website.
The CCDANCTR (studies and references register) was searched using the following free‐text terms. (torture* or ((trauma* or psychotrauma* or violence) and (asylum* or refugee* or hostage*)) or ((organised or organized or mass) and violence) or (surviv* and war) or ((surviv* or victim*) and war) or (polit* and persecut*) or genocide)
Appendix 7. ClinicalTrials.gov and WHO ICTRP (all years to June 2014)
Tortur*
Appendix 8. CINAHL—EBSCO Host (1988 to April 2013)
S1 (MH "Torture") S2 (MH "Torture Survivors") S3 (torture*) S4 ((trauma* or psychotrauma* or violence) and (asylum* or refugee* or hostage*)) S5 ((organi#ed or mass) N3 violence) S6 (MH "Survivors") and (MH "War+") S7 ((surviv* or victim*) N7 war) S8 (polit* N7 persecut*) S9 (genocide) S10 (S1 or S2 or S3 or S4 or S5 or S6 or S7 or S8 or S9) S11 (MH "Clinical Trials+") S12 (PT Clinical trial) S13 (TX clini* N1 trial*) S14 (TX ((singl* N1 blind*) or (singl* N1 mask*)) or TX ((doubl* N1 blind*) or (doubl* N1 mask*)) or TX ((tripl* N1 blind*) or (tripl* N1 mask*)) or TX ((trebl* N1 blind*) or (trebl* N1 mask*))) S15 (TX randomi* control* trial*) S16 (MH "Random Assignment") S17 ((TX random* allocat*) or (TX allocat* random*)) S18 (TX placebo*) S19 (TX (wait* and list* and (control* or group))) S20 ((TX "treatment as usual") or (TX TAU)) S21 (TX (control* N3 (trial* or study or studies or group*))) S22 (MH "Quantitative Studies") S23 (S11 or S21 or S13 or S14 or S15 or S16 or S17 or S18 or S19 or S20 or S21 or S22) S24 (S10 and S21)
Appendix 9. Web of Science (all years to April 2013)
1. torture* 2. ((trauma* or psychotrauma* or violence) and (asylum* or refugee* or hostage*)) 3. ((organized or organised or mass) NEAR/3 violence) 4. ((surviv* or victim*) NEAR/7 war) 5. (polit* NEAR/7 persecut*) 6. genocide 7. (#7 OR #6 OR #5 OR #4 OR #3 OR #2 OR #1) 8. (randomized or randomised) 9. (random* NEAR/3 (allocat* or assign*)) 10. placebo* 11. ((wait* and list*) SAME (control* or group)) 12. ("treatment as usual" or TAU) 13. (control* NEAR/3 (trial or study)) 14 ((singl* or doubl* or tripl* or trebl*) NEAR/3 (blind* OR mask* OR dummy)) 15. (quasi NEAR/3 (experimental or random*)) 16. (#15 OR #14 OR #13 OR #12 OR #11 OR #10 OR #9 OR #8) 17. (#7 and #16)
Appendix 10. LILACS (all years to April 2013)
Tortur*
Appendix 11. OpenSIGLE (all years to April 2013)
Tortur*
Appendix 12. PILOTS—ProQuest Host (all years to April 2013)
Randomised AND tortur* randomized AND tortur* randomly allocated AND tortur* randomly assigned AND tortur* quasi‐random AND tortur* quasi‐randomized AND tortur* quasi‐randomised AND tortur* placebo AND tortur* controlled trial AND tortur* controlled study AND tortur*
Appendix 13. Rehabilitation and Research Centre for Torture Victims (RCT) (all years to April 2013)
Randomised AND tortur* randomized AND tortur* randomly allocated AND tortur* randomly assigned AND tortur* quasi‐random AND tortur* quasi‐randomized AND tortur* quasi‐randomised AND tortur* placebo AND tortur* controlled trial AND tortur* controlled study AND tortur*
Appendix 14. Top 10 journals (all years to April 2013)
1. Social Science and Medicine
Randomised AND tortur* randomized AND tortur* randomly allocated AND tortur* randomly assigned AND tortur* quasi‐random AND tortur* quasi‐randomized AND tortur* quasi‐randomised AND tortur* placebo AND tortur* controlled trial AND tortur* controlled study AND tortur*
2. Journal of Nervous and Mental Disease
Randomised AND tortur* randomized AND tortur* randomly allocated AND tortur* randomly assigned AND tortur* quasi‐random AND tortur* quasi‐randomized AND tortur* quasi‐randomised AND tortur* placebo AND tortur* controlled trial AND tortur* controlled study AND tortur*
3. Journal of Traumatic Stress
Randomised AND tortur* randomized AND tortur* randomly allocated AND tortur* randomly assigned AND tortur* quasi‐random AND tortur* quasi‐randomized AND tortur* quasi‐randomised AND tortur* placebo AND tortur* controlled trial AND tortur* controlled study AND tortur*
4. Torture
Randomised AND tortur* randomized AND tortur* randomly allocated AND tortur* randomly assigned AND tortur* quasi‐random AND tortur* quasi‐randomized AND tortur* quasi‐randomised AND tortur* placebo AND tortur* controlled trial AND tortur* controlled study AND tortur*
5. Nursing Times
Randomised AND tortur* randomized AND tortur* randomly allocated AND tortur* randomly assigned AND tortur* quasi‐random AND tortur* quasi‐randomized AND tortur* quasi‐randomised AND tortur* placebo AND tortur* controlled trial AND tortur* controlled study AND tortur*
6. JAMA
Randomised AND torture randomized AND torture randomly allocated AND torture randomly assigned AND torture quasi‐random AND torture quasi‐randomized AND torture quasi‐randomised AND torture placebo AND torture controlled trial AND torture controlled study AND torture
7. Prehospital and Disaster Medicine
Randomised AND tortur* randomized AND tortur* randomly allocated AND tortur* randomly assigned AND tortur* quasi‐random AND tortur* quasi‐randomized AND tortur* quasi‐randomised AND tortur* placebo AND tortur* controlled trial AND tortur* controlled study AND tortur*
8. Nursing Research
Randomised AND tortur* randomized AND tortur* randomly allocated AND tortur* randomly assigned AND tortur* quasi‐random AND tortur* quasi‐randomized AND tortur* quasi‐randomised AND tortur* placebo AND tortur* controlled trial AND tortur* controlled study AND tortur*
9. American Journal of Public Health
Randomised AND tortur* randomized AND tortur* randomly allocated AND tortur* randomly assigned AND tortur* quasi‐random AND tortur* quasi‐randomized AND tortur* quasi‐randomised AND tortur* placebo AND tortur* controlled trial AND tortur* controlled study AND tortur*
10. Nursing Standard
Randomised AND tortur* randomized AND tortur* randomly allocated AND tortur* randomly assigned AND tortur* quasi‐random AND tortur* quasi‐randomized AND tortur* quasi‐randomised AND tortur* placebo AND tortur* controlled trial AND tortur* controlled study AND tortur*
In June 2014, two additional journals were searched (electronically)—Traumatology and European Journal of Psychotraumatology—using the following terms: (torture* or refugee* or asylum*) (all years to date).
Data and analyses
Comparison 1. Psychological intervention versus control.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Distress | 7 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 End of treatment | 5 | 290 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.15 [‐0.39, 0.09] |
| 1.2 Follow‐up | 4 | 86 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.63 [‐1.07, ‐0.19] |
| 2 Post‐traumatic stress symptoms | 9 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 End of treatment | 7 | 388 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.30 [‐0.66, 0.06] |
| 2.2 Follow‐up | 4 | 86 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.52 [‐0.97, ‐0.07] |
| 3 Post‐traumatic stress caseness | 3 | Odds Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 3.1 End of treatment | 3 | 52 | Odds Ratio (M‐H, Random, 95% CI) | 0.28 [0.06, 1.36] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Bichescu 2007.
| Methods | Study design: randomised controlled trial | |
| Participants | 18 former political detainees under communist Romania, living at home Diagnosis: PTSD on 2 occasions 1 year apart; no signs of disability on MINI Method of diagnosis: CIDI (Composite International Diagnostic Interview, WHO 1997) Age: mean 69 years Sex: 94% men, 6% women Location: Romania |
|
| Interventions | Participants were randomly assigned to: 1. Experimental arm Duration: 5 2‐hour sessions Treatment protocol: narrative exposure (NET) Therapist: Romanian‐speaking female PhD psychology student; therapy in own language 2. Comparator arm Duration: 1 session Treatment protocol: psychoeducation (PED); "standardized treatment" Therapist: Romanian‐speaking female PhD psychology student; therapy in own language |
|
| Outcomes |
Time points for assessment: pretreatment and at 6‐month follow‐up Assessment language: Romanian; measures translated as necessary Primary outcome Symptoms of PTSD (CIDI) for diagnosis and symptom count, no information about validation Secondary outcome Depression (BDI) through interview with translation from English |
|
| baseline characteristics | Mean number of mistreatments 13; no detail Mean of 42 years since release from imprisonment; mean duration of imprisonment 6 years Education, occupational status and marital status recorded |
|
| adherence and completion | All 18 completed treatment and follow‐up | |
| Notes |
Date of study: 2003 Funding source: Hans‐Böckler Foundation and Deutsche Forschungsgemeinschaft Declarations of interest among primary researchers: no declaration Assessment by clinical psychology and MA psychology students who were intended to be blind to treatment, which was not entirely successfull |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | By "random selection procedure of participants' name‐cards": unclear who performed selection |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to render participants nor practitioners blind to allocation. Expectations of benefit not assessed |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Most blind assessors were arranged, but "it was not possible for us to achieve complete blindness in all cases," as participants revealed details of treatment that identified the condition |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants included: no attrition |
| Selective reporting (reporting bias) | Unclear risk | 2 measures used and reported; no protocol available |
| Therapist allegiance | High risk | Allegiance to NET |
| Treatment fidelity | Unclear risk | No information |
| Therapist qualifications | Unclear risk | In training |
| Other bias | Unclear risk | Real‐time translation of assessment measures, so not standardised |
Hensel‐Dittmann 2011.
| Methods | Study design: randomised controlled trial | |
| Participants | 28 clinic outpatients, refugees from various countries—most still seeking asylum Diagnosis: PTSD Method of diagnosis:DSM‐IV Age: not given, but no differences between groups Sex: not given, but no differences between groups Location: Germany |
|
| Interventions | Participants were randomly assigned to: 1. Experimental arm Duration: 10 individual sessions of mean 90 minutes Treatment protocol: Narrative exposure (NET) manualised (Schauer) Therapist: trained, with interpreter when necessary (17/28) 2. Comparator arm Duration: 10 individual sessions of mean 90 minutes Treatment protocol: stress inoculation training (SIT), avoiding any element of exposure Therapist: trained, with interpreter when necessary (17/28) Same therapists for both arms |
|
| Outcomes |
Time points for assessment: pretreatment and at 6‐month and 1‐year follow‐up Assessment language: measures in German; no information on cross‐cultural use Primary outcome PTSD severity score (clinician‐administered scale: CAPS) Secondary outcome PTSD diagnosis: DSM‐IV Depression: Hamilton Depression Scale |
|
| baseline characteristics | 76% had been tortured; remainder had experienced war No differences between groups in length of time in Germany, area of origin, education or co‐morbid psychiatric disorders, but no baseline data given |
|
| adherence and completion | 5 dropouts NET, 2 dropouts SIT (1 SIT participant deported) | |
| Notes |
Date of study: 2004 to 2007 Funding source: European Refugee Fund and Deutsche Forschungsgemeinschaft Declarations of interest among primary researchers: no conflicting interests |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Participants matched pairwise by gender, age and region of origin, then allocated by flipping coin |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to render participants nor practitioners blind to allocation. Expectations of benefit not assessed |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Assessors blind (unless accidentally unblinded) to allocation |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data provided different N at each time point; analysis by intention‐to‐treat, so mixed‐effect models with neither imputation nor LOCF |
| Selective reporting (reporting bias) | Unclear risk | All outcomes reported in trial methods; no protocol available |
| Therapist allegiance | High risk | NET: active treatment |
| Treatment fidelity | Low risk | Manual by Schauer |
| Therapist qualifications | Low risk | Trained therapists |
| Other bias | Unclear risk | Most refugees still had asylum undecided, so may have had an incentive to underreport improvement |
Igreja 2004.
| Methods | Study design: randomised controlled trial | |
| Participants | 137 people, post civil war, mostly rural population seen in their homes Diagnosis: PTSD caseness Method of diagnosis: self‐Inventory for PTSD (Hovens et al, 2001) Age: mean 40 years (SD 14) Sex: 56% men, 44% women Location: Mozambique |
|
| Interventions | Participants were randomly assigned to: 1. Experimental arm Duration: 1 occasionally 2 individual sessions, about 60 minutes Treatment protocol: testimony writing: references to 'testimony method' but no mention of protocol Therapist/interviewer: first study author interpreted into Chi‐Gorongese by native speakers (same sex as participant) 2. Comparator arm Duration: none Treatment protocol: no intervention Therapist: none |
|
| Outcomes |
Time points for assessment: pretreatment and at 11‐month follow‐up Assessment language: all via structured interview, as participants illliterate, interpreted into Chi‐Gorongese Outcomes (not specified as primary or secondary) Post‐traumatic stress symptoms: self‐Inventory for PTSD; only Western data available on performance of scale Psychiatric symptoms: Self‐Report Questionnaire, validated in non‐Western populations Nightmares: Nocturnal Intrusions after Traumatic Experiences Questionnaire; only Western data available on performance of scale |
|
| baseline characteristics | 58% intervention group and 55% control group tortured; many other relevant events of organised violence on Harvard Trauma Questionnaire, validated in non‐Western populations Mean 15 years in war zone Mean 4 living children and 3 dead |
|
| adherence and completion | 6 dropouts | |
| Notes |
Date of study: not given Funding source: part by Associação Esperança Para Todos, Mozambique Declarations of interest among primary researchers: none Third arm (not included here) of non‐case participants |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Participants given consecutive numbers, divided according to caseness, then allocated to treatment or control according to odd or even number |
| Allocation concealment (selection bias) | High risk | None |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to render participants nor practitioners blind to allocation. Expectations of benefit not assessed |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Unclear who conducted assessments—all by interview |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Several dropouts (death, moving away) |
| Selective reporting (reporting bias) | Unclear risk | All outcomes listed in trial reported; no protocol available |
| Therapist allegiance | Unclear risk | No information provided |
| Treatment fidelity | Unclear risk | No information provided |
| Therapist qualifications | Unclear risk | No information provided |
| Other bias | Unclear risk | Real‐time translation of assessment measures, so not standardised |
Neuner 2010.
| Methods | Study design: randomised controlled trial | |
| Participants | 32 adult outpatients at German refugee clinic from Turkey, Balkans, Africa; seeking asylum Diagnosis: none Age: mean age 31.3 years (SD 7.7) Sex: 69% men, 31% women Location: Germany |
|
| Interventions | Participants were randomly assigned to: 1, Experimental arm Duration: median 9 individual sessions of 2 hours each Treatment protocol: narrative exposure therapy (NET), manualised Therapist: trained, experienced, observed by expert, with interpreters 2. Comparator arm Duration: variable Treatment protocol: treatment as usual Therapist: not given |
|
| Outcomes |
Time points for assessment: pretreatment and at 6‐month follow‐up Assessment language: used trained interpreters Primary outcome Post‐traumatic Stress Disorder Scale (PDS), clinician‐administered, for symptom frequency Secondary outcome Diagnosis of PTSD using DSM‐IV in combination with PDS Pain symptoms total using Composite International Diagnostic Interview (CIDI), part C Hopkins Symptom Checklist HSCL‐25 Depression Scale No comments on use of measures in non‐Western populations |
|
| baseline characteristics | All survivors of organised violence; 28 had been tortured Mean 55 months in exile; 5 in each group still applying for asylum, and others refused asylum but granted temporary leave to remain because of mental health Mean 7 years of education |
|
| adherence and completion | 2 dropped out of NET, none from TAU | |
| Notes |
Date of study: not given Funding source: Deutsche Forschungsgemeinschaft Declarations of interest among primary researchers: no declaration |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Participants were randomized into the two groups using a block permutation procedure with blocks of four patients" |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to render participants nor practitioners blind to allocation. Expectations of benefit not assessed |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Tried to keep interviewers for post‐treatment assessment blind to condition, but some unblinded unwittingly by participants |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Used mixed‐effect models for missing data on the 2 who dropped out of NET |
| Selective reporting (reporting bias) | Unclear risk | All outcomes listed in trial reported; no protocol available |
| Therapist allegiance | High risk | Allegiance to NET (treatment arm) |
| Treatment fidelity | Low risk | Manual |
| Therapist qualifications | Low risk | Therapists qualified |
| Other bias | Unclear risk | Real‐time translation of assessment measures, so not standardised Asylum status of most participants not yet determined; possible incentive to underreport improvement |
Paunovic 2001.
| Methods | Study design: randomised controlled trial | |
| Participants | 20 outpatients referred from psychiatric units and torture survivor treatment centre; refugees but no information about countries of origin Diagnosis: PTSD Method of diagnosis:CAPS‐IV clinician‐administered PTSD scale Age: mean 37.9 years (SD 7.6) Sex: 85% men, 15% women Location: Sweden |
|
| Interventions | Participants were randomly assigned to: 1. Experimental arm Duration: 16 to 20 weekly individual sessions of 1 to 2 hours plus homework Treatment protocol: CBT, including exposure Therapist: doctoral student in clinical psychology, supervised by qualified and experienced clinical psychologist 2. Comparator arm Duration: 16 to 20 weekly individual sessions of 1 to 2 hours plus homework Treatment protocol: exposure Therapist: doctoral student in clinical psychology, supervised by qualified and experienced clinical psychologist All therapy in Swedish, in which participants were sufficiently fluent |
|
| Outcomes |
Time points for assessment: pretreatment, post treatment and at 6‐month follow‐up Assessment language: all in Swedish, in which participants were sufficiently fluent Primary outcome Clinician Administered PTSD Scale (CAPS)‐IV for total PTSD severity Secondary outcome Clinician Administered PTSD Scale (CAPS)‐IV for global PTSD severity Hamilton Anxiety Scale Hamilton Depression Scale PTSD Symptom Scale PSS‐SR Self‐report of PTSD Symptoms Impact of Events Scale IES‐R Self‐report of PTSD Symptoms Beck Anxiety Inventory (self‐report) State‐Trait Anxiety Inventory (STAI) (self‐report) Beck Depression Inventory (self‐report) World Assumptions Scale for Cognitive Schemata Quality of Life Inventory (QOLI) (self‐report) for satisfaction weighted by importance No reference to validation in non‐Western populations |
|
| baseline characteristics | 6 torture survivors and others had combat experience or witnessed traumatic events 12 married/steady relationship, 3 single, 1 divorced; 3 full‐time work, 7 unemployed, 6 long‐term sick leave; 10 up to high school education and 6 some university education 75% given steady dose of psychoactive drugs |
|
| adherence and completion | 4 early dropouts/exclusion: 1 E and 2 CBT non‐attendance; 1 CBT hostility to therapist | |
| Notes |
Date of study: not given Funding source: none stated Declarations of interest among primary researchers: no declaration Hypothesis that CBT is more effective, so CBT = treatment and exposure = control |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "The patients were randomly assigned to two treatments, CBT or E, with the provision that no more than two consecutive patients could be randomized to the same condition" |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to render participants nor practitioners blind to allocation. Expectations of benefit not assessed |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | All by self‐report; no third party assessment |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 4 dropouts excluded from analyses |
| Selective reporting (reporting bias) | Unclear risk | All outcomes in trial reported; no protocol available |
| Therapist allegiance | Unclear risk | No information provided |
| Treatment fidelity | Unclear risk | No information provided |
| Therapist qualifications | Unclear risk | In training |
| Other bias | Unclear risk | None |
Pokhariyal 2012.
| Methods | Study design: randomised controlled trial | |
| Participants | 96 survivors of torture: 43 Kenyan torture survivors recruited from People Against Torture or released Kenyan political prisoners and 53 refugees in Kenya under UNHCR refugee programme Diagnosis: none Age: Kenyans mean 36.9 years (SD 11.5); refugees mean 26.7 years (SD 6.5) Sex: Kenyans 81% men, 19% women; refugees 51% men, 49% women Location: Kenya |
|
| Interventions | Participants were randomly assigned to: 1. Experimental arm Duration: mean 5 individual sessions MTP + 5 participants had 1 to 3 sessions CT Treatment protocol: Multi‐sensory trauma processing (MTP) +/‐ conventional treatment (CT) Therapists: members of research team, all experienced and qualified in counselling psychology 2. Comparator arm Duration: mean 9 individual sessions Treatment protocol: conventional treatment (CT) = "eclectic methods of psychotherapy": an assortment of therapeutic techniques with varied or no evidence of efficacy Therapists: members of research team, all experienced and qualified in counselling psychology Interpreted into Kiswahili or Kikuyu for Kenyan participants when necessary |
|
| Outcomes |
Time points for assessment: pretreatment, post treatment Assessment language: in Kiswahili or Kikuyu for Kenyan participants; some used interpreters Primary outcome Stress State Inventory (SSI) (self‐report) (items on PTSD symptoms) Secondary outcome: none SSI developed for US veterans: no comment on cross‐cultural validity |
|
| baseline characteristics | Partial data only Kenyans (N = 26): 18 educated up to secondary level, 7 beyond; 17 married, 6 single, 3 divorced/widowed; 16 Christian, 5 Muslim, 5 other Refugees (N = 30): educated up to secondary level, 10 beyond; 30 married, 17 single, 2 divorced/widowed; 20 Christian, 26 Muslim, 3 other |
|
| adherence and completion | 27 "excluded for various reasons": 35 Kenyans and 34 refugees completed | |
| Notes |
Date of study: not given Funding source: USAID, USIU Declarations of interest among primary researchers: none Kenyan and refugee participants had somewhat different baseline scores and received different doses of treatment, but we combined them for analysis Data were provided individually per subject in tables, so means and standard deviations were calculated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Names of recruits converted to numbers and then "randomly assigned" Kenyans and refugees separately. No further detail |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to render participants nor practitioners blind to allocation. Expectations of benefit not assessed |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Self‐report measure but described as "administered," so unclear |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Only completers analysed |
| Selective reporting (reporting bias) | Unclear risk | Single outcome measure in trial reported; no protocol available |
| Therapist allegiance | Unclear risk | No information provided |
| Treatment fidelity | Unclear risk | No information provided |
| Therapist qualifications | Low risk | Qualified therapists |
| Other bias | Unclear risk | Real‐time translation of assessment measures, so not standardised |
Schauer 2006.
| Methods | Study design: randomised controlled trial | |
| Participants | 32 outpatients in refugee trauma clinic; mostly Kurdish; asylum seekers awaiting determination of asylum claim Diagnosis: PTSD Method of diagnosis:DSM‐IV Age: mean age 31.3 years (SD 7.7) Sex: 69% men, 31% women Location: Germany |
|
| Interventions | Participants were randomly assigned to: 1. Experimental arm Duration: no information Treatment protocol: narrative exposure therapy (NET) (Schauer manual) Therapist: no information 2. Comparator arm Duration: no information Treatment protocol: treatment as usual (various psychotherapies ± pharmacotherapy) Therapist: no information Interpreters used for all |
|
| Outcomes |
Time points for assessment: pretreatment, post treatment and at 6‐month follow‐up Assessment language: various, interpreted Primary outcome Post‐traumatic Distress Scale (PDS) Secondary outcome None |
|
| baseline characteristics | More than half described torture experiences with average of 4 to 5 traumatic events in prison or detention Mean 7 years of education, median 2 children Some taking medication |
|
| adherence and completion | All completed | |
| Notes |
Date of study: not given Funding source: none Declarations of interest among primary researchers: no declaration Data provided by first study author |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to render participants nor practitioners blind to allocation. Expectations of benefit not assessed |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Self‐report |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No attrition |
| Selective reporting (reporting bias) | Unclear risk | Single outcome in trial reported; no protocol available |
| Therapist allegiance | High risk | Allegiance to NET (treatment arm) |
| Treatment fidelity | Low risk | Manual (Schauer) |
| Therapist qualifications | Unclear risk | No information provided |
| Other bias | Unclear risk | Asylum status of participants undecided; may act as incentive to underreport improvement |
ter Heide 2011.
| Methods |
Study design: randomised controlled trial Pilot study for larger trial |
|
| Participants | 20 outpatients of trauma clinic; asylum seekers or refugees from Europe, Middle East, Africa Diagnosis: PTSD Method of diagnosis: modified diagnostic criteria for PTSD Age: mean age 41.5 years (SD 8.8) Sex: 60% men, 40% women Location: Netherlands |
|
| Interventions | Participants were randomly assigned to: 1. Experimental arm Duration: 11 individual sessions weekly or biweekly Treatment protocol: Eye Movement Desensitisation and Reprocessing EMDR: “A therapist manual was designed containing information on study design and guidelines on therapy content” Therapist: trained and 1 session evaluated by supervisor 2. Comparator arm Duration: 11 individual sessions, weekly or biweekly Treatment protocol: stabilisation (present‐centred therapy; no exposure) Therapist: various disciplines, supervised monthly Interpreters used for 3 in each arm Treatments evaluated using fidelity scales |
|
| Outcomes |
Time points for assessment: pretreatment, post treatment and at 3‐month follow‐up Assessment language: “Linguistic difficulties resulted in eight participants needing an interpreter during assessments and three needing extensive help with filling in the questionnaires.” Interviews in Dutch by trained blind assessors, with interpreters as necessary Primary outcome SCID‐I for PTSD symptoms, clinician‐administered Secondary outcome Harvard Trauma Questionnaire HTQ for PTSD symptoms, clinician administered HSCL‐25 for Anxiety, self‐report HSCL‐25 for Depression, self‐report WHOQOL‐BREF for Quality of Life, self‐report “HTQ, HSCL‐25, and WHOQOL‐BREF are self report questionnaires that are widely used with this population and are available in many different languages. All three have good psychometric properties” |
|
| baseline characteristics | 14 reported torture 17 residency status granted; mean 10 years in Netherlands 11 married; 8 primary school education or less; 6 employed |
|
| adherence and completion | 10 (5 in each condition) dropped out. 3 satisfied with symptom reduction, but others disliked methods, symptoms worsened or missing sessions | |
| Notes |
Date of study: 2007 Funding source: part zonMW, Netherlands Declarations of interest among primary researchers: none |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Blocking was applied, with blocks of the latest two patients who had satisfied inclusion criteria. Participants were assigned to their experimental group using simple randomisation through flipping a coin: the outcome (EMDR for heads, stabilisation for tails) was assigned to the patient lowest in the alphabet. An independent research associate performed randomisation" |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to render participants nor practitioners blind to allocation. Expectations of benefit not assessed |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | 33/44 assessments maintained blind (using SCID) for primary outcome; secondary outcomes by self‐report |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Analysis of completers only |
| Selective reporting (reporting bias) | Unclear risk | All outcomes in trial reported; no protocol available |
| Therapist allegiance | Unclear risk | Allegiance possibly to EMDR |
| Treatment fidelity | Low risk | Manual produced for trial |
| Therapist qualifications | Low risk | Trained therapists |
| Other bias | Unclear risk | Real‐time translation of assessment measures, so not standardised |
Yeomans 2010.
| Methods | Study design: randomised controlled trial | |
| Participants | 124 refugees in Internally Displaced Persons camps, referred by church elders Diagnosis: none Age: mean age 38.6 years (SD 12.8) Sex: 56% men, 44% women Location: Burundi |
|
| Interventions | Participants were randomly assigned to: 1. Experimental arm Duration: 3‐day group workshop plus 1 day 1 month later Treatment protocol: 2 arms combined: trauma healing and reconciliation with PTSD psychoeducation, and trauma healing and reconciliation. Both described as standardised and drew on several manuals Therapist: Burundian facilitators, experienced in workshops and briefly trained for this trial 2. Comparator arm Duration: none Treatment protocol: waiting list control Therapist none Therapy in participants' own language |
|
| Outcomes |
Time points for assessment: pretreatment, post treatment Assessment language: all translated in Kirundi, back‐translated into English, compared, adjusted and subjected to expert linguistic scrutiny. Administered orally, as most participants illiterate Primary outcome Harvard Trauma Questionnaire (HTQ) Part IV (HTQa) for PTSD symptoms, self‐report orally. They refer to previous use and Cronbach's alpha in similar population Secondary outcomes HTQ additional items for emotional state related to trauma (HTQb), self‐report orally Hopkins Symptom Checklist (HSCL)‐25 for Anxiety and Depression; 10 additional items in HSCL format for somatic distress, self‐report orally. They refer to cultural sensitivity and previous use and Cronbach's alpha in similar population |
|
| baseline characteristics | "Almost all participants had been directly victimized by violence during or since the conflict in 1993" 95% < 7 years of education; 52.4% Hutu, 47.6% Tutsi |
|
| adherence and completion | 3 dropouts and 4 further losses to assessment post treatment in groups analysed | |
| Notes |
Date of study: 2007‐ Funding source: none Declarations of interest among primary researchers: no declaration Data analysed from trauma healing with and without psychoeducation vs waiting list control |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Participants were blocked according to ethnicity and gender and randomly assigned to condition" |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to render participants nor practitioners blind to allocation. Expectations of benefit not assessed |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Assessment by self‐report: interviewers blind to allocation |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Only completers analysed |
| Selective reporting (reporting bias) | Unclear risk | All outcomes in trial reported; no protocol available |
| Therapist allegiance | Unclear risk | No information provided |
| Treatment fidelity | Unclear risk | No information provided |
| Therapist qualifications | Low risk | Therapists qualified |
| Other bias | Unclear risk | Real‐time translation of assessment measures, so not standardised |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Adenauer 2011 | Participants: most not torture survivors (see NCT00563888) |
| Akhtar 1994 | Participants: most not torture survivors |
| Bass 2013 | Participants: not survivors of torture |
| Carr 2011 | Participants: most not torture survivors |
| Dybdhal 2001 | Participants: most not torture survivors |
| Hijazi 2014 | Participants: not survivors of torture |
| Kalantari 2012 | Participants: not survivors of torture |
| Liedl 2011 | Intervention: not psychological, social or welfare, but physical Participants: 70% torture survivors |
| Meffert 2011 | Participants: not survivors of torture |
| Mills 2012 | Participants: most not torture survivors |
| Morath 2014 | Participants: half war or torture survivors; outcomes biological |
| Neuner 2004 | Participants: most not torture survivors |
| Rees 2013 | Participants: randomisation broken at baseline |
| Schaal 2009 | Participants: not torture survivors |
| Sonne 2013 | Protocol, not full trial |
| Stenmark 2013 | Participants: less than 50% of completers torture survivors |
| Talbot 2013 | Not RCT |
| Walstrom 2013 | Not RCT |
Characteristics of studies awaiting assessment [ordered by study ID]
Bolton 2011.
| Methods | Randomised controlled trial NCT00925262 |
| Participants | Kurdish adults (at least 18 years old) who are torture survivors Significant symptoms of depression |
| Interventions | Cognitive processing therapy vs behavioural activation vs non‐specific counselling |
| Outcomes | Depression symptom severity
PTSD Anxiety symptom severity Function |
| Notes | Completed: not yet published |
Cavka 2005.
| Methods | Randomised trial |
| Participants | Refugee war survivors: not clear from abstract whether torture survivors |
| Interventions | Psychotherapy vs waiting list |
| Outcomes | Post‐traumatic symptoms (Harvard Trauma Questionnaire (HTQ)), psychological distress (SCL‐90‐R), neurohumoral parameters (cortisol) |
| Notes | Abstract only: unable to find full publication, including from study author |
Kolassa 2012.
| Methods | Randomised trial NCT01206790 |
| Participants | Torture survivors |
| Interventions | NET |
| Outcomes | Immunological changes |
| Notes | Study completed but not published |
Robinson 2014.
| Methods | Randomised trial NCT01459068 |
| Participants | Survivors of torture |
| Interventions | Common elements; treatment approach based on transdiagnostic assessment |
| Outcomes | Depression (HSCL‐25 locally adapted), PTSD symptoms, functional impairment |
| Notes | Completed: not yet published; some results on Clinical Trials Register |
Stenmark 2008.
| Methods | Randomised controlled trial |
| Participants | Refugees and asylum seekers in Norway diagnosed with PTSD |
| Interventions | Narrative exposure therapy vs treatment as usual |
| Outcomes | PTSD: clinician administered PTSD scale (CAPS) MINI psychiatric interview Hamilton Rating Scale for Depression |
| Notes | Abstract only; preliminary results |
Weiss 2012.
| Methods | Randomised controlled trial NCT01177072 |
| Participants | Adults exposed to torture and diagnosed with PTSD |
| Interventions | Cognitive processing therapy vs components‐based intervention |
| Outcomes | Trauma symptom severity Function |
| Notes | Completed: results not yet published |
Characteristics of ongoing studies [ordered by study ID]
Knaevelsrud 2011.
| Trial name or title | Effects of exposure for post‐traumatic stress disorder with and without cognitive restructuring in an Internet‐based intervention NCT01508377 |
| Methods | Randomised controlled trial |
| Participants | Adults who had traumatic experience and diagnosis of PTSD Fluent in written Arabic Access to the Internet |
| Interventions | Behavioural exposure for PTSD with cognitive restructuring vs behavioral exposure for PTSD without cognitive restructuring |
| Outcomes | PTSD symptoms Anxiety Depression |
| Starting date | December 2011 |
| Contact information | Christine Knaevelsrud; c.knaevelsrud@bzfo.de |
| Notes | No reply to contact with study author. 'Status unknown' in Clinical Trials Register |
Differences between protocol and review
Data were insufficient for planned sensitivity analyses.
Given the considerable overlap of scale content, the primary outcome, distress, included the PTSD symptom scales that were initially described as secondary outcomes.
Three risk of bias items were added that were appropriate to psychological interventions when neither people taking part nor those delivering the treatment can be blinded to treatment allocation.
Detail has been added to the review regarding subset data and co‐morbidities (under Types of participants) that were not included in the protocol.
Types of comparators were broadened from those envisaged in the protocol; specifically, we added conditions that were not therapist delivered but might be expected to provide therapeutic benefit, such as education, or facilitated group support; this is further addressed in the discussion of potential biases of the review process.
The timing of outcomes measures and the hierarchy of outcomes have been clarified and main comparisons defined in the review compared with the protocol.
A 'Summary of findings' table and use of GRADE to assess the quality of evidence have been added to the review.
Contributions of authors
BK managed the overall review process, conducted the searches, selected studies, authored sections of the manuscript, extracted data, undertook analysis and coded papers.
AW selected studies, authored sections of the manuscript, extracted data, undertook analysis and coded papers.
NP authored sections of the manuscript and resolved differences among selecting papers and coding.
Sources of support
Internal sources
NP and AW were employed by the Medical Foundation, and BK part of the time, while writing the protocol, UK.
External sources
NP and AW were funded by the Oak Foundation, UK.
Declarations of interest
NP and AW are clinical practitioners as well as academics; both have extensive clinical and research experience with torture survivors; AW has conducted a treatment trial in another field of mental health.
New
References
References to studies included in this review
Bichescu 2007 {published data only}
- Bichescu D, Neuner F, Schauer M, Elbert T. Narrative exposure therapy for political imprisonment‐related chronic posttraumatic stress disorder and depression. Behaviour Research and Therapy 2007;45(9):2212‐20. [DOI] [PubMed] [Google Scholar]
Hensel‐Dittmann 2011 {published data only}
- Hensel‐Dittmann D, Schauer M, Ruf M, Catani C, Odenwald M, Elbert T, et al. Treatment of traumatized victims of war and torture: a randomized controlled comparison of narrative exposure therapy and stress inoculation training. Psychotherapy and Psychosomatics 2011;80(6):345‐52. [DOI] [PubMed] [Google Scholar]
Igreja 2004 {published data only}
- Igreja V, Kleijn WC, Schreuder BJ, Dijk JA, Verschuur M. Testimony method to ameliorate post‐traumatic stress symptoms. Community‐based intervention study with Mozambican civil war survivors. British Journal of Psychiatry 2004;184:251‐7. [DOI] [PubMed] [Google Scholar]
Neuner 2010 {published data only}
- Neuner F, Kurreck S, Ruf M, Odenwald M, Elbert T, Schauer M. Can asylum‐seekers with posttraumatic stress disorder be successfully treated? A randomized controlled pilot study. Cognitive Behaviour Therapy 2010;39(3):81‐91. [DOI] [PubMed] [Google Scholar]
Paunovic 2001 {published data only}
- Paunovic N, Ost LG. Cognitive‐behavior therapy vs exposure therapy in the treatment of PTSD in refugees. Behaviour Research and Therapy 2001;39(10):1183‐97. [DOI] [PubMed] [Google Scholar]
Pokhariyal 2012 {published data only}
- Pokhariyal GP, Rono R, Munywoki S. Analysis of treatment methods for victims of torture in Kenya and East Africa region. Traumatology 2013;19(2):107‐17. [Google Scholar]
Schauer 2006 {published data only}
- Schauer M, Elbert T, Gotthardt S, Rockstroh B, Odenwald M, Neuner F. Imaginary reliving in psychotherapy modifies mind and brain [Wiedererfahrung durch Psychotherapie modifiziert Geistund Gehirn*]. Verhaltenstherapie 2006;16(2):96‐103. [Google Scholar]
ter Heide 2011 {published data only}
- ter Heide JJ, Mooren TM, Kleijn W, Jongh A, Kleber RJ. EMDR versus stabilisation in traumatised asylum seekers and refugees: results of a pilot study. European Journal of Psychotraumatology 2011;2:5881. [DOI] [PMC free article] [PubMed] [Google Scholar]
Yeomans 2010 {published data only}
- Yeomans PD, Forman EM, Herbert JD, Yuen E. A randomized trial of a reconciliation workshop with and without PTSD psychoeducation in Burundian sample. Journal of Traumatic Stress 2010;23(3):305‐12. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Adenauer 2011 {published data only}
- Adenauer H, Catani C, Gola H, Keil J, Ruf M, Schauer M, et al. Narrative exposure therapy for PTSD increases top‐down processing of aversive stimuli—evidence from a randomized controlled treatment trial. BMC Neuroscience 2011;12(127):1‐13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Catani C, Neuner F. Change of Neural Network Indicators Through Narrative Treatment of PTSD in Torture Victims. NCT00563888 2007 (accessed 20 June 2014).
Akhtar 1994 {published data only}
- Akhtar P. Project report: therapeutic effects of music on torture survivors and refugees. Torture 1994;4:121‐3. [Google Scholar]
Bass 2013 {published data only}
- Bass JK, Annan J, McIvor Murray S, Kaysen D, Griffiths S, Ketinoglu T, et al. Controlled trial of psychotherapy for Congolese survivors of sexual violence. New England Journal of Medicine 2013;368:2182‐91. [DOI] [PubMed] [Google Scholar]
Carr 2011 {published data only}
- Carr C, d'Ardenne P, Sloboda A, Scott C, Wang D, Priebe S. Group music therapy for patients with persistent post‐traumatic stress disorder: an exploratory randomized controlled trial with mixed methods evaluation. Psychology and Psychotherapy: Theory, Research and Practice 2011;10:1‐24. [DOI] [PubMed] [Google Scholar]
Dybdhal 2001 {published data only}
- Dybdahl R. Children and mothers in war: an outcome study of a psychosocial intervention program. Child Development 2001;72(4):1214‐30. [DOI] [PubMed] [Google Scholar]
Hijazi 2014 {published data only}
- Hijazi AM, Lumley MA, Ziadni MS, Rapport LJ, Arnetz BB. Brief narrative exposure therapy for posttraumatic stress in Iraqi refugees: a preliminary randomized clinical trial. Journal of Traumatic Stress 2014;27:314‐22. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kalantari 2012 {published data only}
- Kalantari M, Yule W, Dyregrov A, Neshatdoost A, Ahmadi SJ. Efficacy of writing for recovery on traumatic grief symptoms of Afghani refugee bereaved adolescents: a randomized control trial. Omega 2012;65:139‐50. [DOI] [PubMed] [Google Scholar]
Liedl 2011 {published data only}
- Liedl A, Muller J, Morina N, Karl A, Denke C, Knaevelsrud C. Physical activity within a CBT intervention improves coping with pain in traumatized refugees: results of a randomized controlled design. Pain 2011;12(2):234‐45. [DOI] [PubMed] [Google Scholar]
Meffert 2011 {published data only}
- Meffert SM, Abdo AO, Abd Alla OA, Almaki YOM, Omer AA, Yousif S, et al. A pilot randomized controlled trial of interpersonal psychotherapy for Sudanese refugees in Cairo, Egypt. Psychological Trauma: Theory, Research, Practice, and Policy 2011:doi: 10.1037/a0023540. [Google Scholar]
Mills 2012 {published data only}
- Mills LK, Teesson M, Back SE, Brady KT, Baker AL, Hopwood S, et al. Integrated exposure‐based therapy for co‐occurring posttraumatic stress disorder and substance dependence: a randomized controlled trial. Journal of the American Medical Association 2012;308(7):690‐9. [DOI] [PubMed] [Google Scholar]
Morath 2014 {published data only}
- Morath J, Gola H, Sommershof A, Hamuni G, Kolassa S, Catani C, et al. The effect of trauma‐focused therapy on the altered T cell distribution in individuals with PTSD: evidence from a randomized controlled trial. Journal of Psychiatric Research 2014;54:1‐10. [DOI] [PubMed] [Google Scholar]
Neuner 2004 {published data only}
- Neuner F, Schauer M, Klaschik C, Karunakara U, Elbert T. A comparison of narrative exposure therapy, supportive counseling, and psychoeducation for treating posttraumatic stress disorder in an African refugee settlement. Journal of Consulting and Clinical Psychology 2004;72(4):579‐87. [DOI] [PubMed] [Google Scholar]
Rees 2013 {published data only}
- Rees B, Travis F, Shapiro D, Chant R. Reduction in posttraumatic stress symptoms in Congolese refugees practicing transcendental meditation. Journal of Traumatic Stress 2013;26:295‐8. [DOI] [PubMed] [Google Scholar]
Schaal 2009 {published data only}
- Schaal S, Elbert T, Neuner F. Narrative exposure therapy versus interpersonal psychotherapy: a pilot randomized controlled trial with Rwandan genocide orphans. Psychotherapy and Psychosomatics 2009;78(5):298‐306. [DOI] [PubMed] [Google Scholar]
Sonne 2013 {published data only}
- Sonne C, Carlsson J, Elklit A, Mortensen EL, Ekstrøm M. Treatment of traumatized refugees with sertraline versus venlafaxine in combination with psychotherapy—study protocol for a randomized clinical trial. Trials 2013;14:137. [DOI] [PMC free article] [PubMed] [Google Scholar]
Stenmark 2013 {published data only}
- Halvorsen JØ, Stenmark H, Neuner F, Nordahl HM. Does dissociation moderate treatment outcomes of narrative exposure treatment for PTSD? A secondary analysis from a randomized controlled clinical trial. Behaviour Research and Therapy 2014;57:21‐8. [DOI] [PubMed] [Google Scholar]
- Stenmark H, Catani C, Neuner F, Elbert T, Holen A. Treating PTSD in refugees and asylum seekers within the general health care system. A randomized controlled multicenter study. Behaviour Research and Therapy 2013;51:641‐7. [DOI] [PubMed] [Google Scholar]
Talbot 2013 {published data only}
- Talbot A, Uwihoreye C, Kamen C, Grant P, McGlynn L, Mugabe I, et al. Treating psychological trauma among Rwandan orphans is associated with a reduction in HIV risk‐taking behaviors: a pilot study. AIDS Education and Prevention 2013;25:468‐79. [DOI] [PubMed] [Google Scholar]
Walstrom 2013 {published data only}
- Walstrom P, Operario D, Zlotnick C, Mutimura E, Benekigeri C, Cohen MH. 'I think my future will be better than my past': examining support group influence on the mental health of HIV‐infected Rwandan women. Global Public Health 2013;8:90‐105. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies awaiting assessment
Bolton 2011 {published data only}
- Bolton P. A Controlled Trial of Mental Health Interventions for Torture Survivors in Kurdistan Scientific title: A Controlled Trial of Mental Health Interventions for Common Mental Health Problems Experienced by Torture Survivors Living in Kurdistan, Iraq. http://clinicaltrials.gov/ct2/show/NCT00925262 2011 (accessed 20 June 2014).
Cavka 2005 {published data only}
- Cavka M, Joksimovic L, Schmitz N, Kruse J. Psychotherapeutic treatment of traumatised refugees with PTSD disorders: a randomised controlled trial. Journal of Psychosomatic Research 2005;58(6):S86. [Google Scholar]
Kolassa 2012 {published data only}
- Kolassa IT. Immunological changes through narrative treatment of post‐traumatic stress disorder (PTSD) in torture victims. http://clinicaltrials.gov/ct2/show/NCT01206790 2010 (accessed 20 June 2014).
Robinson 2014 {published data only}
- Robinson C. Effectiveness of mental health interventions on the Thailand‐Burma border. http://clinicaltrials.gov/ct2/show/NCT01459068 2011 (accessed 20 June 2014).
Stenmark 2008 {published and unpublished data}
- Stenmark H, Catani C, Elbert T, Gøtestam KG. Narrative exposure therapy compared to treatment as usual for refugees with PTSD—preliminary results from a randomized controlled trial. European Psychiatry [abstracts of the 20th European Congress of Psychiatry, EPA 2012 Mar 3‐6; Prague Czech Republic]. 2008; Vol. 23 (Suppl 2):S90.
Weiss 2012 {published data only}
- Weiss WM. Study of Effectiveness of Mental Health Interventions Among Torture Survivors in Southern Iraq. http://clinicaltrials.gov/ct2/show/NCT01177072 2012 (accessed 20 June 2014).
References to ongoing studies
Knaevelsrud 2011 {published data only}
- Knaevelsrud C. Effects of Exposure for Posttraumatic Stress Disorder With and Without Cognitive Restructuring in an Internet‐based Intervention. http://clinicaltrials.gov/ct2/show/NCT01508377 2011 (accessed 20 June 2014).
Additional references
AI 2013
- Amnesty International. Amnesty International Report: The State of the World's Human Rights. http://files.amnesty.org/air13/AmnestyInternational_AnnualReport2013_complete_en.pdf (accessed 25 September 2013).
Basoglu 2001
- Basoglu M, Jaranson JM, Mollica R, Kastrup M. Torture and mental health: a research overview. In: Gerrity E, Keane TM, Tuma F editor(s). Mental Health Consequences of Torture. NY: Kluwer Academic/Plenum Publishers, Inc, 2001. [Google Scholar]
Bisson 2009
- Bisson J, Andrew M. Psychological treatment of post‐traumatic stress disorder (PTSD). Cochrane Database of Systematic Reviews 2009, Issue 1. [DOI: 10.1002/14651858.CD003388.pub3] [DOI] [Google Scholar]
Bogner 2010
- Bögner D, Brewin C, Herlihy J. Refugees’ experiences of Home Office interviews: a qualitative study on the disclosure of sensitive personal information. J Ethnic Migration Studies 2010;36(3):519‐35. [Google Scholar]
Boyle 1999
- Boyle M. Diagnosis. In: Newnes C, Holmes G, Dunn C editor(s). This Is Madness: A Critical Look at Psychiatry and the Future of Mental Health Services. Ross‐on‐Wye: PCCS, 1999. [Google Scholar]
Boyle 2002
- Boyle M. Schizophrenia: A Scientific Delusion?. Second Edition. London: Routledge, 2002. [Google Scholar]
Boynton 2004
- Boynton PM, Greenhalgh T. Selecting, designing, and developing your questionnaire. BMJ 2004;328:1312‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bracken 1995
- Bracken P, Giller J, Summerfield D. Psychological responses of war and atrocity: limitations of current concepts. Social Science and Medicine 1995;40(8):1073‐82. [DOI] [PubMed] [Google Scholar]
Bracken 1998
- Bracken PJ, Celia P. Rethinking the trauma of war. London: Save the Children with Free Association Books, 1998. [Google Scholar]
Burck 2004
- Burck C. Living in several languages: implications for therapy. Journal of Family Therapy 2004;26:314‐39. [Google Scholar]
Burnett 2001
- Burnett A, Peel M. The health of survivors of torture and organised violence. BMJ 2001;322:606‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Campbell 2007
- Campbell T. Psychological assessment, diagnosis, and treatment of torture survivors: a review. Clinical Psychology Review 2007;27:628‐41. [DOI] [PubMed] [Google Scholar]
CAPS
- Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, et al. The development of a clinician‐administered PTSD scale. Journal of Trauma and Stress 1995;8:75–90. [DOI] [PubMed] [Google Scholar]
Crumlish 2010
- Crumlish N, O’Rourke K. A systematic review of treatments for post‐traumatic stress disorder among refugees and asylum seekers. The Journal of Nervous and Mental Disease 2010;198:237‐51. [DOI] [PubMed] [Google Scholar]
Elsass 2009
- Elsass P, Carlsson J, Jespersen K, Phuntsok K. Questioning Western assessment of trauma among Tibetan torture survivors. A quantitative assessment study with comments from Buddhist Lamas. Torture 2009;19(3):194‐203. [PubMed] [Google Scholar]
Fernando 2003
- Fernando S. Cultural Diversity, Mental Health and Psychiatry. Hove: Brunner‐Routledge, 2003. [Google Scholar]
Gorst‐Unsworth 1998
- Gorst‐Unsworth C, Goldenberg E. Psychological sequelae of torture and organised violence suffered by refugees from Iraq. Trauma‐related factors compared with social factors in exile. The British Journal of Psychiatry 1998;172:90‐4. [DOI] [PubMed] [Google Scholar]
Goswami 2013
- Goswami S, Rodriguez‐Sierra O, Cascardi M, Pare D. Animal models of post‐traumatic stress disorder: face validity. Frontiers in Neuroscience 2013;7:89. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gurr 2001
- Gurr R, Quiroga J. Approaches to torture rehabilitation. Torture 2001;11:5‐35. [Google Scholar]
Haenel 1997
- Haenel F. Aspects and problems associated with the use of interpreters in psychotherapy of victims of torture. Torture 1997;7(3):68‐71. [Google Scholar]
Halvorsen 2014
- Halvorsen JØ, Stenmark H, Neuner F, Nordahl HM. Does dissociation moderate treatment outcomes of narrative exposure treatment for PTSD? A secondary analysis from a randomized controlled clinical trial. Behaviour Research and Therapy 2014;57:21‐8. [DOI] [PubMed] [Google Scholar]
Hamilton 1960
- Hamilton M. A rating scale for depression. Journal of Neurology, Neurosurgery and Psychiatry 1960;23:56‐62. [DOI] [PMC free article] [PubMed] [Google Scholar]
Heine 2002
- Heine SJ, Lehman DR, Peng K, Greenholtz J. What’s wrong with cross‐cultural comparisons of subjective Likert scales? The reference‐group effect. Journal of Personality and Social Psychology 2002;82:903‐18. [PubMed] [Google Scholar]
Higgins 2003
- Higgins JPT, Thompson SG, Deeks JJ, Altman DA. Measuring inconsistency in meta‐analyses. British Medical Journal 2003;327:557‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2008a
- Higgins JPT, Altman DG (editors). Chapter 8: Assessing risk of bias in included studies. In: Higgins JPT, Green S editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.2 [updated September 2009]. The Cochrane Collaboration, 2008. www.cochrane‐handbook.org, 2008. [Google Scholar]
Higgins 2008b
- Higgins JPT, Deeks JJ, Altman DG (editors). Chapter 16.5: Special topics in statistics. In: Higgins JPT, Green S editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.2 [updated September 2009]. The Cochrane Collaboration, 2008. www.cochrane‐handbook.org, 2008. [Google Scholar]
Hollifield 2002a
- Hollifield M. Accurate measurement in cultural psychiatry: will we pay the costs?. Transcultural Psychiatry 2002;39:419‐21. [Google Scholar]
Hollifield 2002b
- Hollifield M, Warner T, Lian N, Krakow B, Jenkins JH, Kesler J, et al. Measuring trauma and health status in a refugees: a critical review. Journal of the American Medical Association 2002;288:611‐21. [DOI] [PubMed] [Google Scholar]
IRCT 2010
- International Rehabilitation Council for Torture Victims. 26 June ‐ International Day against Torture. The fight against torture: a key priority for the EU. http://europa.eu/rapid/pressReleasesAction.do?reference=MEMO/07/254. Accessed 25 February 2010.
Jacobs 2001
- Jacobs U, Iacopino V. Torture and its consequences: a challenge to clinical neuropsychology. Professional Psychology—Research and Practice 2001;32(5):458‐64. [Google Scholar]
Jaranson 1995
- Jaranson JM. Government‐sanctioned torture: status of the rehabilitation movement. Transcultural Psychiatric Research Review 1995;32:253‐86. [Google Scholar]
Jaranson 2011
- Jaranson JM, Quiroga J. Evaluating the services of torture rehabilitation programmes: history and recommendations. Torture 2011;21:98‐140. [PubMed] [Google Scholar]
Johnson 2006
- Johnson TP. Methods and frameworks for cross‐cultural measurement. Medical Care 2006;44:S17‐S20. [DOI] [PubMed] [Google Scholar]
Johnson 2008
- Johnson H, Thompson A. The development and maintenance of post‐traumatic stress disorder (PTSD) in civilian adult survivors of war trauma and torture: a review. Clinical Psychology Review 2008;28(1):36‐47. [DOI] [PubMed] [Google Scholar]
Kutchins 1997
- Kutchins H, Kirk S. Making Us Crazy: DSM, The Psychiatric Bible and the Creation of Mental Disorders. New York: Free Press, 1997. [Google Scholar]
Laban 2004
- Laban CJ, Gernaat HB, Komproe IH, Schreuders BA, Jong JT. Impact of a long asylum procedure on the prevalence of psychiatric disorders in Iraqi asylum seekers in The Netherlands. The Journal of Nervous and Mental Disease 2004;192(12):843‐51. [DOI] [PubMed] [Google Scholar]
Laungani 2004
- Laungani P. Asian Perspectives in Counselling and Psychotherapy. Hove: Brunner‐Routledge, 2004. [Google Scholar]
Lee 2007
- Lee DT, Kleinman J. Kleinman A. Rethinking depression: an ethnographic study of the experiences of depression among Chinese. Harvard Review of Psychiatry 2007;15(1):1‐8. [DOI] [PubMed] [Google Scholar]
Lund 2008
- Lund M, Sørensen JH, Christensen JB, Ølholm A. MTV om behandling og rehabilitering af PTSD—herunder traumatiserede flygtninge. Vejle: Udgivet af Region Syddanmark [Published by Center for Quality, South Denmark], 2008. [ISBN 978‐87‐92217‐03‐5] [Google Scholar]
Mahtani 2003
- Mahtani A. The right to appropriate psychological services. International Journal of Human Rights 2003;7:40‐57. [Google Scholar]
McFarlane 2012
- McFarlane C, Kaplan I. Evidence‐based psychological interventions for adult survivors of torture and trauma: a 30‐year review. Transcult Psychiatry 2012;49:539‐67. [DOI] [PubMed] [Google Scholar]
McHorney 2006
- McHorney CA, Fleishman JA. Assessing and understanding measurement equivalence in health outcome measures. Medical Care 2006;44:S205‐S210. [DOI] [PubMed] [Google Scholar]
McIvor 1995
- McIvor RJ. Turner SW. Assessmnet and treatment approaches for survivors of torture. British Journal of Psychiatry 1995;166:705‐11. [DOI] [PubMed] [Google Scholar]
Miranda 2005
- Miranda J, Bernal G, Lau A, Kohn L, Hwang W, Framboise T. State of the science on psychosocial interventions for ethnic minorities. Annual Review of Clinical Psychology 2005;1:113‐42. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mollica 2004
- Mollica R, McDonald L, Massagli M, Silove D. Measuring Trauma, Measuring Torture: Instructions and Guidance on the Utilization of the Harvard Program in Refugee Trauma’s Versions of the Hopkins Symptom Checklist‐25 (HSCL‐25) and the Harvard Trauma Questionnaire (HTQ). Cambridge, MA: Harvard Program in Refugee Trauma, 2004. [Google Scholar]
Montgomery 2011
- Montgomery E, Patel N. Torture rehabilitation: reflections on treatment outcome studies. Torture 2011;21:141‐5. [PubMed] [Google Scholar]
Moreno 2002
- Moreno A, Grodin MA. Torture and its neurological sequelae. Spinal Cord 2002;40(5):213‐23. [DOI] [PubMed] [Google Scholar]
Newlands 2004
- Newlands J, Patel N. Working with diversity: professional practice and ethical considerations. In: Tribe R, Morrissey J editor(s). The Handbook of Professional and Ethical Practice for Psychologists, Counsellors and Psychotherapists. East Sussex: Brunner‐Routledge, 2004:233‐46. [Google Scholar]
NICE 2005
- Post Traumatic Stress Disorder (PTSD). The management of PTSD in adults and children in primary and secondary care. National Clinical Practice Guideline 26 2005.
NICE 2010
- Depression. The treatment and management of depression in adults (updated version). National Clinical Practice Guideline 90 2010.
Nicholl 2004
- Nicholl C, Thompson AR. The psychological treatment of PTSD in adult refugees: a review of the current state of psychological therapies. Journal of Mental Health 2004;13:351‐62. [Google Scholar]
Nickerson 2011
- Nickerson A, Bryant RA, Silove D, Steel Z. A critical review of psychological treatments of posttraumatic stress disorder in refugees. Clinical Psychology Review 2011;31:399‐417. [DOI] [PubMed] [Google Scholar]
Norredam 2005
- Norredam M, Crosby S, Munarriz R, Piwowarczyk L, Grodin M. Urologic complications of sexual trauma among male survivors of torture. Urology 2005;65(1):28‐32. [DOI] [PubMed] [Google Scholar]
Nuesch 2009
- Nuesch E, Trelle S, Reichenbach S, Rutjes AW, Burgi E, Scherer M, et al. The effects of excluding patients from the analysis in randomised controlled trials: meta‐epidemiological study. British Medical Journal 2009;339:b3244. [DOI] [PMC free article] [PubMed] [Google Scholar]
Patel 2000
- Patel N, Bennett E, Dennis M, Dosanjh N, Miller A, Mahtani A, et al. Clinical Psychology, 'Race' and Culture: A Resource Pack for Trainers. Leicester: BPS Books, 2000. [Google Scholar]
Patel 2003a
- Patel N. Clinical psychology: reinforcing inequalities or facilitating empowerment?. The International Journal of Human Rights 2003;7(1):16‐39. [Google Scholar]
Patel 2003b
- Patel N. Speaking with the silent: addressing issues of disempowerment when working with refugee people. In: Tribe R, Raval H editor(s). Working with interpreters in Mental Health. Hove: Brunner‐Routledge, 2003:218‐37. [Google Scholar]
Patel 2004
- Patel N, Mahtani A. Psychological approach to rape as torture. In: Peel M editor(s). Rape as Torture. London: Medical Foundation Publications, 2004. [Google Scholar]
Patel 2007
- Patel N. Torture, psychology and the 'war on terror': a human rights framework. In: Roberts R editor(s). Just War: Psychology Terrorism. Ross‐on‐Wye, UK: PCCS Books, 2007. [Google Scholar]
Patel 2010
- Patel N, Granville‐Chapman C. Health Assessments with Survivors of Torture: Good Practice Clinical Guidelines. Health Assessments with Survivors of Torture: Good Clinical Practice Guidelines. London: Medical Foundation with the Department of Health (UK), 2010. [Google Scholar]
Patel 2011
- Patel N. The psychologisation of torture. In: Rapley M, Moncrieff J, Dillon J editor(s). De‐Medicalising Misery: Psychiatry, Psychology and the Human Condition. London: Palgrave Macmillan, 2011. [Google Scholar]
Pilgrim 1999
- Pilgrim D, Bentall R. The medicalisation of misery: a critical realist analysis of the concept of depression. Journal of Mental Health 1999;8:261‐74. [Google Scholar]
Porter 2005
- Porter M, Haslam M. Predisplacement and postdisplacement factors associated with mental health of refugees and internally displaced persons: a meta‐analysis. Journal of the American Medical Association 2005;294(5):602‐12. [DOI] [PubMed] [Google Scholar]
Quiroga 2005
- Quiroga J, Jaranson JM. Politically‐motivated torture and its survivors: a desk study review of the literature. Torture: Journal on Rehabilitation of Torture Victims and Prevention of Torture 2005;15(2‐3, Thematic issue):1‐111. [Google Scholar]
Rapley 2011
- Rapley M, Moncrieff J, Dillon J. De‐medicalizing Misery: Psychiatry, Psychology and the Human Condition. Houndsmills, Basingstoke Hampshire, England: Palgrave Macmillan, 2011. [Google Scholar]
Rasmussen 1990
- Rasmussen OV. Medical aspects of torture. Danish Medical Bulletin 1990;37(Suppl 1):1‐88. [PubMed] [Google Scholar]
Raval 2003a
- Raval H. Applying theoretical frameworks to the work with interpreters. In: Tribe R, Raval H editor(s). Working with Interpreters in Mental Health. Hove: Brunner‐Routledge, 2003:122‐34. [Google Scholar]
Raval 2003b
- Raval H, Smith J. Therapists' experiences of working with language interpreters. International Journal of Mental Health 2003;32(2):6‐31. [Google Scholar]
Silove 1999
- Silove D. The psychosocial effects of torture, mass human rights violations, and refugee trauma: toward an integrated conceptual framework. Journal of Nervous and Mental Disease 1999;187(4):200‐7. [DOI] [PubMed] [Google Scholar]
Sousa 2011
- Sousa VD, Rojjanasrirat W. Translation, adaptation and validation of instruments or scales for use in cross‐cultural health care research: a clear and user‐friendly guideline. Journal of Evaluation in Clinical Practice 2011;17:268‐74. [DOI] [PubMed] [Google Scholar]
Steel 2009
- Steel Z, Chey T, Silove D, Marnane C, Bryant R, Ommeren M. Association of torture and other potentially traumatic events with mental health outcomes among populations exposed to mass conflict and displacement: a systematic review and meta‐analysis. Journal of the Medical Academy 2009;302(5):537‐49. [DOI] [PubMed] [Google Scholar]
Summerfield 2001
- Summerfield D. The invention of post traumatic stress disorder and the social usefulness of a psychiatric category. British Medical Journal 2001;322:95‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Temple 1997
- Temple B. Watch your tongue: issues in translation and cross‐cultural research. Sociology 1997;31(3):607‐18. [Google Scholar]
Temple 2002
- Temple B, Edwards R. Interpreters/translators and cross‐language research: reflexivity and border crossings. International Journal of Qualitative Methods 2002;1(2):1‐12. [Google Scholar]
Thakker 1999
- Thakker J, Ward T, Strongman KT. Mental disorder and cross‐cultural psychology: a constructivist perspective. Clinical Psychology Review 1999;19(7):843‐74. [DOI] [PubMed] [Google Scholar]
UN 1984
- UN General Assembly. Convention Against Torture and Other Cruel, Inhuman or Degrading Treatment or Punishment (Available online: http://www2.ohchr.org/english/law/pdf/cat.pdf). Vol. 1465, Geneva: United Nations, Treaty Series, 1984 (10 December):85. [Google Scholar]
Van Ommeren 2001
- Ommeren M, Jong JT, Sharma B, Komproe I, Thapa SB, Cardena E. Psychiatric disorders among tortured Bhutanese refugees in Nepal. Archives of General Psychiatry 2001;58(5):475‐82. [DOI] [PubMed] [Google Scholar]
Vara 2012
- Vara R, Patel N. Working with interpreters in qualitative psychological research: methodological and ethical issues. Qualitative Research in Psychology. 2012; Vol. 9, issue 1:75‐87.
Wenk‐Ansohn 2007
- Wenk‐Ansohn M. Treatment of torture survivors—influences of the exile situation on the course of traumatic process and therapeutic possibilities. Torture 2007;17(2):88‐95. [PubMed] [Google Scholar]
Williams 2011
- Williams ME, Thompson SC. The use of community‐based interventions in reducing morbidity from the psychological impact of conflict‐related trauma among refugee populations: a systematic review of the literature. Journal of Immigrant and Minority Health 2011;13:780‐94. [DOI] [PubMed] [Google Scholar]
Williams 2013
- Williams ACdeC, Merwe J. The psychological impact of torture. British Journal of Pain 2013;7:101‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Yates 2005
- Yates SL, Morley S, Eccleston C, Williams ACD. A scale for rating the quality of psychological trials for pain. Pain 2005;117(3):314‐25. [DOI] [PubMed] [Google Scholar]


