Abstract
This study aims to assess the association between intravenous diltiazem and metoprolol in rate control for atrial fibrillation (AF) patients with rapid ventricular rate, focusing on rate control efficacy and hemodynamic adverse events. Following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines, electronic searches were conducted in Embase, PubMed, and Cochrane Central Register of Controlled Trials (CENTRAL) until February 20, 2024. The primary outcome was achieving ventricular rate control < 110/min. Secondary outcomes included new hypotension (systolic blood pressure < 90 mm Hg) and bradycardia (heart rate < 60/min). Nineteen studies (three randomized controlled trials and 16 observational studies) were included in this meta-analysis. Pooled analysis showed intravenous metoprolol resulted in a 39% lower rate control attainment compared to diltiazem (OR: 0.61; 95% CI: 0.44 to 0.84; p = 0.002). There were no significant differences in bradycardia (OR: 0.51; 95% CI: 0.22 to 1.22; p = 0.13) or hypotension risk (OR: 1.08; 95% CI: 0.72 to 1.61; p = 0.72) between the two groups. Intravenous diltiazem demonstrated superior rate control efficacy compared to metoprolol in AF patients with rapid ventricular rate. However, no significant differences were observed in safety outcomes, namely, bradycardia and hypotension.
Keywords: meta-analysis, diltiazem, metoprolol, rate control, atrial fibrillation
Introduction and background
Atrial fibrillation (AF) is prevalent among critically ill patients in the intensive care unit (ICU) and has been linked to heightened mortality rates [1]. Notably, in a large-scale epidemiological investigation, AF was detected in 25.5% of 60,209 hospitalizations for sepsis [2]. Moreover, AF results in about 600,000 visits to the emergency department (ED), 450,000 hospitalizations, and 22,000 deaths every year in the United States [3]. Individuals diagnosed with AF encounter a notably increased likelihood of experiencing cardioembolic stroke by a factor of 5, a three-fold higher risk of heart failure (HF), and twice the mortality rate [4].
Current guidelines for managing AF advocate for intravenous administration of either a beta blocker or a non-dihydropyridine calcium channel blocker to achieve rate control in acute settings [5]. Pharmacokinetic data indicate that intravenous diltiazem has a rapid onset of action within three minutes, albeit with a duration of effect ranging from one to three hours [6]. In comparison, metoprolol administered in doses of 5 mg and 15 mg over 10 minutes demonstrates an onset of action after 20 minutes, with durations of action lasting between five and eight hours [7]. Although pharmacokinetic profiles suggest diltiazem may act more swiftly but with a shorter duration compared to metoprolol, guidelines remain equivocal regarding their preference in unstable AF.
Given the emergence of new studies since the last meta-analysis comparing diltiazem and metoprolol in AF patients, an updated meta-analysis is warranted [8]. The purpose of this review is to offer emergency physicians evidence-based guidance on choosing the suitable medication for controlling heart rate in AF patients who arrive at the emergency department with a rapid ventricular rate. The main goal is to investigate whether there is a correlation between using intravenous diltiazem or metoprolol for rate control in AF patients with rapid ventricular rate, particularly focusing on achieving effective rate control and potential adverse hemodynamic events such as hypotension and bradycardia.
Review
Methodology
We followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines during the execution of this systematic review and meta-analysis.
Search Strategy
We conducted electronic searches in databases including EMBASE, PubMed, and the Cochrane Central Register of Controlled Trials (CENTRAL) from the inception of databases to February 20, 2024. Our search utilized key terms such as "diltiazem," "metoprolol," and "atrial fibrillation," along with Boolean algebra operators and medical subject heading (MeSH) terms. Additionally, we identified supplementary studies by scrutinizing the reference lists of eligible publications. Language restrictions were not applied. Two investigators conducted the literature search, with any discrepancies resolved through discussion.
Inclusion and Exclusion Criteria
Articles were considered for inclusion if they compared the efficacy and safety of intravenous diltiazem versus metoprolol in adult patients (aged 18 years and above) with AF. Inclusion criteria mandated the utilization of clearly defined clinical outcomes pertaining to efficacy (achievement of rate control target) and safety (occurrence of hypotension or bradycardia as adverse events) associated with both medications. We encompassed both randomized controlled trials (RCTs) and non-randomized controlled trials (non-RCTs). Our primary outcome measure was the attainment of ventricular rate control <110/min in hospitalized patients with AF and rapid ventricular rate, while secondary outcomes included the incidence of new hypotension (systolic blood pressure < 90 mm Hg) and bradycardia (heart rate < 60/min) post-administration of intravenous diltiazem or metoprolol. Articles investigating oral medications for chronic rate control in outpatients with AF or focusing on the management of AF in patients with pre-excitation syndromes were excluded. Two independent reviewers screened abstracts obtained from the aforementioned search strategy based on inclusion and exclusion criteria, followed by a detailed evaluation of full-text screening. Ultimately, studies comparing metoprolol to diltiazem for AF management were included.
Data Extraction and Quality Assessment
Data extraction utilized a pre-designed data extraction sheet. Information extracted from included studies encompassed author names, publication year, study design, sample size, and outcomes assessed in this meta-analysis. One investigator entered the data into the Review Manager program (RevMan, version 5.4.1, The Cochrane Collaboration, London, UK), while another verified its accuracy. Quality assessment was performed using the Newcastle-Ottawa Scale for observational studies and the Cochrane risk of bias assessment tool for RCTs.
Data Analysis
We conducted meta-analyses using Review Manager. Dichotomous outcomes were analyzed for odds ratios (ORs) along with 95% confidence intervals (CIs) using the Mantel-Haenszel (MH) random-effects model to address clinical and statistical differences across studies. A p-value < 0.05 indicated statistical significance. Heterogeneity was evaluated visually via forest plots and through statistical tests measuring heterogeneity variance (t2) and inconsistency (I2). Significant heterogeneity was identified if I2 exceeded 50%. We performed subgroup analysis by comparing the effectiveness of two drugs to achieve the rate control in patients with heart failure with reduced ejection fraction (HFrEF).
Results
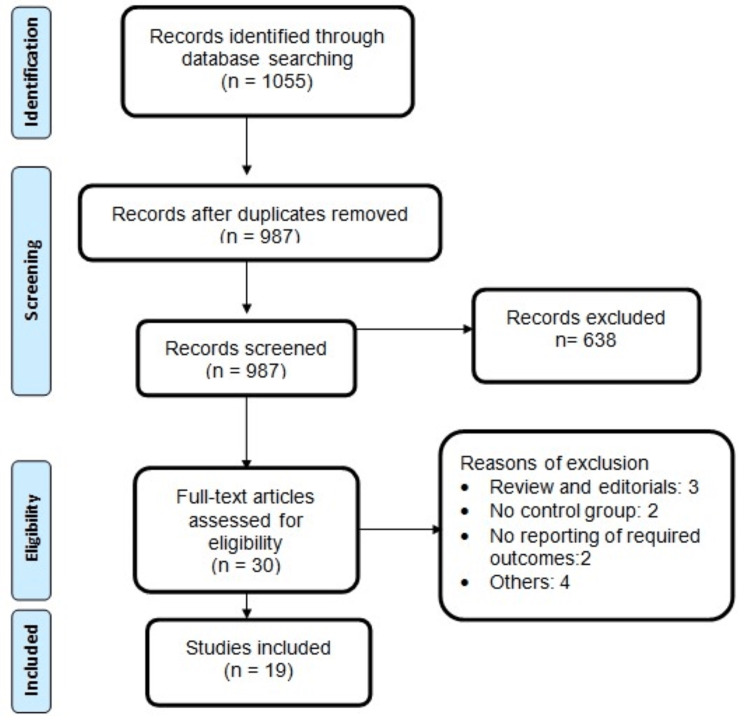
The initial database search retrieved 1055 articles. Following the removal of 68 duplicate records, 987 unique articles underwent initial screening. Abstracts and titles were screened initially, followed by a full-text evaluation of eligible studies based on predefined inclusion and exclusion criteria. Ultimately, 19 studies met the criteria and were included in this meta-analysis, comprising a total of 2596 patients with AF and rapid ventricular rate. The study selection process is depicted in Figure 1. Of the included studies, three were RCTs, while 16 were observational in nature. The majority of studies were conducted in the United States (n = 16). Detailed characteristics of the included studies are presented in Table 1. Table 2 presents the quality assessment of the included studies.
Table 1. Characteristics of included studies.
RCT: randomized-control trial; US: United States; ED: emergency department; ICU: intensive care unit.
| Author | Year | Study design | Region | Study setting | Groups | Sample size | Age | Males (n) |
| Blackburn et al. [9] | 2023 | Observational | US | ED | Metoprolol | 99 | 67.2 | 57 |
| Diltiazem | 206 | 65 | 123 | |||||
| Compagner et al. [10] | 2022 | Observational | US | ED | Metoprolol | 59 | 75.4 | 20 |
| Diltiazem | 134 | 72.3 | 52 | |||||
| Demir et al. [11] | 2021 | Observational | Turkey | ED | Metoprolol | 15 | NS | NS |
| Diltiazem | 26 | |||||||
| Demircan et al. [12] | 2005 | RCT | Turkey | ED | Metoprolol | 20 | NS | NS |
| Diltiazem | 20 | |||||||
| Feeney et al. [13] | 2017 | Observational | US | ED | Metoprolol | 316 | 65 | 200 |
| Diltiazem | 16 | 62 | 10 | |||||
| Fromm et al. [14] | 2015 | RCT | US | ED | Metoprolol | 28 | 69.5 | 15 |
| Diltiazem | 24 | 66.2 | 11 | |||||
| Hasbrouck et al. [15] | 2022 | Observational | US | ED | Metoprolol | 68 | 65 | 51 |
| Diltiazem | 57 | 59 | 44 | |||||
| Hargrove et al. [16] | 2021 | Observational | US | ED | Metoprolol | 19 | 62.9 | 9 |
| Diltiazem | 32 | 62.2 | 21 | |||||
| Hines et al. [17] | 2016 | Observational | US | ED | Metoprolol | 36 | 65.7 | 24 |
| Diltiazem | 51 | 64.2 | 27 | |||||
| Hirschy et al. [18] | 2019 | Observational | US | ED | Metoprolol | 14 | 69 | 9 |
| Diltiazem | 34 | 67 | 22 | |||||
| Kapustova et al. [19] | 2023 | Observational | US | ED | Metoprolol | 15 | 59.8 | 11 |
| Diltiazem | 30 | 59.2 | 21 | |||||
| Katchi et al. [20] | 2014 | Observational | US | ED | Metoprolol | 83 | NS | NS |
| Diltiazem | 90 | |||||||
| McGrath et al. [21] | 2020 | Observational | US | ED | Metoprolol | 166 | 68.4 | 70 |
| Diltiazem | 183 | 68.2 | 83 | |||||
| Medeiros et al. [22] | 2021 | Observational | US | ED | Metoprolol | 15 | 76 | 8 |
| Diltiazem | 51 | 71 | 22 | |||||
| Memis et al. [23] | 2019 | RCT | Turkey | ED | Metoprolol | 50 | 73.36 | NS |
| Diltiazem | 50 | 74.18 | ||||||
| Nicholson et al. [24] | 2020 | Observational | US | ED | Metoprolol | 45 | 64 | 23 |
| Diltiazem | 63 | 68 | 32 | |||||
| Nunez Cruz et al. [25] | 2020 | Observational | US | ED | Metoprolol | 80 | 68 | 35 |
| Diltiazem | 80 | 66 | 42 | |||||
| Personett et al. [26] | 2014 | Observational | US | ICU | Metoprolol | 66 | 77 | 34 |
| Diltiazem | 55 | 76 | 30 | |||||
| Xiao et al. [27] | 2022 | Observational | US | ED | Metoprolol | 100 | 64 | 62 |
| Diltiazem | 100 | 66 | 51 |
Table 2. Quality assessment of included studies.
| Quality assessment of observational studies | ||||||
| Author | Selection | Comparison | Outcome | Overall | ||
| Blackburn et al. [9] | 3 | 1 | 3 | Good | ||
| Compagner et al. [10] | 4 | 1 | 2 | Good | ||
| Demir et al. [11] | 3 | 1 | 3 | Good | ||
| Feeney et al. [13] | 3 | 1 | 2 | Fair | ||
| Hasbrouck et al. [15] | 4 | 1 | 2 | Good | ||
| Hargrove et al. [16] | 3 | 1 | 2 | Fair | ||
| Hines et al. [17] | 3 | 1 | 2 | Fair | ||
| Hirschy et al. [18] | 4 | 1 | 1 | Fair | ||
| Kapustova et al. [19] | 4 | 1 | 2 | Good | ||
| Katchi et al. [20] | 4 | 1 | 2 | Good | ||
| McGrath et al. [21] | 4 | 1 | 2 | Good | ||
| Medeiros et al. [22] | 4 | 2 | 1 | Good | ||
| Nicholson et al. [24] | 4 | 1 | 3 | Good | ||
| Personett et al. [26] | 3 | 1 | 2 | Fair | ||
| Xiao et al. [27] | 4 | 1 | 2 | Good | ||
| Quality assessment of randomized control trials | ||||||
| Author ID | Selection bias | Performance bias | Detection bias | Attrition bias | Reporting bias | Other bias |
| Demircan et al. [12] | No | No | No | No | No | No |
| Fromm et al. [14] | No | No | No | No | No | No |
| Memis et al. [23] | No | Yes | Yes | No | No | No |
Figure 1. PRISMA flowchart of study selection.
PRISMA: Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
Meta-Analysis of Outcomes
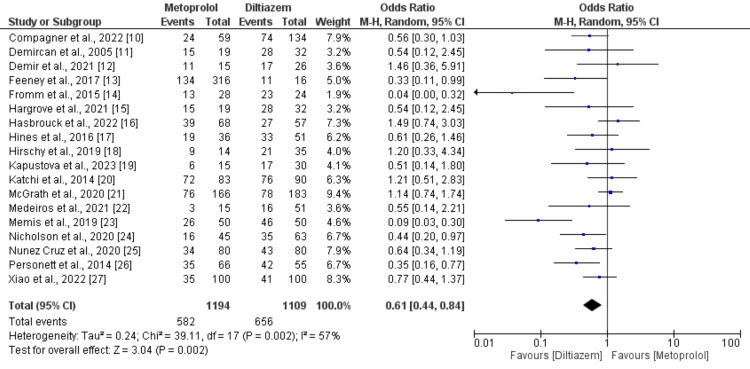
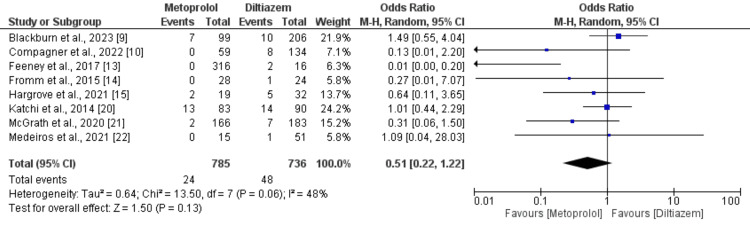
Eighteen studies, comprising 15 observational studies and three RCTs, directly assessed the attainment of rate control targets between metoprolol and diltiazem groups. Pooling data from these 18 studies, each reporting on the accomplishment of rate control target with diltiazem (n = 1109) compared to metoprolol (n=1194) in patients with AF with rapid ventricular rate, revealed that patients who received intravenous metoprolol exhibited a significantly (39%) lower attainment of rate control target compared to those treated with intravenous diltiazem (OR: 0.61; 95% CI: 0.44 to 0.84; p-value: 0.002). Notably, there was substantial heterogeneity (I-square: 57%) as illustrated in Figure 2. Additionally, eight studies, encompassing 1521 patients, reported the incidence of bradycardia as an adverse event with diltiazem versus metoprolol. A meta-analysis of outcomes from these studies indicated no significant difference in the occurrence of bradycardia as an adverse event between metoprolol (3.05%) and diltiazem (6.52%) in patients with AF with rapid ventricular rate (OR: 0.51; 95% CI: 0.22 to 1.22; p-value: 0.13), with moderate heterogeneity (I-square: 48%) depicted in Figure 3.
Figure 2. Comparison of achievement of rate control target.
Figure 3. Comparison of risk of bradycardia.
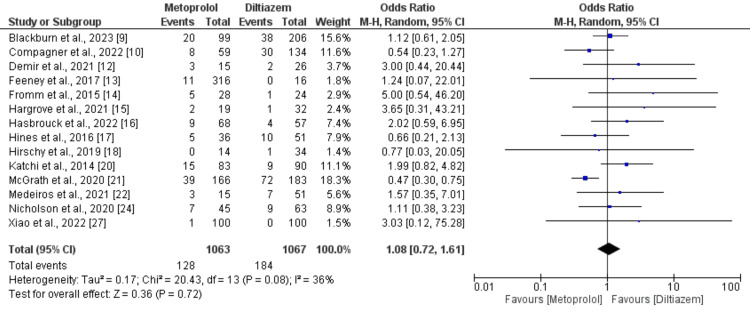
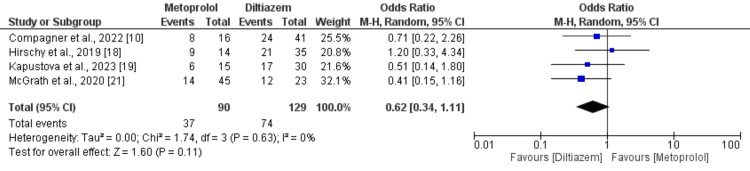
Moreover, 14 studies, comprising 2130 patients, documented hypotension as an adverse event associated with diltiazem versus metoprolol. Analysis of data from these studies did not uncover a significant difference in hypotension incidence between intravenous metoprolol and diltiazem in AF patients with rapid ventricular rate (OR: 1.08; 95% CI: 0.72 to 1.61; p-value: 0.72), with moderate heterogeneity (I-square: 36%), as depicted in Figure 4. Subgroup analysis was conducted, including patients with HFrEF. Only three studies encompassed patients with HFrEF, and the findings are delineated in Figure 5. The combined analysis demonstrated that patients receiving intravenous diltiazem achieved the rate control target significantly more than those treated with intravenous metoprolol. However, the results were statistically insignificant (OR: 0.62, 95% CI: 0.34 to 1.11, p-value: 0.11). No significant heterogeneity was reported among the study results (I-square: 0%).
Figure 4. Comparison of risk of hypotension.
Figure 5. Comparison of achievement of rate control target in patients with HFrEF.
HFrEF: heart failure with reduced ejection fraction.
Discussion
Our meta-analysis indicated that intravenous diltiazem proved more effective than intravenous metoprolol in managing ventricular rate in AF patients. This finding holds significance given the correlation between inadequate rate control and heightened cardiovascular adverse events [28]. However, notable heterogeneity existed among the studies. Both the “American College of Cardiology” and the “Canadian Cardiovascular Society” guidelines consider both agents as Class I recommendations for ventricular rate control in AF, without preference for any of the two drugs [29-30]. Regional variations influence the selection of agents for ventricular rate control in the emergency department, with diltiazem being predominant in North America, while metoprolol is favored in the United Kingdom and Australia [31].
Previous meta-analyses have similarly highlighted diltiazem's favorable outcomes, showing a significant increase in achieving rate control targets compared to metoprolol (OR: 1.92, 95% CI: 1.26 to 2.90) [8]. Additionally, Lan et al.'s [32] meta-analysis corroborated diltiazem's superiority, noting its higher efficacy, quicker onset time, reduced ventricular rate, and minimal impact on blood pressure. These consistent findings underscore diltiazem's suitability as the preferred medication for rate control in AF with rapid ventricular rate, providing substantial evidence for clinical decision-making.
Our study involved subgroup analysis aimed at comparing the efficacy of two drugs in patients diagnosed with HFrEF. The findings revealed that while rate control demonstrated effectiveness in patients administered diltiazem as opposed to metoprolol, no statistically significant variances were observed between the two groups. The probable rationale behind the absence of significant disparities could be attributed to the limited sample size, which consequently resulted in insufficient statistical power to discern notable differences between the groups. It is noteworthy that all four studies examining these drugs in HFrEF patients reported favorable outcomes associated with diltiazem, albeit none reaching statistical significance. This underscores the continued clinical interest in exploring the safety and efficacy profiles of diltiazem in HFrEF patients through prospective clinical trials characterized by larger sample sizes. Such endeavors hold promise for providing clearer insights into the potential benefits of diltiazem therapy in this patient population.
In our safety analysis, we meticulously assessed occurrences of bradycardia and hypotension in patients treated with diltiazem and metoprolol. Notably, our findings revealed no significant disparities between the two groups in any of the safety outcomes examined. This aligns with similar conclusions drawn from the studies conducted by Sharda et al. [8] and Lan et al. [32], wherein both meta-analyses failed to identify any substantial differences between diltiazem and metoprolol concerning incidents of bradycardia and hypotension. Consequently, our study supports the assertion that diltiazem effectively regulates heart rate without compromising patient safety. However, it is essential to note that the majority of studies included in our meta-analysis, as well as those mentioned in prior meta-analyses, were observational in nature. Hence, to affirm these findings with greater certainty, RCTs featuring larger sample sizes are imperative.
Clinical Implications
The meta-analysis underscores diltiazem's superior efficacy over metoprolol in achieving rate control for AF. Clinicians should prioritize diltiazem for acute rate control, mindful of regional practice variations. Safety profiles for both agents are comparable, emphasizing the importance of individualized therapy selection. Further research, particularly prospective trials, is warranted to confirm these findings and refine treatment guidelines, ensuring optimal management strategies for patients with AF and rapid ventricular rate.
Study Limitations
The meta-analysis predominantly comprised retrospective studies, with only three RCTs included. However, these studies were frequently constrained by factors such as selection bias, limited sample sizes, and the absence of blinding in personnel and outcome assessment. Furthermore, certain clinical outcomes, including ICU admission, mortality rates, and the use of inotropes, were not evaluated in this meta-analysis due to insufficient data within the included studies. Furthermore, there was no evaluation performed regarding the relationship between comorbidities such as coronary artery disease, hypertension, diabetes mellitus, obesity, previous stroke or transient ischemic attack, asthma or chronic obstructive pulmonary disease, infections, kidney disease, and peripheral vascular disease, and the achievement of rate control goals, as well as any adverse effects associated with the utilization of diltiazem and metoprolol. This omission was attributed to the unavailability of patient-level data for analysis. Lastly, studies were conducted either in Turkey or the United States. We need multinational RCTs to validate the findings of this study.
Conclusions
In conclusion, our meta-analysis encompassed 18 studies, comprising 15 retrospective studies and 3 RCTs, investigating the efficacy and safety of diltiazem and metoprolol in managing ventricular rate in patients with AF. The pooled analysis demonstrated that intravenous diltiazem achieved a significantly higher rate control target compared to metoprolol, indicating its efficacy in this context. However, no significant differences were observed between the two drugs in terms of safety outcomes, namely, bradycardia and hypotension. Despite these findings, it is crucial to acknowledge the limitations inherent in the predominantly retrospective nature of the studies, as well as the absence of data on various clinical outcomes and comorbidities. Future research, particularly RCT with larger sample sizes, is warranted to validate these findings and inform clinical decision-making.
The authors have declared that no competing interests exist.
Author Contributions
Acquisition, analysis, or interpretation of data: Areeba Khan, Tanya Sinha, Mansoor Ahmad, Samyuktha Balaji, Sandipkumar S. Chaudhari, Divine Besong Arrey Agbor
Drafting of the manuscript: Areeba Khan, Tanya Sinha, Ye Kyaw Myint, Samyuktha Balaji, Sandipkumar S. Chaudhari, Divine Besong Arrey Agbor
Concept and design: Abshiro H. Mayow, Tanya Sinha, Ye Kyaw Myint, Mansoor Ahmad
Critical review of the manuscript for important intellectual content: Abshiro H. Mayow, Mansoor Ahmad
References
- 1.Incident stroke and mortality associated with new-onset atrial fibrillation in patients hospitalized with severe sepsis. Walkey AJ, Wiener RS, Ghobrial JM, Curtis LH, Benjamin EJ. JAMA. 2011;306:2248–2254. doi: 10.1001/jama.2011.1615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Atrial fibrillation among Medicare beneficiaries hospitalized with sepsis: incidence and risk factors. Walkey AJ, Greiner MA, Heckbert SR, et al. Am Heart J. 2013;165:949–955. doi: 10.1016/j.ahj.2013.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Emergency department, hospital inpatient, and mortality burden of atrial fibrillation in the United States, 2006 to 2014. Jackson SL, Tong X, Yin X, George MG, Ritchey MD. Am J Cardiol. 2017;120:1966–1973. doi: 10.1016/j.amjcard.2017.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.A population-based study of the long-term risks associated with atrial fibrillation: 20-year follow-up of the Renfrew/Paisley study. Stewart S, Hart CL, Hole DJ, McMurray JJV. Am J Med. 2002;113:359–364. doi: 10.1016/s0002-9343(02)01236-6. [DOI] [PubMed] [Google Scholar]
- 5.2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. January CT, Wann LS, Alpert JS, et al. J Am Coll Cardiol. 2014;64:0–76. doi: 10.1016/j.jacc.2014.03.022. [DOI] [PubMed] [Google Scholar]
- 6.Diltiazem hydrochloride. [ Feb; 2024 ]. 2007. https://dailymed.nlm.nih.gov/dailymed/getFile.cfm?setid=5e36488b-8f2d-4dc9-b803-af1829e6fdd0&type=pdf https://dailymed.nlm.nih.gov/dailymed/getFile.cfm?setid=5e36488b-8f2d-4dc9-b803-af1829e6fdd0&type=pdf
- 7.Novartis Pharmaceuticals. Metoprolol tartrate. East Hanover, NJ: Novartis Pharmaceuticals. [ Feb; 2024 ]. 2008. https://www.accessdata.fda.gov/drugsatfda_docs/label/2008/017963s062,018704s021lbl.pdf https://www.accessdata.fda.gov/drugsatfda_docs/label/2008/017963s062,018704s021lbl.pdf
- 8.Comparison of diltiazem and metoprolol for atrial fibrillation with rapid ventricular rate: systematic review and meta-analysis. Sharda SC, Bhatia MS. Indian Heart J. 2022;74:494–499. doi: 10.1016/j.ihj.2022.10.195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Metoprolol versus diltiazem in the emergency department for atrial fibrillation with rapid ventricular response. Blackburn M, Edwards L, Woolum J, Bailey A, Dugan A, Slade E. JEM Rep. 2023;2:100020. [Google Scholar]
- 10.Intravenous metoprolol versus diltiazem for atrial fibrillation with concomitant heart failure. Compagner CT, Wysocki CR, Reich EK, Zimmerman LH, Holzhausen JM. Am J Emerg Med. 2022;62:49–54. doi: 10.1016/j.ajem.2022.10.001. [DOI] [PubMed] [Google Scholar]
- 11.Intravenous diltiazem or metoprolol administration in the emergency department for acute rate control of atrial fibrillation patients with rapid ventricular response with unknown ejection fraction. Demi̇r MC, Doğan M, Polat E, Akpi̇nar G. Duzce Med J. 2021;23:10–14. [Google Scholar]
- 12.Comparison of the effectiveness of intravenous diltiazem and metoprolol in the management of rapid ventricular rate in atrial fibrillation. Demircan C, Cikriklar HI, Engindeniz Z, et al. Emerg Med J. 2005;22:411–414. doi: 10.1136/emj.2003.012047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Achieving ventricular rate control in patients taking chronic beta-blocker therapy. Feeney ME, Rowe SL, Mah ND, Barton CA, Ran R. Am J Emerg Med. 2018;36:110–113. doi: 10.1016/j.ajem.2017.09.013. [DOI] [PubMed] [Google Scholar]
- 14.Diltiazem vs. metoprolol in the management of atrial fibrillation or flutter with rapid ventricular rate in the emergency department. Fromm C, Suau SJ, Cohen V, Likourezos A, Jellinek-Cohen S, Rose J, Marshall J. J Emerg Med. 2015;49:175–182. doi: 10.1016/j.jemermed.2015.01.014. [DOI] [PubMed] [Google Scholar]
- 15.Acute management of atrial fibrillation in congestive heart failure with reduced ejection fraction in the emergency department. Hasbrouck M, Nguyen TT. Am J Emerg Med. 2022;58:39–42. doi: 10.1016/j.ajem.2022.03.058. [DOI] [PubMed] [Google Scholar]
- 16.Comparison of sustained rate control in atrial fibrillation with rapid ventricular rate: metoprolol vs. diltiazem. Hargrove KL, Robinson EE, Lusk KA, Hughes DW, Neff LA, Fowler AL. Am J Emerg Med. 2021;40:15–19. doi: 10.1016/j.ajem.2020.11.073. [DOI] [PubMed] [Google Scholar]
- 17.Diltiazem versus metoprolol for rate control in atrial fibrillation with rapid ventricular response in the emergency department. Hines MC, Reed BN, Ivaturi V, Bontempo LJ, Bond MC, Hayes BD. Am J Health Syst Pharm. 2016;73:2068–2076. doi: 10.2146/ajhp160126. [DOI] [PubMed] [Google Scholar]
- 18.Metoprolol vs. diltiazem in the acute management of atrial fibrillation in patients with heart failure with reduced ejection fraction. Hirschy R, Ackerbauer KA, Peksa GD, O'Donnell EP, DeMott JM. Am J Emerg Med. 2019;37:80–84. doi: 10.1016/j.ajem.2018.04.062. [DOI] [PubMed] [Google Scholar]
- 19.Acute rate control with metoprolol versus diltiazem in atrial fibrillation with heart failure with reduced ejection fraction. Kapustova K, Phan B, Allison-Aipa T, Choi M. Am J Emerg Med. 2023;67:126–129. doi: 10.1016/j.ajem.2023.02.019. [DOI] [PubMed] [Google Scholar]
- 20.Treating rapid atrial fibrillation in acute decompensated heart failure: metoprolol and diltiazem are equally safe, yet metoprolol increases conversion to sinus rhythm. Katchi F, Nagabandi S, Shuster J, Novak E, Joseph S. J Card Fail. 2014;20:0. [Google Scholar]
- 21.Evaluation of metoprolol versus diltiazem for rate control of atrial fibrillation in the emergency department. McGrath P, Kersten B, Chilbert MR, Rusch C, Nadler M. Am J Emerg Med. 2021;46:585–590. doi: 10.1016/j.ajem.2020.11.039. [DOI] [PubMed] [Google Scholar]
- 22.Rate control with intravenous diltiazem, verapamil, and metoprolol in acute atrial fibrillation with rapid ventricular rate. Medeiros T, Bui V, Almekdash MH, Keesari R, Lee YR. SAGE Open Med. 2021;9 doi: 10.1177/20503121211017756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Which one is the first choice for rapid ventricular rate atrial fibrillation in emergency department: metoprolol or diltiazem? A randomized clinical trial. Memiş MB, Rohat AK, Öztürk TC, Özge ON, Özgür OR. J Surg Med. 2019;27:13–17. [Google Scholar]
- 24.Hemodynamic comparison of intravenous push diltiazem versus metoprolol for atrial fibrillation rate control. Nicholson J, Czosnowski Q, Flack T, Pang PS, Billups K. Am J Emerg Med. 2020;38:1879–1883. doi: 10.1016/j.ajem.2020.06.034. [DOI] [PubMed] [Google Scholar]
- 25.Evaluation of the blood pressure effects of diltiazem versus metoprolol in the acute treatment of atrial fibrillation with rapid ventricular rate. Nuñez Cruz S, DeMott JM, Peksa GD, Slocum GW. Am J Emerg Med. 2021;46:329–334. doi: 10.1016/j.ajem.2020.10.003. [DOI] [PubMed] [Google Scholar]
- 26.Intravenous metoprolol versus diltiazem for rate control in noncardiac, nonthoracic postoperative atrial fibrillation. Personett HA, Smoot DL, Stollings JL, Sawyer M, Oyen LJ. Ann Pharmacother. 2014;48:314–319. doi: 10.1177/1060028013512473. [DOI] [PubMed] [Google Scholar]
- 27.Intravenous metoprolol versus diltiazem for rate control in atrial fibrillation. Xiao SQ, Ibarra F Jr, Cruz M. Ann Pharmacother. 2022;56:916–921. doi: 10.1177/10600280211056356. [DOI] [PubMed] [Google Scholar]
- 28.Rate control management of atrial fibrillation with rapid ventricular response in the emergency department. Wong BM, Green MS, Stiell IG. Can J Cardiol. 2020;36:509–517. doi: 10.1016/j.cjca.2019.08.040. [DOI] [PubMed] [Google Scholar]
- 29.2011 ACCF/AHA/HRS focused updates incorporated into the ACC/AHA/ESC 2006 guidelines for the management of patients with atrial fibrillation: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Fuster V, Rydén LE, Cannom DS, et al. Circulation. 2011;123:0–367. doi: 10.1161/CIR.0b013e318214876d. [DOI] [PubMed] [Google Scholar]
- 30.Canadian Cardiovascular Society atrial fibrillation guidelines 2010: management of recent-onset atrial fibrillation and flutter in the emergency department. Stiell IG, Macle L. Can J Cardiol. 2011;27:38–46. doi: 10.1016/j.cjca.2010.11.014. [DOI] [PubMed] [Google Scholar]
- 31.An international view of how recent-onset atrial fibrillation is treated in the emergency department. Rogenstein C, Kelly AM, Mason S, Schneider S, Lang E, Clement CM, Stiell IG. Acad Emerg Med. 2012;19:1255–1260. doi: 10.1111/acem.12016. [DOI] [PubMed] [Google Scholar]
- 32.Intravenous diltiazem versus metoprolol for atrial fibrillation with rapid ventricular rate: a meta-analysis. Lan Q, Wu F, Han B, Ma L, Han J, Yao Y. Am J Emerg Med. 2022;51:248–256. doi: 10.1016/j.ajem.2021.08.082. [DOI] [PubMed] [Google Scholar]