Abstract
In vitro, engagement of GITR on Treg cells by the agonistic anti-GITR mAb, DTA-1, appears to abrogate their suppressive function. The consequence of in vivo engagement of GITR by DTA-1 is, however, less clear. In this study, we show that Treg cells isolated from DTA-1-treated mice were as potent as those from untreated mice in suppressing conventional CD4 T cells in vitro, indicating that in vivo GITR ligation does not disable Treg cells. Treatment of Foxp3/GFP knock-in mice with DTA-1 led to a selective reduction of circulating Treg cells, suggesting that DTA-1 is a depleting mAb which preferentially targets Treg cells. In tumour-bearing mice, DTA-1-mediated depletion of Treg cells was most marked in tumours but not in tumour-draining lymph node. These features were confirmed in an adoptive transfer model using tumour antigen-specific Treg cells. Interestingly, Treg cells detected in tumour tissues expressed much higher levels of GITR than those in tumour-draining lymph nodes, indicating that the efficiency of depletion might be correlated with the level of GITR expression. Finally, in vivo labelling of GITR in naive or tumour-bearing mice demonstrated that Treg cells constitutively expressed higher levels of GITR than conventional T cells, independent of location and activation state, consistent with the preferential in vivo depletion of Tregs by DTA-1. Thus, depletion of Treg cells represents a previously unrecognised in vivo activity of DTA-1 which has important implications for the application of anti-GITR antibodies in cancer immunotherapy.
Electronic supplementary material
The online version of this article (doi:10.1007/s00262-010-0866-5) contains supplementary material, which is available to authorized users.
Keywords: Anti-GITR, Regulatory T cells, Depletion, HY, Tumour, Therapy
Introduction
Glucocorticoid-induced tumour necrosis factor receptor (GITR), a member of the tumour necrosis factor receptor (TNFR) family is expressed on T lymphocytes with the primary function of protection from activation-induced cell death [1–3]. Under steady state conditions, CD4+CD25+Foxp3+ regulatory (Treg) cells constitutively express higher levels of GITR than conventional CD4 and CD8 T cells [4, 5]. The outcome of GITR signalling on Treg cells appears to be functional inactivation (i.e, neutralisation of inhibitory function) [4–6], whereas ligation of GITR on conventional T cells provides a co-stimulatory signal promoting activation [7–11].
Since ligation of GITR by DTA-1, an agonistic anti-GITR mAb, disables Treg whilst co-stimulating conventional T cells [12, 13], DTA-1 is an attractive reagent for enhancing T cell immunity against tumour cells [14–18]. Although the effectiveness of DTA-1 in cancer immunotherapy is well established, the mechanisms of action of DTA-1 are complicated by following factors. Firstly, the assumption that DTA-1 disarms Treg cells is based largely, if not exclusively, on in vitro data [4, 5], however, this conclusion has been challenged by a subsequent investigation [11]. Using co-cultures of Treg and conventional CD4 T cells from WT and GITR-deficient mice, Shevach and colleagues showed that GITR engagement on CD25−ve but not CD25+ve T cells is required for neutralising suppression, and the action of DTA-1 is to confer on CD25− T cells resistance to CD25+ve Treg-mediated inhibition, rather than by direct inactivation of Treg cells [11, 12]. Secondly, T cell behaviour in vivo cannot always be predicated on in vitro analysis, and few studies have addressed the impact of DTA-1 on Treg cells in vivo [19]. Inactivation [4, 15, 19], expansion [16] and depletion of Treg cells [20] are three possible outcomes of GITR ligation by DTA-1 on Treg cells. Although it has been proposed [12] and indicated [20] that DTA-1 depletes Tregs in vivo, a formal demonstration has not been made. Thirdly, expression of GITR on Treg has been largely, if not exclusively, investigated in vitro by comparing the pattern of expression before and after activation [4, 5, 11, 21]. In vivo, there is competition between target cells to bind injected antibody effectively lowering the number of molecules bound, in comparison with in vitro studies where an excess of conjugated antibody is used. Evaluation of GITR expression in real time is vital to understand the in vivo mechanisms of DTA-1 action.
To investigate in vivo GITR expression and determine whether DTA-1 selectively targets Treg cells for depletion, several strategies were adopted including the use of Foxp3/GFP knock-in mice [22] and adoptive transfer of tumour-antigen specific Treg cells [23]. Furthermore, a staining protocol enabling in vivo evaluation of GITR expression was developed.
Materials and methods
Mice
Thy1.2 C57BL/6 (B6) and CBA mice were purchased from Harlan Olac (Bicester, UK), and bred in the Central Biological Services Unit at Hammersmith Campus, Imperial College London. TCR-transgenic Marilyn [23] and Foxp3/GFP knock-in [22] mice were kindly provided by Dr. O Lantz and Dr. B Malissen, respectively. Marilyn mice used in this study were Thy1.1+ and Rag2+/−.
Tumour cell line, inoculation and measurement of tumour growth
MB49 is a chemically induced murine bladder carcinoma derived from a B6 male mouse [24]. MB49 cells were maintained in RPMI 1640 Medium (Gibco, UK) supplemented with 10% FCS, 10 mM HEPES, penicillin (100 IU/ml) and streptomycin (100 μg/ml), 5 × 10−5 M 2-ME and 2 mM l-glutamine. 5 × 105 MB49 cells were injected subcutaneously on the right flank of B6 and Foxp3/GFP knock-in mice. Tumour growth was measured every other day and recorded as longest dimension × shortest dimension in millimetres squared (mm2).
mAbs and treatment
DTA-1 is rat IgG2b mAb specific for mouse GITR [4]. GL-113 is rat IgG1 recognising β-galactosidase [25], and PC61 is rat IgG1 against mouse CD25 [26]. mAbs were partially purified from hybridoma culture supernatants by precipitation in 50% ammonium sulphate, and were further purified using protein G column. mAb treatment was conducted by intraperitoneal (i.p.) injection.
Purification of Treg and conventional CD4 T cells
To purify HY-specific Treg cells, spleen and pooled LN cells from Rag2+/− Marilyn females (Thy1.1) were incubated with anti-B220- and anti-CD8-Dynalbeads (Invitrogen, UK). After depletion of B and CD8 cells, the remaining cells were stained with anti-Vβ6FITC, anti-CD25PE and anti-CD4PE/Cy5 before sorting for CD4+CD25+Vβ6+ cells (HY-specific Treg cells). To isolate polyclonal Treg and conventional CD4 T cells from B6 mice, similar procedure was used except that anti-Vβ6FITC was omitted. FACS sorted CD4+CD25+ and CD4+CD25− cells were used as polyclonal Treg and conventional CD4 cells, respectively.
In vitro suppression assay
This was conducted as described previously [27]. In brief, conventional CD4 T cells, alone or mixed with Treg cells at various ratios, were stimulated with anti-CD3 mAb in the presence of accessory cells (irradiated T cell-depleted B6 spleen cells) in round-bottomed 96-well plates for 3 days. Thymidine was added to each well for the last 12 h and proliferation was measured by thymidine uptake.
Adoptive T cell transfer
FACS-sorted Marilyn Treg cells (Thy1.1+) were adoptively transferred to Thy1.2+ B6 female recipients by intravenous (i.v.) injection (1 × 105 /mouse).
FACS analysis
To detect donor cells (Thy1.1 Marilyn Treg) in recipient mice (Thy1.2 B6), the cells from MB49 and its draining lymph node were stained with anti-Vβ6PE, anti-Thy1.1PercP and anti-CD4APC. Donor cells were identified by co-expression of Thy1.1 and Vβ6. To measure the percentage of T cell subsets in MB49, the cells from MB49 tissues were stained with anti-CD4PercP and anti-CD8APC, or anti-CD4APC before intracellular anti-Foxp3FITC staining. Treg cells in Foxp3/GFP mice were identified by co-expression of CD4 and GFP.
In vivo GITR staining
This was conducted by i.v. injection of Foxp3/GFP mice with 5 μg of PE-conjugated DTA-1. GITR expression in T cell subsets was analysed by FACS after CD4 and CD8 staining, but without a further staining of GITR.
Statistical analysis
This was performed using a two-sided Student’s t test and GraphPad Prism software (version 3.02).
Results
Rejection of established MB49 tumours by a single dose of DTA-1 treatment
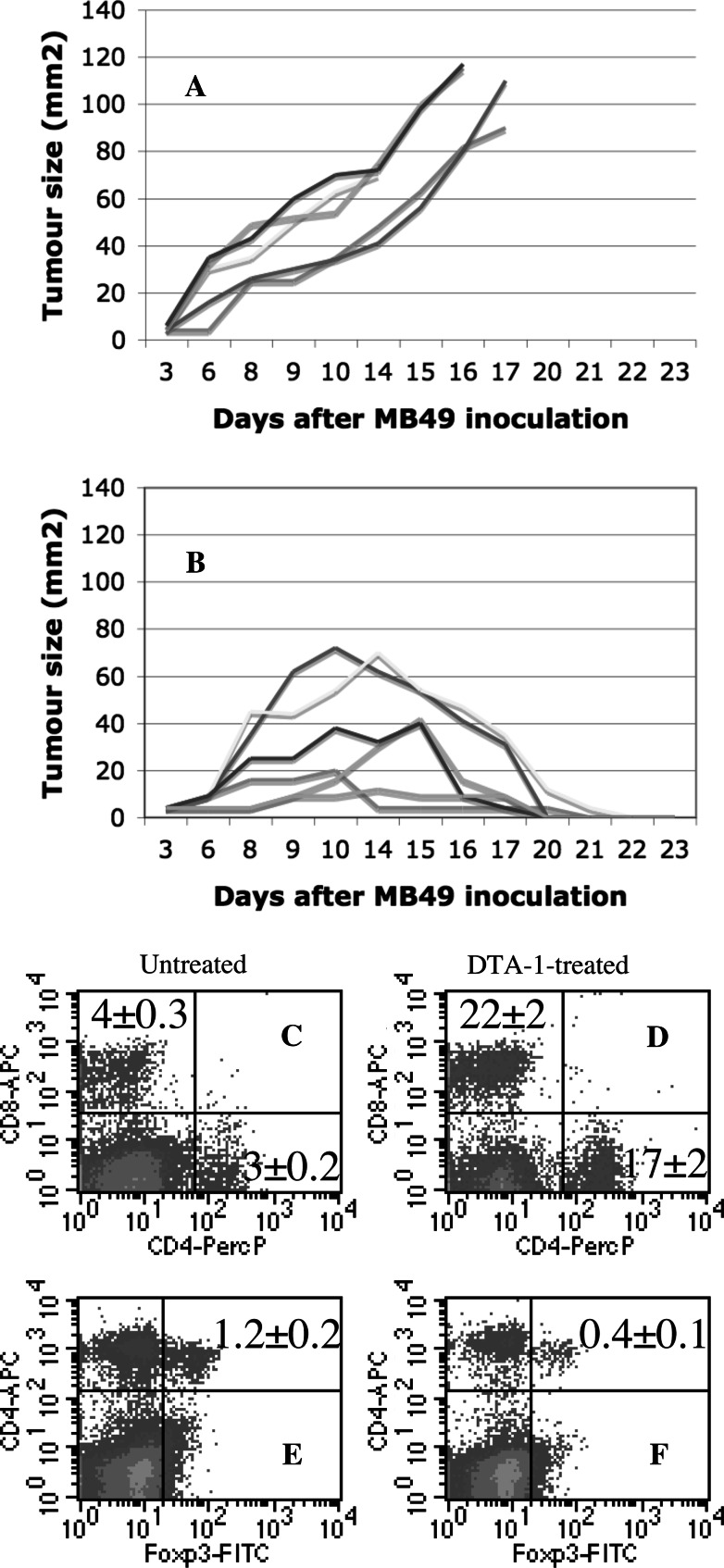
Although administration of DTA-1 alone is sufficient to reject some types of experimental tumours (Meth A and Colon 26 [15]), such a treatment appears to be less effective for other tumours (B16 and RENCA [15, 16]) unless an additional manipulation such as DNA vaccination [17] is included, suggesting that efficiency of DTA-1 therapy is dependent on the characteristics of transplantable tumour. Thus, the starting point of this investigation was to assess the susceptibility of MB49 tumours (murine bladder carcinoma naturally expressing HY) [24] to DTA-1 therapy. Like other tumour cell lines such as B16 and RENCA [16], MB49 does not express GITR (not shown). On day 0, a total of 11 B6 females were subcutaneously inoculated with 5 × 105 MB49 cells, at day 8, 6 randomly chosen mice were given 50 μg of DTA-1 by i.p. injection and the remaining 5 mice were not. Growth of MB49 tumours in the untreated group was very aggressive reaching a volume >100 mm2 by day 17 (Fig. 1a). In contrast, DTA-1 was very effective in treating established MB49 tumours with 100% rejection rate (Fig. 1b). A control rat IgG (GL-113) [25] showed no effect on MB49 growth (not shown). When the proportion of infiltrating T cell populations (CD4+, CD8+ and Foxp3+CD4+) within the MB49 tumours of untreated (Fig. 1c, e) and DTA-1 treated groups (Fig. 1d, f) was compared, we found that DTA-1 treatment was associated with an increased accumulation of CD4 and CD8 T cells but a reduction of Treg cells. Therefore, MB49 can be added to a list of tumours which can be rejected by DTA-1. Given, MB49 tumours are very aggressive and resistant to HY vaccination [28], complete rejection of established tumours following a single dose of DTA-1 administration is very encouraging.
Fig. 1.
DTA-1 is highly effective in treating established tumours. a, b A single injection of DTA-1 results in the regression of established MB49 tumours. A total of 11 B6 female mice were s.c. inoculated with 5 × 105 MB49 cells. 8 days later, the mice were randomly divided into two groups: one group (B, n = 6) was treated with 50 μg of DTA-1 mAb by i.p. injection and the other group was not (A, n = 5). The growth of MB49 tumours was monitored by measuring tumour size every other day. One representative of three independent experiments is shown. c–f Regression of MB49 is correlated with increased accumulation of tumour-infiltrating CD4 and CD8 T cells but decreased accumulation of Treg cells. Untreated and DTA-1-treated mice (3 mice/group) were prepared as described in A and B. At day 15, MB49 tumours isolated from untreated (C and E) and DTA-1-treated mice (D and F) were stained with anti-CD4PerCP and anti-CD8APC (C and D), or anti-CD4PerCP followed by intracellular staining with anti-Foxp3FITC (E and F). Percentage of CD4+, CD8+, or CD4+Foxp3+ cells in MB49 from individual mice in each group is shown as mean ± SEM. One representative of two independent experiments is shown
Treg cells purified from DTA-1-treated mice are competent suppressive cells
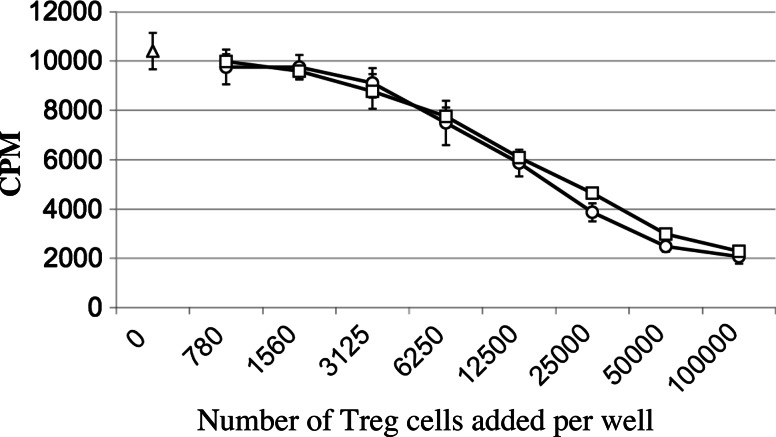
In vitro, DTA-1-mediated GITR signalling on Treg cells abrogates their suppressive activities [4, 5]. As T cell behaviour in vivo cannot be predicated on the in vitro behaviour of T cell co-cultures, we evaluated the inhibitory capacities of Treg cells isolated ex vivo from either untreated or DTA-1-treated mice 1 day after mAb administration. In a standard in vitro suppression assay, Treg cells from DTA-1-treated mice were as potent as those from untreated mice in inhibiting conventional CD4 T cells (from untreated mice) in response to anti-CD3 stimulation (Fig. 2). Likewise, Treg cells from GL-113-treated mice showed similar suppressive activity to those from untreated or DTA-1-treated mice (not shown). Thus, in vivo GITR signalling on Treg cells does not lead to their functional inactivation. This observation is consistent with another report [16].
Fig. 2.
Treg cells isolated from DTA-1 treated mice are competent suppressive cells in vitro. Two groups of B6 mice (3 mice/group) were untreated or treated with anti-GITR by i.p. injection of 50 μg of DTA-1. 24 h later, Treg (CD4+CD25+) and conventional CD4 T cells (CD4+CD25−) were purified from pooled LN and spleen cells of each group by FACS sorting. Conventional CD4 T cells (1 × 105/well) from the untreated group were cultured with anti-CD3 (0.05 μg/ml) and accessory cells (T cell-depleted and irradiated B6 spleen cells, 2 × 105/well) in the absence (open triangles) or presence of various numbers (two time serial diluted from 1 × 105/well to 780 /well) of nTregs from either untreated (open squares) or DTA-1-treated group mice (open circles) in 96-round bottomed plates for 3 days. Thymidine (0.5 μCi/well) was added to each well for the last 12 h. One representative of two independent experiments is shown
DTA-1 treatment in vivo leads to a partial depletion of Treg cells
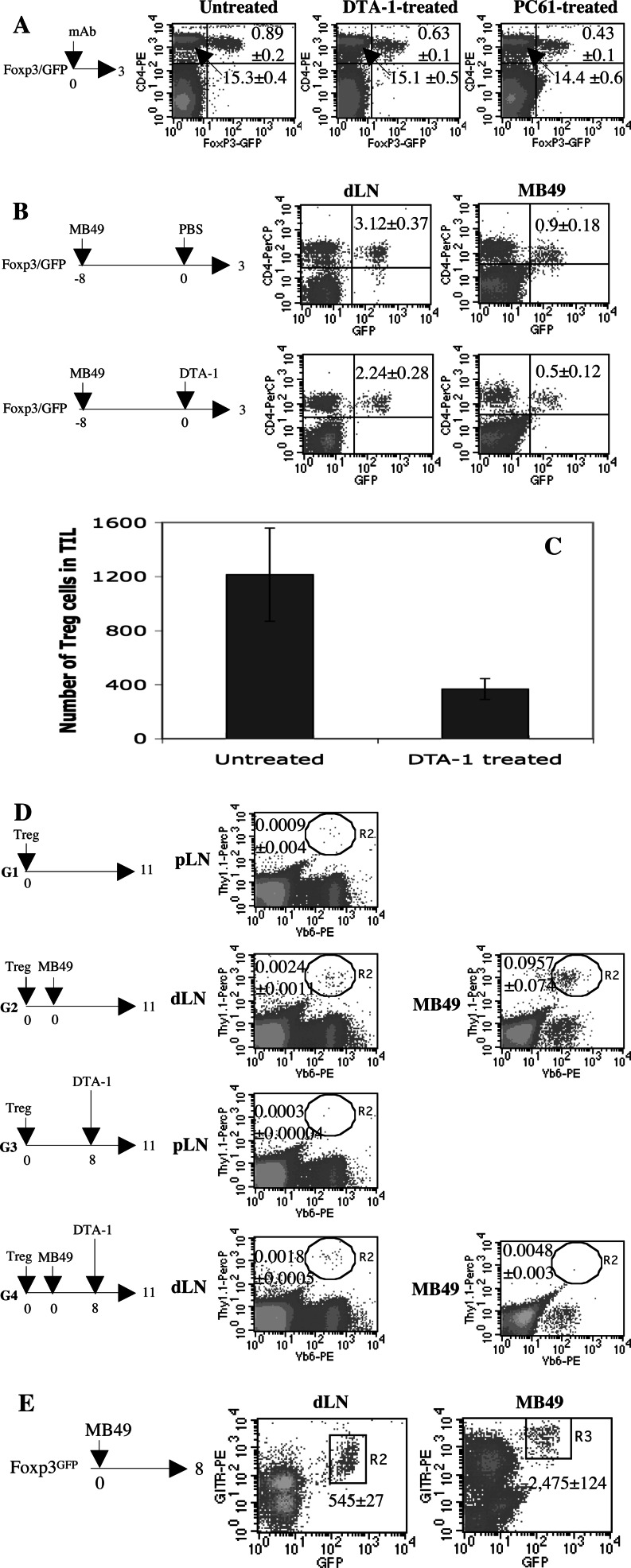
Although early studies indicated that DTA-1 (rat IgG2b) is a non-depleting mAb for Treg cells [4, 15, 19], we repeatedly observed a significant reduction (up to 40%) of circulating CD4+CD25+ cells in B6 mice following a single injection of DTA-1, raising the possibility that DTA-1 is a depleting mAb in vivo. To provide a conclusive demonstration, we used Foxp3/GFP knock-in mice in which Treg and non-Treg cells can be reliably distinguished by GFP expression [22]. 3 days after DTA-1 treatment, the proportion of CD4+GFP+ cells in PBL decreased from 0.89% (untreated) to 0.63% (representing a 30% reduction, p < 0.05), whereas that of the CD4+GFP− population of cells remained unchanged (from 15.3 to 15.1%, left and middle panels of Fig. 3a). However, in the depletion of Treg cells, DTA-1 was less efficient than PC61, a widely used anti-CD25 depleting mAb [26] which resulted in a 52% reduction of circulating Treg cells (right panel of Fig. 3a). The proportion of Treg and non-Treg in the PBL of Foxp3/GFP mice did not change following GL-113 treatment (not shown).
Fig. 3.
DTA-1 is a depleting mAb in vivo. a A single injection of DTA-1 mAb leads to a reduction of the percentage of circulating CD4+Foxp3+ cells. Three groups of Foxp3/GFP knock-in mice (4 mice/group) were untreated or treated with 25 μg of DTA-1 or PC61 by i.p. injection. 3 days later, peripheral blood lymphocyte (PBL) samples were collected from individual mice in each group and stained with anti-CD4PE. Percentage of CD4+GFP– and CD4+GFP+ cells in PBL is shown as mean ± SEM. One representative of three independent experiments is shown. b DTA-1 preferentially depletes tumour-resident Treg cells. Two groups of Foxp3/GFP knock-in mice (4 mice/group) were s.c. inoculated with 5 × 105 MB49 cells on day −8. The mice were untreated or treated with 50 μg of DTA-1 by i.p. injection on day 0. 3 days later, dLN and MB49 tumours from individual mice in each group were stained with anti-CD4PerCP. Percentage of GFP+CD4+ cells is shown as mean ± SEM. One representative of two independent experiments is shown. c The number of tumour-resident Treg cells was profoundly reduced following DTA-1 treatment. Two groups of Foxp3/GFP knock-in mice (4 mice/group) were s.c. inoculated with 5 × 105 MB49 cells on day −8. The mice were untreated or treated with 50 μg of DTA-1 by i.p. injection on day 0. 3 days later, MB49 tumours from individual mice in each group were stained with anti-CD4PerCP. The absolute tumour-infiltrated Treg cell numbers were determined by total tumour cells × % of small lymphocyte gate × % of CD4+GFP+ cells within gated tumour-infiltrated lymphocyte (TIL). d Accumulation of adoptively transferred HY-specific Treg cells in MB49 tumours is profoundly impaired following DTA-1 treatment. HY-specific Treg cells (Thy1.1+) were adoptively transferred to four groups of Thy1.2+ B6 females (4 mice/group) by i.v. injection (1 × 105/mouse). On the same day, the mice in G2 and G4 were inoculated s.c. with MB49 cells (5 × 105/mouse) and the mice in G1 and G3 were not. On day 8, the mice in G3 and G4 were treated with 50 μg of DTA-1 by i.p. injection, and the mice in G1 and G2 were not. On day 11, dLN (pLN for G1 and G3) and MB49 tumours from individual mice in each group were stained with anti-Vβ6PE, anti-Thy1.1PerCP and anti-CD4APC followed by intracellular staining of anti-Foxp3FITC. Percentage of Treg cells of donor origin (Thy1.1+Vβ6+) is shown as mean ± SEM. One representative of two independent experiments is shown. e Tumour-infiltrating Treg cells express higher levels of GITR than those in dLN. Foxp3/GFP knock-in mice (n = 4) were s.c. injected with 5 × 105 MB49 cells on day 0. 8 days later, MB49 and dLN cells from individual mice were stained with anti-GITRPE and anti-CD4PercP. The MFI of GITR by gated GFP+GITR+ cells in dLN and MB49 is shown as mean ± SEM. One representative of four independent experiments is shown
Next, we examined whether DTA-1 treatment would deplete polyclonal Treg cells in tumour-bearing mice. Two groups of Foxp3/GFP knock-in mice were injected s.c. with MB49 cells at day −8, one group was given DTA-1 at day 0 and the other was not. 3 days after DTA-1 administration, each MB49 tumour and its draining LN (dLN) were analysed for the presence of CD4+GFP+ cells. Following i.p. injection of DTA-1, there was a 44% (reduced from 0.9 to 0.5%, p < 0.05) and 28% (from 3.12 to 2.24%) decrease of Treg cells in MB49 tumours and dLN, respectively (Fig. 3b). Treatment of MB49-bearing mice with GL-113 failed to alter the pattern of Treg accumulation in MB49 or dLN (not shown). Data shown in Fig. 3b indicate that DTA-1 depletes tumour-resident Treg cells. However, DTA-1 treatment also increases the proportion of tumour-infiltrating effector T cells (Fig. 1c, d), the decrease of Treg cells might reflect an increase in another cell population. We therefore compared the absolute number of tumour-infiltrated Treg cells from untreated and DTA-1-treated mice. As shown in Fig. 3c, there was a significant reduction of tumour-resident Treg cells following DTA-1 treatment, strongly suggesting that DTA-1 can preferentially deplete tumour-infiltrating Treg cells.
To investigate whether the results obtained from the measurement of polyclonal Tregs in tumour-bearing mice would be applicable to monoclonal Treg cells, we adoptively transferred HY-specific Treg cells (Thy1.1+CD4+Vβ6+CD25+ cells sorted from Rag2+/− Marilyn females) to four groups of Thy1.2 B6 mice which were injected with MB49 cells (G2 and G4) or not (G1 and G3) on the same day of Treg cell transfer, and given DTA-1 (G3 and G4) or not (G1 and G2) on day 8 (Fig. 3d). The impact of DTA-1 treatment on monoclonal Treg cells was determined by comparing the proportion of donor cells in MB49 and dLN between G2 and G4. DTA-1 treatment led to 95% reduction in the accumulation of Marilyn Treg cells in the MB49 tumour (decreased from 0.0957% in G2 to 0.0048% in G4, p < 0.001) (Fig. 3d), whereas depletion in tumour dLN was less marked (0.0024 vs. 0.0018%). However, GL-113 treatment did not influence Marilyn Treg cells in response to MB49 tumours (not shown).
In the same experiment, we also measured the changes in proportions of host Treg cells (Thy1.1−CD4+Foxp3+) in tumour tissues with or without DTA-1 treatment (S-Fig. 1). Comparing the proportion of host Treg cells within the MB49 tumours between G2 and G4 revealed that a single injection of DTA-1 resulted in 38% reduction of recipient tumour-resident Treg cells (0.993–0.575%, p < 0.05). Thus, the results shown in Fig. 3b using Foxp3/GFP knock-in mice were reproducible using WT B6 mice.
Figure 3b–d shows that depletion of polyclonal or monoclonal Treg cells by DTA-1 is more extensive in tumours than in the dLN. We speculated that the environment of a growing MB49 tumour might preferentially increase GITR expression on tumour-infiltrating Treg cells, rendering them more susceptible to depletion. To test this, Foxp3/GFP mice were inoculated with MB49 cells, and 8 days later the expression of GITR by Treg cells in the MB49 tumour was compared with those in dLN. As shown in Fig. 3e, there was a 4.5-fold increase in GITR expression on MB49-infiltrating Treg cells (MFI 545 ± 27 tumour draining LN, MFI 2475 ± 124 tumour; p < 0.05), which is likely to increase sensitivity to DTA-1-induced depletion.
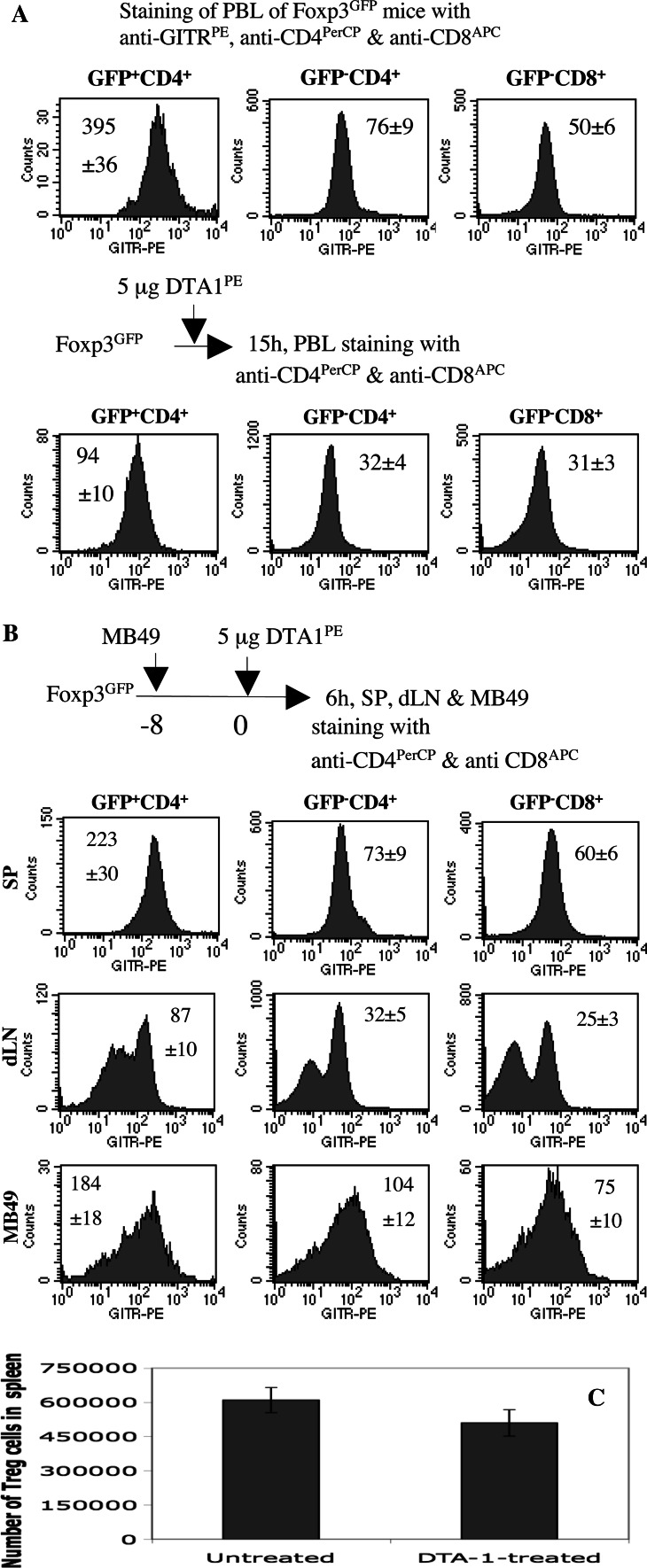
Treg cells are primary cellular targets of DTA-1 in vivo
In vitro staining of PBL from Foxp3/GFP knock-in mice with anti-GITRPE, anti-CD4PerCP and anti-CD8APC clearly demonstrated that Treg cells expressed higher levels of GITR than conventional CD4 and CD8 cells (top of Fig. 4a).
Fig. 4.
Treg cells constitutively express higher levels of GITR than conventional CD4 T cells in vivo. a Treg cells are primary targets of DTA-1. Top panels, the PBL from a group of Foxp3/GFP knock-in mice (n = 3) were stained with anti-GITRPE, anti-CD4PerCP and anti-CD8APC. The expression of GITR by GFP+CD4+, GFP−CD4+ and GFP−CD8+ T cells from individual mice was presented as histograms. MFI of GITR is shown as mean ± SEM. Bottom panels, a group of Foxp3/GFP knock-in mice were given 5 μg of anti-GITRPE (clone DTA-1) by i.v. injection. 15 h later, the PBL from individual mice were stained with anti-CD4PerCP and anti-CD8APC. MFI of GITR by GFP+CD4+, GFP−CD4+ and GFP−CD8+ T cells is presented as mean ± SEM. One representative of three independent experiments is shown. b Tumour-infiltrating Treg, CD4 and CD8 T cells express higher levels of GITR than those in dLN. A group of Foxp3/GFP knock-in mice (n = 4) were s.c. inoculated with MB49 cells (5 × 105/mouse) 8 days previously. On day 0, the mice were i.v. injected with 5 μg of DTA-1PE. 6 h later, spleen, dLN and MB49 tumour cells from individual mice were stained with anti-CD4PerCP and anti-CD8APC. MFI of GITR by GFP+CD4+, GFP−CD4+ and GFP−CD8+ T cells is presented as mean ± SEM. One representative of two independent experiments is shown. c The number of splenic Treg cells was moderately reduced following DTA-1 treatment. Two groups of Foxp3/GFP knock-in mice (4 mice/group) were s.c. inoculated with 5 × 105 MB49 cells on day −8. The mice were untreated or treated with 50 μg of DTA-1 by i.p. injection on day 0. 3 days later, MB49 tumours from individual mice in each group were stained with anti-CD4PerCP. The absolute spleen-resident Treg cell numbers were determined by total spleen cells × % of lymphocyte gate × % of CD4+GFP+ cells within gated lymphocytes
Whether GITR expression in vivo is similar to that seen in vitro is unclear. We therefore performed a pilot experiment to test the feasibility of “in vivo” staining. CBA mice were injected i.v. with 20 μg of anti-CD4PE, and PBL samples collected at various time points were stained with anti-CD3FITC in vitro, before analysing for CD4+CD3+ cells. Cells co-expressing CD4 and CD3 were detectable as early as 18 min after injection, and were still present after 22 h, by which time CD4 molecules were down-regulated, presumably due to antibody-mediated internalisation (S-Fig. 2B).
Having verified this in vivo staining protocol, we applied it to determine the cellular targets of DTA-1. Foxp3/GFP mice were injected i.v. with 5 μg of DTA-1PE, and 15 h later the PBL samples were stained with anti-CD4PercP and anti-CD8APC to allow identification of Foxp3/GFP positive from Foxp3/GFP negative cells in each population. MFI of GITR by Treg cells was threefold higher than that of conventional CD4 and CD8 T cells (bottom panel of Fig. 5a), indicating that in vivo, DTA-1 antibodies primarily bind to Treg cells which have abundant surface GITR molecules compared with non-Treg cells (top panels of Fig. 4a).
Fig. 5.
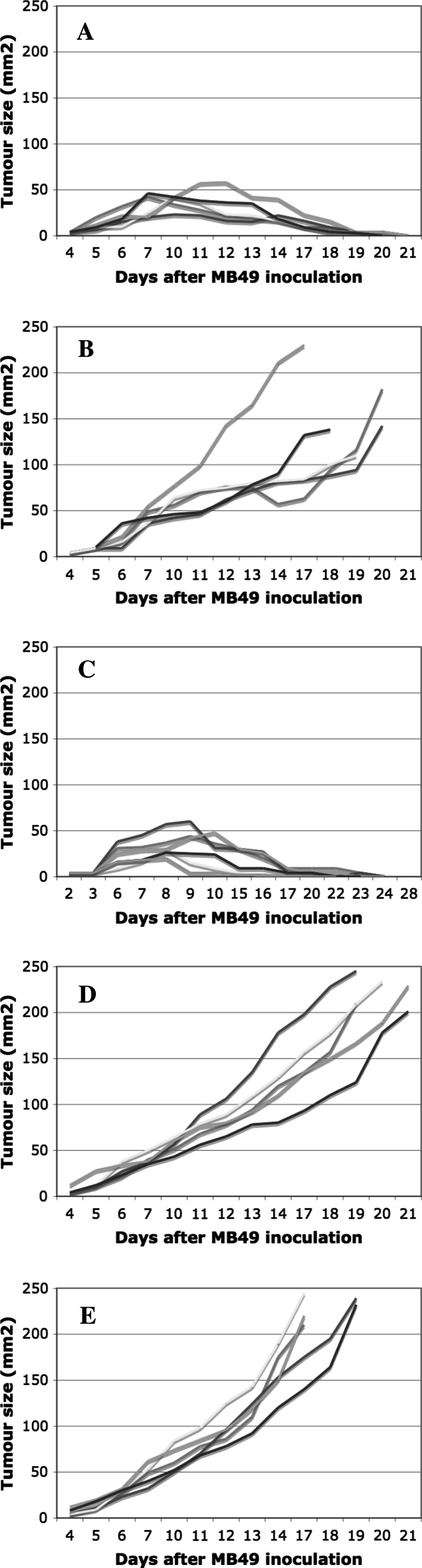
Comparison of DTA-1 and PC61 for their anti-MB49 activities in vivo. a, b. Two groups of B6 female mice (5 mice/group) were treated with 50 μg of PC61 (A) or DTA-1 mAb (B) by i.p. injection. 2 days later, all mice were s.c. inoculated with 5 × 105 MB49 cells. The growth of MB49 tumours was monitored by measuring tumour size every other day. c–e A total of 16 B6 female mice were s.c. inoculated with 5 × 105 MB49 cells. 8 days later, the mice were randomly divided into three groups: group one (C, n = 6) was treated with 50 μg of DTA-1 mAb by i.p. injection, group two (D, n = 5) was treated with 50 μg of PC61 mAb by i.p. injection, and group three (E, n = 5) was treated with 50 μg of DTA-1 and 50 μg of PC61 by i.p. injection. The growth of MB49 tumours was monitored by measuring tumour size every other day
Although Treg cells rather than conventional T cells are the primary targets of DTA-1 under normal conditions, it is not known whether this would be found in tumour-bearing mice. To address this question, we injected 5 μg of DTA-1PE into Foxp3/GFP mice inoculated with MB49 cells 8 days previously. 6 h later, we analysed GITR expression by CD4+GFP+, CD4+GFP− or CD8+GFP− subsets in spleen, dLN and MB49 tumours (Fig. 4b). Several observations can be made. Firstly, Treg cells within MB49 tumours displayed a 2.1-fold higher GITR expression than those in dLN, thus confirming the in vitro staining results shown in Fig. 3d. Secondly, like Treg cells, conventional CD4 and CD8 T cells present in the MB49 tumour also showed higher MFI of GITR than those in dLN. This observation indicates that either the tumour microenvironment can induce and maintain GITR expression on infiltrating T cell subsets or those T cells with higher GITR expression are able to preferentially migrate into the tumour. Finally, GITR expression by Treg cells was consistently higher than that by conventional CD4 or CD8 T cells, regardless of tissue of origin, suggesting that Treg cells constitutively express higher levels of GITR in vivo.
As shown in Fig. 4b, splenic Treg cells appear to express higher GITR than tumour-resident Treg cells (223 vs. 184 of MFI), raising the possibility that splenic Treg might be the primary target of DTA-1. To explore this, we compared changes of Treg cells in spleen and tumour after DTA-1 treatment. A moderate decrease of splenic Treg cell number in MB49-bearing mice was observed following DTA-1 therapy (Fig. 4c), however, the reduction of tumour-resident Treg cells was more significant in the same experiment (Fig. 3c). This disparity may be related to the experimental conditions including antibody dose (5 vs. 50 μg) and duration of treatment (6 vs. 72 h). In addition, we speculate that i.v. delivered DTA-1PE mAb might reach the spleen before entering tumour tissue. Moreover, some mAb will be consumed within the spleen by binding to GITR-expressing cells, thus reducing the amount of mAb available for entry into other tissues. Thus, the local concentration of mAb in the spleen is likely to be higher than that in tumour, as a result, Treg cells in the spleen show higher GITR expression than those in the tumours.
DTA-1 but not PC61 therapy can control established MB49 tumours
If DTA-1 can deplete Treg cells in vivo, it would be of interest to compare DTA-1 with PC61, a standard anti-CD25 depleting mAb. A single injection of PC61 was very effective in treating MB49 tumours when administered to B6 females 2 days before MB49 inoculation [Fig. 5a, 100% (5/5) tumour-free mice]. However, the same treatment protocol using DTA-1 had limited impact on tumour growth [Fig. 5B, 20% (1/5) tumour-free mice]. This difference could be explained by our observations showing PC61 was more potent than DTA-1 in depleting Treg in vivo (Fig. 3a). On the other hand, DTA-1 treatment was very efficient at rejecting established MB49 tumours [Figs. 1b, 5c, 100% (6/6) tumour-free mice] whereas PC61 therapy had no effect (Fig. 5d, 0% tumour-free mice). We speculate that CD25-expressing anti-MB49 effector T cells were depleted by PC61 treatment. In support of this, we were able to show that anti-tumour activity by DTA-1 was completely lost if PC61 was co-injected with DTA-1 on day 8 (Fig. 5e, 0% tumour-free mice). Since DTA-1 leads to partial Treg depletion and timing of DTA-1 administration is the key factor determining the outcome of cancer therapy, we conclude that Treg depletion is one mechanism but cannot be regarded as the only one responsible for cancer therapy by DTA-1, other mechanisms such as co-stimulation of T cells might be in operation.
Discussion
CD4+CD25+ cells isolated from mice given DTA-1 24 h previously were found to be functional Treg cells with similar suppressive activity as those from untreated mice (Fig. 2), suggesting that in vivo GITR signalling does not disable Treg cells. This conclusion is in line with a report showing that Treg cells purified from either rat IgG-treated or DTA-1-treated mice are equally efficient in suppressing allo-MLR [16]. However, only a single ratio of Treg to responder (1:1) was tested in MLR [16], whereas our assay covered a wide range of ratio from 1:1 to 1:128. Since maximum Treg depletion occurred 3 days after DTA-1 administration (Fig. 3a), Tregs were isolated at 24 h after DTA-1 treatment allowing sufficient time for GITR binding and signal transduction (Fig. 4).
As injected DTA-1 mAb preferentially binds to Treg cells (Fig. 4b) but does not inactivate them (Fig. 2), we consider that depletion of Treg cells is an alternative consequence of GITR binding. In support of this, DTA-1 is IgG2b, an isotype shared by a large panel of in vivo depleting mAb with specificity for CD4 (GK1.5 and YTS 191), CD8 (YTS169 and 2.43) and Thy1.2 (30H12). Although DTA-1 has been proposed [12] and indicated [20] to deplete GITR expressing-Treg cells in vivo, a formal demonstration is lacking. In this study we provide evidence showing that DTA-1 is a depleting mAb causing a moderate but significant reduction of endogenous polyclonal Tregs in tumour-free (Fig. 3a) and tumour-bearing Foxp3/GFP knock-in mice (Fig. 3b, c). The most remarkable Treg depletion following DTA-1 treatment is illustrated in adoptive transfer experiments using HY-specific Treg cells (Fig. 3d). Importantly, the reduction of donor Treg cells is more complete in MB49 tissue than dLN (Fig. 3d) and correlates with the level of GITR expression by Treg cells in these two tissues (Fig. 3e).
Discrepancies between our data and other studies [15] regarding the depleting potential of DTA-1 may reflect differences between mouse strains (BALB/c vs. B6) and the cells used for analysis (spleen cells vs. PBL) and the use of different markers (CD25 vs. Foxp3) to identify Treg cells. It becomes increasingly clear that not all CD25+ are Treg cells and not all Treg cells are necessarily CD25+ [29].
Why DTA-1 can only induce a partial Treg depletion in B6 mice is unclear. One reason is likely to be the nature of this particular clone. In this respect, it would be of interest to compare DTA-1 with other anti-GITR clones of IgG2b isotype for efficiency of Treg depletion. In addition, the current treatment regime might be suboptimal, given a single i.p. injection with 50 μg of mAb. Furthermore, Treg cells are composed of distinct subsets which might display different sensitivity to DTA-1-triggered depletion.
Another key element determining efficiency of depletion is the level of expression of the target molecule on the cell surface. There is a clear link between the degree of depletion and the level of GITR expression. Firstly, Treg cells constitutively express higher levels of GITR than conventional CD4 T cells under steady-state conditions (Fig. 4a). Thus DTA-1 seems to selectively target Treg but spare the conventional CD4 T cells (Fig. 3a). The degree of Treg depletion following DTA-1 treatment is moderate in naïve mice, which is perhaps due to relatively low target molecule expression. Secondly, GITR expression on Treg cells is itself variable with the highest level observed on tumour-resident Tregs and lower levels seen on Treg cells from tumour-draining LN (Fig. 3e). Thus, Treg cells in tumour but not those in the dLN are likely to be depleted in the presence of DTA-1 in vivo (Fig. 3b, c). These observations could explain why the percentage of tumour-resident Treg cells but not those within dLN were significantly reduced following DTA-1 administration, as reported [15] and shown in Fig. 1. Finally, timing of DTA-1 treatment determining the efficiency of cancer therapy (Fig. 5) [15, 17], as mAb given on day 8 after tumour inoculation is more effective than that on day 1. A potential interpretation for this observation is that Treg cells in the tumour reach the peak of GITR expression on day 8 (Figs. 3e, 4b), perhaps making them optimally sensitive to DTA-1-mediated depletion (Fig. 3c, d). Like GITR, other Treg-related molecules including CD103, ICOS, PDL1 and OX40 were found to be up-regulated preferentially by Treg cells detected in MB49 mass, compared with those in dLN (data not shown). These results are consistent with two recent reports showing that vast majority of tumour-infiltrating Treg cells are OX40high [30] and GITRhigh [31]. However, this comparison was made with splenic Treg cells from tumour-free naive mice [30] rather than Treg cells from dLN of tumour-bearing mice. In this respect, our data are more informative as GITR expression was assessed on both MB49 tumour-infiltrating Treg cells and those in the tumour dLN.
An alternative interpretation for the reduction of Treg cells (95% reduction, from 0.48 to 0.02%) in tumour tissue following DTA-1 treatment is altered Treg migration. If this hypothesis is correct, one would expect that reduced Treg representation in tumour mass should correlate with increased Treg accumulation in other lymphoid tissues such as dLN and ndLN. However, we observed that the decreased proportion of adoptively transferred Marilyn Treg cells was also evident, but to a less extent, in dLN (64% reduction, from 0.28 to 0.10%) and ndLN (40% reduction, from 0.15 to 0.09%) (S-Fig. 3A), making this explanation unlikely. In addition, the reduction of donor Treg cells in dLN was also evident when absolute cell number was compared between untreated and DTA-1-treated groups (S-Fig. 3B). Nevertheless, LN and tumour tissues are different microenvironments with distinct structures and capacity to recruit Treg cells. The contributions of depletion and altered migration to the reduced accumulation of Tregs in tumour tissues following DTA-1 therapy needs further investigation.
Treg cells promote tumour progression by suppressing anti-tumour immunity via different mechanisms [32, 33]. Treg cells are recruited into the tumour mass because they not only recognise tumour-associated antigens but also normal self-antigens released from the tumour [34]. In addition, tumours are able to induce a subset of DC to produce TGFβ [35] or IDO [36], which trigger endogenous Treg cell expansion and activation. Although the initiation of Treg activation requires TCR engagement, once activated, Treg cells can inhibit T cell responses non-specifically via bystander suppression, thus the action of Treg cells can be both antigen specific and non-specific [37]. In vivo Treg cells can target various populations such as CD8 T cells, APC and innate immune cells including NKT and NK cells via cell-to-cell contact (using CTLA-4 or membrane bound TGFβ) or production of inhibitory cytokines such as TGFβ and IL10 [37]. Treg cells prevent CD8 T cells from differentiation into cytolytic effector cells in vivo without affecting their proliferation or IFNγ production [38, 39]. In addition, Treg cells can exhibit their suppression in the tumour microenvironment. For example, tumour-infiltrating Treg cells can kill anti-tumour effector cells such as CD8 and NK cells locally by releasing granzyme B and perforin [40].
We have not explored the mechanisms of Treg depletion by DTA-1 in great detail. Both expression of FcR and complement by the host appear to be required for optimal Ab-mediated depletion. It has been difficult to determine the relative contributions of T cell costimulation and Treg depetion by DTA-1. In this regard, it would be of interest to compare between DTA-1 and the soluble GITR-L for their effects, as the latter can only deliver co-stimulatory signals without the involvement of Treg depletion. Also, 2F8 [41], is another agonist anti-GITR mAb which is unable to deplete or disable Treg cells in vivo, presumably because of the isotype (rat IgG2a). It has been demonstrated recently that 2F8 treatment significantly accelerates the onset of diabetes in NOD mice by promoting T cell activation without affecting Treg cells [41].
It has been well documented that T cell costimulation by DTA-1 is another key mechanism for cancer immunotherapy [7–11]. We observed that in vivo, GITR signalling enhanced allo-recognition by conventional CD4 T cells, and amplified anti-MB49 responses by adoptively transferred Marilyn CD4 T cells (manuscript in preparation). In this study, we also verified whether successful cancer immunotherapy using DTA-1 could be extended to the aggressive HY+H2b+ MB49 tumour. Given HY vaccination fails to control MB49 growth [28], a complete regression of established MB49 tumours following a single DTA-1 administration is very impressive. As reported [15] and shown in Fig. 1, the proportion of Treg cells in rejecting tumour tissues is dramatically reduced, which appears to be a direct consequence of depletion. Intra-tumour injection of DTA-1 [15] or depleting anti-CD4 mAb [42] results in regression of established tumours, highlighting the impact of local removal of Treg cells on therapeutic outcome.
The current study has two implications. Firstly, the consequence of an in vivo therapeutic antibody treatment can be down-regulation (7D4, anti-CD25), blockade or functional inactivation (YTS 177, non-depleting anti-CD4), co-stimulation (37.51, anti-CD28) or depletion of the target T cell population. Apart from antibody specificity and isotype, outcome depends on cellular targets, expression level of targeted molecules, tissue distribution and modulation under physiological or pathological circumstances. The results of antibody therapy need to be carefully interpreted, as for example, a putative blocking antibody (MR1, anti-CD40L) shown in earlier studies [43], was found to be depleting by a subsequent investigation [44]. Secondly, for the identification of the cellular targets of an antibody and investigation of their expression pattern under different conditions, “in vivo” staining by injection of conjugated antibodies has the advantage of allowing expression to be monitored in real time.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgments
We thank Dr. Shimon Sakaguchi and Dr. Bernard Massile for providing DTA-1 hybridoma cells and Foxp3/GFP knockin mice, respectively. We also thank Dr. Elizabeth Simpson for critically reading the manuscript.
Abbreviations
- dLN
Tumour-draining lymph node
- pLN
Peripheral LN
- nTreg
Natural CD4+CD25+Foxp3+ regulatory T cells
- Mar
Marilyn mice
- PBL
Peripheral blood lymphocytes
- MFI
Mean florescence intensity
- Foxp3/GFP
Foxp3/GFP knock-in mice
Footnotes
This work was supported by a Senior Cancer Research Fellowship to JGC from Cancer Research, UK.
References
- 1.Nocentini G, Giunchi L, Ronchetti S, et al. A new member of the tumor necrosis factor/nerve growth factor receptor family inhibits T cell receptor-induced apoptosis. Proc Natl Acad Sci USA. 1997;94:6216–6221. doi: 10.1073/pnas.94.12.6216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gurney AL, Marsters SA, Huang RM, et al. Identification of a new member of the tumor necrosis factor family and its receptor, a human ortholog of mouse GITR. Curr Biol. 1999;9:215–218. doi: 10.1016/S0960-9822(99)80093-1. [DOI] [PubMed] [Google Scholar]
- 3.Kwon B, Yu KY, Ni J, et al. Identification of a novel activation-inducible protein of the tumor necrosis factor receptor superfamily and its ligand. J Biol Chem. 1999;274:6056–6061. doi: 10.1074/jbc.274.10.6056. [DOI] [PubMed] [Google Scholar]
- 4.Shimizu J, Yamazaki S, Takahashi T, et al. Stimulation of CD25(+)CD4(+) regulatory T cells through GITR breaks immunological self-tolerance. Nat Immunol. 2002;3:135–142. doi: 10.1038/ni759. [DOI] [PubMed] [Google Scholar]
- 5.McHugh RS, Whitters MJ, Piccirillo CA, et al. CD4+ CD25+ immunoregulatory T cells: gene expression analysis reveals a functional role for the glucocorticoid-induced TNF receptor. Immunity. 2002;16:311–323. doi: 10.1016/S1074-7613(02)00280-7. [DOI] [PubMed] [Google Scholar]
- 6.Ji HB, Liao G, Faubion WA, et al. Cutting edge: the natural ligand for glucocorticoid-induced TNF receptor-related protein abrogates regulatory T cell suppression. J Immunol. 2004;172:5823–5827. doi: 10.4049/jimmunol.172.10.5823. [DOI] [PubMed] [Google Scholar]
- 7.Tone M, Tone Y, Adams E, et al. Mouse glucocorticoid-induced tumor necrosis factor receptor ligand is costimulatory for T cells. Proc Natl Acad Sci USA. 2003;100:15059–15064. doi: 10.1073/pnas.2334901100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ronchetti S, Zollo O, Bruscoli S, et al. GITR, a member of the TNF receptor superfamily, is costimulatory to mouse T lymphocyte subpopulations. Eur J Immunol. 2004;34:613–622. doi: 10.1002/eji.200324804. [DOI] [PubMed] [Google Scholar]
- 9.Kohm AP, Williams JS, Miller SD. Cutting edge: ligation of the glucocorticoid-induced TNF receptor enhances autoreactive CD4+ T cell activation and experimental autoimmune encephalomyelitis. J Immunol. 2004;172:4686–4690. doi: 10.4049/jimmunol.172.8.4686. [DOI] [PubMed] [Google Scholar]
- 10.Kanamaru F, Youngnak P, Hashiguchi M, et al. Costimulation via glucocorticoid-induced TNF receptor in both conventional and CD25+ regulatory CD4+ T cells. J Immunol. 2004;172:7306–7314. doi: 10.4049/jimmunol.172.12.7306. [DOI] [PubMed] [Google Scholar]
- 11.Stephens GL, McHugh RS, Whitters MJ, et al. Engagement of glucocorticoid-induced TNFR family-related receptor on effector T Cells by its ligand mediates resistance to suppression by CD4+ CD25+ T cells. J Immunol. 2004;173:5008–5020. doi: 10.4049/jimmunol.173.8.5008. [DOI] [PubMed] [Google Scholar]
- 12.Shevach EM, Stephens GL. The GITR-GITRL interaction: co-stimulation or contrasuppression of regulatory activity? Nat Rev Immunol. 2006;6:613–618. doi: 10.1038/nri1867. [DOI] [PubMed] [Google Scholar]
- 13.Nocentini G, Riccardi C. GITR: a multifaceted regulator of immunity belonging to the tumor necrosis factor receptor superfamily. Eur J Immunol. 2005;35:1016–1022. doi: 10.1002/eji.200425818. [DOI] [PubMed] [Google Scholar]
- 14.Turk MJ, Guevara-Patiño JA, Rizzuto GA, et al. Concomitant tumor immunity to a poorly immunogenic melanoma is prevented by regulatory T cells. J Exp Med. 2004;200:771–782. doi: 10.1084/jem.20041130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ko K, Yamazaki S, Nakamura K, et al. Treatment of advanced tumors with agonistic anti-GITR mAb and its effects on tumor-infiltrating Foxp3 + CD25+ CD4+ regulatory T cells. J Exp Med. 2005;202:885–891. doi: 10.1084/jem.20050940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ramirez-Montagut T, Chow A, Hirschhorn-Cymerman D, et al. Glucocorticoid-induced TNF receptor family related gene activation overcomes tolerance/ignorance to melanoma differentiation antigens and enhances antitumor immunity. J Immunol. 2006;176:6434–6442. doi: 10.4049/jimmunol.176.11.6434. [DOI] [PubMed] [Google Scholar]
- 17.Cohen AD, Diab A, Perales MA, et al. Agonist anti-GITR antibody enhances vaccine-induced CD8(+) T-cell responses and tumor immunity. Cancer Res. 2006;66:4904–4912. doi: 10.1158/0008-5472.CAN-05-2813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhou P, L’italien L, Hodges D, et al. Pivotal roles of CD4+ effector T cells in mediating agonistic anti-GITR mAb-induced-immune activation and tumor immunity in CT26 tumors. J Immunol. 2007;179:7365–7375. doi: 10.4049/jimmunol.179.11.7365. [DOI] [PubMed] [Google Scholar]
- 19.Valzasina B, Guiducci C, Dislich H, et al. Triggering of OX40 (CD134) on CD4(+)CD25+ T cells blocks their inhibitory activity: a novel regulatory role for OX40 and its comparison with GITR. Blood. 2005;105:2845–2851. doi: 10.1182/blood-2004-07-2959. [DOI] [PubMed] [Google Scholar]
- 20.Sharma S, Dominguez AL, Manrique SZ, et al. Systemic targeting of CpG-ODN to the tumor microenvironment with anti-neu-CpG hybrid molecule and T regulatory cell depletion induces memory responses in BALB-neuT tolerant mice. Cancer Res. 2008;68:7530–7540. doi: 10.1158/0008-5472.CAN-08-1635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Suvas S, Kim B, Sarangi PP, et al. In vivo kinetics of GITR and GITR ligand expression and their functional significance in regulating viral immunopathology. J Virol. 2005;79:11935–11942. doi: 10.1128/JVI.79.18.11935-11942.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wang Y, Kissenpfennig A, Mingueneau M, et al. Th2 lymphoproliferative disorder of LatY136F mutant mice unfolds independently of TCR-MHC engagement and is insensitive to the action of Foxp3 + regulatory T cells. J Immunol. 2008;180:1565–1575. doi: 10.4049/jimmunol.180.3.1565. [DOI] [PubMed] [Google Scholar]
- 23.Grandjean I, Duban L, Bonney EA, et al. Are major histocompatibility complex molecules involved in the survival of naive CD4+ T Cells? J Exp Med. 2003;198:1089–1102. doi: 10.1084/jem.20030963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Summerhayes IC, Franks LM. Effects of donor age on neoplastic transformation of adult mouse bladder epithelium in vitro. J Natl Cancer Inst. 1979;62:1017–1023. [PubMed] [Google Scholar]
- 25.Gulbenkian AR, Egan RW, Fernandez X, et al. Interleukin-5 modulates eosinophil accumulation in allergic guinea pig lung. Am Rev Respir Dis. 1992;146:263–266. doi: 10.1164/ajrccm/146.1.263. [DOI] [PubMed] [Google Scholar]
- 26.Lowenthal JW, Corthesy P, Tougne C, et al. High and low affinity IL 2 receptors: analysis by IL 2 dissociation rate and reactivity with monoclonal anti-receptor antibody PC61. J Immunol. 1985;135:3988–3994. [PubMed] [Google Scholar]
- 27.Chai JG, Tsang JY, Lechler R, et al. CD4+ CD25+ T cells as immunoregulatory T cells in vitro. Eur J Immunol. 2002;32:2365–2375. doi: 10.1002/1521-4141(200208)32:8<2365::AID-IMMU2365>3.0.CO;2-2. [DOI] [PubMed] [Google Scholar]
- 28.Yang AS, Monken CE, Lattime EC. Intratumoral vaccination with vaccinia-expressed tumor antigen and granulocyte macrophage colony-stimulating factor overcomes immunological ignorance to tumor antigen. Cancer Res. 2003;63:6956–6961. [PubMed] [Google Scholar]
- 29.Fontenot JD, Rasmussen JP, Williams LM, et al. Regulatory T cell lineage specification by the forkhead transcription factor Foxp3. Immunity. 2005;22:329–341. doi: 10.1016/j.immuni.2005.01.016. [DOI] [PubMed] [Google Scholar]
- 30.Piconese S, Valzasina B, Colombo MP. OX40 triggering blocks suppression by regulatory T cells and facilitates tumor rejection. J Exp Med. 2008;205:825–839. doi: 10.1084/jem.20071341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lutsiak ME, Tagaya Y, Adams AJ, et al. Tumor-induced impairment of TCR signaling results in compromised functionality of tumor-infiltrating regulatory T cells. J Immunol. 2008;180:5871–5881. doi: 10.4049/jimmunol.180.9.5871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zou W. Regulatory T cells, tumour immunity and immunotherapy. Nat Rev Immunol. 2006;6:295–307. doi: 10.1038/nri1806. [DOI] [PubMed] [Google Scholar]
- 33.Qin FX. Dynamic behavior and function of Foxp3 + regulatory T cells in tumor bearing host. Cell Mol Immunol. 2009;6:3–13. doi: 10.1038/cmi.2009.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sakaguchi S. Naturally arising CD4+ regulatory T cells for immunological self-tolerance and negative control of immune responses. Annu Rev Immunol. 2004;22:531–562. doi: 10.1146/annurev.immunol.21.120601.141122. [DOI] [PubMed] [Google Scholar]
- 35.Ghiringhelli F, Puig PE, Roux S, et al. Tumor cells convert immature myeloid dendritic cells into TGF-beta-secreting cells inducing CD4+ CD25+ regulatory T cell proliferation. J Exp Med. 2005;202:919–929. doi: 10.1084/jem.20050463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sharma MD, Baban B, Chandler P, et al. Plasmacytoid dendritic cells from mouse tumor-draining lymph nodes directly activate mature Tregs via indoleamine 2, 3-dioxygenase. J Clin Invest. 2007;117:2570–2582. doi: 10.1172/JCI31911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tang Q, Bluestone J. The Foxp3 + regulatory T cell: a jack of all trades, master of regulation. Nat Rev Immunol. 2008;9:239–244. doi: 10.1038/ni1572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mempel TR, Pittet MJ, Khazaie K, et al. Regulatory T cells reversibly suppress cytotoxic T cell function independent of effector differentiation. Immunity. 2006;25:129–141. doi: 10.1016/j.immuni.2006.04.015. [DOI] [PubMed] [Google Scholar]
- 39.Khazaie K, von Boehmer H. The impact of CD4+ CD25+ Treg on tumor specific CD8+ T cell cytotoxicity and cancer. Semin Cancer Biol. 2006;16:124–136. doi: 10.1016/j.semcancer.2005.11.006. [DOI] [PubMed] [Google Scholar]
- 40.Cao X, Cai SF, Fehniger TA, et al. Granzyme B and perforin are important for regulatory T cell-mediated suppression of tumour clearance. Immunity. 2007;27:635–646. doi: 10.1016/j.immuni.2007.08.014. [DOI] [PubMed] [Google Scholar]
- 41.You S, Poulton L, Cobbold S, et al. Key role of the GITR/GITRLigand pathway in the development of murine autoimmune diabetes: a potential therapeutic target. PLoS One. 2009;4:7848. doi: 10.1371/journal.pone.0007848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Yu P, Lee Y, Liu W, et al. Intratumor depletion of CD4+ cells unmasks tumor immunogenicity leading to the rejection of late-stage tumors. J Exp Med. 2005;201:779–791. doi: 10.1084/jem.20041684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Larsen CP, Elwood ET, Alexander DZ, et al. Long-term acceptance of skin and cardiac allografts after blocking CD40 and CD28 pathways. Nature. 1996;381:434–438. doi: 10.1038/381434a0. [DOI] [PubMed] [Google Scholar]
- 44.Monk NJ, Hargreaves RE, Marsh JE, et al. Fc-dependent depletion of activated T cells occurs through CD40L-specific antibody rather than costimulation blockade. Nat Med. 2003;10:1275–1280. doi: 10.1038/nm931. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.