Abstract
Aplasia cutis congenita (ACC) is a group of rare heterogeneous disorders characterised by absent areas of skin at birth. The majority of cases involve the scalp region. ACC limited to one lower limb is extremely rare. We report an usual case of ACC limited to the left thigh of which healing occurred in utero. The case was managed conservatively and the disease course has been favourable with no limitations in limb function and an entirely normal development. Most cases of ACC are self-healing, justifying a conservative approach. This holds further true for ACC limited to one lower limb where the majority of cases reported to date show a favourable disease course with minimal conservative treatment.
Keywords: Dermatology, Skin, Medical management, Dermatological
Background
Aplasia cutis congenita (ACC) is a group of rare heterogeneous disorders characterised by localised or widespread areas of skin defects at birth.1 The prevalence is estimated to be 5.1 in 100.000 births.2 Lesions may occur at various depths with sometimes even the complete absence of bone tissue.2 ACC may occur as an isolated finding or in association with genetic syndromes with impaired development.2 The majority of cases (96.4%) appear in the scalp region.2 ACC involving the limbs often occurs bilaterally.3 Isolated defects limited to one lower limb are extremely rare.4 5 We report an unusual case of ACC limited to the left thigh of which healing occurred in utero.
Case presentation
A male term neonatal patient presented with an atrophic plaque on the left thigh which had been present since birth.
There was no relevant disease, drug or family history of the mother in her 30s. Before the pregnancy was discovered, the mother had used the morning-after pill. Meconium-stained amniotic fluid was observed during labour without any other signs of fetal distress.
The patient was born at 40 weeks and 6 days through a non-traumatic vaginal delivery with a weight of 3735 g, head circumference of 36.4 cm and excellent Apgar scores (9/10/10). The placenta was clinically normal and blood gas analysis revealed no abnormalities. Physical examination revealed no dysmorphic features or blistering. However, a well-demarcated gyriform-shaped erythematous atrophic plaque of 1.5 by 2 cm with central purple discolouration was observed on the lateral side of the left thigh (figure 1A). Dermatoscopy revealed erythema and white streaks centrally with telangiectasia at the border (figure 1B).
Figure 1.
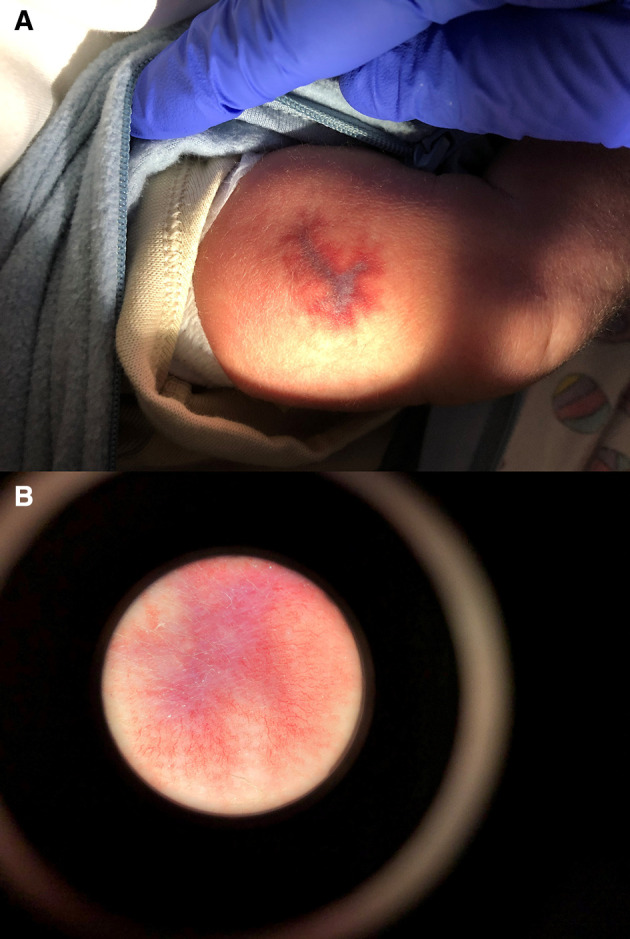
(A) Clinical features on the day of birth: a well-demarcated gyriform-shaped erythematous atrophic plaque of 1.5 by 2 cm with central purple discolouration on the lateral side of the left thigh. (B) Dermatoscopic features on the day of birth: erythema and white streaks centrally with telangiectasia at the border.
Outcome and follow-up
A localised livedo reticularis, cutis marmorata telangiectatica congenital (CMTC), congenital Volkmann ischaemic contracture and ACC were considered. Since the lesion did not improve with warming, a livedo reticularis was ruled out. A CMTC was considered unlikely due to the absence of other anomalies such as limb asymmetry and no signs of neurological impairment. Also, an echo performed after 6 months revealed scar tissue reaching the fascia without involvement of the underlying muscles. The lesion was managed conservatively with vaseline, and at follow-up after 3 months, an atrophic mobile scar was observed (figure 2). Based on the clinical features and disease course, a diagnosis of ACC at the limb was made. The function of the left leg and the development of the patient have been entirely normal.
Figure 2.
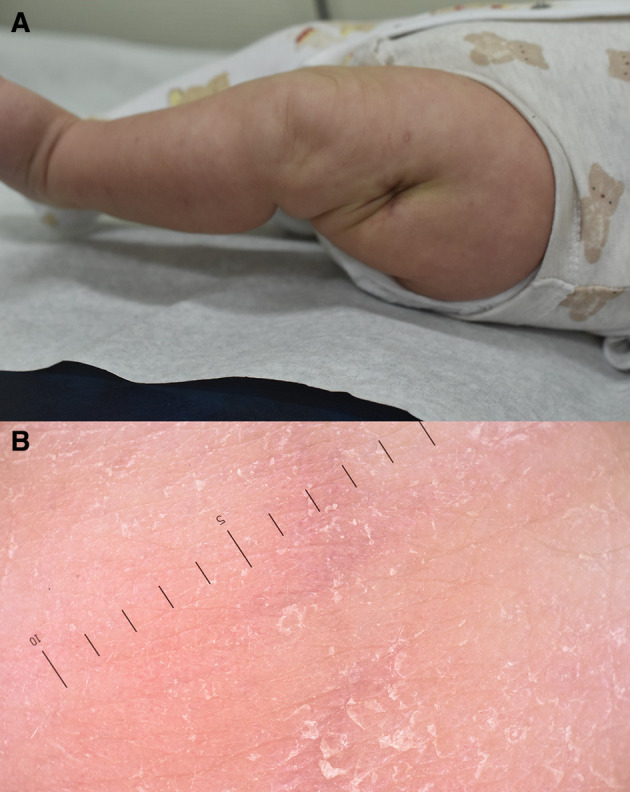
(A) Clinical features 3 months after birth. (B) Dermatoscopic features 3 months after birth.
Discussion
ACC is a group of rare heterogeneous disorders characterised by absent areas of skin at birth.1 Clinically, ACC appears as a well-demarcated ulcerated skin defect, however, the defect may also heal in utero.1 Histopathological findings are non-specific.5 The aetiology of ACC is unknown.2 The most widely accepted pathophysiological model describes a disruption of skin during fetal development.6 ACC can be due to exogenous factors such as placental infarcts, intrauterine infections, trauma and teratogenic substances.6 Teratogenic substances implicated in the pathogenesis of ACC include methimazole, valproic acid, benzodiazepines, diclofenac and heparin.2 ACC can also be associated with several genetic syndromes with impaired mental and physical development such as Adams-Oliver syndrome and Johanson-Blizzard syndrome.2 The only known gene that has been associated with non-syndromic ACC is BMS1 which has been described in a five-generation family with autosomal dominant inherited ACC.7
ACC can be classified into nine different groups according to Frieden.1 Our case is best classified as type VII ACC since the lesion was located on the left thigh without other anomalies. It is not clear whether the morning-after pill has any effect on the pathophysiology of ACC.
Similar to ACC involving the upper limb and/or occurring bilaterally,8–12 ACC limited to one lower limb is extremely rare. To date, only five cases4 5 13–15 have been reported with type VII ACC limited to one lower limb (table 1).
Table 1.
Cases with type VII ACC limited to one lower limb
| Author | Gestational age | Location | Associated skin defects, blistering and/or malformations | Relevant maternal and/or family history | Histology | Treatment | Disease course |
| Current case | 40 weeks and 6 days | Atrophic skin lesion of 1.5 by 2 cm on the lateral side of the left thigh | No | No | N/A | Vaseline ointment | Spontaneous healing with minor scar formation and normal limb function |
| Freire-Maia et al (1980)14 | Unknown | Skin defect on the pretibial area of the right leg extending to the medial side of the foot | Unknown | Unknown | Unknown | Vitamin A sterile gauze dressings | Spontaneous healing with scar formation, limb function unknown |
| Bigliardi et al (2004)4 | 41 weeks | Widespread ulceration of the pretibial area, knee and distal part of the thigh of the right leg | No | No | Non-specific inflammatory infiltrate in the dermis with proliferation of blood vessels | Silver sulfadiazine ointment and wet gauze dressings | Spontaneous healing with minor scar formation and normal limb function |
| Lee et al (2008)5 | 39 weeks | Large ulcer of 20 cm on the right leg extending from the knee to the medial dorsal of the foot | No | No | Absent epidermis, inflammatory infiltrate and proliferation of blood vessels in the dermis | Mupirocin ointment and wet petroleum gauze dressings | Spontaneous healing with minor scar formation and normal limb function |
| Pająk et al (2014)15 | 25 weeks | A sharply demarcated skin defect of 4 by 1.5 cm extending into the subcutaneous tissue on the medial side of the right thigh | A superficial skin defect on the penis which healed spontaneously after a few days without scar tissue, no other skin defects, blistering and/or malformations | Anhydramnios and cervical incompetence, elevated markers of inflammation and cervical swab with enterococcus faecalis, caesarean section due to impending asphyxia | N/A | Mupirocin ointment and hydrofiber with silver ion dressings, sutures to approximate the skin, hydrogel and silver ointment dressings | Healing with minor scar formation and normal limb function |
| Doi et al (2022)13 | 39 weeks | Large skin defect on the left leg extending from the patella to the medial side of the ankle | No | No | Absent epidermis, appendages with proliferation of blood vessels in the dermis | Petroleum jelly and gentamicin ointment | Spontaneous healing, scar formation and limb function unknown |
ACC, aplasia cutis congenita.
Bigliardi et al 4 report a male term neonatal patient with a widespread ulceration of the pretibial area, knee and distal part of the thigh on the right leg. The birth had been through forceps delivery with a clinically normal placenta. Management had been conservative with silver sulfadiazine ointment and wet gauze dressings. Spontaneous healing with minor scar formation occurred within 3 months.
Lee et al 5 describe a male term neonatal patient with an ulcer of 20 cm on the right leg extending from the knee to the medial dorsal of the foot. The birth had been through vaginal delivery. Treatment consisted of mupirocin ointment and wet petroleum gauze dressings, and follow-up after 2 years revealed minimal scar formation.
Doi et al 13 report a female neonatal patient with a large skin defect on the left leg extending from the patella to the medial side of the ankle. Treatment was conservative with petroleum jelly and gentamicin ointment, and healing occurred after 2 months. An X-ray performed after 3 months showed a slightly shorter left tibia compared with the right side. No contractures were observed after 1 year.
Freire-Maia et al 14 describe a female neonatal patient from consanguineous parents with a skin defect on the pretibial area of the right leg extending to the medial side of the foot. Labour had been normal, and the patient was otherwise healthy. The lesion was managed conservatively with vitamin A sterile gauze dressings and healing occurred after a few months with scar formation.
In three cases4 5 13 (data was lacking for Freire-Maia et al 14), there were no skin defects, blistering or malformations anywhere else on the body, and there was no relevant maternal and family history. The function of the limb as well as the development of the patients has been normal.
Pająk et al 15 report a premature male born after 25 weeks of gestation by caesarean section due to impending asphyxia with Apgar scores of 4/6/6. The pregnancy was complicated by anhydramnios and cervical incompetence after which cervical cerclage was performed in the 18th week of gestation. The mother had elevated markers of inflammation the week before birth and a swab from the cervix the day before birth showed enterococcus faecalis after which treatment was initiated with betamethasone and intravenous ampicillin. After birth, a sharply demarcated skin defect of 4 by 1.5 cm extending into the subcutaneous tissue was observed on the medial side of the right thigh. Besides a superficial skin defect on the penis which healed spontaneously after a few days without scar tissue, no other skin defects, blistering or malformations were seen elsewhere on the body. The patient was admitted to the neonatal intensive care unit due to respiratory failure, pneumonia and retinopathy of prematurity. Wound swabs were taken from the lesion which showed no pathogens and treatment consisted of mupirocin ointment and hydrofiber with silver ion dressings. After 4 days, the wound was treated surgically by single non-absorbable sutures approximating the skin. The sutures were removed after 1 week and due to wound dehiscence centrally, adhesive external sutures were placed in combination with hydrogel and silver ointment dressings. Follow-up after 14 months showed little scar formation with no functional impairment of the leg.
Most cases of ACC are self-healing.6 This holds further true for type VII ACC limited to one lower limb where all cases reported to date show a favourable disease course with minimal treatment,4 5 13–15 justifying a conservative approach. Surgical treatment in type VII ACC of the lower limb may be advised such as reported by Pająk et al 15 in which surgical treatment was performed due to the extreme prematurity of the patient. Even then, surgical treatment had been minimally invasive with only sutures to approximate the skin with afterwards no limitation in limb function and a favourable disease course.
Interestingly, Neri et al 16 describe a case of type VII ACC located on the upper limb with a similar aspect and signs of limb dysfunction without apparent neurological involvement in which more extensive surgical treatment was performed by debridement of the ulceration followed by a reconstructive skin graft and occupational therapy with afterwards a favourable disease course.
Therefore, surgical treatment should be considered depending on clinical aspects such as the depth of the lesion, limb function, prematurity and potential concerns regarding scarring. In addition, ACC is a clinical diagnosis and if a biopsy is deemed necessary, an ultrasound should be performed to image the size and depth of the lesion to avoid damage to the underlying structures and to guide potential surgical interventions.17
The appearance of the lesion in our case suggests in utero healing as no ulceration or other skin defects were observed at birth. This is to our knowledge the first case report of type VII ACC limited to one lower limb of which healing occurred in utero.
Learning points.
Aplasia cutis congenita (ACC) involving the limbs often occurs bilaterally, isolated defects limited to one lower limb are extremely rare.
ACC is a clinical diagnosis, a biopsy is often not necessary.
Most cases of type VII ACC limited to the lower limb are self-healing, justifying a conservative approach.
Footnotes
Contributors: KTQ and LEV were responsible for drafting of the text, sourcing and editing of clinical images, investigation results, drawing original diagrams and algorithms, and critical revision for important intellectual content. KTQ, CW, KvM and LEV gave final approval of the manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Case reports provide a valuable learning resource for the scientific community and can indicate areas of interest for future research. They should not be used in isolation to guide treatment choices or public health policy.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Consent obtained from parent(s)/guardian(s).
References
- 1. Frieden IJ. Aplasia cutis congenita: a clinical review and proposal for classification. J Am Acad Dermatol 1986;14:646–60. 10.1016/s0190-9622(86)70082-0 [DOI] [PubMed] [Google Scholar]
- 2. Coi A, Barisic I, Garne E, et al. Epidemiology of aplasia cutis congenita: a population‐based study in Europe. Acad Dermatol Venereol 2023;37:581–9. 10.1111/jdv.18690 [DOI] [PubMed] [Google Scholar]
- 3. Ahčan U, Janeič T. Management of aplasia cutis congenita in a non-scalp location. British Journal of Plastic Surgery 2002;55:530–2. 10.1054/bjps.2002.3915 [DOI] [PubMed] [Google Scholar]
- 4. Bigliardi PL, Braschler C, Kuhn P, et al. Unilateral aplasia cutis congenita on the leg. Pediatr Dermatol 2004;21:454–7. 10.1111/j.0736-8046.2004.21406.x [DOI] [PubMed] [Google Scholar]
- 5. Lee JS, Yun SJ, Lee JB, et al. A case of aplasia cutis congenita, type VII. Ann Dermatol 2008;20:70–3. 10.5021/ad.2008.20.2.70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Brackenrich J, Brown A. Aplasia cutis congenita. In: StatPearls. Treasure Island (FL): StatPearls Publishing, 2022. [PubMed] [Google Scholar]
- 7. Marneros AG. BMS1 is mutated in aplasia cutis congenita. PLoS Genet 2013;9:e1003573. 10.1371/journal.pgen.1003573 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Davidson AW, Hosalkar HS, Hill RA, et al. Radial dysplasia with localized cutis aplasia congenita. J Pediatr Orthop B 2003;12:398–401. 10.1097/01.bpb.0000060283.77027.5f [DOI] [PubMed] [Google Scholar]
- 9. Droubi D, Rothman IL. Aplasia cutis congenita of the arm with associated radial dysplasia: case report, review of the literature, and proposed classification. Pediatr Dermatol 2014;31:356–9. 10.1111/j.1525-1470.2012.01876.x [DOI] [PubMed] [Google Scholar]
- 10. Mushtaq S, Nofal A. Frieden’s type 7 aplasia cutis congenita in a premature neonate. J Dtsch Dermatol Ges 2021;19:766–7. 10.1111/ddg.14418 [DOI] [PubMed] [Google Scholar]
- 11. Amaaoune F, Chakiri R. Congenital cutaneous aplasia of the limbs: a case report. Ann Med Surg (Lond) 2022;76:103496. 10.1016/j.amsu.2022.103496 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Li G, Zhang A, Yang S, et al. Type VII aplasia cutis congenita in neonates related to maternal HBV infection. Clin Cosmet Investig Dermatol 2023;16:499–504. 10.2147/CCID.S396071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Doi C, Muto J, Yatsuzuka K, et al. A case of aplasia cutis congenita type VII with tibial dysplasia. Clin Exp Dermatol 2022;47:412–3. 10.1111/ced.14900 [DOI] [PubMed] [Google Scholar]
- 14. Freire-Maia N, Pinheiro M, Ortega CC. Recessive aplasia cutis congenita of the limbs. J Med Genet 1980;17:123–6. 10.1136/jmg.17.2.123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Pająk A, Szczygieł A, Paluszyńska D, et al. Congenital skin aplasia on the lower limb in a premature infant with ELBW--case report. Ital J Pediatr 2014;40:88. 10.1186/s13052-014-0088-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Neri I, Magnano M, Pini A, et al. Congenital volkmann syndrome and aplasia cutis of the forearm: a challenging differential diagnosis. JAMA Dermatol 2014;150:978–80. 10.1001/jamadermatol.2014.111 [DOI] [PubMed] [Google Scholar]
- 17. Humphrey SR, Hu X, Adamson K, et al. A practical approach to the evaluation and treatment of an infant with aplasia cutis congenita. J Perinatol 2018;38:110–7. 10.1038/jp.2017.142 [DOI] [PubMed] [Google Scholar]


