Abstract
A fundamental challenge in administering immunotherapies for cancer is the establishment of biomarkers that can predict patients’ responsiveness to treatment. In this study, our aim was to predict the immunologic and clinical responses of vaccination therapy with an Ii-key-modified HER-2/neu peptide (Ii-key/HER-2(776–790) or AE37), applied in our recent phase I study in patients with prostate cancer. To this end, we retrospectively analyzed our data derived from immunologic determinations before, during and after primary series of vaccinations with AE37, as well as after one AE37 booster injection. Using the obtained data, we then observed the relationship between the immunologic parameters and clinical outcome of patients. We found that preexisting levels of transforming growth factor beta (TGF-β) had an inverse correlation with in vivo and in vitro immunologic responses to the AE37 vaccine which were measured as delayed-type hypersensitivity (DTH) and interferon gamma (IFN-γ) production in response to the native HER-2(776–790) (or AE36) peptide, respectively. Patients with preexistent IFN-γ immunity to AE36 developed positive DTH reactions after primary vaccinations and booster. Moreover, we could detect a direct correlation between IFN-γ production and DTH reactions in response to AE36 challenge in our vaccinated patients. DTH reactions were a stronger indicator for patients’ overall survival (OS) than preexistent or vaccine-induced IFN-γ immunity. In contrast, we found that preexisting TGF-β levels were correlated with shorter patients’ OS. These retrospective analyses suggest that the above biomarkers at the time-points measured offer promise for evaluating immunologic and clinical responses to AE37-based vaccinations.
Keywords: AE37, HER-2/neu vaccine, TGF-β, IFN-γ, DTH, Prostate cancer
Introduction
Developing effective therapeutic vaccines for prostate cancer is still a challenging issue, which requires further understanding of tumor progression and proper clinical trial design. Limiting toxic effects of chemotherapeutic agents and prolonging survival rate are promising purposes of active immunotherapy in prostate cancer. Results from clinical trials demonstrated that prostate cancer vaccines are safe with low toxicity [1]. Recent immunotherapy trials in prostate cancer have indicated that active immune responses can be achieved with therapeutic cancer vaccines, providing long-term clinical benefit for cancer patients [2, 3]. The relatively indolent nature of prostate cancer, compared with some other types of metastatic disease, allows time for an immune response to be generated, making it a good candidate for immune-based therapies [4]. Recently, sipuleucel-T, a type of active autologous cellular immunotherapy (the first vaccine which got an FDA approval), demonstrated its effectiveness in reducing the risk of death in metastatic castration-resistant prostate cancer [4]. However, beyond sipuleucel-T, several novel immunotherapies are currently in development, and enrollment in clinical trials should be considered [2, 4, 5]. Despite encouraging results from vaccination trials in prostate cancer, still there is a significant need to further improve clinical efficacy. The proper clinical design as well as combining vaccines with other treatments is essential for developing an effective prostate cancer vaccine strategy. Moreover, the methods of response evaluations in vaccination strategies should be standardized and the best surrogate markers should be chosen for optimizing vaccine activity to select the best treatment schedules.
A common feature of prostate cancer cells is the autocrine production of growth factors promoting tumorigenicity and loss of tumor suppressor function [6, 7]. Therefore, it is important to find biological markers that will reflect the risk of locoregional progression and metastases in order to improve the patient outcome. TGF-β has pleiotropic effects on adaptive immunity, especially in the regulation of effector and regulatory CD4+ T cell responses, mainly acting as a suppressive element [8]. In addition, TGF-β is a key regulator in carcinogenesis [9]. Loss of TGF-β sensitivity in carcinoma cells is frequently accompanied by increased expression of TGF-β in the same cells [10]. TGF-β is found to be elevated in cancer cells compared to normal epithelial cells and appears to be even more elevated in poorly differentiated tumors. In prostate cancer, increased local expression of TGF-β has been associated with higher tumor grade, increased invasiveness and metastatic progression [11].
Immunizing against a specific tumor antigen enables the comparison of various assays to measure tumor-specific immunity which can be statistically assessed in terms of their validity to act as surrogate endpoints that correlate with clinical outcomes. Delayed-type hypersensitivity (DTH) reactions represent a reliable measurement, of the few used, to assess effective vaccination targeting tumor antigens [12]. Immunologic monitoring from clinical trials proposes that DTH reactions may represent a consistent in vivo immunologic process which reflects the development of systemic anti-tumor immunity in cancer patients after vaccination [13–16]. Another equally important issue is to analyze the function of effector cells during immune-based treatments. Analysis of vaccine-driven cytokines expression provides a functional property of effector T lymphocytes. IFN-γ secretion measurement, mainly by ELISPOT, has been widely applied to detect frequencies of functional effector T cells [17–19].
Work from our laboratory has shown that the HER-2(776–790) epitope serves as a compelling tumor antigen and that CD4+ T cells primed with the synthetic HER-2(776–790) peptide help autologous CTL for increased antitumor activity [20, 21]. We have shown that HER-2(776–790) chemically linked to a tetra-peptide from the invariant chain of MHC class II molecules (Ii-key/HER-2(776–790) hybrid peptide or AE37) induces more potent immunologic responses both in vitro and in vivo compared with the non-modified HER-2(776–790) peptide (AE36) [22]. In a phase I trial, we have immunized 29 prostate cancer patients with AE37 plus GM-CSF as for an adjuvant. The vaccine was given monthly for 6 months and was well tolerated with minimal toxicity. AE37-induced strong immunologic responses in vivo (DTH) and in vitro (IFN-γ production) could be measured in the majority of patients and was correlated with decreases in TGF-β plasma levels [16]. Long-term immunity to AE37 was still detectable 6 months post-vaccinations and could be considerably prolonged for an additional period of 36 months after one single booster AE37 injection [23].
Herein, by retrospectively analyzing the data from our AE37 trial, we addressed a critical challenge in immune-based treatments of cancer: finding biomarkers acting as surrogates that can predict patients’ responsiveness to treatment.
Materials and methods
Study design
A detailed description of the phase I trial design, time schedule for vaccinations and immune monitoring have been described elsewhere [16, 23]. In brief, the study included patients who received one single booster injection with AE37 after primary vaccinations. Patients were castrate-sensitive and non-metastatic (n = 16), castrate-resistant and metastatic (n = 4), castrate-sensitive and metastatic (n = 2) and one patient was castrate-resistant and non-metastatic. Analyses were performed by comparing data from immune monitoring performed 1 month after the last (6th) vaccination (R6). Long-term (LT) assessment was done 6 months after the last vaccination. The booster injection was given just after LT and long-term booster (LTB) was performed 1 month later.
Immunologic assays
Methods for the evaluation of in vivo responses by DTH and in vitro responses by IFN-γ ELISPOT as well as determination of TGF-β levels in plasma samples by ELISA have been previously reported [16].
Statistical considerations
The immunologic response was analyzed after primary vaccinations (R6 and LT) and after booster (LTB) against baseline (i.e., preexisting) TGF-β and IFN-γ or DTH at R6. By analyzing TGF-β and IFN-γ responses, patients were subgrouped according to their baseline values for TGF-β levels and IFN-γ-specific spots (i.e., above/equal or below, the respective median value). Positive and negative DTH responses at R6 (orthogonal mean ≥ or <5 mm, respectively) were considered as an additional criterion for subgrouping patients when comparing DTH vs. in vitro immunity to AE36 and OS. In a second model, comparisons between DTH and IFN-γ changes were made while on-study, at R6, LT and LTB. Using standard approaches, we determined current survival status for all patients on the trial. OS was calculated from the date of enrollment on-study to death or the date of last follow-up. A secondary OS analysis was done from the time of disease diagnosis. GraphPad Prism version 5 software was used for statistical analysis of data. The nonparametric Mann–Whitney t test with a 95 % confidence interval was used for statistical evaluation of patient groups at different time-points. Linear regression and nonparametric Spearman’s test were applied for correlation analyses. Kaplan–Meier curves and log-rank test were used for the evaluation of OS. Statistically significant differences were considered when the p value was ≤0.05.
Results
Preexisting TGF-β levels correlate with the magnitude of in vitro and in vivo vaccine-induced immunologic responses
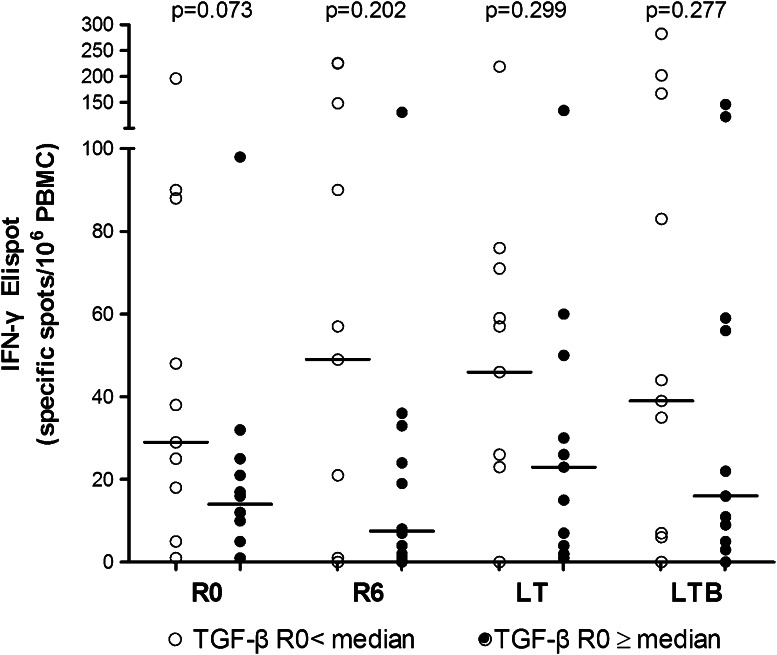
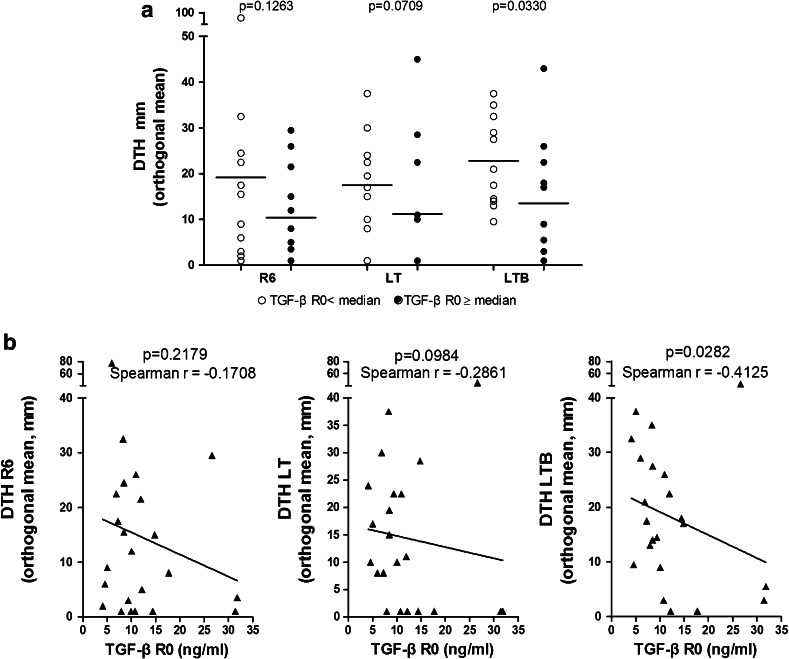
We have stratified our patients (n = 23) who had received a booster with AE37 6 months after primary vaccinations [23], in two groups based on their TGF-β plasma levels determined at R0 (i.e., pre-vaccination): those with values above/equal (n = 12) or below (n = 11) median TGF-β (high or low TGF-β producers, respectively) [23]. As shown in Fig. 1, low TGF-β producers had increased vaccine-induced frequencies of IFN-γ-producing T cells (IFN-γ immunity) against the native, AE36, peptide as compared with high TGF-β producers. Interestingly, this inverse correlation between TGF-β and IFN-γ immunity levels could even be detected before vaccinations (R0) at which time-period was even more intense reaching levels close to significance (Fig. 1). An inverse correlation was also observed when analyzing pre-vaccination TGF-β levels vs. AE36-DTH reactions: there was a strong trend for higher DTH reactions in the group of low TGF-β producers vs. the high TGF-β producers during LT, which reached significance at LTB (Fig. 2a). Regression analyses between TGF-β plasma levels at R0 and DTH reactions at R6, LT and LTB also demonstrated a significant correlation between TGF-β at R0 and DTH at LTB (Fig. 2b, right panel).
Fig. 1.
Inverse correlation between preexisting (R0) TGF-β levels and in vitro IFN-γ production in response to stimulation with AE36 either pre (R0)- or after vaccinations (1 and 6 months later, R6 and LT, respectively) and 1 month after AE37 booster (LTB). (Open circle), patients (n = 11) with preexisting TGF-β levels lower than the median TGF-β at R0 (9.87 ng/mL, as determined in [23] ) and (filled circle), patients (n = 12) with preexisting TGF-β levels higher or equal than the median TGF-β at R0. Bars represent median values
Fig. 2.
a Inverse correlation between preexisting TGF-β levels and in vivo AE37-induced immunity to the native AE36 peptide measured as DTH at the indicated time-points. See also legend to Fig. 1. b Linear regression analysis of DTH change on study (DTH measurements at the indicated time-points) and pre-vaccine TGF-β levels
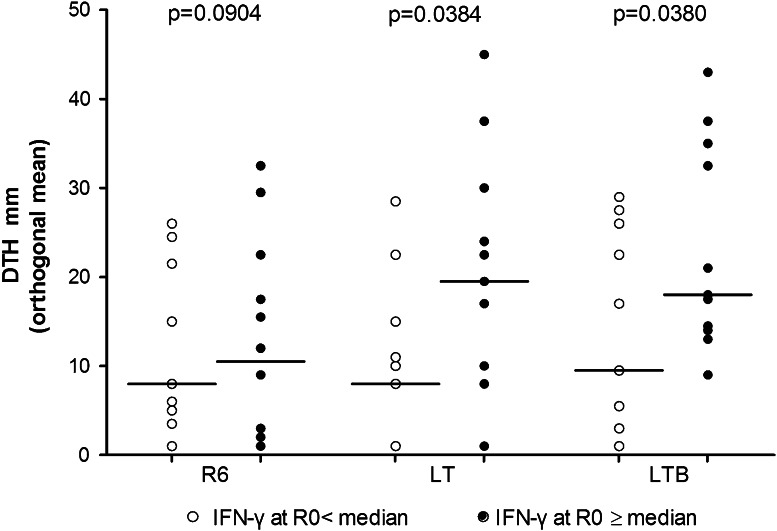
Preexisitng IFN-γ responses to AE36 correlate with positive vaccine-induced DTH reactions
We also compared preexisting IFN-γ immunity with DTH reactions during the course of vaccinations. As in the previous paragraph, our patients were subgrouped according to the levels of their IFN-γ immunity at R0: those who were above or equal (high producers) (n = 12) and those who were below (low producers) to median IFN-γ production (n = 11) [23]. As shown in Fig. 3, high producers developed significantly higher DTH reactions over low producers at later time-points after the end of primary vaccinations (LT and LTB).
Fig. 3.
Preexisting IFN-γ immunity to AE36 correlates with increased DTH reactions. (Open circle), patients (n = 11) with preexisting, (R0), IFN-γ immunity to AE36 at levels lower than the median AE36-induced IFN-γ immunity at R0 (17 specific spots/106 PBMC, as determined in [23] ) and (filled circle), patients (n = 12) with preexisting IFN-γ levels higher or equal to the median IFN-γ at R0. Bars represent median values
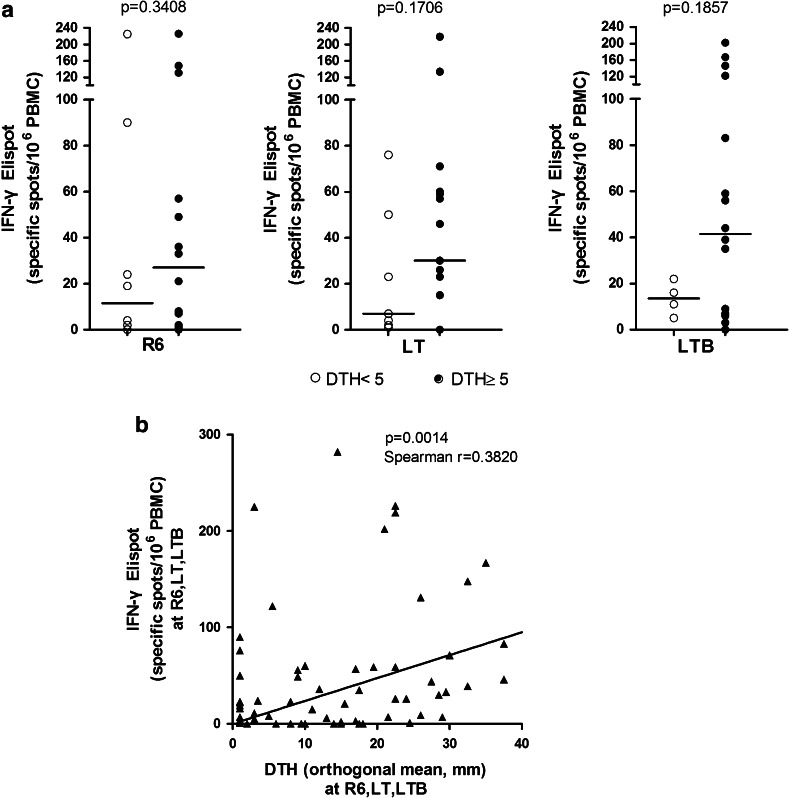
Correlations between vaccine-induced DTH reactions and IFN-γ immunity
Individualized skin tests against AE36 were placed at R6 for the same patients, as in the previous paragraphs. DTH tests <5 mm and ≥5 mm were categorized as negative and positive, respectively, and were correlated with values from in vitro IFN-γ-based ELISPOT assays against AE36 which were performed (for each one of the skin tested patients) at R6, LT and LTB. We have compared DTH ≥ 5 mm versus DTH < 5 mm, as we [16] and others [15, 24] have considered the 5-mm induration threshold as discriminating between vaccine responders from non-responders. Also in this case, there was a trend for increased levels of IFN-γ immunity in the group of patients with positive DTH (n = 15), [vs. those with negative DTH (n = 8)], which was more evident at later time-periods post primary vaccinations (Fig. 4a). Given the importance of defining immunologic surrogates predicting response to vaccination, we also analyzed patients’ individual values for IFN-γ and DTH levels throughout vaccinations. As shown in Fig. 4b, there was a statistical significant correlation observed between increases in IFN-γ and DTH responses.
Fig. 4.
a DTH responders (n = 15) (filled circle), produce higher IFN-γ levels in response to stimulation with the AE36 peptide in vitro, than DTH non-responders (n = 8) (open circle). Comparisons were made during R6, LT and LTB. b Linear regression analysis of DTH and IFN-γ changes on study (DTH and IFN-γ measurements at the indicated time-points)
Correlates with overall survival (OS)
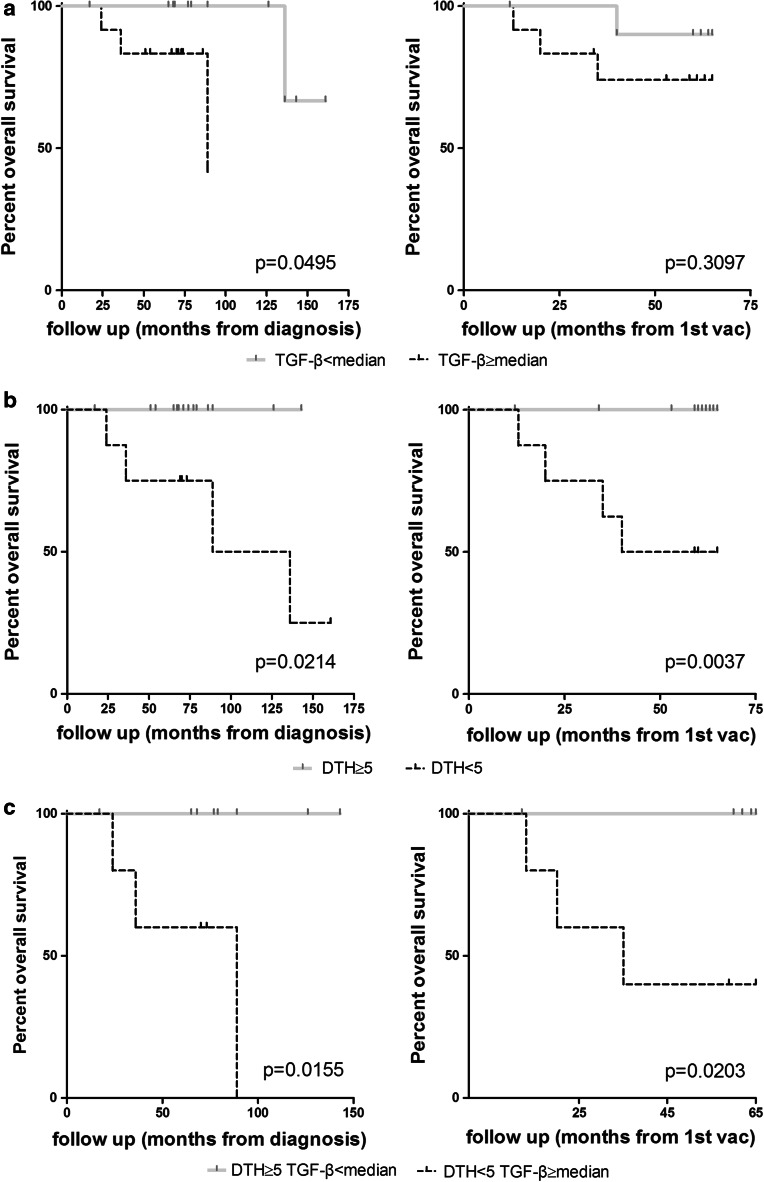
Figure 5 shows the median OS (mOS) of the study population from the time of diagnosis and from first vaccination. At a median follow-up from diagnosis of 73 months (range 17–161 months), mOS to the group of low TGF-β producers (n = 11) was not reached, whereas mOS for high TGF-β producers (n = 12) was 89 months (p < 0.045; Fig. 5a, left). mOS was not reached in either group when this was calculated from first vaccination (median follow-up 60 months; range 12–65 months) with a trend toward increased mOS for low TGF-β producers (p = 0.3097; Fig. 5a, right). We also analyzed mOS of our vaccinated patients by DTH reactions after the primary series of vaccinations (R6). As depicted in Fig. 5b, all patients with positive DTH (n = 15) were still alive, whereas patients with negative DTH (n = 8) had a mOS of 112.5 months (p = 0.0214; Fig. 5b, left). These 2 groups also demonstrated significant differences in mOS when this was calculated from first vaccination (not reached by those with positive DTH vs. 52.5 months by those with negative DTH; p < 0.0037) (Fig. 5b, right).
Fig. 5.
a Correlation between preexisting TGF-β levels and clinical outcome. Kaplan–Meier plots comparing the overall survival of vaccinated prostate cancer patient groups shown in Fig. 1. b Correlation between the strength of DTH reactions and clinical outcome. Kaplan–Meier plots comparing the overall survival of DTH responders versus DTH non-responders shown in Fig. 4. c Correlation between the strength of DTH reactions combined with preexisting TGF-β levels and clinical outcome. Kaplan–Meier plots comparing the overall survival of vaccinated patients who were DTH responders and had preexisting TGF-β levels lower than the median TGF-β at R0 (n = 8) versus DTH non-responders with preexisting TGF-β levels higher than the median TGF-β at R0 (n = 5)
We have also analyzed mOS in a group of patients who combined both low TGF-β production and positive DTH reactions (n = 8) vs. those with high TGF-β production and negative DTH reactions (n = 5). As expected, mOS was significantly higher in the former group (all patients alive) vs. the latter, irrespective of the date for OS calculation (Fig. 5c) and further improved when compared to single group analyses (see Fig. 5a, b).
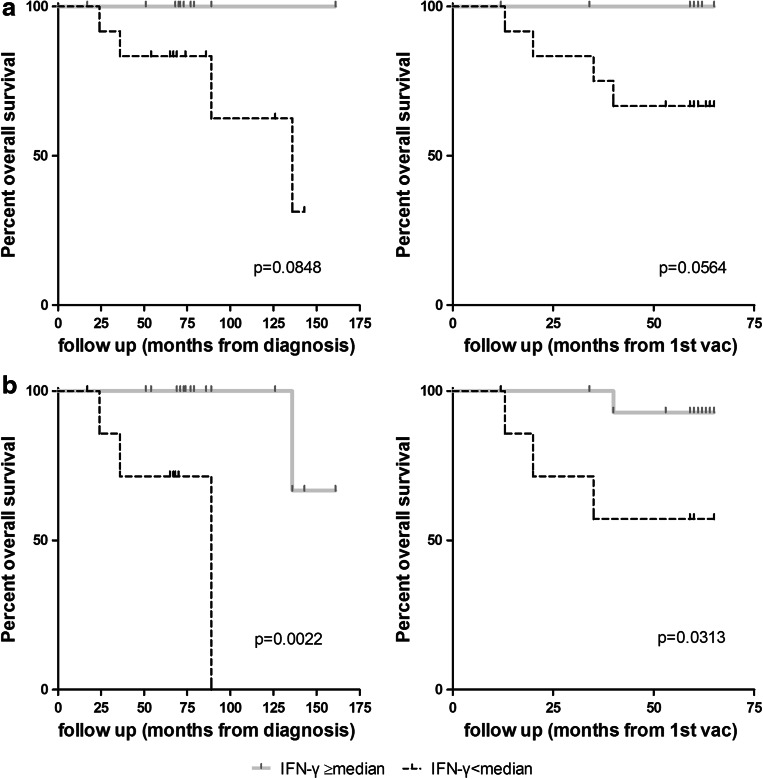
Preexisting IFN-γ immunity to the AE36 peptide was also positively correlated with OS. Thus, high IFN-γ producers (n = 12) in response to stimulation with AE36 before the onset of primary vaccinations (R0) had a trend for increased mOS vs. the low IFN-γ producers (n = 11) (Fig. 6a). Importantly, patients with increased vaccine-induced IFN-γ immunity after the end of primary vaccinations (LT) (n = 15) had a statistically significant increase in mOS vs. those with low IFN-γ responses at this time-period (n = 8) (Fig. 6b).
Fig. 6.
Correlation between preexisting and AE37-induced IFN-γ levels and clinical outcome. Kaplan–Meier plots comparing the overall survival of a vaccinated prostate cancer patient groups shown in Fig. 3 and b of patients who responded with increased IFN-γ production (higher or equal to the median of specific spots at R0) 6 months after the end of primary vaccinations (LT) (n = 15) vs. those who developed IFN-γ responses lower than the median (n = 8)
Discussion
Unlike conventional cytotoxic drugs, which act directly on the tumor, cancer immunotherapeutics (mostly in the form of cancer vaccines) demonstrate new kinetics involving the generation of specific cellular immune responses, which need to be translated into antitumor responses to eventually delay tumor progression and potentially result in improved survival [17]. This is the new concept of long-term benefit without immediate and marked reduction in tumor size which implies that, over the prospect of observing tumor growth while waiting for an immunotherapy to show clinical benefit, intermediate biomarkers to evaluate immunologic response in the absence of clinical response are required. Moreover, for improving clinical outcome, further to increasing vaccine potency and minimizing treatment-related toxicities, it is imperative to recognize prognostic/predictive biomarkers of clinical benefit that may guide to select and optimize the therapeutic strategies for patients most likely to gain benefit. By retrospectively analyzing the data from our AE37 phase I study vaccinating prostate cancer patients [16], we have identified biomarkers addressing these points. Our study demonstrates lower preexisting TGF-β plasma levels in patients who responded better immunologically to the AE37 vaccine (measured by DTH and IFN-γ-based ELISPOT assays) and survived longer compared to those having higher preexisting TGF-β levels. An even more significant correlation with preexisting TGF-β levels could be detected when OS was calculated form disease diagnosis. Furthermore, patients who had increased frequencies of preexisting T cells producing IFN-γ in response to stimulation with the native AE36 HER-2/neu peptide demonstrated significantly higher DTH reactions and enhanced survival as opposed to those with compromised preexisting immunity to AE36. A third finding was the positive correlation between in vivo (DTH) and in vitro (IFN-γ) immunity to AE36 after primary vaccinations and after booster. Finally, patients who developed positive DTH reactions demonstrated a significant survival benefit over those who had negative DTH reactions.
TGF-β plays an integral role in regulating immune responses having pleiotropic effects on adaptive immunity, especially in the regulation of the function of effector CD8+ and CD4+ T cells as well as of regulatory CD4+ T cell responses [25]. Raised TGF-β serum concentrations were independently detected in patients with various types of cancer and were associated with poor survival [26]. Retrospective analyses of data from published clinical studies have discovered a pattern of 7 cytokines, also including TGF-β, potentially representing a manifestation of the underlying systemic immune response in the cancer patients who were included in those studies and also suggesting a prognostic and predictive role of this cytokine platform [26]. Herein, we show that pre-vaccination levels of TGF-β may act both as prognostic and predictive factors for OS and vaccine-induced immunity, respectively. We tend to believe that the levels of this suppressive mediator at enrollment may determine the extent of AE37-induced immunity not only during early vaccinations but also throughout the primary vaccination period and later on (i.e., LT, LTB and LTI). In fact, our recent report demonstrated an inverse correlation between TGF-β levels throughout and post-primary vaccinations and post-booster with ΑΕ37-induced AE36-specific IFN-γ immunity [23]. The present follow-up analysis from the time of first diagnosis revealed a significantly improved survival for the group of vaccinated patients who exhibited lower TGF-β plasma levels. We have not tested TGF-β levels for the time-period between first diagnosis to enrollment and thus we cannot be certain whether TGF-β high or low producers at enrollment behaved similarly during this period. Notwithstanding, we may speculate that expression levels of TGF-β, if low, may positively regulate patients’ overall immune status which then could be decisive not only for enabling the generation of robust immunity during active immunotherapies, but also for improving patients’ benefit from standard therapies. In such a case, standard therapies (ranging from chemotherapies to androgen-directed approaches) could act synergistically with the endogenous antitumor immunity producing measurable clinical benefits in addition to extending survival.
Another important finding is the inverse relation between preexisting TGF-β with IFN-γ immunity to the AE36 peptide. Thus, lower preexisting TGF-β levels in patients were correlated with higher preexisting IFN-γ immunity, which supports the above speculation. This situation at pre-vaccination may also satisfactorily justify the increased immunity induced during and after vaccination and after booster resulting in prolonged OS. At this point, we should stress that the way our phase I study was designed, does not allow drawing any conclusions as to whether this less suppressed spontaneous immunity along with previous standard therapies has taken much of the responsibility for patients’ survival benefit over the immunity elicited by the AE37 vaccine. Another possible explanation could be provided by an interaction between both types of immunity which suggests that the immunity induced during vaccinations with AE37 boosts preexisting antitumor immune responses. Recent data from our laboratory show that preexisting frequencies of PSA-specific CD8+ T cells were enhanced during vaccinations (unpublished observations), thus supporting the latter possibility (however, without excluding the former one).
Our results also indicate that significant DTH responses, which develop in cancer patients post-immunization, are, potentially, a reflection of the development of systemic cell-mediated IFN-γ immunity. More important, the magnitude of DTH reactions was highly correlated with survival benefit. In fact, our results show that the development of tumor antigen-specific DTH responses was a stronger indicator for OS than preexistent or vaccine-induced IFN-γ immunity. In a previous study, de Vries [27] investigated the predictive value of vaccine-specific T cells in biopsies from DTH challenges and showed that the presence of such cells within the DTH sites correlated with clinical outcome. In a recent report [14], vaccine-specific T cells in melanoma patients who had clinical benefit from vaccination with melanoma peptides pulsed DCs were readily detected in DTH biopsies but were largely undetected in peripheral blood. Coulie et al. [28] detected only low frequencies of vaccine-specific T cells in peripheral blood in melanoma patients who demonstrated large shrinkage of their metastatic lesions. Sensitized memory CD4+ T lymphocytes of the Th1 phenotype have been found to represent the lymphocyte subpopulation responsible for initiating a DTH response [29]. Then, the development of a positive DTH reaction is mediated by the release of Th1 cytokines by these memory CD4+ T cells followed by the accumulation of cytotoxic CD8+ T cells, macrophages and other inflammatory cells [29]. Recruitment of memory CD4+ T cells to the DTH site is a specific process as activated CD4+ T cells express chemokine receptors which are involved in their recruitment [29, 30]. Thus, the conditions to obtain positive DTH reactions are more stringent in that the vaccine-specific memory T cells have to migrate and proliferate in vivo, and this might select for high-quality cytotoxic CD8+ T cells capable of eradicating tumor in vivo. On the other hand, the frequencies of vaccine-specific T cells in peripheral blood samples may vary widely when collected at different time-points hampering to a certain extent the accuracy of assays applied. This may become more evident, in the field of cancer immunotherapy, by the generally low frequencies of circulating tumor antigen-specific T cells reported in patients [31]. It should be also considered that depending on the kinetics of their peak response to vaccine-challenge (or rechallenge), the vaccine-specific T (memory) cells by the time of blood collection may have sequestered at primary or secondary lymphoid organs or other tissues and therefore will not be detectable in blood samples. To overcome this obstacle, it is important to know the optimal time during a vaccine regimen for measuring the development of systemic vaccine-induced immunity, which by itself is a difficult task, mostly due to its dependence on various factors including the nature of the vaccine and the adjuvant, but also the stage and type of the vaccinated cancer patients.
In the clinical development paradigm for cancer vaccines, it is highly required to evaluate the immunologic profile of the responder and to correlate immunologic data with clinical response. Moreover, the methods of response evaluations in vaccination strategies should be standardized and the best surrogate markers should be chosen for optimizing vaccine activity to select the best treatment schedules. It should be emphasized that the findings described in this study are hypothesis-generating only, since no final conclusions can be drawn due to the relatively small number of patients and the heterogeneity of the sampled patient population. However, based on the retrospective analysis of the results of our phase I trial, a new phase II trial is warranted to validate the roles of TGF-β, IFN-γ and DTH as biomarkers for assessing vaccine efficacy both in terms of immunologic and clinical responses.
Conflict of interest
The authors declare that they have no conflict of interest.
Abbreviations
- DTH
Delayed-type hypersensitivity
- FDA
Food and drug administration
- GM-CSF
Granulocyte–macrophage colony-stimulating factor
- IFN-γ
Interferon gamma
- LT
Long term
- LTB
Long-term booster
- LTI
Long-term immunity
- OS
Overall survival
- TGF-β
Transforming growth factor beta
References
- 1.Di Lorenzo G, Buonerba C, Kantoff PW. Immunotherapy for the treatment of prostate cancer. Nat Rev Clin Oncol. 2011;8:551–561. doi: 10.1038/nrclinonc.2011.72. [DOI] [PubMed] [Google Scholar]
- 2.Cheng ML, Fong L. Beyond sipuleucel-T: immune approaches to treating prostate cancer. Curr Treat Options Oncol. 2014;15:115–126. doi: 10.1007/s11864-013-0267-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.May KF, Jr, Gulley JL, Drake CG, Dranoff G, Kantoff PW. Prostate cancer immunotherapy. Clin Cancer Res. 2011;17:5233–5238. doi: 10.1158/1078-0432.CCR-10-3402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schlom J. Therapeutic cancer vaccines: current status and moving forward. J Natl Cancer Inst. 2012;104:599–613. doi: 10.1093/jnci/djs033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Baxevanis CN. Outlining novel scenarios for improved therapeutic cancer vaccines: the PANVAC paradigm. Expert Rev Vaccines. 2012;11:275–277. doi: 10.1586/erv.11.193. [DOI] [PubMed] [Google Scholar]
- 6.Cowen D, Troncoso P, Khoo VS, Zagars GK, von Eschenbach AC, Meistrich ML, Pollack A. Ki-67 staining is an independent correlate of biochemical failure in prostate cancer treated with radiotherapy. Clin Cancer Res. 2002;8:1148–1154. [PubMed] [Google Scholar]
- 7.Khor LY, Bae K, Paulus R, et al. MDM2 and Ki-67 predict for distant metastasis and mortality in men treated with radiotherapy and androgen deprivation for prostate cancer: RTOG 92-02. J Clin Oncol. 2009;27:3177–3184. doi: 10.1200/JCO.2008.19.8267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Travis MA, Sheppard D. TGF-beta activation and function in immunity. Annu Rev Immunol. 2014;32:51–82. doi: 10.1146/annurev-immunol-032713-120257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bierie B, Moses HL. Tumour microenvironment: TGFbeta: the molecular Jekyll and Hyde of cancer. Nat Rev Cancer. 2006;6:506–520. doi: 10.1038/nrc1926. [DOI] [PubMed] [Google Scholar]
- 10.Steiner MS, Zhou ZZ, Tonb DC, Barrack ER. Expression of transforming growth factor-beta 1 in prostate cancer. Endocrinology. 1994;135:2240–2247. doi: 10.1210/endo.135.5.7956947. [DOI] [PubMed] [Google Scholar]
- 11.Barrack ER. TGF beta in prostate cancer: a growth inhibitor that can enhance tumorigenicity. Prostate. 1997;31:61–70. doi: 10.1002/(SICI)1097-0045(19970401)31:1<61::AID-PROS10>3.0.CO;2-M. [DOI] [PubMed] [Google Scholar]
- 12.Disis ML, Schiffman K, Gooley TA, McNeel DG, Rinn K, Knutson KL. Delayed-type hypersensitivity response is a predictor of peripheral blood T-cell immunity after HER-2/neu peptide immunization. Clin Cancer Res. 2000;6:1347–1350. [PubMed] [Google Scholar]
- 13.Holmes JP, Benavides LC, Gates JD, et al. Results of the first phase I clinical trial of the novel II-key hybrid preventive HER-2/neu peptide (AE37) vaccine. J Clin Oncol. 2008;26:3426–3433. doi: 10.1200/JCO.2007.15.7842. [DOI] [PubMed] [Google Scholar]
- 14.Lesterhuis WJ, Schreibelt G, Scharenborg NM, et al. Wild-type and modified gp100 peptide-pulsed dendritic cell vaccination of advanced melanoma patients can lead to long-term clinical responses independent of the peptide used. Cancer Immunol Immunother. 2011;60:249–260. doi: 10.1007/s00262-010-0942-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lopez MN, Pereda C, Segal G, et al. Prolonged survival of dendritic cell-vaccinated melanoma patients correlates with tumor-specific delayed type IV hypersensitivity response and reduction of tumor growth factor beta-expressing T cells. J Clin Oncol. 2009;27:945–952. doi: 10.1200/JCO.2008.18.0794. [DOI] [PubMed] [Google Scholar]
- 16.Perez SA, Kallinteris NL, Bisias S, et al. Results from a phase I clinical study of the novel Ii-Key/HER-2/neu(776–790) hybrid peptide vaccine in patients with prostate cancer. Clin Cancer Res. 2010;16:3495–3506. doi: 10.1158/1078-0432.CCR-10-0085. [DOI] [PubMed] [Google Scholar]
- 17.Hoos A, Eggermont AM, Janetzki S, et al. Improved endpoints for cancer immunotherapy trials. J Natl Cancer Inst. 2010;102:1388–1397. doi: 10.1093/jnci/djq310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ishikawa T, Kokura S, Sakamoto N, et al. Whole blood interferon-gamma levels predict the therapeutic effects of adoptive T-cell therapy in patients with advanced pancreatic cancer. Int J Cancer. 2013;133:1119–1125. doi: 10.1002/ijc.28117. [DOI] [PubMed] [Google Scholar]
- 19.Zamarron BF, Chen W. Dual roles of immune cells and their factors in cancer development and progression. Int J Biol Sci. 2011;7:651–658. doi: 10.7150/ijbs.7.651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Perez SA, von Hofe E, Kallinteris NL, Gritzapis AD, Peoples GE, Papamichail M, Baxevanis CN. A new era in anticancer peptide vaccines. Cancer. 2010;116:2071–2080. doi: 10.1002/cncr.24988. [DOI] [PubMed] [Google Scholar]
- 21.Sotiriadou NN, Kallinteris NL, Gritzapis AD, et al. Ii-Key/HER-2/neu(776–790) hybrid peptides induce more effective immunological responses over the native peptide in lymphocyte cultures from patients with HER-2/neu+ tumors. Cancer Immunol Immunother. 2007;56:601–613. doi: 10.1007/s00262-006-0213-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Voutsas IF, Gritzapis AD, Mahaira LG, Salagianni M, von Hofe E, Kallinteris NL, Baxevanis CN. Induction of potent CD4+ T cell-mediated antitumor responses by a helper HER-2/neu peptide linked to the Ii-Key moiety of the invariant chain. Int J Cancer. 2007;121:2031–2041. doi: 10.1002/ijc.22936. [DOI] [PubMed] [Google Scholar]
- 23.Perez SA, Anastasopoulou EA, Tzonis P, Gouttefangeas C, Kalbacher H, Papamichail M, Baxevanis CN. AE37 peptide vaccination in prostate cancer: a 4-year immunological assessment updates on a phase I trial. Cancer Immunol Immunother. 2013;62:1599–1608. doi: 10.1007/s00262-013-1461-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Reyes D, Salazar L, Espinoza E, et al. Tumour cell lysate-loaded dendritic cell vaccine induces biochemical and memory immune response in castration-resistant prostate cancer patients. Br J Cancer. 2013;109:1488–1497. doi: 10.1038/bjc.2013.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Prud’homme GJ. Pathobiology of transforming growth factor beta in cancer, fibrosis and immunologic disease, and therapeutic considerations. Lab Invest. 2007;87:1077–1091. doi: 10.1038/labinvest.3700669. [DOI] [PubMed] [Google Scholar]
- 26.Lippitz BE. Cytokine patterns in patients with cancer: a systematic review. Lancet Oncol. 2013;14:e218–e228. doi: 10.1016/S1470-2045(12)70582-X. [DOI] [PubMed] [Google Scholar]
- 27.de Vries IJ, Bernsen MR, Lesterhuis WJ, et al. Immunomonitoring tumor-specific T cells in delayed-type hypersensitivity skin biopsies after dendritic cell vaccination correlates with clinical outcome. J Clin Oncol. 2005;23:5779–5787. doi: 10.1200/JCO.2005.06.478. [DOI] [PubMed] [Google Scholar]
- 28.Coulie PG, Karanikas V, Colau D, Lurquin C, Landry C, Marchand M, Dorval T, Brichard V, Boon T. A monoclonal cytolytic T-lymphocyte response observed in a melanoma patient vaccinated with a tumor-specific antigenic peptide encoded by gene MAGE-3. Proc Natl Acad Sci USA. 2001;98:10290–10295. doi: 10.1073/pnas.161260098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Vukmanovic-Stejic M, Reed JR, Lacy KE, Rustin MH, Akbar AN. Mantoux test as a model for a secondary immune response in humans. Immunol Lett. 2006;107:93–101. doi: 10.1016/j.imlet.2006.08.002. [DOI] [PubMed] [Google Scholar]
- 30.Nacher M, Blazquez AB, Shao B, Matesanz A, Prophete C, Berin MC, Frenette PS, Hidalgo A. Physiological contribution of CD44 as a ligand for E-selectin during inflammatory T-cell recruitment. Am J Pathol. 2011;178:2437–2446. doi: 10.1016/j.ajpath.2011.01.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Singh SK, Tummers B, Schumacher TN, et al. The development of standard samples with a defined number of antigen-specific T cells to harmonize T cell assays: a proof-of-principle study. Cancer Immunol Immunother. 2013;62:489–501. doi: 10.1007/s00262-012-1351-0. [DOI] [PMC free article] [PubMed] [Google Scholar]