Abstract
Objective
This study aimed to determine whether there is a difference in the efficacy of nivolumab in patients with advanced non-small cell lung cancer (NSCLC) presenting with or without brain metastases.
Materials and methods
Patients with advanced NSCLC treated with nivolumab monotherapy were retrospectively analyzed. They were divided into two cohorts according to the presence or absence of brain metastases. The differences between the two cohorts in objective response rate (ORR), disease control rate (DCR), progression-free survival (PFS), duration of response (DOR) and overall survival (OS) were investigated, and the intracranial efficacy, including intracerebral objective response rate (IORR), intracranial disease control rate (IDCR) and intracranial progression-free survival (iPFS), were examined in the brain metastasis (BM) cohort.
Results
Seventy-three patients (32 with brain metastases and 41 without) were included. The ORRs of the BM cohort and the non-brain metastasis (non-BM) cohort were 25.0% and 19.5% (p = 0.574), DCRs were 53.1% and 56.1% (p = 0.800), respectively. Their median PFS were 2.8 and 4.9 months (p = 0.204), median DORs were 9.8 and 28.8 months (p = 0.003), and median OS were 14.8 and 20.2 months (p = 0.114), respectively. According to the Cox multivariate regression analysis, BM was not an independent prognostic factor. The IORR and IDCR of the BM cohort were 28.1% and 46.9%, respectively, with a median iPFS of 2.2 months.
Conclusions
The efficacy of nivolumab is comparable in patients with NSCLC presenting with and without brain metastases, but the results must be verified in large-scale prospective studies.
Keywords: Non-small cell lung cancer, Brain metastases, PD-1, Immunotherapy, Nivolumab
Background
The brain is a common metastatic site of lung cancer. The incidence of brain metastases (BMs) in patients with non-small cell lung cancer (NSCLC) is approximately 30% [1]. Moreover, with the advances in treatment and the prolongation of patient survival in recent years, the incidence of BMs may continue to increase. BMs are an important factor affecting patient prognosis. Although therapy for advanced NSCLC has developed rapidly in recent years, the median survival of patients with NSCLC presenting BMs is only approximately 7 months [2]. Tyrosine kinase inhibitors can achieve good outcomes in patients with driver gene mutations [3]. However, drug treatments for patients who are negative for driver gene mutations are still lacking.
Immune checkpoint inhibitors (ICIs) are the most important advancement in the treatment of NSCLC in patients who are negative for mutations in driver genes. Of these ICIs, the PD-1 monoclonal antibodies (mAbs), which are represented by nivolumab and pembrolizumab, and the PD-L1 mAbs, which are represented by atezolizumab, have replaced docetaxel and obtained the status of second-line treatments for advanced NSCLC based on a series of studies (CHECKMATE 017, CHECKMATE 057, KEYNOTE 010, and OAK) [4–7]. However, as macromolecular drugs, the evidence for their efficacies in the treatment of BMs is still inadequate. Therefore, in the present study, we examined the difference in the efficacy of nivolumab in patients with advanced NSCLC presenting with and without BMs to provide more evidence of the efficacy of PD-1 mAbs in treating patients with NSCLC complicated with BMs.
Materials and methods
Patients
Patients who were histologically or cytologically confirmed to have stage IIIB–IV NSCLC according to the Union for International Cancer Control (UICC) staging system (eighth edition) and treated with nivolumab monotherapy in the Affiliated Cancer Hospital and the First Affiliated Hospital of Zhengzhou University from January 2016 to September 2018 were retrospectively investigated. Every enrolled patient underwent brain MRI as a part of baseline assessment prior to nivolumab treatment. Based on the MRI results, the patients were divided into two cohorts: with or without BMs. The activity, number of BMs and previous treatment status were not specified. At least one measurable lesion based on the RECIST 1.1 criteria was required, and for the BM cohort, at least one additional intracranial lesion was required.
Eighty-seven patients were treated with nivolumab monotherapy during the specified period. After excluding 9 patients without baseline MRI data and 5 patients without measurable lesions, 73 patients were enrolled. The clinicopathological features of the patients, including demographic data, Eastern Cooperative Oncology Group Performance Status (ECOG PS) score, pathological subtype, clinical stage, driver gene status, and number of treatment lines, were collected. The patients’ electronic imaging data were retrieved and re-examined to verify the efficacy evaluation and the time at which the disease was evaluated as progressive disease (PD). The patients’ survival status and time of death were obtained by an in-person interview or telephone follow-up.
Treatment and evaluation
Nivolumab was administered at a dose of 3 mg/kg once every two weeks until it was unable to be continued due to disease progression, intolerable side effects, or a request from the patient to terminate the treatment. Starting from the application of the first dose, the patient was subjected to an imaging evaluation every six weeks using MRI to assess intracranial lesions and computed tomography (CT) to assess systemic lesions. The efficacy evaluation was based on the RECIST 1.1 standard, which was based on the objective response rate (ORR), including complete remission (CR) and partial remission (PR), and the disease control rate (DCR), including CR, PR and stable disease (SD). Progression-free survival (PFS) was defined as the duration from the administration of the first treatment dose to disease progression or death, and the last follow-up date was used for patients without disease progression who survived. Overall survival (OS) was defined as the duration from the administration of the first treatment dose to patient death, and the last follow-up date was used for survivors. Indicators of intracranial efficacy in the BM cohort, including the intracerebral objective response rate (IORR), intracranial disease control rate (IDCR) and intracranial progression-free survival (iPFS), were evaluated.
Statistical analysis
The differences in ORR and DCR between the two cohorts were assessed using the chi-square test. The survival analysis was performed using the Kaplan–Meier method, in which the median PFS, iPFS, OS were calculated to generate survival curves, and the differences in PFS and OS between the two cohorts were assessed using the log-rank test. The Cox regression model was used in the multivariate analysis to examine the effects of BM status, sex, age, ECOG PS score, pathological subtype, clinical stage, driver gene status, and number of treatment lines on survival. It was also used in the multivariate analysis to examine the effects of prior radiotherapy (RT), number of BMs, central nervous system (CNS) symptoms, use of corticosteroids, PS score, and number of treatment lines on survival of patients with BMs. All statistical analyses were performed using the SPSS 25.0 statistical software.
Results
Baseline characteristics
Of the 73 included patients, 32 were in the BM cohort, and 41 were in the non-BM cohort. The pathological tumor subtypes of the two cohorts were significantly different (p = 0.020); specifically, patients in the BM cohort exhibited a predominance of adenocarcinoma, while patients in the non-BM cohort exhibited a predominance of squamous cell carcinoma. Regarding the clinical stage, the non-BM cohort included more patients with stage IVA tumors (p < 0.001). The two cohorts did not exhibit significantly differences in the other baseline characteristics, including sex, age, ECOG PS score, driver gene status, and number of treatment lines (Table 1).
Table 1.
Patients’ baseline characteristics
| Characteristic | BMs (n = 32) | Without BMs (n = 41) | p value |
|---|---|---|---|
| Sex, n (male/female) | 25/7 | 30/11 | 0.626 |
| Mean age, years | 57.7 ± 7.7 | 60.0 ± 11.2 | 0.324 |
| ECOG PS, n | 0.228 | ||
| 0–1 | 27 | 39 | |
| ≥ 2 | 5 | 2 | |
| Histological subtype, n | 0.020 | ||
| Squamous carcinoma | 7 | 20 | |
| Adenocarcinoma | 24 | 18 | |
| Others | 1 | 3 | |
| Stage, n | < 0.001 | ||
| IVA (M1a) | 0 | 18 | |
| IVA (M1b) | 2 | 0 | |
| IVB (M1c) | 30 | 20 | |
| IIIB/IIIC | 0 | 3 | |
| Lines of therapy, n | 0.295 | ||
| 2nd line | 28 | 32 | |
| ≥ 3rd line | 4 | 9 | |
| Driver gene status, n | 0.354 | ||
| EGFR mutations | 3 | 1 | |
| KRAS mutations | 1 | 3 | |
| Other mutations | 3 | 3 | |
| Negative | 16 | 15 | |
| Unknown | 9 | 19 | |
None of the 32 patients with BMs received concurrent brain RT with nivolumab. However, half (16/32) had received prior RT for BMs, and the median time from the completion of RT to initiation of nivolumab was 1.2 months; RT was completed in most patients within 3 months before the initiation of nivolumab therapy (14/16). Additional details about the BMs, including the number of lesions, presence or absence of symptoms, RT methods, and use of corticosteroids, are shown in Table 2.
Table 2.
Baseline characteristics of patients with BMs
| Characteristics | Patients with BMs (n = 32) | |
|---|---|---|
| No | % | |
| Number of BMs | ||
| 1 | 10 | 31.3 |
| 2–3 | 7 | 21.9 |
| > 3 | 15 | 46.9 |
| Symptomatic BMs | 7 | 21.9 |
| Prior RT for BMs | 16 | 50.0 |
| Whole-brain RT | 10 | 31.3 |
| Stereotactic radiosurgery | 6 | 18.8 |
| Interval between nivolumab therapy and RT | ||
| < 3 months before nivolumab therapy | 14 | 43.8 |
| > 3 months before nivolumab therapy | 2 | 6.3 |
| Use of corticosteroidsa | 11 | 34.4 |
aReceived corticosteroids at a dose of ≥ 10 mg of prednisone equivalents daily within 30 days of the initiation of nivolumab therapy
Tumor response
For patients in the BM cohort, the tumor responses were as follows: PR 8 patients, SD 9 patients, PD 15 patients, ORR 25.0%, and DCR 53.1%. For patients in the non-BM cohort, the treatment outcomes were as follows: PR 8 patients, SD 15 patients, PD 18 patients, ORR 19.5%, and DCR 56.1%. The differences in ORR and DCR between the two cohorts were not significant (p = 0.574 and 0.800, respectively).
Progression-free survival (PFS) and duration of response (DOR)
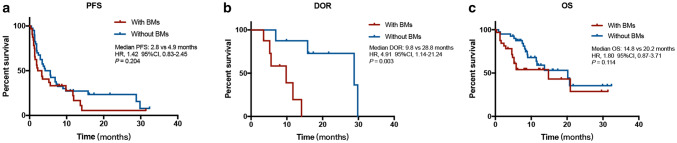
After the median follow-up of 8.0 months, 59 of the 73 patients exhibited disease progression or died, with a median PFS of 3.6 months. In the BM cohort, 26 patients exhibited disease progression (6 with intracranial progression, 7 with extracranial progression and 13 with progression in both areas), with a median PFS of 2.8 months. In the non-BM cohort, 33 patients progressed or died (1 with intracranial progression, 30 with extracranial progression, 1 with progression in both areas and 1 who died without progression), with a median PFS of 4.9 months. As shown in Fig. 1a, the difference in the median PFS between the two cohorts was not significant [hazard ratio (HR) = 1.42; 95% confidence interval (CI) 0.83–2.45; p = 0.204].
Fig. 1.
a PFS of the BM and non-BM cohorts. b DOR in the BM and non-BM cohorts. c OS of the BM and non-BM cohorts
The median DORs in the BM and non-BM cohorts were 9.8 months and 28.8 months, respectively. In addition, in contrast to PFS, the difference in median DOR between the two cohorts was significant (HR = 4.91; 95% CI 1.14–21.24; p = 0.003), as shown in Fig. 1b.
Overall survival (OS)
As of the last follow-up visit, 33 of the 73 patients had died, with a median OS of 14.8 months. Sixteen patients in the BM cohort died, with a median OS of 14.8 months, and 17 patients in the non-BM died, with a median OS of 20.2 months. As shown in Fig. 1c, the difference in the median OS between the two cohorts was not significant (HR = 1.80; 95% CI 0.87–3.71; p = 0.114). According to the Cox multivariate regression analysis which considered BM status, sex, age, ECOG PS score, pathological subtype, clinical stage, driver gene status, and number of treatment lines, ECOG PS (≥ 2) was the only factor influencing prognosis (HR = 24.25; 95% CI 6.07–96.94; p < 0.001), while BMs were not an independent prognostic factor (HR = 0.91; 95% CI 0.37–2.23; p = 0.834).
Intracranial efficacy
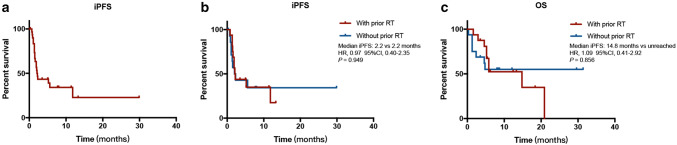
For the 32 patients in the BMs cohort, the intracranial efficacy evaluation results were as follows: CR: 2 patients, PR: 7 patients, SD: 6 patients, PD: 17 patients, IORR: 28.1%, and IDCR: 46.9%. As shown in Table 3, significant differences in IORR and IDCR were not observed between patients who received or were not treated with prior brain RT. As of the last follow-up visit, 19 patients in the BM cohort achieved intracranial PD, with a median iPFS of 2.2 months (Fig. 2a). The median iPFS was 2.2 months (HR = 0.97; 95% CI 0.40–2.35; p = 0.949) for both patients who had or had not received RT (Fig. 2c). However, in terms of failed sites of progression, a greater number of patients who did not receive prior RT presented with simultaneous intracranial and extracranial progression (Table 3). The median OS was 14.8 months for patients treated with prior RT, and OS has not yet been reached for patients without prior RT (HR = 1.09; 95% CI 0.41–2.92; p = 0.856), respectively (Fig. 2c). In the Cox multivariate regression analysis considering prior RT, number of BMs, CNS symptoms, use of corticosteroids, PS score, and number of treatment lines, the use of corticosteroids (≥ 10 mg of prednisone equivalents daily within 30 days of the initiation of nivolumab therapy) was the only variable related to OS and exerted a negative effect (HR = 25.29; 95% CI 3.49–183.13; p = 0.001).
Table 3.
Intracranial efficacy and failed sites of progression of patients with BMS who were previously treated with or without brain RT
| With prior RT | Without prior RT | p value | |
|---|---|---|---|
| IORR, % | 25 | 31.3 | 0.999 |
| IDCR, % | 50 | 43.8 | 0.723 |
| iPFS, month | 2.2 | 2.2 | 0.949 |
| OS, month | 14.8 | NR | 0.856 |
| Failed sites of progression, n | 0.034 | ||
| Intracranial | 4 | 2 | |
| Extracranial | 5 | 2 | |
| Both | 5 | 8 | |
NR not reached
Fig. 2.
a iPFS of the BM cohort. b iPFS of patients in the BM cohort stratified according to prior RT status. c OS of patients in the BM cohort stratified according to prior RT status
In the cohort without BMs, only two cases of CNS metastases occurred during disease progression: 1 case with simple intracranial progression and the other case with simultaneous extracranial progression. By the last follow-up visit, 4 patients presented CNS metastases. The CNS metastasis rates at 24 months and 30 months were 13.1%.
Discussion
Patients with NSCLC complicated with BMs, particularly patients who are negative for mutations in driver genes, have been challenging to treat due to their poor prognosis and the lack of effective therapies. Previously, the standard treatment for this type of patients was whole-brain RT, which prolonged the survival of patients with BMs by approximately threefold (from 1–2 months to 3–6 months) [8]. Subsequently, with advances in RT and supporting evidence from multiple clinical studies, stereotactic radiosurgery gradually replaced whole-brain RT for patients with localized (1–3 in number), small lesions (< 4 cm in size) [9]. For patients with a single BM, a good PS score and controllable extracranial lesions, surgery is also a reasonable treatment strategy [10]. Due to the presence of the blood–brain barrier, drug treatments have long been ignored in the treatment of BMs. In recent years, the academic community has begun to recognize that when BMs occur, the normal blood–brain barrier has already been destroyed and is completely different in patients with BMs from the normal brain tissue [11–13]. The benefits of conventional platinum-based chemotherapy, with or without bevacizumab, for patients with NSCLC presenting BMs are similar to patients with NSCLC without BMs [14, 15].
Nevertheless, for macromolecular drugs such as PD-1/PD-L1 mAbs, widespread concerns exist regarding their intracranial efficacies. Some studies have shown that this concern may not be validated. In an interim analysis in a Phase 2 clinical trial of the application of pembrolizumab in patients with malignant melanoma and patients with NSCLC presenting with BMs that included 39 patients with NSCLC and BMs, 34 patients were PD-L1-positive (Cohort 1) and 5 were PD-L1-negative (Cohort 2). The outcomes of Cohort 1 patients were as follows: IORR: 29.4%, median iPFS: 10.7 months, median OS: 8.9 months, and 2-year survival rate: 31%. No cases of remission occurred in Cohort 2 [16]. In a multicenter retrospective study that included 43 NSCLC patients with NSCLC presenting with BMs who were treated with nivolumab, the outcomes were as follows: IORR 19%, IDCR 51%, iPFS 3.9 months, and median OS 7.5 months [17]. Another retrospective study from Italy involved 409 patients with nonsquamous NSCLC presenting with asymptomatic or controlled BMs who received nivolumab treatment as a second-line or higher order treatment; the ORR and DCR were 17% and 39%, respectively, the median PFS was 3.0 months, and the median OS was 8.6 months [18].
Although these studies revealed the efficacy of PD-1 mAbs in patients with NSCLC presenting BMs, data directly comparing the systemic effects on patients with or without BMs are still lacking. Our research provided these data in the real world, while further enriching the evidence database for nivolumab in patients with NSCLC complicated with BMs. Not surprisingly, patients with and without BMs achieved similar survival benefits (both PFS and OS). However, the DOR of the BM cohort was significantly shorter than the non-BM cohort, suggesting that patients in the BM cohort whose efficacy was evaluated as SD also experienced considerable survival benefits. Studies with a larger sample size are needed to confirm whether this observation is a universal phenomenon.
At the same time, we also discussed the effect of brain RT administered prior to nivolumab on the prognosis. In the present study, a significant difference in outcomes was not observed between patients who received or did not receive prior brain RT. However, from the numerical perspective, the OS of the patients who received RT was shorter than the patients who did not receive RT. A potential explanation for this finding may be that in the real world, the BMs of patients who received brain RT are mainly symptomatic or uncontrolled. The prognosis of those patients is relatively poor. Therefore, a prospective study is required to determine whether brain RT enhances the efficacy of nivolumab in patients with BMs. In the multivariate regression analysis, the use of corticosteroids was the only variable that affected the OS of patients with BMs. A potential explanation is the immunosuppressive effects of corticosteroids [19], or the severe CNS or systemic symptoms (e.g., dyspnea) occurred in the patients who needed to use corticosteroids. In the non-BM cohort, only four patients experienced CNS metastases, and the CNS metastasis rates at 24 months and 30 months were 13.1%. Perhaps PD-1 mAbs are better at preventing BMs than treating them.
Although the outcome is not ideal, the expression of PD-L1 can be used as a predictor of PD-1/PD-L1 mAb efficacy, which has been confirmed in multiple first- and second-line clinical trials [4, 6, 7]. PD-L1 is expressed at similar levels in BMs of lung cancer lesions and extracranial lesions [20]. This finding may be one of the theoretical foundations for the hypothesis that the efficacy of this treatment for BMs is similar to extracranial lesions. The aforementioned Phase 2 clinical trial on pembrolizumab also indicated that the intracranial efficacy is poor in PD-L1-negative patients [16]. However, the correlations between the efficacies of different drugs and PD-L1 expression vary, and in the case of nivolumab, the correlation between PD-L1 expression and efficacy remains unclear [5, 21]. When approving its indications, the Food and Drug Administration (FDA) and China Food and Drug Administration (CFDA) did not require PD-L1 testing for nivolumab. Meanwhile, IHC 28-8 pharmDx, the only FDA-approved PD-L1 test for nivolumab, has not yet been approved in China. Therefore, in this study, acceptable PD-L1 test results were lacking. Further investigations are required to determine whether the PD-L1 status of extracranial lesions correlates with the efficacy of treatment for BMs in patients with BMs receiving nivolumab treatment.
Conclusions
In summary, when treated with nivolumab, the outcomes of patients with NSCLC presenting BMs were comparable to patients without BMs. A significant correlation between prior RT and intracranial efficacy was not observed. However, as this study employed a retrospective design and a small sample size, we cannot exclude the effect of selection bias on the research results, such as the imbalance in the pathological type and disease stage in the baseline characteristics. Therefore, these results must be verified in prospective studies. Meanwhile, the efficacy of a combination of PD-1 mAbs with chemotherapy, RT or even anti-angiogenic drugs in patients with BMs, and methods to distinguish patients with BMs who are more likely to benefit from PD-1 mAbs should be explored in the future.
Acknowledgements
American Journal Experts (AJE) provided English editing services. The authors thank all the patients and their families.
Abbreviations
- BMs
Brain metastases
- CFDA
China Food and Drug Administration
- CI
Confidence interval
- CNS
Central nervous system
- CR
Complete remission
- CT
Computed tomography
- DCR
Disease control rate
- DOR
Duration of response
- ECOG PS
Eastern Cooperative Oncology Group Performance Status
- FDA
Food and Drug Administration
- HR
Hazard ratio
- ICIs
Immune checkpoint inhibitors
- IDCR
Intracranial disease control rate
- IORR
Intracerebral objective response rate
- iPFS
Intracranial progression-free survival
- mAbs
Monoclonal antibodies
- non-BMs
Non-brain metastases
- NSCLC
Non-small cell lung cancer
- ORR
Objective response rate
- OS
Overall survival
- PD
Progressive disease
- PFS
Progression-free survival
- PR
Partial remission
- RT
Radiotherapy
- SD
Stable disease
- UICC
Union for International Cancer Control
Author contributions
GZ and RC contributed to the study design, data analysis, interpretation of the findings, and preparation of the manuscript. ZM and HW contributed to the study design and critical review of the manuscript. YZ, XY and PL contributed to the data analysis, interpretation of the findings, and critical review of the manuscript. MZ, XZ, JY and YN contributed to the collection and organization of the data. All authors read and approved the final manuscript.
Funding
No relevant funding was received.
Compliance with ethical standards
Conflict of interest
None of the authors have actual or potential conflicts of interest, including any financial, personal or other relationships with other people or organizations that could inappropriately influence (bias) this article, to declare.
Ethical approval
This study was approved by the ethics committees of the Affiliated Cancer Hospital and the First Affiliated Hospital of Zhengzhou University. The approval dates were October 12, 2018 and October 24, 2018, respectively. We confirm that all methods were performed in accordance with the relevant guidelines and regulations.
Informed consent
Due to the retrospective nature of the study and because no patient specimens were used, the requirement for informed consent was waived by the ethics committees.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Guowei Zhang and Ruirui Cheng contributed equally to this study.
References
- 1.Quint LE, Tummala S, Brisson LJ, Francis IR, Krupnick AS, Kazerooni EA, Iannettoni MD, Whyte RI, Orringer MB. Distribution of distant metastases from newly diagnosed non-small cell lung cancer. Ann Thorac Surg. 1996;62(1):246–250. doi: 10.1016/0003-4975(96)00220-2. [DOI] [PubMed] [Google Scholar]
- 2.Sperduto PW, Kased N, Roberge D, Xu Z, Shanley R, Luo X, Sneed PK, Chao ST, Weil RJ, Suh J, Bhatt A, Jensen AW, Brown PD, Shih HA, Kirkpatrick J, Gaspar LE, Fiveash JB, Chiang V, Knisely JP, Sperduto CM, Lin N, Mehta M. Summary report on the graded prognostic assessment: an accurate and facile diagnosis-specific tool to estimate survival for patients with brain metastases. J Clin Oncol. 2012;30(4):419–425. doi: 10.1200/JCO.2011.38.0527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yang JJ, Zhou C, Huang Y, Feng J, Lu S, Song Y, Huang C, Wu G, Zhang L, Cheng Y, Hu C, Chen G, Zhang L, Liu X, Yan HH, Tan FL, Zhong W, Wu YL. Icotinib versus whole-brain irradiation in patients with EGFR-mutant non-small-cell lung cancer and multiple brain metastases (BRAIN): a multicentre, phase 3, open-label, parallel, randomised controlled trial. Lancet Respir Med. 2017;5(9):707–716. doi: 10.1016/S2213-2600(17)30262-X. [DOI] [PubMed] [Google Scholar]
- 4.Borghaei H, Paz-Ares L, Horn L, Spigel DR, Steins M, Ready NE, Chow LQ, Vokes EE, Felip E, Holgado E, Barlesi F, Kohlhaufl M, Arrieta O, Burgio MA, Fayette J, Lena H, Poddubskaya E, Gerber DE, Gettinger SN, Rudin CM, Rizvi N, Crino L, Blumenschein GR, Jr, Antonia SJ, Dorange C, Harbison CT, Graf Finckenstein F, Brahmer JR. Nivolumab versus docetaxel in advanced nonsquamous non-small-cell lung cancer. N Engl J Med. 2015;373(17):1627–1639. doi: 10.1056/NEJMoa1507643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brahmer J, Reckamp KL, Baas P, Crino L, Eberhardt WE, Poddubskaya E, Antonia S, Pluzanski A, Vokes EE, Holgado E, Waterhouse D, Ready N, Gainor J, Aren Frontera O, Havel L, Steins M, Garassino MC, Aerts JG, Domine M, Paz-Ares L, Reck M, Baudelet C, Harbison CT, Lestini B, Spigel DR. Nivolumab versus docetaxel in advanced squamous-cell non-small-cell lung cancer. N Engl J Med. 2015;373(2):123–135. doi: 10.1056/NEJMoa1504627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Herbst RS, Baas P, Kim DW, Felip E, Perez-Gracia JL, Han JY, Molina J, Kim JH, Arvis CD, Ahn MJ, Majem M, Fidler MJ, de Castro G, Lubiniecki GM, Shentu Y, Im E, Dolled-Filhart M, Garon EB. Pembrolizumab versus docetaxel for previously treated, PD-L1-positive, advanced non-small-cell lung cancer (KEYNOTE-010): a randomised controlled trial. Lancet. 2016;387(10027):1540–1550. doi: 10.1016/S0140-6736(15)01281-7. [DOI] [PubMed] [Google Scholar]
- 7.Rittmeyer A, Barlesi F, Waterkamp D, Park K, Ciardiello F, von Pawel J, Gadgeel SM, Hida T, Kowalski DM, Dols MC, Cortinovis DL, Leach J, Polikoff J, Barrios C, Kabbinavar F, Frontera OA, De Marinis F, Turna H, Lee JS, Ballinger M, Kowanetz M, He P, Chen DS, Sandler A, Gandara DR, Group OAKS Atezolizumab versus docetaxel in patients with previously treated non-small-cell lung cancer (OAK): a phase 3, open-label, multicentre randomised controlled trial. Lancet. 2017;389(10066):255–265. doi: 10.1016/S0140-6736(16)32517-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Komaki R, Chang E. Intracranial metastases: current management strategies. MA: Blackwell Publishing Malden; 2004. Whole-brain radiation therapy; pp. 126–138. [Google Scholar]
- 9.Linskey ME, Andrews DW, Asher AL, Burri SH, Kondziolka D, Robinson PD, Ammirati M, Cobbs CS, Gaspar LE, Loeffler JS. The role of stereotactic radiosurgery in the management of patients with newly diagnosed brain metastases: a systematic review and evidence-based clinical practice guideline. J Neurooncol. 2010;96(1):45–68. doi: 10.1007/s11060-009-0073-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kalkanis SN, Kondziolka D, Gaspar LE, Burri SH, Asher AL, Cobbs CS, Ammirati M, Robinson PD, Andrews DW, Loeffler JS. The role of surgical resection in the management of newly diagnosed brain metastases: a systematic review and evidence-based clinical practice guideline. J Neurooncol. 2010;96(1):33–43. doi: 10.1007/s11060-009-0061-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fidler IJ, Yano S, Zhang R-d, Fujimaki T, Bucana CD. The seed and soil hypothesis: vascularisation and brain metastases. Lancet Oncol. 2002;3(1):53–57. doi: 10.1016/S1470-2045(01)00622-2. [DOI] [PubMed] [Google Scholar]
- 12.Lockman PR, Mittapalli RK, Taskar KS, Rudraraju V, Gril B, Bohn KA, Adkins CE, Roberts A, Thorsheim HR, Gaasch JA. Heterogeneous blood-tumor barrier permeability determines drug efficacy in mouse brain metastases of breast cancer. Clin Cancer Res. 2010;1564:2010. doi: 10.1158/1078-0432.CCR-10-1564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Percy DB, Ribot EJ, Chen Y, McFadden C, Simedrea C, Steeg PS, Chambers AF, Foster PJ. In vivo characterization of changing blood-tumor barrier permeability in a mouse model of breast cancer metastasis: a complementary magnetic resonance imaging approach. Invest Radiol. 2011;46(11):718–725. doi: 10.1097/RLI.0b013e318226c427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Barlesi F, Gervais R, Lena H, Hureaux J, Berard H, Paillotin D, Bota S, Monnet I, Chajara A, Robinet G. Pemetrexed and cisplatin as first-line chemotherapy for advanced non-small-cell lung cancer (NSCLC) with asymptomatic inoperable brain metastases: a multicenter phase II trial (GFPC 07-01) Ann Oncol. 2011;22(11):2466–2470. doi: 10.1093/annonc/mdr003. [DOI] [PubMed] [Google Scholar]
- 15.Bennouna J, Falchero L, Schott R, Bonnetain F, Coudert M, Yahia BBH, Chouaid C. Bevacizumab in combination with platinum-based chemotherapy in patients with advanced non-squamous non-small cell lung cancer with or without brain metastases: a French cohort study (EOLE) Oncology. 2018;94(1):55–64. doi: 10.1159/000480702. [DOI] [PubMed] [Google Scholar]
- 16.Goldberg SB, Gettinger SN, Mahajan A, Herbst RS, Chiang AC, Lilenbaum R, Jilaveanu L, Rowen E, Gerrish H, Komlo A (2018) Durability of brain metastasis response and overall survival in patients with non-small cell lung cancer (NSCLC) treated with pembrolizumab. American Society of Clinical Oncology
- 17.Gauvain C, Vauleon E, Chouaid C, Le Rhun E, Jabot L, Scherpereel A, Vinas F, Cortot AB, Monnet I. Intracerebral efficacy and tolerance of nivolumab in non-small-cell lung cancer patients with brain metastases. Lung Cancer. 2018;116:62–66. doi: 10.1016/j.lungcan.2017.12.008. [DOI] [PubMed] [Google Scholar]
- 18.Crinò L, Bronte G, Bidoli P, Cravero P, Minenza E, Cortesi E, Garassino MC, Proto C, Cappuzzo F, Grossi F (2019) Nivolumab and brain metastases in patients with advanced non-squamous non-small cell lung cancer. Lung Cancer [DOI] [PubMed]
- 19.Ferrara R, Lai WV, Hendriks L, Sabari JK, Caramella C, Plodkowski AJ, Halpenny D, Chaft JE, Planchard D, Riely GJ. Impact of baseline steroids on efficacy of programmed cell death-1 and programmed death-ligand 1 blockade in patients with non–small-cell lung cancer. J Clin Oncol. 2018;36:2872–2878. doi: 10.1200/JCO.2018.79.0006. [DOI] [PubMed] [Google Scholar]
- 20.Lu BY, Gupta R, Ribeiro M, Stewart T, Chiang V, Contessa JN, Adeniran A, Kluger HM, Jilaveanu L, Schalper KA (2018) PD-L1 expression and tumor-infiltrating lymphocytes in lung cancer brain metastases. American Society of Clinical Oncology
- 21.Carbone DP, Reck M, Paz-Ares L, Creelan B, Horn L, Steins M, Felip E, van den Heuvel MM, Ciuleanu T-E, Badin F. First-line nivolumab in stage IV or recurrent non-small-cell lung cancer. N Engl J Med. 2017;376(25):2415–2426. doi: 10.1056/NEJMoa1613493. [DOI] [PMC free article] [PubMed] [Google Scholar]