ABSTRACT
Laparoscopic adjustable gastric band (LAGB) surgery is now an uncommon bariatric procedure; however, complications may still be encountered. A 64-year-old man with a history of LAGB placement 13 years prior presented with 2 months of epigastric pain. He endorsed chronic heavy nonsteroidal anti-inflammatory drug use. Computed tomography showed inflammation around the LAGB tubing with near-complete, circumferential erosion of the LAGB into the fundus. Upper endoscopy confirmed erosion of the LAGB along with port tubing into the gastroesophageal junction and fundus. The patient was referred to a foregut surgeon who performed robotic band removal.
KEYWORDS: gastric band, band erosion, bariatric, NSAID use
INTRODUCTION
Laparoscopic adjustable gastric band (LAGB) surgery was a popular bariatric procedure option in the late 1990s and early 2000s. Following publication of sleeve gastrectomy outcomes in 2008, LAGB utilization rapidly declined.1 The American Society for Metabolic and Bariatric Surgery estimated that gastric banding accounted for only 1.2% of bariatric surgeries in 2020, down from 35.4% in 2011.2 Although less common now, late LAGB complications including ischemia, pseudoachalasia, and band erosion may still be encountered.3
Band erosion is uncommon and rarely reported beyond 10 years postplacement. Erosion at 11 and 15 years are among the longest procedure-to-erosion onset times reported in the literature.4–6 Case reports highlight the dangers of LAGB erosion, including gastric emphysema or distal migration which can, respectively, lead to emphysematous gastritis or obstruction with perforation.6,7 Therefore, identification of risk factors toward LAGB erosion is critical. We report a case of near-complete intraluminal LAGB erosion, 13 years after initial placement and in the setting of heavy nonsteroidal anti-inflammatory drug (NSAID) use.
CASE REPORT
A 64-year-old man with a history of LAGB placement in 2010 presented with 2 months of progressive epigastric pain with meals. Pertinent history regarding his LAGB included a severe port site infection 6 months after his procedure, with subsequent port and tubing replacement. Afterward, he had denied further procedure related adverse events. During this new presentation, he noted the pain resembled that of his prior port site infection, although he denied fevers and chills. The patient also denied dysphagia, nausea, emesis, regurgitation, diarrhea, melena, and hematochezia. Further history revealed that the patient had been taking up to 12 ibuprofen tablets per day, sometimes with aspirin powder, in the prior months for chronic joint and back pain.
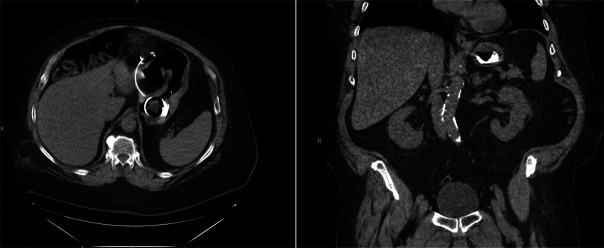
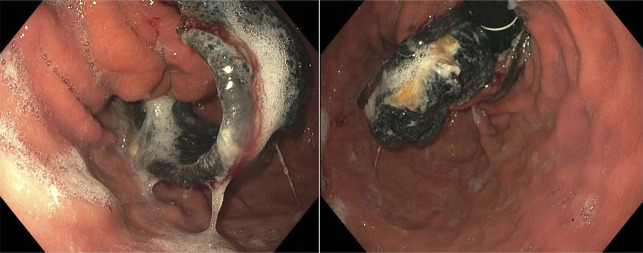
On evaluation, the patient was afebrile and hemodynamically stable. Physical examination was notable for epigastric tenderness to palpation but otherwise unremarkable. The patient had no significant laboratory abnormalities. Computed tomography of the abdomen revealed inflammatory changes surrounding the tubing and the adjacent fat, along with near-complete, circumferential erosion of the LAGB into the stomach (Figure 1). Barium esophagram did not demonstrate extravasation of contrast. Subsequently, upper endoscopy was performed and confirmed erosion of almost the entire LAGB along with port tubing into the gastroesophageal junction and fundus (Figure 2). The patient was referred to a foregut surgeon and underwent robotic removal of the LAGB and gastrojejunal tube placement.
Figure 1.
Computed tomography showing axial and coronal views of the eroded gastric band into the gastroesophageal junction and fundal region.
Figure 2.
Upper endoscopy confirming near circumferential erosion of the gastric band into the gastroesophageal junction and fundus.
DISCUSSION
The effectiveness of LAGB is reflected by a systematic review and meta-analysis by O'Brien et al, which showed a weighted mean excess weight loss percentage of 45.9% among 17 reports with at least 10 years of follow-up. This was unfortunately met with an average reoperation percentage of 47.8%.8 Despite this and the greater popularity of alternatives such as the gastric sleeve, a complex interaction of patient-centered factors may mean LAGB is still favored for some individuals.
LAGB placement can lead to wide variety of complications, including pouch dilation, band slippage, port infection, and band erosion.9 Median time to erosion varies greatly among reports, ranging from 8.5 to 48 months.5,10 Few reports demonstrate erosion beyond 10 years. At present, we identified 2 studies with erosion at 11 years and one report of an erosion 15 years post-LAGB placement.4–6 The lack of reports on erosion beyond 10 years is likely in part due to a high rate of band removal. A study in France with almost 53,000 patients showed an annual removal rate of 6%.11 While no definitive lifespan for LAGB exists, the mean time to removal was 6.75 years in one study.12 Another study showed only 45.2% of patients had their original band with a mean follow-up of 11.6 years.13 Repeating LAGB surgery for erosion seems to carry a markedly higher rate of re-erosion, cited at 27% in a retrospective cohort with 37 repeated LAGB placements following initial erosion. Patients who desire further weight loss or who regain weight can consider other bariatric surgeries such as Roux-en-Y gastric bypass.14
The etiology of LAGB erosion is likely multifactorial and includes variables such as trauma during placement, chronic ischemia from band compression, and surgeon experience.15,16 NSAIDs are known to induce gastric mucosal ischemia through inhibition of prostaglandin formation. As our patient had excessive NSAID intake, it is likely this contributed. Interestingly, despite heavy NSAID usage, the rest of our patient's visualized stomach and duodenum did not demonstrate gross inflammation or ulceration. Nonetheless, minimization of NSAIDs should be strongly encouraged in this population. Another potential risk factor is port site infection, which our patient had 6 months after his surgery, although he remained adverse event free for almost the next 13 years. In a study of 63 LAGB erosion cases, 8% of patients had prior port site infection.4
Prompt identification of LAGB erosion is crucial because distal migration and obstruction with perforation can occur.6,17 There is even reported gastric emphysema stemming from an eroded LAGB, which carries a high mortality risk.7 At present, there are limited guidelines on post-LAGB placement surveillance in asymptomatic patients. In 2020, the International Federation for the Surgery of Obesity and Metabolic Disorders recommended upper endoscopy on the basis of symptoms.18 The number of erosions is likely under-reported given that patients may experience asymptomatic erosion, as seen in a report by Yun et al.19 To counter the concern for under-diagnosis, some institutions may implement annual upper gastrointestinal series, with one group finding esophageal dilatation and dysmotility on upper gastrointestinal series in 47.9% of patients with asymptomatic LAGB.20
In conclusion, we present a case of late-onset LAGB erosion, 13 years after the initial placement. This case also demonstrates the utilization of upper endoscopy in diagnosis of an eroded LAGB. Gastroenterologists need to be vigilant in care of patients presenting with upper gastrointestinal symptoms especially in patients with prior LAGB placement. As this occurred alongside heavy NSAID use, appropriate counseling, follow-up, and routine medication reconciliation are imperative.
DISCLOSURES
Author contributions: Z. Makovich: document drafting, article guarantor; B. Patel: conceptualization of case report and critical revision.
Financial disclosure: None to report.
Previous presentation: A full abstract of this case report was presented at the 2023 American College of Gastroenterology (ACG) Conference; October 22, 2023; Vancouver, Canada.
Informed consent was obtained for this case report.
REFERENCES
- 1.Seeras K, Acho RJ, Prakash S. Laparoscopic gastric band placement. In: StatPearls. StatPearls Publishing: Treasure Island, FL, 2023. [PubMed] [Google Scholar]
- 2.ASMBS. Estimate of Bariatric Surgery Numbrs, 2011-2020. American Society for Metabolic and Bariatric Surgery: Newberry, FL, 32669, 2022. [Google Scholar]
- 3.Lim R, Beekley A, Johnson DC, Davis KA. Early and late complications of bariatric operation. Trauma Surg Acute Care Open. 2018;3(1):e000219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chisholm J, Kitan N, Toouli J, Kow L. Gastric band erosion in 63 cases: Endoscopic removal and rebanding evaluated. Obes Surg. 2011;21(11):1676–81. [DOI] [PubMed] [Google Scholar]
- 5.Himpens J, Cadière GB, Bazi M, Vouche M, Cadière B, Dapri G. Long-term outcomes of laparoscopic adjustable gastric banding. Arch Surg. 2011;146:802–7. [DOI] [PubMed] [Google Scholar]
- 6.Abeysekera A, Lee J, Ghosh S, Hacking C. Migration of eroded laparoscopic adjustable gastric band causing small bowel obstruction and perforation. BMJ Case Rep. 2017;2017:bcr2017219954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Su MZ, Munro WS. Gastric emphysema secondary to laparoscopic gastric band erosion. Int J Surg Case Rep. 2014;5(10):727–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.O'Brien PE, Hindle A, Brennan L, et al. Long-term outcomes after bariatric surgery: A systematic review and meta-analysis of weight loss at 10 or more years for all bariatric procedures and a single-centre review of 20-year outcomes after adjustable gastric banding. Obes Surg. 2019;29(1):3–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Eid I, Birch DW, Sharma AM, Sherman V, Karmali S. Complications associated with adjustable gastric banding for morbid obesity: A surgeon's guides. Can J Surg. 2011;54(1):61–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yoon CI, Pak KH, Kim SM. Early experience with diagnosis and management of eroded gastric bands. J Korean Surg Soc. 2012;82(1):18–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lazzati A, De Antonio M, Paolino L, et al. Natural history of adjustable gastric banding: Lifespan and revisional rate: A nationwide study on administrative data on 53,000 patients. Ann Surg. 2017;265(3):439–45. [DOI] [PubMed] [Google Scholar]
- 12.Kirshtein B, Kirshtein A, Perry Z, et al. Laparoscopic adjustable gastric band removal and outcome of subsequent revisional bariatric procedures: A retrospective review of 214 consecutive patients. Int J Surg. 2016;27:133–7. [DOI] [PubMed] [Google Scholar]
- 13.Trujillo MR, Muller D, Widmer JD, Warschkow R, Muller MK. Long-term follow-up of gastric banding 10 years and beyond. Obes Surg. 2016;26(3):581–7. [DOI] [PubMed] [Google Scholar]
- 14.Barreto SG, Chisholm J, Mehdorn AS, Collins J, Schloithe A, Kow L. Eroded gastric band: Where to next? An analysis of the largest contemporary series. Obes Surg. 2020;30(7):2469–74. [DOI] [PubMed] [Google Scholar]
- 15.Niville E, Dams A, Vlasselaers J. Lap-band erosion: Incidence and treatment. Obes Surg. 2001;11(6):744–7. [DOI] [PubMed] [Google Scholar]
- 16.Egberts K, Brown WA, O'Brien PE. Systematic review of erosion after laparoscopic adjustable gastric banding. Obes Surg. 2011;21(8):1272–9. [DOI] [PubMed] [Google Scholar]
- 17.Taskin M, Zengin K, Unal E. Intraluminal duodenal obstruction by a gastric band following erosion. Obes Surg. 2001;11(1):90–2. [DOI] [PubMed] [Google Scholar]
- 18.Quake SYL, Mohammadi-Zaniani G, Musbahi A, Old O, Courtney M, Small P. Routine use of esophago-gastro-duodenoscopy (EGD) in bariatric surgery-an international survey of our current practice. Obes Surg. 2022;32(11):3627–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yun GY, Kim WS, Kim HJ, et al. Asymptomatic gastric band erosion detected during routine gastroduodenoscopy. Clin Endosc. 2016;49(3):294–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Friedman DT, Duffy AJ. Outcomes of routine upper gastrointestinal series screening and surveillance after laparoscopic adjustable gastric banding. Surg Endosc. 2020;34(5):2178–83. [DOI] [PubMed] [Google Scholar]