Abstract
In recent years, immune cells were shown to play critical roles in tumor growth and metastatic progression. In this context, neutrophils were shown to possess both pro- and anti-tumor properties. To exert their anti-tumor effect, neutrophils need to migrate towards, and form physical contact with tumor cells. Neutrophils secrete H2O2 in a contact-dependent mechanism, thereby inducing a lethal Ca2+ influx via the activation of the H2O2-dependent TRPM2 Ca2+ channel. Here, we explored the mechanism regulating neutrophil chemoattraction to tumor cells. Interestingly, we found that TRPM2 plays a role in this context as well, since it regulates the expression of potent neutrophil chemoattractants. Consequently, cells expressing reduced levels of TRPM2 are not approached by neutrophils. Together, these observations demonstrate how tumor cells expressing reduced levels of TRPM2 evade neutrophil cytotoxicity in two interrelated mechanisms—downregulation of neutrophil chemoattractants and blocking of the apoptotic Ca2+-dependent cascade. These observations demonstrate a critical role for TRPM2 in neutrophil-mediated immunosurveillance and identify cells expressing low levels of TRPM2, as a potential target for cancer therapy.
Electronic supplementary material
The online version of this article (10.1007/s00262-018-2249-2) contains supplementary material, which is available to authorized users.
Keywords: Neutrophils, TRPM2, CXCL2, Immune evasion
Introduction
Traditionally, cancer research focused on understanding the biology of tumor cells in search of potential therapeutic targets. However, in the past decade, it has become apparent that various aspects of cancer biology are dictated by the non-malignant cells present in the tumor microenvironment. The tumor microenvironment consists of various cell types and is highly populated with immune cells [1]. Although the immune system has the capacity to fight malignant cells, it ultimately fails. During tumorigenesis, tumor cells undergo intensive selection to express genes that allow survival in an otherwise immune cell-rich hostile environment. Characterization of the key genes mediating immune evasion is critical for the development of novel therapeutic approaches. This is exemplified by the characterization of immune checkpoints, which has led to the development of the highly efficient immune checkpoint inhibitor therapies.
Neutrophils, the most abundant type of white blood cells in the human circulation, are known for their role in inflammation and in fighting infections [2]. In cancer, neutrophils were widely described for their pro-tumor properties [3–8] and are considered a poor prognostic marker [9]. In this respect, neutrophils were shown to promote tumor growth and metastatic progression by modulating tumor angiogenesis [5, 10], production of tumor supporting chemokines [6, 11], modulating immune responses [7, 12], mediating immune evasion [8, 10, 13], and directly promoting metastatic seeding [14, 15]. In contrast, we and others have shown that neutrophils have an important role in limiting tumor progression and metastatic seeding via direct cytotoxicity [16–18]. Neutrophils were shown to have the capacity to directly eliminate tumor cells both at the primary site and at the premetastatic site and that their recruitment is dependent on c-MET tyrosine kinase receptor [17–19]. In addition, neutrophils were shown to have the capacity to enhance anti-tumor innate immune responses. While these observations attribute conflicting roles to neutrophils, they actually stem from the existence of distinct neutrophil subpopulations that may either promote or inhibit tumor growth and progression [20].
To exert their cytotoxic effect, neutrophils need to reach tumor cells, identify them as a target for elimination, and induce a lethal apoptotic sequence. Recently [21, 22], we demonstrated that the lethal apoptotic sequence is mediated by transient receptor potential melastatin 2 (TRPM2), a ubiquitously expressed H2O2-dependent Ca2+-permeable channel [23–26]. However, the mechanisms regulating the events preceding tumor cell killing via TRPM2 activation, i.e., neutrophil chemoattraction and tumor cell recognition, remain unknown.
Our study shows the critical role played by TRPM2 in neutrophil cytotoxicity. Moreover, this channel was also found to be important for cytokine production [27] and neutrophil migration towards monocytes [28] and endothelial cells [29]. We, therefore, assessed the consequences of modulating TRPM2 expression in tumor cells on neutrophil chemoattraction. We show that reduced TRPM2 levels downregulate CXCL2 expression in tumor cells. CXCL2 is a key ligand for CXCR2 which is critical for neutrophil recruitment to tumors [30, 31]. Accordingly, low levels of CXCL2 impair neutrophil migration towards tumor cells and prevent the formation of physical contact, a critical neutrophil cytotoxicity checkpoint. Altogether, these findings identify a dual role for TRPM2 in regulating neutrophil cytotoxicity—promoting neutrophil attraction via CXCL2 expression and initiating the apoptotic cascade by mediating Ca2+ influx in response to H2O2 [32].
Materials and methods
Mice
5–6-week-old female BALB/c mice were used in all in vivo experiments. Mice were housed in a specific pathogen-free colony at a constant room temperature with a 12 h light/dark cycle, and provided with food and water ad libitum.
Cell lines
4T1 and AT3 mouse breast tumor cells and Lewis Lung Carcinoma cells (LLC) were cultured in DMEM containing 10% heat-inactivated fetal calf serum (FCS). TRPM2kd 4T1 cells were generated as previously described [30]. Control cells were transduced an empty vector (pLKO). TRPM2kd cells with CXCL2 overexpression were generated by retroviral transduction with CXCL2-MigR1 plasmid.
Neutrophil purification
Circulating NDN were purified as previously described [30].
Neutrophil-tumor cell co-culture
Trypan blue exclusion assay: 104 tumor cells were co-cultured with 105 NDN (1:10 ratio) in a transparent 96-well plate. Following 8 h of incubation, Trypan blue staining was used to quantify tumor cells death. Each well was visually assessed, and Trypan blue positive and negative cells were counted.
The in vitro killing assay was performed as previously described [30].
Antibodies
Rat α-Mouse CXCL2 (R&D, MAB542).
Plasmids
Retroviral MigR1-CXCL2 vector: the open-reading frame of mouse CXCL2 (NM_009140.2) was prepared from cDNA of 4T1 breast cancer cells using forward primer 5′-CAGTCCGCTCGAGGCCGCCACCATGGCCCCTCCCACCTGCCGGCTCC-3′ containing an XhoI restriction site, Kozac sequence followed by the ATG initiation code and reverse primer 5′-ACTTCCGGAATTCTCAGTTAGCCTTGCCTTTGTTCAG-3′ containing an EcoRI restriction site and the stop codon. The amplified CXCL2 PCR product was digested by XhoI and EcoRI (New England BioLabs) and inserted into MigR1 (retroviral vector containing IRES-GFP) plasmid kindly provided by Prof. Warren Pear, Philadelphia. Retroviral MigR1-Luc vector for functional killing assay was prepared as described before [33].
Migration assay
4T1 cells were seeded and incubated overnight. Supernatant was transferred to the bottom chamber of a Millicell®24 migration plate (Merck Millipore, 5 µm). Isolated NDN were added to the top chamber and incubated for 30 min at 37 °C. Following incubation, the top chamber was removed and the number of migrated neutrophils was counted using the Image J.
Holomonitor imaging
2 × 105 TRPM2wt, TRPM2kd, or TRPM2kd-CXCL2 o.e. 4T1 cells were plated on 35 mm tissue culture plates. Following 24 h of incubation, 2 × 106 NDN were added to the tumor cell culture and were monitored using the Holomonitor M4 imaging system for 24 h. The first 9 h of co-culture were taken for analysis using the HolostudioTM software. The analysis includes two parameters: (1) migration—the shortest distance between the starting point of cell analysis and the end point; (2) motility—how far the cells had moved from their starting point at the beginning of the analysis until the end point. All movements were taken into account, including cells which had moved in a random direction.
qPCR
Total RNA was isolated with TRI-Reagent (Sigma) and cDNA was made using AB high-capacity cDNA kit (Applied Biosystems) according to the manufacturer’s instructions. Real-time PCR analyses were done using the Sybr-Green Master Mix and CFX384 BioRad. The following primer sequences were used for mouse gene expression analyses: GAPDH-F—5′-GCCTTCCGTGTTCCTACC-3′, GAPDH-R—5′-CCTGCTTCACCACCTTCTT-3′, CXCL1-F—5′-GCTGGGATTCACCTCAAGAA-3′, CXCL1-R—5′-TGTGGCTATGACTTCGGTTTG-3′, CXCL2-F—5′-GAACAAAGGCAAGGCTAACTG-3′, CXCL2-F—5′-GAACAAAGGCAAGGCTAACTG-3′, CXCL2-R—5′-AACATAACAACATCTGGGCAAT-3′, CXCL5-F—5′-AAAAACCAGAAGGAGGTCTGTC-3′, CXCL5-R—5′-GAACACTGGCCGTTCTTTC-3′, TRPM2-F—5′-GACCCAAGGAACACAGACAA-3′, TRPM2-R—5′-AGCCTCTTCAGCTCCATATCA-3′.
Selection with H2O2
4T1 cell selection with H2O2 was performed as previously described [30].
CXCL2 expression and secretion
To assess CXCL2 levels in tumor cells in TRPM2kd, we seeded 2 × 105 control and TRPM2kd tumor cells in 6-well plates. Following overnight incubation, the amount of CXCL2 in the supernatant of 4T1 control or 4T1 shRNA to TRPM2 cells growth medium was analyzed using the Murine MIP-2 ELISA Development Kit (Peprotech, 900-M152) according to the manufacturer’s instructions. The enzymatic activity was measured by high-sensitivity TMB substrate solution (GenDEPOT) and the intensity of converted TMB was measured after 15 min at 650 nm using the Tecan Plate-Reader. In addition, the cells were washed and analyzed by qPCR to evaluate CXCL2 mRNA expression. As neutrophils have the ability to produce and secrete CXCL2, both of these experiments were done in the absence of neutrophils.
Statistical analysis
For studies comparing differences between two groups, we used unpaired Student’s t tests. Differences were considered significant when p < 0.05. Data are presented as mean ± SEM.
Results
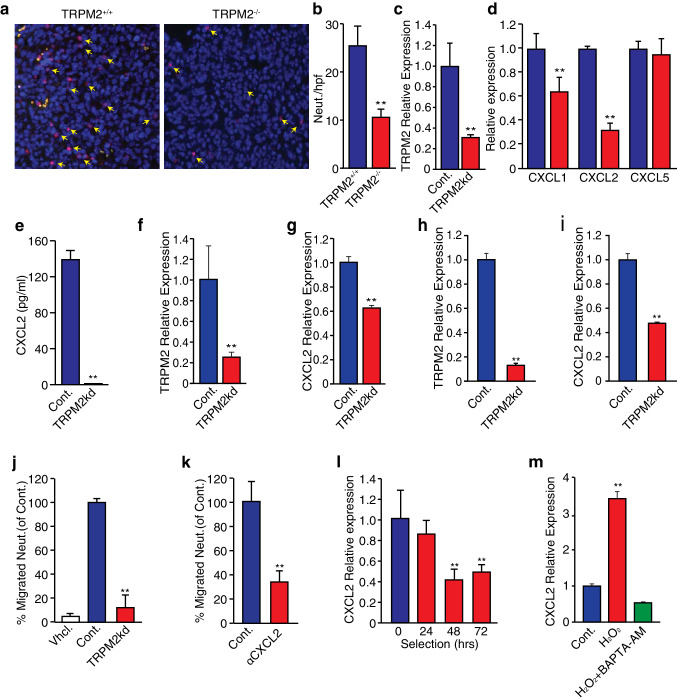
Tumor cell-expressed TRPM2 regulates neutrophil chemoattraction via CXCL2
We have previously shown that tumor-secreted factors can induce a cytotoxic phenotype in circulating neutrophils [17]. In a recent study, we explored the mechanism used by neutrophils to kill tumor cells and identified a critical role of TRPM2, an H2O2-dependent Ca2+ channel. We showed that downregulation of TRPM2 expression in tumor cells blocks neutrophil cytotoxicity, providing these cells with an increased metastatic capacity. To study the consequences of TRPM2 loss on tumor growth and metastatic progression we generated TRPM2 knockout (TRPM2−/−) 4T1 tumor cells using CRISPR technology [21]. We found that TRPM2−/− primary tumors show growth retardation compared with TRPM2+/+ tumors. However, TRPM2−/− tumors were more metastatic due to their inherent resistance to neutrophil cytotoxicity at the premetastatic lung [21]. Histological examination of neutrophils at the primary tumor showed a dramatic reduction in neutrophil recruitment to the TRPM2−/− tumors compared with TRPM2+/+ tumors (Fig. 1a, b). This observation suggests that neutrophil chemoattraction towards tumor cells is TRPM2-dependent. To examine this possibility, we assessed the expression level of potential neutrophil chemoattractants in control and TRPM2 knockdown (TRPM2kd) 4T1 cells generated using TRPM2-specific shRNAs (Fig. 1c) [21]. Specifically, we examined the expression levels of CXCL1, CXCL2, and CXCL5, in control and TRPM2kd cells (Fig. 1d). We found no significant difference in the expression level of CXCL5 (Fig. 1d). In contrast, we found a reduction in CXCL1 expression and a more dramatic reduction in CXCL2 expression (Fig. 1d). The previous studies have demonstrated a link between TRPM2 and the expression of CXCL2 [28, 29]. We therefore focused on the more robust effect of TRPM2kd on CXCL2 expression and used ELISA to quantify CXCL2 secretion. We found that CXCL2 secretion was virtually abolished in TRPM2kd cells corroborating the qPCR observations (Fig. 1e). Similarly, knocking down TRPM2 leads to reduced expression CXCL2 in both AT3 (Fig. 1f, g) and LLC cells (Fig. 1h, i) providing a wider scope for this observation.
Fig. 1.
TRPM2 affects CXCL2 expression and neutrophil chemoattraction. a Representative IHC staining of Ly6G+ neutrophils (red, arrows) in 4T1 TRPM2−/− and TRPM+/+ tumors (n = 5). b Number of neutrophils per 4T1 TRPM2−/− and TRPM+/+ tumors area. c Relative expression of TRPM2 in control and TRPM2kd 4T1 cells. d Relative expression of CXCL1, CXCL2 and CXCL5 in control and TRPM2kd 4T1 cells. e CXCL2 secretion by control and TRPM2kd cells. Relative expression of TRPM2 (f) and CXCL2 (g) in control and TRPM2kd AT3 cells. Relative expression of TRPM2 (h) and CXCL2 (i) in control and TRPM2kd LLC cells. j Neutrophil migration towards vehicle and media conditioned by control or TRPM2kd cells. k Neutrophil migration in the absence (Cont.) or presence of CXCL2 neutralizing antibody (αCXCL2). l Relative expression of CXCL2 in tumor cells selected with H2O2. m Relative expression of CXCL2 in control, H2O2 treated and H2O2 + BAPTA-AM treated 4T1 cells. These experiments were repeated at least three times with similar results. Statistical significance was determined using unpaired student’s t test. *p < 0.05, **p < 0.01
To test the functional consequence of TRPM2kd on neutrophil chemotaxis, we isolated circulating neutrophils from 4T1 tumor bearing mice and tested their migration in a Boyden chamber assay. As expected, neutrophil chemotaxis towards medium conditioned by TRPM2kd cells was dramatically reduced compared to that of control cells (Fig. 1j). This observation demonstrated that TRPM2 loss in tumor cells results in impaired neutrophil chemoattraction. However, neutrophils may be attracted by factors other than CXCL2 [2]. To conclusively determine the role played by CXCL2 in attracting neutrophils to tumor cells in this context, we treated tumor cell conditioned media with a CXCL2 neutralizing antibody. We showed that blocking CXCL2 has a profound effect on neutrophil chemoattraction, demonstrating that CXCL2 is a critical chemoattractant in this context (Fig. 1k). We have previously shown that challenging tumor cells with H2O2 selects for H2O2-resistant TRPM2low tumor cells [21]. qPCR analysis on CXCL2 expression in H2O2-selected cells showed the progressive reduction in CXCL2 expression and provided further evidence for the correlation between TRPM2 and CXCL2 expression (Fig. 1l). Collectively, these observations suggest that CXCL2 expression might be dependent on TRPM2 mediated Ca2+ signaling. To test this hypothesis, we evaluated the consequences of Ca2+ chelation on the induction of CXCL2 expression by H2O2 [28]. Corroborating the previous studies, we show that H2O2 induces a dramatic increase in CXCL2 expression (Fig. 1m). However, this increase is completely blocked in the presence of BAPTA-AM, indicating that Ca2+ is indispensible for the induction of CXCL2 expression (Fig. 1m).
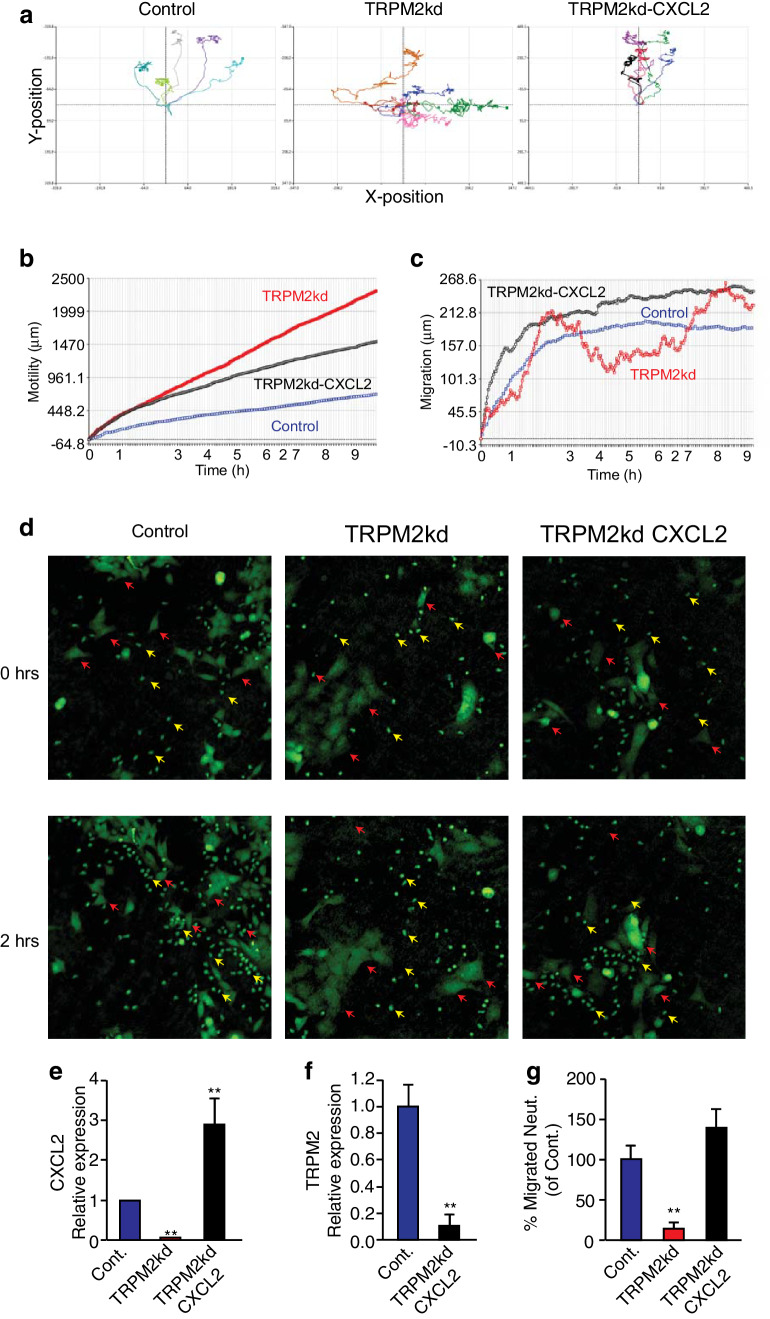
Overexpression of CXCL2 in TRPM2kd cells rescues neutrophil chemoattraction
Next, we used time-lapse microscopy to examine the consequences of reduced TRPM2 expression in tumor cells on neutrophil migration. As expected, neutrophils migrated towards control cells with high efficiency, i.e., taking a short path towards the cells and arriving within minutes. Importantly, once neutrophils reached tumor cells, they paused and persisted in their vicinity (Fig. 2a left panel, b, c). This may also be appreciated visually, as following 2 h of co-culture, most of the neutrophils were seen either attached or in close proximity to the tumor cells (Fig. 2d, left panel, Supplementary video 1 part 1). Using the same methodology to assess neutrophil migration towards TRPM2kd cells, we noted a very different pattern. Neutrophils in culture with TRPM2kd cells demonstrated more of a Brownian motion (Fig. 2a, middle panel) and took a significantly longer path to reach the tumor cells (Fig. 2b, c). Unlike neutrophils co-cultured with control tumor cells, neutrophils cultured with TRPM2kd cells were randomly distributed and did not accumulate in the vicinity of the tumor cells (Fig. 2d, middle panel, Supplementary video 1 part 2). As reduced CXCL2 expression in TRPM2kd cells may explain neutrophils’ poor migration, we tested whether CXCL2 overexpression in TRPM2kd cells can rescue the migration phenotype. Importantly, overexpression of CXCL2 in TRPM2kd cells (Fig. 2e) did not upregulate TRPM2 expression, suggesting that TRPM2 is hierarchally upstream from CXCL2 (Fig. 2f). CXCL2 overexpression in TRPM2kd cells rescued the migration phenotype in a Boyden chamber assay (Fig. 2g). Moreover, CXCL2 overexpression in TRPM2kd cells restored the migration towards tumor cells (Fig. 2a, right panel, b, c) and neutrophils’ ability to reach TRPM2kd cells quickly (Fig. 2d, Supplementary video 1 part 3) and via a short path (Fig. 2a, right panel, b, c).
Fig. 2.
CXCL2 overexpression in TRPM2kd 4T1 cells restores neutrophil chemoattraction. a Migration plots of five random neutrophils towards control (left), TRPM2kd (middle), and CXCL2-overexpressing TRPM2kd 4T1 cells (right). b Cumulative distance neutrophils travel when co-cultured with control, TRPM2kd or CXCL2 overexpressing TRPM2kd 4T1 cells (n = 10). c Absolute distance neutrophils migrated from their initial position when cultured with control, TRPM2kd, or CXCL2 overexpressing TRPM2kd 4T1 cells (n = 10). d Localization of neutrophils (smaller cells, yellow arrows) when cultured with control, TRPM2kd, or CXCL2 overexpressing TRPM2kd cells (larger cells, red arrows) at time 0 and at 2 h. e Relative expression of CXCL2 in control, TRPM2kd, and CXCL2 overexpressing TRPM2kd (TRPM2kd–CXCL2) 4T1 cells. f Relative expression of TRPM2 in control and CXCL2 overexpressing TRPM2kd 4T1 cells. g Neutrophil chemotaxis towards media conditioned by control, TRPM2kd and CXCL2 overexpressing TRPM2kd 4T1 cells. Results represent the average of ten representative cells. These experiments were repeated three times with similar results. Statistical significance was determined using unpaired student’s t test. *p < 0.05, **p < 0.01
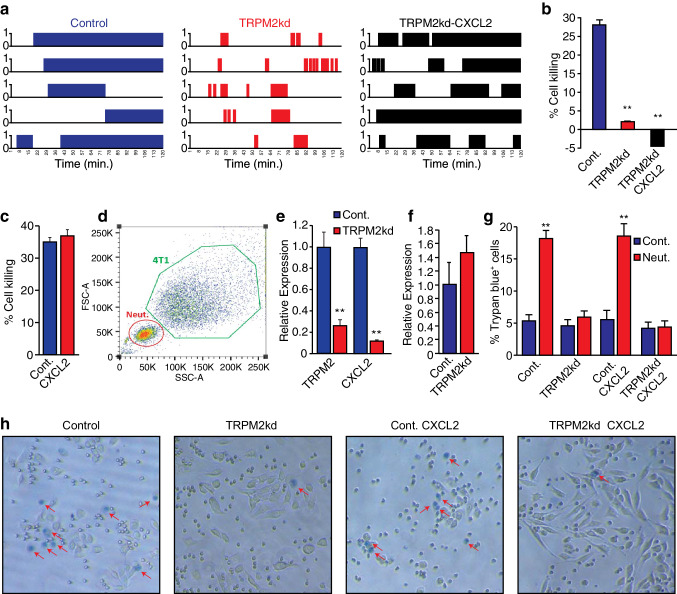
CXCL2 overexpression does not render TRPM2kd cells susceptible to neutrophil cytotoxicity
The observations above, together with the notion that physical contact is required for neutrophil cytotoxicity [17], highlight the critical role played by CXCL2 in mediating the chemoattraction of neutrophils towards tumor cells. However, we have recently shown that TRPM2 is important for neutrophil cytotoxicity as it mediates a Ca2+ influx that leads to tumor cell death. We therefore questioned whether TRPM2kd cells are neutrophil-resistant due to intrinsic resistance or due to impaired neutrophil attraction. To conclusively determine the role TRPM2 plays in neutrophil cytotoxicity, we tested whether TRPM2kd cells overexpressing CXCL2 remain neutrophil-resistant or become susceptible to neutrophil cytotoxicity. As physical contact is a critical factor in neutrophil cytotoxicity, we first tested if CXCL2 overexpression restores neutrophil-tumor cell contact. Using time-lapse microscopy, we observed that, while neutrophils formed prolonged physical contact with control tumor cells, they interacted only briefly with TRPM2kd cells (Fig. 3a, compare left and middle panels). CXCL2 overexpression restored the prolonged interaction between neutrophils and tumor cells (Fig. 3a, compare middle and right panels). Notably, even though neutrophils were attracted to and formed prolonged interaction with TRPM2kd cells overexpressing CXCL2, CXCL2-overexpressing TRPM2kd cells remained neutrophil-resistant (Fig. 3b). This suggests that TRPM2 plays a role in regulating both neutrophil attraction via CXCL2 and in mediating the lethal Ca2+ influx in response to H2O2. We then tested whether CXCL2 expression is a limiting factor in neutrophils’ capacity to kill tumor cells. To test this, we generated CXCL2 overexpressing 4T1 cells and compared their susceptibility to neutrophil cytotoxicity to that of control cells. Our data show that there is no significant difference between control and CXCL2 overexpressing tumor cells with regard to their susceptibility to neutrophil cytotoxicity (Fig. 3c). Next, we tested whether the presence of neutrophils in the co-culture affects CXCL2 expression in control and TRPM2kd cells. To this end, we sorted control and TRPM2kd cells following overnight co-culture with neutrophils (Fig. 3d). We then used qPCR to assess the expression of CXCL2 in the sorted tumor cells. Our data show that TRPM2kd cells maintain the reduced levels of both TRPM2 and CXCL2 compared with control cells following the co-culture with neutrophil (Fig. 3e). Notably, neutrophils co-cultured with TRPM2kd cells express higher, albeit not statistically significant, levels of CXCL2 compared with neutrophils cultured with control cells (Fig. 3f). Importantly, we repeated the co-culture experiments using a non-redundant approach and obtained similar results (Fig. 3g, h). Collectively, our data show that TRPM2 regulates neutrophil chemoattraction to tumor cells by modulating CXCL2 expression in tumor cells, a critical component in the cascade of events required for neutrophil cytotoxicity.
Fig. 3.
TRPM2 expression in tumor cells is crucial for neutrophils cytotoxicity. a Graphic representation of the interaction between control, TRPM2kd, or CXCL2 overexpressing TRPM2kd 4T1 cells and neutrophils where 1 represents physical contact and 0 represents no contact (n = 5). b Neutrophil cytotoxicity towards control, TRPM2kd, and CXCL2 overexpressing TRPM2kd 4T1 cells. c Extent of neutrophil cytotoxicity towards control (Cont.) and CXCL2 overexpressing (CXCL2) 4T1 tumor cells. d Representative FACS strategy showing FSC and SSC of neutrophil-tumor cell co-culture used for sorting out tumor cells. e Relative expression of TRPM2 and CXCL2 in sorted Control (Cont.) and TRPM2kd (TRPM2kd) tumor cells following co-culture with neutrophils. f CXCL2 expression in neutrophils cultured with control (Cont.) and TRPM2kd (TRPM2kd) 4T1 cells. g Cell death (% Trypan blue+ cells) in control, TRPM2kd, CXCL2 overexpressing control, and CXCL2 overexpressing TRPM2kd cells culture alone (Cont.) or in co-culture with neutrophils (Neut.). h Representative images of Trypan blue staining of control, TRPM2kd, CXCL2 overexpressing control, and CXCL2 overexpressing TRPM2kd cells following 8 h of co-culture with neutrophils (red arrows indicate Trypan blue+ cells). *p < 0.05, **p < 0.01
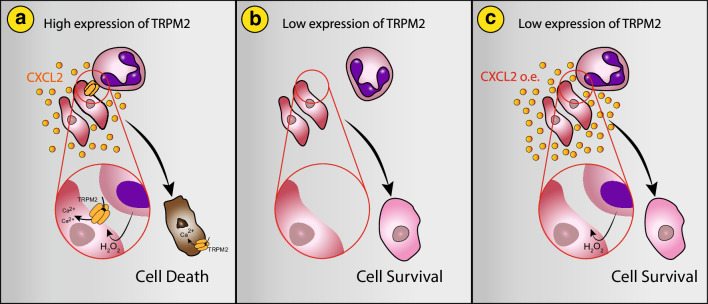
Discussion
In recent years, it has become apparent that tumor growth and metastatic progression are dictated not only by tumor cell autonomous traits, but also by the tumor microenvironment. Immune cells make a major component of the tumor microenvironment and were shown to play various roles. In this context, the role played by neutrophils was mostly shown to be tumor promoting [34, 35]. However, neutrophils are not a homogenous population and may also possess anti-tumor properties [17, 20, 36]. Furthermore, neutrophils display a significant functional plasticity and may possess anti- or pro-tumor properties at different stages of cancer progression [37, 38].
The anti-tumoral function of neutrophils largely depends on their ability to kill tumor cells. This may be done either autonomously or via ADCC. Regardless, the killing of tumor cells requires the successful completion of three consecutive steps: (1) neutrophil chemoattraction to and the formation of intimate physical contact with tumor cells; (2) the recognition of tumor cells as a target; (3) secretion of H2O2 and activation of a downstream chain of events leading to tumor cell apoptosis. In a recent study, we showed that anti-tumor neutrophil cytotoxicity is mediated via the ubiquitously expressed H2O2-dependent Ca2+ channel, TRPM2 [21]. We further showed that, when neutrophils approach tumor cells, they secrete H2O2. Consequently, TRPM2 allows the influx of Ca2+ ions, ultimately leading to tumor cell death (Fig. 4a). However, this process is critically dependent on neutrophil attraction to tumor cells and the recognition of tumor cells as a target for elimination. The mechanisms regulating both aspects remain obscure.
Fig. 4.
TRPM2 regulates neutrophil cytotoxicity and chemoattraction. a TRPM2-expressing tumor cells secrete CXCL2 enabling neutrophil chemoattraction and cytotoxicity in response to H2O2. b Impaired secretion of CXCL2 in TRPM2low tumor cells hinders neutrophil chemoattraction and cytotoxicity. c CXCL2 overexpression in TRPM2low tumor cells rescues neutrophil chemoattraction. CXCL2 overexpressing TRPM2low tumor cells remain neutrophil-resistant due to impaired Ca2+ influx in response to neutrophil H2O2
A critical aspect of the interaction between neutrophils and tumor cells is neutrophils’ chemoattraction. As demanded by their multiple roles as the first responders of the immune system, neutrophils are equipped with multiple chemokine receptors and are capable of responding to a wide array of chemotactic factors. These include factors such as IL1β, CXCL12, and IL6, and potent neutrophil chemoattractants which were implicated as key mediators of cancer progression [39–41]. In addition, neutrophil CXCR2 was found to play a critical role in neutrophil recruitment in cancer [30, 31], and its ligands CXCL1, CXCL2, and CXCL5, expressed by tumor cells and stromal cells in the tumor microenvironment were implicated in the process [42]. In the current study, we explore the molecular mechanism that regulates neutrophil chemoattraction towards tumor cells. We noticed that, upon TRPM2 knockdown, CXCL2 expression was dramatically reduced, suggesting a regulatory role for TRPM2. Indeed, stimulation of cells with H2O2 results in a dramatic increase in CXCL2 expression, blocking of Ca2+ influx in this context abrogates the stimulatory effect of H2O2 and blocks the induction of CXCL2 expression (Fig. 1m). A similar observation was made by Yamamoto et al. [28] where TRPM2 was found to be essential for ROS-induced CXCL2 expression in monocytes. These observations led us to examine the ability of neutrophils to migrate towards tumor cells. Using real-time microscopy, we found that, indeed, reduced levels of TRPM2, and the consequent reduced levels of CXCL2, result in impaired neutrophil chemoattraction (Fig. 4b). This translates not only to reduced attraction, but also to impaired neutrophil–tumor cell interaction and consequently neutrophil-resistance (Fig. 4b). Importantly, ectopic overexpression of CXCL2 in TRPM2kd cells (which express low levels of TRPM2) rescues the chemoattraction and physical interaction phenotype, corroborating the role of TRPM2 in this process (Fig. 4c). Still, although neutrophils are attracted to and form physical contact with TRPM2kd cells overexpressing CXCL2, these cells remain neutrophil-resistant (Fig. 4c). This implies that, regardless of whether neutrophils are attracted to tumor cells or not, in the absence of TRPM2-mediated Ca2+ influx, tumor cells are not susceptible to neutrophil cytotoxicity. Of note, neutrophils may be attracted to tumor cells via chemokines other than CXCL2. For example, our data also show that TRPM2 regulates the expression of CXCL1, another potent neutrophil chemoattractant (Fig. 1d).
Taken together, our data identify TRPM2 as a critical mediator of neutrophil–tumor cell interaction. Tumor cells usually express higher levels of TRPM2 compared with the neighboring healthy cells [21]. This makes tumor cells susceptible to neutrophil cytotoxicity while sparing the non-malignant cells. Importantly, tumor cells are a heterogeneous population of cells and certain cells may express reduced levels of TRPM2. These cells evade neutrophil cytotoxicity in two interrelated modes. The first is the lack of TRPM2, a factor required for transducing the cytotoxic effect of neutrophil-secreted H2O2. The second is evading neutrophils altogether by expressing reduced levels of neutrophil chemoattractants. This highlights tumor cells expressing low levels of TRPM2 as cells with increased metastatic potential and, therefore, as highly attractive targets for cancer therapy.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Abbreviations
- ADCC
Antibody-dependent cellular cytotoxicity
- ATCC
American Type Culture Collection
- CXCL1
Chemokine (C-X-C motif) ligand 1
- CXCL2
Chemokine (C-X-C motif) ligand 2
- CXCL5
Chemokine (C-X-C motif) ligand 5
- CXCL12
Chemokine (C-X-C motif) ligand 12
- CXCR2
Chemokine receptor type 2
- IL1β
Interleukin 1 beta
- IL6
Interleukin 6
- MET
Mesenchymal–epithelial transition tyrosine kinase receptor
- NDN
Normal density neutrophils
- qPCR
Quantitative real-time PCR
- TRPM2
Transient receptor potential melastatin 2
Author contributions
MG and ZG conceived and designed the experiments; MG, TFL, TZ, and RVS performed the experiments; ZG supervised the experiments; MG and ZG wrote the manuscript.
Funding
Zvi Granot was supported by Grants from the I-CORE Gene Regulation in Complex Human Disease, Center no. 41/11, the Israel Science Foundation (756/15), the Israel Cancer Research Foundation (RCDA), The Rosetrees Trust, and the Israel Cancer Association.
Compliance with ethical standards
Conflict of interest
The authors declare no conflict of interests.
References
- 1.Gajewski TF, Schreiber H, Fu YX. Innate and adaptive immune cells in the tumor microenvironment. Nat Immunol. 2013;14(10):1014–1022. doi: 10.1038/ni.2703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kolaczkowska E, Kubes P. Neutrophil recruitment and function in health and inflammation. Nat Rev Immunol. 2013;13(3):159–175. doi: 10.1038/nri3399. [DOI] [PubMed] [Google Scholar]
- 3.Galdiero MR, Bonavita E, Barajon I, Garlanda C, Mantovani A, Jaillon S. Tumor associated macrophages and neutrophils in cancer. Immunobiology. 2013;218(11):1402–1410. doi: 10.1016/j.imbio.2013.06.003. [DOI] [PubMed] [Google Scholar]
- 4.Galli SJ, Borregaard N, Wynn TA. Phenotypic and functional plasticity of cells of innate immunity: macrophages, mast cells and neutrophils. Nat Immunol. 2011;12(11):1035–1044. doi: 10.1038/ni.2109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nozawa H, Chiu C, Hanahan D. Infiltrating neutrophils mediate the initial angiogenic switch in a mouse model of multistage carcinogenesis. Proc Natl Acad Sci USA. 2006;103(33):12493–12498. doi: 10.1073/pnas.0601807103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.De Larco JE, Wuertz BR, Furcht LT. The potential role of neutrophils in promoting the metastatic phenotype of tumors releasing interleukin-8. Clin Cancer Res. 2004;10(15):4895–4900. doi: 10.1158/1078-0432.CCR-03-0760. [DOI] [PubMed] [Google Scholar]
- 7.Coffelt SB, Kersten K, Doornebal CW, Weiden J, Vrijland K, Hau CS, Verstegen NJM, Ciampricotti M, Hawinkels L, Jonkers J, de Visser KE. IL-17-producing gammadelta T cells and neutrophils conspire to promote breast cancer metastasis. Nature. 2015;522(7556):345–348. doi: 10.1038/nature14282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Moses K, Brandau S. Human neutrophils: their role in cancer and relation to myeloid-derived suppressor cells. Semin Immunol. 2016;28(2):187–196. doi: 10.1016/j.smim.2016.03.018. [DOI] [PubMed] [Google Scholar]
- 9.Cho H, Hur HW, Kim SW, Kim SH, Kim JH, Kim YT, Lee K. Pre-treatment neutrophil to lymphocyte ratio is elevated in epithelial ovarian cancer and predicts survival after treatment. Cancer Immunol Immunother. 2009;58(1):15–23. doi: 10.1007/s00262-008-0516-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Faget J, Groeneveld S, Boivin G, Sankar M, Zangger N, Garcia M, Guex N, Zlobec I, Steiner L, Piersigilli A, Xenarios I, Meylan E. Neutrophils and snail orchestrate the establishment of a pro-tumor microenvironment in lung cancer. Cell Rep. 2017;21(11):3190–3204. doi: 10.1016/j.celrep.2017.11.052. [DOI] [PubMed] [Google Scholar]
- 11.Engblom C, Pfirschke C, Zilionis R, Da Silva Martins J, Bos SA, Courties G, Rickelt S, Severe N, Baryawno N, Faget J, Savova V, Zemmour D, Kline J, Siwicki M, Garris C, Pucci F, Liao HW, Lin YJ, Newton A, Yaghi OK, Iwamoto Y, Tricot B, Wojtkiewicz GR, Nahrendorf M, Cortez-Retamozo V, Meylan E, Hynes RO, Demay M, Klein A, Bredella MA, Scadden DT, Weissleder R, Pittet MJ. Osteoblasts remotely supply lung tumors with cancer-promoting SiglecF(high) neutrophils. Science. 2017 doi: 10.1126/science.aal5081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Michaeli J, Shaul ME, Mishalian I, Hovav AH, Levy L, Zolotriov L, Granot Z, Fridlender ZG. Tumor-associated neutrophils induce apoptosis of non-activated CD8 T-cells in a TNFalpha and NO-dependent mechanism, promoting a tumor-supportive environment. Oncoimmunology. 2017;6(11):e1356965. doi: 10.1080/2162402X.2017.1356965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chao T, Furth EE, Vonderheide RH. CXCR2-dependent accumulation of tumor-associated neutrophils regulates T-cell immunity in pancreatic ductal adenocarcinoma. Cancer Immunol Res. 2016;4(11):968–982. doi: 10.1158/2326-6066.CIR-16-0188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wculek SK, Malanchi I. Neutrophils support lung colonization of metastasis-initiating breast cancer cells. Nature. 2015;528(7582):413–417. doi: 10.1038/nature16140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Donati K, Sepult C, Rocks N, Blacher S, Gerard C, Noel A, Cataldo D. Neutrophil-derived interleukin 16 in premetastatic lungs promotes breast tumor cell seeding. Cancer Growth Metast. 2017;10:1179064417738513. doi: 10.1177/1179064417738513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Colombo MP, Lombardi L, Stoppacciaro A, Melani C, Parenza M, Bottazzi B, Parmiani G. Granulocyte colony-stimulating factor (G-CSF) gene transduction in murine adenocarcinoma drives neutrophil-mediated tumor inhibition in vivo. Neutrophils discriminate between G-CSF-producing and G-CSF-nonproducing tumor cells. J Immunol. 1992;149(1):113–119. [PubMed] [Google Scholar]
- 17.Granot Z, Henke E, Comen EA, King TA, Norton L, Benezra R. Tumor entrained neutrophils inhibit seeding in the premetastatic lung. Cancer Cell. 2011;20(3):300–314. doi: 10.1016/j.ccr.2011.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lopez-Lago MA, Posner S, Thodima VJ, Molina AM, Motzer RJ, Chaganti RS. Neutrophil chemokines secreted by tumor cells mount a lung antimetastatic response during renal cell carcinoma progression. Oncogene. 2013;32(14):1752–1760. doi: 10.1038/onc.2012.201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Finisguerra V, Di Conza G, Di Matteo M, Serneels J, Costa S, Thompson AA, Wauters E, Walmsley S, Prenen H, Granot Z, Casazza A, Mazzone M. MET is required for the recruitment of anti-tumoural neutrophils. Nature. 2015;522(7556):349–353. doi: 10.1038/nature14407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sagiv JY, Michaeli J, Assi S, Mishalian I, Kisos H, Levy L, Damti P, Lumbroso D, Polyansky L, Sionov RV, Ariel A, Hovav AH, Henke E, Fridlender ZG, Granot Z. Phenotypic diversity and plasticity in circulating neutrophil subpopulations in cancer. Cell Rep. 2015;10(4):562–573. doi: 10.1016/j.celrep.2014.12.039. [DOI] [PubMed] [Google Scholar]
- 21.Gershkovitz M, Caspi Y, Fainsod-Levi T, Katz B, Michaeli J, Khawaled S, Lev S, Polyansky L, Shaul ME, Sionov RV, Cohen-Daniel L, Aqeilan RI, Shaul YD, Mori Y, Karni R, Fridlender ZG, Binshtok AM, Granot Z. TRPM2 mediates neutrophil killing of disseminated tumor cells. Cancer Res. 2018;78(10):2680–2690. doi: 10.1158/0008-5472.CAN-17-3614. [DOI] [PubMed] [Google Scholar]
- 22.Gershkovitz M, Fainsod-Levi T, Khawaled S, Shaul ME, Sionov RV, Cohen-Daniel L, Aqeilan RI, Shaul Y, Fridlender ZG, Granot Z. Microenvironmental cues determine tumor cell susceptibility to neutrophil cytotoxicity. Cancer Res. 2018 doi: 10.1158/0008-5472.CAN-18-0540. [DOI] [PubMed] [Google Scholar]
- 23.Hara Y, Wakamori M, Ishii M, Maeno E, Nishida M, Yoshida T, Yamada H, Shimizu S, Mori E, Kudoh J, Shimizu N, Kurose H, Okada Y, Imoto K, Mori Y. LTRPC2 Ca2+-permeable channel activated by changes in redox status confers susceptibility to cell death. Mol Cell. 2002;9(1):163–173. doi: 10.1016/S1097-2765(01)00438-5. [DOI] [PubMed] [Google Scholar]
- 24.Montell C, Birnbaumer L, Flockerzi V. The TRP channels, a remarkably functional family. Cell. 2002;108(5):595–598. doi: 10.1016/S0092-8674(02)00670-0. [DOI] [PubMed] [Google Scholar]
- 25.Zeng X, Sikka SC, Huang L, Sun C, Xu C, Jia D, Abdel-Mageed AB, Pottle JE, Taylor JT, Li M. Novel role for the transient receptor potential channel TRPM2 in prostate cancer cell proliferation. Prostate Cancer Prostatic Dis. 2010;13(2):195–201. doi: 10.1038/pcan.2009.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Knowles H, Li Y, Perraud AL. The TRPM2 ion channel, an oxidative stress and metabolic sensor regulating innate immunity and inflammation. Immunol Res. 2013;55(1–3):241–248. doi: 10.1007/s12026-012-8373-8. [DOI] [PubMed] [Google Scholar]
- 27.Syed Mortadza SA, Wang L, Li D, Jiang LH. TRPM2 channel-mediated ROS-sensitive Ca(2+) signaling mechanisms in immune cells. Front Immunol. 2015;6:407. doi: 10.3389/fimmu.2015.00407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yamamoto S, Shimizu S, Kiyonaka S, Takahashi N, Wajima T, Hara Y, Negoro T, Hiroi T, Kiuchi Y, Okada T, Kaneko S, Lange I, Fleig A, Penner R, Nishi M, Takeshima H, Mori Y. TRPM2-mediated Ca2+ influx induces chemokine production in monocytes that aggravates inflammatory neutrophil infiltration. Nat Med. 2008;14(7):738–747. doi: 10.1038/nm1758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mittal M, Nepal S, Tsukasaki Y, Hecquet CM, Soni D, Rehman J, Tiruppathi C, Malik AB. Neutrophil activation of endothelial cell-expressed TRPM2 mediates transendothelial neutrophil migration and vascular injury. Circ Res. 2017;121(9):1081–1091. doi: 10.1161/CIRCRESAHA.117.311747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jablonska J, Wu CF, Andzinski L, Leschner S, Weiss S. CXCR2-mediated tumor-associated neutrophil recruitment is regulated by IFN-beta. Int J Cancer. 2014;134(6):1346–1358. doi: 10.1002/ijc.28551. [DOI] [PubMed] [Google Scholar]
- 31.Yu PF, Huang Y, Han YY, Lin LY, Sun WH, Rabson AB, Wang Y, Shi YF. TNFalpha-activated mesenchymal stromal cells promote breast cancer metastasis by recruiting CXCR2(+) neutrophils. Oncogene. 2017;36(4):482–490. doi: 10.1038/onc.2016.217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Miller BA. The role of TRP channels in oxidative stress-induced cell death. J Membr Biol. 2006;209(1):31–41. doi: 10.1007/s00232-005-0839-3. [DOI] [PubMed] [Google Scholar]
- 33.Sionov RV, Assi S, Gershkovitz M, Sagiv JY, Polyansky L, Mishalian I, Fridlender ZG, Granot Z. Isolation and characterization of neutrophils with anti-tumor properties. J Vis Exp. 2015;100:e52933. doi: 10.3791/52933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Powell DR, Huttenlocher A. Neutrophils in the tumor microenvironment. Trends Immunol. 2016;37(1):41–52. doi: 10.1016/j.it.2015.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fridlender ZG, Albelda SM. Tumor-associated neutrophils: friend or foe? Carcinogenesis. 2012;33(5):949–955. doi: 10.1093/carcin/bgs123. [DOI] [PubMed] [Google Scholar]
- 36.Jablonska J, Granot Z. Neutrophil, quo vadis? J Leukoc Biol. 2017;102(3):685–688. doi: 10.1189/jlb.3MR0117-015R. [DOI] [PubMed] [Google Scholar]
- 37.Fridlender ZG, Sun J, Kim S, Kapoor V, Cheng G, Ling L, Worthen GS, Albelda SM. Polarization of tumor-associated neutrophil phenotype by TGF-beta: “N1” versus “N2” TAN. Cancer Cell. 2009;16(3):183–194. doi: 10.1016/j.ccr.2009.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jablonska J, Leschner S, Westphal K, Lienenklaus S, Weiss S. Neutrophils responsive to endogenous IFN-beta regulate tumor angiogenesis and growth in a mouse tumor model. J Clin Invest. 2010;120(4):1151–1164. doi: 10.1172/JCI37223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Apte RN, Dotan S, Elkabets M, White MR, Reich E, Carmi Y, Song X, Dvozkin T, Krelin Y, Voronov E. The involvement of IL-1 in tumorigenesis, tumor invasiveness, metastasis and tumor-host interactions. Cancer Metastasis Rev. 2006;25(3):387–408. doi: 10.1007/s10555-006-9004-4. [DOI] [PubMed] [Google Scholar]
- 40.Nagarsheth N, Wicha MS, Zou W. Chemokines in the cancer microenvironment and their relevance in cancer immunotherapy. Nat Rev Immunol. 2017;17(9):559–572. doi: 10.1038/nri.2017.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Caetano MS, Zhang H, Cumpian AM, Gong L, Unver N, Ostrin EJ, Daliri S, Chang SH, Ochoa CE, Hanash S, Behrens C, Wistuba II, Sternberg C, Kadara H, Ferreira CG, Watowich SS, Moghaddam SJ. IL6 blockade reprograms the lung tumor microenvironment to limit the development and progression of K-ras-mutant lung cancer. Cancer Res. 2016;76(11):3189–3199. doi: 10.1158/0008-5472.CAN-15-2840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sionov RV, Fridlender ZG, Granot Z. The multifaceted roles neutrophils play in the tumor microenvironment. Cancer Microenviron. 2015;8(3):125–158. doi: 10.1007/s12307-014-0147-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.