Abstract
Radiation therapy (RT) is an integral part of prostate cancer treatment across all stages and risk groups. Immunotherapy using a live, attenuated, Listeria monocytogenes-based vaccines have been shown previously to be highly efficient in stimulating anti-tumor responses to impact on the growth of established tumors in different tumor models. Here, we evaluated the combination of RT and immunotherapy using Listeria monocytogenes-based vaccine (ADXS31-142) in a mouse model of prostate cancer. Mice bearing PSA-expressing TPSA23 tumor were divided to 5 groups receiving no treatment, ADXS31-142, RT (10 Gy), control Listeria vector and combination of ADXS31-142 and RT. Tumor growth curve was generated by measuring the tumor volume biweekly. Tumor tissue, spleen, and sera were harvested from each group for IFN-γ ELISpot, intracellular cytokine assay, tetramer analysis, and immunofluorescence staining. There was a significant tumor growth delay in mice that received combined ADXS31-142 and RT treatment as compared with mice of other cohorts and this combined treatment causes complete regression of their established tumors in 60 % of the mice. ELISpot and immunohistochemistry of CD8+ cytotoxic T Lymphocytes (CTL) showed a significant increase in IFN-γ production in mice with combined treatment. Tetramer analysis showed a fourfold and a greater than 16-fold increase in PSA-specific CTLs in animals receiving ADXS31-142 alone and combination treatment, respectively. A similar increase in infiltration of CTLs was observed in the tumor tissues. Combination therapy with RT and Listeria PSA vaccine causes significant tumor regression by augmenting PSA-specific immune response and it could serve as a potential treatment regimen for prostate cancer.
Electronic supplementary material
The online version of this article (doi:10.1007/s00262-012-1257-x) contains supplementary material, which is available to authorized users.
Keywords: Radiation therapy, Listeria PSA vaccine, Immunotherapy, Prostate cancer
Introduction
Radiation therapy (RT) is an integral part of prostate cancer treatment across all stages and risk groups. Despite RT and surgery, 10–40 % of patients have recurrence of their cancer within 5 years [1–3]. The addition of androgen deprivation therapy improves the survival of patients, but without an enhancement in the cure rate [4, 5]. Recently, a dendritic cell (DC)-based vaccine, Sipuleucel-T (Provenge, APC8015, Dendreon Corp, WA, USA), was shown to confer a survival advantage in men with metastatic castration-resistant prostate cancer (CRPC) [6] and is now FDA approved for its treatment. This has generated enthusiasm for immunotherapeutic strategies to be considered for the treatment of metastatic prostate cancer [7]. Preclinical studies and a clinical trial with a prostate cancer vaccine have demonstrated that RT and immunotherapy can be combined to enhance their mutual efficacies [8–10]. Unlike surgery, RT does not deplete the patient of tumor-associated antigens (TAA) and allows for the induction of an effective immune response. Irradiated tumor cells die slowly over time from apoptosis, necrosis and/or mitotic catastrophe, leading to the clearance of the dying cells by the immune system and access of tumor antigens to the antigen processing and presentation pathways [11, 12]. Irradiation induces immunogenic cell death [13–15]. Irradiation of a colon carcinoma cell line CT26 leads to the translocation of cytosolic calreticulin to the cell membrane and provides a phagocytosis signal to dendritic cells (DC) [15]. Irradiation also induces the secretion of HMGB1 by tumor cells, and this acts as a ligand for toll-like receptor (TLR) 4, which subsequently leads to DC recruitment and activation [13, 16]. As for its direct action on tumor cells, RT increases the cell surface expression of MHC class I molecules and amplifies the diversity of peptide antigen presentation by tumor cells [16]. It also increases the expression of Fas/CD95, which leads to an increased susceptibility of tumor cells to cytotoxic T lymphocyte (CTL)-mediated cell killing [17, 18]. Further, the level of interferon (IFN)-γ in the tumor microenvironment and IFN-γ-inducible genes is increased following RT, and this leads to the inhibition of cellular proliferation, angiogenesis, an increase in caspase-mediated cell killing, and an increase in MHC class I expression on non-irradiated tumor cells [19, 20]. RT also affects the tumor vasculature leading to an increase in the expression of endothelial adhesion molecules: VCAM-1, ICAM-1, P-selectin, and E-selectin [21, 22]. These observations suggest that a combination of RT and immunotherapy will have greater potential in improving the chances of success for the treatment of cancer when compared to monotherapy.
Prostate specific antigen (PSA) is a 34 kD glycoprotein with serine protease activity that is secreted by prostate epithelial and ductal cells [23]. There is a detectable increase in PSA levels in nearly all patients with prostate adenocarcinoma, which has led to its routine use in the clinic for diagnosis, risk assessment, and treatment monitoring [24, 25]. PSA is exclusively expressed by the prostate, which limits any potential widespread toxicity for its use as target antigen in immunotherapy, and it has been shown to be an immunogenic target of CTLs [26, 27]. Interestingly, multiple PSA-based immunotherapeutic strategies including DNA vaccines, recombinant viruses, Listeria-based vaccines, and DCs have been shown to effectively induce PSA-specific T cell responses in preclinical studies [28–31]. Finally, PSA has been validated as an immunotherapeutic target in clinical trials [25, 32].
A live-attenuated recombinant Listeria monocytogenes (Lm)-based PSA vaccine (ADXS31-142) has recently been developed for therapeutic use in prostate cancer [31, 33]. The ability of Lm to elicit strong and effective innate and adaptive immune responses makes it an ideal vector for cancer immunotherapy. Lm is actively phagocytosed by antigen-presenting cells (APCs) and replicates in the cytosol after escaping from the phagosome, through the expression of its virulence factors [34, 35]. This escape and intracellular proliferation of Lm allows for the generation of both CD4+ and CD8+ immune responses due to the processing of antigens through both the MHC class I and class II processing pathways [36, 37]. Antigen-specific CD8+ T cells mediate cytotoxic effects on the tumor cells, while antigen-specific CD4+ T cells help in the release of anti-tumoral cytokines such as IFNγ, TNFα, and IL-2 [36–39]. Lm-based vaccines have been shown to induce the accumulation of T cells within the tumor microenvironment, increase the secretion of cytotoxic and anti-angiogenic cytokines, and cause a decrease in regulatory T cells in the tumors [40, 41]. The efficacy of Lm vaccines in inducing long-lasting tumor immunity has been demonstrated for a number of tumor antigens including HPV16-E7 and Her-2/neu in both transplantable and transgenic mouse models of cancer [31, 40, 42–44].
The combination of immunotherapy and RT has been previously studied in several animal models. Combinations of immunomodulatory agents such as Toll-like receptor 9 (TLR9) ligands with RT have been shown to induce adaptive immune responses and improve survival in mouse models of glioma and lung cancer [45, 46]. It has also been observed that the injection of immature DCs into irradiated tumors leads to DC maturation and efficient anti-tumor immunity [47]. RT has also been tested in combination with DNA-based vaccines as well as using viral vectors, and these combinations lead to an increase in CTL infiltration into the tumors [48, 49]. Additionally, epitope spreading has been observed with RT combinations, as evidenced by the generation of CTLs directed toward other tumor-associated antigens than just the TAA used in the vaccine [48]. In this study, we explore the combination of local irradiation with immunotherapy using live-attenuated Lm-based vaccine ADXS31-142, in a mouse model of prostate cancer.
Materials and methods
Mice and cell lines
6- to 8-week-old male C57BL/6 mice (Jackson Labs, Bar Harbor, ME) were housed at the animal facility at the Albert Einstein College of Medicine, and all experiments were performed in accordance with protocols approved by the institutional animal care and use committee (IACUC). The TPSA23 cell line was created by transfection of PSA expression plasmid in the TRAMPC-1 murine prostate adenocarcinoma cell line and has been described previously [31]. TPSA23 cells were grown and maintained in DMEM (Atlanta Biologicals, Lawrenceville, GA) supplemented with 4 mM glutamine (Invitrogen, Carlsbad, CA), 1.5 g/l sodium bicarbonate (Invitrogen, Carlsbad, CA), 4.5 g/l glucose (Invitrogen, Carlsbad, CA), 5 g/ml insulin (Sigma-Aldrich, St. Louis, MO), 10 nM dehydroisoandrosterone (Sigma-Aldrich, St. Louis, MO), 5 % fetal bovine serum (Atlanta Biologicals, Lawrenceville, GA), 5 % NuSerum IV (BD Biosciences, San Diego, CA), and 5 μg/ml blasticidin (Invitrogen, Carlsbad, CA).
Vaccine preparation
The details of the construction of ADXS31-142 and the control Listeria vaccine ADXS-HPV16E7 have been described previously [31, 33]. The vaccine stocks were prepared and stored as 1 ml aliquots in freezer at −70 °C. Before injection, vaccine stocks were thawed at 37 °C for 2–3 min and then washed twice with phosphate-buffer saline (PBS) and resuspended in PBS at a final concentration of 5 × 108 colony forming units (CFU)/ml. Each mouse was immunized intraperitoneally with 200 μl of this suspension.
Flow cytometry antibodies
Antibodies used in the following studies were the following: anti-CD8-FITC, anti-CD3-PE-Cy7, and anti-IFN-γ APC, all purchased from BD (Franklin Lakes, NJ). For tetramer staining, the H-2Db PSA tetramer (HCIRNKSVIL) was conjugated to PE (NIH tetramer facility, Atlanta, GA) and the ovalbumin H-2Db PE tetramer (Beckman Coulter, Brea, CA).
RT and immunotherapy
1 × 106 TPSA23 cells were injected subcutaneously in the flank of C57BL/6 mice on day 0. Mice (10/group) with palpable tumors (~0.5 cm diameter) were treated as following: ADXS31-142 (108 CFU/mice); both ADXS31-142 (108 CFU) and RT (RT); RT only; control Listeria vaccine; and naïve untreated mice. Immunization with the Listeria-based vaccine was performed on days 10, 17, and 21 post-tumor implantation. On day 12 post-tumor implantation, single fraction external beam RT of 10 Gy was delivered using a 320 KvP, Phillips MGC-40 Orthovoltage irradiator at a 50 cm SSD with a 2-mm copper filter and a dose rate of 72 cGy/min after exposing the flank tumor and shielding the thorax, head and neck, abdomen, and extremities with lead blocks. The RT was given under anesthesia with 100 μl of a mixture of 100 mg/ml of ketamine (Fort Doge Animal Health, Fort Doge, IA) and 20 mg/ml of xylazine (Lloyd Laboratories, Shenandoah, IA). Tumors were measured twice a week by calipers and mean tumor volume (MTV) was calculated using the formula 0.5 × W2 × L. Tumors, spleen, and serum were harvested from 2 mice from each group on day 28, and the remainder when the tumors were 20 mm in diameter.
Tumor-infiltrating lymphocyte (TIL) isolation
Excised tumors were minced into pieces smaller than 1 mm and then incubated in PBS containing 1 mg/ml DNAse I (Roche Diagnostics, Indianapolis, IN) and 2 mg/ml collagenase (Fisher Scientific, Pittsburgh, PA) for 1 h at 37 °C. The lysate was then passed through a 70-μm cell strainer prior to red blood cell lysis. The single cell suspension obtained was used for the further analysis of TILs.
ELISpot assay
IFN-γ ELISpot assays were performed according to manufacturer’s protocol using a commercial ELISpot kit (Mabtech, Stockholm, Sweden). Briefly, plates were coated overnight with 0.015 mg/ml of an anti-mouse IFN-γ monoclonal antibody (clone AN18). For stimulation, cells were incubated in the presence of either 0.01 mg/ml of an immunodominant PSA epitope HCIRNKSVIL (Biomatik Corporation, Wilmington, DE) [50] or PMA (10 ng/ml Fisher Scientific, Pittsburgh, PA) and 0.5 μg/ml ionomycin (Fisher Scientific, Pittsburgh, PA), 0.01 mg/ml BSA (US Biological, Boston, MA). The HCIRNKSVIL peptide was pre-treated with the tris (2-carboxyethyl) phospine (TCEP) disulfide-reducing resin (Thermo-Scientific, Rockford, IL) to reduce any disulfide bonds. The spots were counted using an automatic ELISpot reader (Autoimmun Diagnostika, Strassberg, Germany).
Intracellular cytokine and tetramer staining
The intracellular IFN-γ cytokine staining assay was performed as described previously [51] using the Cytofix/Cytoperm with GolgiStop kit (Pharmingen, Becton–Dickinson, San Jose, CA). For PSA tetramer staining, splenocytes or TILs were cultured overnight in the presence of IL-2 and were incubated with H-2Db PSA tetramer conjugated to PE (NIH tetramer facility, Atlanta, GA) in ice for 30 min. A separate set of control population was incubated with Ovalbumin H-2Db tetramer conjugated to PE (Beckman Coulter, Brea, CA). Cells were then stained with FITC-conjugated anti-CD8 mAb, PE-Cy7-conjugated anti-CD3 mAb, and Live/Dead Fixable Cell stain kit (Invitrogen, Carlsbad, CA) and then washed and fixed in 4 % paraformaldehyde (Fisher Scientific, Pittsburgh, PA). Flow cytometry samples were analyzed on an LSRII (BD, Franklin Lakes, NJ), and the data were analyzed using the FlowJo v7.0 (Tree Star Inc, Ashland, OR) software.
Statistical analysis
Tumor dimensions were caliper measured biweekly and evaluated for response rate (RR), complete response (CR) and partial response (PR). Mean tumor volume (MTV) was calculated using the formula 0.5 × W2 × L (W, width and L, length), and tumor growth delay (TGD) was calculated based on the MTV of the combination arm. Kaplan–Meier analysis with tumor volume and paired t test was performed between the cohorts in SPSS v13. The study endpoint was tumor diameter >2 cm according to the protocols of institutional animal facility, which was reached in the control groups in approximately 6 weeks. Immune assays were analyzed using Student’s t test.
Results
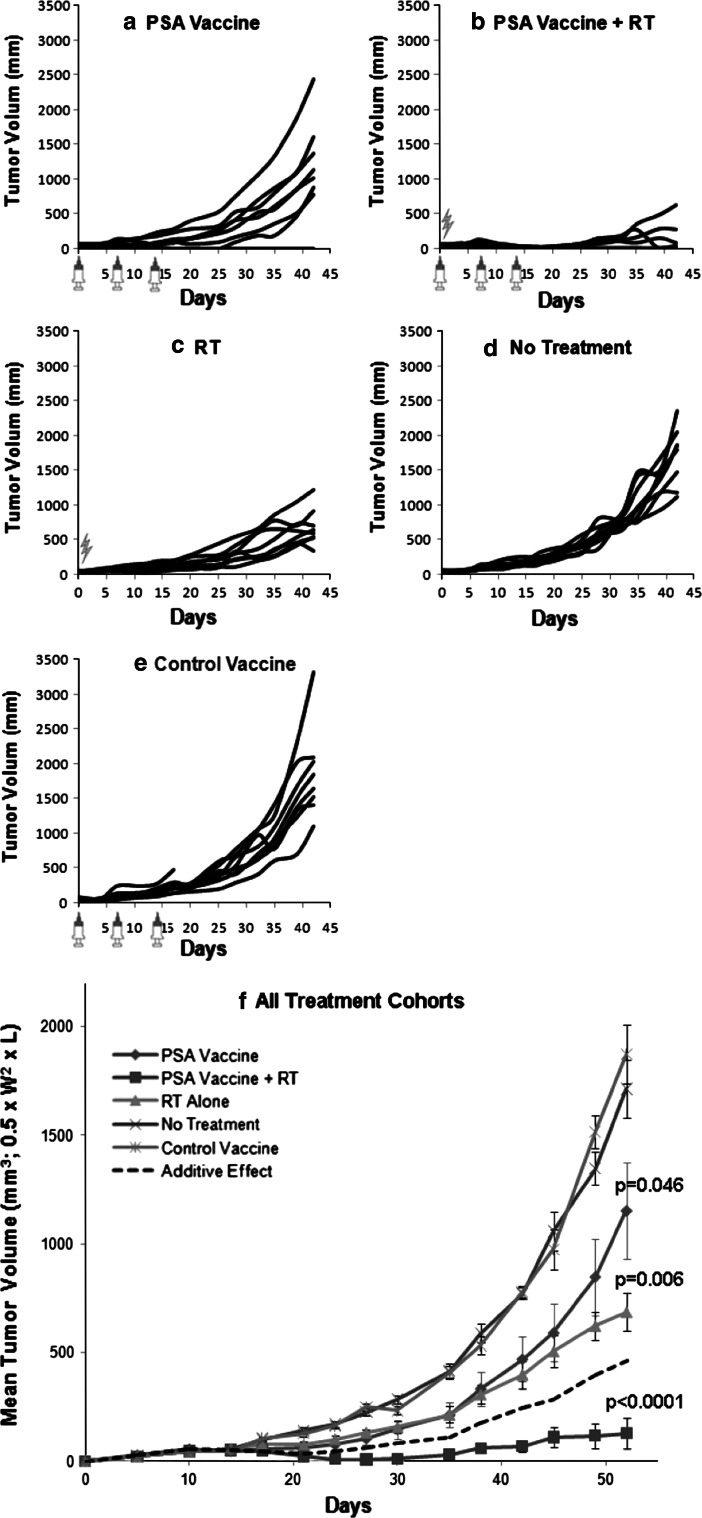
Synergistic effect of RT and immunotherapy on tumor growth
The ADXS31-142 PSA vaccine has previously been shown to cause tumor growth delay of established TPSA23 tumors in syngeneic C57BL/6 male mice [31]. However, tumors eventually recurred in these mice after being treated with vaccine alone. We, therefore, examined whether the combination of vaccine with RT could improve the efficacy of either immunotherapy or RT, administered as a single-modality treatment. Since prostate cancer RT could benefit from hypo-fractionated (larger dose per fraction) regimens [52–54], we chose to treat the murine prostate tumors with a single fraction of 10 Gy. A combination of ADXS31-142 PSA vaccine and RT reduces tumor growth as early as 1-week post-vaccination and causes complete regression of established tumors in 60 % of the mice (Fig. 1a–e, Supplemental Fig S1). In contrast, treatment with either RT or ADXS31-142 alone caused a significant delay in tumor growth, but had minimal complete regression (≤10 %). This suggests that the combination of vaccine and RT treatment has curative effect that ultimately causes a stronger impact on tumor treatment.
Fig. 1.
Tumor regression upon combined RT and PSA vaccine treatment. On day 0, C57/B6 mice (n = 50) bearing palpable TPSA23 tumors (~5 mm in diameter) were randomized to one of five treatment arms: a PSA vaccine, ADXS31-142 vaccine, b PSA vaccine, ADXS31-142 vaccine + RT, c RT, d no treatment and e control Lm vaccine (ADXS31-134) vaccine. Listeria vaccines (1 × 108 CFU) were administrated on days 1, 7, and 14 while a single-dose RT (10 Gy) was given on day 0. Tumor volume was measured biweekly until the study endpoint (20 mm in diameter) is reached. The tumor growth of each individual mouse from each group is shown in a–e while the statistical difference of mean tumor volume from each group is shown in f. Additive effect (dashed line in f) is calculated by the product of percent decrease by individual treatments
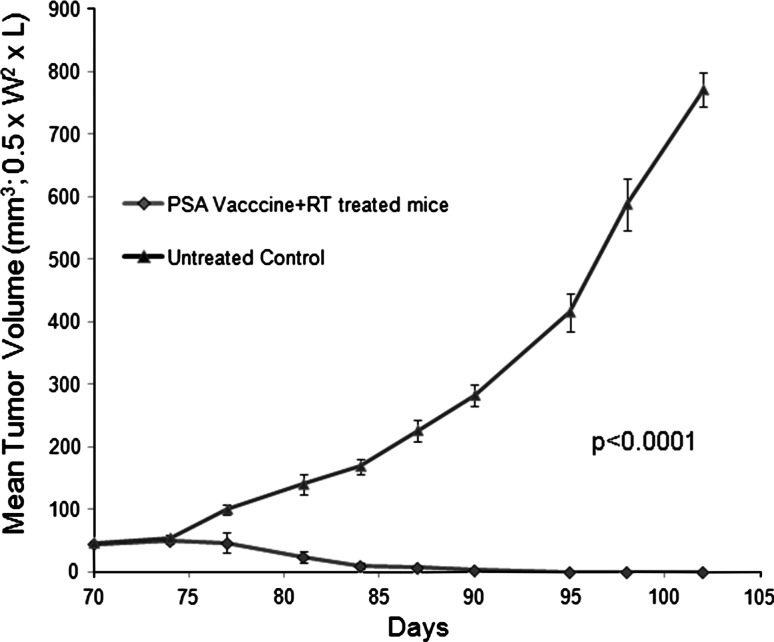
Further, we tested whether the mice surviving after combination therapy with ADXS31-142 (PSA Vaccine) and RT developed protective immune memory against prostate tumors. Mice that had complete regression following combination therapy were administered a tumor challenge 3-month post-first vaccination. TPSA23 tumor cells (1 × 106 cells) were implanted in the opposite flank as the original tumor, and the mice were observed for any tumor growth. We found that the mice treated with combination therapy did not (Fig. 2) develop tumors possibly due to the induction of systemic and lasting immunity to the TPSA23.
Fig. 2.
Protective effect against challenged TPSA23 cells in mice cured by combined RT and Listeria PSA vaccine, ADXS31-142 vaccine treatment. Untreated mice and mice with CR from the combined treatment group (N = 6/group) were challenged with TPSA23 cells (1 × 106) 3 months after first vaccination. Tumor volume was measured biweekly until the study endpoint is reached in untreated mice. A p value is given to show the statistical difference of tumor volume between these two groups
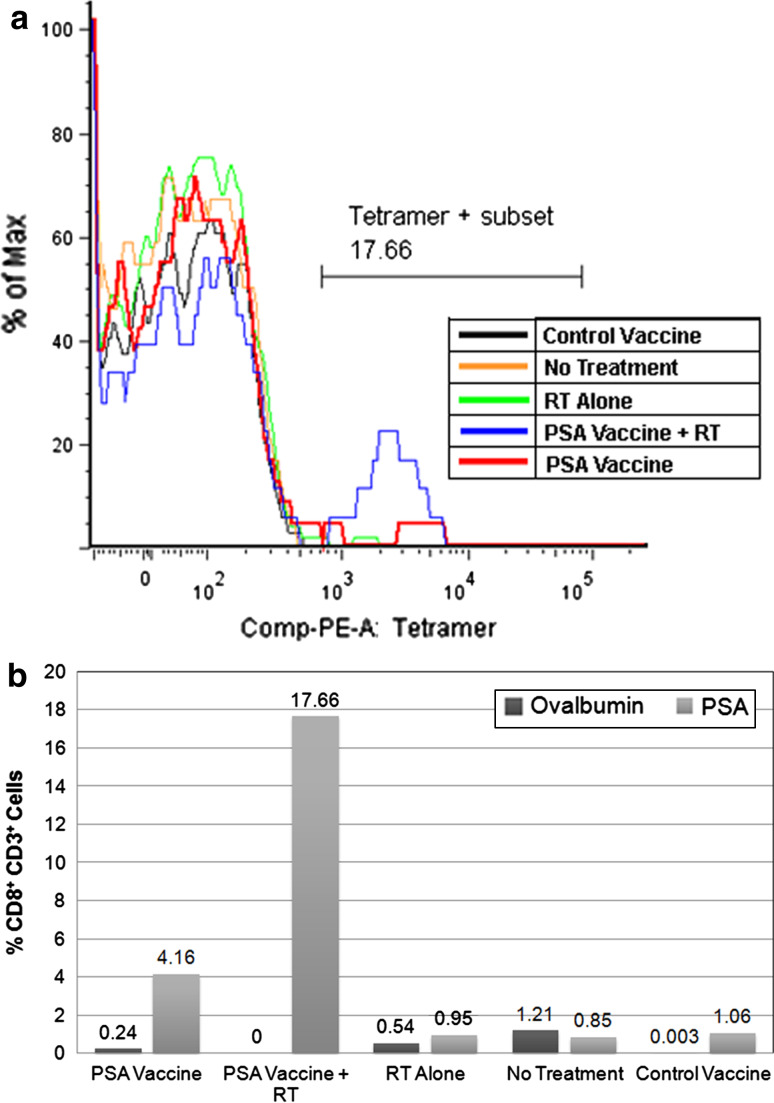
Combination therapy induces PSA-specific T cell responses and enhances their ability to secrete IFNγ
To understand whether the tumoricidal effects of the combination therapy are due to an enhancement in the generation of PSA-specific T cell responses, we examined the peripheral immune responses in the splenocytes of tumor-bearing mice in each treatment cohorts. Splenocytes were analyzed for the presence of PSA-specific CTLs by H-2Db PSA tetramer analysis. PE-conjugated, MHC I H-2Db PSA tetramer binds specifically to the TCRs recognizing the PSA-derived peptide epitope, HCIRNKSVIL, and was specifically designed for this purpose by the NIH tetramer facility. The results show that vaccination with ADXS31-142 resulted in 4 % of PSA tetramer positive cells and combination of RT with ADXS31-142 vaccine resulted in 17 % of PSA tetramer positive cells (Fig. 3b) in the splenocytes. This suggests that overall there was a fourfold increase in the generation of PSA-specific T cells after treatment with combination therapy when compared to ADXS31-142 vaccine group. In naïve, RT, or control Listeria vaccine-treated group, PSA tetramer-specific T cells were not detected (Fig. 3).
Fig. 3.
Enrichment of splenic PSA-specific T cells in mice treated with combined RT and Listeria PSA vaccine, ADXS31-142 vaccine. Splenocytes of mice from each cohort were stained with PE-conjugated PSA65–74/H-2Db tetramer, FITC-conjugated anti-CD8, and PE-Cy7-conjugated anti-CD3 antibodies. The percentage of PSA65–74/H-2Db tetramer+ (a, b) and control OVA257–264/H-2Kb tetramer+ cells (b) within CD8+CD3+ T cells is shown
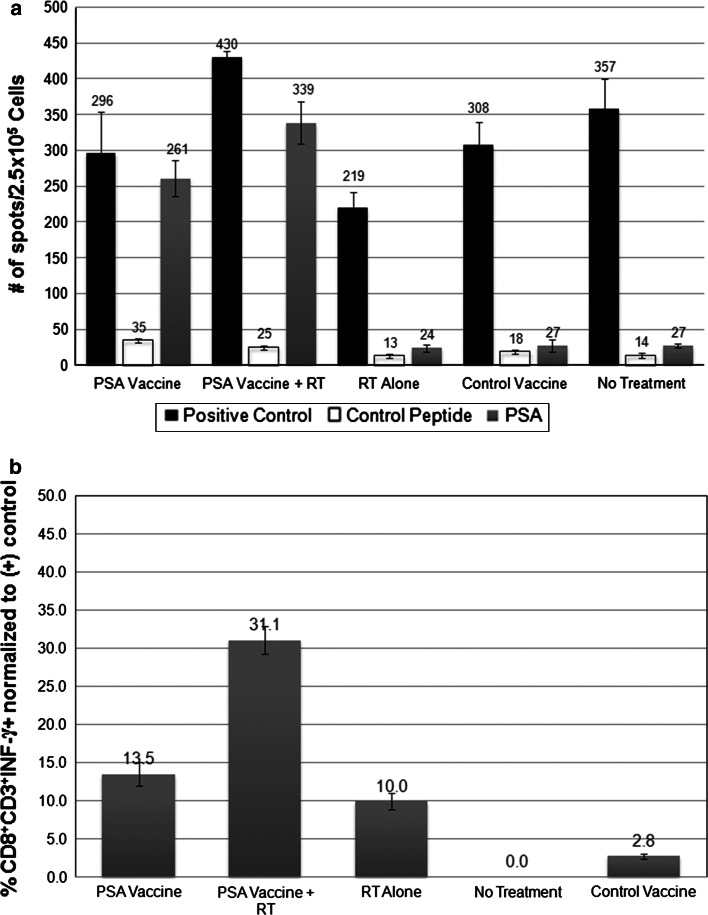
Further, we analyzed the functional ability of T cells to synthesize cytokine IFN-γ using ELISpot and intracellular cytokine staining. We observed that there was a 7- and 13-fold increase in the number of cells secreting IFN-γ after treatment with ADXS31-142 vaccine alone and RT + vaccine therapy, respectively (Fig. 4a, Supplementary Fig S2).
Fig. 4.
Increased Interferon-γ releasing splenic PSA-specific T cells in mice treated with combined RT and Listeria PSA vaccine, ADXS31-142 vaccine. Splenocytes from mice of each cohort were stimulated with either PSA65–74 peptide, control peptide, or a mixture of PMA and Ionomycin. The release of Interferon-γ from PSA-specific T cells was detected by ELISpot (a) and intracelluar cytokine staining assay (b). PMA and Ionomycin are non-specific activators of lymphocyte and serves as positive control for both assays. The number of IFN-γ releasing T cells per 2.5 × 105 splenocytes is shown in ELISpot assay (a) while the percentage of CD8+CD3+IFN-γ cells (normalized to the positive control) is shown in intracelluar cytokine staining assay (b)
Analysis of the functional ability using intracellular cytokine staining specific for IFN-γ (Fig. 4b, Supplementary Fig S3) shows a twofold increase in the production of IFN-γ + CD8+ T cells following the combination therapy when compared to ADXS31-142 alone. The results obtained with intracellular cytokine staining were consistent with those of ELISpot assay, suggesting the combination therapy increases the functional ability of PSA-specific T cells to secrete cytokine IFN-γ.
Increase in PSA-specific T cell tumor infiltration following combination therapy
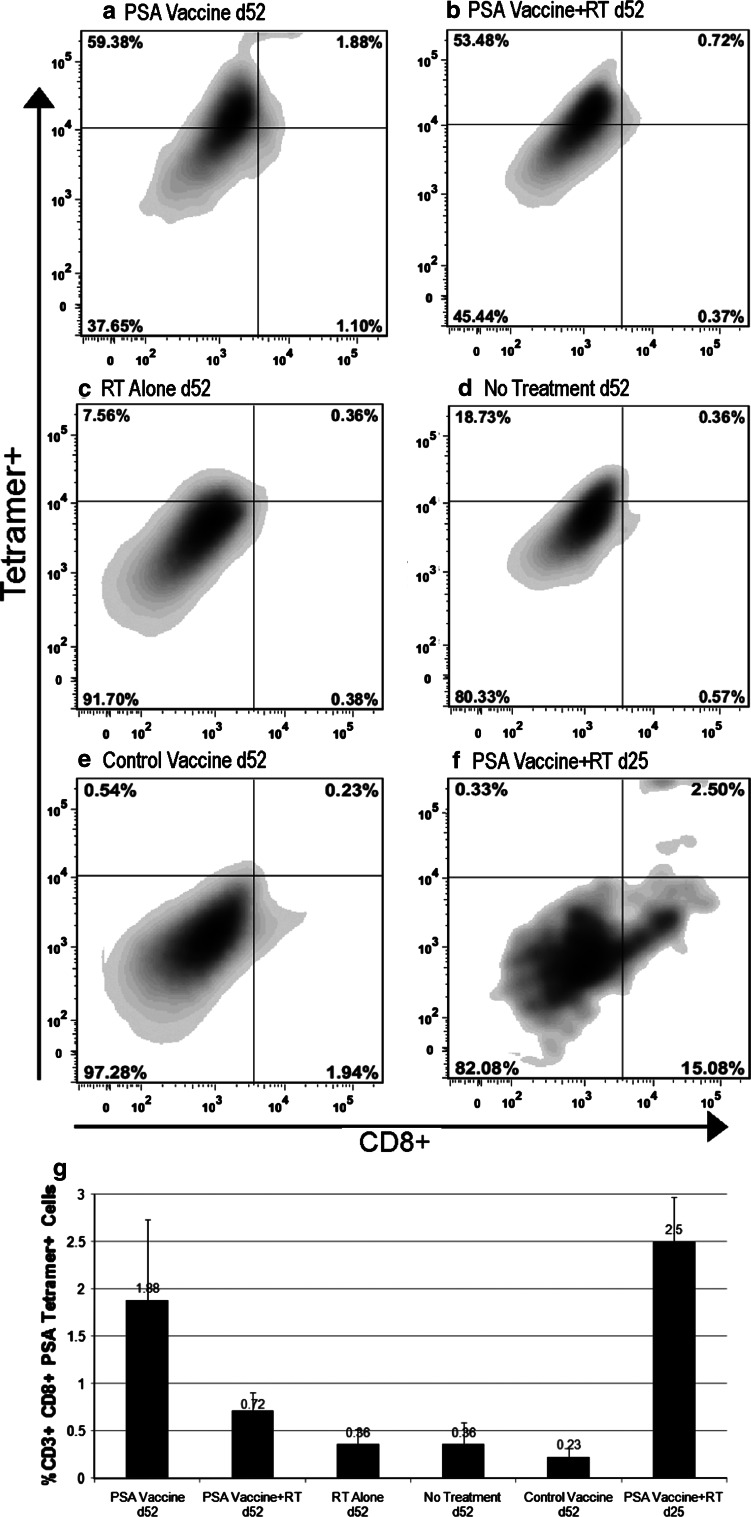
Effective therapies should not only lead to an increase in antigen-specific T cells but also cause significant infiltration of these T cells into the tumor microenvironment. We, therefore, examined whether there is an increase in the infiltration of the PSA-specific T cells in the irradiated tumor microenvironment (Fig. 5). To assess this, tumors were harvested at the end of our experiments to determine the extent of PSA-specific TILs in partially regressing tumors of the ADXS31-142–treated group and compared them with the tumor regrowth seen in the animals treated with combination therapy. The results showed eightfold increase in the infiltration of PSA-specific CD8+ T cells following vaccine alone compared to control (Fig. 5g). RT alone or no treatment did not cause any infiltration of PSA-specific T cells (Fig. 5g). There was a twofold increase in PSA-specific TIL following the combination therapy compared to RT alone (Fig. 5g).
Fig. 5.
Accumulation of PSA-specific T cells in tumor tissue in mice treated with combined RT and PSA vaccine, ADXS31-142 vaccine. Tumor-infiltrating lymphocytes (TILs) were collected on d52 from mice received PSA vaccine (a), PSA vaccine, ADXS31-142 vaccine + RT (b), RT (c), no treatment (d), and Control vaccine (e). TILs from PSA vaccine, ADXS31-142 vaccine + RT group were also collected on d25 before a significant shrinkage of tumor volume was observed (f). Cells were stained with PE-conjugated PSA65–74/H-2Db tetramer, FITC-conjugated anti-CD8, and PE-Cy7-conjugated anti-CD3 antibodies. Percentage of PSA65–74/H-2Db Tetramer+CD8+ cells within CD3+ cells shown in a–f represents data of one mouse from each group. The statistical difference of these PSA-specific T cells among all the groups is shown in g
The lower percentage of PSA-specific TILs in the RT + ADXS31-142 group versus the ADXS31-142–treated group may have been the result of tumors in the combination therapy group being harvested from tumors that were growing subsequent to a complete response, or it is possible that the tumor recurred due to a potential deficiency of PSA-specific CD8+ T cells. Conversely, there may have been significant infiltration of PSA-specific CD8 T cells at an earlier point following treatment, which subsequently decreased over time following the therapy.
In order to determine whether there was significant CD8 T cell infiltration at an earlier time point, we repeated this study and harvested tumors that were actively regressing on day 25. We observed that there was a sevenfold increase in tumor infiltration of the PSA-specific CD8 T cells in the combination therapy group compared to the untreated mice (Fig. 5g), supporting the hypothesis that there is an increased infiltration of these cells earlier in the actively regressing tumors. Overall, the combination therapy treatment impacts on the immune response by causing increased induction of PSA-specific T cells in the periphery and consequently, an increased infiltration of these cells in the tumor microenvironment.
Discussion
RT is an effective treatment for localized prostate cancer. However, up to 40 % of patients fail RT [1–3, 55]. Immunotherapy has been explored as a treatment in patients with metastatic hormone refractory prostate cancer. Sipuleucel-T (Provenge, recently approved by the FDA) shows an approximately 4-month increase in survival for these patients, demonstrating an effect of immunotherapy to increase survival in prostate cancer [56]. Although RT has the potential to induce immune responses from dying tumor cells [9], a combination of immunotherapy and RT has not been used in clinical practice. As a prelude to designing clinical trials of RT and tumor vaccine, we examined the tumoricidal and immunological effects of combining a Listeria PSA vaccine with RT in a murine model of prostate cancer.
Listeria monocytogenes-based vaccines have been used previously in several mouse models of cancer [31, 40, 42, 43, 57]. The therapeutic anti-tumor efficacy of these vaccines correlated with the generation of TAA-specific immune responses. Two different bioengineered strains of Listeria monocytogenes expressing PSA have been shown to be very effective in causing tumor regression in mouse models of prostate cancer [31]. The study described here demonstrates that the treatment with ADXS31-142 vaccine causes growth retardation and partial regression of established tumors. Interestingly, the complete regression of tumors was only observed when ADXS31-142 Listeria PSA vaccine was combined with a single fraction of 10 Gy RT (Fig. 1). Furthermore, we demonstrate that the combination therapy induces a systemic immune protection to tumor challenge, 3-month post-RT (Fig. 2), indicating the generation of a strong PSA-specific immune response with induction of immunological memory. There was an increase in PSA-specific CD8 T cells as measured by PSA tetramer staining (Fig. 4) with subsequent increase in IFN-γ secretion upon stimulation with an immunodominant PSA epitope (Fig. 3), indicating enhanced responsiveness of the PSA-specific CD8+ T cells following combination therapy. These PSA-specific CD8 T cells actively infiltrate irradiated tumors and are found in large numbers at early time points in actively regressing tumors following RT and ADXS31-142 immunotherapy (Fig. 5).
PSA has been widely used previously as TAA for targeting human prostate cancer in various preclinical as well as clinical studies and several studies have shown that tolerance against PSA in humans can be overcome by repeated immunizations [58, 59]. Noteworthy, PSA is a foreign antigen in mice, and thus, no tolerance is expected toward this antigen. As a next step, we will be investigating this combination treatment approach in further in PSA transgenic mice, where immunological tolerance can be addressed [60].
The dose of 10 Gy of RT was chosen for this study since there is emerging evidence that the α/β ratio, a measure of the response of tumor or tissue to a radiation fraction size, of prostate cancer could be approximately 1.5, leading to a predicted benefit in treating prostate cancer patients with hypo-fractionated (larger dose per fraction) regiments [52–54]. The dose for high-dose-rate brachytherapy treatment for prostate cancer is about 10 Gy/fraction, and a phase I study was recently completed for the definitive treatment of prostate cancer with a total dose of 50 Gy delivered in 10 Gy per fraction [61, 62]. It is also proposed that a regimen of hypo-fractionated RT is more ablative than standard fractionated RT (1.8–2.0 Gy fraction size) and therefore ablative doses of hypo-fractionated RT could release tumor antigens for induction of a strong protective immune response to TAA. In this study, we examined the immunological effects of one fraction of 10 Gy, which was expected to be suboptimal towards tumor control (Fig. 1). However, it is even more noteworthy that the combination of Listeria PSA vaccine with a sublethal dose of RT was tumoricidal and caused complete regression of established tumors with RT amplifying the immune response toward PSA.
The interaction of RT and immunotherapy are not fully delineated, although the potential of combination therapies are being actively studied [9]. There is evidence of radiosensitization in the treatment of head and neck cancers with cetuximab, showing that RT could impact on the effectiveness of an immunotherapy [63]. The use of mouse models of cancer with combination therapies will allow us to better understand the interplay of radiation and immunotherapy on the immune system and the efficacy of cancer treatments. RT leaves the tumor antigens in the mouse and allows for the generation of an effective immune response to these antigens, unlike surgery. Furthermore, unlike chemotherapy, RT is a local therapy and does not demonstrate the systemic toxicity and immunosuppressive effects of chemotherapy. In addition, there are sufficient pre-clinical evidence to suggest that RT induces an immunogenic cell death by increasing tumor neo-antigen presentation in MHC I on tumor cell surface, increases translocation of calreticulin, and secretion of HMGB1 [13–16]. In our study, the Listeria PSA vaccine potentially amplified the immunogenic effects of RT by activating antigen-presenting cells that were presented with PSA and tumor antigens released from irradiated cells in the context of innate “danger” signals from the bacterial cell wall and nucleic acids of the attenuated Listeria vaccine.
Although the treatment options for early-stage prostate cancer are multiple and highly effective, treatment for patients with intermediate and advanced disease are limited to RT and ADT, with less success [64]. In this setting, where RT is already a standard part of patient care, immunotherapy makes an attractive combination therapy to enhance the efficacy of RT alone. The possibility exists that combination therapy of the type described here may allow for lower doses of RT to be used than the current standard, thus increasing the safety of RT-immunotherapy or hypo-fractionated regimens. Clinically, the safety of using a live-attenuated Listeria monocytogenes-based vaccine has been addressed in a trial of cervical cancer with an HPV16-E7 vaccine, and this vaccine is currently in phase II trials [65, 66]. Due to its limited toxicity and the evidence of strong immune responses in mouse models, a combination of RT and ADXS31-142 is promising for further evaluation in clinical trials of prostate cancer.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplemental Figure 1: Tumor response in representative mice on d34 from each of the cohorts: A) PSA Vaccine, B), PSA Vaccine +RT, C)RT Alone, D) No Treatment and E) Control Vaccine. (TIFF 3668 kb)
Supplemental Figure 2: Representative wells after subjecting the splenocytes from each cohort to ELISpot analysis. A) Non-specific stimulation with PMA, B) Negative control stimulation with BSA, and C-G stimulation with PSA, C) PSA Vaccine, D), PSA Vaccine +RT, E)RT Alone, F) No Treatment and G) Control Vaccine. (TIFF 276 kb)
Supplemental Figure 3: FACS analysis for IFN-γ in CD8+CD3+ cells. A) PSA Vaccine, B), PSA Vaccine +RT, C)RT Alone, D) No Treatment and E) Control Vaccine. (TIFF 3480 kb)
Acknowledgments
This work was supported in part by the NIH grants, R01EB009040, RC2 AI087612 and U19AI091175 to CG.
Conflicts of interest
Dr. Anu Wallecha, Dr. Reshma Singh, and Dr. John Rothman are employed by Advaxis Inc and own stock in that company.
References
- 1.Kuban DA, Tucker SL, Dong L, Starkschall G, Huang EH, Cheung MR, Lee AK, Pollack A. Long-term results of the M. D. Anderson randomized dose-escalation trial for prostate cancer. Int J Radiat Oncol Biol Phys. 2008;70(1):67–74. doi: 10.1016/j.ijrobp.2007.06.054. [DOI] [PubMed] [Google Scholar]
- 2.Kupelian PA, Potters L, Khuntia D, Ciezki JP, Reddy CA, Reuther AM, Carlson TP, Klein EA. Radical prostatectomy, external beam radiotherapy <72 Gy, external beam radiotherapy > or = 72 Gy, permanent seed implantation, or combined seeds/external beam radiotherapy for stage T1-T2 prostate cancer. Int J Radiat Oncol Biol Phys. 2004;58(1):25–33. doi: 10.1016/S0360-3016(03)00784-3. [DOI] [PubMed] [Google Scholar]
- 3.Tollefson MK, Leibovich BC, Slezak JM, Zincke H, Blute ML. Long-term prognostic significance of primary Gleason pattern in patients with Gleason score 7 prostate cancer: impact on prostate cancer specific survival. J Urol. 2006;175(2):547–551. doi: 10.1016/S0022-5347(05)00152-7. [DOI] [PubMed] [Google Scholar]
- 4.Bolla M, Collette L, Blank L, Warde P, Dubois JB, Mirimanoff RO, Storme G, Bernier J, Kuten A, Sternberg C, Mattelaer J, Lopez Torecilla J, Pfeffer JR, Lino Cutajar C, Zurlo A, Pierart M. Long-term results with immediate androgen suppression and external irradiation in patients with locally advanced prostate cancer (an EORTC study): a phase III randomised trial. Lancet. 2002;360(9327):103–106. doi: 10.1016/S0140-6736(02)09408-4. [DOI] [PubMed] [Google Scholar]
- 5.D’Amico AV, Manola J, Loffredo M, Renshaw AA, DellaCroce A, Kantoff PW. 6-month androgen suppression plus radiation therapy vs radiation therapy alone for patients with clinically localized prostate cancer: a randomized controlled trial. JAMA. 2004;292(7):821–827. doi: 10.1001/jama.292.7.821. [DOI] [PubMed] [Google Scholar]
- 6.Kantoff PW, Higano CS, Shore ND, Berger ER, Small EJ, Penson DF, Redfern CH, Ferrari AC, Dreicer R, Sims RB, Xu Y, Frohlich MW, Schellhammer PF. Sipuleucel-T immunotherapy for castration-resistant prostate cancer. N Engl J Med. 2010;363(5):411–422. doi: 10.1056/NEJMoa1001294. [DOI] [PubMed] [Google Scholar]
- 7.Joniau S, Abrahamsson PA, Bellmunt J, Figdor C, Hamdy F, Verhagen P, Vogelzang NJ, Wirth M, Van Poppel H, Osanto S. Current vaccination strategies for prostate cancer. Eur Urol. 2012;61(2):290–306. doi: 10.1016/j.eururo.2011.09.020. [DOI] [PubMed] [Google Scholar]
- 8.Demaria S, Bhardwaj N, McBride WH, Formenti SC. Combining radiotherapy and immunotherapy: a revived partnership. Int J Radiat Oncol Biol Phys. 2005;63(3):655–666. doi: 10.1016/j.ijrobp.2005.06.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hodge JW, Guha C, Neefjes J, Gulley JL (2008) Synergizing radiation therapy and immunotherapy for curing incurable cancers. Opportunities and challenges. Oncology (Williston Park) 22 (9):1064–1070 (discussion 1075, 1080–1061, 1084) [PMC free article] [PubMed]
- 10.Kantoff PW, Schuetz TJ, Blumenstein BA, Glode LM, Bilhartz DL, Wyand M, Manson K, Panicali DL, Laus R, Schlom J, Dahut WL, Arlen PM, Gulley JL, Godfrey WR. Overall survival analysis of a phase II randomized controlled trial of a Poxviral-based PSA-targeted immunotherapy in metastatic castration-resistant prostate cancer. J Clin Oncol. 2010;28(7):1099–1105. doi: 10.1200/JCO.2009.25.0597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sauter B, Albert ML, Francisco L, Larsson M, Somersan S, Bhardwaj N. Consequences of cell death: exposure to necrotic tumor cells, but not primary tissue cells or apoptotic cells, induces the maturation of immunostimulatory dendritic cells. J Exp Med. 2000;191(3):423–434. doi: 10.1084/jem.191.3.423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shimamura H, Sunamura M, Tsuchihara K, Egawa S, Takeda K, Matsuno S. Irradiated pancreatic cancer cells undergo both apoptosis and necrosis, and could be phagocytized by dendritic cells. Eur Surg Res. 2005;37(4):228–234. doi: 10.1159/000087868. [DOI] [PubMed] [Google Scholar]
- 13.Apetoh L, Ghiringhelli F, Tesniere A, Obeid M, Ortiz C, Criollo A, Mignot G, Maiuri MC, Ullrich E, Saulnier P, Yang H, Amigorena S, Ryffel B, Barrat FJ, Saftig P, Levi F, Lidereau R, Nogues C, Mira JP, Chompret A, Joulin V, Clavel-Chapelon F, Bourhis J, Andre F, Delaloge S, Tursz T, Kroemer G, Zitvogel L. Toll-like receptor 4-dependent contribution of the immune system to anticancer chemotherapy and radiotherapy. Nat Med. 2007;13(9):1050–1059. doi: 10.1038/nm1622. [DOI] [PubMed] [Google Scholar]
- 14.Obeid M, Panaretakis T, Joza N, Tufi R, Tesniere A, van Endert P, Zitvogel L, Kroemer G. Calreticulin exposure is required for the immunogenicity of gamma-irradiation and UVC light-induced apoptosis. Cell Death Differ. 2007;14(10):1848–1850. doi: 10.1038/sj.cdd.4402201. [DOI] [PubMed] [Google Scholar]
- 15.Obeid M, Tesniere A, Ghiringhelli F, Fimia GM, Apetoh L, Perfettini JL, Castedo M, Mignot G, Panaretakis T, Casares N, Metivier D, Larochette N, van Endert P, Ciccosanti F, Piacentini M, Zitvogel L, Kroemer G. Calreticulin exposure dictates the immunogenicity of cancer cell death. Nat Med. 2007;13(1):54–61. doi: 10.1038/nm1523. [DOI] [PubMed] [Google Scholar]
- 16.Reits EA, Hodge JW, Herberts CA, Groothuis TA, Chakraborty M, Wansley EK, Camphausen K, Luiten RM, de Ru AH, Neijssen J, Griekspoor A, Mesman E, Verreck FA, Spits H, Schlom J, van Veelen P, Neefjes JJ. Radiation modulates the peptide repertoire, enhances MHC class I expression, and induces successful antitumor immunotherapy. J Exp Med. 2006;203(5):1259–1271. doi: 10.1084/jem.20052494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chakraborty M, Abrams SI, Camphausen K, Liu K, Scott T, Coleman CN, Hodge JW. Irradiation of tumor cells up-regulates Fas and enhances CTL lytic activity and CTL adoptive immunotherapy. J Immunol. 2003;170(12):6338–6347. doi: 10.4049/jimmunol.170.12.6338. [DOI] [PubMed] [Google Scholar]
- 18.Garnett CT, Palena C, Chakraborty M, Tsang KY, Schlom J, Hodge JW. Sublethal irradiation of human tumor cells modulates phenotype resulting in enhanced killing by cytotoxic T lymphocytes. Cancer Res. 2004;64(21):7985–7994. doi: 10.1158/0008-5472.CAN-04-1525. [DOI] [PubMed] [Google Scholar]
- 19.Boehm U, Klamp T, Groot M, Howard JC. Cellular responses to interferon-gamma. Annu Rev Immunol. 1997;15:749–795. doi: 10.1146/annurev.immunol.15.1.749. [DOI] [PubMed] [Google Scholar]
- 20.Burnette BC, Liang H, Lee Y, Chlewicki L, Khodarev NN, Weichselbaum RR, Fu YX, Auh SL. The efficacy of radiotherapy relies upon induction of type i interferon-dependent innate and adaptive immunity. Cancer Res. 2011;71(7):2488–2496. doi: 10.1158/0008-5472.CAN-10-2820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lugade AA, Moran JP, Gerber SA, Rose RC, Frelinger JG, Lord EM. Local radiation therapy of B16 melanoma tumors increases the generation of tumor antigen-specific effector cells that traffic to the tumor. J Immunol. 2005;174(12):7516–7523. doi: 10.4049/jimmunol.174.12.7516. [DOI] [PubMed] [Google Scholar]
- 22.Lugade AA, Sorensen EW, Gerber SA, Moran JP, Frelinger JG, Lord EM. Radiation-induced IFN-gamma production within the tumor microenvironment influences antitumor immunity. J Immunol. 2008;180(5):3132–3139. doi: 10.4049/jimmunol.180.5.3132. [DOI] [PubMed] [Google Scholar]
- 23.Kaminski JM, Summers JB, Ward MB, Huber MR, Minev B. Immunotherapy and prostate cancer. Cancer Treat Rev. 2003;29(3):199–209. doi: 10.1016/S0305-7372(03)00005-7. [DOI] [PubMed] [Google Scholar]
- 24.Catalona WJ. Clinical utility of measurements of free and total prostate-specific antigen (PSA): a review. Prostate Suppl. 1996;7:64–69. doi: 10.1002/(SICI)1097-0045(1996)7+<64::AID-PROS9>3.0.CO;2-J. [DOI] [PubMed] [Google Scholar]
- 25.Kantoff PW, Talcott JA. The prostate specific antigen. Its use as a tumor marker for prostate cancer. Hematol Oncol Clin North Am. 1994;8(3):555–572. [PubMed] [Google Scholar]
- 26.Correale P, Walmsley K, Nieroda C, Zaremba S, Zhu M, Schlom J, Tsang KY. In vitro generation of human cytotoxic T lymphocytes specific for peptides derived from prostate-specific antigen. J Natl Cancer Inst. 1997;89(4):293–300. doi: 10.1093/jnci/89.4.293. [DOI] [PubMed] [Google Scholar]
- 27.Xue BH, Zhang Y, Sosman JA, Peace DJ. Induction of human cytotoxic T lymphocytes specific for prostate-specific antigen. Prostate. 1997;30(2):73–78. doi: 10.1002/(SICI)1097-0045(19970201)30:2<73::AID-PROS1>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 28.Elzey BD, Siemens DR, Ratliff TL, Lubaroff DM. Immunization with type 5 adenovirus recombinant for a tumor antigen in combination with recombinant canarypox virus (ALVAC) cytokine gene delivery induces destruction of established prostate tumors. Int J Cancer. 2001;94(6):842–849. doi: 10.1002/ijc.1556. [DOI] [PubMed] [Google Scholar]
- 29.Hodge JW, Schlom J, Donohue SJ, Tomaszewski JE, Wheeler CW, Levine BS, Gritz L, Panicali D, Kantor JA. A recombinant vaccinia virus expressing human prostate-specific antigen (PSA): safety and immunogenicity in a non-human primate. Int J Cancer. 1995;63(2):231–237. doi: 10.1002/ijc.2910630215. [DOI] [PubMed] [Google Scholar]
- 30.Pavlenko M, Roos AK, Leder C, Hansson LO, Kiessling R, Levitskaya E, Pisa P. Comparison of PSA-specific CD8+ CTL responses and antitumor immunity generated by plasmid DNA vaccines encoding PSA-HSP chimeric proteins. Cancer Immunol Immunother. 2004;53(12):1085–1092. doi: 10.1007/s00262-004-0559-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Shahabi V, Reyes–Reyes M, Wallecha A, Rivera S, Paterson Y, Maciag P. Development of a Listeria monocytogenes based vaccine against prostate cancer. Cancer Immunol Immunother. 2008;57(9):1301–1313. doi: 10.1007/s00262-008-0463-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gulley JL, Arlen PM, Bastian A, Morin S, Marte J, Beetham P, Tsang KY, Yokokawa J, Hodge JW, Menard C, Camphausen K, Coleman CN, Sullivan F, Steinberg SM, Schlom J, Dahut W. Combining a recombinant cancer vaccine with standard definitive radiotherapy in patients with localized prostate cancer. Clin Cancer Res. 2005;11(9):3353–3362. doi: 10.1158/1078-0432.CCR-04-2062. [DOI] [PubMed] [Google Scholar]
- 33.Wallecha A, Maciag PC, Rivera S, Paterson Y, Shahabi V. Construction and characterization of an attenuated Listeria monocytogenes strain for clinical use in cancer immunotherapy. Clin Vaccine Immunol. 2009;16(1):96–103. doi: 10.1128/CVI.00274-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Barry RA, Bouwer HG, Portnoy DA, Hinrichs DJ. Pathogenicity and immunogenicity of Listeria monocytogenes small-plaque mutants defective for intracellular growth and cell-to-cell spread. Infect Immun. 1992;60(4):1625–1632. doi: 10.1128/iai.60.4.1625-1632.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tilney LG, Portnoy DA. Actin filaments and the growth, movement, and spread of the intracellular bacterial parasite, Listeria monocytogenes. J Cell Biol. 1989;109(4 Pt 1):1597–1608. doi: 10.1083/jcb.109.4.1597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hsieh CS, Macatonia SE, Tripp CS, Wolf SF, O’Garra A, Murphy KM (1993) Development of TH1 CD4+ T cells through IL-12 produced by Listeria-induced macrophages. Science (New York, NY 260 (5107):547–549 [DOI] [PubMed]
- 37.Ikonomidis G, Paterson Y, Kos FJ, Portnoy DA. Delivery of a viral antigen to the class I processing and presentation pathway by Listeria monocytogenes. J Exp Med. 1994;180(6):2209–2218. doi: 10.1084/jem.180.6.2209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Beatty GL, Paterson Y. Regulation of tumor growth by IFN-gamma in cancer immunotherapy. Immunol Res. 2001;24(2):201–210. doi: 10.1385/IR:24:2:201. [DOI] [PubMed] [Google Scholar]
- 39.Beck-Engeser GB, Monach PA, Mumberg D, Yang F, Wanderling S, Schreiber K, Espinosa R, III, Le Beau MM, Meredith SC, Schreiber H. Point mutation in essential genes with loss or mutation of the second allele: relevance to the retention of tumor-specific antigens. J Exp Med. 2001;194(3):285–300. doi: 10.1084/jem.194.3.285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gunn GR, Zubair A, Peters C, Pan ZK, Wu TC, Paterson Y. Two Listeria monocytogenes vaccine vectors that express different molecular forms of human papilloma virus-16 (HPV-16) E7 induce qualitatively different T cell immunity that correlates with their ability to induce regression of established tumors immortalized by HPV-16. J Immunol. 2001;167(11):6471–6479. doi: 10.4049/jimmunol.167.11.6471. [DOI] [PubMed] [Google Scholar]
- 41.Hussain SF, Paterson Y. CD4+ CD25+ regulatory T cells that secrete TGFbeta and IL-10 are preferentially induced by a vaccine vector. J Immunother. 2004;27(5):339–346. doi: 10.1097/00002371-200409000-00002. [DOI] [PubMed] [Google Scholar]
- 42.Maciag PC, Seavey MM, Pan ZK, Ferrone S, Paterson Y. Cancer immunotherapy targeting the high molecular weight melanoma-associated antigen protein results in a broad antitumor response and reduction of pericytes in the tumor vasculature. Cancer Res. 2008;68(19):8066–8075. doi: 10.1158/0008-5472.CAN-08-0287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Singh R, Dominiecki ME, Jaffee EM, Paterson Y. Fusion to Listeriolysin O and delivery by Listeria monocytogenes enhances the immunogenicity of HER-2/neu and reveals subdominant epitopes in the FVB/N mouse. J Immunol. 2005;175(6):3663–3673. doi: 10.4049/jimmunol.175.6.3663. [DOI] [PubMed] [Google Scholar]
- 44.Singh R, Paterson Y. In the FVB/N HER-2/neu transgenic mouse both peripheral and central tolerance limit the immune response targeting HER-2/neu induced by Listeria monocytogenes-based vaccines. Cancer Immunol Immunother. 2007;56(6):927–938. doi: 10.1007/s00262-006-0237-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Chakravarty PK, Guha C, Alfieri A, Beri V, Niazova Z, Deb NJ, Fan Z, Thomas EK, Vikram B. Flt3L therapy following localized tumor irradiation generates long-term protective immune response in metastatic lung cancer: its implication in designing a vaccination strategy. Oncology. 2006;70(4):245–254. doi: 10.1159/000096288. [DOI] [PubMed] [Google Scholar]
- 46.Meng Y, Carpentier AF, Chen L, Boisserie G, Simon JM, Mazeron JJ, Delattre JY. Successful combination of local CpG-ODN and radiotherapy in malignant glioma. Int J Cancer. 2005;116(6):992–997. doi: 10.1002/ijc.21131. [DOI] [PubMed] [Google Scholar]
- 47.Kim KW, Kim SH, Shin JG, Kim GS, Son YO, Park SW, Kwon BH, Kim DW, Lee CH, Sol MY, Jeong MH, Chung BS, Kang CD. Direct injection of immature dendritic cells into irradiated tumor induces efficient antitumor immunity. Int J Cancer. 2004;109(5):685–690. doi: 10.1002/ijc.20036. [DOI] [PubMed] [Google Scholar]
- 48.Chakraborty M, Abrams SI, Coleman CN, Camphausen K, Schlom J, Hodge JW. External beam radiation of tumors alters phenotype of tumor cells to render them susceptible to vaccine-mediated T-cell killing. Cancer Res. 2004;64(12):4328–4337. doi: 10.1158/0008-5472.CAN-04-0073. [DOI] [PubMed] [Google Scholar]
- 49.Tseng CW, Trimble C, Zeng Q, Monie A, Alvarez RD, Huh WK, Hoory T, Wang MC, Hung CF, Wu TC. Low-dose radiation enhances therapeutic HPV DNA vaccination in tumor-bearing hosts. Cancer Immunol Immunother. 2009;58(5):737–748. doi: 10.1007/s00262-008-0596-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Pavlenko M, Leder C, Roos AK, Levitsky V, Pisa P. Identification of an immunodominant H-2D(b)-restricted CTL epitope of human PSA. Prostate. 2005;64(1):50–59. doi: 10.1002/pros.20221. [DOI] [PubMed] [Google Scholar]
- 51.Shang XY, Chen HS, Zhang HG, Pang XW, Qiao H, Peng JR, Qin LL, Fei R, Mei MH, Leng XS, Gnjatic S, Ritter G, Simpson AJ, Old LJ, Chen WF. The spontaneous CD8+ T-cell response to HLA-A2-restricted NY-ESO-1b peptide in hepatocellular carcinoma patients. Clin Cancer Res. 2004;10(20):6946–6955. doi: 10.1158/1078-0432.CCR-04-0502. [DOI] [PubMed] [Google Scholar]
- 52.Dasu A. Is the alpha/beta value for prostate tumours low enough to be safely used in clinical trials? Clin Oncol (R Coll Radiol) 2007;19(5):289–301. doi: 10.1016/j.clon.2007.02.007. [DOI] [PubMed] [Google Scholar]
- 53.King CR, Fowler JF. A simple analytic derivation suggests that prostate cancer alpha/beta ratio is low. Int J Radiat Oncol Biol Phys. 2001;51(1):213–214. doi: 10.1016/S0360-3016(01)01651-0. [DOI] [PubMed] [Google Scholar]
- 54.Fowler J, Chappell R, Ritter M. Is alpha/beta for prostate tumors really low? Int J Radiat Oncol Biol Phys. 2001;50(4):1021–1031. doi: 10.1016/S0360-3016(01)01607-8. [DOI] [PubMed] [Google Scholar]
- 55.Pollack A, Zagars GK, Smith LG, Lee JJ, von Eschenbach AC, Antolak JA, Starkschall G, Rosen I. Preliminary results of a randomized radiotherapy dose-escalation study comparing 70 Gy with 78 Gy for prostate cancer. J Clin Oncol. 2000;18(23):3904–3911. doi: 10.1200/JCO.2000.18.23.3904. [DOI] [PubMed] [Google Scholar]
- 56.Higano CS, Schellhammer PF, Small EJ, Burch PA, Nemunaitis J, Yuh L, Provost N, Frohlich MW. Integrated data from 2 randomized, double-blind, placebo-controlled, phase 3 trials of active cellular immunotherapy with sipuleucel-T in advanced prostate cancer. Cancer. 2009;115(16):3670–3679. doi: 10.1002/cncr.24429. [DOI] [PubMed] [Google Scholar]
- 57.Neeson P, Pan ZK, Paterson Y. Listeriolysin O is an improved protein carrier for lymphoma immunoglobulin idiotype and provides systemic protection against 38C13 lymphoma. Cancer Immunol Immunother. 2008;57(4):493–505. doi: 10.1007/s00262-007-0388-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Gulley J, Chen AP, Dahut W, Arlen PM, Bastian A, Steinberg SM, Tsang K, Panicali D, Poole D, Schlom J, Michael Hamilton J. Phase I study of a vaccine using recombinant vaccinia virus expressing PSA (rV-PSA) in patients with metastatic androgen-independent prostate cancer. Prostate. 2002;53(2):109–117. doi: 10.1002/pros.10130. [DOI] [PubMed] [Google Scholar]
- 59.Heiser A, Coleman D, Dannull J, Yancey D, Maurice MA, Lallas CD, Dahm P, Niedzwiecki D, Gilboa E, Vieweg J. Autologous dendritic cells transfected with prostate-specific antigen RNA stimulate CTL responses against metastatic prostate tumors. J Clin Invest. 2002;109(3):409–417. doi: 10.1172/JCI14364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Williams SA, Xu Y, De Marzo AM, Isaacs JT, Denmeade SR. Prostate-specific antigen (PSA) is activated by KLK2 in prostate cancer ex vivo models and in prostate-targeted PSA/KLK2 double transgenic mice. Prostate. 2010;70(7):788–796. doi: 10.1002/pros.21111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Boike TP, Lotan Y, Cho LC, Brindle J, DeRose P, Xie XJ, Yan J, Foster R, Pistenmaa D, Perkins A, Cooley S, Timmerman R. Phase I dose-escalation study of stereotactic body radiation therapy for low- and intermediate-risk prostate cancer. J Clin Oncol. 2011;29(15):2020–2026. doi: 10.1200/JCO.2010.31.4377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Grills IS, Martinez AA, Hollander M, Huang R, Goldman K, Chen PY, Gustafson GS. High dose rate brachytherapy as prostate cancer monotherapy reduces toxicity compared to low dose rate palladium seeds. J Urol. 2004;171(3):1098–1104. doi: 10.1097/01.ju.0000113299.34404.22. [DOI] [PubMed] [Google Scholar]
- 63.Bonner JA, Harari PM, Giralt J, Azarnia N, Shin DM, Cohen RB, Jones CU, Sur R, Raben D, Jassem J, Ove R, Kies MS, Baselga J, Youssoufian H, Amellal N, Rowinsky EK, Ang KK. Radiotherapy plus cetuximab for squamous-cell carcinoma of the head and neck. N Engl J Med. 2006;354(6):567–578. doi: 10.1056/NEJMoa053422. [DOI] [PubMed] [Google Scholar]
- 64.D’Amico AV, Chen MH, Renshaw AA, Loffredo B, Kantoff PW. Risk of prostate cancer recurrence in men treated with radiation alone or in conjunction with combined or less than combined androgen suppression therapy. J Clin Oncol. 2008;26(18):2979–2983. doi: 10.1200/JCO.2007.15.9699. [DOI] [PubMed] [Google Scholar]
- 65.Maciag PC, Radulovic S, Rothman J. The first clinical use of a live-attenuated Listeria monocytogenes vaccine: a phase I safety study of Lm-LLO-E7 in patients with advanced carcinoma of the cervix. Vaccine. 2009;27(30):3975–3983. doi: 10.1016/j.vaccine.2009.04.041. [DOI] [PubMed] [Google Scholar]
- 66.Radulovic S, Brankovic-Magic M, Malisic E, Jankovic R, Dobricic J, Plesinac-Karapandzic V, Maciag PC, Rothman J. Therapeutic cancer vaccines in cervical cancer: phase I study of Lovaxin-C. J BUON. 2009;14(Suppl 1):S165–S168. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Figure 1: Tumor response in representative mice on d34 from each of the cohorts: A) PSA Vaccine, B), PSA Vaccine +RT, C)RT Alone, D) No Treatment and E) Control Vaccine. (TIFF 3668 kb)
Supplemental Figure 2: Representative wells after subjecting the splenocytes from each cohort to ELISpot analysis. A) Non-specific stimulation with PMA, B) Negative control stimulation with BSA, and C-G stimulation with PSA, C) PSA Vaccine, D), PSA Vaccine +RT, E)RT Alone, F) No Treatment and G) Control Vaccine. (TIFF 276 kb)
Supplemental Figure 3: FACS analysis for IFN-γ in CD8+CD3+ cells. A) PSA Vaccine, B), PSA Vaccine +RT, C)RT Alone, D) No Treatment and E) Control Vaccine. (TIFF 3480 kb)