Abstract
Studies on the prognostic importance of tumor-infiltrating lymphocytes have mainly focused on T cells, while little is known about the role of tumor-infiltrating B lymphocytes. We investigated the prevalence of CD20+ B cells by immunohistochemistry in primary melanoma samples of 106 patients and analyzed in relation to clinicopathological parameters and patients’ survival. The majority of samples contained a significant amount of B lymphocytes, predominantly dispersed in the stroma surrounding tumor deposits (mean peritumoral and intratumoral densities: 178.7 ± 156.1 vs. 4.9 ± 6.9 cells/mm2, respectively). B cells organized in follicle-like aggregates were also observed in 26% of the samples. B-cell density correlated with that of activated (CD25+ or OX40+) T lymphocytes. Infiltration by CD20+ lymphocytes did not correlate with tumor thickness, while the presence of B-cell aggregates was observed more frequently in thick melanomas. On the other hand, B-cell infiltration was more pronounced in nonmetastatic or lymph node metastatic tumors, compared to visceral metastatic ones. Accordingly, high number of these cells provided significant survival advantage (P = 0.0391 and P = 0.0136 for intra- and peritumoral infiltration, respectively). Furthermore, combination of peritumoral B-cell density with the number of activated T lymphocytes identified patient subgroups with different disease outcome, which was most favorable in the case of high density, while very poor in the case of low density of both cell types. Multivariate survival analysis identified tumor thickness and CD20+/OX40+ cell density combination as significant independent prognostic factors. Taken together, our results show correlation between low number of CD20+ B lymphocytes and melanoma progression, indicating a possible role of tumor-infiltrating B cells in antitumoral immune response. It was also reflected in better outcome of the disease since the density of B lymphocytes alone as well as in combination with that of activated T cells proved of prognostic importance in patients with malignant melanoma.
Keywords: Melanoma, Metastasis, Survival, B cell, Immunohistochemistry
Introduction
Human solid tumors often contain infiltrating lymphocytes (TIL), potentially reflecting an ongoing host immune response to the tumor. The presence of a lymphoid infiltrate (without distinction of lymphocyte types) or the intensity of T-cell infiltration has been shown to correlate with favorable prognosis in a variety of human cancers [1–5]. Several studies revealed differential prognostic impact of the lymphocyte subsets (e.g., CD4+ or CD8+), as well as the importance of distinguishing TILs according to location within the tumor [3, 6, 7].
In the case of cutaneous melanoma, the published results are also contradictory; while some investigators reported that a prominent lymphocytic infiltrate, especially in the vertical growth phase, was associated with good prognosis [8, 9], others found no significant correlation [10, 11]. Few reports have been published on immunohistochemical evaluation of lymphocyte subpopulations [12].
In most tumor types, including melanoma, lymphocytic infiltrates consist largely of T cells, with considerably lower numbers of B- and NK cells. A notable exception is medullary carcinoma of the breast, characterized by a prominent lymphoplasmacytic infiltrate that has been correlated with favorable prognosis [13]. However, significant extent of infiltration by B lymphocytes was also reported in the case of several other types of cancer [5, 14–16].
Earlier works evaluating the composition of the inflammatory infiltrate in melanoma reported the absence or infrequent presence of B lymphocytes [17, 18]. More recent studies also found low numbers of infiltrating B cells, compared to the amount of T lymphocytes, in primary melanomas [12, 19]. The prognostic significance of their presence has been evaluated in only one study involving 58 patients with cutaneous melanoma, finding no significant relationship between the amount of infiltrating B cells and survival [12].
In our earlier studies on patients with cutaneous melanoma, infiltration by T cells expressing the activation markers CD25 and OX40 [20], high peritumoral density of DC-LAMP+ mature DCs, as well as combinations of high DC densities with high numbers of activated T lymphocytes [21] were associated with longer survival of the patients. These results suggest that the presence of activated T cells and antigen presenting DCs, cell types of crucial importance in cellular immune reactions, at the primary site could be a marker of a functional immune response against melanoma progression and influence the outcome of the disease. In the present work, we extended our studies to B lymphocytes that have not been extensively studied in cutaneous melanoma, similarly to most other tumor types. We investigated the prevalence of B lymphocytes expressing CD20 by immunohistochemistry in primary tumor samples obtained from 106 patients with cutaneous melanoma. B-cell density results were evaluated with regard to their association with tumor thickness, the development of metastases, patients’ survival, and other clinicopathological parameters, as well as with the density of activated T cells.
Materials and methods
Patient characteristics
Archival tissue samples were obtained from 106 patients with primary cutaneous melanoma who underwent surgery between 1980 and 2001 at the National Institute of Oncology, and at the Institute of Dermato-Venerology, Semmelweis University, Budapest. The study was approved by the ethics committees of both institutions. Samples were selected to obtain a study group involving a higher number of medium thick or thick (>1.0 mm) melanoma samples than their normal ratio, which have a more uncertain prognosis than thin tumors. Prior to surgery, none of the patients received any antitumor treatment. All surviving patients had follow-up data for at least 5 years. Clinical and pathological characteristics are summarized in Table 1. Tumors were grouped into four thickness categories based on the 6th edition of AJCC (American Joint Committee on Cancer) Cancer Staging Manual [22] (≤1.0 mm, 1.01–2.0 mm, 2.01–4.0 mm, >4.0 mm), and into three categories according to disease progression during the follow-up period (nonmetastatic, lymph node metastatic, visceral metastatic). Distribution according to stages [22] was as follows: st. IA, 16; IB, 13; IIA, 23; IIB, 30; IIC, 17; IIIA, 6; IIIB, 1. Fifty-three patients had no metastases developed during the follow-up period, while 16 patients had metastases confined to regional lymph nodes, which were excised. Thirty-seven patients developed distant visceral metastases. The 5-year survival of patients in both the nonmetastatic and the lymph node metastatic groups was 100%, while only 2 patients developing distant visceral metastases survived for more than 5 years (62 and 72 months); no patients died of melanoma-unrelated causes. Tumors with clinical regression and/or histological signs of extensive regression were not included in the study.
Table 1.
Patient and tumor characteristics
| Patient group | All patients | Nonmetastatic | LN metastatic* | Visceral metastatic |
|---|---|---|---|---|
| Age—median (range) | 53 (16–76) | 53 (27–76) | 52 (32–76) | 55 (16–76) |
| Sex | ||||
| Male | 45 | 19 | 9 | 17 |
| Female | 61 | 34 | 7 | 20 |
| Location | ||||
| Extremities | 42 | 23 | 5 | 14 |
| Trunk | 57 | 28 | 9 | 20 |
| Head | 7 | 2 | 2 | 3 |
| Type | ||||
| SSM | 66 | 38 | 9 | 19 |
| NM | 37 | 14 | 6 | 17 |
| ALM | 2 | 1 | 1 | – |
| LMM | 1 | – | – | 1 |
| Thickness (mm) | ||||
| <1.0 | 17 | 15 | 2 | – |
| 1.01–2.0 | 23 | 11 | 5 | 7 |
| 2.01–4.0 | 38 | 17 | 5 | 16 |
| >4.0 | 28 | 10 | 4 | 14 |
| Ulceration | ||||
| Present | 46 | 17 | 6 | 23 |
| Absent | 60 | 36 | 10 | 14 |
| 5-year survival (%) | 71/106 (67) | 53/53 (100) | 16/16(100) | 2/37(5) |
SSM superficial spreading melanoma, NM nodular melanoma, ALM acral lentiginous melanoma, LM lentigo maligna melanoma
* Only regional lymph node metastases during the follow-up period (5 years)
Immunohistochemical detection of B cells in melanoma samples
In this study, 3-μm sections from formalin-fixed, paraffin-embedded cutaneous melanoma samples were used. Immunohistochemistry was performed on deparaffinated sections after microwave antigen retrieval. Endogenous peroxidase activity was blocked with incubation of the slides in 3% H2O2 in methanol, and nonspecific binding sites were blocked with 20% goat serum. Monoclonal anti-CD20cy (clone L26, Dako, Glostrup, Denmark; diluted 1:100) was used as primary antibody and mouse IgG2a (Sigma, St. Louis, MO) for negative control. Biotinylated anti-mouse/anti-rabbit Ig was used as secondary reagent, followed by Streptavidin-peroxidase treatment (LSAB2 System, HRP; Dako). Antibody binding was visualized with 3-amino-9-ethylcarbazole (AEC; Vector Laboratories, Inc., Burlingame, CA), and then the slides were counterstained with hematoxylin. Double staining for CD20 and CD25 or CD134 was performed in a subset of cases. Incubation with the first primary antibody (monoclonal anti-CD25, Novocastra Laboratories, Newcastle upon Tyne, UK, or anti-CD134, PharMingen, San Diego, CA) was followed by biotin/Streptavidin-peroxidase treatment (LSAB2 System, HRP; Dako), using Vector SG as chromogen (Vector Laboratories). Then the second primary antibody was applied (monoclonal anti-CD20cy, Dako) and developed by Streptavidin–alkaline phosphatase treatment (LSAB2 System, Alkaline Phosphatase; Dako), using fuchsin as chromogen (Vector Laboratories).
Evaluation of the immune reactions
Slides were examined using a graticule of 10 × 10 squares, calibrated as 0.25 mm2 at 200× magnification. Counting was performed independently by two investigators (AL and JK, both blinded to the clinical information), and the mean value of their separate counts was used for the analysis. Because the distribution of stained cells in the tumors was heterogeneous, the entire tumor area was analyzed in every case, and density of positive cells/mm2 is given. Areas of B-cell aggregates, when present (in 26% of samples), were not taken in account for the evaluation because of the difficulty of the accurate determination of B-cell number in these areas, resulting from the extremely high cell density and overlapping cell borders. The number of CD20+ cells was registered separately in intratumoral (lymphocytes infiltrating melanoma cell nests) and peritumoral areas (lymphocytes distributed in the infiltrate along the margin and the base of melanomas). The proportion of patients with significant density of CD20+ cells was also calculated, using cutoff values set up separately for intra- and peritumoral localization (3 and 170 cells/mm2, respectively), based on the mean of the given variable in the whole patient group, with minor modification for higher discriminative power. Density values of T cells expressing the activation markers CD25 or OX40 derived from our previous paper [20]. Cutoff levels used for peritumoral CD25+ and OX40+ cells were 75 and 20 cells/mm2, respectively.
Statistical analysis
Comparisons between cell densities in different tumor groups were made using the Mann–Whitney U test, while χ2 test was used for comparing the proportions of samples with high cell densities. Associations between tumor thickness and cell densities and between the densities of the different cell types were evaluated by the Pearson test. Univariate analysis of survival was performed by the Kaplan–Meier method, and the statistical analysis was carried out by the Mantel–Cox test. In multivariate analysis, independent prognostic factors were determined by the Cox proportional hazards model. All statistics were calculated using the BMDP Statistical Software Pack.
Results
Detection of B lymphocytes in melanoma samples
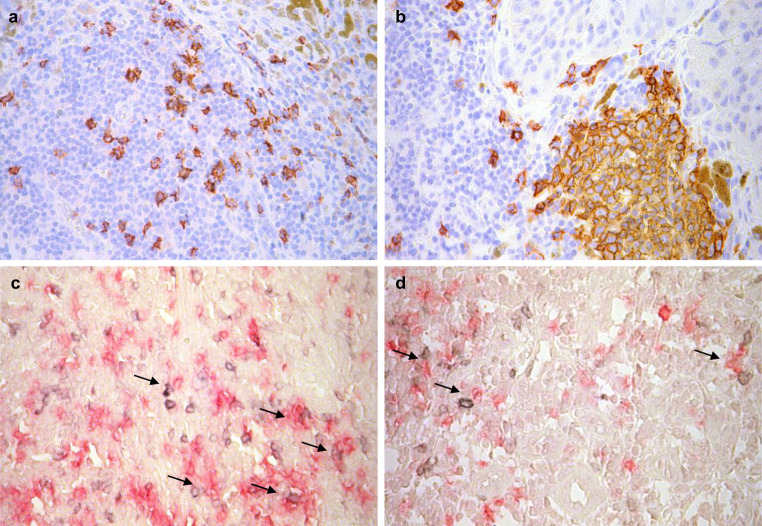
By immunohistochemical examination of 106 primary melanoma samples, CD20 expression was detected predominantly on lymphocytes dispersed in the stroma surrounding tumor deposits (Fig. 1a). Adjacent to tumor cell nests, B cells clustered in dense aggregates resembling follicles (Fig. 1b), ranging in size from approximately 0.1–0.8 mm, were also observed in 28 of 106 samples (26%).
Fig. 1.
CD20+ B lymphocytes (AEC, red) dispersed in the infiltrate (a) and clustered in dense aggregate (b) in melanoma. Double staining for OX40 or CD25 (developed by Vector SG, gray signal) and CD20 (developed by fuchsin, red signal). CD20+ B cells can be seen in close contact with CD25+ (c) and OX40+ (d) T lymphocytes (arrows). Pictures were taken using ×40 objective
The density of CD20+ lymphocytes was determined distinguishing intratumoral (lymphocytes infiltrating the melanoma cell nests) and peritumoral infiltrate (lymphocytes surrounding the tumor deposits). In the majority of cases, peritumoral density of labeled cells greatly exceeded their intralesional density, with a 36-fold difference in average (mean ± SD, 178.7 ± 156.1 vs. 4.9 ± 6.9 cells/mm2). All samples contained at least a few stromal CD20+ lymphocytes, their density being higher than 10 cells/mm2 in most cases (91/106, 86%), while intratumoral B-cell infiltration was below 1 cell/mm2 in 66 of 106 cases (62%).
Double staining for CD20 and the T-cell activation markers CD25 or OX40 demonstrated the association of B cells with activated T lymphocytes (Fig. 1c, d). Furthermore, significant correlations were found between peritumoral density of B cells and activated T lymphocytes (r = 0.3062, P < 0.02 and r = 0.4105, P < 0.001 for CD25+ and OX40+ cells, respectively; n = 67) where density values for activated T cells derived from our previous work [20].
Correlation of B-cell density with clinicopathologic parameters
The intensity of infiltration by CD20+ lymphocytes did not correlate with the thickness of melanomas (intratumoral: r = −0.0723, peritumoral: r = 0.0730; P > 0.05). For intra- and peritumoral B-cell densities, cutoff values of 3 and 170 cells/mm2 were introduced, respectively (see in “Materials and methods”), and the proportion of melanomas with “significant cell density”, defined as higher than the cutoff value, was calculated. Using these cutoff values, the distribution of patients with significant intra- or peritumoral infiltration by CD20+ cells was analyzed according to clinicopathologic parameters (Table 2). A lower prevalence of melanomas with high peritumoral B-cell density was observed for extremity tumors compared to axial location, while there was no significant difference in the case of other patient or tumor characteristics as patient age and gender or histological type and ulceration of the tumor. On the other hand, the organization of B lymphocytes in follicle-like structures was observed more frequently in thick melanomas, in patients over 53 years and in tumors of axial location (Table 2).
Table 2.
Proportion of patients with significant B-cell density in groups with different patient and tumor characteristics
| Patient no. | Intratumoral (>3 cells/mm2) | Peritumoral (>170 cells/mm2) | Presence of B-cell aggregates | ||||
|---|---|---|---|---|---|---|---|
| No. (%) | P | No. (%) | P | No. (%) | P | ||
| All patients | 106 | 45 (42) | 42 (40) | 28 (26) | |||
| Age | |||||||
| <53 years | 53 | 26 (49) | 20 (38) | 9 (17) | |||
| >53 years | 53 | 19 (36) | n.s. | 22 (42) | n.s. | 19 (36) | 0.0276 |
| Sex | |||||||
| Male | 45 | 21 (47) | 19 (42) | 15 (33) | |||
| Female | 61 | 24 (39) | n.s. | 23 (38) | n.s. | 13 (21) | n.s. |
| Location | |||||||
| Extremities | 42 | 19 (45) | 10 (24) | 6 (14) | |||
| Axial (trunk + head) | 64 | 26 (41) | n.s. | 32 (50) | 0.0070 | 22 (34) | 0.0218 |
| Type# | |||||||
| SSM | 29 | 10 (34) | 12 (41) | 8 (28) | |||
| NM | 36 | 17 (47) | n.s. | 17 (47) | n.s. | 14 (39) | n.s. |
| Thickness (mm) | |||||||
| <1.0 | 17 | 6 (35) | 6 (35) | 1 (6) | |||
| 1.01–2.0 | 23 | 12 (52) | 7 (30) | 5 (22) | |||
| 2.01–4.0 | 38 | 17 (45) | 15 (39) | 10 (26) | |||
| >4.0 | 28 | 10 (36) | n.s. | 14 (50) | n.s. | 12 (43) | 0.0494 |
| Ulceration | |||||||
| Present | 46 | 18 (39) | 17 (37) | 14 (30) | |||
| Absent | 60 | 27 (45) | n.s. | 25 (42) | n.s. | 14 (23) | n.s. |
| Metastatic pattern | |||||||
| Nonmetastatic + LN metastatic | 69 | 35 (51) | 34 (49) | 16 (23) | |||
| Visceral metastatic | 37 | 10 (27) | 0.0186 | 8 (22) | 0.0055 | 12 (32) | n.s. |
| Survival | |||||||
| >5 years | 71 | 35 (49) | 34 (48) | 16 (23) | |||
| <5 years | 35 | 10 (29) | 0.0423 | 8 (23) | 0.0132 | 12 (34) | n.s. |
n.s. Not significant, SSM superficial spreading melanoma, NM nodular melanoma, ALM acral lentiginous melanoma, LM lentigo maligna melanoma
#ALM (2) and LMM (1) cases are not shown; only for cases >2.0 mm
The intensity of B-cell infiltration was also compared in tumors that either did not metastasize or gave only regional lymph node metastases during the follow-up period (5 years) with those developing visceral metastases. Nonmetastatic and lymph node metastatic cases were evaluated together, because there was no significant difference in their B-cell density values (data not shown), and the relative malignancy of the disease, reflected by survival data, was identical in patients belonging to these two groups (100% 5-year survival). Both intra- and peritumoral infiltration by CD20+ lymphocytes were more pronounced in nonmetastatic or lymph node metastatic tumors, compared to visceral metastatic ones (Fig. 2). Similarly, the proportion of patients with significant intra- or peritumoral B-cell density exhibited approximately twofold differences between the two patient groups (Table 2). The appearance of B-cell follicles was similar in the tumor groups irrespectively of metastatic pattern.
Fig. 2.
B-cell density according to metastasis formation. Data are presented as mean and SEM of CD20+ cell density
Survival analysis according to B-cell and activated T-cell density
Kaplan–Meier analysis according to the density of CD20+ lymphocytes, using the same cutoff levels as in the comparisons described above, revealed that high number of these cells provided significant survival advantage (Fig. 3a, b). The percentage of patients with more than 5 years survival was higher in the case of high intra- or peritumoral B-cell density (78% vs. 59% and 81% vs. 58%, respectively; Table 2). The presence of B-cell aggregates did not show association with survival.
Fig. 3.
Kaplan–Meier survival curves for melanoma patients, subdivided according to the intratumoral (a) or peritumoral (b) B-cell density, or to peritumoral densities of CD20+ and CD25+ (c) or CD20+ and OX40+ cells (d)
In our previous paper [20], we have demonstrated the prognostic significance of peritumoral infiltration by T lymphocytes expressing CD25 or OX40 markers. Although density values for B cells and activated T cells showed strong correlations (as shown above), high density samples for the different cell populations did not completely overlap. Therefore, it was possible to evaluate survival curves for patient subgroups characterized by different combinations of high or low peritumoral B-cell and activated T-cell densities. Kaplan–Meier analysis evaluating all potential subgroups separately resulted in significant differences in the case of both CD25 and OX40 (Fig. 3c, d). Low peritumoral B-cell density values combined with low activated T lymphocyte numbers identified a subgroup of patients with strikingly poor survival (36% 5-year survival for both markers; P = 0.0004 in Kaplan–Meier analysis comparing these subgroups with all others), while high B-cell/high activated T-cell density groups fared best (85 and 86% 5-year survival for CD25 and OX40, respectively).
When all these parameters (density values for B lymphocytes and activated T cells, as well as B-cell/T-cell marker combinations) were tested in multivariate analysis, together with other prognostic factors (tumor thickness, localization, histological type, ulceration, patients’ age and sex), tumor thickness (relative risk: 1.275, P = 0.000), and low CD20+/low OX40+ combination (relative risk: 1.696, P = 0.001) proved significant independent predictors of poor prognosis.
Discussion
Malignant melanoma of the skin is considered one of the most immunogenic among human neoplasms. The overwhelming majority of investigations of the phenotype and functional activity of TILs in melanoma, as in other tumor types, have focused on T lymphocytes, while considerably less is known about tumor-infiltrating B cells.
Although T lymphocytes undoubtedly predominate in melanoma infiltrates and early studies, generally performed on small patient cohorts, described the absence or rare presence (<2%) of B cells [17, 18], more recent works reported frequencies between ~15 and 20% of all infiltrating lymphocytes [12, 19]. In our cohort of 106 patients, we found significant amount of B cells in the peritumoral infiltrate in the majority of samples, while only a small fraction of the cells infiltrated the melanoma cell nests. We did not evaluate the prevalence of B cells as a percentage of all infiltrating lymphocytes, but comparing B-cell and T-cell density values based on our earlier work [23] on a subset (n = 52) of samples used in the present study yields an average percentage value of 16%, in the same range as observed in recent studies cited above [12, 19].
In some earlier works, efforts were made to evaluate the prevalence of B lymphocytes according to a few selected characteristics of melanomas [12, 19]. To the best of our knowledge, however, ours is the first study that comprehensively analyzed the associations of B-cell infiltration with several clinicopathologic factors in a relatively large patient cohort. The number of CD20+ lymphocytes did not show correlation with the studied patient and tumor parameters, with the exception of tumor site: melanomas on the trunk or head contained a significant peritumoral B-cell infiltrate more frequently than those located to the extremities. The reason for this difference is not clear; an earlier study evaluating overall TIL density did not describe such an association [11], while B-cell infiltration has not been evaluated in this respect.
Our study confirmed the presence of significant, in some cases impressive density of B lymphocytes in infiltrates of primary cutaneous melanoma. Similarly, considerable numbers of infiltrating B cells were observed in the case of several other tumor types [5, 14–16]. However, it is not clear whether the increased amount of B cells is a consequence of tumor antigen-specific humoral immune response or that of nonspecific recruitment by inflammatory chemoattractants in the tumor microenvironment. Signs of antigen-selected B-cell response have been documented in studies applying immunoglobulin gene analysis on tumor tissues from several types of cancer [15, 24–28]. Tumor-reactive B cells have been cloned from a number of human tumors including melanoma [29–31].
In a recent publication, the potential importance of tertiary lymphoid structures, consisting of clusters of T lymphocytes with adjacent B-cell follicles, was emphasized in lung carcinoma [32]. Moreover, mature dendritic cells (DCs) were shown to localize preferentially to these lymphoid structures, and their density was found to be associated with patients’ survival. Similar structures or B-cell follicles have also been observed in a number of tumor types such as colorectal, hepatocellular, breast and ovarian carcinoma and uveal melanoma [7, 14, 15, 27, 28, 33], but this phenomenon has not been described in cutaneous melanoma. In our patient group, we observed the presence of B lymphocytes organized in follicle-like structures in 26% of samples. The presence of B-cell aggregates was more prevalent in thick melanomas, in tumors of axial location and in patients over 53 years, but no correlation was observed with the metastatic pattern or with patients’ survival. Nonetheless, in our earlier study, on patients with cutaneous melanoma, high density of DC-LAMP+ mature DCs proved indicator of favorable prognosis [21]. However, we did not notice correlation between the presence or absence of B-cell aggregates and DC-LAMP+ DCs. In some of the above mentioned tumor types, the presence of follicular dendritic cells (FDCs) in B-cell follicles, resembling ectopic germinal centers, was also mentioned [15, 27, 28, 32]. In our melanoma samples, we found CD21+ FDC network in only 3 of 15 cases studied (not shown). The presence of extranodal lymphoid follicles in tumors could also be consistent with the hypothesis that at least a portion of tumor-infiltrating B cells are result of in situ antigen-driven expansion instead of nonspecific accumulation.
The clinical significance of the above findings is not clear, and it is still a matter of debate how systemic B-cell response or in situ B-cell accumulation influence the biological behavior of tumors. Experimental data obtained in a transgenic mouse carcinogenesis model indicate a role of B cells in contributing to epithelial cancer development via promotion of the establishment of chronic inflammation by B-cell derived factors [34]. Moreover, enhanced antitumor immunity and reduced growth or progression of experimental tumors was observed in B-cell deficient of depleted mice [35–37]. However, other studies on murine tumors yielded the opposite results, namely, impaired T-cell response and enhanced tumor growth in the absence of B lymphocytes [38, 39]. The discrepancy regarding the systemic pro- or antitumor effects of B lymphocytes may be related to the diversity of their functional activities; they can be involved in several phases of the immune reactions via a plethora of mechanisms from antigen presentation through antibody production to the regulation of the activity of other immune cells [16]. The potential tumor-promoting role of antibodies or immune complexes has long been known, and the ability of B cells to negatively regulate immune responses through the secretion of inhibitory factors is also documented [40–42]. On the other hand, B lymphocytes may function as effective antigen presenting cells promoting antitumor T-cell response [43, 44]. A critical contribution of B lymphocytes to the optimal activation of CD4+ memory T cells has been demonstrated in experiments using B-cell deficient mice [45, 46]. One of the mechanisms proposed for B lymphocyte-mediated CD4+ T-cell expansion is costimulation via OX40L expressed by activated B cells [47]. Our findings of strong correlation between the densities of B cells and lymphocytes expressing T-cell activation markers CD25 and especially OX40, as well as their colocalization may suggest a possibility of B cells playing a role in antigen presentation and costimulation of T lymphocytes in primary melanomas.
The clinical relevance of contrasting findings obtained in experimental models evaluating the pro- or antitumor effects of B cells can be judged on the basis of studies on the prognostic effect of systemic B-cell response in cancer patients, but the results of these are controversial [48]. Regarding a potential prognostic significance of tumor-infiltrating B lymphocytes, their number was correlated with longer survival times in some studies [4, 16, 49].
In our present study on melanoma patients, both intra- and peritumoral CD20+ cell densities were found associated with the outcome of the disease, with significantly higher values in cases that did not develop visceral metastases during the 5-year follow-up period. Consequently, infiltration by B lymphocytes correlated with patient survival in univariate analysis. These differences were even more pronounced (data not shown) when only melanomas thicker than 1.0 mm were included in the study, representing a group characterized with a more heterogeneous metastatic potential and prognosis compared to thin tumors. To the best of our knowledge, this is the first report on the prognostic significance of the prevalence of B lymphocytes infiltrating human cutaneous melanoma. An earlier study involving a smaller number of patients found no significant relationship between the amount of infiltrating B cells and survival [12]. The difference in the size of the studied patient cohorts or methodological differences (i.e., evaluating cell density in a few randomly chosen areas vs. in the whole tumor area in our study) could account for this discrepancy.
We also evaluated the prognostic effect of combination of B-cell and activated T-lymphocyte density values, resulting in patient subgroups with markedly different survival where combinations of low B-cell/low activated T lymphocyte density predicted strikingly poor prognosis compared to other subgroups. In our earlier studies, high peritumoral densities of CD25+ and OX40+ lymphocytes alone [20] and in combination with high numbers of antigen presenting dendritic cells [21] proved predictors of favorable disease outcome, which we considered as a sign of the presence of an “immunological functional unit” of antigen presenting dendritic cells and activated T cells in primary melanoma. Our present findings suggest that B lymphocytes infiltrating cutaneous melanomas may also be involved in this functional unit, potentially as antigen presenting cells whose presence carries prognostic information similarly to that of dendritic cells.
In conclusion, we have shown that an increased density of B lymphocytes infiltrating primary cutaneous melanomas was associated with a lower occurrence of distant metastases and longer survival of patients. Combination of peritumoral B-cell density with the number of activated T lymphocytes identified patient subgroups with different disease outcome, with strikingly poor prognosis in the case of low density of both cell types. Our results suggest a possible role of tumor-infiltrating B cells in a functional immune response against melanoma, reflected in better outcome of the disease.
Acknowledgments
The authors thank K. Derecskei, I. Sinka and M. Kónya (National Institute of Oncology, Budapest) for their excellent technical assistance. The study was supported by the National Scientific Research Fund OTKA 72836 (AL), Hungarian Ministry of Health grant ETT 308/2003 (AL), and NKFP1a-0024-05 (JT).
References
- 1.Vesalainen S, Lipponen P, Talja M, Syrjanen K. Histological grade, perineural infiltration, tumour-infiltrating lymphocytes and apoptosis as determinants of long-term prognosis in prostatic adenocarcinoma. Eur J Cancer. 1994;30A:1797–1803. doi: 10.1016/0959-8049(94)E0159-2. [DOI] [PubMed] [Google Scholar]
- 2.Setälä LP, Kosma VM, Marin S, Lipponen PK, Eskelinen MJ, Syrjanen KJ, Alhava EM. Prognostic factors in gastric cancer: the value of vascular invasion, mitotic rate and lymphoplasmacytic infiltration. Br J Cancer. 1996;74:766–772. doi: 10.1038/bjc.1996.434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Galon J, Costes A, Sanchez-Cabo F, Kirilovsky A, Mlecnik B, Lagorce-Pagès C, Tosolini M, Camus M, Berger A, Wind P, Zinzindohué F, Bruneval P, Cugnenc P-H, Trajanoski Z, Fridman W-H, Pagès F. Type, density, and location of immune cells within human colorectal tumors predict clinical outcome. Science. 2006;313:1960–1964. doi: 10.1126/science.1129139. [DOI] [PubMed] [Google Scholar]
- 4.Al-Shibli KI, Donnem T, Al-Saad S, Persson M, Bremnes RM, Busund L-T. Prognostic effect of epithelial and stromal lymphocyte infiltration in non-small cell lung cancer. Clin Cancer Res. 2008;14:5220–5227. doi: 10.1158/1078-0432.CCR-08-0133. [DOI] [PubMed] [Google Scholar]
- 5.Lee HE, Chae SW, Lee YJ, Kim MA, Lee HS, Lee BL, Kim WH. Prognostic implications of type and density of tumour-infiltrating lymphocytes in gastric cancer. Br J Cancer. 2008;99:1704–1711. doi: 10.1038/sj.bjc.6604738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Naito Y, Saito K, Shiiba K, Ohuchi A, Saigenji K, Nagura H, Ohtani H. CD8+ T cells infiltrated within cancer cell nests as a prognostic factor in human colorectal cancer. Cancer Res. 1998;58:3491–3494. [PubMed] [Google Scholar]
- 7.Sato E, Olson SH, Ahn J, Bundy B, Nishikawa H, Qian F, Jungbluth AA, Frosina D, Gnjatic S, Ambrosone C, Kepner J, Odunsi T, Ritter G, Lele S, Chen Y-T, Ohtani H, Old LJ, Odunsi K. Intraepithelial CD8+ tumor-infiltrating lymphocytes and a high CD8+/regulatory T cell ratio are associated with favorable prognosis in ovarian cancer. Proc Natl Acad Sci USA. 2005;102:18538–18543. doi: 10.1073/pnas.0509182102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Clark WH, Jr, Elder DE, Guerry D, IV, Braitman LE, Trock BJ, Schultz D, Synnestvedt M, Halpern AC. Model predicting survival in stage I melanoma based on tumor progression. J Natl Cancer Inst. 1989;81:1893–1904. doi: 10.1093/jnci/81.24.1893. [DOI] [PubMed] [Google Scholar]
- 9.Clemente CG, Mihm MC, Jr, Bufalino R, Zurrida S, Collini P, Cascinelli N. Prognostic value of tumor infiltrating lymphocytes in the vertical growth phase of primary cutaneous melanoma. Cancer. 1996;77:1303–1310. doi: 10.1002/(SICI)1097-0142(19960401)77:7<1303::AID-CNCR12>3.0.CO;2-5. [DOI] [PubMed] [Google Scholar]
- 10.Barnhill RL, Fine JA, Roush GC, Berwick M. Predicting five-year outcome for patients with cutaneous melanoma in a population-based study. Cancer. 1996;78:427–432. doi: 10.1002/(SICI)1097-0142(19960801)78:3<427::AID-CNCR8>3.0.CO;2-G. [DOI] [PubMed] [Google Scholar]
- 11.Taylor RC, Patel A, Panageas KS, Busam KJ, Brady MS. Tumor-infiltrating lymphocytes predict sentinel lymph node positivity in patients with cutaneous melanoma. J Clin Oncol. 2007;25:869–875. doi: 10.1200/JCO.2006.08.9755. [DOI] [PubMed] [Google Scholar]
- 12.Hillen F, Beaten CIM, van de Winkel A, Creytens D, van der Schaft DWJ, Winnepenninckx V, Griffioen AW. Leukocyte infiltration and tumor cell plasticity are parameters of aggressiveness in primary cutaneous melanoma. Cancer Immunol Immunother. 2008;57:97–106. doi: 10.1007/s00262-007-0353-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ridolfi RL, Rosen PP, Port A, Kinne D, Miké V. Medullary carcinoma of the breast: a clinicopathologic study with 10 year follow-up. Cancer. 1977;40:1365–1385. doi: 10.1002/1097-0142(197710)40:4<1365::AID-CNCR2820400402>3.0.CO;2-N. [DOI] [PubMed] [Google Scholar]
- 14.Whelchel JC, Farah SE, McLean IW, Burnier MN. Immunohistochemistry of infiltrating lymphocytes in uveal malignant melanoma. Invest Ophthalmol Vis Sci. 1993;34:2603–2606. [PubMed] [Google Scholar]
- 15.Coronella-Wood JA, Hersh EM. Naturally occurring B-cell responses to breast cancer. Cancer Immunol Immunother. 2003;52:715–738. doi: 10.1007/s00262-003-0409-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nelson BH. CD20+ B cells: the other tumor-infiltrating lymphocytes. J Immunol. 2010;185:4977–4982. doi: 10.4049/jimmunol.1001323. [DOI] [PubMed] [Google Scholar]
- 17.Hersey P, Murray E, Grace J, McCarthy WH. Current research on immunopathology of melanoma: analysis of lymphocyte populations in relation to antigen expression and histological features of melanoma. Pathology. 1985;17:385–391. doi: 10.3109/00313028509105490. [DOI] [PubMed] [Google Scholar]
- 18.Ralfkaier E, Hou-Jensen K, Gatter KC, Drzewiecki KT, Mason DY. Immunohistological analysis of the lymphoid infiltrate in cutaneous malignant melanomas. Virchow Arch A. 1987;410:355–361. doi: 10.1007/BF00711292. [DOI] [PubMed] [Google Scholar]
- 19.Hussein MR, Elsers DAH, Fadel SA, Omar A-EM. Immunohistological characterization of tumour infiltrating lymphocytes in melanocytic skin lesions. J Clin Pathol. 2006;59:316–324. doi: 10.1136/jcp.2005.028860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ladányi A, Somlai B, Gilde K, Fejös Z, Gaudi I, Tímár J. T-cell activation marker expression on tumor-infiltrating lymphocytes as prognostic factor in cutaneous malignant melanoma. Clin Cancer Res. 2004;10:521–530. doi: 10.1158/1078-0432.CCR-1161-03. [DOI] [PubMed] [Google Scholar]
- 21.Ladányi A, Kiss J, Somlai B, Gilde K, Fejős Z, Mohos A, Gaudi I, Tímár J. Density of DC-LAMP+ mature dendritic cells in combination with activated T lymphocytes infiltrating primary cutaneous melanoma is a strong independent prognostic factor. Cancer Immunol Immunother. 2007;56:1459–1469. doi: 10.1007/s00262-007-0286-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Balch CM, Buzaid AC, Soong S-J, Atkins MB, Cascinelli N, Coit DG, Fleming ID, Gershenwald JE, Houghton A, Jr, Kirkwood JM, McMasters KM, Mihm MF, Morton DL, Reintgen DS, Ross MI, Sober A, Thompson JA, Thompson JF. Final version of the American Joint Committee on Cancer staging system for cutaneous melanoma. J Clin Oncol. 2001;19:3635–3648. doi: 10.1200/JCO.2001.19.16.3635. [DOI] [PubMed] [Google Scholar]
- 23.Kiss J, Tímár J, Somlai B, Gilde K, Fejős Z, Gaudi I, Ladányi A. Association of microvessel density with infiltrating cells in human cutaneous malignant melanoma. Pathol Oncol Res. 2007;13:21–31. doi: 10.1007/BF02893437. [DOI] [PubMed] [Google Scholar]
- 24.Hansen MH, Nielsen H, Ditzel HJ. The tumor-infiltrating B cell response in medullary breast cancer is oligoclonal and directed against the autoantigen actin exposed on the surface of apoptotic cancer cells. Proc Natl Acad Sci USA. 2001;98:12659–12664. doi: 10.1073/pnas.171460798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.O’Brien PM, Tsirimonaki E, Coomber DW, Millan DW, Davis JA, Campo MS. Immunoglobulin genes expressed by B-lymphocytes infiltrating cervical carcinoma show evidence of antigen-driven selection. Cancer Immunol Immunother. 2001;50:523–532. doi: 10.1007/s00262-001-0234-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Coronella JA, Tellemann P, Kingsbury GA, Truong TD, Hays S, Junghans RP. Evidence for an antigen-driven humoral immune response in medullary ductal breast cancer. Cancer Res. 2001;61:7889–7899. [PubMed] [Google Scholar]
- 27.Coronella JA, Spier C, Welch M, Trevor KT, Stopeck AT, Villar H, Hersh EM. Antigen-driven oligoclonal expansion of tumor-infiltrating B cells in infiltrating ductal carcinoma of the breast. J Immunol. 2002;169:1829–1836. doi: 10.4049/jimmunol.169.4.1829. [DOI] [PubMed] [Google Scholar]
- 28.Nzula S, Going JJ, Stott DI. Antigen-driven clonal proliferation, somatic hypermutation, and selection of B lymphocytes infiltrating human ductal breast carcinomas. Cancer Res. 2003;63:3275–3280. [PubMed] [Google Scholar]
- 29.Yeilding NM, Gerstner C, Kirkwood JM. Analysis of two human monoclonal antibodies against melanoma. Int J Cancer. 1992;52:967–973. doi: 10.1002/ijc.2910520623. [DOI] [PubMed] [Google Scholar]
- 30.Punt CJA, Barbuto JAM, Zhang H, Grimes WJ, Hatch KD, Hersh EM. Anti-tumor antibody produced by human tumor-infiltrating and peripheral blood B lymphocytes. Cancer Immunol Immunother. 1994;38:225–232. doi: 10.1007/BF01533513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kotlan B, Simsa P, Teillaud J-L, Fridman WH, Toth J, McKnight M, Glassy MC. Novel ganglioside antigen identified by B cells in human medullary breast carcinomas: the proof of principle concerning the tumor-infiltrating B lymphocytes. J Immunol. 2005;175:2278–2285. doi: 10.4049/jimmunol.175.4.2278. [DOI] [PubMed] [Google Scholar]
- 32.Dieu-Nosjean M-C, Antoine M, Danel C, Heudes D, Wislez M, Poulot V, Rabbe N, Laurans L, Tartour E, de Chaisemartin L, Lebecque S, Fridman W-H, Cadranel J. Long-term survival for patients with non–small-cell lung cancer with intratumoral lymphoid structures. J Clin Oncol. 2008;26:4410–4417. doi: 10.1200/JCO.2007.15.0284. [DOI] [PubMed] [Google Scholar]
- 33.Suzuki A, Masuda A, Nagata H, Kameoka S, Kikawada Y, Yamakawa M, Kasajima T. Mature dendritic cells make clusters with T cells in the invasive margin of colorectal carcinoma. J Pathol. 2002;196:37–43. doi: 10.1002/path.1018. [DOI] [PubMed] [Google Scholar]
- 34.de Visser KE, Korets LV, Coussens LM. De novo carcinogenesis promoted by chronic inflammation is B lymphocyte dependent. Cancer Cell. 2005;7:411–423. doi: 10.1016/j.ccr.2005.04.014. [DOI] [PubMed] [Google Scholar]
- 35.Brodt P, Gordon J. Anti-tumor immunity in B lymphocyte-deprived mice. I. immunity to a chemically induced tumor. J Immunol. 1978;121:359–362. [PubMed] [Google Scholar]
- 36.Qin Z, Richter G, Schüler T, Ibe S, Cao X, Blankenstein T. B cells inhibit induction of T cell-dependent tumor immunity. Nat Med. 1998;4:627–630. doi: 10.1038/nm0598-627. [DOI] [PubMed] [Google Scholar]
- 37.Shah S, Divekar AA, Hilchey SP, Cho H-M, Newman CL, Shin S-U, Nechustan H, Challita-Eid PM, Segal BM, Yi KH. Increased rejection of primary tumors in mice lacking B cells: inhibition of anti-tumor CTL and TH1 cytokine responses by B cells. Int J Cancer. 2005;117:574–586. doi: 10.1002/ijc.21177. [DOI] [PubMed] [Google Scholar]
- 38.Schultz KR, Klarnet JP, Gieni RS, HayGlass KT, Greenberg PD. The role of B cells for in vivo T cell responses to a Friend virus-induced leukemia. Science. 1990;249:921–923. doi: 10.1126/science.2118273. [DOI] [PubMed] [Google Scholar]
- 39.DiLillo DJ, Yanaba K, Tedder TF. B cells are required for optimal CD4+ and CD8+ T cell tumor immunity: therapeutic B cell depletion enhances B16 melanoma growth in mice. J Immunol. 2010;184:4006–4016. doi: 10.4049/jimmunol.0903009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kaliss N. Immunological enhancement of tumor homografts in mice: a review. Cancer Res. 1958;18:992–1003. [PubMed] [Google Scholar]
- 41.Salinas FA, Wee KH. Prognostic and pathogenetic implications of immune complexes in human cancer. Adv Immun Cancer Ther. 1986;2:189–209. doi: 10.1007/978-1-4613-9558-4_4. [DOI] [PubMed] [Google Scholar]
- 42.Johansson M, DeNardo DG, Coussens LM. Polarized immune responses differentially regulate cancer development. Immunol Rev. 2008;222:145–154. doi: 10.1111/j.1600-065X.2008.00600.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lapointe R, Bellemare-Pelletier A, Housseau F, Thibodeau J, Hwu P. CD40-stimulated B lymphocytes pulsed with tumor antigens are effective antigen-presenting cells that can generate specific T cells. Cancer Res. 2003;63:2836–2843. [PubMed] [Google Scholar]
- 44.Li Q, Grover AC, Donald EJ, Carr A, Yu J, Whitfield J, Nelson M, Takeshita N, Chang AE. Simultaneous targeting of CD3 on T cells and CD40 on B or dendritic cells augments the antitumor reactivity of tumor-primed lymph node cells. J Immunol. 2005;175:1424–1432. doi: 10.4049/jimmunol.175.3.1424. [DOI] [PubMed] [Google Scholar]
- 45.Linton P-J, Harbertson J, Bradley LM. A critical role for B cells in the development of memory CD4 cells. J Immunol. 2000;165:5558–5565. doi: 10.4049/jimmunol.165.10.5558. [DOI] [PubMed] [Google Scholar]
- 46.Rivera A, Chen CC, Ron N, Dougherty JP, Ron Y. Role of B cells as antigen-presenting cells in vivo revisited: antigen-specific B cells are essential for T cell expansion in lymph nodes and for systemic T cell responses to low antigen concentrations. Int Immunol. 2001;13:1583–1593. doi: 10.1093/intimm/13.12.1583. [DOI] [PubMed] [Google Scholar]
- 47.Linton P-J, Bautista B, Biederman E, Bradley ES, Harbertson J, Kondrack RM, Padrick RC, Bradley LM. Costimulation via OX40L expressed by B cells is sufficient to determine the extent of primary CD4 cell expansion and Th2 cytokine secretion in vivo. J Exp Med. 2003;197:875–883. doi: 10.1084/jem.20021290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Reuschenbach M, von Knebel Doeberitz M, Wentzensen N. A systematic review of humoral immune response against tumor antigens. Cancer Immunol Immunother. 2009;58:1535–1544. doi: 10.1007/s00262-009-0733-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Milne K, Köbel M, Kalloger SE, Barnes RO, Gao D, Gilks CB, Watson PH, Nelson BH. Systematic analysis of immune infiltrates in high-grade serous ovarian cancer reveals CD20, FoxP3 and TIA-1 as positive prognostic factors. PLoS One. 2009;4:e6412. doi: 10.1371/journal.pone.0006412. [DOI] [PMC free article] [PubMed] [Google Scholar]