Abstract
CTLA-4 blockade by means of ipilimumab (IPI) potentiates the immune response and improves overall survival (OS) in a minority of metastatic melanoma (MM) patients. We investigated the role of soluble CTLA-4 (sCTLA-4) as a possible biomarker for identifying this subset of patients. sCTLA-4 levels were analyzed at baseline in sera from 113 IPI-treated MM patients by ELISA, and the median value (200 pg/ml) was used to create two equally sized subgroups. Associations of sCTLA-4 with best overall response (BOR) to IPI and immune-related adverse events (irAEs) were evaluated through logistic regression. Kaplan–Meier and Cox regression methods were used to analyze OS. A remarkable association between sCTLA-4 levels and BOR was found. Specifically, the proportion of patients with sCTLA-4 > 200 pg/ml in irSD or irPD (immune-related stable or progressive disease) was, respectively, 80% (OR = 0.23; 95%CL = 0.03–1.88) and 89% (OR = 0.11; 95%CL = 0.02–0.71) and was lower than that observed among patients in irCR/irPR (immune-related complete/partial response). sCTLA-4 levels increased during IPI treatment, since the proportion of patients showing sCTLA > 200 pg/ml after 3 cycles was 4 times higher (OR = 4.41, 95%CL = 1.02–19.1) than that after 1 cycle. Moreover, a significantly lower death rate was estimated for patients with sCTLA-4 > 200 pg/ml (HR = 0.61, 95%CL = 0.39–0.98). Higher baseline sCTLA-4 levels were also associated with the onset of any irAE (p value = 0.029), in particular irAEs of the digestive tract (p value = 0.041). In conclusion, our results suggest that high sCTLA-4 serum levels might predict favorable clinical outcome and higher risk of irAEs in IPI-treated MM patients.
Electronic supplementary material
The online version of this article (10.1007/s00262-018-2258-1) contains supplementary material, which is available to authorized users.
Keywords: Soluble CTLA-4, Ipilimumab, Best response, Adverse events, Overall survival
Introduction
Ipilimumab (IPI), the human monoclonal antibody targeting CTLA-4 immune checkpoint, was approved for the treatment of metastatic melanoma (MM) after the demonstration that it improves overall survival (OS) in both pre-treated and untreated MM patients [1, 2]. However, the benefit in terms of long-lasting disease control and long-term survival was limited to a relatively small fraction of patients (about 20%) [1, 3].
The antitumor mechanism of action proposed for IPI relies on the blockade of CTLA-4 binding to CD80 and CD86 ligands on the antigen presenting cells (APC), resulting in T-cell activation, intratumoral infiltration, and tumor-specific effector functions [4, 5]. Indeed, IPI may prevent the physiological inhibitory function exerted by CTLA-4, upon binding to ligands, on cell proliferation, interleukin-2 production and cell cycle progression of activated T cells [6, 7]. Several molecular mechanisms, either cell intrinsic or cell extrinsic, have been proposed for CTLA-4 inhibitory function operating in both conventional T (Tconv) and regulatory T (Treg) cells. Among those, competition with the costimulatory CD28 homologue for binding to the shared ligands CD80/CD86 on APC is likely to be the major mechanism along with downregulation of CD80 and CD86 on APC via trans-endocytosis [reviewed in 8].
Most functional studies on CTLA-4 have focused on the membrane-bound receptor isoform (full-length; flCTLA-4), but other CTLA-4 isoforms can also be expressed, including a soluble form of CTLA-4 (sCTLA-4) which originates from a spliced mRNA transcript that lacks the transmembrane sequence [9]. sCTLA-4 has been detected in normal human serum [10]; higher serum levels have been reported in autoimmune diseases [11] and in tumors such as pediatric B-acute lymphoblastic leukemia [12], breast cancer [13], lung, esophageal, and other cancers [14], thus supporting its important role in T-cell-mediated immune regulation.
Indeed, sCTLA-4, that can be secreted by both Tconv and Treg cells [15], is able to bind CD80/CD86 ligands on APC and might interfere with their interaction with flCTLA-4 or CD28 on T-cell surface [16] leading to upregulation or downregulation of the immune response [16, 17].
The evidence that IPI may be clinically efficacious in only a fraction of MM patients highlights the need to identify baseline biomarkers allowing to select patients who may benefit most from IPI treatment.
Several potential biomarkers including those of the systemic inflammatory response, neutrophil–lymphocyte ratio, soluble factors, lactate dehydrogenase (LDH), absolute lymphocyte count (ALC) [18], and epigenetic features of melanoma and tumor microenvironment [19] have been proposed.
We recently reported on CTLA-4 gene variants (SNVs) as possible biomarkers predictive of IPI efficacy and improved long-term survival [20] as well as of onset of endocrine adverse events [21] in a cohort of IPI-treated MM patients.
In the present study, we measured the serum levels of sCTLA-4 in a subgroup of this previous MM cohort and evaluated their correlation with response to IPI therapy, immune-related adverse events (irAEs) and OS. In some patients we also investigated serum sCTLA-4 levels during the course of IPI treatment to evaluate their possible variations.
Materials and methods
Patient characteristics and serum collection
This study included 113 patients, aged 24–85 years, presenting stage IV MM; these patients, whose pre-treatment sera were available for testing sCTLA-4, are part of the previous cohort of 173 patients we analyzed for CTLA-4 SNVs [20, 21]. Among the 113 patients, 89 were enrolled between July 2010 and January 2012 through the Italian Expanded Access Program (EAP) [22], whereas 24 patients were enrolled between February 2012 and September 2013 when IPI became available in Italy.
Patients were treated intravenously with IPI (3 mg/kg) every 3 weeks for a maximum of 4 doses as previously described [20]. Clinical response was assessed as the best overall response (BOR) using immune-related response criteria (irRC) [23] and classified as immune-related complete response (irCR), partial response (irPR), stable disease (irSD), or progressive disease (irPD).
All patients were monitored for onset of adverse events (AEs), including immune-related adverse events (irAEs), graded according to the NCI Common Terminology Criteria for Adverse Events (CTCAE) version 3, 2006 [24]. These included irAEs of skin (rash and pruritus), digestive tract (gastro-intestinal: diarrhea, nausea and vomiting; liver and pancreas disorders: hepatitis, transaminases or amylase and lipase increase) and endocrine system (hypophysitis, hypothyroidism and thyroiditis).
Serum samples were collected from 113 patients at baseline (before starting the first IPI cycle) and from 59 (52.2%) of them also at each IPI cycle before the infusion (patients before cycle 2: N = 47; before cycle 3: N = 10; before cycle 4: N = 2).
We also collected serum samples from 108 healthy blood donors recruited at the participating centers as controls (HC, 56.5% male, median age: 48.3; range = 24.0–66.2).
Detection of sCTLA-4 by ELISA
Aliquots from MM patient and HC sera were centrifuged (1500g for 10 min at 4 °C), and supernatants were stored at –80 °C until the sCTLA-4 analysis was performed.
sCTLA-4 was measured using an sCTLA-4-specific enzyme-linked immunosorbent assay (ELISA) kit (Bender MedSystems, Milan, Italy) according to manufacturer’s protocol. Each sample was tested undiluted (100 µl/well) in duplicate with deviation between duplicates lower than 10% for any value reported. The lowest sensitivity threshold was 100 pg/ml.
CTLA-4 genotyping
Genotyping of CTLA-4 SNVs − 1661A > G (rs4553808), − 1577G > A (rs11571316), − 658C > T (rs11571317), − 319C > T (rs5742909), + 49A > G (rs231775) and CT60G > A (rs3087243) was performed as previously described [20].
Statistical analysis
Patient and disease characteristics were explored using descriptive statistics. Discrete variables (e.g., gender, ECOG-PS) were expressed as relative frequencies (percentages), while continuous variables (e.g., age and time from diagnosis) were summarized using median and range values. Analysis of contingency tables and related Chi-square test was used to assess the associations between categorical variables, while the nonparametric median test was applied to compare distributions of continuous variables among subgroups of subjects.
In all analytical contexts, baseline sCTLA-4 levels were used as a dichotomous factor, a priori categorized according to 200 pg/ml, which was the median value of MM patients. This can be considered a reasonable threshold given the quite small sample size and the fairly high frequency of sCTLA-4 zero values (N = 43, 38.1%) among MM patients. In addition, the median guarantees two equally sized subgroups.
Multinomial logistic regression (MLR) modelling was used to analyze the association between sCTLA-4 levels and the best overall response (BOR: irCR + irPR, irSD and irPD) while adjusting for individual baseline characteristics: age at 1st IPI cycle, gender, time from diagnosis, LDH levels, brain, liver, and cutaneous metastases, participating center and the derived neutrophil-to-lymphocyte ratio (dNLR). The dNLR, calculated as ANC/(WBC–ANC), was used in agreement with the previous studies [25, 26], where only the absolute neutrophil count (ANC) and white cell count (WBC) were recorded.
MLR can be considered as an extension of the more widely used binomial logistic regression modelling (BLR) for dichotomous outcome (i.e., responders vs non-responders) in that it allows to perform simultaneously two binary comparisons: irSD vs irCR + irPR and irPD vs irCR + irPR. Within each comparison, odds ratio (OR) point estimate, along with 95% confidence limits (95%CL), was computed and considered as an index of association between sCTLA-4 levels and the clinical outcome.
BLR modelling with a random intercept was used to assess the relationship between the longitudinal trajectory of dichotomized sCTLA-4 repeated measurements and the number of IPI cycles administered [27]. This method is particularly appropriate for analyzing longitudinal data given its capability to attenuate some statistical drawbacks due to the correlation among sCTLA-4 measurements performed on the same subject.
To evaluate the correlation between sCTLA-4 levels and irAE development, a BLR analysis was performed using the presence/absence of specific side effects as a binary response. In addition, in this case, regression results were adjusted for baseline patient characteristics.
Analysis of correlation of sCTLA4 levels with OS, as estimated from the date of first IPI cycle to the date of last contact or death from any cause, was carried out using the Kaplan–Meier method, while the Cox regression modelling was applied to estimate the correlation between cumulative death rates and sCTLA4 levels controlling for imbalances in baseline patient characteristics. Death rate (hazard) ratio (HR) and corresponding 95%CL were used as an index of association [28].
Statistical inference on HR/OR was carried out using the likelihood ratio test, and a two-tailed p value < 0.050 was considered as statistically significant. All analyses were performed using Stata (StataCorp. Stata Statistical Software. Release 13.1. College Station, TX (USA), 2013).
Results
Patient features, disease characteristics, and treatment regimens
Overall, 113 MM patients were enrolled from July 2010 to September 2013. The observation period ended by June 30th, 2015. Based on tumor location, the primary melanoma subtype was cutaneous (N = 90, 79.7%) or mucosal (N = 12, 10.6%). For the remaining 11 (9.7%) patients, the primary tumor site was unknown.
Table 1 shows the main patient features, disease characteristics, and pre/post-IPI treatment regimens. Namely, at the time of the first IPI cycle, 23 (20.4%) patients had brain metastases and 38 (33.6%) had liver metastases. Among them, 7 patients (6.2%) presented metastases at both sites. The other 59 (52.2%) patients had metastases at sites different from brain and/or liver, mostly lung (n = 57, 50.4%) and lymph nodes (n = 42, 37.2%). Overall, about one-third of all patients (n = 38, 33.6%) presented distant disease at 3 or more sites.
Table 1.
Patient and disease characteristics, and treatment regimens
| Characteristics | N (%) |
|---|---|
| Age, years, at 1st IPI‡ cycle (median, range) | 58.4 (28.4–85.0) |
| Gender | |
| Male | 62 (54.9) |
| Female | 51 (45.1) |
| Primary melanoma subtype | |
| Cutaneous | 90 (79.8) |
| Mucosal | 12 (10.6) |
| Unknown | 11 (9.7) |
| ECOG§ performance status | |
| 0 | 73 (64.6) |
| 1 | 31 (27.4) |
| 2 | 8 (7.1) |
| Unknown | 1 (0.9) |
| Serum LDH¶ | |
| Normal level | 44 (38.9) |
| ≥ Upper limit of normal (ULN) | 59 (52.2) |
| Unknown | 10 (8.9) |
| Number of metastasis sites at 1st IPI cycle | |
| 1 | 42 (37.2) |
| 2 | 33 (29.2) |
| ≥ 3 | 38 (33.6) |
| Brain metastases | |
| Present | 23 (20.4) |
| Absent | 90 (79.7) |
| Liver metastases | |
| Present | 38 (33.6) |
| Absent | 75 (66.4) |
| Metastases other than brain and/or liverδ | |
| Yes | 59 (26.7) |
| No (only brain or/and liver) | 54 (24.4) |
| Number of therapies prior to IPI | |
| 1 | 66 (58.4) |
| 2 | 33 (29.2) |
| ≥ 3 | 14 (12.4) |
| Chemotherapy& prior to IPI | |
| Yes | 99 (87.6) |
| No | 14 (12.4) |
| Immunotherapy# prior to IPI | |
| Yes | 25 (22.1) |
| No | 88 (77.9) |
| Targeted therapy† prior to IPI | |
| Yes | 14 (12.4) |
| No | 99 (87.6) |
| Therapy post-IPI* | |
| Yes | 42 (37.2) |
| No | 71 (62.8) |
| Derived neutrophil-to-lymphocyte ratio | |
| ≤ 2.2 | 52 (46.0) |
| > 2.2 | 53 (46.9) |
| Unknown | 8 (7.1) |
| Whole sample | 113 (100.0) |
‡IPI ipilimumab
§ECOG-PS Eastern Cooperative Oncology Group-Performance Status
¶LDH, lactate dehydrogenase, δone or more sites of distant disease other than brain and/or liver (mostly lung and lymph node)
&Including mainly: dacarbazine, temozolomide and fotemustine
#Including mainly interferon alpha and interleukin-2
†BRAF/MEK inhibitors including vemurafenib and dabrafenib
*Including IPI, chemotherapy, BRAF/MEK inhibitors and anti-PD-1
Eighty-two (72.6%) patients received the 4 doses of IPI as scheduled; the remaining 31(28.4%) patients received 3 or less doses.
Most patients (n = 66, 58.4%) received 1 line of systemic therapy prior to treatment with IPI, while 33 (29.2%) and 14 (12.4%) received 2 or ≥ 3 lines, respectively. Chemotherapy was the most frequent regimen used (n = 99, 87.5%) followed by immunotherapy (n = 25, 22.1%) and targeted therapy (n = 14, 12.4%). Among the patients receiving immunotherapy, 14 received interferon alone, 10 received chemotherapy associated with interferon and/or interleukin-2 and 1 received Mage-3 vaccine. Ipilimumab was never administered.
Following IPI therapy, 41 (39.4%) patients among the 104 who experienced disease progression received further systemic treatment including chemotherapy, BRAF/MEK inhibitors, anti-PD-1, or IPI re-treatment.
Detection of sCTLA-4 in MM serum samples at baseline and level correlation with prognostic factors
We investigated whether sCTLA-4 could be detected through ELISA assay in sera from the MM patients at baseline and in sera from HC subjects matched to MM patients by participating centers to increase the comparability between the two groups.
The contribution of participating centers in terms of number of recruited patients did not vary significantly (range = 11.5%-22.1%, Chi-square test p value = 0.168).
Overall, individual levels of sCTLA-4 ranged widely from 0 to 10660.0 pg/ml (mean ± SD = 876.9 pg/ml ± 1738.3 pg/ml) in the MM patients and from 0 to 5736.1 pg/ml (mean ± SD = 641.2 pg/ml ± 1055.5 pg/ml) in the HC subjects. sCTLA-4 median levels in MM patients were slightly lower than those in the HC group (200.0 pg/ml vs 263.5 pg/ml), but this difference was not statistically significant.
Baseline serum sCTLA-4 levels were correlated with MM prognostic factors including LDH levels, ECOG, dNLR, and other patient characteristics (age at 1st IPI cycle, melanoma subtype, number of chemo- and immune therapies prior to IPI and number of metastatic locations) among which the dALC, a derived lymphocyte count (= WBC–ANC) which can be regarded as an estimate of the actual ALC [25, 26]. Spearman correlation analysis between sCTLA-4 levels and the aforementioned factors showed very low and statistically non-significant associations ranging from − 0.19 (sCTLA-4 vs dNLR) to + 0.17 (sCTLA-4 vs gender).
Correlation of baseline sCTLA-4 levels with BOR
Table 2 reports the joint distribution of BOR and sCTLA-4 levels, and the results of the MLR modelling. Of the 113 patients, 19 (16.8%) showed irPR + irCR, 16 (14.2%) irSD, and 78 (69.0%) irPD. Using irCR + irPR category as a base outcome, the frequency of irSD responses resulted to be about 80% lower in MM patients with sCTLA-4 > 200 pg/ml compared to those with sCTLA-4 ≤ 200 pg/ml (OR = 0.23; 95%CL = 0.03–1.88; p value = 0.169). In addition, a statistically significant reduction of about 90% was observed in patients with higher sCTLA-4 levels when irPD category was compared to irCR + irPR category (OR = 0.11; 95%CL = 0.02–0.71; p value = 0.020). We also performed the MLR analysis on the patient population deprived of the mucosal melanoma subgroup and we obtained completely overlapping results (Supplementary Table 1).
Table 2.
Association of sCTLA-4 serum levels with best overall response (BOR) in IPI-treated MM patients
| sCTLA-4 levels | Total | irCR + irPR | irSD | irPD | irSD vs irCR + irPR | irPD vs irCR + irPR | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | OR | 95%CL | p value | OR | 95%CL | p value | ||
| ≤ 200 pg/ml | 57 | 7 | 36.8 | 7 | 43.8 | 43 | 55.1 | 1.00 | (Ref.) | 0.169 | 1.00 | (Ref.) | 0.020 |
| > 200 pg/ml | 56 | 12 | 63.2 | 9 | 56.3 | 35 | 44.9 | 0.23 | 0.03–1.88 | 0.11 | 0.02–0.71 | ||
| Whole sample | 113 | 19 | 100.0 | 16 | 100.0 | 78 | 100.0 | – | – | – | – | – | – |
Association of sCTLA-4 serum levels with BOR was estimated through a multinomial logistic regression modelling using the value 200 pg/ml as cutoff point for serum sCTLA-4 levels. Detection of sCTLA-4 levels was performed by ELISA. All samples were tested in duplicate with deviation between duplicates lower than 10% for any reported value
IPI ipilimumab, irCR immune-related complete response, irPR immune-related partial response, irSD immune-related stable disease, irPD immune-related progressive disease, OR odds ratio adjusted for age at 1st IPI cycle, gender, time from diagnosis, LDH levels, dNLR pre-IPI immunotherapy, brain, liver and cutaneous metastases and participating center, 95%CL 95% confidence, p value significance level of the likelihood ratio test, Ref. reference category
Moreover, higher values of sCTLA-4 were associated with a better disease responsiveness in the study population. In particular, sCTLA-4 median levels decreased from responders (irCR + irPR, 440.4 pg/ml) to patients with stable disease (irSD, 268.5 pg/ml) and then to progressors (irPD, 108.4 pg/ml; Fig. 1).
Fig. 1.
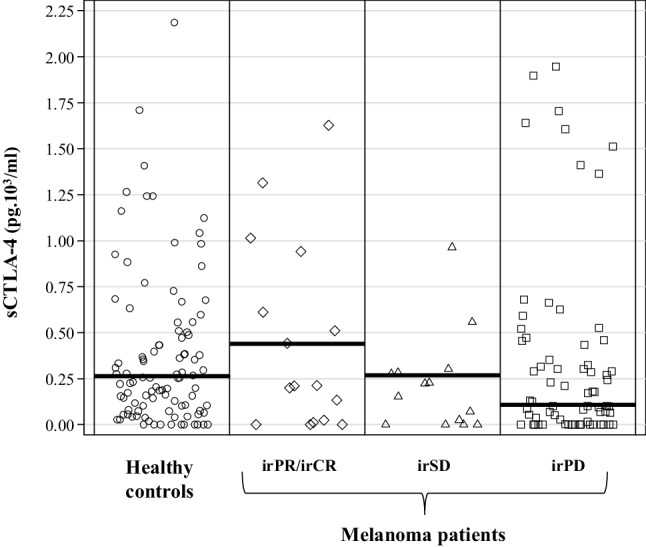
Analysis of sCTLA-4 serum levels in healthy controls and IPI-treated MM patients classified according to the best overall response: irPR/irCR, irSD, irPD. sCTLA-4 levels were evaluated by ELISA testing in duplicate wells. Results were expressed as sCTLA-4 concentrations (pg × 103/ml); the horizontal lines in each column represent median values of each subgroup. To point out the difference between median sCTLA-4 levels, only data in the range 0.00–2.25 pg × 103/ml were plotted. irPR/irCR immune-related partial/complete response, irSD immune-related stable disease, irPD immune-related progressive disease
As we previously reported that BOR to IPI may be influenced by CTLA-4 SNVs which are known to affect the levels of sCTLA-4 mRNA expression [29], we also investigated the possible correlation between SNVs and sCTLA-4 levels in the MM patients, but we did not find any remarkable association.
Longitudinal detection of sCTLA-4 in MM serum samples
Whenever possible, we assessed changes in serum sCTLA-4 levels during the course of IPI treatment. Thus, besides the 113 baseline serum samples, 59 additional sera were withdrawn prior to the sequential IPI cycles; out of these samples, 47 were collected before the 2nd cycle and the other 12 before the 3rd or the 4th cycle.
Logistic regression with a random intercept applied to the dichotomized sCTLA-4 (sCTLA-4 > 200 pg/ml vs sCTLA-4 ≤ 200 pg/ml) showed an increasing dose–response relationship between the number of IPI cycles and the proportion of patients with sCTLA-4 > 200 pg/ml. In particular, after three or more IPI cycles this proportion was more than four times higher than that observed after a single cycle (OR = 4.41, 95%CL = 1.02–19.1, p value for linear trend = 0.016) (Table 3).
Table 3.
Joint effect of number of IPI cycles and best overall response on the proportion of MM patients with elevated (> 200 pg/ml) sCTLA-4 serum levels
| Factors and levels | sCTLA-4 levels > 200 pg/ml vs ≤ 200 pg/ml | p value | |
|---|---|---|---|
| OR | 95%CL | ||
| Number of IPI cycles | |||
| 1 | 1.00 | (Ref.) | 0.016 |
| 2 | 1.57 | 0.95–2.62 | |
| ≥ 3 | 4.41 | 1.02–19.1 | |
| Best overall response | |||
| irCR + irPR | 1.00 | (Ref.) | 0.034 |
| irSD | 0.32 | 0.06–1.73 | |
| irPD | 0.17 | 0.04–0.68 | |
The association between the number of IPI cycles and BOR with sCTLA-4 serum levels (sCTLA-4 > 200 pg/ml vs sCTLA-4 ≤ 200 pg/ml) was estimated through a random-intercept binomial logistic regression modelling. Each OR represents the ratio between the proportion of patients with sCTLA-4 > 200 in a specific category and the same proportion in the reference category
IPI ipilimumab, irCR immune-related complete response, irPR immune-related partial response, irSD immune-related stable disease, irPD immune-related progressive disease, OR odds ratio adjusted for age, gender, time from diagnosis, LDH levels, dNLR, pre-IPI immunotherapy, brain, liver and cutaneous metastases, and participating center, 95%CL 95% confidence limit for OR, p value significance level of the likelihood ratio test for linear trend, Ref reference category
Moreover, a statistically significant worsening in clinical conditions was found to be inversely correlated with higher levels of sCTLA-4. Specifically, compared to responsive disease (irCR + irPR), stable (irSD) and progressive (irPD) disease gave rise, respectively, to a proportion of patients with sCTLA-4 > 200 pg/ml close to 70% (OR = 0.32, 95%CL = 0.06–1.73) and 80% (OR = 0.17, 95%CL = 0.04–0.68) lower (Table 3).
Correlation of baseline sCTLA-4 levels with occurrence of irAEs
We evaluated potential correlations between sCTLA-4 levels at baseline and the development of irAEs. Twenty-eight out of the 113 patients (24.8%) developed at least one irAE of any grade. These included cutaneous (n = 13; 11.5%), endocrine (n = 5; 4.4%) and digestive tract (n = 18; 15.9%) irAEs.
Increased levels of baseline sCTLA-4 were significantly associated with the development of any irAE. Indeed, the percentage of patients who developed irAEs among patients with sCTLA-4 > 200 pg/ml was about twice that observed among patients with sCTLA-4 ≤200 pg/ml (30.5% vs 16.4%; Table 4).
Table 4.
Association between sCTLA-4 serum levels and immune-related adverse events in IPI-treated MM patients
| Immune-related adverse events | sCTLA-4 levels | Total | OR | 95%CL | p value | |||
|---|---|---|---|---|---|---|---|---|
| ≤ 200 pg/ml | > 200 pg/ml | |||||||
| N | % | N | % | |||||
| Any | ||||||||
| No | 47 | 77.0 | 38 | 64.4 | 85 | 1.00 | (Ref.) | 0.029 |
| Yes | 10 | 16.4 | 18 | 30.5 | 28 | 3.63 | 1.14–11.5 | |
| Cutaneous | ||||||||
| No | 52 | 85.2 | 48 | 81.4 | 100 | 1.00 | (Ref.) | 0.140 |
| Yes | 5 | 8.2 | 8 | 13.6 | 13 | 3.26 | 0.68–15.6 | |
| Endocrine | ||||||||
| No | 55 | 90.2 | 53 | 89.8 | 108 | 1.00 | (Ref.) | 0.439 |
| Yes | 2 | 3.3 | 3 | 5.1 | 5 | 2.49 | 0.25–25.1 | |
| Digestive tract | ||||||||
| No | 51 | 83.6 | 44 | 74.6 | 95 | 1.00 | (Ref.) | 0.041 |
| Yes | 6 | 9.8 | 12 | 20.3 | 18 | 5.61 | 1.07–29.4 | |
| Whole sample | 61 | 100.0 | 59 | 100.0 | 113 | –s | – | – |
Association between sCTLA-4 serum levels (sCTLA-4 > 200 pg/ml vs sCTLA-4 ≤ 200 pg/ml) and immune-related adverse events was estimated through the binomial logistic regression modelling
IPI ipilimumab, OR odds ratio adjusted for age at 1st IPI cycle, gender, time from diagnosis, LDH levels, dNLR, pre-IPI immunotherapy, brain, liver and cutaneous metastases, and participating center; 95%CL 95% confidence limit, p value significance level of the likelihood ratio test Ref.: reference category
BLR analysis confirmed the results obtained in descriptive analysis. After adjusting for baseline characteristics, patients with sCTLA-4 > 200 pg/ml showed a more than threefold increased risk of developing any irAE compared to patients with sCTLA-4 ≤200 pg/ml (OR = 3.63; 95%CL = 1.14–11.5, p value = 0.029). Similar results were also found when site-specific irAEs were considered: cutaneous irAEs (OR = 3.26; 95%CL = 0.68–15.6, p value = 0.140), endocrine irAEs (OR = 2.49; 95%CL = 0.25–25.1, p value = 0.439) and digestive tract irAEs (OR = 5.61; 95%CL = 1.07–29.4, p value = 0.041) (Table 4).
Correlation of baseline sCTLA-4 levels with overall survival
We estimated overall survival probabilities through the Kaplan–Meier method. During the follow-up period (median = 7.3, range = 0.1–52.9 months) 99 (87.6%) out of the 113 patients deceased. Although patients with higher sCTLA-4 levels showed a better life expectancy above all during the first 2 years of observation, differences in survival were not statistically significant. A similar trend was observed also in the patient population deprived of the mucosal melanoma subgroup (Supplementary Table 2).
To take into account potential imbalances in baseline patient characteristics, a multivariate Cox regression analysis was applied to compare cumulative death rates in the two sCTLA-4 subgroups (> 200 pg/ml vs ≤ 200 pg/ml). MM patients with sCTLA-4 > 200 pg/ml experienced a statistically significant better prognosis showing a 40% lower risk of death (HR = 0.61, 95%CL = 0.39–0.98, p value = 0.039) as compared to patients with sCTLA-4 ≤200 pg/ml (Fig. 2).
Fig. 2.
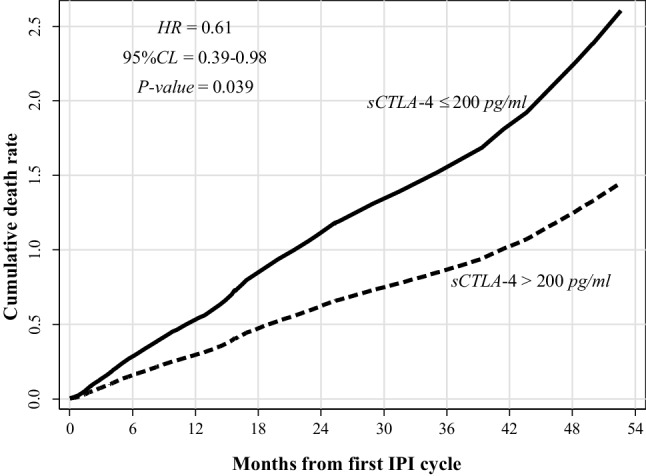
Time distribution of cumulative death rates. Time distribution has been evaluated according to sCTLA-4 levels (> 200 pg/ml vs ≤ 200 pg/ml) by Cox regression modelling adjusted for age, gender, ECOG, LDH levels, dNLR, brain and liver metastases, and participating centers. HR hazard ratio
Discussion
Although CTLA-4 blockade has significantly improved the survival of MM patients only a minority of them achieves long-term disease control. Therefore, there is an urgent need of biomarkers to identify patients who potentially could benefit from CTLA-4 blockade treatment.
In the present study, we investigated the possible role of serum sCTLA-4 levels as predictive biomarker of response, survival and irAE occurrence in MM patients treated with IPI therapy.
The potential of sCTLA-4 as a predictive biomarker in the context of MM has not been investigated so far except for one preliminary study in a small cohort of MM patients who received IPI therapy [30] suggesting that higher pre-treatment serum CTLA-4 levels can be linked to clinical benefit.
The present study, based on a larger cohort of MM patients, further demonstrated that patients with sCTLA-4 serum levels higher than the median value at baseline (200 pg/ml) had better outcomes in terms of both response to IPI and survival as compared to patients with lower sCTLA-4 serum levels (≤ 200 pg/ml). However, they were at higher risk of developing irAEs. The observation of this favorable effect on response and survival was maintained if mucosal patients were excluded from the study population (see Supplementary Tables 1 and 2).
In particular, MLR analysis pointed out a remarkably greater share of responsive (irCR + irPR) patients with sCTLA-4 > 200 pg/ml with respect to stable (irSD) and progressive (irPD) patients.
Cox analysis showed a significant death risk reduction of about 40% in patients with sCTLA-4 levels > 200 pg/ml as compared to patients with levels ≤ 200 pg/ml.
Interestingly, sCTLA-4 median value in MM patients was slightly lower than that found in the healthy controls, although not significantly. A reduced production of sCTLA-4 due to dysregulated T-cell activation in MM patients would probably leads to a poor competition with the membrane form flCTLA-4 on cytotoxic T cells, thus increasing T-cell downregulation. sCTLA-4 levels lower than that of HC have been found also in other tumors such as clear cell renal cell carcinoma [31] and colorectal cancer [32] which suggests a possible role of sCTLA-4 in promoting tumor immune tolerance.
The increased levels of sCTLA-4 expression that we here found in the IPI-responding MM patients might exhibit its effect in blocking the inhibitory function of flCTLA-4 and allow host cytotoxic T cells to attack the tumor cells, thereby enhancing the antitumor effect in synergy with IPI.
On the other hand, since sCTLA-4 could also inhibit T-cell costimulation by interfering with CD28/B7 ligand interaction on APC [11, 12], its role in preventing an adaptive anti-tumor immune response cannot be ruled out. However, we do not favor this hypothesis because of the association we observed between high sCTLA-4 levels and better BOR in our study population.
The analysis of the sera collected from the same patient at different time points during IPI therapy showed that the ability to produce circulating sCTLA4 increased with the number of IPI administrations. Indeed, as the number of IPI cycles increased, also the proportion of patients showing higher sCTLA-4 levels increased, whereas it decreased with the progression of disease.
The increase in sCTLA-4 serum levels along IPI therapy might reflect the activation status of T cells and thus a systemic response to the tumor antigens due to the blockade of CTLA-4/B7 interaction by means of IPI which potentiates T-cell costimulation.
sCTLA-4 found in patient serum may derive primarily from both effector Tconv and Treg circulating cells, although Tregs appear to be the predominant producers of sCTLA-4 [15]. However, sCTLA-4 may also be locally produced by melanoma cells and released directly into the blood. Indeed, we previously showed that melanoma cells are capable of expressing sCTLA-4 transcript and release sCTLA-4 in the culture supernatant [33].
Treatment with IPI antibody is typically associated with the onset of irAEs which are strongly linked to its immune-based mechanism of action. Previous studies have suggested that the presence of irAEs during IPI therapy may be associated with greater antitumor efficacy and clinical benefit [34]. However, conflicting results on this issue have also been reported [22].
We found a significant association between higher sCTLA-4 levels at baseline and the onset of any irAE, in particular irAEs of the digestive tract (mainly gastro-intestinal and hepatic events). Indeed, patients with sCTLA-4 > 200 pg/ml showed a more than fivefold increased risk of digestive tract irAEs as compared to patients with sCTLA-4 ≤200 pg/ml. This finding is not surprising given that increased levels of serum sCTLA-4 have been found in patients with inflammatory bowel disease (e.g., Chron’s disease) [35], ulcerative colitis [36], liver disease (e.g., chronic HBV infection) [37] and autoimmune pancreatitis [38], i.e., diseases with a pathogenesis related to the dysregulation of autoreactive T cells. In IPI-treated patients, high levels of sCTLA-4 which reflect an increased T-cell activation upon therapy might block interactions between flCTLA-4 expressed by autoreactive T cells, as well as Tregs, and B7 ligands and thereby enhance T-cell cytotoxicity and reduce Treg immunosuppressive function.
Moreover, in our cohort, stable and responsive patients showed a relative frequency of irAEs which was more thant 5-times higher than that in progressive patients (adjusted OR = 5.42, 95%CL = 1.15–19.4, p value < 0.001). It is worth noting that this finding is consistent with the association of higher sCTLA-4 levels with both better BOR and higher irAE frequency and strengthens the predictive role of sCTLA-4. Unfortunately, the sample size of our study did not allow to assess the association between sCTLA-4 levels and irAE grades given the very low frequency of patients presenting low (1/2) or high (3/4) grade. In addition, grade 1 and 2 adverse events are noticeably under-reported in Expanded Access Programs.
All these findings support a potentially important role of high sCTLA-4 levels in improving the outcome of IPI-treated patients as compared to other biomarkers such as the low LDH levels [39], or those factors that show evidence of a pre-treatment activated T-cell infiltrate such as the IFN-γ signature [40] and the high density of CD8, PD-1 and PD-L1 expressing cells at the tumor invasive margin [41] or peripheral blood factors including the high relative eosinophil count (REC) and relative lymphocyte count (RLC), low LDH and limited visceral metastases [42] in melanoma patients treated with PD-1 blockade.
Our data are in line with previous reports by our group [43, 44] and by others [45] showing a favorable prognostic role of high CTLA-4 expression levels in different tumor types. Indeed, we previously demonstrated association of a better OS with high CTLA-4 levels in pleural effusions as well as in tumor tissues from malignant mesothelioma [43] and NSCLC patients [44]. Similar results for sCTLA-4 were found also in patients with different types of cancers treated with radiotherapy, chemotherapy, and/or chemo-radiotherapy [14].
In conclusion, the present study evidenced a positive correlation between serum sCTLA-4 overexpression at baseline and clinical outcome of MM patients undergoing immunotherapy with ipilimumab, in terms of better response to IPI, higher frequency of irAEs and improved OS. Thus, CTLA-4 in its soluble isoform, might be used as a biomarker for predicting the efficacy of IPI in patients with MM although further investigations are needed to ascertain this hypothesis and to investigate the underlying molecular mechanisms.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
The authors would like to thank the patients and investigators who participated in the Italian Expanded Access Program (EAP). This work was supported by the Italian Melanoma Intergroup (IMI). The authors also thank the blood donors and staff of all centers, in particular the Transfusion Center of the IRCCS Ospedale Policlinico San Martino, Genoa, Italy, and the research nurse P. Peirano for collection of blood samples from melanoma patients.
Abbreviations
- ANC
Absolute neutrophil count
- BOR
Best overall response
- CTLA-4
Cytotoxic T lymphocyte antigen-4
- dALC
Derived lymphocyte count
- dNLR
Derived neutrophil–lymphocyte ratio
- EAP
Expanded access program
- flCTLA-4
Full-length CTLA-4
- HR
Hazard ratio
- IPI
Ipilimumab
- irAE
Immune-related adverse events
- irCR
Immune-related complete response
- irPD
Immune-related progressive disease
- irPR
Immune-related partial response
- irSD
Immune-related stable disease
- MLR
Multinomial logistic regression
- MM
Metastatic melanoma
- OR
Odds ratio
- sCTLA-4
Soluble CTLA-4
- SNV
Single nucleotide variants
- Tconv
Conventional T cells
- Treg
Regulatory T cells
Authors’ contributions
Study concept and design, and study supervision: MPP and Paola Queirolo. Recruitment and management of metastatic melanoma patients: Paola Queirolo, FF, LS, ET, PFF, EC, MG, FDG, GCAC, PM, Pietro Quaglino, PAA, ES, and FS. ELISA assay for detection of sCTLA-4: AM, SL, RC, and BB. SNV genotyping: AM, RC, BB, and MR. Acquisition, analysis, or interpretation of data: MPP, VF, AM, BD, MR, FS, and Paola Queirolo. Drafting of the manuscript: MPP, VF, BD, FS, and Paola Queirolo. Statistical analyses: VF and BD. Administrative, technical, or material support: AM, BB, PFF, CM, ST, EP, PF, SO-A, and MC. Critical revision of the manuscript for important intellectual content: MPP, VF, BD, PFF, MR, FS, and Paola Queirolo. All authors read and approved the final manuscript.
Funding
This work was supported by grants from the Italian Ministry of Health (5 × 1000 funds 2013 and 2014 to Pistillo), Italy. This work was supported by the Italian Melanoma Intergroup (IMI). The Expanded Access Program (EAP) was sponsored by Bristol-Myers Squibb.
Compliance with ethical standards
Conflict of interest
Queirolo is member of the advisory board and consultant of Roche, Novartis, Bristol-Myers Squibb, Merck Sharp & Dohme, Amgen. Ferrucci participated to Bristol-Myers Squibb, Novartis and Roche advisory boards, has served as consultant and received travel support from Bristol-Myers Squibb, Roche, Novartis, Merck Sharp & Dohme. Ascierto has/had a consultant/advisory role for Bristol-Myers Squibb, Roche-Genentech, Merck Sharp & Dohme, Novartis, Ventana, Amgen, Array. He received also research grants from Bristol-Myers Squibb, Roche-Genentech, Ventana, Array. All other authors have declared no conflict of interest. The Expanded Access Program (EAP) was sponsored by Bristol-Myers Squibb.
Ethical approval
Patients were recruited in six Italian centers. The study was approved by the local Ethics Committee (EC) of the Liguria Region (CE-IST OMA07.024 emended on 2 January 2011) and by the EC of each participating center. All procedures performed in the study were in accordance with the Helsinki declaration.
Informed consent
All patients provided signed informed consent before enrolment. Additional informed consent was obtained from healthy blood donors in compliance with the Institutional regulations.
References
- 1.Hodi FS, O’Day SJ, McDermott DF, Weber RW, Sosman JA, Haanen JB, et al. Improved survival with ipilimumab in patients with metastatic melanoma. N Engl J Med. 2010;363:711–723. doi: 10.1056/NEJMoa1003466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Robert C, Thomas L, Bondarenko I, O’Day S, Weber J, Garbe C, et al. Ipilimumab plus dacarbazine for previously untreated metastatic melanoma. N Engl J Med. 2011;364:2517–2526. doi: 10.1056/NEJMoa1104621. [DOI] [PubMed] [Google Scholar]
- 3.Schadendorf D, Hodi FS, Robert C, Weber JS, Margolin K, Hamid O, et al. Pooled analysis of long-term survival data from Phase II and Phase III trials of Ipilimumab in unresectable or metastatic melanoma. J Clin Oncol. 2015;33:1889–1894. doi: 10.1200/JCO.2014.56.2736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Peggs KS, Quezada SA, Korman AJ, Allison JP. Principles and use of anti-CTLA-4 antibody in human cancer immunotherapy. Curr Opin Immunol. 2006;18:206–231. doi: 10.1016/j.coi.2006.01.011. [DOI] [PubMed] [Google Scholar]
- 5.Tarhini AA, Edington H, Butterfield LH, Lin Y, Shuai Y, Tawbi H, et al. Immune monitoring of the circulation and the tumor microenvironment in patients with regionally advanced melanoma receiving neoadjuvant ipilimumab. PLoS One. 2014;9:e87705. doi: 10.1371/journal.pone.0087705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brunner MC, Chambers CA, Chan FK, Hanke J, Winoto A, Allison JP. CTLA-4-mediated inhibition of early events of T cell proliferation. J Immunol. 1999;162:5813–5820. [PubMed] [Google Scholar]
- 7.Walker LS, Sansom DM. The emerging role of CTLA4 as a cell-extrinsic regulator of T cell responses. Nat Rev Immunol. 2011;11:852–863. doi: 10.1038/nri3108. [DOI] [PubMed] [Google Scholar]
- 8.Walker SK, Sansom DM. Confusing signals: recent progress in CTLA-4 biology. Trends Immunol. 2015;36:63–70. doi: 10.1016/j.it.2014.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Oaks MK, Hallett KM. Cutting edge: a soluble form of CTLA-4 in patients with autoimmune thyroid disease. J Immunol. 2000;164:5015–5018. doi: 10.4049/jimmunol.164.10.5015. [DOI] [PubMed] [Google Scholar]
- 10.Magistrelli G, Jeannin P, Herbault N, Benoit De Coignac A, Gauchat JF, et al. A soluble form of CTLA-4 generated by alternative splicing is expressed by nonstimulated human T cells. Eur J Immunol. 1999;29:3596–3602. doi: 10.1002/(SICI)1521-4141(199911)29:11<3596::AID-IMMU3596>3.0.CO;2-Y. [DOI] [PubMed] [Google Scholar]
- 11.Simone R, Pesce G, Antola P, Rumbullaku M, Bagnasco M, Bizzaro N, Saverino D. The soluble form of CTLA-4 from serum of patients with autoimmune diseases regulates T-cell responses. Biomed Res Int. 2014;2014:215763. doi: 10.1155/2014/215763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Simone R, Tenca C, Fais F, Luciani M, De Rossi G, Pesce G, et al. A soluble form of CTLA-4 is present in paediatric patients with acute lymphoblastic leukaemia and correlates with CD1d + expression. PLoS One. 2012;7:e44654. doi: 10.1371/journal.pone.0044654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Erfani N, Razmkhah M, Ghaderi A. Circulating soluble CTLA4 (sCTLA4) is elevated in patients with breast cancer. Cancer Invest. 2010;28:828–832. doi: 10.3109/07357901003630934. [DOI] [PubMed] [Google Scholar]
- 14.Liu Q, Hu P, Deng G, Zhang J, Liang N, Xie J, et al. Soluble cytotoxic T-lymphocyte antigen 4: a favorable predictor in malignant tumors after therapy. Onco Targets Ther. 2017;10:2147–2154. doi: 10.2147/OTT.S128451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ward FJ, Dahal LN, Wijesekera SK, Abdul-Jawad SK, Kaewarpai T, Xu H, et al. The soluble isoform of CTLA-4 as a regulator of T-cell responses. Eur J Immunol. 2013;43:1274–1285. doi: 10.1002/eji.201242529. [DOI] [PubMed] [Google Scholar]
- 16.Rydén A, Bolmeson C, Jonson CO, Cilio CM, Faresjö M. Low expression and secretion of circulating soluble CTLA-4 in peripheral blood mononuclear cells and sera from type 1 diabetic children. Diabetes Metab Res Rev. 2012;28:84–96. doi: 10.1002/dmrr.1286. [DOI] [PubMed] [Google Scholar]
- 17.Sato S, Fujimoto M, Hasegawa M, Komura K, Yanaba K, Hayakawa I. Serum soluble CTLA-4 levels are increased in diffuse cutaneous systemic sclerosis. Rheumatology. 2004;43:1261–1266. doi: 10.1093/rheumatology/keh303. [DOI] [PubMed] [Google Scholar]
- 18.Zaragoza J, Caille A, Beneton N, Bens G, Christiann F, Maillard H, Machet L. High neutrophil to lymphocyte ratio measured before starting ipilimumab treatment is associated with reduced overall survival in patients with melanoma. Br J Dermatol. 2016;174:146–151. doi: 10.1111/bjd.14155. [DOI] [PubMed] [Google Scholar]
- 19.Seremet T, Koch A, Jansen Y, Schreuer M, Wilgenhof S, Del Marmol VJ, et al. Molecular and epigenetic features of melanomas and tumor immune microenvironment linked to durable remission to ipilimumab-based immunotherapy in metastatic patients. J Transl Med. 2016;14(1):232. doi: 10.1186/s12967-016-0990-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Queirolo P, Dozin B, Morabito A, Banelli B, Piccioli P, Fava C, et al. Association of CTLA-4 gene variants with response to therapy and long-term survival in metastatic melanoma patients treated with ipilimumab: an Italian melanoma intergroup study. Front Immunol. 2017;8:386. doi: 10.3389/fimmu.2017.00386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Queirolo P, Dozin B, Morabito A, Banelli B, Carosio R, Fontana V, et al. CTLA-4 gene variant—1661A > G may predict the onset of endocrine adverse events in metastatic melanoma patients treated with ipilimumab. Eur J Cancer. 2018;97:59–61. doi: 10.1016/j.ejca.2018.04.005. [DOI] [PubMed] [Google Scholar]
- 22.Ascierto PA, Simeone E, Sileni VC, Pigozzo J, Maio M, Altomonte M, et al. Clinical experience with ipilimumab 3 mg/kg: real-world efficacy and safety data from an expanded access program cohort. J Transl Med. 2014;12:116. doi: 10.1186/1479-5876-12-116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wolchok JD, Hoos A, O’Day S, Weber JS, Hamid O, Lebbé C, et al. Guidelines for the evaluation of immune therapy activity in solid tumors: immune-related response criteria. Clin Cancer Res. 2009;15:7412–7420. doi: 10.1158/1078-0432.CCR-09-1624. [DOI] [PubMed] [Google Scholar]
- 24. National Cancer Institute (2006) Common terminology criteria for adverse events v3.0 (CTCAE). http://ctep.cancer.gov/protocolDevelopment/electronic_applications/docs/ctcaev3.pdf. Accessed 30 Dec 2015
- 25.Ferrucci PF, Ascierto PA, Pigozzo J, Del Vecchio M, Maio M, Antonini Cappellini GC, et al. Baseline neutrophils and derived neutrophil-to-lymphocyte ratio: prognostic relevance in metastatic melanoma patients receiving ipilimumab. Ann Oncol. 2016;27:732–738. doi: 10.1093/annonc/mdw016. [DOI] [PubMed] [Google Scholar]
- 26.Proctor MJ, McMillan DC, Morrison DS, Fletcher CD, Horgan PG, Clarke SJ. A derived neutrophil to lymphocyte ratio predicts survival in patients with cancer. Br J Cancer. 2012;107:695–699. doi: 10.1038/bjc.2012.292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kleinbaum DG, Klein M. Logistic regression. 3. New York: Springer; 2010. [Google Scholar]
- 28.Kleinbaum DG, Klein M. Survival analysis. 2. New York: Springer; 2005. [Google Scholar]
- 29.Ueda H, Howson JM, Esposito L, Heward J, Snook H, Chamberlain G, et al. Association of the T-cell regulatory gene CTLA4 with susceptibility to autoimmune disease. Nature. 2003;423:506–511. doi: 10.1038/nature01621. [DOI] [PubMed] [Google Scholar]
- 30.Leung AM, Lee AF, Ozao-Choy J, Ramos RI, Hamid O, O’Day SJ, et al. Clinical benefit from ipilimumab therapy in melanoma patients may be associated with serum CTLA4 levels. Front Oncol. 2014;4:110. doi: 10.3389/fonc.2014.00110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Masuda A, Arai K, Nishihara D, Mizuno T, Yuki H, Kambara T, et al. Clinical significance of serum soluble T cell regulatory molecules in clear cell renal cell carcinoma. Biomed Res Int. 2014;2014:396064. doi: 10.1155/2014/396064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kucukhuseyin O, Turan S, Yanar K, Arikan S, Duzkoylu Y, Aydin S, et al. Individual and combined effects of CTLA4-cd28 variants and oxidant-antioxidant status on the development of colorectal cancer. Anticancer Res. 2015;35:5391–5400. [PubMed] [Google Scholar]
- 33.Laurent S, Queirolo P, Boero S, Salvi S, Piccioli P, Boccardo S, et al. The engagement of CTLA-4 on primary melanoma cell lines induces antibody-dependent cellular cytotoxicity and TNF-α production. J Transl Med. 2013;11:108. doi: 10.1186/1479-5876-11-108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Weber JS, Kähler KC, Hauschild A. Management of immune-related adverse events and kinetics of response with ipilimumab. J Clin Oncol. 2012;30:2691–2697. doi: 10.1200/JCO.2012.41.6750. [DOI] [PubMed] [Google Scholar]
- 35.Chen Z, Zhou F, Huang S, Jiang T, Chen L, Ge L, Xia B. Association of cytotoxic T lymphocyte associated antigen-4 gene (rs60872763) polymorphism with Crohn’s disease and high levels of serum sCTLA-4 in Crohn’s disease. J Gastroenterol Hepatol. 2011;26:924–930. doi: 10.1111/j.1440-1746.2011.06662.x. [DOI] [PubMed] [Google Scholar]
- 36.Jiang T, Ge LQ, Chen ZT, Li C, Zhou F, Luo Y, Xia B. Effect of cytotoxic T lymphocyte-associated molecule 4 1661 gene polymorphism on its expression and transcription in ulcerative colitis. J Dig Dis. 2010;11:369–375. doi: 10.1111/j.1751-2980.2010.00462.x. [DOI] [PubMed] [Google Scholar]
- 37.Cao J, Zhang L, Huang S, Chen P, Zou L, Chen H, et al. Aberrant production of soluble co-stimulatory molecules CTLA-4 and CD28 in patients with chronic hepatitis B. Microb Pathog. 2011;51:262–267. doi: 10.1016/j.micpath.2011.06.003. [DOI] [PubMed] [Google Scholar]
- 38.Umemura T, Ota M, Hamano H, Katsuyama Y, Muraki T, Arakura N, et al. Association of autoimmune pancreatitis with cytotoxic T-lymphocyte antigen 4 gene polymorphisms in Japanese patients. Am J Gastroenterol. 2008;103:588–594. doi: 10.1111/j.1572-0241.2007.01750.x. [DOI] [PubMed] [Google Scholar]
- 39.Kelderman S, Heemskerk B, van Tinteren H, van den Brom RR, Hospers GA, van den Eertwegh AJ, et al. Lactate dehydrogenase as a selection criterion for ipilimumab treatment in metastatic melanoma. Cancer Immunol Immunother. 2014;63:449–458. doi: 10.1007/s00262-014-1528-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ayers M, Lunceford J, Nebozhyn M, Murphy E, Loboda A, Kaufman DR, et al. IFN-γ-related mRNA profile predicts clinical response to PD-1 blockade. J Clin Invest. 2017;127:2930–2940. doi: 10.1172/JCI91190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Tumeh PC, Harview CL, Yearley JH, Shintaku IP, Taylor EJ, Robert L, et al. PD-1 blockade induces responses by inhibiting adaptive immune resistance. Nature. 2014;515:568–571. doi: 10.1038/nature13954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Weide B, Martens A, Hassel JC, Berking C, Postow MA, Bisschop K, et al. Baseline biomarkers for outcome of melanoma patients treated with pembrolizumab. Clin Cancer Res. 2016;22:5487–5496. doi: 10.1158/1078-0432.CCR-16-0127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Roncella S, Laurent S, Fontana V, Ferro P, Franceschini MC, Salvi S, et al. CTLA-4 in mesothelioma patients: tissue expression, body fluid levels and possible relevance as a prognostic factor. Cancer Immunol Immunother. 2016;65:909–917. doi: 10.1007/s00262-016-1844-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Salvi S, Fontana V, Boccardo S, Merlo DF, Margallo E, Laurent S, Morabito A, et al. Evaluation of CTLA-4 expression and relevance as a novel prognostic factor in patients with non-small cell lung cancer. Cancer Immunol Immunother. 2012;61:1463–1472. doi: 10.1007/s00262-012-1211-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hu P, Liu Q, Deng G, Zhang J, Liang N, Xie J, Zhang J. The prognostic value of cytotoxic T-lymphocyte antigen 4 in cancers: a systematic review and meta-analysis. Sci Rep. 2017;7:42913. doi: 10.1038/srep42913. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


